Professional Documents
Culture Documents
Cyclophosphamide Docetaxel Epirubicin100 Fluorouracil Pertuzumab Trastuzumab FEC T HP
Cyclophosphamide Docetaxel Epirubicin100 Fluorouracil Pertuzumab Trastuzumab FEC T HP
Uploaded by
padmashreem21Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cyclophosphamide Docetaxel Epirubicin100 Fluorouracil Pertuzumab Trastuzumab FEC T HP
Cyclophosphamide Docetaxel Epirubicin100 Fluorouracil Pertuzumab Trastuzumab FEC T HP
Uploaded by
padmashreem21Copyright:
Available Formats
Chemotherapy Protocol
BREAST CANCER
CYCLOPHOSPHAMIDE-DOCETAXEL-EPIRUBICIN (100)- FLUOROURACIL-
PERTUZUMAB-TRASTUZUMAB
(FE100CT-HP)
Regimen
• Breast Cancer – Cyclophosphamide-Docetaxel-Epirubicin (100)-Fluorouracil-
Pertuzumab-Trastuzumab (FE100CT-HP)
Indication
• Neo-adjuvant / adjuvant therapy of breast cancer
• WHO Performance status 0, 1, 2
Toxicity
Drug Adverse Effect
Cyclophosphamide Dysuria, haemorrhagic cystitis, taste disturbances
Docetaxel Hypersensitivity, fluid retention, neuropathy, joint pains, nail
changes, fatigue
Epirubicin Cardio-toxicity, urinary discolouration (red)
Fluorouracil Diarrhoea, stomatitis
Pertuzumab Diarrhoea, hypersensitivity reactions, headache, reduced
appetite, dyspnoea, cough, vomiting, nausea, constipation,
rash, pain, oedema, fatigue, asthenia, cardiotoxicity
Trastuzumab Cardio toxicity, acute respiratory distress syndrome, infusion
related effects
The adverse effects listed are not exhaustive. Please refer to the relevant Summary
of Product Characteristics for full details.
The diarrhoea can be severe in patients treated with pertuzumab. It is important to
ensure patients are given appropriate therapy for the treatment of diarrhoea. This is
not included in the regimen on Aria and must be added from the support folder.
Monitoring
Regimen
• FBC, U&E’s and LFT’s prior to cycles 1 to 8 inclusive. During the
administration of trastuzumab with pertuzumab alone this may be reduced to
every three months.
• Ensure adequate cardiac function before and at regular intervals during
treatment. Baseline LVEF should be measured, particularly in patients with a
Version 1.1 (Feb 2020) Page 1 of 17
Breast–Cyclophosphamide-Docetaxel-Epirubicin (100)-Fluorouracil-Pertuzumab-Trastuzumab (FE100CTHP)
history of cardiac problems or in the elderly. An echocardiogram should be
conducted before cycle four and then three monthly thereafter.
• HER2 status before initiating therapy
• Patients with complete or partial dihydropyrimidine dehydrogenase (DPD)
deficiency are at increased risk of severe and fatal toxicity during treatment
with fluorouracil. All patients should be tested for DPD deficiency before
initiation (cycle 1) to minimise the risk of these reactions
Dose Modifications
The dose modifications listed are for haematological, liver and renal function only.
Dose adjustments may be necessary for other toxicities as well.
In principle all dose reductions due to adverse drug reactions should not be re-
escalated in subsequent cycles without consultant approval. It is also a general rule
for chemotherapy that if a third dose reduction is necessary treatment should be
stopped. The following guidelines apply to chemotherapy only.
Please discuss all dose reductions / delays with the relevant consultant before
prescribing if appropriate. The approach may be different depending on the clinical
circumstances. The following is a general guide only.
Haematological
Prior to prescribing the following treatment criteria must be met on day 1 of
treatment.
Criteria Eligible Level
Neutrophils equal to or more than 1x109/L
Platelets equal to or more than 100x109/L
Consider blood transfusion if patient symptomatic of anaemia or has a haemoglobin
of less than 8g/dL (80g/l)
In the adjuvant / neo-adjuvant setting always check with the relevant
consultant before delaying or reducing the dose in response to a toxicity.
For the FEC arm of treatment consider delaying treatment for 7 days to allow the
platelets and neutrophils to be 100x109/L and 1x109/L or above respectively. Always
check with the relevant consultant before prescribing a dose reduction or delay.
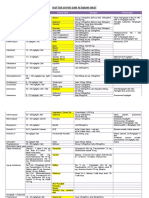
For docetaxel the following table applies.
Version 1.1 (Feb 2020) Page 2 of 17
Breast–Cyclophosphamide-Docetaxel-Epirubicin (100)-Fluorouracil-Pertuzumab-Trastuzumab (FE100CTHP)
Previous Docetaxel Dose
2
Toxicity Grade 100mg/m 75mg/m2 60mg/m2
(NCI-CTC)
1 100mg/m2 75mg/m2 60mg/m2
Delay until Delay until
Delay until grade
2 grade 1 then grade 1 then
1 then 75mg/m2
100mg/m2 60mg/m2
Neutropenia Delay until Delay until
Delay until grade
3 grade 1 then grade 1 then
1 then 75mg/m2
100mg/m2 60mg/m2
Delay until
Delay until grade
4 grade 1 then Stop
1 then 60mg/m2
75mg/m2
Delay until
Delay until grade
3 grade 1 then Stop
1 then 60mg/m2
Febrile 75mg/m2
Neutropenia Delay until
Delay until grade
4 grade 1 then Stop
1 then 60mg/m2
75mg/m2
Greater than
or equal to 100mg/m2 75mg/m2 60mg/m2
100x109/L
Delay until Delay until
Platelets
greater than or greater than or
Less than
9 equal to equal to Stop
100x10 /L
100x109/L then 100x109/L then
75mg/m2 60mg/m2
No dose modifications for haematological toxicity are necessary for pertuzumab or
trastuzumab. If treatment is not tolerated it should be stopped.
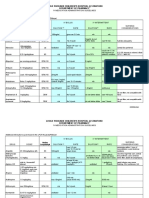
Kidney Impairment
Drug Creatinine Clearance (ml/min) Dose (% of original
dose)
more than 20 100
Cyclophosphamide 10-20 75
Less than 10 50
Docetaxel No dose adjustment necessary
Epirubicin Dose reduce in severe impairment only
Fluorouracil Consider dose reduction in severe renal impairment only
The safety and efficacy of pertuzumab has not been
Pertuzumab
established in renal impairment
Trastuzumab No dose adjustment necessary
Version 1.1 (Feb 2020) Page 3 of 17
Breast–Cyclophosphamide-Docetaxel-Epirubicin (100)-Fluorouracil-Pertuzumab-Trastuzumab (FE100CTHP)
Liver Impairment
Drug Recommendation
Cyclophosphamide Dose reduction may not be necessary
Bilirubin (umol/L) Dose (% of original)
Epirubicin 24-51 50
52-85 25
85 or greater Contra-indicated
If the AST 2-4xULN give 50% of the dose, then if then
AST is greater than 4xULN then give 25% dose
Drug Bilirubin AST/ALT Alk Phos Dose
(μmol/L) (units) (units) (% of original
dose)
1.5xULN 2.5xULN
Docetaxel N/A and Give 75%
or greater or greater
Greater
3.5xULN 6xULN or Not
than and/or and
or greater greater Recommended
ULN
Drug Bilirubin AST/ALT Dose
µmol/L units (%of original
dose)
Less than 85 Less than 180 100%
More than 85 or More than 180 CI
Fluorouracil In moderate hepatic impairment reduce the initial dose by one
third. In severe hepatic impairment reduce initial dose by one
half. These doses may be increased if no toxicity occurs
Drug Recommendation
The safety and efficacy of pertuzumab has not been
Pertuzumab
established in hepatic impairment
No dose adjustment necessary
Trastuzumab
Other
Dose reductions or interruptions in therapy are not necessary for those toxicities that
are considered unlikely to be serious or life threatening. For example, alopecia,
altered taste or nail changes.
Docetaxel
Peripheral neuropathy at NCI-CTC grade 3 should result in a dose reduction from
100mg/m2 to 75mg/m2 or 75mg/m2 to 60mg/m2 depending on the dose given in the
previous cycle. If the NCI-CTC grade 3 neuropathy occurred at doses lower than
100mg/m2 or a NCI-CTC grade 4 toxicity develops CONSIDER stopping treatment.
Version 1.1 (Feb 2020) Page 4 of 17
Breast–Cyclophosphamide-Docetaxel-Epirubicin (100)-Fluorouracil-Pertuzumab-Trastuzumab (FE100CTHP)
Excessive tearing / lacrimation are related to cumulative docetaxel doses and occur
after a median of 400mg/m². Symptomatic treatment with hypromellose 0.3% eye
drops four times a day may help. However, if the ocular irritation continues reduce
the docetaxel dose to 80% of the original dose in the first instance.
Delay the docetaxel where a NCI-CTC grade 3 cutaneous toxicity is present on day
one of the cycle until it resolves to NCI-CTC grade 1 or below. The subsequent
doses of docetaxel should be reduced to from 100mg/m2 to 75mg/m2 or from
75mg/m2 to 60mg/m2. If it occurs with a dose of 60mg/m2 or if there is no recovery
after two weeks, docetaxel treatment should be stopped. Where a NCI-CTC grade 3
cutaneous toxicity occurs between cycles with recovery by day one then reduce the
docetaxel dose as described. Docetaxel should be stopped in response to a NCI-
CTC grade 4 cutaneous toxicity.
Epirubicin
Discontinue epirubicin if cardiac failure develops.
Pertuzumab
The diarrhoea can be severe in patients treated with pertuzumab. It is important to
ensure patients are given appropriate therapy for the treatment of diarrhoea. This is
not included in the regimen on Aria and must be added from the support folder.
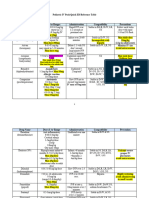
Pertuzumab and Trastuzumab
Cardiac
The LVEF should be fifty or above before starting cycle one of pertuzumab and
trastuzumab.
Subsequent Echocardiograms
The flow chart below describes the process to be followed if there is an
asymptomatic decline in LVEF during pertuzumab and trastuzumab treatment. This
is taken from the study protocol as used in the reference section. Study treatment
refers to pertuzumab and trastuzumab.
Version 1.1 (Feb 2020) Page 5 of 17
Breast–Cyclophosphamide-Docetaxel-Epirubicin (100)-Fluorouracil-Pertuzumab-Trastuzumab (FE100CTHP)
In general patients who develop symptomatic cardiac dysfunction should have
pertuzumab and trastuzumab discontinued, be commenced on ACE inhibitor therapy
and be referred to a cardiologist. Further treatment should be discussed with the
relevant oncology consultant.
Version 1.1 (Feb 2020) Page 6 of 17
Breast–Cyclophosphamide-Docetaxel-Epirubicin (100)-Fluorouracil-Pertuzumab-Trastuzumab (FE100CTHP)
Regimen
The complete course of FE100C is always administered first and is followed by
docetaxel, pertuzumab and trastuzumab.
FE100C 21 day cycle for cycles 1, 2, 3
Drug Dose Days Administration
Cyclophosphamide 500mg/m2 1 Intravenous bolus
Epirubicin 100mg/m² 1 Intravenous bolus
Fluorouracil 500mg/m² 1 Intravenous bolus
Followed by;
Cycle 4
Drug Dose Days Administration
Intravenous infusion in 250ml sodium
Docetaxel 75mg/m2 1
chloride 0.9% over 60 minutes
Intravenous infusion in 250ml sodium
Pertuzumab 840mg 1
chloride 0.9% over 60 minutes
Intravenous infusion in 250ml sodium
Trastuzumab 8mg/kg 1
chloride 0.9% over 90 minutes
Followed by;
Cycle 5, 6, 7
Drug Dose Days Administration
2* Intravenous infusion in 250ml sodium
Docetaxel 75mg/m 1
chloride 0.9% over 60 minutes
Intravenous infusion in 250ml sodium
Pertuzumab 420mg 1
chloride 0.9% over 30 minutes
Intravenous infusion in 250ml sodium
Trastuzumab 6mg/kg 1
chloride 0.9% over 30 minutes
*The dose of docetaxel can be increased to 100mg/m2 if the patient tolerates
75mg/m2
Cycles 8-21 inclusive
Drug Dose Days Administration
Intravenous infusion in 250ml sodium
Pertuzumab 420mg 1
chloride 0.9% over 30 minutes
Intravenous infusion in 250ml sodium
Trastuzumab 6mg/kg 1
chloride 0.9% over 30 minutes
Version 1.2 (November 2020) Page 7 of 17
Breast–Cyclophosphamide-Docetaxel-Epirubicin (100)-Fluorouracil-Pertuzumab-Trastuzumab (FE100CTHP)
Dose Information
• Cyclophosphamide will be dose banded in accordance with the national dose
bands (20PM).
• Docetaxel will be dose banded in accordance with the national dose
bands(20mg/ml).
• The dose of docetaxel may be increased to 100mg/m2 from cycle five
onwards if well tolerated.
• Docetaxel induced fluid retention can lead to weight gain. This is not a reason
to alter the doses
• Epirubicin will be dose banded in accordance with the national dose bands
(2PM).
• The maximum lifetime cumulative dose of epirubicin is 900mg/m².
• Fluorouracil will be dose banded in accordance with the national dose bands
(25PM).
• If the time between two sequential infusions of pertuzumab is less than six
weeks, the 420mg dose should be administered as soon as possible without
regard to the next planned dose. If the time between two sequential infusions
is 6 weeks or more, the initial loading dose of 840mg should be re-
administered as a 60 minute intravenous infusion followed every 3 weeks
thereafter by a maintenance dose of 420 mg administered over a period of 30
to 60 minutes.
• Trastuzumab will be dose rounded to the nearest 50mg (up if halfway)
• If the patient misses a dose of trastuzumab by fourteen days or less, then the
usual maintenance dose of 6mg/kg should be given as soon as possible. Do
not wait until the next planned cycle. Subsequent maintenance doses should
be given according to the previous schedule
• If the patient misses a dose of trastuzumab by more than fourteen days, a re-
loading dose of 8mg/kg should be given over 90 minutes. Subsequent
maintenance doses should then be given every 21 days from that point
Administration Information
• Hypersensitivity reactions tend to occur with the first or second infusion of
docetaxel. Docetaxel infusion should not be interrupted for minor symptoms
such as flushing or localised rashes. Immediately discontinue the infusion for
severe reactions which include profound hypotension, bronchospasm and
generalised erythema.
• Docetaxel doses of more than 200mg should be diluted in 500ml sodium
chloride 0.9% (maximum concentration 0.74mg/ml)
Version 1.2 (November 2020) Page 8 of 17
Breast–Cyclophosphamide-Docetaxel-Epirubicin (100)-Fluorouracil-Pertuzumab-Trastuzumab (FE100CTHP)
• Pertuzumab has been associated with hypersensitivity and infusion related
reactions. Patients should be observed for 60 minutes after the first infusion
and for 30 – 60 minutes after subsequent infusions. If patients have tolerated
the first two infusions with no infusion related reactions consideration can be
given to reducing this observation period.
• Trastuzumab is associated with hypersensitivity reactions. The SPC
recommends patients should be observed for six hours following the start of
the first infusion of trastuzumab and for two hours following the start of
subsequent infusions. In practice these times have been reduced. If the
patient has tolerated the first two infusions with no infusion related effects
consideration can be given to reducing or stopping this observation period.
Extravasation
• Cyclophosphamide – neutral
• Docetaxel – exfoliant
• Epirubicin – vesicant
• Fluorouracil – inflammitant
• Pertuzumab – neutral
• Trastuzumab - neutral
Additional Therapy
• FE100C antiemetics day 1
15-30 minutes prior to chemotherapy;
- dexamethasone 8mg oral or intravenous
- ondansetron 8mg oral or intravenous
As take home medication
- dexamethasone 4mg twice a day for 3 days oral
- metoclopramide 10mg three times a day when required oral
- ondansetron 8mg twice a day for 3 days oral
Growth factor according to local formulary choice. For example;
- filgrastim or bioequivalent 30 million units once a day subcutaneous for five
days starting on day five of the cycle
- lenograstim or bioequivalent 33.6 million units once a day subcutaneous for
five days starting on day five of the cycle
- pegfilgrastim or bioequivalent 6mg once a day subcutaneous on day two of
the cycle
Version 1.2 (November 2020) Page 9 of 17
Breast–Cyclophosphamide-Docetaxel-Epirubicin (100)-Fluorouracil-Pertuzumab-Trastuzumab (FE100CTHP)
Docetaxel
15-30 minutes before chemotherapy
- metoclopramide 10mg oral or intravenous
As take home medication
- metoclopramide 10mg three times a day when required oral
• To prevent fluid retention and hypersensitivity reactions prescribe
dexamethasone 8mg twice a day oral for three days starting 24 hours before
docetaxel administration. On the occasions where individuals attend for
treatment and have forgotten to take the dexamethasone pre-medication
administer dexamethasone 20mg as a once only dose intravenous bolus. The
patient should be counselled to take the dexamethsone 8mg twice a day the
following day.
• Growth factor according to local formulary choice. For example;
- filgrastim or bioequivalent 30 million units once a day subcutaneous for
seven days starting on day three of the cycle
- lenograstim or bioequivalent 33.6 million units once a day subcutaneous
for seven days starting on day three of the cycle
- pegfilgrastim or bioequivalent 6mg once a day subcutaneous on day two
of the cycle
• For treatment of pertuzumab or trastuzumab infusion reactions ‘once only
when required’ doses of the following should be prescribed;
- chlorphenamine 10mg intravenous
- hydrocortisone 100mg intravenous
- paracetamol 1000mg once oral
• Mouthwashes according to local or national policy on the treatment of
mucositis
• Gastric protection with a proton pump inhibitor or a H2 antagonist may be
considered in patients considered at high risk of GI ulceration or bleed.
References
1.von Minckwitz G, Proctor M, de Azambuja et al. Adjuvant pertuzumab and trastuzumab in early HER 2 positive
breast cancer. N Engl J Med 2017; 377 (2): 122-131.
2. Ramshorst M, van der Voot A, van Werkhoven E et al. Neoadjuvant chemotherapy with or without anthracyclines
in the presence of dual HER2 blockade for HER2-positive breast cancer (TRAIN-2): a multicentre, open-label,
randomised, phase 3 trial. Lancet Oncology 2018: 19 (12); 1630-1640
Version 1.2 (November 2020) Page 10 of 17
Breast–Cyclophosphamide-Docetaxel-Epirubicin (100)-Fluorouracil-Pertuzumab-Trastuzumab (FE100CTHP)
REGIMEN SUMMARY
Cyclophosphamide-Docetaxel-Epirubicin (100)-Fluorouracil-Pertuzumab-
Trastuzumab (FE100CT-HP)
FE100C
Cycle 1, 2 Day 1
1. Dexamethasone 8mg oral or intravenous
2. Ondansetron 8mg oral or intravenous
3. Epirubicin 100mg/m² intravenous bolus over 10 minutes
4. Fluorouracil 500mg/m² intravenous bolus over 10 minutes
5. Cyclophosphamide 500mg/m² intravenous bolus over 10 minutes
Take Home Medicines
6. Dexamethasone 4mg twice a day for 3 days oral starting on day two of the cycle
Administration Instructions
Take 4mg twice a day (morning and lunch) for 3 days starting on day two of the cycle
7. Metoclopramide 10mg three times a day when required oral
Administration Instructions
When required for nausea. Please supply five days or an original pack if appropriate.
8. Ondansetron 8mg twice a day for 3 days oral starting on the evening of day one
of the cycle
Administration Instructions
Take 8mg twice a day for three days starting on the evening of day one of the cycle
9. Growth factor according to local formulary choice.
Administration Instructions
Dispense according to local formulary choices;
- filgrastim or bioequivalent 30 million units once a day subcutaneous for 5 days starting on day 5 of the cycle
- lenograstim or bioequivalent 33.6million units once a day subcutaneous for 5 days starting on day 5 of the
cycle
- pegfilgrastim or bioequivalent 6mg once a day subcutaneous on day 2 of the cycle
FE100C
Cycle 3 Day 1
10. Dexamethasone 8mg oral or intravenous
11. Ondansetron 8mg oral or intravenous
12. Epirubicin 100mg/m² intravenous bolus over 10 minutes
13. Fluorouracil 500mg/m² intravenous bolus over 10 minutes
14. Cyclophosphamide 500mg/m² intravenous bolus over 10 minutes
Version 1.2 (November 2020) Page 11 of 17
Breast–Cyclophosphamide-Docetaxel-Epirubicin (100)-Fluorouracil-Pertuzumab-Trastuzumab (FE100CTHP)
Take Home Medicines
14. Dexamethasone 4mg twice a day for 3 days oral starting on day two of the cycle
Administration Instructions
Take 4mg twice a day (morning and lunch) for 3 days starting on day two of the cycle
15. Metoclopramide 10mg three times a day when required oral
Administration Instructions
When required for nausea. Please supply five days or an original pack if appropriate
16. Ondansetron 8mg twice a day for 3 days oral starting on the evening of day one
of treatment
Administration Instructions
Take 8mg twice a day for three days starting on the evening of day one of the cycle
17. Growth factor according to local formulary choice.
Administration Instructions
Dispense according to local formulary choices;
- filgrastim or bioequivalent 30million units once a day subcutaneous for 5 days starting on day 5 of the cycle
- lenograstim or bioequivalent 33.6million units once a day subcutaneous for 5 days starting on day 5 of the
cycle
- pegfilgrastim or bioequivalent 6mg once a day subcutaneous on day 2 of the cycle
18. Dexamethasone 8mg twice a day oral for three days starting the day before the
docetaxel infusion
Administration Instructions
This is the supply for the next cycle. Take in the morning and at lunchtime
Docetaxel-Pertuzumab-Trastuzumab
Cycle 4 Day Minus 1
19. Dexamethasone 8mg twice a day oral*
Cycle 4 Day 1
20. Pertuzumab 840mg intravenous infusion in 250ml sodium chloride 0.9% over 60
minutes
21. Administration Instructions
The first infusion of pertuzumab should be given over 60 minutes. If this is well tolerated subsequent infusions
may be given over 30 minutes
22. Trastuzumab 8mg/kg intravenous infusion in 250ml sodium chloride 0.9% over 90
minutes
Administration Instructions
The first infusion of trastuzumab must be administered over 90 minutes. If this is well tolerated administer
subsequent infusions over 30 minutes
23. Metoclopramide 10mg oral or intravenous
24. Dexamethasone 8mg twice a day oral (from TTO)*
Administration Instructions
Ensure the patient has taken the dexamethasone pre-medication the day before and the day of docetaxel
administration (and the day after). On the occasions where individuals attend for treatment and have forgotten to
take the dexamethasone pre-medication administer dexamethasone 20mg (or equivalent dose) IV stat 15-30
minutes before chemotherapy. If the patient has already taken a dose of dexamethasone do not administer this
dose
Version 1.2 (November 2020) Page 12 of 17
Breast–Cyclophosphamide-Docetaxel-Epirubicin (100)-Fluorouracil-Pertuzumab-Trastuzumab (FE100CTHP)
25. Docetaxel 75mg/m² intravenous infusion in 250ml sodium chloride 0.9% over 60
minutes
Administration Instructions
Ensure the patient has taken the dexamethasone pre-medication the day before and the day of docetaxel
administration (and the day after). On the occasions where individuals attend for treatment and have forgotten to
take the dexamethasone pre-medication administer dexamethasone 20mg (or equivalent dose) IV stat 15-30
minutes before chemotherapy.
26. Chlorphenamine 10mg intravenous when required for infusion related reactions
27. Hydrocortisone 100mg intravenous when required for infusion related reactions
28. Paracetamol 1000mg oral when required for infusion related reactions
Administration Instructions
Please check if the patient has taken paracetamol. Maximum dose is 4g per 24 hours. There should be 4 hours
between doses
Take Home Medicines
29. Dexamethasone 8mg twice daily oral for 3 days starting the day before the
docetaxel infusion
Administration Instructions
This is the supply for the next cycle. Take in the morning and at lunchtime
30. Metoclopramide 10mg three times a day oral when required
Administration Instructions
When required for nausea. Please supply five days or an original pack if appropriate.
31. Growth factor according to local formulary choice.
Administration Instructions
Dispense according to local formulary choices;
-filgrastim or bioequivalent 30 million units once a day subcutaneous for 7 days starting on day 3 of the cycle
-lenograstim or bioequivalent 33.6 million units once a day subcutaneous for 7 days starting on day 3 of the
cycle
-pegfilgrastim or bioequivalent 6mg once a day subcutaneous on day 2 of the cycle
Cycle 5, 6 Day Minus 1
32. Dexamethasone 8mg twice a day oral*
Cycle 5, 6 Day 1
33. Pertuzumab 420mg intravenous infusion in 250ml sodium chloride 0.9% over 60
minutes
Administration Instructions
The first infusion of pertuzumab should be given over 60 minutes. If this is well tolerated subsequent infusions
may be given over 30 minutes
34. Trastuzumab 6mg/kg intravenous infusion in 250ml sodium chloride 0.9% over 90
minutes
Administration Instructions
The first infusion of trastuzumab must be administered over 90 minutes. If this is well tolerated administer
subsequent infusions over 30 minutes
35. Metoclopramide 10mg oral or intravenous
Version 1.2 (November 2020) Page 13 of 17
Breast–Cyclophosphamide-Docetaxel-Epirubicin (100)-Fluorouracil-Pertuzumab-Trastuzumab (FE100CTHP)
36. Dexamethasone 8mg twice a day oral (from TTO)*
Administration Instructions
Ensure the patient has taken the dexamethasone pre-medication the day before and the day of docetaxel
administration (and the day after). On the occasions where individuals attend for treatment and have forgotten to
take the dexamethasone pre-medication administer dexamethasone 20mg (or equivalent dose) IV stat 15-30
minutes before chemotherapy. If the patient has already taken a dose of dexamethasone do not administer this
dose
37. Warning – Check Docetaxel Dose
Administration Instructions
The dose of docetaxel may be increased to 100mg/m2 in those individuals who tolerate the 75mg/m2 dose with
no issues. The dose in ARIA is set at 75mg/m2
38. Docetaxel 75mg/m² intravenous infusion in 250ml sodium chloride 0.9% over 60
minutes
Administration Instructions
Ensure the patient has taken the dexamethasone pre-medication the day before and the day of docetaxel
administration (and the day after). On the occasions where individuals attend for treatment and have forgotten to
take the dexamethasone pre-medication administer dexamethasone 20mg (or equivalent dose) IV stat 15-30
minutes before chemotherapy.
39. Chlorphenamine 10mg intravenous when required for infusion related reactions
40. Hydrocortisone 100mg intravenous when required for infusion related reactions
41. Paracetamol 1000mg oral when required for infusion related reactions
Administration Instructions
Please check if the patient has taken paracetamol. Maximum dose is 4g per 24 hours. There should be 4 hours
between doses
Take Home Medicines
42. Metoclopramide 10mg three times a day oral when required
Administration Instructions
When required for nausea. Please supply five days or an original pack if appropriate
43. Dexamethasone 8mg twice a day oral for 3 days starting the day before the
docetaxel infusion.
Administration Instructions
This is the supply for the next cycle. Take in the morning and at lunchtime
44. Growth factor according to local formulary choice.
Administration Instructions
Dispense according to local formulary choices;
- filgrastim or bioequivalent 30 million units once a day subcutaneous for 7 days starting on day 3 of the cycle
- lenograstim or bioequivalent 33.6 million units once a day subcutaneous for 7 days starting on day 3 of the
cycle
- pegfilgrastim or bioequivalent 6mg once a day subcutaneous on day 2 of the cycle
Cycle 7 Day Minus 1
45. Dexamethasone 8mg twice a day oral*
Cycle 7 Day 1
46. Pertuzumab 420mg intravenous infusion in 250ml sodium chloride 0.9% over 60
minutes
Administration Instructions
The first infusion of pertuzumab should be given over 60 minutes. If this is well tolerated subsequent infusions
may be given over 30 minutes
Version 1.2 (November 2020) Page 14 of 17
Breast–Cyclophosphamide-Docetaxel-Epirubicin (100)-Fluorouracil-Pertuzumab-Trastuzumab (FE100CTHP)
47. Trastuzumab 6mg/kg intravenous infusion in 250ml sodium chloride 0.9% over 90
minutes
Administration Instructions
The first infusion of trastuzumab must be administered over 90 minutes. If this is well tolerated administer
subsequent infusions over 30 minutes
48. Metoclopramide 10mg oral or intravenous
49. Dexamethasone 8mg twice a day oral (from TTO)*
Administration Instructions
Ensure the patient has taken the dexamethasone pre-medication the day before and the day of docetaxel
administration (and the day after). On the occasions where individuals attend for treatment and have forgotten to
take the dexamethasone pre-medication administer dexamethasone 20mg (or equivalent dose) IV stat 15-30
minutes before chemotherapy. If the patient has already taken a dose of dexamethasone do not administer this
dose
50. Docetaxel 75mg/m² intravenous infusion in 250ml sodium chloride 0.9% over 60
minutes
Administration Instructions
Ensure the patient has taken the dexamethasone pre-medication the day before and the day of docetaxel
administration (and the day after). On the occasions where individuals attend for treatment and have forgotten to
take the dexamethasone pre-medication administer dexamethasone 20mg (or equivalent dose) IV stat 15-30
minutes before chemotherapy.
51. Chlorphenamine 10mg intravenous when required for infusion related reactions
52. Hydrocortisone 100mg intravenous when required for infusion related reactions
53. Paracetamol 1000mg oral when required for infusion related reactions
Administration Instructions
Please check if the patient has taken paracetamol. Maximum dose is 4g per 24 hours. There should be 4 hours
between doses
Take Home Medicines
54. Metoclopramide 10mg three times a day oral when required
Administration Instructions
When required for nausea. Please supply five days or an original pack if appropriate
55. Growth factor according to local formulary choice.
Administration Instructions
Dispense according to local formulary choices;
- filgrastim or bioequivalent 30 million units once a day subcutaneous for 7 days starting on day 3 of the cycle
- lenograstim or bioequivalent 33.6 million units once a day subcutaneous for 7 days starting on day 3 of the
cycle
- pegfilgrastim or bioequivalent 6mg once a day subcutaneous on day 2 of the cycle
Cycle 8 – 21 (inclusive)
Day 1
56. Pertuzumab 420mg intravenous infusion in 250ml sodium chloride 0.9% over 60
minutes
Administration Instructions
The first infusion of pertuzumab should be given over 60 minutes. If this is well tolerated subsequent infusions
may be given over 30 minutes
57. Trastuzumab 6mg/kg intravenous infusion in 250ml sodium chloride 0.9% over 90
minutes
Administration Instructions
The first infusion of trastuzumab must be administered over 90 minutes. If this is well tolerated administer
subsequent infusions over 30 minutes
Version 1.2 (November 2020) Page 15 of 17
Breast–Cyclophosphamide-Docetaxel-Epirubicin (100)-Fluorouracil-Pertuzumab-Trastuzumab (FE100CTHP)
58. Chlorphenamine 10mg intravenous when required for infusion related reactions
59. Hydrocortisone 100mg intravenous when required for infusion related reactions
60. Paracetamol 1000mg oral when required for infusion related reactions
Administration Instructions
Please check if the patient has taken paracetamol. Maximum dose is 4g per 24 hours. There should be 4 hours
between doses
* In Aria Planner the dexamethasone 8mg twice daily will appear on days 1, 2, 3 of treatment. This is the supply for
the next cycle. The administration instructions reflect this. On the last cycle no dexamethasone will appear for
prescribing.
Version 1.2 (November 2020) Page 16 of 17
Breast–Cyclophosphamide-Docetaxel-Epirubicin (100)-Fluorouracil-Pertuzumab-Trastuzumab (FE100CTHP)
DOCUMENT CONTROL
Version Date Amendment Written By Approved By
Updated monitoring with DPD Donna Kimber
Rebecca Wills
1.2 Nov 2020 testing Pharmacy
Pharmacist
Coding removed Technician
Admin instructions updated for
Rebecca Wills Dr Deborah Wright
1.1 Feb 2020 GCSF following docetaxel in the
Pharmacist Pharmacist
regimen summary
Dr Sanjay Raj
Dr Deborah Wright
1 Nov 2019 None Consultant Clinical
Pharmacist
Oncologist
This chemotherapy protocol has been developed as part of the chemotherapy
electronic prescribing project. This was and remains a collaborative project that
originated from the former CSCCN. These documents have been approved on behalf
of the following Trusts;
Hampshire Hospitals NHS Foundation Trust
NHS Isle of Wight
Portsmouth Hospitals NHS Trust
Salisbury NHS Foundation Trust
University Hospital Southampton NHS Foundation Trust
Western Sussex Hospitals NHS Foundation Trust
All actions have been taken to ensure these protocols are correct. However, no
responsibility can be taken for errors which occur as a result of following these
guidelines.
Version 1.2 (November 2020) Page 17 of 17
Breast–Cyclophosphamide-Docetaxel-Epirubicin (100)-Fluorouracil-Pertuzumab-Trastuzumab (FE100CTHP)
You might also like
- Pediatrics Drug Doses - DocToon PDFDocument49 pagesPediatrics Drug Doses - DocToon PDFBharat Jamod100% (1)
- History Indian ViewDocument12 pagesHistory Indian ViewSumbula RahmanNo ratings yet
- Brain Cancer Treatment Regimens (Part 1 of 5)Document5 pagesBrain Cancer Treatment Regimens (Part 1 of 5)Rubana Reaz TanaNo ratings yet
- Docetaxel-Gemcitabinev1 2Document8 pagesDocetaxel-Gemcitabinev1 2Salman FaridziNo ratings yet
- In PDoxorubicin Ifosfamide Ver 1Document7 pagesIn PDoxorubicin Ifosfamide Ver 1Huỳnh Minh ĐôngNo ratings yet
- Icm - Infusion Prescribing InfoDocument2 pagesIcm - Infusion Prescribing InfoNatia UtmelidzeNo ratings yet
- Huitm Paediatrics Antimicrobial Dosing GuideDocument6 pagesHuitm Paediatrics Antimicrobial Dosing Guidedrnurulhikmah.kkiatuaranNo ratings yet
- Temozolomide RT 7 DayDocument6 pagesTemozolomide RT 7 Daysoomro rehmanNo ratings yet
- Temozolomide Concomitant NHSDocument4 pagesTemozolomide Concomitant NHSSyed Touseef AhmedNo ratings yet
- Carboplatin PaclitaxelgynaeDocument5 pagesCarboplatin PaclitaxelgynaefazarNo ratings yet
- CMSCN R IgevDocument2 pagesCMSCN R Igevdiana8827534No ratings yet
- Drug DilutionDocument4 pagesDrug Dilutiondr.rrajesh92No ratings yet
- Leukemia Treatment Regimens 7937Document3 pagesLeukemia Treatment Regimens 7937Irfan FathurrahmanNo ratings yet
- Albumin ProtocolDocument2 pagesAlbumin ProtocolNehal ElnagarNo ratings yet
- Temozolomide 150Document6 pagesTemozolomide 150soomro rehmanNo ratings yet
- Medicamento Dosis Vxdía Presentación ComercialDocument2 pagesMedicamento Dosis Vxdía Presentación ComercialIsmal MachacaNo ratings yet
- Docetaxel Carboplatin Trastuzumab T Carbo H Breast Cancer Adjuvant ProtocolDocument14 pagesDocetaxel Carboplatin Trastuzumab T Carbo H Breast Cancer Adjuvant ProtocolsmokkerNo ratings yet
- Endometrialcarcinoma r0416 7941Document2 pagesEndometrialcarcinoma r0416 7941crisibarra911No ratings yet
- Chemotherapy Protocol: RegimenDocument10 pagesChemotherapy Protocol: RegimenparaskaushikNo ratings yet
- EC-DH Epirubicin Cyclophosphamide Followed by Docetaxel With Trastuzumab Protocol V1.1Document11 pagesEC-DH Epirubicin Cyclophosphamide Followed by Docetaxel With Trastuzumab Protocol V1.1smokkerNo ratings yet
- Daftar Dosis Dan Sediaan ObatDocument7 pagesDaftar Dosis Dan Sediaan Obatdoru ubungNo ratings yet
- Bendamustine-Rituximab NHS RegimenDocument9 pagesBendamustine-Rituximab NHS RegimenLuana MNo ratings yet
- Picu NotesDocument65 pagesPicu NotesAhmed Mohammed100% (2)
- Enoxaparin Info SheetDocument7 pagesEnoxaparin Info SheetjafarkassimNo ratings yet
- Breast Cancer RegimensDocument6 pagesBreast Cancer RegimensMohammad Arwan HamdaniNo ratings yet
- ABVDDocument3 pagesABVDEsther WanguiNo ratings yet
- GOOVCATX ProtocolDocument7 pagesGOOVCATX Protocolthanh ngôNo ratings yet
- Heparin Dose Adjustment in The Prescence of Renal ImpairmentDocument5 pagesHeparin Dose Adjustment in The Prescence of Renal ImpairmentRPR KSVNo ratings yet
- Pediatric PharmacologyDocument30 pagesPediatric PharmacologyHussamNo ratings yet
- Brentuximab-Vedotin NHS RegimenDocument6 pagesBrentuximab-Vedotin NHS RegimenLuana MNo ratings yet
- Temozolomide Adjuvant NHSDocument5 pagesTemozolomide Adjuvant NHSSyed Touseef AhmedNo ratings yet
- NAVELBINE 20 MG, 30mg CapsulesDocument2 pagesNAVELBINE 20 MG, 30mg Capsulesddandan_2No ratings yet
- CVP Plus Rituximab (R-CVP) For Lymphoma: Page 1 of 2Document2 pagesCVP Plus Rituximab (R-CVP) For Lymphoma: Page 1 of 2Andreea NeculceaNo ratings yet
- Comparison Chart:: Sodium-Glucose Co-Transporter 2 (Sglt2) InhibitorsDocument5 pagesComparison Chart:: Sodium-Glucose Co-Transporter 2 (Sglt2) InhibitorsAditya MadhavpeddiNo ratings yet
- Antibiotik: Dosis Nama Dagang Sediaan Keterangan Anak Dewasa AmoxicilinDocument6 pagesAntibiotik: Dosis Nama Dagang Sediaan Keterangan Anak Dewasa AmoxicilinaandhiiraaNo ratings yet
- Daftar Dosis Dan Sediaan Obat AnakDocument4 pagesDaftar Dosis Dan Sediaan Obat AnaklayaliaNo ratings yet
- Cisplatin-Pemetrexed (NSCLC)Document5 pagesCisplatin-Pemetrexed (NSCLC)Sindu SankarNo ratings yet
- جرعات الاطفالDocument50 pagesجرعات الاطفالWael Hamdy100% (1)
- EC-D With HP Epirubicin Cyclophosphamide Followed by Docetaxel Trastuzumab Pertuzumab Neo-Adjuvant and Adjuvant Protocol V2.1Document20 pagesEC-D With HP Epirubicin Cyclophosphamide Followed by Docetaxel Trastuzumab Pertuzumab Neo-Adjuvant and Adjuvant Protocol V2.1smokkerNo ratings yet
- Gentamicin AssignmentDocument13 pagesGentamicin Assignmentqg2dkn9zcyNo ratings yet
- Lung Cancer Treatment Regimens (Part 1 of 4)Document4 pagesLung Cancer Treatment Regimens (Part 1 of 4)Rubana Reaz TanaNo ratings yet
- DilutionDocument12 pagesDilutioncristina tina100% (1)
- Pediatric IV Push Quick ED Reference TableDocument4 pagesPediatric IV Push Quick ED Reference TableTayyab RazaNo ratings yet
- Temozolomide 200Document6 pagesTemozolomide 200soomro rehmanNo ratings yet
- GCC Anti Emetic Guidelines 2003Document2 pagesGCC Anti Emetic Guidelines 2003damondouglasNo ratings yet
- Transdermal Opioid Patches: Quick Reference Guide: Important InformationDocument2 pagesTransdermal Opioid Patches: Quick Reference Guide: Important Informationemilia_sweetyNo ratings yet
- LTC-Parkinsonism 1079Document1 pageLTC-Parkinsonism 1079DanielleNo ratings yet
- CAPIRI Capecitabine-Irinotecan (COLORECTAL CANCER)Document5 pagesCAPIRI Capecitabine-Irinotecan (COLORECTAL CANCER)Sindu SankarNo ratings yet
- Drugs & DosagesDocument29 pagesDrugs & DosagesCristina VelasquezNo ratings yet
- Revlimid-Spc enDocument100 pagesRevlimid-Spc enlamprinilNo ratings yet
- Antibiotics PDFDocument4 pagesAntibiotics PDFNilamdeen Mohamed ZamilNo ratings yet
- Antidiabetic AgentsDocument2 pagesAntidiabetic AgentsDanielleNo ratings yet
- PICU Drug Boluses: Drug Dose /KG Range Administration NotesDocument5 pagesPICU Drug Boluses: Drug Dose /KG Range Administration NotesMaria BudnicNo ratings yet
- LYRICE ProtocolDocument6 pagesLYRICE ProtocolInas UthmanNo ratings yet
- InP Cisplatin (75) Docetaxel (75) Fluorouracil (4000)Document7 pagesInP Cisplatin (75) Docetaxel (75) Fluorouracil (4000)Varun KashyapNo ratings yet
- L 51 R Hypercvad R MaDocument7 pagesL 51 R Hypercvad R MaMohamed MahmoudNo ratings yet
- Medication DilutionDocument23 pagesMedication DilutionamgdanielaNo ratings yet
- Pediatric Drug DosageDocument49 pagesPediatric Drug Dosagecarlsonrenovatio100% (3)
- Critical Care Medications: Anti-Arrhythmics Study Guide: Critical Care EssentialsFrom EverandCritical Care Medications: Anti-Arrhythmics Study Guide: Critical Care EssentialsNo ratings yet
- Work Permit System: Course Title-S 21Document77 pagesWork Permit System: Course Title-S 21ravindra dolaiNo ratings yet
- Shipping Interview Questions With AnswersDocument21 pagesShipping Interview Questions With Answerssaurabh meshramNo ratings yet
- Guia Autoaprendizaje Estudiante 8vo Grado Ingles f1 s3 PDFDocument5 pagesGuia Autoaprendizaje Estudiante 8vo Grado Ingles f1 s3 PDFmonkey dNo ratings yet
- Changing An Occupied BedDocument6 pagesChanging An Occupied BedMARY ERLYN RICARTONo ratings yet
- HSSC Paper PDF (7) - WatermarkDocument15 pagesHSSC Paper PDF (7) - WatermarkJitender TanwarNo ratings yet
- Automatic Stop OrdersDocument1 pageAutomatic Stop OrdersHartiniNo ratings yet
- New Product Development To CommercializationDocument9 pagesNew Product Development To Commercializationhellofrom theothersideNo ratings yet
- Introduction To Guidance and CounsellingDocument40 pagesIntroduction To Guidance and CounsellingMie Che Othman80% (5)
- Lesson Plan in English 8 q4Document60 pagesLesson Plan in English 8 q4Fel Mark BarcebalNo ratings yet
- (2021) Bagaimana Remaja Menjadi Peer-Counselor Di Masa PandemiDocument13 pages(2021) Bagaimana Remaja Menjadi Peer-Counselor Di Masa PandemiNyutub nyanNo ratings yet
- Phsu PHSC Phso DescriptionsDocument2 pagesPhsu PHSC Phso Descriptionsapi-660990706No ratings yet
- Fdar NCPDocument3 pagesFdar NCPjasper pachingelNo ratings yet
- Adventist Youth Honors Answer Book/Household Arts/Nutrition: WikibooksDocument8 pagesAdventist Youth Honors Answer Book/Household Arts/Nutrition: WikibooksJoey Moonga MoongaNo ratings yet
- Nwogbe Love: Career ObjectivesDocument3 pagesNwogbe Love: Career ObjectivesArthur PentaxNo ratings yet
- Targeted Drug Delivery - Concepts and DesignDocument788 pagesTargeted Drug Delivery - Concepts and Designmalin.oloier100% (1)
- Đề số 1Document4 pagesĐề số 1LanChiVũ0% (1)
- ADEA AADSAS General Instructions BookletDocument53 pagesADEA AADSAS General Instructions Bookletd_yuminNo ratings yet
- Apollo Hospitals Balance SheetDocument27 pagesApollo Hospitals Balance SheetSheik AllaudinNo ratings yet
- Advanced Nutrition Test 2023 PDFDocument3 pagesAdvanced Nutrition Test 2023 PDFajjaNo ratings yet
- Chapter I IntroductionDocument34 pagesChapter I IntroductionJamie HaravataNo ratings yet
- Dialog English NurilDocument2 pagesDialog English NurilMuhammad Nuril Wahid FauziNo ratings yet
- Emotional SobrietyDocument2 pagesEmotional SobrietyUrsulaNo ratings yet
- 1 s2.0 S105687271930621X MainDocument8 pages1 s2.0 S105687271930621X MainabganNo ratings yet
- English Project FinalDocument27 pagesEnglish Project FinalVirendra NaikNo ratings yet
- BIS&FSSAIDocument16 pagesBIS&FSSAIHency RoseNo ratings yet
- Reconstruction of The EarDocument10 pagesReconstruction of The EarFabian Camelo OtorrinoNo ratings yet
- FOP/NBC Survey On Police Officer Mental and Behavioral HealthDocument6 pagesFOP/NBC Survey On Police Officer Mental and Behavioral HealthEd PraetorianNo ratings yet
- Emergency Preparedness and Response During An Explosion/Bomb ThreatDocument11 pagesEmergency Preparedness and Response During An Explosion/Bomb ThreatI AM NOT CHINESENo ratings yet
- Assignment Individual Section 42Document3 pagesAssignment Individual Section 42Afiqah YusriNo ratings yet