Professional Documents
Culture Documents
The Future of Cystic Fibrosis Treatment From Dise
The Future of Cystic Fibrosis Treatment From Dise
Uploaded by
Alexander LozaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Future of Cystic Fibrosis Treatment From Dise
The Future of Cystic Fibrosis Treatment From Dise
Uploaded by
Alexander LozaCopyright:
Available Formats
Series
Cystic Fibrosis 3
The future of cystic fibrosis treatment: from disease
mechanisms to novel therapeutic approaches
Simon Y Graeber, Marcus A Mall
With the 2019 breakthrough in the development of highly effective modulator therapy providing unprecedented Lancet 2023; 402: 1185–98
clinical benefits for over 90% of patients with cystic fibrosis who are genetically eligible for treatment, this rare disease Published Online
has become a front runner of transformative molecular therapy. This success is based on fundamental research, September 9, 2023
https://doi.org/10.1016/
which led to the identification of the disease-causing CFTR gene and our subsequent understanding of the disease S0140-6736(23)01608-2
mechanisms underlying the pathogenesis of cystic fibrosis, working together with a continuously evolving clinical
See Comment page 1113
research and drug development pipeline. In this Series paper, we focus on advances since 2018, and remaining
This is the third in a Series of
knowledge gaps in our understanding of the molecular mechanisms of CFTR dysfunction in the airway epithelium four papers about cystic fibrosis
and their links to mucus dysfunction, impaired host defences, airway infection, and chronic inflammation of the (papers 2 and 4 are published in
lungs of people with cystic fibrosis. We review progress in (and the remaining obstacles to) pharmacological The Lancet Respiratory Medicine).
All papers in the Series are
approaches to rescue CFTR function, and novel strategies for improved symptomatic therapies for cystic fibrosis,
available at www.thelancet.com/
including how these might be applicable to common lung diseases, such as bronchiectasis and chronic obstructive series/cystic-fibrosis-2023
pulmonary disease. Finally, we discuss the promise of genetic therapies and gene editing approaches to restore CFTR Department of Pediatric
function in the lungs of all patients with cystic fibrosis independent of their CFTR genotype, and the unprecedented Respiratory Medicine,
opportunities to transform cystic fibrosis from a fatal disease to a treatable and potentially curable one. Immunology and Critical Care
Medicine (S Y Graeber MD,
M A Mall MD) and Cystic
Introduction current focus lies on gene replacement strategies for the Fibrosis Center (S Y Graeber,
The discovery of the cystic fibrosis transmembrane approximately 10% of patients who are not eligible for M A Mall), Charité–
regulator (CFTR) gene in 1989 has provided a basis for (or do not tolerate) CFTR modulator therapy and, Universitätsmedizin Berlin,
corporate member of Freie
understanding the pathogenesis of chronic progressive therefore, have the highest unmet need. This endeavour
Universität Berlin and
lung disease, which is responsible for most of the disease will be supported by advances in genetic therapy Humboldt-Universität zu
burden and shortened life expectancy in patients with approaches. Other technological advances range from Berlin, Berlin, Germany;
cystic fibrosis. Over the past four decades, the cystic multi-omics technologies that enable comprehensive German Center for Lung
Research, associated partner
fibrosis community has been dedicated to basic and studies of gene expression and function at the single cell
site, Berlin, Germany
translational research addressing the mechanisms and level, to the establishment of patient-derived model (S Y Graeber, M A Mall); Berlin
consequences of CFTR dysfunction in the lung and its systems for preclinical research and precision medicine Institute of Health at Charité–
links to a characteristic pathogenetic cascade of airway approaches, and unprecedented opportunities for gene Universitätsmedizin Berlin,
Berlin, Germany (S Y Graeber,
mucus plugging, chronic bacterial infection, and editing with the prospect of a cure. Having been
M A Mall)
inflammation that determines the clinical phenotype incorporated since 2013 into basic and translational
Correspondence to:
and outcomes of the disease. In parallel, an exemplary cystic fibrosis research, these developments have already Prof Marcus A Mall, Department
drug development pipeline has been established to led to the novel insights into pathogenetic mechanisms of Pediatric Respiratory
translate basic research findings into novel therapies and progress with therapeutic strategies discussed in Medicine, Immunology and
Critical Care Medicine, Charité–
that target each step of this cascade. This collaborative this Review, and will be an important armamentarium
Universitätsmedizin Berlin,
effort first led to the approval of therapies that improve 13353 Berlin, Germany
mucus clearance and reduce bacterial burden in the Marcus.Mall@charite.de
lungs to ease symptoms, and more recently to highly Search strategy and selection criteria
effective small-molecule CFTR-modulator drugs that We searched PubMed and ClinicalTrials.gov from Jan 1, 2003,
address the underlying cause of the disease and provide to Feb 28, 2023, and updated the search through
unprecedented clinical benefits to an increasing patient July 20, 2023, with the search terms “cystic fibrosis”, “CFTR”,
population of currently approximately 90% of patients “CFTR function”, “cystic fibrosis and mucus”, “cystic fibrosis
with cystic fibrosis and responsive CFTR genotypes.1–4 and host defense”, “cystic fibrosis and inflammation”, “CFTR
Despite this breakthrough, important knowledge gaps modulators”, “cystic fibrosis and alternative ion channels”,
and challenges remain that have to be overcome to “cystic fibrosis and gene therapy”, “cystic fibrosis and genetic
develop effective therapies for all patients with cystic therapies”, “cystic fibrosis and anti-inflammatory”, and “cystic
fibrosis independent of their individual CFTR genotypes, fibrosis and anti-infective”. Only articles written in English
including patients with cystic fibrosis from minority were included. We largely selected relevant publications and
racial and ethnic groups who are less likely to be eligible clinical trials from 2018 to 2023, but also included original
for CFTR modulators on the basis of their genotypes.5 To descriptions and highly relevant older publications.
overcome the disparities in treatment options, the
www.thelancet.com Vol 402 September 30, 2023 1185
Series
for achieving the ultimate goal of future cystic fibrosis channel that plays a key role in the transport of chloride
therapy that fully restores CFTR function and and bicarbonate across the apical membrane of epithelial
homeostasis to the lungs (and ideally other affected cells. Proper CFTR function is essential for maintaining
organs) in all people with cystic fibrosis. homeostasis in the airways and other affected organs,
including the exocrine pancreas, gastrointestinal tract,
Progress in understanding the molecular sweat glands.1,6 Early work on the structure and function
mechanisms of CFTR dysfunction of the CFTR anion channel revealed that it is composed
Breakthroughs in the development of therapies that of two transmembrane domains, two nucleotide binding
target the underlying cause of cystic fibrosis were made domains, and a regulatory domain; that it is activated by
For more on the Cystic Fibrosis
Mutation Database see http:// possible by the discovery that this disease is caused by protein kinase A-dependent phosphorylation and
www.genet.sickkids.on.ca/ mutations in the CFTR gene, which encodes an anion conductive for chloride and bicarbonate; and that CFTR-
mediated transport of these anions plays a key role in
homoeostatic regulation of fluid volume, pH, and salt
A concentration on the surface of the airways and other
Mucociliary clearance epithelia (figure 1).7–10 Over 2000 variants have been
Mucin crosslinking
identified in the CFTR gene and reported to the Cystic
HCO3– ENaC SLC26A9
Fibrosis Mutation Database, and approximately 700 have
S S been verified as disease-causing. On the basis of these
Cl– Na+ Cl– Cl– discoveries, understanding the basic molecular
mechanisms underlying how sequence variants in CFTR
can cause CFTR dysfunction became possible.11 These
CFTR TMEM16A
include deficient CFTR synthesis caused by nonsense,
frameshift, and canonical splicing mutations leading to
premature termination codons (class I mutations);
impaired folding and trafficking defects leading to few to
H20 H20 H20 H20 no CFTR channels at the cell membrane (class II
mutations); and impaired function of mutant CFTR
expressed at the cell membrane. This impaired function
CFTR
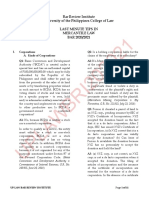
Figure 1: The molecular mechanisms and consequences of CFTR dysfunction
in cystic fibrosis airways
(A) In healthy airways, the CFTR chloride channel is mainly expressed in the
apical cell membrane of secretory cells, where it has an important role in anion
B (chloride and bicarbonate) and fluid secretion. CFTR is expressed with ENaC,
which constitutes the limiting pathway for sodium and fluid absorption.
Impaired mucociliary clearance Coordinated regulation of these processes is essential for the proper formation
of a thin protective mucus gel from mucins secreted by goblet cells and effective
Mucin crosslinking mucociliary clearance that provide an important, innate host defence
S
S
mechanism of the lung (in conjunction with macrophages patrolling airway
S
Class IV S surfaces). (B) In patients with cystic fibrosis, CFTR dysfunction can be caused by
S
S different molecular mechanisms. Mutations in CFTR can lead to premature
HCO3– ENaC SLC26A9
IL-1ß Proteases termination codons resulting in an absence of the full-length protein (class I
IL-8
Class III Cl– Na+ Cl– Cl– mutations), protein folding and trafficking defects leading to little functional
CFTR TNF-α CFTR at the apical cell membrane (class II mutations), impaired channel gating
resulting in reduced open probability (class III mutations), impaired channel
conductance (class IV mutations), a reduced number of CFTR channels caused by
alternative splicing (class V mutations), or a reduced stability and shortened
TMEM16A
half-life of CFTR channels expressed at the apical membrane (class VI
mutations). Deficient CFTR-mediated secretion of chloride, bicarbonate, and
Class VI fluid onto airway surfaces leads to the formation of hyperconcentrated and
highly viscoelastic mucus that impedes mucociliary clearance and sets the stage
H20 H20 H20 H20 for chronic bacterial infection with cystic fibrosis-associated pathogens such as
Pseudomonas aeruginosa. This infection triggers chronic airway inflammation,
including the activation of macrophages and recruitment of neutrophils into
Class II the airway lumen, leading to the release of proinflammatory cytokines
(eg, IL-1β, IL-8, and TNF-α), reactive oxygen species that further increase mucus
Class V viscoelasticity via disulfide mucin cross-linking, and proteases such as neutrophil
elastase, which play an important role in structural lung damage and lung
Class I function decline. Figure created with BioRender.com. CFTR=cystic fibrosis
transmembrane conductance regulator. ENaC=epithelial sodium channel.
SLC26A9=solute carrier family 26 member 9. TMEM16A=transmembrane
member 16A. IL=interleukin. TNF=tumour necrosis factor.
1186 www.thelancet.com Vol 402 September 30, 2023
Series
can be due to defects in channel gating (class III with cryo-electron microscopy at an unprecedented
mutations), conductance (class IV mutations), abundance resolution. In 2022, with this approach, the correctors
(class V mutations), and stability (class VI mutations) of tezacaftor and elexacaftor were shown to bind to distinct
the mutant CFTR protein (figure 1). The most common sites on the F508del protein and the presence of both
mutation, F508del, which affects at least one allele in correctors was shown to be required to synergistically rectify
approximately 85% of patients with cystic fibrosis is a interdomain assembly defects and rescue F508del channel
class II mutation that results in almost no CFTR channels structure and function.19 This approach will provide
at the cell membrane. Besides elucidating the unprecedented opportunities to gain insights into the
pathogenesis of cystic fibrosis at the molecular level, this molecular mechanisms and response to pharmacological
classification already predicted that different therapeutic repair of rare CFTR mutations and enhance precision
approaches would be necessary to tackle CFTR medicine for patients with cystic fibrosis.
dysfunction caused by these different molecular
mechanisms, thus providing an important conceptual The expression of CFTR and alternative ion
framework for the development of CFTR modulators. channel targets in the airway epithelium
In this context, recognising that the most common In the airway epithelium, CFTR works in concert with
mutation, F508del, exhibits two distinct intramolecular other ion channels that participate in the homoeostatic
defects that independently impair folding (ie, instability of regulation of ion and fluid transport and pH on airway
nucleotide-binding domain 1 and impaired interdomain surfaces (figure 1). The amiloride-sensitive epithelial
assembly) was crucial, as this work predicted that sodium channel (ENaC) has long received attention in
addressing both defects would be necessary to effectively relation to the pathogenesis of cystic fibrosis lung disease
restore CFTR function.12,13 That particular mutations can as this channel is rate limiting for sodium and fluid
cause multiple molecular defects has also been increasingly absorption and its activity is increased in the airways of
recognised, and this is exemplified by the most common patients with cystic fibrosis.20 On the basis of these results
mutation, F508del, that not only affects protein folding and studies in mice with airway-specific overexpression
and plasma membrane expression, but also leads to of ENaC, increased ENaC activity, in addition to CFTR
deficient channel gating and reduced stability at the dysfunction, is predicted to be a key determinant of the
plasma membrane, as well as by other common mutations depletion of airway surface liquid and mucus
including W1282X, R334W, A455E, R347P, N1303K, and hyperconcentration characteristic of cystic fibrosis.21
R117H, which were also found to cause multiple defects.14 More recently, two alternative chloride channels were
Despite these insights that might at least partly explain the identified at the molecular level that might compensate
heterogeneity in responsiveness of CFTR function to for CFTR dysfunction. First, transmembrane member
pharmacological rescue, which has been observed among 16A (TMEM16A) was identified22 in 2008 as the calcium-
distinct mutations belonging to the same class both in activated chloride channel that is transiently activated by
vitro and in patients,15,16 the molecular and functional purinergic signalling in healthy and cystic fibrosis
consequences of many rare CFTR mutations remain airways.23 Although TMEM16A function remains intact
unknown. Facing these challenges, the concept of in people with cystic fibrosis, a 2021 study24 found that
theratyping has been introduced in cystic fibrosis research, non-cystic fibrosis chronic rhinosinusitis with nasal
whereby CFTR mutations are classified according to their polyps is associated with impaired TMEM16A-mediated
responsiveness to CFTR-directed therapeutics in vitro.17 epithelial chloride secretion, underscoring its potential
The implementation of this concept is strongly facilitated as a disease modifier and therapeutic target. The
by the development of patient-derived model systems since molecular identification of TMEM16A also allowed for
2013, which use an individual’s rectal cells to generate the study of its localisation in the airway epithelium. This
intestinal organoids or primary nasal or bronchial epithelial chloride channel is mainly expressed in response to
cells to generate highly differentiated airway epithelia that inflammatory stimuli in the apical membrane of mucin-
retain many of the properties of native patient tissues.18 producing goblet cells, indicating that TMEM16A-
These patient-derived models are expected to make mediated chloride and fluid secretion might be crucial
important contributions to personalised treatment for for proper secretion and clearance of mucins released
patients with cystic fibrosis as they can be used to predict from goblet cells in inflamed airways.24 Second, solute
responses to therapy in patients with rare mutations for carrier family 26 member 9 (SLC26A9) was identified as
whom clinical trials are not feasible, and to individual a constitutively active chloride channel that is coexpressed
treatment optimisation as an increased number of with CFTR in the airways and several other organs
molecularly distinct CFTR-modulating drugs are entering affected by cystic fibrosis.25 SLC26A9-mediated chloride
the clinical arena. secretion is also induced by inflammatory stimuli,
These advances are complemented by another suggesting a role in the coordinate secretion of fluid and
breakthrough in basic cystic fibrosis research, namely the mucins to maintain mucus hydration and clearance
possibility of studying the structure of human wild-type and under conditions of mucus hypersecretion. Furthermore,
F508del CFTR and the effects of current CFTR correctors emerging evidence from functional and genetic studies
www.thelancet.com Vol 402 September 30, 2023 1187
Series
suggests that SLC26A9 interacts with CFTR, and that a osmotic pressure of cystic fibrosis mucus to levels that
SLC26A9 variant (Rs7512462) is associated with the exceed those of the subjacent periciliary layer, causing
severity of lung disease and response to CFTR modulator compression of the cilia and impaired mucociliary
therapy in patients with cystic fibrosis.26 These alternative clearance.34,35 Second, an increase in disulfide crosslinking
chloride channels remain an active area of research, through the oxidation of free thiols contained in the large
including in emerging work on the functional cross-talk secreted mucins MUC5B and MUC5AC, which is caused
between TMEM16A and SLC26A9 and CFTR, which was by oxidant acids generated by the activity of peroxidases
reviewed in 2022.27,28 Collectively, these studies support secreted by neutrophils in chronic airway inflammation,
TMEM16A and SLC26A9 as potential disease modifiers has been identified as an important mechanism
and novel therapeutic targets for cystic fibrosis. underlying the increased viscoelasticity and dysfunction
In addition to the growing knowledge of alternative ion of the mucus gel in cystic fibrosis airways.36 Third, studies
channel targets, technological advances that enabled in the cystic fibrosis pig model identified abnormalities in
studies of the transcriptome of single cells contributed mucus strands generated in the submucosal glands of the
important novel insights into the cell type expression of large cartilaginous airways that also contribute to impaired
CFTR in the airway epithelium. Although CFTR was mucociliary clearance in cystic fibrosis. In the absence of
initially assumed to be predominantly expressed in CFTR, the elasticity of these strands is also increased,
ciliated respiratory epithelial cells, single-cell RNA hindering their detachment from submucosal grand
sequencing studies of freshly isolated epithelial cells ducts upon secretion into the airway lumen and
from large and small airways identified non-ciliated consequently the clearance of the inhaled particles bound
secretory cells as the dominant CFTR-expressing cell to these strands from the lung.37 These studies also
type in the superficial airway epithelium of the human indicated that both deficient CFTR-mediated chloride and
lung, followed by basal cells. CFTR expression in ciliated bicarbonate secretion are implicated in the pathogenesis
cells was found to be infrequent and low.29 The highest of mucus dysfunction in cystic fibrosis. Before their
amount of CFTR expression per cell was found in secretion, mucin macromolecules are densely packed in
ionocytes, a rare cell type that constitutes less than 1% of secretory vesicles in the presence of high calcium
the airway epithelial cells along the tracheobronchial concentrations and acidic pH, and a 2019 in vitro study38
tree. Although the functional relevance of CFTR showed that removal of calcium and an increase in the pH
expression in ionocytes and the role of this rare cell type to 7·4 both facilitate mucin expansion from this compact
in cystic fibrosis pathogenesis remains to be established, conformation.39 As bicarbonate chelates calcium ions and
the results of these studies provide important information is implicated in pH regulation, these results point to an
on the cell types in which CFTR expression needs to be important role of impaired CFTR-mediated bicarbonate
restored (eg, by gene replacement therapies), suggesting secretion in atypical mucus structure and function in the
a focus on the secretory cells of the superficial airway airways and other affected organs, including the intestine
epithelium. and pancreas, in patients with cystic fibrosis.40 Collectively,
these results have greatly furthered our understanding of
Linking CFTR dysfunction to airway mucus the links between CFTR dysfunction and mucociliary
obstruction, impaired host defence, and chronic dysfunction that hinder proper host defences against
inflammation inhaled and aspirated irritants and pathogens and provide
A striking and characteristic consequence of CFTR the basis for chronic infection and inflammation in cystic
dysfunction is the accumulation of highly viscoelastic fibrosis airways.
mucus that obstructs the airways, leads to airflow Besides impaired mucociliary clearance, studies in
limitation, and forms a nidus for chronic airway infection newborn pigs with cystic fibrosis showed that deficient
and inflammation, which in turn produce progressive CFTR-mediated bicarbonate secretion turns the pH of the
lung damage in patients with cystic fibrosis (figure 1).30,31 airway surface liquid acidic, leading to reduced activity of
The genesis of atypical mucus properties and impaired antimicrobial peptides, which makes pigs with cystic
mucociliary clearance in cystic fibrosis has been linked to fibrosis more susceptible to infection with pathogens
several different mechanisms. First, studies in bronchial such as Staphylococcus aureus and Pseudomonas
epithelial cultures and sputum from patients with cystic aeruginosa.41,42 However, the clinical relevance of this
fibrosis and mice with airway-specific overexpression of independent mechanism of impaired host defence
ENaC showed that tipping the balance between CFTR- remains to be established, as measurements in 2017 in
mediated secretion and ENaC-mediated absorption humans gave similar values for airway pH in children
towards net fluid absorption leads to airway surface liquid with and without cystic fibrosis.43 In addition, CFTR
depletion and hyperconcentration of the mucus gel dysfunction in monocytes and macrophages has been
covering airway surfaces from approximately 2% solids in implicated in impaired host defence in cystic fibrosis
healthy individuals to approximately 10% solids in people airways, and this notion is supported by data showing
with cystic fibrosis.21,32,33 This increase in mucus some improvement of impaired phagocytosis and the
concentration was shown to produce an increase in the killing of bacteria by the macrophages of patients with
1188 www.thelancet.com Vol 402 September 30, 2023
Series
cystic fibrosis given highly effective CFTR modulator function in the airways of patients with at least one
therapy.44–47 With technical advances in next generation F508del allele to approximately 50% of that measured in
sequencing of bacterial genes, it has become clear that healthy people, and that this degree of functional rescue
chronic airway infection in cystic fibrosis is not only rapidly decreases sputum pathogen density and improves
caused by classic cystic fibrosis-associated pathogens, microbiome composition and inflammation markers
such as P aeruginosa, but also by severe abnormalities of during the first year of therapy in adolescent and adult
the airway microbiome, including reduced diversity, patients with cystic fibrosis.15,60,61 However, despite these
evenness, and richness of bacterial species that are improvements, airway infection and inflammation
resilient to antibiotic therapy and associated with the persist to a lesser degree that is probably more similar to
severity of cystic fibrosis lung disease.48–50 Studies in those observed in other chronic lung diseases such as
young children with cystic fibrosis showed that non-cystic fibrosis bronchiectasis.60,61 These results
abnormalities in the airway microbiome develop early in indicate that with current CFTR modulator therapies
life and are associated with airway inflammation and the there will be a continued need for novel anti-infective
development of bronchiectasis even before the detection and anti-inflammatory therapies, at least for patients
of cystic fibrosis-associated pathogens.51 Taken together, with cystic fibrosis and established lung disease. To
these results indicate that, once established, this dysbiosis tackle this problem, multi-omics technologies provide
is an important driver of chronic airway inflammation unprecedented opportunities to study the alterations and
leading to the recruitment and activation of neutrophils effects of pharmacological improvement of CFTR
into the airway lumen, which in turn results in the excess function on gene expression, the epigenome, proteome,
release of neutrophil elastase and other neutrophil serine and metabolome in single cells and supernatant from
proteases (eg, cathepsin G and proteinase 3) that play airway samples (sputum and bronchoalveolar lavage) to
important roles in progressive structural lung damage understand the pathways and molecular mechanisms
and mucus hypersecretion and dysregulation of underlying residual infection and inflammation that
inflammation and airway ion transport.52–54 could lead to the identification of novel targets for the full
In addition to bacterial triggers, emerging evidence restoration of airway homoeostasis and other hallmarks
from the cystic fibrosis ferret model treated with broad- of health.62,63
spectrum antibiotics, and ENaC-overexpressing mice
reared under germ-free conditions suggests that mucus Progress and the remaining challenges of
plugging can induce airway inflammation in the absence pharmacological approaches to restore CFTR
of bacterial infection, probably via the regional generation function
of hypoxic conditions leading to the release of danger- The development of highly effective CFTR modulator
associated molecular patterns, such as interleukin (IL)-1 therapy, which combines the restoration of the folding
α from hypoxic epithelial cells triggering neutrophilic and gating defects of mutant CFTR channels with
inflammation via IL-1 receptor signaling.55–57 A recent a combination of corrector and potentiator compounds,
conundrum of relevance to CFTR-directed therapeutics has led to unprecedented improvements in lung
relates to observations indicating that airway function and other clinical outcomes in eligible patients,
inflammation can have both detrimental and beneficial transforming the landscape of clinical care for patients
effects on CFTR function. On one hand, in 2013, with cystic fibrosis.3 The current small molecule
neutrophil elastase was shown to degrade CFTR and combination therapy consisting of two distinct
disable its channel function.58 On the other hand, in correctors, the type III corrector elexacaftor and the
2021, the exposure of epithelial cells in cystic fibrosis type I corrector tezacaftor, in combination with the
airways to supernatant from mucopurulent material potentiator ivacaftor (ETI) has been studied most
collected from cystic fibrosis airways was found to extensively in patients with at least one copy of the
augment the biochemical and functional rescue of common F508del mutation (figure 2).64–70 With this triple
F508del-CFTR by double or triple CFTR modulator combination, as predicted by basic research,12,13,19 it
therapy.59 Research on the identification of the specific became possible to overcome the ceiling effect observed
factors mediating these divergent effects on CFTR might for the pharmacological rescue of F508del with earlier
lead to novel strategies for augmentation of mutant dual combination therapies that contained only one type
CFTR function in patients treated with current CFTR I corrector (lumacaftor or tezacaftor).71 The effect of this
modulator therapies. Another pertinent issue in the era advancement is apparent in observational studies
of highly effective modulator therapy relates to the showing a statistically significant improvement in the
question of to what extent chronic airway infection and restoration of CFTR function in the airways and intestine
inflammation can be reversed and homoeostasis restored from approximately 10–20% in F508del-homozygous
upon pharmacological restoration of CFTR function. patients treated with dual combination modulators to
Emerging data from observational studies in the post- approximately 40–50% of typical CFTR function in
approval setting show that triple combination therapy patients with at least one F508del allele.15,72 As
with elexacaftor–tezacaftor–ivacaftor (ETI) restores CFTR a conceptually important advance, studies in patients
www.thelancet.com Vol 402 September 30, 2023 1189
Series
Improved mucociliary clearance
approximately 50% of patients with cystic fibrosis and
no F508del allele responded clinically to ETI, including
a large subset of patients who carried a CFTR variant
Anti-infectives
Mucolytics S
Protease that is not currently approved for ETI. These approaches
S inhibitors
CFTR S
S are important for patients with extremely rare CFTR
S
HCO3– ENaC SLC26A9
S variants as they might establish a path to their eligibility
–
IL-1ß IL-8 Proteases for CFTR modulator therapy.17,18
Cl– ENaC Na+ Cl– TMEM16A Cl Cl–
Potentiator potentiator TNF-α Despite this breakthrough, there are still both
inhibitor
challenges and opportunities for further improvement
for this CFTR modulator-responsive patient population.3,4
TMEM16A Reported data in 2019, in ferrets with cystic fibrosis,
Enhancer suggest that starting CFTR modulator therapy already in
utero might have the greatest therapeutic effect on lung
mRNA therapy
lipid nanoparticle disease and extra-pulmonary manifestations of cystic
H20 H 20 H20 H20 fibrosis; however, a path for the clinical development of
Corrector 1
preventive treatment starting in utero does not exist yet.77
ASO Natural history studies have established a relationship
Corrector 2 between the degree of CFTR dysfunction and disease
Gene
editing severity,78,79 and emerging data from observational studies
show substantial residual airway infection and
Amplifier Readthrough DNA therapy inflammation at least in adult patients with chronic lung
agents viral vector
disease treated with ETI.60,61 These studies provide a
rationale for aiming to enhance the pharmacological
Figure 2: Current and future therapies to restore CFTR function and improve airway mucus clearance, restoration of mutant CFTR function further, ideally
infection, and inflammation in patients with cystic fibrosis
Highly effective modulator therapies address the underlying folding defects (with correctors) or gating defects towards the levels of healthy carriers, and several
(with potentiators) of the CFTR channel. Their efficacy might be further improved by increasing CFTR mRNA approaches are currently being pursued to achieve this
expression (with amplifiers) or by using molecules that enhance channel activity at the cell membrane. goal. First, additional small molecule correctors are being
Readthrough agents are currently being developed for CFTR nonsense mutations. Pharmacological targeting of developed on the basis of high-throughput screening
alternative ion channels, such as ENaC and the alternative chloride channels TMEM16A and SLC26A9, offers
mutation-agnostic approaches to compensate for CFTR dysfunction in the airways. Emerging gene therapies for campaigns. The novel corrector vanzacaftor is currently
cystic fibrosis include inhaled delivery of CFTR mRNA in lipid nanoparticles or CFTR cDNA in viral vectors as being tested in combination with tezacaftor and the more
mutation-agnostic approaches to restore CFTR function, and mutation-specific strategies, such as the modulation durable potentiator deutivacaftor in clinical trials in
of splicing with ASO and gene editing. Novel approaches to symptomatic therapies include the development of
patients with at least one F508del allele,80 and novel
mucolytic agents to reduce excess mucin crosslinking, phage therapy to tackle chronic Pseudomonas infection as a
novel anti-infective strategy, and protease inhibition to reduce inflammation and proteolytic damage of the cystic chemical entities have been identified that, in
fibrosis lung. Figure created with BioRender.com. ASO=antisense oligo nucleotides. CFTR=cystic fibrosis combination, lead to the functional correction of F508del
transmembrane conductance regulator. ENaC=epithelial sodium channel. SLC26A9=solute carrier family and other processing mutations up to 100% of wild-type
26 member 9. TMEM16A=transmembrane member 16A. IL=interleukin. TNF=tumour necrosis factor.
CFTR function in cell lines and primary human airway
epithelia in vitro.81 In addition to the development of
with one F508del allele and a gating or residual function modulators with enhanced efficacy, a new class of CFTR
mutation responsive to ivacaftor on the other allele amplifiers has been identified that enhances the efficiency
showed that treating both mutations affected by distinct of translation of CFTR mRNA, thereby increasing the
molecular mechanisms has additive therapeutic amount of mutant CFTR protein available for functional
benefits.73 In addition, in vitro studies in heterologous rescue by modulators.6 An alternative approach to
cells have identified 177 rare CFTR variants that respond enhance the effects of CFTR modulators was established
to ETI and contributed to its approval for patients with at in 2022 with the development of a PI3Kγ mimetic peptide.
least one of these responsive CFTR variants by the US In airway epithelial cells, PI3Kγ decreases intracellular
Food and Drug Administration (FDA), but not the cyclic adenosine monophosphate (cAMP) levels through
European Medicines Agency. As a result, over 90% of the kinase-dependent activation of phosphodiesterases,
patients with cystic fibrosis are now genetically eligible whereas treatment with a cell-permeable PI3Kγ mimetic
for highly effective modulator therapy. However, specific peptide leads to an increase in cAMP and protein kinase
mutations might be preferentially permeant to chloride A, thereby enhancing the phosphorylation and gating of
but not bicarbonate, and the effects of CFTR modulators both wild-type CFTR and F508del-CFTR rescued by
on the restoration of bicarbonate transport remain to be modulators.82 This PI3Kγ mimetic peptide was also
established.74 The list of responsive CFTR variants found, via a similar molecular mechanism, to have anti-
continues to grow on the basis of theratyping approaches inflammatory effects reducing neutrophilic inflammation
with patient-derived model systems75 and the assessment in mice, which might provide additional benefits to
of clinical responses used in 2023 in the French patients with cystic fibrosis. Although they are at early
Compassionate Program,76 which found that stages of development, these approaches hold promise to
1190 www.thelancet.com Vol 402 September 30, 2023
Series
further enhance CFTR function and long-term clinical Globally, approximately 10% of individuals with cystic
benefits in patients eligible for CFTR modulator fibrosis (including a substantial subgroup of patients
treatment (figure 2). ineligible for modulator treatment) are affected by CFTR
Drug Clinical stage Clinical trial identifier Company
Restoration of CFTR function
CFTR modulator Vanzacaftor–tezacaftor– Phase 3 NCT05033080; NCT05076149 Vertex Pharmaceuticals
deutivacaftor
Readthrough agent ELX-02 Phase 2 NCT04135495; NCT04126473 Eloxx Pharmaceuticals
CFTR modulator SION-638 Phase 1 NA Sionna Therapeutics
Readthrough agent Preclinical ·· Icagen
CFTR enhancer (PI3Kγ KIT2014 Preclinical ·· Kither Biotech
mimetic peptide)
CFTR modulator Preclinical ·· Reata Pharmaceuticals
Readthrough agent SRI-41315 Preclinical ·· Southern Research
Mucociliary clearance
ENaC inhibitor ETD001 Phase 1 NCT04926701 Enterprise Therapeutics
TMEM16A potentiator GDC-6988 (formerly ETD002) Phase 1 NCT04488705 Roche (Genentech)
Mucolytic (thiol-modified Aer-01 (formerly MUC-31) Preclinical ·· Aer Therapeutics
carbohydrate)
Genetic therapy
CFTR DNA therapy via 4D-710 Phase 1 NCT05248230 4D Molecular Therapeutics
adeno-associated virus
vector
CFTR messenger RNA LUNAR-CF (ARCT-032) Phase 1 NCT05712538 Arcturus Therapeutics
therapy via lipid
nanoparticles
CFTR messenger RNA VX-522 mRNA Phase 1 NCT05668741 Vertex Pharmaceuticals
therapy via lipid
nanoparticles
Antisense oligonucleotide SPL84 Phase 1 NA SpliSense
for splicing modulation
CFTR DNA therapy via CGT-001 Preclinical ·· Carbon Biosciences
adeno-associated virus
vector
CFTR DNA therapy via Preclinical ·· Spirovant Sciences
adeno-associated virus
vector
CFTR DNA therapy via BI 3720931 Preclinical ·· Boehringer Ingelheim
lentivirus vector
CFTR DNA therapy via non- Preclinical ·· Carmine Therapeutics
viral extracellular vesicles
CFTR DNA therapy via Preclinical ·· Gensaic
bacteriophage-derived
particles
CFTR messenger RNA Preclinical ·· Nanite
therapy via polymer
nanoparticles
CFTR messenger RNA Preclinical ·· ReCode Therapeutics
therapy via lipid
nanoparticles
Integration of donor DNA Preclinical ·· SalioGen Therapeutics
via helper RNA that encodes
for saliogase
Antisense oligonucleotide SPL23 Preclinical ·· SpliSense
for splicing modulation
Transfer RNA therapy via Preclinical ·· The University of Hamburg and
lipid nanoparticles for Arcturus Therapeutics
splicing modulation
(Table continues on next page)
www.thelancet.com Vol 402 September 30, 2023 1191
Series
Drug Clinical stage Clinical trial identifier Company
(Continued from previous page)
Anti-inflammatory
Cathepsin C inhibitor Brensocatib Phase 2 NCT05090904 Insmed
Normalising lipid imbalance LAU-7b Phase 2 NCT03265288 Laurent Pharmaceuticals
Cathepsin C inhibitor BI 1291583 Phase 1 NCT05833035 Boehringer Ingelheim
Neutrophil elastase inhibitor Lonodelestat (formerly Phase 1 NCT03748199 Santhera
POL6014)
Anti-infective
Disruption of bacterial cell Inhaled Colistin (ColiFin) Phase 2 NA Spexis and PARI Pharma
membrane
Disruption of bacterial iron Inhaled gallium (AR-501; Phase 2 NCT03669614 Aridis Pharmaceuticals
metabolism Panaecin)
Disruption of bacterial iron Intravenous gallium Phase 2 NCT04294043 Cystic Fibrosis Foundation
metabolism
Phage therapy AP-PA02 Phase 2 NCT04596319 Armata Pharmaceuticals
Phage therapy BX004-A Phase 2 NCT05010577 BiomX
Destruction of bacterial cell Inhaled nitric oxide (LungFit Phase 2 NCT04685720 Beyond Air
wall GO)
Triazol antifungal agent Opelconazole Phase 2 NCT05037851 Pulmocide
Inhibition of bacterial ACG-701 (formerly ARV-1801) Phase 2 NCT05641298 Aceragen
protein synthesis
Inhibition of bacterial Lefamulin (Xenleta) Phase 1 NCT05225805 Nabriva Therapeutics
protein synthesis
Inhibition of bacterial Oral amikacin (MAT2501) Preclinical ·· Matinas BioPharma
protein synthesis
Inhibition of bacterial Tobramycin/Ca-EDTA Preclinical ·· Respirion Pharmaceuticals
protein synthesis
Inhibition of bacterial Oxazolidinone inhibitor Preclinical ·· TB Alliance
protein synthesis
Inhibition of bacterial and CSA-131 Preclinical ·· Kinnear Pharmaceuticals
fungal growth
Disruption of bacterial outer Inhaled murepavadin Preclinical ·· Spexis
membrane
The pipeline includes new therapies that are being funded by the Cystic Fibrosis Foundation (CFF), tested in clinical trials in the Cystic Fibrosis Foundation Therapeutic
For more on the Cystic Fibrosis Development Network (TDN) and the European Cystic Fibrosis Society Clinical Trial Network (ECFS-CTN), or were identified by the literature search for this Series paper.
Foundation Therapeutic CFTR=cystic fibrosis transmembrane conductance regulator. ENaC=epithelial sodium channel. NA=not available. TMEM16A=transmembrane member 16A.
Development Network see
Table: The cystic fibrosis drug development pipeline
https://www.cff.org/researchers/
therapeutics-development-
network
For more on the European Cystic class I mutations that cause premature termination being tested in a phase 2 trial in patients with cystic
Fibrosis Society Clinical Trial codons (PTCs), which prevent translation of a full-length fibrosis and at least one G542X mutation (table).85 Parallel
Network see https://www.ecfs. protein.2 The development of effective readthrough strategies to identify more efficacious or less toxic
eu/ctn
therapies that restore CFTR function by suppressing readthrough agents include the screening and preclinical
translation termination at PTCs is, therefore, an attractive investigation of approved drug libraries with the potential
approach to reduce the remaining group of patients who for rapid translation of promising candidates to clinical
are not eligible for pharmacological restoration of CFTR. trials, and the large high-throughput screening of novel
Early proof-of-concept studies showed that PTCs in chemical entities. The latter approach led to the
CFTR can be suppressed by aminoglycoside antibiotics, identification of SRI-41315, a compound that reduces the
such as gentamycin.83 However, their poor efficacy and abundance of the termination factor eRF1 leading to an
toxicity impeded clinical development and led to the extended pause at stop codons and suppression of PTCs,
search for more efficacious and well tolerated resulting in the restoration of CFTR expression and
aminoglycoside analogues. The currently most advanced function in airway epithelial cells in people with cystic
investigational readthrough agent, ELX-02, which fibrosis.86 Furthermore, SRI-41315 was also shown to
showed a dose-dependent improvement of readthrough augment aminoglycoside-mediated readthrough,
of PTCs resulting in functional restoration of full-length suggesting combination therapies with readthrough
CFTR in cystic fibrosis models in vitro and in vivo, was agents that target distinct components of the translation
well tolerated in a clinical phase 1 trial84 and is currently machinery might be a promising treatment strategy for
1192 www.thelancet.com Vol 402 September 30, 2023
Series
cystic fibrosis and potentially other diseases caused by Previous attempts to stimulate the alternative calcium-
PTCs. As PTCs also trigger nonsense-mediated mRNA activated chloride channel TMEM16A with denufosol,
decay (NMD), limiting the amount of mRNA available an inhaled uridine-5ʹ-triphosphate analogue designed to
for translational readthrough, NMD inhibition provides increase intracellular calcium in airway epithelial cells
an additional strategy to augment the efficacy of via activation of P2Y2 receptors, did not show clinical
readthrough agents. Once full-length CFTR protein is efficacy, probably due to the rapid inactivation of
formed, its activity can be further augmented by CFTR denufosol by exonucleotidases present in inflamed cystic
modulators. Indeed studies in intestinal organoids from fibrosis airways.89–91 In 2020, the first small molecule
patients with cystic fibrosis and various PTC mutations potentiator of TMEM16A (ETX001) was reported and
showed synergistic effects of combination therapy with shown to activate calcium-activated anion and fluid
the readthrough agent ELX-02, the NMD inhibitor secretion in bronchial epithelial cells from patients with
SMG1i, and CFTR modulation with ETI with levels of cystic fibrosis, and inhaled ETX001 improved mucociliary
functional correction of CFTR that exceeded those clearance in sheep.92 Because TMEM16A conducts both
observed with lumacaftor–ivacaftor in organoids from chloride and bicarbonate, its activation provides
F508del-homozygous patients.87 The results of these in an approach to compensate for CFTR dysfunction more
vitro studies in patient-derived organoids are promising completely, including abnormalities in mucus function
as they suggest that, reminiscent to the rescue of F508del and host defence that are related to deficient CFTR-
with CFTR correctors, there might be an opportunity to mediated bicarbonate transport. A related investigational
overcome the ceiling effect of a single readthrough agent compound (GDC-6988) has entered early clinical
with combination therapy that targets several molecular development (table). Another promising preclinical
mechanisms and provides clinical efficacy for patients strategy to enhance the activity of TMEM16A is blocking
with a spectrum of PTC mutations (figure 2). the binding of microRNA-9 to its 3’ untranslated region,
which is involved in the downregulation of TMEM16A
Alternative ion channel targets to circumvent expression.93 If successful in the clinical arena, this new
CFTR dysfunction in the airway epithelium class of ion channel modulator would be an attractive
Pharmacological targeting of alternative ion channels is approach to improve mucus clearance in patients with
an attractive mutation-agnostic approach to circumvent cystic fibrosis and potentially other muco-obstructive
the consequences of CFTR dysfunction in the airways lung diseases.
that, in the era of highly effective modulator therapies,
holds promise for patients who are genetically ineligible The promise of genetic therapies and gene
for CFTR modulators (figure 2). Given the role of ENaC editing approaches
in the pathogenesis of airway surface liquid depletion in To address the current disparity in treatment options for
cystic fibrosis, its inhibition has been the focus of the approximately 10% of patients with cystic fibrosis
approaches aiming to improve mucus hydration and who are genetically ineligible for or intolerant of CFTR
clearance. Several small molecule ENaC inhibitors were modulator therapy, and given the remaining challenges
developed that are more potent and more durable than with pharmacological solutions for this patient
amiloride and show improved airway surface hydration population (including patients with large CFTR deletions
and mucociliary clearance in human airway epithelial that include the promoter and intronic regions of the
cultures and sheep. However, successful translation of gene), enormous efforts are being put into gene
ENaC-directed approaches to patients is still pending and replacement and gene editing strategies based on nucleic
most clinical development programmes have been acid-based therapies to restore CFTR function in the
terminated.6,88 The inability of ENaC inhibitors to progress lungs.94–96 This revival of genetic therapies for cystic
through clinical development has been attributed to fibrosis is underpinned by important advances in gene
limitations in dosing to avoid unwanted systemic side- delivery and gene editing technologies, and a robust
effects, such as hyperkalaemia caused by ENaC inhibition pipeline including several distinct approaches has been
in the kidney or insufficient airway deposition by established and is currently undergoing preclinical and
inhalation as a route of delivery in patients with cystic early clinical development (figure 2; table).
fibrosis and chronic lung disease, which is characterised First, inhalation of stable CFTR mRNA packaged in
by heterogeneous airway mucus plugging that is not a lipid nanoparticles designed to penetrate mucus for the
feature of the preclinical sheep model. A novel, highly optimised targeting of airway epithelial cells is being
potent ENaC inhibitor, ETD001, was safe and well pursued to restore expression of wild-type CFTR in
tolerated in a phase 1 trial in healthy volunteers (NCT a mutation-agnostic fashion.94,95 This approach is expected
04926701), so dosing issues with earlier compounds to result in less immunogenicity than viral delivery
might be overcome and clinical testing in patients with systems, but relies on frequent redosing as the inhaled
cystic fibrosis might be informative as to whether mRNA is degraded intracellularly. Interim results of the
improving airway hydration alone is sufficient to improve first randomised, double-blind, placebo-controlled
clinical outcomes. phase 1/2 clinical study of MRT5005 in adult patients
www.thelancet.com Vol 402 September 30, 2023 1193
Series
with cystic fibrosis and two severe class I or II CFTR the potential of this approach to treat patients with cystic
mutations showed that treatment was generally safe and fibrosis and specific CFTR splicing and nonsense
well tolerated through 28 days of follow-up, although mutations.94 These studies showed that targeted antisense
some febrile and hypersensitivity reactions were noted oligonucleotide-based splicing modulation is highly
that mostly resolved within 1–2 days allowing continued effective in producing correctly spliced mRNA in patients
treatment. Lung function remained stable after with the 3849+10 kb C→T splicing mutation,102 and can
treatment, but no beneficial effects on forced expiratory induce skipping of CFTR exon 23, which harbours the
volume in 1 sec were observed in this small first-in- W1282X nonsense mutation,103 thereby restoring CFTR
human trial.97 Other early phase studies testing the safety function to airway epithelial cells. Lead antisense
and tolerability of mRNA replacement therapy are oligonucleotide candidates for this approach are currently
currently under way (NCT05668741 and NCT05712538). being advanced to a proof-of-concept trial in patients
Second, adeno-associated virus (AAV) gene therapy with carrying these specific mutations.94 Second, engineered
improved AAV capsids optimised for lung gene transfer transfer RNAs for the suppression of nonsense mutations
and reduced immunogenicity has been developed for in the CFTR gene were shown to re-establish CFTR
cystic fibrosis gene therapy, with clinical trials underway.94 expression and function in cell systems and patient-
The AAV-based gene therapy 4D-710 (comprising an AAV derived epithelia and provide another promising
capsid carrying a transgene cassette encoding human approach for patients with PTCs.94–106 Finally, important
CFTR with a deletion in the regulatory domain advances in gene editing have been made.107 With
[CFTRΔR]) has been developed for more durable vector- CRISPR-based adenine base editing and prime editing
based expression of CFTR in airway epithelial cells and is (and without the need for double-strand breaks that are
currently being tested in a first phase 1/2, single dose, required for conventional CRISPR/Cas9-mediated
open-label trial in adult patients with cystic fibrosis who genome engineering), several CFTR nonsense mutations
are ineligible for or unable to tolerate CFTR modulator and F508del were successfully repaired in the genome of
therapy (NCT05248230). The deletion of part of the CFTR intestinal organoids from patients with cystic fibrosis,
transgene is necessary due to the poor packaging capacity leading to effective restoration of CFTR function with no
of AAV, and the consequences of this truncation on detectable off-target effects during repair.108,109 These
CFTR function are currently unknown. Similar to preclinical results support the notion that gene editing
adenovirus, AAV vectors induce immunogenicity, which might be safely applied in human cells to correct
hampers repeated dosing without losing efficacy.96 Third, individual CFTR mutations in the genome for complete
optimised lentiviral vectors hold promise for efficient and life-long restoration of CFTR function as a potential
gene therapy for cystic fibrosis. Pseudotyped lentiviral cure of cystic fibrosis.
vectors containing envelope proteins from other viruses Despite these recent advances, substantial obstacles
have enhanced transduction efficiency in the lung, their remain that still have to be overcome to translate these
larger packaging capacity allows expression of full-length nucleic acid-based therapy approaches into effective
human CFTR, their integration into the host genome therapies for patients. These include effective delivery to
facilitates durable gene expression after a single dose, the right cell types in chronically inflamed and mucus-
and repeated administration was shown to be possible obstructed cystic fibrosis airways without off-target
without loss of efficacy.98 In preclinical studies, lentivirus- effects, including immunogenicity. To achieve this goal,
based gene therapy was shown to provide efficient and innate defence mechanisms need to be overcome and a
durable gene transfer to the mouse lung, efficient better understanding of where CFTR function needs to
restoration of CFTR function in cystic fibrosis intestinal be restored in the lung is needed, particularly in view of
organoids from patients with class I mutations, and the poorly defined role of the high levels of CFTR
a first-in-man trial of BI 3720931 as a long-lasting expression in ionocytes in the pathogenesis of cystic
therapeutic option for patients with cystic fibrosis is fibrosis lung disease.29 Furthermore, to what extent
currently in preparation.94,99 The results of these pilot repeated dosing is necessary and feasible for all nucleic
trials, including safety and tolerability data, and initial acid-based therapy approaches is currently unknown,
data on the efficacy and durability of CFTR restoration and the potential risk of oncogenicity (especially for viral
will probably be decisive for future directions with vectors that integrate into the host genome) will require
mutation-agnostic gene replacement therapy for cystic long-term safety monitoring. Finally, all current strategies
fibrosis. focus on inhaled delivery of nucleic acid-based therapies
In addition to these mutation-agnostic approaches, to the lungs and how CFTR function might be restored
several strategies for mutation-specific nucleic acid-based in other affected organs to improve the health of patients
therapies are being developed. First, preclinical studies with cystic fibrosis who are ineligible for modulator
with antisense oligonucleotides that can bind to their therapy remains unclear. These obstacles also contribute
target RNA and modulate its splicing, as were shown in to the challenges around clinical trial designs in the
2016 for other genetic diseases such as spinal muscular small population of patients with CF who are ineligible
atrophy and Duchenne muscular dystrophy,100,101 support for or intolerant of modulator therapy.110
1194 www.thelancet.com Vol 402 September 30, 2023
Series
Novel strategies for symptomatic therapies to reduction of free neutrophil elastase activity in sputum,
improve mucociliary clearance and reduce which was associated with improvements in clinical
airway inflammation and infection outcomes.114 Whether this promising antiprotease strategy
For a long time, symptomatic therapies targeting can sufficiently reduce the protease burden in the lungs
mucociliary dysfunction, chronic airway infection, and and improve clinical outcomes of patients with cystic
inflammation were the backbone of substantial fibrosis remains to be seen in ongoing clinical trials (eg,
improvements in the life expectancy and quality of life of NCT05090904).
patients with cystic fibrosis.1,2 With the emergence of Finally, novel anti-infective approaches to fight chronic
highly effective CFTR modulators, these symptomatic infection with P aeruginosa and other proinflammatory
therapies will remain important both for genetically pathogens more effectively remain a high priority.115
ineligible and intolerant patients, and for eligible patients Several novel antibiotic approaches, including systemic
with chronic lung disease and irreversible structural lung or inhaled administration of gallium (which was shown
damage, such as bronchiectasis and residual inflam to disrupt iron-dependent biological processes and lead
mation, and infection, on modulator therapy.2 A robust to the killing of antibiotic-resistant P aeruginosa strains in
pipeline of symptomatic therapies with enhanced vitro), are being actively studied in early phase clinical
efficacy, therefore, remains important to overcome the trials in the Cystic Fibrosis Foundation Therapeutic
remaining challenges related to airway mucus Development Network (CFF-TDN) and European Cystic
obstruction, chronic inflammation, and infection in Fibrosis Society Clinical Trial Network (ECFS-CTN;
multimodal cystic fibrosis care (table). table). In addition to pharmacological approaches,
Insights into the role of excess crosslinking of mucins inhaled phage therapies,116 such as AP-PA02 and
via disulfide bonds in the pathogenesis of the atypical BX004-A, that use a cocktails of bacteriophages to attack
viscoelasticity of cystic fibrosis mucus led to the and lyse chronically adapted and antibiotic-resistant
development of novel small molecule reducing agents as P aeruginosa strains in the lungs of patients with cystic
mucolytics in 2015 that are more potent than fibrosis provide a promising strategy to tackle the
N-acetylcysteine, the only FDA-approved drug in this remaining problem of chronic Pseudomonas infection as
class that did not improve mucus clearance and lung a key trigger for chronic inflammation and mucus
function in patients.36 In preclinical studies, two novel hypersecretion (eg, NCT04596319, NCT05010577). For
mucin-reducing agents, P3001 and the thiol-saccharide more detailed information on new developments and
mucolytic MUC-031, were shown to improve the approaches and unmet clinical needs related to novel
viscoelastic properties of cystic fibrosis sputum ex vivo anti-infective therapies, we refer the reader to reviews
and reduce airway mucus plugging and inflammation from the past 2 years.117–120
in a mouse model of cystic fibrosis lung disease.111,112 Given the increasingly recognised roles of airway
These encouraging results obtained with two distinct mucus obstruction, chronic inflammation, and infection
compounds in preclinical models provide a rationale for in a range of other lung diseases including bronchiectasis
clinical testing in patients with cystic fibrosis and other and COPD,31,121–123 innovative symptomatic therapies that
muco-obstructive lung diseases. have been developed for cystic fibrosis might also provide
In the area of anti-inflammatory therapies, progress has benefits to patients with high unmet needs in these
been made in the development of strategies designed to common lung diseases.
target free neutrophil elastase activity in the airways,
which constitutes a key risk factor for lung disease Conclusion
progression in children and adults with cystic fibrosis.53,54 Improving our understanding of underlying disease
Lonodelestat, a highly potent and selective inhibitor mechanisms in conjunction with a robust drug
of human neutrophil elastase, is in early clinical development pipeline has enabled the development of
development as an inhaled anti-inflammatory therapy for highly effective CFTR modulator therapy that provides
cystic fibrosis. In a 4-week, phase 1 trial in patients with unprecedented improvement in clinical outcomes for
cystic fibrosis, short-term inhalation of lonodelestat was approximately 90% of patients with cystic fibrosis who are
well tolerated and resulted in the inhibition of neutrophil genetically eligible for treatment. Despite this
elastase activity in sputum.113 As an alternative approach, breakthrough, an iterative process of fundamental and
brensocatib, an oral reversible inhibitor of cathepsin C clinical research remains instrumental to solving the
(also known as dipeptidyl peptidase 1), has been developed remaining challenges, with a current focus on the genetic
as a systemic anti-inflammatory strategy. Cathepsin C is or pharmacological restoration of CFTR function in the
responsible for the activation of all neutrophil serine small patient population who are ineligible for modulator
proteases, including cathepsin G and proteinase 3, in therapy and have the highest unmet medical need, and
addition to neutrophil elastase, and its inhibition further functional improvement in the large, eligible
therefore provides the potential for broader antiproteolytic population towards full restoration of CFTR function.
effects. In a 24-week, phase 2 trial in patients with non- With gene editing approaches that enable the correction of
cystic fibrosis bronchiectasis, brensocatib led to a individual CFTR mutations in the genome of patient cells,
www.thelancet.com Vol 402 September 30, 2023 1195
Series
effective treatment for all patients with cystic fibrosis is 12 Mendoza JL, Schmidt A, Li Q, et al. Requirements for efficient
now on the horizon. Further improvement of symptomatic correction of ΔF508 CFTR revealed by analyses of evolved
sequences. Cell 2012; 148: 164–74.
therapies remains important for multimodal manage 13 Rabeh WM, Bossard F, Xu H, et al. Correction of both NBD1
ment, especially for patients with chronic lung disease, energetics and domain interface is required to restore ΔF508 CFTR
and might be applicable for tackling airway mucus folding and function. Cell 2012; 148: 150–63.
14 Veit G, Avramescu RG, Chiang AN, et al. From CFTR biology
plugging, chronic inflammation, and infection in toward combinatorial pharmacotherapy: expanded classification of
common lung diseases such as bronchiectasis and COPD. cystic fibrosis mutations. Mol Biol Cell 2016; 27: 424–33.
Contributors 15 Graeber SY, Vitzthum C, Pallenberg ST, et al. Effects of elexacaftor/
SYG and MAM jointly performed the literature search and conceptualised tezacaftor/ivacaftor therapy on CFTR function in patients with
cystic fibrosis and one or two F508del alleles.
the content and figures of this Series paper. SYG designed the original draft
Am J Respir Crit Care Med 2022; 205: 540–49.
of the figures and reviewed and edited the manuscript. MAM wrote the
16 Dekkers JF, Wiegerinck CL, de Jonge HR, et al. A functional CFTR
original draft of the manuscript and reviewed and edited the figures. Both
assay using primary cystic fibrosis intestinal organoids. Nat Med
authors approved the final version of this Series paper for submission. 2013; 19: 939–45.
Declaration of interests 17 Clancy JP, Cotton CU, Donaldson SH, et al. CFTR modulator
No funding was provided specifically for this Series paper. SYG reports theratyping: current status, gaps and future directions. J Cyst Fibros
grants from the Christiane Herzog Foundation, the German Cystic 2019; 18: 22–34.
Fibrosis Association (Mukoviszidose), Vertex Pharmaceuticals, 18 Ramalho AS, Amato F, Gentzsch M. Patient-derived cell models for
and a fellowship from the Berlin Institute of Health Charité Clinician personalized medicine approaches in cystic fibrosis. J Cyst Fibros
Scientist Program; lecture honoraria from Chiesi and Vertex 2023; 22 (suppl): S32-8.
Pharmaceuticals; and advisory board participation for Chiesi and Vertex 19 Fiedorczuk K, Chen J. Molecular structures reveal synergistic rescue
Pharmaceuticals outside the submitted work. MAM reports grants from of Δ508 CFTR by Trikafta modulators. Science 2022; 378: 284–90.
the German Research Foundation (DFG; grant numbers SFB-TR 84 and 20 Boucher RC, Stutts MJ, Knowles MR, Cantley L, Gatzy JT.
SFB 1449; project numbers 431232613 and 450557679), the German Na+ transport in cystic fibrosis respiratory epithelia. Abnormal
basal rate and response to adenylate cyclase activation. J Clin Invest
Federal Ministry of Education and Research (BMBF; grant number
1986; 78: 1245–52.
82DZL009B1), the German Innovation Fund (grant number
21 Mall M, Grubb BR, Harkema JR, O’Neal WK, Boucher RC.
01NVF19008), and Vertex Pharmaceuticals; consulting fees from AbbVie,
Increased airway epithelial Na+ absorption produces cystic fibrosis-
Antabio, Arrowhead Pharmaceuticals, Boehringer Ingelheim, Enterprise like lung disease in mice. Nat Med 2004; 10: 487–93.
Therapeutics, Kither Biotech, Prieris, Recode, Santhera, Splisense, and
22 Caputo A, Caci E, Ferrera L, et al. TMEM16A, a membrane protein
Vertex Pharmaceuticals; lecture honoraria from Vertex Pharmaceuticals; associated with calcium-dependent chloride channel activity. Science
travel support from Boehringer Ingelheim and Vertex Pharmaceuticals; 2008; 322: 590–94.
a patent on the Scnn1b-transgenic mouse as an animal model for chronic 23 Pedemonte N, Galietta LJ. Structure and function of TMEM16
obstructive pulmonary disease and cystic fibrosis, a patent on the medical proteins (anoctamins). Physiol Rev 2014; 94: 419–59.
uses of thiol-functionalised polyglycerol derivatives, and a patent on 24 Salomon JJ, Albrecht T, Graeber SY, et al. Chronic rhinosinusitis
receptor for advanced glycation endproducts (RAGE) proteins for the with nasal polyps is associated with impaired TMEM16A-mediated
treatment of fibrosis and DNA damage-mediated diseases; and advisory epithelial chloride secretion. J Allergy Clin Immunol 2021;
board participation with AbbVie, Antabio, Arrowhead Pharmaceuticals, 147: 2191–201.
Boehringer Ingelheim, Enterprise Therapeutics, Kither Biotech, Pari, 25 Balázs A, Mall MA. Role of the SLC26A9 chloride channel as
and Vertex Pharmaceuticals outside the submitted work. MAM is disease modifier and potential therapeutic target in cystic fibrosis.
a Fellow of the European Respiratory Society (FERS). Front Pharmacol 2018; 9: 1112.
26 Gong J, He G, Wang C, et al. Genetic evidence supports the
References
development of SLC26A9 targeting therapies for the treatment of
1 Shteinberg M, Haq IJ, Polineni D, Davies JC. Cystic fibrosis. Lancet
lung disease. NPJ Genom Med 2022; 7: 28.
2021; 397: 2195–211.
27 Galietta LJV. TMEM16A (ANO1) as a therapeutic target in cystic
2 Bell SC, Mall MA, Gutierrez H, et al. The future of cystic fibrosis
fibrosis. Curr Opin Pharmacol 2022; 64: 102206.
care: a global perspective. Lancet Respir Med 2020; 8: 65–124.
28 Gorrieri G, Zara F, Scudieri P. SLC26A9 as a potential modifier and
3 Taylor-Cousar JL, Robinson PD, Shteinberg M, Downey D. CFTR
therapeutic target in cystic fibrosis lung disease. Biomolecules 2022;
modulator therapy: transforming the landscape of clinical care in
12: 202.
cystic fibrosis. Lancet 2023; published online Sept 9. https://doi.
org/10.1016/S0140-6736(23)01609-4. 29 Okuda K, Dang H, Kobayashi Y, et al. Secretory cells dominate
airway CFTR expression and function in human airway superficial
4 Hisert KB, Birket S, Clancy JP, et al. Understanding and addressing
epithelia. Am J Respir Crit Care Med 2021; 203: 1275–89.
the needs of people with cystic fibrosis in the era of CFTR
modulator therapy. Lancet Respir Med 2023; published online Sept 9. 30 Boucher RC. Muco-obstructive lung diseases. N Engl J Med 2019;
https://doi.org/10.1016/S2213-2600(23)00324-7. 380: 1941–53.
5 McGarry ME, McColley SA. Cystic fibrosis patients of minority race 31 Fahy JV, Dickey BF. Airway mucus function and dysfunction.
and ethnicity less likely eligible for CFTR modulators based on N Engl J Med 2010; 363: 2233–47.
CFTR genotype. Pediatr Pulmonol 2021; 56: 1496–503. 32 Henderson AG, Ehre C, Button B, et al. Cystic fibrosis airway
6 Mall MA, Mayer-Hamblett N, Rowe SM. Cystic fibrosis: secretions exhibit mucin hyperconcentration and increased osmotic
emergence of highly effective targeted therapeutics and potential pressure. J Clin Invest 2014; 124: 3047–60.
clinical implications. Am J Respir Crit Care Med 2020; 33 Matsui H, Grubb BR, Tarran R, et al. Evidence for periciliary liquid
201: 1193–208. layer depletion, not abnormal ion composition, in the pathogenesis
7 Stoltz DA, Meyerholz DK, Welsh MJ. Origins of cystic fibrosis of cystic fibrosis airways disease. Cell 1998; 95: 1005–15.
lung disease. N Engl J Med 2015; 372: 1574–75. 34 Hill DB, Button B, Rubinstein M, Boucher RC. Physiology and
8 Riordan JR. CFTR function and prospects for therapy. pathophysiology of human airway mucus. Physiol Rev 2022;
Annu Rev Biochem 2008; 77: 701–26. 102: 1757–836.
9 Boucher RC. Airway surface dehydration in cystic fibrosis: 35 Button B, Cai LH, Ehre C, et al. A periciliary brush promotes the
pathogenesis and therapy. Annu Rev Med 2007; 58: 157–70. lung health by separating the mucus layer from airway epithelia.
Science 2012; 337: 937–41.
10 Sheppard DN, Welsh MJ. Structure and function of the CFTR
chloride channel. Physiol Rev 1999; 79 (suppl): S23–45. 36 Yuan S, Hollinger M, Lachowicz-Scroggins ME, et al. Oxidation
increases mucin polymer cross-links to stiffen airway mucus gels.
11 Welsh MJ, Smith AE. Molecular mechanisms of CFTR chloride
Sci Transl Med 2015; 7: 276ra27.
channel dysfunction in cystic fibrosis. Cell 1993; 73: 1251–54.
1196 www.thelancet.com Vol 402 September 30, 2023
Series
37 Pino-Argumedo MI, Fischer AJ, Hilkin BM, et al. Elastic mucus 61 Schaupp L, Addante A, Völler M, et al. Longitudinal effects of
strands impair mucociliary clearance in cystic fibrosis pigs. elexacaftor/tezacaftor/ivacaftor on sputum viscoelastic properties,
Proc Natl Acad Sci USA 2022; 119: e2121731119. airway infection and inflammation in patients with cystic fibrosis.
38 Hughes GW, Ridley C, Collins R, Roseman A, Ford R, Thornton DJ. Eur Respir J 2023; 62: 2202153.
The MUC5B mucin polymer is dominated by repeating structural 62 López-Otín C, Kroemer G. Hallmarks of health. Cell 2021;
motifs and its topology is regulated by calcium and pH. Sci Rep 184: 33–63.
2019; 9: 17350. 63 Rajewsky N, Almouzni G, Gorski SA, et al. LifeTime and improving
39 Quinton PM. Cystic fibrosis: impaired bicarbonate secretion and European healthcare through cell-based interceptive medicine.
mucoviscidosis. Lancet 2008; 372: 415–17. Nature 2020; 587: 377–86.
40 Quinton PM. Role of epithelial HCO3– transport in mucin secretion: 64 Goralski JL, Hoppe JE, Mall MA, et al. Phase 3 open-label clinical
lessons from cystic fibrosis. Am J Physiol Cell Physiol 2010; trial of elexacaftor/tezacaftor/ivacaftor in children aged 2–5 years
299: C1222–33. with cystic fibrosis and at least one F508del allele.
41 Shah VS, Meyerholz DK, Tang XX, et al. Airway acidification Am J Respir Crit Care Med 2023; 208: 59–67.
initiates host defense abnormalities in cystic fibrosis mice. Science 65 Sutharsan S, McKone EF, Downey DG, et al. Efficacy and safety of
2016; 351: 503–07. elexacaftor plus tezacaftor plus ivacaftor versus tezacaftor plus
42 Pezzulo AA, Tang XX, Hoegger MJ, et al. Reduced airway surface ivacaftor in people with cystic fibrosis homozygous for F508del-
pH impairs bacterial killing in the porcine cystic fibrosis lung. CFTR: a 24-week, multicentre, randomised, double-blind, active-
Nature 2012; 487: 109–13. controlled, phase 3b trial. Lancet Respir Med 2022; 10: 267–77.
43 Schultz A, Puvvadi R, Borisov SM, et al. Airway surface liquid pH is 66 Mall MA, Brugha R, Gartner S, et al. Efficacy and safety of
not acidic in children with cystic fibrosis. Nat Commun 2017; elexacaftor/tezacaftor/ivacaftor in children 6 through 11 years of age
8: 1409. with cystic fibrosis heterozygous for F508del and a minimal
44 Cavinato L, Luly FR, Pastore V, et al. Elexacaftor/tezacaftor/ivacaftor function mutation: a phase 3b, randomized, placebo-controlled
corrects monocyte microbicidal deficiency in cystic fibrosis. study. Am J Respir Crit Care Med 2022; 206: 1361–69.
Eur Respir J 2023; 61: 2200725. 67 Zemanick ET, Taylor-Cousar JL, Davies J, et al. A phase 3 open-label
45 Zhang S, Shrestha CL, Robledo-Avila F, et al. Cystic fibrosis study of elexacaftor/tezacaftor/ivacaftor in children 6 through
macrophage function and clinical outcomes after elexacaftor/ 11 years of age with cystic fibrosis and at least one F508del allele.
tezacaftor/ivacaftor. Eur Respir J 2023; 61: 2102861. Am J Respir Crit Care Med 2021; 203: 1522–32.
46 Brinkert K, Hedtfeld S, Burhop A, et al. Rescue from 68 Griese M, Costa S, Linnemann RW, et al. Safety and efficacy of
Pseudomonas aeruginosa airway infection via stem cell elexacaftor/tezacaftor/ivacaftor for 24 weeks or longer in people
transplantation. Mol Ther 2021; 29: 1324–34. with cystic fibrosis and one or more F508del alleles: interim results
of an open-label phase 3 clinical trial. Am J Respir Crit Care Med
47 Di A, Brown ME, Deriy LV, et al. CFTR regulates phagosome
2021; 203: 381–85.
acidification in macrophages and alters bactericidal activity.
Nat Cell Biol 2006; 8: 933–44. 69 Heijerman HGM, McKone EF, Downey DG, et al. Efficacy and
safety of the elexacaftor plus tezacaftor plus ivacaftor combination
48 Blanchard AC, Waters VJ. Microbiology of cystic fibrosis airway
regimen in people with cystic fibrosis homozygous for the F508del
disease. Semin Respir Crit Care Med 2019; 40: 727–36.
mutation: a double-blind, randomised, phase 3 trial. Lancet 2019;
49 Caverly LJ, LiPuma JJ. Cystic fibrosis respiratory microbiota: 394: 1940–48.
unraveling complexity to inform clinical practice.
70 Middleton PG, Mall MA, Dřevínek P, et al. Elexacaftor-tezacaftor-
Expert Rev Respir Med 2018; 12: 857–65.
ivacaftor for cystic fibrosis with a single Phe508del allele.
50 Marsland BJ, Gollwitzer ES. Host-microorganism interactions in N Engl J Med 2019; 381: 1809–19.
lung diseases. Nat Rev Immunol 2014; 14: 827–35.
71 Taylor-Cousar JL, Mall MA, Ramsey BW, et al. Clinical development
51 Muhlebach MS, Zorn BT, Esther CR, et al. Initial acquisition and of triple-combination CFTR modulators for cystic fibrosis patients
succession of the cystic fibrosis lung microbiome is associated with with one or two F508del alleles. ERJ Open Res 2019; 5: 00082-2019.
disease progression in infants and preschool children. PLoS Pathog
72 Graeber SY, Dopfer C, Naehrlich L, et al. Effects of lumacaftor-
2018; 14: e1006798.
ivacaftor therapy on cystic fibrosis transmembrane conductance
52 McKelvey MC, Weldon S, McAuley DF, Mall MA, Taggart CC. regulator function in Phe508del homozygous patients with cystic
Targeting proteases in cystic fibrosis lung disease. paradigms, fibrosis. Am J Respir Crit Care Med 2018; 197: 1433–42.
progress, and potential. Am J Respir Crit Care Med 2020; 201: 141–47.
73 Barry PJ, Mall MA, Álvarez A, et al. Triple therapy for cystic fibrosis
53 Sly PD, Gangell CL, Chen L, et al. Risk factors for bronchiectasis in Phe508del-gating and -residual function genotypes. N Engl J Med
children with cystic fibrosis. N Engl J Med 2013; 368: 1963–70. 2021; 385: 815–25.
54 Mayer-Hamblett N, Aitken ML, Accurso FJ, et al. Association 74 Choi JY, Muallem D, Kiselyov K, Lee MG, Thomas PJ, Muallem S.
between pulmonary function and sputum biomarkers in cystic Aberrant CFTR-dependent HCO3- transport in mutations associated
fibrosis. Am J Respir Crit Care Med 2007; 175: 822–28. with cystic fibrosis. Nature 2001; 410: 94–97.
55 Rosen BH, Evans TIA, Moll SR, et al. Infection is not required for 75 Ramalho AS, Fürstová E, Vonk AM, et al. Correction of CFTR
mucoinflammatory lung disease in CFTR-knockout ferrets. function in intestinal organoids to guide treatment of cystic fibrosis.
Am J Respir Crit Care Med 2018; 197: 1308–18. Eur Respir J 2021; 57: 1902426.
56 Fritzsching B, Zhou-Suckow Z, Trojanek JB, et al. Hypoxic 76 Burgel PR, Sermet-Gaudelus I, Durieu I, et al. The French
epithelial necrosis triggers neutrophilic inflammation via IL-1 Compassionate Program of elexacaftor–tezacaftor–ivacaftor in
receptor signaling in cystic fibrosis lung disease. people with cystic fibrosis with advanced lung disease and no
Am J Respir Crit Care Med 2015; 191: 902–13. F508del CFTR variant. Eur Respir J 2023; 2202437.
57 Livraghi-Butrico A, Kelly EJ, Klem ER, et al. Mucus clearance, 77 Sun X, Yi Y, Yan Z, et al. In utero and postnatal VX-770
MyD88-dependent and MyD88-independent immunity modulate administration rescues multiorgan disease in a ferret model of
lung susceptibility to spontaneous bacterial infection and cystic fibrosis. Sci Transl Med 2019; 11: eaau7531.
inflammation. Mucosal Immunol 2012; 5: 397–408.
78 McCague AF, Raraigh KS, Pellicore MJ, et al. Correlating cystic
58 Le Gars M, Descamps D, Roussel D, et al. Neutrophil elastase fibrosis transmembrane conductance regulator function with
degrades cystic fibrosis transmembrane conductance regulator via clinical features to inform precision treatment of cystic fibrosis.
calpains and disables channel function in vitro and in vivo. Am J Respir Crit Care Med 2019; 199: 1116–26.
Am J Respir Crit Care Med 2013; 187: 170–79.
79 McKone EF, Emerson SS, Edwards KL, Aitken ML. Effect of
59 Ribeiro CMP, Gentzsch M. Impact of airway inflammation on the genotype on phenotype and mortality in cystic fibrosis:
efficacy of CFTR modulators. Cells 2021; 10: 3260. a retrospective cohort study. Lancet 2003; 361: 1671–76.
60 Nichols DP, Morgan SJ, Skalland M, et al. Pharmacologic 80 Uluer AZ, MacGregor G, Azevedo P, et al. Safety and efficacy of
improvement of CFTR function rapidly decreases sputum pathogen vanzacaftor–tezacaftor–deutivacaftor in adults with cystic fibrosis:
density, but lung infections generally persist. J Clin Invest 2023; randomised, double-blind, controlled, phase 2 trials.
133: e167957. Lancet Respir Med 2023; 11: 550–62.
www.thelancet.com Vol 402 September 30, 2023 1197
Series
81 Veit G, Xu H, Dreano E, et al. Structure-guided combination 104 Albers S, Allen EC, Bharti N, et al. Engineered tRNAs suppress
therapy to potently improve the function of mutant CFTRs. Nat Med nonsense mutations in cells and in vivo. Nature 2023; 618: 842–48.
2018; 24: 1732–42. 105 Ko W, Porter JJ, Sipple MT, Edwards KM, Lueck JD. Efficient
82 Ghigo A, Murabito A, Sala V, et al. A PI3Kγ mimetic peptide suppression of endogenous CFTR nonsense mutations using
triggers CFTR gating, bronchodilation, and reduced inflammation anticodon-engineered transfer RNAs. Mol Ther Nucleic Acids 2022;
in obstructive airway diseases. Sci Transl Med 2022; 14: eabl6328. 28: 685–701.
83 Wilschanski M, Yahav Y, Yaacov Y, et al. Gentamicin-induced 106 Lueck JD, Yoon JS, Perales-Puchalt A, et al. Engineered transfer
correction of CFTR function in patients with cystic fibrosis and RNAs for suppression of premature termination codons.
CFTR stop mutations. N Engl J Med 2003; 349: 1433–41. Nat Commun 2019; 10: 822.
84 Leubitz A, Vanhoutte F, Hu MY, et al. A randomized, double-blind, 107 Amaral MD, Harrison PT. Development of novel therapeutics for all
placebo-controlled, multiple dose escalation study to evaluate the individuals with CF (the future goes on). J Cyst Fibros 2023;
safety and pharmacokinetics of ELX-02 in healthy subjects. 22 (suppl 1): S45–49.
Clin Pharmacol Drug Dev 2021; 10: 859–69. 108 Geurts MH, de Poel E, Pleguezuelos-Manzano C, et al. Evaluating
85 Kerem E. ELX-02: an investigational read-through agent for the CRISPR-based prime editing for cancer modeling and CFTR repair
treatment of nonsense mutation-related genetic disease. in organoids. Life Sci Alliance 2021; 4: e202000940.
Expert Opin Investig Drugs 2020; 29: 1347–54. 109 Geurts MH, de Poel E, Amatngalim GD, et al. CRISPR-based
86 Sharma J, Du M, Wong E, et al. A small molecule that induces adenine editors correct nonsense mutations in a cystic fibrosis
translational readthrough of CFTR nonsense mutations by eRF1 organoid biobank. Cell Stem Cell 2020; 26: 503–10.
depletion. Nat Commun 2021; 12: 4358. 110 Mayer-Hamblett N, Clancy JP, Jain R, et al. NAdvancing the
87 de Poel E, Spelier S, Suen SWF, et al. Functional restoration of pipeline of cystic fibrosis clinical trials: a new roadmap with a global
CFTR nonsense mutations in intestinal organoids. J Cyst Fibros trial network perspective. Lancet Respir Med 2023; published online
2022; 21: 246–53. Sept 9. https://doi.org/10.1016/S2213-2600(23)00297-7.
88 Mall MA. ENaC inhibition in cystic fibrosis: potential role in the 111 Addante A, Raymond W, Gitlin I, et al. A novel thiol-saccharide
new era of CFTR modulator therapies. Eur Respir J 2020; mucolytic for the treatment of muco-obstructive lung diseases.
56: 2000946. Eur Respir J 2023; 61: 2202022.
89 Ratjen F, Durham T, Navratil T, et al. Long term effects of denufosol 112 Ehre C, Rushton ZL, Wang B, et al. An improved inhaled mucolytic
tetrasodium in patients with cystic fibrosis. J Cyst Fibros 2012; to treat airway muco-obstructive diseases. Am J Respir Crit Care Med
11: 539–49. 2019; 199: 171–80.
90 Moss RB. Pitfalls of drug development: lessons learned from trials 113 Barth P, Bruijnzeel P, Wach A, et al. Single dose escalation studies
of denufosol in cystic fibrosis. J Pediatr 2013; 162: 676–80. with inhaled POL6014, a potent novel selective reversible inhibitor
91 Gentzsch M, Mall MA. Ion channel modulators in cystic fibrosis. of human neutrophil elastase, in healthy volunteers and subjects
Chest 2018; 154: 383–93. with cystic fibrosis. J Cyst Fibros 2020; 19: 299–304.
92 Danahay HL, Lilley S, Fox R, et al. TMEM16A potentiation: a novel 114 Chalmers JD, Haworth CS, Metersky ML, et al. Phase 2 trial of the
therapeutic approach for the treatment of cystic fibrosis. DPP-1 inhibitor brensocatib in bronchiectasis. N Engl J Med 2020;
Am J Respir Crit Care Med 2020; 201: 946–54. 383: 2127–37.
93 Sonneville F, Ruffin M, Coraux C, et al. MicroRNA-9 downregulates 115 Murray TS, Stanley G, Koff JL. Novel approaches to multidrug-
the ANO1 chloride channel and contributes to cystic fibrosis lung resistant infections in cystic fibrosis. Clin Chest Med 2022;
pathology. Nat Commun 2017; 8: 710. 43: 667–76.
94 Allaire NE, Griesenbach U, Kerem B, Lueck JD, Stanleigh N, 116 Trend S, Fonceca AM, Ditcham WG, Kicic A, Cf A. The potential of
Oren YS. Gene, RNA, and ASO-based therapeutic approaches in phage therapy in cystic fibrosis: essential human-bacterial-phage
Cystic Fibrosis. J Cyst Fibros 2023; 22 (suppl 1): S39–44. interactions and delivery considerations for use in Pseudomonas
95 Harrison PT. CFTR RNA- and DNA-based therapies. aeruginosa-infected airways. J Cyst Fibros 2017; 16: 663–70.
Curr Opin Pharmacol 2022; 65: 102247. 117 Sanya DRA, Onésime D, Vizzarro G, Jacquier N. Recent advances
96 McLachlan G, Alton EWFW, Boyd AC, et al. Progress in respiratory in therapeutic targets identification and development of treatment
gene therapy. Hum Gene Ther 2022; 33: 893–912. strategies towards Pseudomonas aeruginosa infections.
BMC Microbiol 2023; 23: 86.
97 Rowe SM, Zuckerman JB, Dorgan D, et al. Inhaled mRNA therapy
for treatment of cystic fibrosis: Interim results of a randomized, 118 Ong T, Ramsey BW. Cystic fibrosis: a review. JAMA 2023;
double-blind, placebo-controlled phase 1/2 clinical study. 329: 1859–71.
J Cyst Fibros 2023; published online April 29. https://doi. 119 Elborn JS, Blasi F, Burgel PR, Peckham D. Role of inhaled
org/10.1016/j.jcf.2023.04.008. antibiotics in the era of highly effective CFTR modulators.
98 Mitomo K, Griesenbach U, Inoue M, et al. Toward gene therapy for Eur Respir Rev 2023; 32: 220154.
cystic fibrosis using a lentivirus pseudotyped with Sendai virus 120 Barton TE, Frost F, Fothergill JL, Neill DR. Challenges and
envelopes. Mol Ther 2010; 18: 1173–82. opportunities in the development of novel antimicrobial
99 Alton EW, Beekman JM, Boyd AC, et al. Preparation for a first-in- therapeutics for cystic fibrosis. J Med Microbiol 2022; published
man lentivirus trial in patients with cystic fibrosis. Thorax 2017; online Dec 21. https://doi.org/10.1099/jmm.0.001643.
72: 137–47. 121 Mall MA, Criner GJ, Miravitlles M, et al. Cystic fibrosis
100 Finkel RS, Chiriboga CA, Vajsar J, et al. Treatment of infantile-onset transmembrane conductance regulator in COPD: a role in
spinal muscular atrophy with nusinersen: a phase 2, open-label, respiratory epithelium and beyond. Eur Respir J 2023; 61: 2201307.
dose-escalation study. Lancet 2016; 388: 3017–26. 122 Dunican EM, Elicker BM, Henry T, et al. Mucus plugs and
101 Mendell JR, Goemans N, Lowes LP, et al. Longitudinal effect of emphysema in the pathophysiology of airflow obstruction and
eteplirsen versus historical control on ambulation in Duchenne hypoxemia in smokers. Am J Respir Crit Care Med 2021; 203: 957–68.
muscular dystrophy. Ann Neurol 2016; 79: 257–71. 123 Chalmers JD, Chang AB, Chotirmall SH, Dhar R, McShane PJ.
102 Oren YS, Irony-Tur Sinai M, Golec A, et al. Antisense Bronchiectasis. Nat Rev Dis Primers 2018; 4: 45.
oligonucleotide-based drug development for cystic fibrosis patients
carrying the 3849+10 kb C-to-T splicing mutation. J Cyst Fibros 2021; Copyright © 2023 Elsevier Ltd. All rights reserved.
20: 865–75.
103 Oren YS, Avizur-Barchad O, Ozeri-Galai E, et al. Antisense
oligonucleotide splicing modulation as a novel cystic fibrosis
therapeutic approach for the W1282X nonsense mutation.
J Cyst Fibros 2022; 21: 630–36.
1198 www.thelancet.com Vol 402 September 30, 2023
You might also like
- Seniors 2013: Belen High School & Infinity High SchoolDocument16 pagesSeniors 2013: Belen High School & Infinity High SchoolVCNews-BulletinNo ratings yet
- Arcitura Microservice ArchitectDocument20 pagesArcitura Microservice Architecttest test0% (2)
- The Future of Cystic Fibrosis Care: A Global PerspectiveDocument60 pagesThe Future of Cystic Fibrosis Care: A Global PerspectiveAdam ClarkeNo ratings yet
- Comment: Pseudomonas Aeruginosa. CFTR Modulator TherapiesDocument2 pagesComment: Pseudomonas Aeruginosa. CFTR Modulator TherapiesBrenda RodriguesNo ratings yet
- FQ Revison Lancet 2020Document60 pagesFQ Revison Lancet 2020Adriana AsturizagaNo ratings yet
- The Journal of Pathology - 2023 - Jones - Recent Advances in Pathology The 2023 Annual Review Issue of The Journal ofDocument3 pagesThe Journal of Pathology - 2023 - Jones - Recent Advances in Pathology The 2023 Annual Review Issue of The Journal ofShahid ShaikhNo ratings yet
- Immunotherapy in Triple-Negative Breast Cancer - Insights Into Tumor Immune Landscape and Therapeutic OpportunitiesDocument25 pagesImmunotherapy in Triple-Negative Breast Cancer - Insights Into Tumor Immune Landscape and Therapeutic OpportunitiesLee Foo WengNo ratings yet
- The Journal of Pathology CR - 2024 - Knight - The Glasgow Microenvironment Score An Exemplar of Contemporary BiomarkerDocument16 pagesThe Journal of Pathology CR - 2024 - Knight - The Glasgow Microenvironment Score An Exemplar of Contemporary Biomarkerenrichedenlightenment05No ratings yet
- Advances in Cancer Immunotherapy 2019 - Latest TrendsDocument21 pagesAdvances in Cancer Immunotherapy 2019 - Latest TrendsSWAGATIKA CHANDANo ratings yet
- RCCM 201910-1943SODocument16 pagesRCCM 201910-1943SOanu deepNo ratings yet
- Molecular Biomarkers of Bladder Cancer: A Mini-ReviewDocument10 pagesMolecular Biomarkers of Bladder Cancer: A Mini-ReviewaldyNo ratings yet
- 1 s2.0 S1567576924004533 MainDocument10 pages1 s2.0 S1567576924004533 Mainmincuandrada10No ratings yet
- Fimmu 14 1326374Document3 pagesFimmu 14 1326374Maria PopescuNo ratings yet
- The Role of Automated Cytometry in The New Era of Cancer Immunotherapy (Review)Document7 pagesThe Role of Automated Cytometry in The New Era of Cancer Immunotherapy (Review)Andrea SbranaNo ratings yet
- 1 s2.0 S1040842820302067 MainDocument10 pages1 s2.0 S1040842820302067 MainbrendaNo ratings yet
- Ascierto 2018Document14 pagesAscierto 2018TrabelsiNo ratings yet
- Targeted Therapies To Improve CFTR Function in CysDocument17 pagesTargeted Therapies To Improve CFTR Function in CysAnthony Bravo CortezNo ratings yet
- Lung Cancer ProjectDocument92 pagesLung Cancer ProjectMICHAEL ADEYEMONo ratings yet
- Propofol-TIVA Versus Inhalational Anesthesia For Cancer SurgeryDocument9 pagesPropofol-TIVA Versus Inhalational Anesthesia For Cancer SurgerygonjdelzNo ratings yet
- José Domínguez Clinical Implications of MolecularDocument16 pagesJosé Domínguez Clinical Implications of MolecularcarolNo ratings yet
- Molecular Profiling in Muscle-Invasive Bladder Cancer: More Than The Sum of Its PartsDocument11 pagesMolecular Profiling in Muscle-Invasive Bladder Cancer: More Than The Sum of Its PartsJoel ChávezdrumsNo ratings yet
- Airway Microbiota As A Modulator of Lung Cancer: Molecular SciencesDocument19 pagesAirway Microbiota As A Modulator of Lung Cancer: Molecular SciencesFirman Kusuma AtmajaNo ratings yet
- Fphar 10 01137Document8 pagesFphar 10 01137Kajelcha FikaduNo ratings yet
- The Effect of Anesthetic Technique On - Opioid Receptor Expression and Immune Cell Infiltration in Breast CancerDocument5 pagesThe Effect of Anesthetic Technique On - Opioid Receptor Expression and Immune Cell Infiltration in Breast CanceroliviafabitaNo ratings yet
- Phenotypic, Functional, and Metabolic Heterogeneity of Immune Cells Infiltrating Non Small Cell Lung CancerDocument14 pagesPhenotypic, Functional, and Metabolic Heterogeneity of Immune Cells Infiltrating Non Small Cell Lung CancerWilliamRayCassidyNo ratings yet
- Selle2015 PDFDocument12 pagesSelle2015 PDFatikha apriliaNo ratings yet
- Fimmu 11 577869Document18 pagesFimmu 11 577869nataliaNo ratings yet
- Systematic Review of The Role of Corticosteroids in Cervicofacial InfectionsDocument11 pagesSystematic Review of The Role of Corticosteroids in Cervicofacial InfectionsLesly Karem Chávez RimacheNo ratings yet
- Hepatocellular Carcinoma: Clinical Frontiers and PerspectivesDocument13 pagesHepatocellular Carcinoma: Clinical Frontiers and PerspectivesMisnariahIdrusNo ratings yet
- Drake 2006Document3 pagesDrake 2006Ruben NatarîșNo ratings yet
- Diagnostic Strategy of Metagenomic Next-Generation Sequuencing For Gram Negative Bacteria in Respiratory InfectionsDocument7 pagesDiagnostic Strategy of Metagenomic Next-Generation Sequuencing For Gram Negative Bacteria in Respiratory Infectionsd4rkgr455No ratings yet
- Copd 14 2219Document9 pagesCopd 14 2219Ruby FirdausNo ratings yet
- Pittsburgh Lung Conference: PneumoniaDocument4 pagesPittsburgh Lung Conference: PneumoniaYudha Rental'sNo ratings yet
- LancetDocument11 pagesLancetvieira.beatrizNo ratings yet
- Pneumonita ICI-related in NSCLCDocument9 pagesPneumonita ICI-related in NSCLCAndrei BuruianăNo ratings yet
- Cancer Immunotherapy Meets Oncology: In Honor of Christoph HuberFrom EverandCancer Immunotherapy Meets Oncology: In Honor of Christoph HuberCedrik Michael BrittenNo ratings yet
- Ni Hms 957840Document19 pagesNi Hms 957840dokterlisaNo ratings yet
- EORTC Guidelines 2017Document18 pagesEORTC Guidelines 2017Cata RodriguezNo ratings yet
- Promises and Challenges of Adoptive T-Cell Therapies For Solid TumoursDocument18 pagesPromises and Challenges of Adoptive T-Cell Therapies For Solid TumoursdianaNo ratings yet
- The Role of CD44 in Cancer Chemoresistance A Concise ReviewDocument13 pagesThe Role of CD44 in Cancer Chemoresistance A Concise ReviewZihao WuNo ratings yet
- Bergh 2013Document4 pagesBergh 2013bixagif369No ratings yet
- Internal Medicine Journal - 2021 - Teh - Consensus Guidelines For Antifungal Prophylaxis in Haematological Malignancy andDocument22 pagesInternal Medicine Journal - 2021 - Teh - Consensus Guidelines For Antifungal Prophylaxis in Haematological Malignancy andLeva IonutNo ratings yet
- 2023 Monteleone Tagerted Therapy of IL34 As A Prmosing Approach To Overcome Cancer ResistanceDocument12 pages2023 Monteleone Tagerted Therapy of IL34 As A Prmosing Approach To Overcome Cancer Resistancephilippe.lacroix38490No ratings yet
- PIIS2213260022005355Document16 pagesPIIS2213260022005355evelyn.minichNo ratings yet
- Shifting Paradigms of Nontuberculous Mycobacteria in Cystic FibrosisDocument6 pagesShifting Paradigms of Nontuberculous Mycobacteria in Cystic FibrosisRezky Fitria YandraNo ratings yet
- Cancer ModellingDocument15 pagesCancer ModellingAzza Ahmed100% (1)
- Church 2015Document1 pageChurch 2015TrabelsiNo ratings yet
- Bronchiectasis - NonCFDocument10 pagesBronchiectasis - NonCFNiniek Iin FNo ratings yet
- TX CancerDocument5 pagesTX CancerChelsea Reyna TolentinoNo ratings yet
- Imun PDFDocument4 pagesImun PDFLeyni SabatiniNo ratings yet
- Bussines EngineringDocument9 pagesBussines EngineringWhulan Rhana TonapaNo ratings yet
- Immune Crosstalk in Cancer Progression and Metatic Spread (2020)Document15 pagesImmune Crosstalk in Cancer Progression and Metatic Spread (2020)EshaNo ratings yet
- Breast Cancer and Biomedical Informatics: The Prognochip ProjectDocument6 pagesBreast Cancer and Biomedical Informatics: The Prognochip ProjectRuanita VeigaNo ratings yet
- Cancers Make Their Own Luck - Theories of Cancer OriginsDocument15 pagesCancers Make Their Own Luck - Theories of Cancer Originszhe zhNo ratings yet
- 10.1007/978 3 662 46410 6Document522 pages10.1007/978 3 662 46410 6Francisco Ibañez Irribarra100% (1)
- The Immunoscore: Colon Cancer and BeyondDocument24 pagesThe Immunoscore: Colon Cancer and BeyondcollianairaNo ratings yet
- Management of Pulmonary Metastases: A Narrative Review On The Oncologist's PerspectiveDocument18 pagesManagement of Pulmonary Metastases: A Narrative Review On The Oncologist's Perspectivetdywaweru5No ratings yet
- GENETHERAPYDocument10 pagesGENETHERAPYylttravelsNo ratings yet
- 七大地方性真菌诊疗指南 欧洲2021Document11 pages七大地方性真菌诊疗指南 欧洲2021zzqNo ratings yet
- Bioinformatics For Precision Medicine in Oncology Principles and Application To The SHIVA Clinical TrialDocument17 pagesBioinformatics For Precision Medicine in Oncology Principles and Application To The SHIVA Clinical Trial伊伊No ratings yet
- Nac Etiologia Implicacion para La Seleccion de La Poblacion Diseño de Estudios Cid 2008Document4 pagesNac Etiologia Implicacion para La Seleccion de La Poblacion Diseño de Estudios Cid 2008Gustavo GomezNo ratings yet
- Diagnosis of Endometrial Biopsies and Curettings: A Practical ApproachFrom EverandDiagnosis of Endometrial Biopsies and Curettings: A Practical ApproachNo ratings yet
- Complete The Sentences With The Correct Past FormDocument3 pagesComplete The Sentences With The Correct Past FormNinia BilbaoNo ratings yet
- Pte Mag PDFDocument68 pagesPte Mag PDFhollowNo ratings yet
- The Structure Pattern of Ngrasani GossipDocument14 pagesThe Structure Pattern of Ngrasani GossipCyrielle GbNo ratings yet
- Making Words LPDocument6 pagesMaking Words LPapi-282019703100% (1)
- HuhuDocument1 pageHuhuBelle RoseNo ratings yet
- An Open Letter To LG - From AAP Delhi ConvenorDocument2 pagesAn Open Letter To LG - From AAP Delhi ConvenorFirstpostNo ratings yet
- Arya Samaj PDFDocument368 pagesArya Samaj PDFÁlex TremoNo ratings yet
- Business Model Innovation in PDocument8 pagesBusiness Model Innovation in PahmadNo ratings yet
- Beautiful From WithinDocument87 pagesBeautiful From WithinHenrique AlissonNo ratings yet
- Differential GeometryDocument125 pagesDifferential Geometrynimbigli7943100% (1)
- CWTS Reviewer Module 1 4Document7 pagesCWTS Reviewer Module 1 4Aether SkywardNo ratings yet
- Stuart A Green LTC USN Cognitive Warfare and The Role of The Media FinalDocument13 pagesStuart A Green LTC USN Cognitive Warfare and The Role of The Media FinalPrometheo100% (1)
- Assessment II - Project ManagementDocument21 pagesAssessment II - Project ManagementJürg Müller0% (2)
- Contemporary ArtsDocument7 pagesContemporary ArtsAngel Padilla CatacutanNo ratings yet
- Owens Cmty Coll ToledoDocument145 pagesOwens Cmty Coll ToledoHarpreet BolaNo ratings yet
- Ocb LoadDocument74 pagesOcb Loadneeraj kumar singh100% (2)
- Worksheet On EidsDocument3 pagesWorksheet On Eidszewdie.nataniaNo ratings yet
- 6 Psychoanalytic Theory: Clues From The Brain: Commentary by Joseph LeDoux (New York)Document7 pages6 Psychoanalytic Theory: Clues From The Brain: Commentary by Joseph LeDoux (New York)Maximiliano PortilloNo ratings yet
- USSH - Writing B1 - TopicsDocument2 pagesUSSH - Writing B1 - TopicsMu MiNo ratings yet
- DocumentDocument3 pagesDocumentJunko CaytonNo ratings yet
- Final Project IkbalDocument60 pagesFinal Project Ikbalikbal666No ratings yet
- Bar Review Institute University of The Philippines College of Law Last Minute Tips in Mercantile Law BAR 2020/2021Document11 pagesBar Review Institute University of The Philippines College of Law Last Minute Tips in Mercantile Law BAR 2020/2021Suprema LexNo ratings yet
- The Organizational Career - Not Dead But in Need of Redefinition (Clarke, M. 2012)Document21 pagesThe Organizational Career - Not Dead But in Need of Redefinition (Clarke, M. 2012)Pickle_PumpkinNo ratings yet
- Lean Six Sigma Measure Phase Tollgate TemplateDocument41 pagesLean Six Sigma Measure Phase Tollgate TemplateSteven Bonacorsi100% (16)
- Atal Bihari VajpayeeDocument33 pagesAtal Bihari VajpayeeFiraFfirehsNo ratings yet
- Selected Articles by Eminent Authors 1 PDFDocument244 pagesSelected Articles by Eminent Authors 1 PDFabdullaNo ratings yet
- Stress QuestionnaireDocument2 pagesStress Questionnairehammads88100% (1)
- Lululemon LetterDocument5 pagesLululemon LetterCNBCDigitalNo ratings yet