Professional Documents
Culture Documents
QCHMWRV F4 FJ 7 XJ Q9 DW 6 Q8 P B
QCHMWRV F4 FJ 7 XJ Q9 DW 6 Q8 P B
Uploaded by
Favio Alvarez De BejarCopyright:
Available Formats
You might also like
- Sataloff's Comprehensive Textbook of Otolaryngology Head and Neck Surgery - Vol2 (2016) .Unitedvrg Rhinology Allergy ImmunologyDocument979 pagesSataloff's Comprehensive Textbook of Otolaryngology Head and Neck Surgery - Vol2 (2016) .Unitedvrg Rhinology Allergy ImmunologyChandramohan Setty50% (2)
- Textbook of Surgery For Dental StudentssDocument399 pagesTextbook of Surgery For Dental StudentssDiana Mihaela Ilie50% (2)
- Duties of Scrub Nurse & Circulating NurseDocument2 pagesDuties of Scrub Nurse & Circulating Nurseimafashionista90% (21)
- 404 Veterinary Referral Hospital - BrochureDocument11 pages404 Veterinary Referral Hospital - BrochureJoanne FagnouNo ratings yet
- Basic Dental Implant SurgeryDocument33 pagesBasic Dental Implant Surgerymuhammad100% (1)
- Delays in Imaging Diagnosis of Acute Abdominal PainDocument7 pagesDelays in Imaging Diagnosis of Acute Abdominal PainWillie VanegasNo ratings yet
- Multimodality Approach For Imaging of Non-Traumatic Acute Abdominal EmergenciesDocument13 pagesMultimodality Approach For Imaging of Non-Traumatic Acute Abdominal EmergenciesfalisNo ratings yet
- Indicacoes Exames Complementares de Imagem No AbdomeDocument12 pagesIndicacoes Exames Complementares de Imagem No AbdomeHannaNo ratings yet
- Abdominal Ultrasound For Pediatric Blunt Trauma FAST Is Not Always BetterDocument3 pagesAbdominal Ultrasound For Pediatric Blunt Trauma FAST Is Not Always BetterInryuu ZenNo ratings yet
- 2017 - Practical Approach To Imaging of The Pediatric Acute AbdomenDocument18 pages2017 - Practical Approach To Imaging of The Pediatric Acute AbdomenRevivo RindaNo ratings yet
- 268 2010 Article 694Document8 pages268 2010 Article 694I Gusti Rai SutrawanNo ratings yet
- Original ArticleDocument5 pagesOriginal ArticlehengkyNo ratings yet
- Indications For Abdominal Imaging: When and What To Choose?Document12 pagesIndications For Abdominal Imaging: When and What To Choose?musdalifahNo ratings yet
- Surgeon-Performed Ultrasound As A Diagnostic Tool in AppendicitisDocument6 pagesSurgeon-Performed Ultrasound As A Diagnostic Tool in Appendicitisansar ahmedNo ratings yet
- Cervical Angiograms in Cervical Spine Trauma Patients 5 Years After The Data: Has Practice Changed?Document4 pagesCervical Angiograms in Cervical Spine Trauma Patients 5 Years After The Data: Has Practice Changed?edi_wsNo ratings yet
- Online Radiography Continuing EducationDocument39 pagesOnline Radiography Continuing EducationAndy WijayaNo ratings yet
- PEDIATRIC Blunt Abdominal Injury MGMT Guidelines AlgorithmDocument6 pagesPEDIATRIC Blunt Abdominal Injury MGMT Guidelines AlgorithmHaidir MuhammadNo ratings yet
- Iaim 2015 0206 17Document13 pagesIaim 2015 0206 17fahrunisaNo ratings yet
- Preoperative Computed Tomography Angiography in Autologous Breast Reconstruction-Incidence and Impact of IncidentalomasDocument6 pagesPreoperative Computed Tomography Angiography in Autologous Breast Reconstruction-Incidence and Impact of IncidentalomasNora Vianey Alcantara VelascoNo ratings yet
- Ditkofsky 2015Document28 pagesDitkofsky 2015Allython Jureth Peña ReyesNo ratings yet
- Abdomino-Pelvic CT Project Work UPDATED - 105912 - 020107 - 011052Document36 pagesAbdomino-Pelvic CT Project Work UPDATED - 105912 - 020107 - 011052sommylydiiNo ratings yet
- Entero SequencesDocument12 pagesEntero SequencesKelvin SueyzyNo ratings yet
- Cervical Spine Clearance 2009Document7 pagesCervical Spine Clearance 2009Abdulelah Al.luhaybiNo ratings yet
- PIIS0196064418311594Document8 pagesPIIS0196064418311594NanaNo ratings yet
- Focused Sonography in Detecting Hemoperitoneum in Blunt Abdominal Trauma Patients, Correlation With Computed TomographyDocument6 pagesFocused Sonography in Detecting Hemoperitoneum in Blunt Abdominal Trauma Patients, Correlation With Computed TomographyDhaniNo ratings yet
- EcografiaMedicinaInterna InternaDocument7 pagesEcografiaMedicinaInterna InternaGinés López MartínezNo ratings yet
- Proposal New - 060952Document33 pagesProposal New - 060952sommylydiiNo ratings yet
- To Determine Validity of Ultrasound in Predicting Acute Appendicitis AmongDocument6 pagesTo Determine Validity of Ultrasound in Predicting Acute Appendicitis AmongIkki DongNo ratings yet
- The Role of Imaging in Cervical Cancer Staging - ESGOESTROESP Guidelines (Update 2023)Document32 pagesThe Role of Imaging in Cervical Cancer Staging - ESGOESTROESP Guidelines (Update 2023)Limbert Rodríguez TiconaNo ratings yet
- Musculosketal Imaging in Physical TherapyDocument14 pagesMusculosketal Imaging in Physical TherapyWasemBhatNo ratings yet
- Structured Versus Narrative Reporting of Pelvic MRI in Perianal Fistulizing Disease: Impact On Clarity, Completeness, and Surgical PlanningDocument10 pagesStructured Versus Narrative Reporting of Pelvic MRI in Perianal Fistulizing Disease: Impact On Clarity, Completeness, and Surgical PlanningqrscentralNo ratings yet
- WP Esaote Vnav Ob-GynDocument4 pagesWP Esaote Vnav Ob-Gynapi-237460689No ratings yet
- 2 - From FAST To E FAST An Overview of The Evolution of Ultrasound Based Traumatic Injury AssessmentDocument8 pages2 - From FAST To E FAST An Overview of The Evolution of Ultrasound Based Traumatic Injury AssessmentMarcelo RibeiroNo ratings yet
- Performance and Practice Guidelines For Excisional Breast BiopsyDocument4 pagesPerformance and Practice Guidelines For Excisional Breast BiopsyPPDS Bedah FK UNRI Angkatan 2No ratings yet
- Role of Computed Tomography (CT) Scan in Staging of Cervical CarcinomaDocument6 pagesRole of Computed Tomography (CT) Scan in Staging of Cervical CarcinomaTriponiaNo ratings yet
- The Role of Abdominal X-Rays in The Investigation of Suspected Acute AppendicitisDocument5 pagesThe Role of Abdominal X-Rays in The Investigation of Suspected Acute AppendicitisFitri RachmadaniNo ratings yet
- Expert Consensus Contouring Guidelines For Intensity Modulated Radiation Therapy in Esophageal and Gastroesophageal Junction CancerDocument10 pagesExpert Consensus Contouring Guidelines For Intensity Modulated Radiation Therapy in Esophageal and Gastroesophageal Junction CancermarrajoanaNo ratings yet
- болезнь КронаDocument7 pagesболезнь КронаAlexander NatroshviliNo ratings yet
- Blunt Abdiminal TraumaDocument6 pagesBlunt Abdiminal TraumaErdyNo ratings yet
- Jo Clinical Oncology AssignmentDocument10 pagesJo Clinical Oncology Assignmentapi-711592723No ratings yet
- PalateDocument41 pagesPalatearif sudiantoNo ratings yet
- Historical Overview: Abstract: Several Studies Have Demonstrated That A Diagnosis Based SolelyDocument8 pagesHistorical Overview: Abstract: Several Studies Have Demonstrated That A Diagnosis Based SolelyLuh Tu PebriyantiNo ratings yet
- BJR 85 1029Document9 pagesBJR 85 1029Anna MariaNo ratings yet
- Bandi 2008 Chest Wall InvasionDocument6 pagesBandi 2008 Chest Wall Invasionmarvic gabitanNo ratings yet
- DTSCH Arztebl Int-115 0031Document12 pagesDTSCH Arztebl Int-115 0031Monika Diaz KristyanindaNo ratings yet
- JTD 11 03 936Document8 pagesJTD 11 03 936Heru SigitNo ratings yet
- Abdominal USG in EDDocument9 pagesAbdominal USG in EDanon_773331597No ratings yet
- DMFR 20170301Document7 pagesDMFR 20170301Ana PaulaNo ratings yet
- Ultrasound in Gynecology and ObstetricsDocument197 pagesUltrasound in Gynecology and ObstetricsAli Murtaza AbbasNo ratings yet
- 0100 3984 RB 51 06 0VII PDFDocument2 pages0100 3984 RB 51 06 0VII PDFMarcelitaTaliaDuwiriNo ratings yet
- Clinical Anatomy - 2020 - Le Saint Grant - Arterial Anatomy of The Anterior Abdominal Wall Ultrasound Evaluation As ADocument6 pagesClinical Anatomy - 2020 - Le Saint Grant - Arterial Anatomy of The Anterior Abdominal Wall Ultrasound Evaluation As AarifNo ratings yet
- He 2016Document5 pagesHe 2016Anonymous 44bTHDeHkbNo ratings yet
- Fafaj2021 Tanaka Score ReliabilityDocument6 pagesFafaj2021 Tanaka Score ReliabilityEham AroraNo ratings yet
- 2009 PelvimetryDocument5 pages2009 PelvimetryayupurnamasariiNo ratings yet
- 1618 4726 1 PB PDFDocument6 pages1618 4726 1 PB PDFDrive IyasNo ratings yet
- Comprehensive Ultrasound Diagnosis For Intraductal Spread of Primary Breast CancerDocument10 pagesComprehensive Ultrasound Diagnosis For Intraductal Spread of Primary Breast CancerferdiNo ratings yet
- Management Guidelines For Penetrating Abdominal Trauma: Walter L. Biffl and Ernest E. MooreDocument9 pagesManagement Guidelines For Penetrating Abdominal Trauma: Walter L. Biffl and Ernest E. MooreArsy Mira PertiwiNo ratings yet
- Clinical Oncology AssignmentDocument9 pagesClinical Oncology Assignmentapi-691277740No ratings yet
- POZE Professor - Dr. - Dieter - Beyer, - Professor - Dr. - Ulrich - (B-Ok - CC) PDFDocument463 pagesPOZE Professor - Dr. - Dieter - Beyer, - Professor - Dr. - Ulrich - (B-Ok - CC) PDFUffie-Isabela GheNo ratings yet
- The Incidence and Risk of Early Postoperative Small Bowel Obstruction After Laparoscopic Resection For Colorectal Cancer 2014Document7 pagesThe Incidence and Risk of Early Postoperative Small Bowel Obstruction After Laparoscopic Resection For Colorectal Cancer 2014alemago90No ratings yet
- Thoracoscopy:: A Real-Life PerspectiveDocument6 pagesThoracoscopy:: A Real-Life Perspective1411731No ratings yet
- A New Classification For Surgical NEC During Exploratory Laparotomy: Introduction and Reproducibility AssessmentDocument9 pagesA New Classification For Surgical NEC During Exploratory Laparotomy: Introduction and Reproducibility AssessmentCirugia Pediatrica La RazaNo ratings yet
- 10 1053@j Semnuclmed 2020 07 005Document10 pages10 1053@j Semnuclmed 2020 07 005anon_813722240No ratings yet
- Management of Postoperative HypoxemiaDocument14 pagesManagement of Postoperative HypoxemiaFavio Alvarez De BejarNo ratings yet
- Population Preference For Treatment of Uncomplicated AppendicitisDocument6 pagesPopulation Preference For Treatment of Uncomplicated AppendicitisFavio Alvarez De BejarNo ratings yet
- Human Water and Electrolyte BalanceDocument10 pagesHuman Water and Electrolyte BalanceFavio Alvarez De BejarNo ratings yet
- Towards Evidence-Based and Personalised Care of Acute PancreatitisDocument7 pagesTowards Evidence-Based and Personalised Care of Acute PancreatitisFavio Alvarez De BejarNo ratings yet
- ProstatectomyDocument9 pagesProstatectomymardsz100% (1)
- Ca. Ca.: - .,.1b1h1tlesDocument179 pagesCa. Ca.: - .,.1b1h1tleshNo ratings yet
- Laser Innovation: Ease of Use Battery Powered Green Aiming BeamDocument2 pagesLaser Innovation: Ease of Use Battery Powered Green Aiming BeamNatalia PalarieNo ratings yet
- Rüsch Urology: For Almost Every ApplicationDocument72 pagesRüsch Urology: For Almost Every ApplicationSaad MouatassimNo ratings yet
- Metzenbaum Scissors Are Surgical: Scissors Tissue Tungsten CarbideDocument5 pagesMetzenbaum Scissors Are Surgical: Scissors Tissue Tungsten CarbideRhea Leliza PrudenteNo ratings yet
- Robotic HysterectomyDocument14 pagesRobotic HysterectomyPrincess Brigitte R. PATE�ANo ratings yet
- 2024 USFSSTG001V4 US DeLorean STG Rev1aDocument70 pages2024 USFSSTG001V4 US DeLorean STG Rev1aNathaly GuevaraNo ratings yet
- Vascular InjuryDocument26 pagesVascular InjuryEka NataNo ratings yet
- Musculoskeletal Physical TherapyDocument5 pagesMusculoskeletal Physical TherapyAbiha AnisNo ratings yet
- Supraglottic Airway Devices A Review in A New Era of Airway Management 2155 6148 1000647Document9 pagesSupraglottic Airway Devices A Review in A New Era of Airway Management 2155 6148 1000647Riris SihotangNo ratings yet
- Cardiac Surgery TextbookDocument2 pagesCardiac Surgery Textbookoguzguneri2010No ratings yet
- DM General Surgery CurriculumDocument45 pagesDM General Surgery CurriculumGiovanni HenryNo ratings yet
- ACHQC Abdominal Core Surgery Rehabilitation Protocol Patient Guide 6.17.20Document43 pagesACHQC Abdominal Core Surgery Rehabilitation Protocol Patient Guide 6.17.20Brka223No ratings yet
- Use Only: Anesthetics Considerations in PeritonitisDocument9 pagesUse Only: Anesthetics Considerations in Peritonitisade_liaNo ratings yet
- Surgery For Recurrent Soft Tissue SarcomaDocument584 pagesSurgery For Recurrent Soft Tissue SarcomaAr-pardo RogerNo ratings yet
- Comments From The Injured Worker SurveyDocument117 pagesComments From The Injured Worker Surveyvaluecare1542No ratings yet
- Knowledge, Attitude and Perception of Patients.9Document6 pagesKnowledge, Attitude and Perception of Patients.9KarlaPadrelananNo ratings yet
- 03 Bartholin Gland Procedure + Inform ConsentDocument4 pages03 Bartholin Gland Procedure + Inform ConsentelenNo ratings yet
- Hospital Case CardiacDocument3 pagesHospital Case CardiacAnup MohapatraNo ratings yet
- Argumentative Writing - PresentationDocument2 pagesArgumentative Writing - PresentationMaria Cecilia Annette RahardjaNo ratings yet
- Preoperative AssessmentDocument3 pagesPreoperative AssessmentStepyn SalvadorNo ratings yet
- Not For Reproduction: Doctor'S Order/Nurse'S Compliance Sheet (Authenticate All Orders)Document2 pagesNot For Reproduction: Doctor'S Order/Nurse'S Compliance Sheet (Authenticate All Orders)Mcgee OcnicnatNo ratings yet
- Pre-Board Exam For July 2011 NLEDocument37 pagesPre-Board Exam For July 2011 NLEdammenoel100% (2)
- Mindanao Sanitarium & Hospital College: Brgy San Miguel, Iligan City 9200Document5 pagesMindanao Sanitarium & Hospital College: Brgy San Miguel, Iligan City 9200Kabang MoaNo ratings yet
- Blue 783 Clinical Management of Jehovahs Witnesses and Other Patients Who Refuse Blood ComponentsDocument21 pagesBlue 783 Clinical Management of Jehovahs Witnesses and Other Patients Who Refuse Blood ComponentsMarkez CharlezNo ratings yet
QCHMWRV F4 FJ 7 XJ Q9 DW 6 Q8 P B
QCHMWRV F4 FJ 7 XJ Q9 DW 6 Q8 P B
Uploaded by
Favio Alvarez De BejarOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
QCHMWRV F4 FJ 7 XJ Q9 DW 6 Q8 P B
QCHMWRV F4 FJ 7 XJ Q9 DW 6 Q8 P B
Uploaded by
Favio Alvarez De BejarCopyright:
Available Formats
DOI: 10.
1590/0100-6991e-20223172en Scientific comunication
DECOMP Report: Answers surgeons expect from an abdominal
wall imaging exam
Relatório DECOMP: Respostas que os cirurgiões esperam de um exame de
imagem da parede abdominal
Christiano Marlo Paggi Claus1 ; Marcio Cavalieiri2; Flávio Malcher3; Carlos Trippia4; Antonio Luis Eiras-Araujo5; Eric Pauli6;
Leandro Totti Cavazzola7.
A B S T R A C T
Abdominal wall (AW) hernias are a common problem faced by general surgeons. With an essentially clinical diagnosis, abdominal hernias
have been considered a simple problem to be repaired. However, long-term follow-up of patients has shown disappointing results, both
in terms of complications and recurrence. In this context, preoperative planning with control of comorbidities and full knowledge of the
hernia and its anatomical relationships with the AW has gained increasing attention. Computed tomography (CT) appears to be the best
option to determine the precise size and location of abdominal hernias, presence of rectus diastase and/or associated muscle atrophy,
as well as the proportion of the hernia in relation to the AW itself. This information might help the surgeon to choose the best surgical
technique (open vs MIS), positioning and fixation of the meshes, and eventual need for application of botulinum toxin, preoperative
pneumoperitoneum or component separation techniques. Despite the relevance of the findings, they are rarely described in CT scans
as radiologists are not used to report findings of the AW as well as to know what information is really needed. For these reasons, we
gathered a group of surgeons and radiologists to establish which information about the AW is important in a CT. Finally, a structured
report is proposed to facilitate the description of the findings and their interpretation.
Keywords: Hernia. Hernia, Abdominal. Tomography. Radiology.
TECHNICAL NOTE scar. Imaging may help surgeons on surgical planning.
The size and content of the hernia, the volume of the
F or many years, the diagnosis and evaluation of hernias
of the abdominal wall (AW) was made through physical
examination and it was considered a waste to request an
hernia sac, the hernia’s proximity to bone structures or
even associated muscle atrophy can all be determined on
imaging. These guide the need for preoperative measures
imaging study to evaluate “only” a hernia. The diagnosis or intra-operative measures to increase the compliance/
is usually clinical, based on symptoms and physical volume of the abdominal cavity, define the approximate
examination. Increasingly, however, surgeons interested size, best position for mesh and mesh fixation methods
in hernia repair find utility in imaging exams1. They may and well as suggest both perioperative risks and
be necessary to confirm hernia defect size, for example a postoperative results2-4.
hernia occurring in the setting of obesity or an incisional Ultrasonography (US), computed tomography
hernia with multiple defects under a fibrotic surgical (CT) or magnetic resonance imaging (MRI) all have value
1 - Universidade Positivo, Clínica Cirúrgica e Cirurgia Minimamente Invasiva - Curitiba - PR - Brasil 2 - Hospital Municipal Lourenço Jorge, Clínica Ci-
rúrgica - Rio de Janeiro - RJ - Brasil 3 - New York University Grossman School of Medicine, Abdominal Core Health - New York - NY - Estados Unidos
4 - Hospital Nossa Senhora das Graças, Radiologia - Curitiba - PR - Brasil 5 - Universidade Federal do Rio de Janeiro e Instituto D’Or de Ensino e Pesquisa,
Radiologia - Rio de Janeiro - RJ - Brasil 6 - Penn State Hershey Medical Center, Minimally Invasive and Bariatric Surgery - Hershey - PA - Estados Unidos
7 - Universidade Federal do Rio Grande do Sul, Cirurgia - Porto Alegre - RS - Brasil
Rev Col Bras Cir 49:e20223172
Claus
2 DECOMP Report: Answers surgeons expect from anabdominal wall imaging exam
to the hernia surgeon. The value increases when imaging between bone structures and adjacent muscles. This
is used in conjunction with a thorough history and physical knowledge, combined with the emergence of new
examination. Nevertheless, the lack of uniform definition surgical techniques and a better understanding of the
of what a hernia is and the lack of standardization in the anatomy of the AW by surgeons, allows surgical planning
interpretation of image examinations create difficulties in in an individualized way. For this, the standardization of
both clinical care and academic research; there is simply the necessary information for an image exam is essential,
a paucity of high-level scientific evidence on hernia but unfortunately this is not yet routine. To overcome this
imaging1. For example, an incisional hernia may be defined issue, surgeons must interact more with the interpreting
as “a defect/hole, with or without bulging” in one study radiologist, or (alternatively) become experts in the proper
but as abdominal “wall weakness” in another5. Likewise, evaluation of these imaging studies4,10.
radiologists do not utilize standard reporting techniques To guide surgeons and radiologists, we created
when looking at the abdominal wall and commonly a study group, including representatives of the two
report clinically irrelevant hernia-related information specialties, aiming to create guidelines for surgeons and
while neglecting critically important information. Hernia mainly radiologists on the fundamental descriptions
surgeons and radiologists commonly have different for an adequate assessment of the AW from an image
interpretations of the same imaging study6,7. perspective. Information was grouped into four topics
Despite reporting inaccuracies, most studies covering: defect; hernia content; musculature and previous
comparing the accuracy of diagnostic methods point to event. In each section, we made a brief correlation of the
CT as the exam of choice1,5,8. It shows the best correlation aspects required for the exam with its relevance from a
between the imaging findings, physical examination, and practical/clinical point of view. The ultimate goal is the
the operative findings, in addition to allowing the images proper planning of the surgery. To make reading more
to be reassessed by the surgical team or other radiologists dynamic, we organize it in a Q&A format. At the end, we
later. Notably, CT scans are free of the operator factor propose a structured report model aimed at standardizing
present in ultrasound acquisition. There is generally no relevant information: the DECOMP report (DEfect;
need to use intravenous contrast. Although CT images COntent (hernia); Musculature; Previous events).
are static, they can be performed with maneuvers that
increase intra-abdominal pressure, which facilitates the Image information for evaluation of ventral hernia
identification of abdominal hernias1,8.
Ultrasonography, in addition to being less Like any imaging exam, a good interpretation
expensive and widely available, is a more dynamic exam begins with a descriptive indication from the surgeon,
and can be very useful with the interaction of the patient, for whom the radiologist can seek answers to the main
making it possible to perform maneuvers to increase questions about the evaluated case. Good communication
intra-abdominal pressure and point out the site of pain between the requesting professionals and the executors
or bulging1.9. Unfortunately, ultrassonography accuracy is essential and the kickoff is a good and clear indication
depends on the operator and the images generated are of the exam and expectations.
often of little value to the surgeon. Magnetic resonance
imaging is more expensive, less available and there are General CT Protocol
no studies showing its superiority in relation to CT in the
evaluation of abdominal wall defects1. In addition, the Technical parameters of the examination do not
images generated are generally more difficult for surgeons differ from those when performing “regular” abdominal
to assess, since they are not used to interpreting them5. CT. The only points that deserve more attention are:
The use of the imaging in the context of AW • the use of intravenous (IV) contrast is not
hernias goes far beyond just establishing confirmation essential for assessing the abdominal wall
of the diagnosis, but it allows the evaluation of complex defects and can be avoided.
(large) hernias, their content and the relationships • in suspicion of incarceration / strangulation
Rev Col Bras Cir 49:e20223172
Claus
DECOMP Report: Answers surgeons expect from anabdominal wall imaging exam 3
IV contrast may show signs of impairment (EHS) classification of primary and incisional AW hernias11.
of vascular supply to the hernia content In this way, the surgeon can:
like reduction or absence of parietal • decide the surgical technique to be
enhancement or even engorgement of the employed (conventional/open surgery vs
mesenteric vessels laparoscopic/robotic). Very large or large
• the same goes for the postoperative hernias (diameter over 10cm) are less prone
evaluation where IV contrast is not to minimally invasive techniques due to the
necessary, except in cases of collection with technical difficulty of adequately closing the
suspected infection where it can help to defect.
differentiate it. • indicate preoperative patient preparation
• Valsalva maneuver is only necessary if there measures such as the use of botulinum
is diagnostic doubt. In cases where the toxin chemodenervation and/or
diagnosis is already established, it usually induced progressive pre-operative
does not provide additional information. pnemoperitoneum, aiming to paralyze the
Although some surgeons may consider it lateral muscles and increase abdominal
different, the diagnosis of loss of domain compliance, and allow reduced tension at
must be done during the examination defect/midline closure.
without Valsalva. • planning for the need for component
separation technique(s).
DEFECT • define approximate mesh size and type. This
is critically important in practice locations
1. What is the defect location? where the mesh needs to be requested and
acquired preoperatively.
The precise location of the hernia defect is
essential for the planning and execution of the surgery.
Umbilical stalk, xiphoid and pubic symphysis should be
used as a reference for midline hernias; and costal margin,
iliac crest, semilunaris line and midline for lateral hernias.
In addition, hernias close to bony structures
are usually considered more complex for repair. This is
since the musculature close to bone structures has less
complacency, as well the greater difficulty creating space
for overlapping and mesh fixation. This information can
alter the operative technique, planned mesh position and
fixation method.
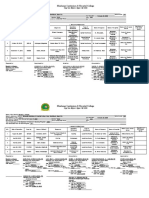
2. How big is the hernia defect? Figure 1. Schematic illustration of the measures of the hernia defect
in two axes: longitudinal and transverse, according to the EHS classifi-
cation.
A simple measurement of the size of the defect
is one of the most important aspects for surgical planning. 3. How many hernia defects are present?
A linear measurement of the largest hernia dimensions in
both longitudinal and transverses axis is required (Figure When there is more than one defect, information
1). This allows a classification of the hernia (small/medium/ on the locations and the distance between the first and
large) helping to predict the degree of difficulty of fascial last defect edges. The same goes for incisional hernias
closure. We suggest the use of the European Hernia Society with multiple defects (Figure 2). Additional and minor
Rev Col Bras Cir 49:e20223172
Claus
4 DECOMP Report: Answers surgeons expect from anabdominal wall imaging exam
defects undiagnosed by physical examination may go among others. Incarceration, defined when the hernia
unnoticed during surgery, especially if performed using content cannot be reduced manually, is generally of
open technique. clinical diagnosis and cannot be given by imaging
methods alone. Despite this, some of the aspects found
may be indicative, increasing the suspicion of hernia
incarceration:
• presence of hernia sac with narrow neck
in a small defect in the wall;
• presence of fluid inside the hernia sac;
• parietal thickening (greater than or
equal to 4mm) and/or distention of the
herniated intestinal segment and dilation
of the intestinal loops upstream inside
the abdominal cavity (apart from the
first criterion, the others are considered
an imminent risk of strangulation of the
incarcerated content).
Presence of these criteria, with incarcerated
Figure 2. Schematic illustration for measuring multiple defects, accor-
ding to EHS classification.
intestinal content, is a factor that should draw the
attention of both the radiologist and the surgeon to a
probable indication for urgent surgery.
HERNIA CONTENT Strangulated hernia is defined when the
vascular supply of the herniated content is compromised,
4. Does the hernia contain viscera? determining ischemia. As image criteria that determine
the suspicion of the diagnosis of strangulation of the
Presence of viscera such as intestinal loops hernia content we can observe (Figure 3):
or bladder inside the hernia sac brings some important • dilation of the segment of the intestinal
information about the case. First, it may indicate a greater loop located inside the hernia sac in the
risk of complications such as intestinal obstruction and shape of a “U” or “C”, due to obstruction
greater severity in the event of a strangulation. The of the afferent and efferent intestinal
knowledge of this fact can help in defining the need for segments (“closed loop” obstruction).
surgery or at least in planning the time when it should • thickening of the intestinal wall.
be performed. In addition, the presence of viscera • hypo or hyperattenuation of the wall in
inside the hernia sac is associated with greater difficulty relation to the usual pattern and parietal
in dissecting it and greater risk of an iatrogenic injury low uptake by means of intravenous
compared to hernias that contain only fat. contrast of the ischemic intestinal
segment.
5. Is the hernia content incarcerated or strangulated? • intestinal pneumatosis.
• fluid inside the hernia sac.
Incarceration of the hernia content is an • engorgement of the mesenteric vessels
indication of greater surgical difficulty. The risk of and obliteration of the mesenterial
complications, including possible iatrogenic injury to adipose plane of the herniated segment.
incarcerated content is greater. The surgeon may need Presence of one or more of these findings is
maneuvers for reduction such as external compression, suggestive of strangulation of the hernia content and
intra-operative enlargement of the hernia defect, urgent surgical intervention should be considered12,13.
Rev Col Bras Cir 49:e20223172
Claus
DECOMP Report: Answers surgeons expect from anabdominal wall imaging exam 5
preoperatively; visceral-reduction surgery; component
separation techniques. All these possibilities aim to
increase abdominal capacity and/or compliance18-21.
For tomographic assessment of the risk of
LOD in bulky hernias, we used the method described by
Tanaka et al because it is simple to understand and can
be performed by most mutislice tomographic equipment,
as well as being easily measured by the radiologist at
their standard workstation (Figures 4 and 5)14. The hernia
Figure 3. CT image showing a strangulated abdominal hernia: small sac and the abdominal cavity are considered ellipsoid
bowel loop segment with signs of ischemia characterized by parietal
thickening, mesentery densification, fluid in the hernia sac, and slight structures, allowing the calculation of volume estimation
reduction in contrast uptake. In addition to distention of the proximal using the multiplication between the measurements in a
intestinal loops.
straight line of the longitudinal axes (cranio-caudal - CC,
transversal - T and anteroposterior - AP) by the constant
6. What is the relationship between sac/hernia volume, according to the simplified formula:
content volume and abdominal cavity volume? Volume of the hernia sac or abdominal cavity:
CC x T x AP x 0.52
The relationship between the volume of the
hernia sac versus the volume of the abdominal cavity is
the best criterion for defining whether there is a loss of
domain (LOD). LOD is defined when the volume of the
sac/hernia content is greater than 25% of the volume of
the abdominal cavity14,15. This fundamental information
allows the surgeon to consider that:
• there may not be enough space to reduce
all herniated contents into the abdominal
cavity and still achieve a complete primary
fascial closure.
• the significant increase in intra-abdominal
pressure, due to the reduction of a large
volume of content in the abdominal cavity,
Figure 4. Representative illustration of the evaluation of the volume
can cause important ventilatory restriction of the abdominal cavity and the volume of the hernia sac in suspected
due to the upward compression of the cases of LOD.
diaphragm. Although rare, patients may
even develop abdominal compartment
syndrome16. In addition, the risk of hernia
recurrence and even evisceration are
significantly increased17.
With this assessment prior to the procedure,
surgeons can use several strategies to reduce the
consequences of the condition described above.
Although it is not the objective of this work, we can cite
as alternatives: preoperative preparation (weight loss
and respiratory physiotherapy); progressive preoperative Figure 5. CT image illustrating how measurements are performed to
assess the volume of the abdominal cavity and hernia sac in suspected
pneumoperitoneum and application of botulinum toxin cases of LOD.
Rev Col Bras Cir 49:e20223172
Claus
6 DECOMP Report: Answers surgeons expect from anabdominal wall imaging exam
Some pre-established criteria are important for below the umbilicus, at the level of the umbilicus or even
greater precision in calculating the volume: in complete)23-25.
A- The largest measurement of each axis RD is usually asymptomatic, and often not even
should be used, even in different tomographic sections noticed by patients. It does not cause complications and
to calculate the volume of the hernia sac, as well as the its treatment, from an aesthetic point of view, is usually
volume of the abdominal cavity. addressed by plastic surgeons. However, RD represents
B- To determine the abdominal volume a weakness of the midline abdominal wall22. Patients
cavity (AVC), some reference points must be used: The with midline hernias (umbilical, epigastric or incisional)
measurement of the anteroposterior axis of the abdominal with associated RD may be at increased risk of hernia
cavity is determined by the line that joins the muscle recurrence or bulging in the postoperative period (Figure
groups of the healthy (anterior) wall and the line that 6). Currently, important changes in the choice of surgical
passes through the transverse processes of the vertebra procedure have occurred in patients with midline hernias
(posterior). The CC distance is made between the first associated with RD. In general, more comprehensive
cut showing the diaphragm and the last cut showing the surgeries or at least with mesh have been recommended
tailbone. The transverse distance (T) through the parietal to reduce the effects of weakness caused by RD on the
peritoneum on each side of the abdominal cavity. risk of recurrence. Information regarding the presence
C- To determine the hernia sac volume (HSV), or absence of RD (and the size of the longest distance
the following references should be used: Measurement of / separation of the rectus abdominis muscles) should be
the limits of the parietal peritoneum of the hernia sac for part of every image evaluation report of the abdominal
the CC and T axes. For the AP axis, the distance between wall.
the anterior parietal sac peritoneum hernia to a line that
joins the muscle groups of the healthy wall (posterior
limit).
RV = HSV/ AVC
if >25% = loss of domain
MUSCULATURE
7. Does the patient have Rectus Abdominal Diastasis
(RD)?
RD is defined as the increase in the distance
between the medial edges of the two abdominals of the
rectus abdominis muscle in the anterior midline, caused by
laxity and thinning of the aponeurosis of the alba line22. The
rectus abdominis muscles may have normal thickness or Figure 6. CT image showing a small hernia defect but with important
diastasis/weakness of the AW.
more often atrophy (myoaponeurotic laxity). This distance
can be measured clinically by digital pulp or quantitatively
by imaging methods such as US, CT or MRI. Although
there is no consensus on the normality of the distance 8. What is the width of the rectus muscles?
between the medial edges of the rectus abdominis belly,
most of the literature considers the presence of diastasis Although we understand that this information
when greater than 20mm. In addition, it can be classified is a little more specific, the transverse measurement of
according to the position (just above the umbilicus, only the rectus abdominis width on each side (at the height
Rev Col Bras Cir 49:e20223172
Claus
DECOMP Report: Answers surgeons expect from anabdominal wall imaging exam 7
of the largest transverse measurement of the defect) in progress over time. Setting expectations in the pre-
relation to defect size is used as a predictor for the need operative period is key27.
for muscle component separation, as described in the Breast reconstructions with transposition of the
Carbonel Equation26. Rectus defect ratio is calculated by rectus abdominis muscle flaps (TRAM) after mastectomy
simple addition of the right and left rectus widths divided are still common, and may lead to important weakness
by the hernia width (Figures 7 and 8). Authors reported of the abdominal wall and bulging. All these findings
that approximately 80% of patients with RDR <1 require certainly interfere not only in the planning of the
components separation whereas when RDR was >2 only surgical tactic but also in the postoperative functional
10% required CS. Measuring the diameter of the rectus and cosmetic results.
muscle is only necessary for midline hernia.
RDR = RR + LR / DS 10. Is there an intraparietal hernia?
RR - right rectus
LR - left rectus Some hernias, especially on the lateral wall of
DS - defect size the abdomen, can occur without a defect of all muscle
groups layers. In these cases, usually the external oblique
muscle/aponeurosis is intact, and the hernia is contained
within the muscular layers of the AW (Figure 9). Without
this information, the surgeon may miss the hernia defect
during an open approach, when they encounter the
Figure 7. Schematic representation of the measurements of the hernia
defect (DS) and right (RR) and left (RL) rectus muscle case according to intact external oblique myofascial layer.
the Carbonel equation.
Figure 8. CT image showing the relationship between the measure-
ment of the defect (DS) and the rectus muscles (RR and RL) to assess any
need for separation of chemical or surgical components.
9. Is there muscle rupture or atrophy?
Patients who have already undergone any
surgical intervention may have muscle weakness,
atrophy (denervation) or muscle tissue loss. This usually
Figure 9. Illustration demonstrating intraparietal hernia. External obli-
occurs after surgeries with lateral incisions or flanks que muscle is intact.
(lumbotomy type) that can cause damage to the neuro-
vascular bundles that supply the central abdomen. PREVIOUS EVENTS
Denervation atrophy of the musculature medial to the
nerve transection may occur. In addition, denervation 11. Are there any signs of previous surgical
may result in bulging without a formal hernia defect manipulation or complication?
(pseudo-hernia). It is important to differentiate between
a hernia and a “pseudo-hernia” as denervation related Presence of a mesh or even tacks for fixation
bulging and asymmetry can persist after repair and can may indicate previous surgical manipulation and therefore
Rev Col Bras Cir 49:e20223172
Claus
8 DECOMP Report: Answers surgeons expect from anabdominal wall imaging exam
a greater degree of technical complexity in an upcoming CONTENT
repair. This may be even more relevant in cases where the
mesh was placed in the intraperitoneal position. It is true 4- Incarceration and/or strangulation signs:
that in some cases, neither the meshes nor the fixation - Not
devices (currently absorbable devices, radiotransparent, - Yes: what signs:
are becoming more popular) are detectable, but indirect
signs such as loss of contour of anatomical planes can 5- Content of the hernia sac:
indicate them. Adipose tissue / omentum / intestinal loop
The importance of the detailed description (which segment) / bladder / ureter / vascular structures
of the surgeon regarding possible repairs or previous (which) / solid organ/ other
interventions in the indication of the exam is crucial
to allow the interpretation of subtle findings by the 6- Relationship between the volume of the
radiologist. A comprehensive review of the patient’s hernia sac in relation to the volume of the abdominal
prior operative reports can indicate the type of mesh, cavity (>25%):
its location and anatomic plane of implantation, which - Not
can make identification possible. Additionally, looking for - Yes: risk of loss of domain
non-anatomical folds and wrinkles from mesh contracture
can facilitate mesh identification on CT imaging. MUSCULATURE
Evaluation of collections or fistulous tracts
(sinuses) by imaging is also important to decide on 7- Rectus Muscles diastasis:
surgical steps such as dividing the treatment into steps Not
to resolve the entire chronic infection or foreign body Yes: width (mm) / extensions (cm) / position
reaction before a new attempt at definitive repair with a
new prosthesis. 8- Transverse width of the rectus muscles (just
The concept of a standardized report for for midline defects):
abdominal wall imaging exams is proposed here: - width:right: mm
- left: mm
DECOMP report
9- Presence of atrophy and/or denervation of
DEFECT the AW muscles
1- Location of the hernia defect(s): - Not
A) Midline: cm from the xiphoid and/or pubic -Yes: location / muscle group(s) / thickness
symphysis and/or the umbilical scar (mm)
B) Lateral: which anatomical position? cm
from iliac crest and/or costal margin and/or linea alba / 10- The hernia is intraparietal?
linea semilunaris - Not
- Yes: location
2-Defect size (measured on the transverse and
longitudinal axes, respectively: cm). PREVIOUS EVENTS
3- Presence of more than one hernia defect: 11- Signs of previous manipulation, mesh
- Not. implant or complication in the cavity and/or abdominal
- Yes (distance between the defect ends: wall:
-cm) - repetition of the entire description of the second - Not
hernia defect according to the structured report above. - Yes: which / where
Rev Col Bras Cir 49:e20223172
Claus
DECOMP Report: Answers surgeons expect from anabdominal wall imaging exam 9
CONCLUSIONS correlations (flow and contrast enhancement) as they
directly interfere in the diagnosis and management, the
The better understanding between surgeons precise descriptions of abdominal hernias have the same
and radiologists in the evaluation of hernia of the AW will impact mainly on surgical planning.
likely improve hernia repair outcomes. At this moment, for the fastest and widest
We understand that this proposal brings more dissemination of this concept, it is essential that surgeons
challenges to radiologists during the evaluation of the involve and encourage radiologists to adopt the routine
image exam. The report may even take a little longer. performance of a structured report with the necessary
However, in the same way that not only the description of information about AW. And we believe that the
a nodule of an abdominal organ is important, but also the structured report proposal, presented in this article, can
precise size and location, anatomical and characteristic help radiologists in their work.
R E S U M O
Hérnias da parede abdominal são um problema bastante comum enfrentado pelo cirurgiões gerais. De diagnóstico essencialmente clínico,
as hérnias abdominais durante muito tempo têm sido consideradas um problema de simples reparo. Entretanto, o acompanhamento
de longo prazo dos pacientes têm demonstrado resultados desapontadores, tanto em termos de complicações quanto risco de
recidiva da hérnia. Neste contexto, o planejamento pré-operatório com controle de comorbidades e pleno conhecimento da hérnia e
suas relações anatômicas com a parede abdominal têm ganho cada vez mais atenção. A tomografia de abdome parece ser a melhor
opção para determinar o tamanho e localização precisos das hérnias abdominais, presença de diastase de músculo reto e/ou atrofia
da parede associada, assim como proporção da hérnia em relação a parede abdominal. Essas informações podem auxiliar o cirurgião
na escolha da melhor técnica cirúrgica (aberta vs. MIS), posicionamento e fixação das telas, e eventual necessidade de aplicação de
toxina botulínica, pneumoperitônio pré-operatório ou técnicas de separação de componentes. Apesar da relevância dos achados,
eles são raramente descritos em exames de tomografia uma vez que os radiologistas não estão acostumados a olhar para a parede
abdominal assim como não sabem quais as informações são realmente necessárias. Por estes motivos, nós reunimos um grupo de
cirurgiões e radiologistas visando estabelecer quais são as informações da parede abdominal mais importantes em um exame de
tomografia assim como propor um laudo estruturado para facilitar a descrição dos achados e sua interpretação.
Palavras-chave: Hérnia. Hérnia Abdominal. Tomografia. Radiologia.
REFERENCES ventral hernia repair complications. Insights Imaging.
2019;10(1):40. doi: 10.1186/s13244-019-0730-x.
1. Kroese LF, Sneiders D, Kleinrensink GJ, Muysoms 5. Xu Z, Asman AJ, Baucom RB, Abramson RG,
F, Lange JF. Comparing diferent modalities for the Poulose BK, Landman BA. Quantitative CT
diagnosis of incisional hernia: a systematic review. Imaging of Ventral Hernias: Preliminary Validation
Hernia. 2018;22(2):229-42 .doi: 10.1007/s10029- of an Anatomical Labeling Protocol. PLoS ONE.
017-1725-5. 2015;10(10):e0141671. doi:10.1371/journal.
2. Mallory MA, Ashley SW. Computed Tomographic pone.0141671.
Imaging in the Diagnosis of Recurrent Ventral 6. Busby LP, Courtier JL, Glastonbury CM. Bias in
Hernia. JAMA Surg. 2016;151(1):13-4. doi: 10.1001/ Radiology: The How and Why of Misses and
jamasurg.2015.2587. Misinterpretations. Radiographics. 2018;38(1):236-
3. Parikh KR, Al-Hawary M, Millet JD, Burney R, Finks 47. doi: 10.1148/rg.2018170107.
J, Maturen K. Incisional Hernia Repair: What the 7. Schwartz LH, Panicek DM, Berk AR, Li Y, Hricak H.
Radiologist Needs to Know. AJR Am J Roentgenol. Improving communication of diagnostic radiology
2017;209(6):1239-46. doi: 10.2214/AJR.17.18137. findings through structured reporting. Radiology.
4. Patil AR, Nandikoor S, Mohanty HS, Godhi S, Bhat 2011;260(1):174-81. doi: 10.1148/radiol.11101913.
R. Mind the gap: imaging spectrum of abdominal 8. Naguib N, Rafique H, Rao PFD, Longworth T,
Rev Col Bras Cir 49:e20223172
Claus
10 DECOMP Report: Answers surgeons expect from anabdominal wall imaging exam
Soukias JM, Masoud A. A review of the incidence jss.2016.11.051.
of iatrogenic hernia in both laparoscopic and open 17. Trujillo CN, Fowler A, Al-temimi M; Ali A, Johna S,
colorectal surgery: Using CT as the gold standard of Tessier D. Complex Ventral Hernias: A Review of Past
detection, cohort study. Int J Surg. 2015;19:87-90. to Present. Perm J. 2018;22:17-015. doi: 10.7812/
doi: 10.1016/j.ijsu.2015.05.026. TPP/17-015.
9. Bjork LB, Bellew SD, Kummer T. Point-of-Care 18. Blair LJ, Ross SW, Huntington CR, Watkins JD,
Ultrasound Diagnosis of Traumatic Abdominal Wall Prasad T, Lincourt AE, et al. Computed tomographic
Hernia. Pediatr Emerg Care. 2017;33(5):367-9. doi: measurements predict component separation in
10.1097/PEC.0000000000001126. ventral hernia repair. J Surg Res. 2015;199(2):420-7.
10. Holihan JL, Karanjawala B, Ko A, Askenasy EP, doi: 10.1016/j.jss.2015.06.033.
Matta EJ, Gharbaoui L, et al. Use of Computed 19. Cuminal L, Rousset P, Passot G, Caillot JL, Valette
Tomography in Diagnosing Ventral Hernia PJ, Muller A. Image-guided preoperative progressive
Recurrence: A Blinded, Prospective, Multispecialty pneumoperitoneum for large incisional hernia
Evaluation. JAMA Surg. 2016;151(1):7-13. doi: repair. Diagn Interv Imaging. 2017;98(6):507-9. doi:
10.1001/jamasurg.2015.2580. 10.1016/j.diii.2017.02.006.
11. Muysoms FE, Miserez M, Berrevoet F, Campanelli 20. Elstner KE, Read JW, Rodriguez-Acevedo O, Cosman
G, Champault GG, Chelala E, et al. Classification PH, Dardam AN, Jacombns ASW, et al. Preoperative
of primary and incisional abdominal wall hernias. chemical component relaxation using Botulinum
Hernia 2009;13(4):407-14. doi: 10.1007/s10029- toxin A: enabling laparoscopic repair of complex
009-0518-x. ventral hernia. Surg Endosc. 2017:31(2):761-8 doi:
12. Aguirre DA, Santosa AC, Casola G, Silrin CB. 10.1007/s00464-016-5030-7.
Abdominal Wall Hernias: Imaging Features, 21. Farooque F, Jacombs ASW, Roussos E, Read JW,
Complications, and Diagnostic Pitfalls at Multi– Dardano AN, Edye M, et al. Preoperative abdominal
Detector Row CT. Radiographics. 2005;25(6):1501- muscle elongation with botulinum toxin A for
20. doi: 10.1148/rg.256055018. complex incisional ventral hernia repair. ANZ J Surg.
13. Mueck KM, Holihan JL, Mo J, Flores-Gonzales JR, Ko 2016;86(1-2):79-83. doi: 10.1111/ans.13258.
TC, Kao LS, et al. Computed tomography findings 22. Reinpold W, Köckerling F, Bittner R, Conze J, Fortelny
associated with the risk for emergency ventral R, Koch A, et al. Classification of Rectus Diastasis - A
hernia repair. The Am J Surg. 2017;214(1):42-6. doi: Proposal by the German Hernia Society (DHG) and
10.1016/j.amjsurg.2016.09.035. the International Endohernia Society (IEHS). Front.
14. Tanaka EY, Yoo JH, Rodrigues Jr AJ, Utiyama EM, Surg. 2019;6:1. doi: 10.3389/fsurg.2019.00001.
Birolini D, Rasslan S. A computerized tomography 23. Coldron Y, Stokes M, Newham D, Cook K.
scan method for calculating the hernia sac and Postpartum characteristics of rectus abdominis on
abdominal cavity volume in complex large incisional ultrasound imaging. Man Ther. 2008;13(2):112-21.
hernia with loss of domain. Hernia. 2010;14(1): 63- doi: 10.1016/j.math.2006.10.001.
9. doi: 10.1007/s10029-009-0560-8. 24. van de Water ATM, Benjamin DR. Measurement
15. Passot G, Villeneuve L, Sabbagh C, Renard Y, methods to assess diastasis of the rectus abdominis
Regimbeau J-M, Verhaeghe P, et al. Definition muscle (DRAM): A systematic review of their
of Giant Ventral Hernias: Development of measurement properties and meta-analytic reliability
Standardization through a Practice Survey. Int J Surg. generalization. Man Ther. 2016;21:41-53. doi:
2016;28:136-40. doi: 10.1016/j.ijsu.2016.01.097. 10.1016/j.math.2015.09.013.
16. Mommers EHH, Wegdam JA, Wolk S, Nienhuijs 25. Corvino A, De Rosa D, Sbordone C, Nunziata
SW, Reilingh TSdeV. Impact of hernia volume on A, Corvino F, Varelli C, et al. Diastasis of rectus
pulmonary complications following complex hernia abdominis muscles: patterns of anatomical variation
repair. J Surg Res. 2017;211:8-13. doi: 10.1016/j. as demonstrated by ultrasound. Pol J Radiol.
Rev Col Bras Cir 49:e20223172
Claus
DECOMP Report: Answers surgeons expect from anabdominal wall imaging exam 11
2019;84:e542-e548. doi:10.5114/pjr.2019.91303. 10.1007/s10029-020-02181-y.
26. Love MW, Warren JA, Davis S, Ewing JA, Hall AM, 27. Flum DR, Horvath K, Koepsell T. Have Outcomes of
Cobb WS, et al. Computed tomography imaging in Incisional Hernia Repair Improved With Time? Ann
ventral hernia repair: can we predict the need for Surg. 2003 ;237(1) :129-35. doi:10.1097/00000658-
myofascial release? Hernia. 2020;25(2):471-7. doi: 200301000-00018.
Received in: 25/08/2021 Mailing address:
Accepted for publication: 03/11/2021 Christiano Marlo Paggi Claus
Conflict of interest: no. E-mail: christiano.claus@gmail.com
Funding source: none.
Rev Col Bras Cir 49:e20223172
You might also like
- Sataloff's Comprehensive Textbook of Otolaryngology Head and Neck Surgery - Vol2 (2016) .Unitedvrg Rhinology Allergy ImmunologyDocument979 pagesSataloff's Comprehensive Textbook of Otolaryngology Head and Neck Surgery - Vol2 (2016) .Unitedvrg Rhinology Allergy ImmunologyChandramohan Setty50% (2)
- Textbook of Surgery For Dental StudentssDocument399 pagesTextbook of Surgery For Dental StudentssDiana Mihaela Ilie50% (2)
- Duties of Scrub Nurse & Circulating NurseDocument2 pagesDuties of Scrub Nurse & Circulating Nurseimafashionista90% (21)
- 404 Veterinary Referral Hospital - BrochureDocument11 pages404 Veterinary Referral Hospital - BrochureJoanne FagnouNo ratings yet
- Basic Dental Implant SurgeryDocument33 pagesBasic Dental Implant Surgerymuhammad100% (1)
- Delays in Imaging Diagnosis of Acute Abdominal PainDocument7 pagesDelays in Imaging Diagnosis of Acute Abdominal PainWillie VanegasNo ratings yet
- Multimodality Approach For Imaging of Non-Traumatic Acute Abdominal EmergenciesDocument13 pagesMultimodality Approach For Imaging of Non-Traumatic Acute Abdominal EmergenciesfalisNo ratings yet
- Indicacoes Exames Complementares de Imagem No AbdomeDocument12 pagesIndicacoes Exames Complementares de Imagem No AbdomeHannaNo ratings yet
- Abdominal Ultrasound For Pediatric Blunt Trauma FAST Is Not Always BetterDocument3 pagesAbdominal Ultrasound For Pediatric Blunt Trauma FAST Is Not Always BetterInryuu ZenNo ratings yet
- 2017 - Practical Approach To Imaging of The Pediatric Acute AbdomenDocument18 pages2017 - Practical Approach To Imaging of The Pediatric Acute AbdomenRevivo RindaNo ratings yet
- 268 2010 Article 694Document8 pages268 2010 Article 694I Gusti Rai SutrawanNo ratings yet
- Original ArticleDocument5 pagesOriginal ArticlehengkyNo ratings yet
- Indications For Abdominal Imaging: When and What To Choose?Document12 pagesIndications For Abdominal Imaging: When and What To Choose?musdalifahNo ratings yet
- Surgeon-Performed Ultrasound As A Diagnostic Tool in AppendicitisDocument6 pagesSurgeon-Performed Ultrasound As A Diagnostic Tool in Appendicitisansar ahmedNo ratings yet
- Cervical Angiograms in Cervical Spine Trauma Patients 5 Years After The Data: Has Practice Changed?Document4 pagesCervical Angiograms in Cervical Spine Trauma Patients 5 Years After The Data: Has Practice Changed?edi_wsNo ratings yet
- Online Radiography Continuing EducationDocument39 pagesOnline Radiography Continuing EducationAndy WijayaNo ratings yet
- PEDIATRIC Blunt Abdominal Injury MGMT Guidelines AlgorithmDocument6 pagesPEDIATRIC Blunt Abdominal Injury MGMT Guidelines AlgorithmHaidir MuhammadNo ratings yet
- Iaim 2015 0206 17Document13 pagesIaim 2015 0206 17fahrunisaNo ratings yet
- Preoperative Computed Tomography Angiography in Autologous Breast Reconstruction-Incidence and Impact of IncidentalomasDocument6 pagesPreoperative Computed Tomography Angiography in Autologous Breast Reconstruction-Incidence and Impact of IncidentalomasNora Vianey Alcantara VelascoNo ratings yet
- Ditkofsky 2015Document28 pagesDitkofsky 2015Allython Jureth Peña ReyesNo ratings yet
- Abdomino-Pelvic CT Project Work UPDATED - 105912 - 020107 - 011052Document36 pagesAbdomino-Pelvic CT Project Work UPDATED - 105912 - 020107 - 011052sommylydiiNo ratings yet
- Entero SequencesDocument12 pagesEntero SequencesKelvin SueyzyNo ratings yet
- Cervical Spine Clearance 2009Document7 pagesCervical Spine Clearance 2009Abdulelah Al.luhaybiNo ratings yet
- PIIS0196064418311594Document8 pagesPIIS0196064418311594NanaNo ratings yet
- Focused Sonography in Detecting Hemoperitoneum in Blunt Abdominal Trauma Patients, Correlation With Computed TomographyDocument6 pagesFocused Sonography in Detecting Hemoperitoneum in Blunt Abdominal Trauma Patients, Correlation With Computed TomographyDhaniNo ratings yet
- EcografiaMedicinaInterna InternaDocument7 pagesEcografiaMedicinaInterna InternaGinés López MartínezNo ratings yet
- Proposal New - 060952Document33 pagesProposal New - 060952sommylydiiNo ratings yet
- To Determine Validity of Ultrasound in Predicting Acute Appendicitis AmongDocument6 pagesTo Determine Validity of Ultrasound in Predicting Acute Appendicitis AmongIkki DongNo ratings yet
- The Role of Imaging in Cervical Cancer Staging - ESGOESTROESP Guidelines (Update 2023)Document32 pagesThe Role of Imaging in Cervical Cancer Staging - ESGOESTROESP Guidelines (Update 2023)Limbert Rodríguez TiconaNo ratings yet
- Musculosketal Imaging in Physical TherapyDocument14 pagesMusculosketal Imaging in Physical TherapyWasemBhatNo ratings yet
- Structured Versus Narrative Reporting of Pelvic MRI in Perianal Fistulizing Disease: Impact On Clarity, Completeness, and Surgical PlanningDocument10 pagesStructured Versus Narrative Reporting of Pelvic MRI in Perianal Fistulizing Disease: Impact On Clarity, Completeness, and Surgical PlanningqrscentralNo ratings yet
- WP Esaote Vnav Ob-GynDocument4 pagesWP Esaote Vnav Ob-Gynapi-237460689No ratings yet
- 2 - From FAST To E FAST An Overview of The Evolution of Ultrasound Based Traumatic Injury AssessmentDocument8 pages2 - From FAST To E FAST An Overview of The Evolution of Ultrasound Based Traumatic Injury AssessmentMarcelo RibeiroNo ratings yet
- Performance and Practice Guidelines For Excisional Breast BiopsyDocument4 pagesPerformance and Practice Guidelines For Excisional Breast BiopsyPPDS Bedah FK UNRI Angkatan 2No ratings yet
- Role of Computed Tomography (CT) Scan in Staging of Cervical CarcinomaDocument6 pagesRole of Computed Tomography (CT) Scan in Staging of Cervical CarcinomaTriponiaNo ratings yet
- The Role of Abdominal X-Rays in The Investigation of Suspected Acute AppendicitisDocument5 pagesThe Role of Abdominal X-Rays in The Investigation of Suspected Acute AppendicitisFitri RachmadaniNo ratings yet
- Expert Consensus Contouring Guidelines For Intensity Modulated Radiation Therapy in Esophageal and Gastroesophageal Junction CancerDocument10 pagesExpert Consensus Contouring Guidelines For Intensity Modulated Radiation Therapy in Esophageal and Gastroesophageal Junction CancermarrajoanaNo ratings yet
- болезнь КронаDocument7 pagesболезнь КронаAlexander NatroshviliNo ratings yet
- Blunt Abdiminal TraumaDocument6 pagesBlunt Abdiminal TraumaErdyNo ratings yet
- Jo Clinical Oncology AssignmentDocument10 pagesJo Clinical Oncology Assignmentapi-711592723No ratings yet
- PalateDocument41 pagesPalatearif sudiantoNo ratings yet
- Historical Overview: Abstract: Several Studies Have Demonstrated That A Diagnosis Based SolelyDocument8 pagesHistorical Overview: Abstract: Several Studies Have Demonstrated That A Diagnosis Based SolelyLuh Tu PebriyantiNo ratings yet
- BJR 85 1029Document9 pagesBJR 85 1029Anna MariaNo ratings yet
- Bandi 2008 Chest Wall InvasionDocument6 pagesBandi 2008 Chest Wall Invasionmarvic gabitanNo ratings yet
- DTSCH Arztebl Int-115 0031Document12 pagesDTSCH Arztebl Int-115 0031Monika Diaz KristyanindaNo ratings yet
- JTD 11 03 936Document8 pagesJTD 11 03 936Heru SigitNo ratings yet
- Abdominal USG in EDDocument9 pagesAbdominal USG in EDanon_773331597No ratings yet
- DMFR 20170301Document7 pagesDMFR 20170301Ana PaulaNo ratings yet
- Ultrasound in Gynecology and ObstetricsDocument197 pagesUltrasound in Gynecology and ObstetricsAli Murtaza AbbasNo ratings yet
- 0100 3984 RB 51 06 0VII PDFDocument2 pages0100 3984 RB 51 06 0VII PDFMarcelitaTaliaDuwiriNo ratings yet
- Clinical Anatomy - 2020 - Le Saint Grant - Arterial Anatomy of The Anterior Abdominal Wall Ultrasound Evaluation As ADocument6 pagesClinical Anatomy - 2020 - Le Saint Grant - Arterial Anatomy of The Anterior Abdominal Wall Ultrasound Evaluation As AarifNo ratings yet
- He 2016Document5 pagesHe 2016Anonymous 44bTHDeHkbNo ratings yet
- Fafaj2021 Tanaka Score ReliabilityDocument6 pagesFafaj2021 Tanaka Score ReliabilityEham AroraNo ratings yet
- 2009 PelvimetryDocument5 pages2009 PelvimetryayupurnamasariiNo ratings yet
- 1618 4726 1 PB PDFDocument6 pages1618 4726 1 PB PDFDrive IyasNo ratings yet
- Comprehensive Ultrasound Diagnosis For Intraductal Spread of Primary Breast CancerDocument10 pagesComprehensive Ultrasound Diagnosis For Intraductal Spread of Primary Breast CancerferdiNo ratings yet
- Management Guidelines For Penetrating Abdominal Trauma: Walter L. Biffl and Ernest E. MooreDocument9 pagesManagement Guidelines For Penetrating Abdominal Trauma: Walter L. Biffl and Ernest E. MooreArsy Mira PertiwiNo ratings yet
- Clinical Oncology AssignmentDocument9 pagesClinical Oncology Assignmentapi-691277740No ratings yet
- POZE Professor - Dr. - Dieter - Beyer, - Professor - Dr. - Ulrich - (B-Ok - CC) PDFDocument463 pagesPOZE Professor - Dr. - Dieter - Beyer, - Professor - Dr. - Ulrich - (B-Ok - CC) PDFUffie-Isabela GheNo ratings yet
- The Incidence and Risk of Early Postoperative Small Bowel Obstruction After Laparoscopic Resection For Colorectal Cancer 2014Document7 pagesThe Incidence and Risk of Early Postoperative Small Bowel Obstruction After Laparoscopic Resection For Colorectal Cancer 2014alemago90No ratings yet
- Thoracoscopy:: A Real-Life PerspectiveDocument6 pagesThoracoscopy:: A Real-Life Perspective1411731No ratings yet
- A New Classification For Surgical NEC During Exploratory Laparotomy: Introduction and Reproducibility AssessmentDocument9 pagesA New Classification For Surgical NEC During Exploratory Laparotomy: Introduction and Reproducibility AssessmentCirugia Pediatrica La RazaNo ratings yet
- 10 1053@j Semnuclmed 2020 07 005Document10 pages10 1053@j Semnuclmed 2020 07 005anon_813722240No ratings yet
- Management of Postoperative HypoxemiaDocument14 pagesManagement of Postoperative HypoxemiaFavio Alvarez De BejarNo ratings yet
- Population Preference For Treatment of Uncomplicated AppendicitisDocument6 pagesPopulation Preference For Treatment of Uncomplicated AppendicitisFavio Alvarez De BejarNo ratings yet
- Human Water and Electrolyte BalanceDocument10 pagesHuman Water and Electrolyte BalanceFavio Alvarez De BejarNo ratings yet
- Towards Evidence-Based and Personalised Care of Acute PancreatitisDocument7 pagesTowards Evidence-Based and Personalised Care of Acute PancreatitisFavio Alvarez De BejarNo ratings yet
- ProstatectomyDocument9 pagesProstatectomymardsz100% (1)
- Ca. Ca.: - .,.1b1h1tlesDocument179 pagesCa. Ca.: - .,.1b1h1tleshNo ratings yet
- Laser Innovation: Ease of Use Battery Powered Green Aiming BeamDocument2 pagesLaser Innovation: Ease of Use Battery Powered Green Aiming BeamNatalia PalarieNo ratings yet
- Rüsch Urology: For Almost Every ApplicationDocument72 pagesRüsch Urology: For Almost Every ApplicationSaad MouatassimNo ratings yet
- Metzenbaum Scissors Are Surgical: Scissors Tissue Tungsten CarbideDocument5 pagesMetzenbaum Scissors Are Surgical: Scissors Tissue Tungsten CarbideRhea Leliza PrudenteNo ratings yet
- Robotic HysterectomyDocument14 pagesRobotic HysterectomyPrincess Brigitte R. PATE�ANo ratings yet
- 2024 USFSSTG001V4 US DeLorean STG Rev1aDocument70 pages2024 USFSSTG001V4 US DeLorean STG Rev1aNathaly GuevaraNo ratings yet
- Vascular InjuryDocument26 pagesVascular InjuryEka NataNo ratings yet
- Musculoskeletal Physical TherapyDocument5 pagesMusculoskeletal Physical TherapyAbiha AnisNo ratings yet
- Supraglottic Airway Devices A Review in A New Era of Airway Management 2155 6148 1000647Document9 pagesSupraglottic Airway Devices A Review in A New Era of Airway Management 2155 6148 1000647Riris SihotangNo ratings yet
- Cardiac Surgery TextbookDocument2 pagesCardiac Surgery Textbookoguzguneri2010No ratings yet
- DM General Surgery CurriculumDocument45 pagesDM General Surgery CurriculumGiovanni HenryNo ratings yet
- ACHQC Abdominal Core Surgery Rehabilitation Protocol Patient Guide 6.17.20Document43 pagesACHQC Abdominal Core Surgery Rehabilitation Protocol Patient Guide 6.17.20Brka223No ratings yet
- Use Only: Anesthetics Considerations in PeritonitisDocument9 pagesUse Only: Anesthetics Considerations in Peritonitisade_liaNo ratings yet
- Surgery For Recurrent Soft Tissue SarcomaDocument584 pagesSurgery For Recurrent Soft Tissue SarcomaAr-pardo RogerNo ratings yet
- Comments From The Injured Worker SurveyDocument117 pagesComments From The Injured Worker Surveyvaluecare1542No ratings yet
- Knowledge, Attitude and Perception of Patients.9Document6 pagesKnowledge, Attitude and Perception of Patients.9KarlaPadrelananNo ratings yet
- 03 Bartholin Gland Procedure + Inform ConsentDocument4 pages03 Bartholin Gland Procedure + Inform ConsentelenNo ratings yet
- Hospital Case CardiacDocument3 pagesHospital Case CardiacAnup MohapatraNo ratings yet
- Argumentative Writing - PresentationDocument2 pagesArgumentative Writing - PresentationMaria Cecilia Annette RahardjaNo ratings yet
- Preoperative AssessmentDocument3 pagesPreoperative AssessmentStepyn SalvadorNo ratings yet
- Not For Reproduction: Doctor'S Order/Nurse'S Compliance Sheet (Authenticate All Orders)Document2 pagesNot For Reproduction: Doctor'S Order/Nurse'S Compliance Sheet (Authenticate All Orders)Mcgee OcnicnatNo ratings yet
- Pre-Board Exam For July 2011 NLEDocument37 pagesPre-Board Exam For July 2011 NLEdammenoel100% (2)
- Mindanao Sanitarium & Hospital College: Brgy San Miguel, Iligan City 9200Document5 pagesMindanao Sanitarium & Hospital College: Brgy San Miguel, Iligan City 9200Kabang MoaNo ratings yet
- Blue 783 Clinical Management of Jehovahs Witnesses and Other Patients Who Refuse Blood ComponentsDocument21 pagesBlue 783 Clinical Management of Jehovahs Witnesses and Other Patients Who Refuse Blood ComponentsMarkez CharlezNo ratings yet