Professional Documents
Culture Documents
Severe Illness Anxeit Treated by Integrating Inpatient Psychotherapy With Medical Care and Minimizing Reassurance
Severe Illness Anxeit Treated by Integrating Inpatient Psychotherapy With Medical Care and Minimizing Reassurance
Uploaded by
Jan LAWOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Severe Illness Anxeit Treated by Integrating Inpatient Psychotherapy With Medical Care and Minimizing Reassurance
Severe Illness Anxeit Treated by Integrating Inpatient Psychotherapy With Medical Care and Minimizing Reassurance
Uploaded by
Jan LAWCopyright:
Available Formats
CASE REPORT
published: 22 March 2019
doi: 10.3389/fpsyt.2019.00150
Severe Illness Anxiety Treated by
Integrating Inpatient Psychotherapy
With Medical Care and Minimizing
Reassurance
Albert T. Higgins-Chen 1*, Sarah B. Abdallah 2 , Jennifer B. Dwyer 1,3 , Alfred P. Kaye 1,4 ,
Gustavo A. Angarita 1 and Michael H. Bloch 1,3
1
Department of Psychiatry, Yale School of Medicine, Yale University, New Haven, CT, United States, 2 Yale School of
Medicine, Yale University, New Haven, CT, United States, 3 Child Study Center, Yale School of Medicine, Yale University, New
Haven, CT, United States, 4 Veterans Administration National Center for PTSD, West Haven, CT, United States
Illness anxiety disorder (IAD, formerly hypochondriasis) is characterized by preoccupation
with fear of serious illness despite medical reassurance. IAD is common, debilitating,
challenging to treat, and results in high healthcare utilization. Outpatient management of
IAD is challenging because patients can compulsively seek reassurance from numerous
Edited by:
providers, which interferes with learning more productive coping skills. We present
Rafael Christophe Freire, the case of a woman with severe IAD who presented to the emergency room with
Universidade Federal do Rio de
increasing frequency over several months, despite regular outpatient medical visits and
Janeiro, Brazil
escalating psychiatric care. We made the unusual decision to hospitalize her for IAD for 1
Reviewed by:
Aislinn Joanmarie Williams, month, in the absence of typical hospitalization criteria. This hospitalization allowed us to
The University of Iowa, United States consolidate all medical and psychiatric care into a single provider team and train all staff
Veruska Andrea Dos Santos,
Federal University of Rio de Janeiro,
and family to communicate with her in a consistent manner. We successfully treated
Brazil her by integrating a general cognitive-behavioral therapy (CBT) protocol into medical
*Correspondence: care and decision-making. In response to her numerous health concerns, we minimized
Albert T. Higgins-Chen
medical work-up, reassurance, and reactive medication changes, and instead used the
a.higginschen@yale.edu
concerns as opportunities to reinforce the psychotherapy. This approach allowed us to
Specialty section: simplify her medication regimen and manage her co-morbid hypertension and vitamin
This article was submitted to
deficiencies. Though inpatient hospitalization is likely infeasible in most cases of IAD,
Mood and Anxiety Disorders,
a section of the journal outpatient providers may create similar treatment plans based on the example of our
Frontiers in Psychiatry case report, without needing highly specialized expertise. Such a plan would require a
Received: 22 November 2018 straightforward understanding of IAD psychology, which we review here, combined with
Accepted: 28 February 2019
Published: 22 March 2019
readily accessible tools including a universal CBT protocol, online CBT courses, and
Citation:
clinical symptom scales. We discuss our approach for responding to health concerns,
Higgins-Chen AT, Abdallah SB, maintaining therapeutic alliance, integrating CBT principles into patient interactions, and
Dwyer JB, Kaye AP, Angarita GA and managing medications. Since patients with IAD share health concerns with all providers,
Bloch MH (2019) Severe Illness
Anxiety Treated by Integrating staff, and family, we also include our own IAD communication guide, appropriate for a
Inpatient Psychotherapy With Medical general audience, that demonstrates how to respond in these conversations.
Care and Minimizing Reassurance.
Front. Psychiatry 10:150. Keywords: illness anxiety disorder, health anxiety, hypochondriasis, panic disorder, psychotherapy, CBT
doi: 10.3389/fpsyt.2019.00150 (cognitive-behavioral therapy), case report
Frontiers in Psychiatry | www.frontiersin.org 1 March 2019 | Volume 10 | Article 150
Higgins-Chen et al. Inpatient Psychotherapy for Illness Anxiety
INTRODUCTION health, worried that she or her loved ones would die, and
researched symptoms and medications on the Internet for over
Illness anxiety disorder (IAD) is characterized by excessive 4 hours each day. She began presenting to the emergency
concern about acquiring or having serious medical illnesses that room (ER) for normal physical sensations and anxiety-related
interferes with normal functioning, persisting despite normal symptoms, and each time she was reassured by a normal
medical workup and reassurance. Patients with IAD may seek medical workup. Over the next 3 months, the frequency of
excessive medical care or request frequent changes to medical ER visits steadily increased despite escalating psychiatric care,
care (care-seeking type), or may avoid medical care, fearing the medication changes, and regular outpatient medical visits. She
possibility of true disease, or adverse effects of treatment (care- started aripiprazole but self-discontinued it, believing it caused a
avoidant type). IAD and somatic symptom disorder are DSM- dizzy spell and a globus sensation, even though these symptoms
5 diagnoses that correspond best to hypochondriasis in DSM- began before the aripiprazole trial. The globus sensation caused
IV. Illness anxiety is common, with studies reporting lifetime a fear of choking for 2 weeks, so she ate very little and lost 20
prevalence of 2–13% in the general population, and 5–30% pounds. One poor-quality EKG in the ER showed prolonged
in patients with comorbid medical conditions (1, 2). Previous QTc of 490, prompting her to call her primary medical doctor
experiences with illness, especially those associated with strongly (PMD) daily for a week despite subsequent normal EKGs. She
negative emotions can contribute to anxiety disorders including entered an intensive outpatient program (IOP), which attempted
IAD (3, 4). Severe IAD often results in high healthcare utilization to trial various medications over 2 months while tapering
and is unlikely to resolve sporadically (5). Thus, all physicians lamotrigine and escitalopram. She also had her first inpatient
should be prepared to work with IAD patients and refer them for psychiatric hospitalization for 3 days for passive suicidal ideation.
proper treatment. Clomipramine was discussed for possible obsessive-compulsive
Well-intentioned physicians may try repeatedly reassuring disorder (OCD). However, each time a new medication was
patients or changing medical management to allay patients’ started she read about side effects, believed she had them, and
anxieties, but unfortunately this is counter-productive in the presented to the ER.
absence of concurrent psychotherapy. According to cognitive- Four months into her IAD course, her PMD measured a blood
behavioral models that form the basis for effective evidence- pressure of 210/120 after she had stopped her lisinopril and
based treatment for IAD (6), the relief associated with hydrochlorothiazide for 2 months from fear of side effects. She
reassurance makes the patient more likely to seek reassurance in had no symptoms and resumed her antihypertensives. However,
response to future health concerns. Similarly, changing medical she began checking her blood pressure 5 or more times per
management based solely on patient anxiety only results in day, constantly worried about having a stroke, and presented
worse anxiety to the new plan. Both actions distract from to the ER ten times in 1 week. Given she had utilized so many
psychotherapeutic interventions targeting underlying cognitive emergency resources, she was considered for standard psychiatric
biases that generated anxiety in the first place. Many generalized hospitalization but did not meet criteria. Our inpatient unit was
cognitive-behavioral therapy (CBT) protocols may be effectively able to offer intensive psychotherapy, so she was transferred to us.
applied to IAD (2). However, the primary challenge for IAD On admission, she reported her mood as anxious and
treatment is integrating CBT with medical care. Our case depressed, with no suicidal ideation. Scales administered for
highlights this challenge and can serve as a guide for any self-reported symptoms indicated severe IAD (Table 1). They
outpatient provider to integrate readily available resources to also indicated moderate depression and severe panic, but her
treat IAD. presentation was more consistent with IAD. We also considered
generalized anxiety disorder (GAD), but her ruminations focused
CASE REPORT primarily on health and not on other topics. The only lifetime
symptom on a Y-BOCS symptom inventory for OCD was
We present a woman in her 40’s who was never married, lived “concern with illness or disease” so we did not complete a Y-
with mother, boyfriend, and three children, and was unemployed BOCS scale, as any findings would be more consistent with IAD.
and on Social Security disability. She had a 20-year history of Laboratory studies were notable for iron-deficiency anemia (Hgb
generalized anxiety and major depression that was in remission 8.6, ferritin 3, at her baseline), low vitamin D, and borderline-
for the past 5 years with outpatient therapy, escitalopram 40 mg, low vitamin B12. For these long-standing deficiencies we tested
and lamotrigine 100 mg daily. Medical conditions included transglutaminase IgG/IgA levels but they did not indicate celiac
hypertension, long-standing iron deficiency anemia, a 30 pack- disease. MMSE was 30/30.
year history of tobacco use, but no alcohol or substance use. We diagnosed the patient with IAD with minimal somatic
She had faced numerous health problems in various family symptoms. Given comorbid depression, we opted for CBT using
members over the past 2 years, most notably her brother’s the Unified Protocol for Transdiagnostic Treatment of Emotional
sudden unexpected death shortly after doctors told him he Disorders (UP) (7). We completed 12 CBT sessions, three
was in remission from a serious illness. Other family diagnoses times per week for up to 90 min each, at a rate of about one
included cancer, stroke, retinal detachment, bipolar disorder, and UP workbook chapter per session. We provide UP worksheets
multiple suicides. to record her thoughts, feelings, sensations, and behaviors in
The patient developed severe illness anxiety shortly after her different contexts. UP chapters addressed: (1) motivations for
son’s ICU hospitalization for influenza. She ruminated about change, (2) reducing cognitive distortions by recognizing and
Frontiers in Psychiatry | www.frontiersin.org 2 March 2019 | Volume 10 | Article 150
Higgins-Chen et al. Inpatient Psychotherapy for Illness Anxiety
TABLE 1 | Patient’s scores on clinical symptom scales over time.
Location Admission Discharge Outpatient IOP IOP IOP Outpatient
Time (weeks) 0 4 6 7 10 15 24
SHAI (healthy anxiety) 41 45 35 27 - - 10
PHQ-9 (depression) 19 8 7 7 5 7 4
PDSS-SR9 (panic) 19 - - - 7 4 2
SHAI, Short Health Anxiety Inventory; maximum 54; score > 27 supports diagnosis of IAD over other anxiety disorders. PHQ-9, Patient Health Questionnaire for depression; maximum
27; score > 20 supports diagnosis of severe depression, 15–19 moderately severe, 10–14 moderate, 5–9 mild, 0–4 minimal. PDSS, Panic Disorder Severity Scale; maximum 28; score
> 14 supports diagnosis of severe panic, 10–13 moderate, 6–9 mild, 2–5 minimal. IOP, intensive outpatient program. We also performed a Y-BOCS symptom inventory which did not
find evidence for current or past obsessive-compulsive disorder.
correcting automatic negative appraisals of situations as well herself of the IAD cycle while receiving the injection. She feared
as weighing evidence, (3) increasing distress tolerance through the lamotrigine taper would cause a seizure, so she asked us
mindfulness and non-judgmental awareness of emotions, (4) numerous times to delay the taper and sought reassurance for
reducing emotional avoidance, and (5) exposure therapy to weeks after it was stopped. For psychotherapy purposes, we did
anxiety-provoking stimuli. delay a dose reduction by 3 days and asked her to notice the
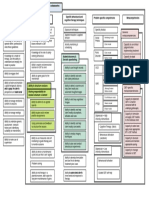
We also introduced a simple cognitive model of illness result. She had predicted this would reduce her anxiety, but
anxiety (Figure 1): her fears of being sick or experiencing it actually caused far greater anxiety over those 3 days as she
serious medication side effects made her anxious, so she either awaited the eventual dose change. In later therapy sessions, she
avoided the problem (e.g., by refusing medications) or sought developed the insight that this was an example of unhelpful
reassurance, and the reward of her short-term relief only made emotional avoidance. Ultimately, she finished her lamotrigine
her original thoughts stronger. She realized that to break this taper and received escitalopram 20 mg and vitamins B12 and
cycle, she needed to replace reassurance-seeking with other D. However, she did not consistently take iron or the increased
coping skills and expose herself to the anxiety-provoking stimuli antihypertensive dose during the admission.
she was avoiding, and this realization allowed her to better engage We also had her apply the IAD cycle when she approached
in therapy. us multiple times per day about various minor symptoms and
Importantly, this psychotherapy used a readily accessible normal physical sensations (tight muscles, pinching sensations,
protocol and did not involve specialized CBT for IAD, as sweaty palms, etc.). While we addressed any possibly emergent
multiple generalized forms of CBT are effective for IAD (2). The medical concerns, we deliberately avoided immediate clinical
key advance of this case was to incorporate psychotherapeutic assessments and reassurance for most benign symptoms. Instead,
principles into medical care and decision-making. To that end, we calmly asked her to apply psychotherapy principles to each
we encouraged the patient to apply the IAD cycle and the concern, so she eventually realized that any reassurance-seeking
CBT concepts during any conversation about medical care. For would only bring temporary relief and worsen her anxiety
example, we had opted to simplify her medication regimen as in the long term. Psychoeducation was provided on anxiety
much as possible, as we felt over-fixation on medications in the symptoms and on how to manage symptoms in a non-medical
outpatient setting had worsened her illness anxiety and distracted manner (e.g., tennis ball self-massage for tense muscles). Several
from psychotherapy. We established a plan early on to increase times she expressed frustration that her medical concerns were
her mid-taper escitalopram dose from 15 to 20 mg, finish her not addressed, stating, “Psychiatric patients can have medical
lamotrigine taper, increase her antihypertensives and start iron problems too!” We maintained the therapeutic alliance through
and vitamin supplements. As expected, she expressed numerous self-disclosure: we told her that as physicians, we did feel
concerns about the changes, often changed her mind about uncomfortable not immediately addressing her medical concerns
what she wanted and why, frequently researched side effects on but employed this communication strategy because it was in her
the computer, and often refused changes. We recognized these best interest and we wanted to help her recover.
behaviors were manifestations of avoidance common in anxiety The patient regularly raised her health concerns with all
disorders, and thus changing the plan based on her concerns staff on the unit and her family throughout her hospitalization.
would worsen her anxiety in the long term. We responded by Thus, we implemented multiple psychoeducation sessions for
having long, patient conversations with her about why the plan staff and family so they could understand why IAD was driving
would help her and made very few changes to it. We frequently the patient to seek reassurance, avoid getting frustrated with
redirected her attention to the IAD cycle, and eventually she the patient, and respond appropriately. Furthermore, we created
realized the primary problem was her anxiety rather than valid a written communication guide that includes specific scenarios
concerns about side effects. and responses along with CBT principles they could discuss
The medications also became a form of exposure therapy. For with the patient. We provide a modified copy here in the
example, when she had fears that a vitamin B12 injection would Supplementary Information.
cause anaphylaxis, we incorporated it into a therapy session by For continuing care after discharge, we sent the
asking her to describe her emotional experience and remind communication guide and UP to outpatient psychiatric
Frontiers in Psychiatry | www.frontiersin.org 3 March 2019 | Volume 10 | Article 150
Higgins-Chen et al. Inpatient Psychotherapy for Illness Anxiety
FIGURE 1 | A cognitive-behavioral model of illness anxiety. A feedback loop of thoughts of being sick and safety behaviors (avoidance or reassurance-seeking) causes
worsening of illness anxiety over time. Cognitive, exposure, and behavioral therapies as well as strong therapeutic alliance can break the cycle and improve symptoms.
and medical providers to continue the management strategy Short Health Anxiety Inventory (SHAI; 0–3 scale for each item).
that worked well in the inpatient setting. We also prescribed an Various cutoff scores for IAD have been utilized, ranging from
online course specifically designed for health anxiety through the 15 to 38, with 27 providing balance between sensitivity and
website ThisWayUp (https://thiswayup.org.au/). We suggested specificity when differentiating between IAD and other anxiety
further ThisWayUp courses on panic, depression, and stress disorders (10).
management which she completed over 3 months after discharge. Cognitive behavioral therapy (CBT) is the mainstay of
A visiting nurse would administer her medications to provide treatment for IAD. No CBT subtype has yet proven superior
continuing exposure therapy and ensure her hypertension was to our knowledge. Several studies support CBT (8, 11, 12) or
adequately addressed. Though she had significant anxiety about specific subtypes, including cognitive (13), exposure response
leaving the hospital, she discharged home without difficulty (13), group (14), or mindfulness CBT (15). In the outpatient
after 1 month. setting, therapy may take 3 or more months to demonstrate
Though she still met criteria for severe IAD at discharge improvements over standard care, but the benefits usually persist
(Table 1), this was expected given that 3 months of even at 5-year follow-up (2, 8). Online CBT for health anxiety and
psychotherapy are needed to observe clear benefits of CBT comorbid depression is an effective supplement or alternative
(2, 8). Nevertheless, she had learned skills that allowed her to to in-person psychotherapy (16, 17). Online courses such
better function with her anxiety in the community without as ThisWayUp (https://thiswayup.org.au/) have the additional
regularly presenting to the ER. We followed up with the benefit of incorporating clinical symptom scales reported to the
patient 4 months after discharge, after she had finished her prescribing physician.
treatment at IOP level of care and the ThisWayUp online Medications can supplement IAD treatment. Randomized
course. Though she still had some anxiety, she no longer met controlled trials support efficacy of SSRIs in treating IAD though
criteria for IAD (Table 1), spent almost no time on Internet they are less effective than psychotherapy (18, 19). Case reports
research, and was able to address a family member’s surgery suggest TCAs such as clomipramine may also be helpful (6).
without significant anxiety. She received continued care for However, IAD patients often prefer and tolerate psychological
severe hypertension, vitamin deficiency, and anemia, including treatment better than pharmacological treatment (20). Providers
with intravenous iron. She made a total of 4 ER visits over 4 should be aware that excessive focus on medications to treat IAD
months, substantially lower than the 10 visits in 1 week prior may actually worsen the anxiety.
to admission. While most medical providers may not provide dedicated
psychotherapy, they can help reinforce CBT skills in the setting
DISCUSSION of medical decision-making if they are familiar with the concepts.
The model we taught to our patient, family, and staff illustrates
Our case demonstrates the utility of integrating psychotherapy the core mechanism of IAD and how CBT targets different
with medical care in treating IAD, and many aspects of our features of IAD (Figure 1). IAD worsens over time because
management can be replicated by outpatient medical providers. of the self-reinforcing cycle of anxiety and safety behaviors.
Measurement-based care through clinical symptom scales can An obsessional thought or fear of illness causes anxiety, which
help provide the proper diagnosis. For example, the cardinal prompts the patient to either seek reassurance or avoid the
symptoms and underlying psychology behind OCD, panic issue. The temporary relief of the safety behavior is rewarding
disorder, and IAD overlap significantly, but clinical scales can and strengthens the original obsessional thought and automatic
adequately distinguish between them (9). We used the 18-item behavior while also preventing the patient from realizing the
Frontiers in Psychiatry | www.frontiersin.org 4 March 2019 | Volume 10 | Article 150
Higgins-Chen et al. Inpatient Psychotherapy for Illness Anxiety
fear was unfounded in the first place. Specific cognitive biases is problematic as patients may not be empowered to apply
make patients particularly vulnerable to this cycle (9). Increased psychotherapeutic principles in the same setting where they
intolerance of uncertainty drives patients to seek out expert are making healthcare decisions, and innovations in healthcare
opinion even if there is a negligible chance of disease. Increased delivery are needed to address this issue.
body vigilance and catastrophic misinterpretation causes them In conclusion, evidence-based CBT is highly effective for the
to constantly scan their bodies and find evidence for serious treatment of IAD, but a major challenge is integrating it into
illness. Core beliefs about health may be erroneous, e.g., medical care. Though most physicians do not directly provide
“health means having no physical or mental symptoms at psychotherapy, they can care for patients by understanding
all.” (6) Psychotherapy systematically modifies these thoughts the underlying psychology of IAD, helping patients apply
and behaviors. CBT principles during medical decision-making, avoiding
The key advance of this case report is illustrating how excessive reassurance or medication changes, and educating
to help patients apply CBT concepts in the context of real- all staff and family about how to respond to patients’
world medical decision-making. Instead of offering immediate health concerns.
reassurance or reactive medication changes, we used a set of
communication strategies to encourage the patient to employ DATA AVAILABILITY
CBT in response to all health concerns. Of note, patients with
IAD raise health concerns with various medical providers, staff, All datasets generated for this study are included in the
and families. Based on our experience, all these individuals can manuscript and/or the Supplementary Files.
be recruited to help the patient apply CBT assuming they receive
proper psychoeducation. Thus, we present a communication
guide (Supplementary Information), appropriate for a general ETHICS STATEMENT
audience, that provides psychoeducation and communication
This study was performed in accordance with the provisions
strategies for everyone involved in the patient’s care.
of the Declaration of Helsinki and the Yale University Human
Integration of psychotherapy and medical care might be
Subjects Committee. We obtained written informed consent
replicated in the outpatient setting by regular check-ins
from the patient authorizing publication of the clinical case. She
with psychiatric and medical providers who are in frequent
read the case report before publication and her anonymity has
communication with each other. In integrated primary care
been preserved.
settings, providers with psychotherapy training could consult
on cases and join medical visits with the primary physician. A
plan should be developed between outpatient providers and the AUTHOR CONTRIBUTIONS
patient to avoid excessive ER visits. Nurses may be more effective
than psychologists at engaging patients in IAD treatment (21), AH-C and SA served as primary physicians for the patient during
as they can discuss both the psychological and medical issues. the hospitalization, collected and analyzed the data, and wrote the
A visiting nurse can administer medications as a form of manuscript. JD, AK, GA, and MB provided supervision for care
exposure therapy and reduce IAD’s interference with important of the patient and reviewed the manuscript.
medical care.
Hospitalizing patients for IAD alone is likely not an option FUNDING
for most cases in the current healthcare system. However, in
severe cases of IAD, it can be extremely difficult in the outpatient This work and AH-C was supported by the IMPORT
setting to prevent excessive medical care-seeking, and each time grant 2R25MH071584-11, awarded to the Yale Department of
the patient receives reassurance this may reinforce maladaptive Psychiatry by NIMH. JD was supported by the grant T32
behavior. We observed that hospitalization limits the patient to MH018268-33. AK was supported by grants T32 MH19961
a single combined team providing psychiatric and medical care, and T32 MH14276. Support was provided by the Clinical
thus preventing reassurance-seeking from various ER providers Neuroscience Research Unit at the Connecticut Mental Health
and providing an opportunity for extinction of the maladaptive Center and the State of Connecticut Department of Mental
behavior. This is reminiscent of eating disorder treatment, where Health and Addiction Services. This publication does not express
inpatient and partial hospitalization programs can impose limits the views of the Department of Mental Health and Addiction
on eating behaviors long enough for CBT to take effect. We Services or the State of Connecticut. The views and opinions
suggest similar programs for IAD can be explored. In the future, expressed are those of the authors.
such programs might not necessarily require a full month; a
recent paper on a novel 4-day intensive protocol for OCD showed SUPPLEMENTARY MATERIAL
sustained remission for 4 years in 56 of 77 patients (22). New
treatment options for IAD are needed in modern healthcare The Supplementary Material for this article can be found
systems, where psychotherapy and medical care are usually online at: https://www.frontiersin.org/articles/10.3389/fpsyt.
delivered by separate providers with very different training. This 2019.00150/full#supplementary-material
Frontiers in Psychiatry | www.frontiersin.org 5 March 2019 | Volume 10 | Article 150
Higgins-Chen et al. Inpatient Psychotherapy for Illness Anxiety
REFERENCES anxiety). J Anxiety Disord. (2015) 30:1–7. doi: 10.1016/j.janxdis.2014.
12.012
1. Weck F, Richtberg S, Neng J. Epidemiology of hypochondriasis and health 15. McManus F, Surawy C, Muse K, Vazquez-Montes M, Mark Williams JG.
anxiety: comparison of different diagnostic criteria. Curr Psychiatry Rev. A randomized clinical trial of mindfulness-based cognitive therapy versus
(2014) 10:14–23. doi: 10.2174/1573400509666131119004444 unrestricted services for health anxiety (hypochondriasis). J Consult Clin
2. Tyrer P. Recent advances in the understanding and treatment of health Psychol. (2012) 80:817–28. doi: 10.1037/a0028782
anxiety. Curr Psychiatry Rep. (2018) 20:49. doi: 10.1007/s11920-018-0912-0 16. Hedman E, Hesser H, Andersson E, Axelsson E, Ljótsson B. The mediating
3. Weck F, Neng JMB, Göller K, Müller-Marbach AM. Previous experiences with effect of mindful non-reactivity in exposure-based cognitive behavior
illness and traumatic experiences: a specific risk factor for hypochondriasis? therapy for severe health anxiety. J Anxiety Disord. (2017) 50:15–22.
Psychosomatics. (2014) 55:362–71. doi: 10.1016/j.psym.2013.10.005 doi: 10.1016/j.janxdis.2017.04.007
4. Bennett P, Patterson K, Noble S. Predicting post-traumatic stress and health 17. Andrews G, Basu A, Cuijpers P, Craske MG, McEvoy P, English CL, et al.
anxiety following a venous thrombotic embolism. J Health Psychol. (2016) Computer therapy for the anxiety and depression disorders is effective,
21:863–71. doi: 10.1177/1359105314540965 acceptable and practical health care: an updated meta-analysis. J Anxiety
5. Fink P, Ørnbøl E, Christensen KS. The outcome of health anxiety in primary Disord. (2018) 55:70–8. doi: 10.1016/j.janxdis.2018.01.001
care. A two-year follow-up study on health care costs and self-rated health. 18. Greeven A, Van Balkom AJLM, Visser S, Merkelbach JW, Van Rood YR, Van
PLoS ONE. (2010) 5:e9873. doi: 10.1371/journal.pone.0009873 Dyck R, et al. Cognitive behavior therapy and paroxetine in the treatment
6. Abramowitz JS, Braddock AE. Hypochondriasis: conceptualization, of hypochondriasis: a randomized controlled trial. Am J Psychiatr. (2007)
treatment, and relationship to obsessive-compulsive disorder. Psychiatr 164:91–9. doi: 10.1176/ajp.2007.164.1.91
Clin North Am. (2006) 29:503–19. doi: 10.1016/j.psc.2006.02.008 19. Fallon BA, Petkova E, Skritskaya N, Sanchez-Lacay A, Schneier
7. Barlow DH, Farchione TJ, Fairholme CP, Ellard KK, Boisseau CL, Allen LB, F, Vermes D, et al. A double-masked, placebo-controlled study of
et al. Unified Protocol for Transdiagnostic Treatment of Emotional Disorders: fluoxetine for hypochondriasis. J Clin Psychopharmacol. (2008) 28:638–45.
Therapist Guide. New York, NY: Oxford University Press (2011). doi: 10.1097/JCP.0b013e31818d21cf
8. Tyrer P, Salkovskis P, Tyrer H, Wang D, Crawford MJ, Dupont S, et al. 20. Walker J, Vincent N, Furer P, Cox B, Kjernisted K. Treatment preference
Cognitive-behaviour therapy for health anxiety in medical patients (Champ): in hypochondriasis. J Behav Ther Exp Psychiatr. (1999) 30:251–8.
a randomised controlled trial with outcomes to 5 years. Health Technol Assess. doi: 10.1016/S0005-7916(99)00027-0
(2017) 21:1–88. doi: 10.3310/hta21500 21. Tyrer H, Tyrer P, Lisseman-Stones Y, McAllister S, Cooper S, Salkovskis P,
9. Deacon B, Abramowitz JS. Is hypochondriasis related to obsessive-compulsive et al. Therapist differences in a randomised trial of the outcome of cognitive
disorder, panic disorder, or both? an empirical evaluation. J Cogn Psychother. behaviour therapy for health anxiety in medical patients. Int J Nurs Stud.
(2008) 22:115–27. doi: 10.1891/0889-8391.22.2.115 (2015) 52:686–94. doi: 10.1016/j.ijnurstu.2014.11.013
10. Alberts NM, Hadjistavropoulos HD, Jones SL, Sharpe D. The short health 22. Hansen B, Kvale G, Hagen K, Havnen A, Öst LG. The Bergen 4-
anxiety inventory: a systematic review and meta-analysis. J Anxiety Disord. day treatment for OCD: four years follow-up of concentrated ERP in
(2013) 27:68–78. doi: 10.1016/j.janxdis.2012.10.009 a clinical mental health setting. Cogn Behav Ther. (2018) 48:89–105.
11. Barsky AJ, Ahern DK. Cognitive behavior therapy for hypochondriasis: doi: 10.1080/16506073.2018.1478447
a randomized controlled trial. JAMA. (2004) 291:1464–70.
doi: 10.1001/jama.291.12.1464 Conflict of Interest Statement: The authors declare that the research was
12. Olatunji BO, Kauffman BY, Meltzer S, Davis ML, Smits JAJ, Powers MB. conducted in the absence of any commercial or financial relationships that could
Cognitive-behavioral therapy for hypochondriasis/health anxiety: a meta- be construed as a potential conflict of interest.
analysis of treatment outcome and moderators. Behav Res Ther. (2014) 58:65–
74. doi: 10.1016/j.brat.2014.05.002 Copyright © 2019 Higgins-Chen, Abdallah, Dwyer, Kaye, Angarita and Bloch. This
13. Weck F, Neng JMB, Richtberg S, Jakob M, Stangier U. Cognitive is an open-access article distributed under the terms of the Creative Commons
therapy versus exposure therapy for hypochondriasis (health anxiety): a Attribution License (CC BY). The use, distribution or reproduction in other forums
randomized controlled trial. J Consult Clin Psychol. (2015) 83:665–76. is permitted, provided the original author(s) and the copyright owner(s) are credited
doi: 10.1037/ccp0000013 and that the original publication in this journal is cited, in accordance with accepted
14. Weck F, Gropalis M, Hiller W, Bleichhardt G. Effectiveness of cognitive- academic practice. No use, distribution or reproduction is permitted which does not
behavioral group therapy for patients with hypochondriasis (health comply with these terms.
Frontiers in Psychiatry | www.frontiersin.org 6 March 2019 | Volume 10 | Article 150
You might also like
- Test Bank For Foundations of Addictions Counseling 4th Edition David Capuzzi Mark D StaufferDocument8 pagesTest Bank For Foundations of Addictions Counseling 4th Edition David Capuzzi Mark D Stauffermarisgemma0j3vNo ratings yet
- The Role of SocioculturalDocument24 pagesThe Role of SocioculturalloloasbNo ratings yet
- Mental Health Nursing Case StudyDocument11 pagesMental Health Nursing Case Studyapi-499028250No ratings yet
- Psychiatric Mental Health Comprehensive Case StudyDocument8 pagesPsychiatric Mental Health Comprehensive Case Studyapi-544869292No ratings yet
- Final Capstone PaperDocument15 pagesFinal Capstone Paperapi-478784238No ratings yet
- Current: Don't Be Fooled by HypochondriaDocument6 pagesCurrent: Don't Be Fooled by HypochondriaNikita UmalkarNo ratings yet
- MH Nursing Clinical Case StudyDocument10 pagesMH Nursing Clinical Case Studyapi-546041293No ratings yet
- Pediatr - Rev CEFALEA AlternDocument9 pagesPediatr - Rev CEFALEA AlternIvan LiconNo ratings yet
- Running Head: Comprehensive Case Study 1Document11 pagesRunning Head: Comprehensive Case Study 1api-546355462No ratings yet
- Depressao Ansiedade Pcte TerminalDocument4 pagesDepressao Ansiedade Pcte Terminalgabrielapetitot_9179No ratings yet
- Illness Anxeity Disorder A Case Report and Brief Review of The LiteratureDocument4 pagesIllness Anxeity Disorder A Case Report and Brief Review of The LiteratureJan LAWNo ratings yet
- Tugas Skill - UnlockedDocument9 pagesTugas Skill - Unlockednamasaya1No ratings yet
- Ix43m ZvabwDocument27 pagesIx43m ZvabwUsman Ahmad TijjaniNo ratings yet
- I3h9y Mel19Document27 pagesI3h9y Mel19Usman Ahmad TijjaniNo ratings yet
- 10 Page Mental HealthDocument13 pages10 Page Mental Healthapi-736365670No ratings yet
- Psychological Interventions For The Management of Bipolar DisorderDocument9 pagesPsychological Interventions For The Management of Bipolar DisorderFausiah Ulva MNo ratings yet
- DEPRESSDocument23 pagesDEPRESSWong Chew Nie100% (1)
- Aisha Isyaku Term PaperDocument27 pagesAisha Isyaku Term PaperUsman Ahmad TijjaniNo ratings yet
- Annals of Psychiatry and Clinical NeuroscienceDocument2 pagesAnnals of Psychiatry and Clinical NeuroscienceFiorenzo TassottiNo ratings yet
- Abram Hoffer, Linus Pauling, James Greenblatt - Functional Psychiatry For Treatment of Anxiety-Psychiatry Redefined (2024)Document16 pagesAbram Hoffer, Linus Pauling, James Greenblatt - Functional Psychiatry For Treatment of Anxiety-Psychiatry Redefined (2024)Alina BreazuNo ratings yet
- MH Case Study 1Document13 pagesMH Case Study 1api-601489653No ratings yet
- 10 Page Case StudyDocument11 pages10 Page Case Studyapi-663754509No ratings yet
- Case Study PaperDocument8 pagesCase Study Paperapi-622485867No ratings yet
- Kasus 4 FMDocument14 pagesKasus 4 FMGroup 6 Virgi Ahmad TyphaldyNo ratings yet
- Nejmcp 002896Document5 pagesNejmcp 002896Rendra DananjayaNo ratings yet
- Psychiatric Mental Health Comprehensive Case StudyDocument14 pagesPsychiatric Mental Health Comprehensive Case Studyapi-662323379100% (1)
- Anxiety Among PhysiciansDocument1 pageAnxiety Among PhysiciansAinun QalbiNo ratings yet
- Prone Vs Supine Positioning For Breast Cancer RadiotherapyDocument3 pagesProne Vs Supine Positioning For Breast Cancer RadiotherapyJave GajellomaNo ratings yet
- Schizoaffective Bipolar Case StudyDocument10 pagesSchizoaffective Bipolar Case Studyapi-546593615No ratings yet
- Bipolar EditedDocument6 pagesBipolar EditedmartinNo ratings yet
- Case Study PaperDocument12 pagesCase Study Paperapi-545001894No ratings yet
- Psychiatric Mental Health Comprehensive Case StudyDocument12 pagesPsychiatric Mental Health Comprehensive Case Studyapi-662890978No ratings yet
- Factitious Disorder - Patient Pretending To Long Stay at The HospitalDocument3 pagesFactitious Disorder - Patient Pretending To Long Stay at The HospitalJAVED ATHER SIDDIQUINo ratings yet
- Brainsci 09 00031Document3 pagesBrainsci 09 00031IgnacioJoséCalderónPérezNo ratings yet
- Tyrer 2018 - HipocondriaDocument8 pagesTyrer 2018 - HipocondriaBeltraoNayaraNo ratings yet
- Comprehensive Case StudyDocument12 pagesComprehensive Case Studyapi-739556104No ratings yet
- The Emotional Impact of Covid-19 On Humanity "I M Carrying The Covid-19 Virus and Will Infect and Kill My Only Child".Document4 pagesThe Emotional Impact of Covid-19 On Humanity "I M Carrying The Covid-19 Virus and Will Infect and Kill My Only Child".International Journal of Innovative Science and Research TechnologyNo ratings yet
- A Single-Session Crisis Intervention Therapy Model For Emergency PsychiatryDocument6 pagesA Single-Session Crisis Intervention Therapy Model For Emergency Psychiatryamm90No ratings yet
- NDT 81677 Adherence and Re Hospitalizations in Patients With Schizophr 040115Document6 pagesNDT 81677 Adherence and Re Hospitalizations in Patients With Schizophr 040115Elsa OctaviaNo ratings yet
- 1 s2.0 S2213422019300150 MainDocument6 pages1 s2.0 S2213422019300150 MainMonaNo ratings yet
- Bipolar Disorder Implications For Nursing PracticeDocument5 pagesBipolar Disorder Implications For Nursing PracticeFátima Lopes100% (2)
- Evaluation of Depression and Suicidal Patients in The Emergency RoomDocument15 pagesEvaluation of Depression and Suicidal Patients in The Emergency RoomjuanpbagurNo ratings yet
- Bipolar Disorder: Case StudyDocument13 pagesBipolar Disorder: Case Studyapi-607314474No ratings yet
- Case Study On Pulmonary Tuberculosis: January 2017Document3 pagesCase Study On Pulmonary Tuberculosis: January 2017Nova DenisaNo ratings yet
- Official Handout For Somatoform DisordersDocument17 pagesOfficial Handout For Somatoform DisorderskeziahNo ratings yet
- 156122-Article Text-407418-1-10-20170517Document5 pages156122-Article Text-407418-1-10-20170517Monique MaraisNo ratings yet
- Case StudyDocument14 pagesCase Studyapi-607939779No ratings yet
- Bipolaridad 1Document12 pagesBipolaridad 1JambisNo ratings yet
- Bipolar Disorder Research Paper Thesis StatementDocument4 pagesBipolar Disorder Research Paper Thesis Statementaypewibkf100% (1)
- Psicological MedicineDocument2 pagesPsicological MedicineMonica EspinalNo ratings yet
- MH Clinical Case StudyDocument9 pagesMH Clinical Case Studyapi-546463844No ratings yet
- Manejo Depresion 1Document10 pagesManejo Depresion 1Luis HaroNo ratings yet
- Park, 2019 - NEJM - DepressionDocument10 pagesPark, 2019 - NEJM - DepressionFabian WelchNo ratings yet
- Chavez TinocomDocument13 pagesChavez Tinocomapi-641827342No ratings yet
- Depression Among Patients Attending Physiotherapy Clinics in Erbil CityDocument6 pagesDepression Among Patients Attending Physiotherapy Clinics in Erbil Citysarhang talebaniNo ratings yet
- Depression: Annals of Internal MedicinetDocument16 pagesDepression: Annals of Internal MedicinetjesusNo ratings yet
- A Practical Guide To The Use of Psychotropic Medications During Pregnancy and LactationDocument13 pagesA Practical Guide To The Use of Psychotropic Medications During Pregnancy and Lactationpinguin.bloomNo ratings yet
- Generalized Anxiety DisorderDocument16 pagesGeneralized Anxiety Disordernns5rrg2rdNo ratings yet
- Cochise Tail Oa Group ProjectDocument13 pagesCochise Tail Oa Group Projectapi-644444841No ratings yet
- Treatment of Pediatric Migraine: Current Treatment Options in Neurology January 2015Document20 pagesTreatment of Pediatric Migraine: Current Treatment Options in Neurology January 2015akshayajainaNo ratings yet
- Jurnal Kedokteran Dan Kesehatan Indonesia Keme Suko Koade EnglishDocument11 pagesJurnal Kedokteran Dan Kesehatan Indonesia Keme Suko Koade Englishangga faltraNo ratings yet
- Inpatient Geriatric Psychiatry: Optimum Care, Emerging Limitations, and Realistic GoalsFrom EverandInpatient Geriatric Psychiatry: Optimum Care, Emerging Limitations, and Realistic GoalsHoward H. FennNo ratings yet
- Using Motivational Interviewing To Manage Process Markers of Ambivalence and Resistance in Cognitive Behavioral TherapyDocument11 pagesUsing Motivational Interviewing To Manage Process Markers of Ambivalence and Resistance in Cognitive Behavioral TherapyJan LAWNo ratings yet
- Toward A Theory of Motivational InterviewingDocument11 pagesToward A Theory of Motivational InterviewingJan LAWNo ratings yet
- Sound Healing Mood, Emotional, and Spiritual Well-Being InterrelationshipsDocument12 pagesSound Healing Mood, Emotional, and Spiritual Well-Being InterrelationshipsJan LAWNo ratings yet
- On The Use of AI For Generation of Functional Music To Improve Mental HealthDocument6 pagesOn The Use of AI For Generation of Functional Music To Improve Mental HealthJan LAWNo ratings yet
- The Global Economic Burden of Health Anxiety Hypochondriasis A Systematic ReviewDocument11 pagesThe Global Economic Burden of Health Anxiety Hypochondriasis A Systematic ReviewJan LAWNo ratings yet
- Impact of Singing Bowl Playing On The Brain Using EegDocument13 pagesImpact of Singing Bowl Playing On The Brain Using EegJan LAWNo ratings yet
- Suicidal Ideation - StatPearls - NCBI BookshelfDocument35 pagesSuicidal Ideation - StatPearls - NCBI BookshelfJan LAWNo ratings yet
- On CitizenshipDocument98 pagesOn CitizenshipJan LAWNo ratings yet
- Weighing Patients Within Cognitive-Behavioural Therapy For EatingDocument10 pagesWeighing Patients Within Cognitive-Behavioural Therapy For EatingJan LAWNo ratings yet
- Social Work With Children and Families Developing Advanced PracticeDocument268 pagesSocial Work With Children and Families Developing Advanced PracticeJan LAW100% (1)
- The Effects of Strength Exercise On Hippocampus Volume and Functional Fitness Od Older WomenDocument7 pagesThe Effects of Strength Exercise On Hippocampus Volume and Functional Fitness Od Older WomenJan LAWNo ratings yet
- Working With Denied Child Abuse The Resolutions ApproachDocument225 pagesWorking With Denied Child Abuse The Resolutions ApproachJan LAWNo ratings yet
- Current Views On Neuroplasticity What Is New and What Is OldDocument14 pagesCurrent Views On Neuroplasticity What Is New and What Is OldJan LAWNo ratings yet
- Unsettling ExilesDocument321 pagesUnsettling ExilesJan LAWNo ratings yet
- Counselling Skills For Becoming A Wiser PractitionerDocument232 pagesCounselling Skills For Becoming A Wiser PractitionerJan LAWNo ratings yet
- Social Work and Climate Justice International PerspectivesDocument219 pagesSocial Work and Climate Justice International PerspectivesJan LAWNo ratings yet
- Counsellor Competencies Developing Counselling Skills For Education Career and OccupationDocument246 pagesCounsellor Competencies Developing Counselling Skills For Education Career and OccupationJan LAW100% (1)
- BPD Concept MapDocument3 pagesBPD Concept Mapsammillepointer86No ratings yet
- Professional Counseling ConsentDocument3 pagesProfessional Counseling ConsentBLAST REHANNo ratings yet
- Kennedy Axis VDocument14 pagesKennedy Axis VMihaelaNo ratings yet
- Depressed Medical Students' Use of Mental HealthDocument4 pagesDepressed Medical Students' Use of Mental HealthKoas HAYUU 2022No ratings yet
- SLM MET 4 - Powers of The Mind 1Document22 pagesSLM MET 4 - Powers of The Mind 1KITHNo ratings yet
- SW 109 Topic 5 MaladjustmentDocument11 pagesSW 109 Topic 5 MaladjustmentROSARIO CHARLENE IRISH P.No ratings yet
- CBT Competences - Map Sept 2015Document1 pageCBT Competences - Map Sept 2015Roxana BlejeruNo ratings yet
- Case Scenario 1 SchizophreniaDocument3 pagesCase Scenario 1 SchizophreniaJane LaquihonNo ratings yet
- Deviance Conformity and Social Control in Canada Canadian 4th Edition Bereska Test BankDocument22 pagesDeviance Conformity and Social Control in Canada Canadian 4th Edition Bereska Test Bankpseudolatakia.drbn100% (28)
- 04f 5 Vanderbilt Scales Scoring Instructions - WMDocument3 pages04f 5 Vanderbilt Scales Scoring Instructions - WMThi LêNo ratings yet
- Freedom From DistractibilityDocument4 pagesFreedom From DistractibilityΚων/να ΠαπNo ratings yet
- Hydrotherapy in OTDocument4 pagesHydrotherapy in OTPauleen SenoNo ratings yet
- Psychiatric Morbidity Among Female Commercial Sex Workers: Marboh Goretti Iaisuklang, Arif AliDocument6 pagesPsychiatric Morbidity Among Female Commercial Sex Workers: Marboh Goretti Iaisuklang, Arif AliAmit TamboliNo ratings yet
- CBT For Psychosis Process-Orientated Therapies and The Third Wave (Caroline Cupitt (Editor) ) (Z-Library)Document190 pagesCBT For Psychosis Process-Orientated Therapies and The Third Wave (Caroline Cupitt (Editor) ) (Z-Library)Néstor X. PortalatínNo ratings yet
- ChisuaDocument11 pagesChisuaDewanti PramitasariNo ratings yet
- ADHD Teens (Colleen Alexander-Roberts)Document264 pagesADHD Teens (Colleen Alexander-Roberts)asis musliminNo ratings yet
- Catatonia 1Document34 pagesCatatonia 1pallavi priyamNo ratings yet
- Adhd Research Paper PDFDocument7 pagesAdhd Research Paper PDFgw1w9reg100% (1)
- Chapter 13Document5 pagesChapter 13April Rose ElopreNo ratings yet
- Neebs Mental Health Nursing 5Th Edition PDF Full Chapter PDFDocument53 pagesNeebs Mental Health Nursing 5Th Edition PDF Full Chapter PDFbiliuskaraev100% (6)
- 10 1002@nur 22006Document3 pages10 1002@nur 22006RAMON ZANIPATIN CHRISTIAN DANIELNo ratings yet
- Internship ReportDocument16 pagesInternship ReportRACHANA MURALIDHAR 1833279No ratings yet
- Chap 17Document2 pagesChap 17Divine Rose TuquibNo ratings yet
- Happy Mind, Happy Life: A Mental Health ProgramDocument14 pagesHappy Mind, Happy Life: A Mental Health ProgramGian Marion MocaliNo ratings yet
- Psychotherapy - MCQs - BDocument18 pagesPsychotherapy - MCQs - BphanishashidharNo ratings yet
- Final INTERNSHIP REPORT 3Document30 pagesFinal INTERNSHIP REPORT 3ASMITA SHARMANo ratings yet
- Eating DisordersDocument15 pagesEating DisordersJana Marie CorpuzNo ratings yet
- Eating Disorders in ChildrenDocument16 pagesEating Disorders in Childrenzaireenbelo2No ratings yet