Professional Documents
Culture Documents
Case Study Format
Case Study Format
Uploaded by
janOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Case Study Format
Case Study Format
Uploaded by
janCopyright:
Available Formats
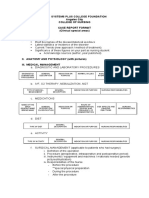
CASE STUDY FORMAT
I. INTRODUCTION
A. Background of the study
1. Patient Case Description
2. Micro Case Situation
3. Macro Case Situation
B. Objective (general & specific showing Knowledge, Skills & Attitude)
C. Scope and Delimitation
D. Theoretical Framework
II. BIOGRAPHIC DATA
Patients’ initial
Address
Age
Sex
Race
Marital Status
Occupation
Religion
Health care financing/source of medical care
Date of Admission
III. CHIEF COMPLAINT OR REASON FOR VISIT
Clinical diagnosis upon admission:
IV. NURSING HISTORY (with guide questionnaire)
A. History of Present Illness
B. Past Medical History
C. Family History of Illness (Genogram-both grandfather/mother {until 3rd generation})
D. Developmental History (for Pediatric cases only; with Assessment Guide)
E. Psychiatric History for Mental Health
F. Obstetric History (for OB cases only; with Assessment Guide)
Note: Assessment guide used should be attached at the back of the case study report.
V. FUNCTIONAL HEALTH PATTERN (with guide questionnaire)
1. Health Perception and Health Management Pattern
2. Nutrition and Metabolic Pattern
3. Elimination Pattern
4. Activity-Exercised Pattern (use Barthel index)
5. Sleep-rest Pattern
6. Cognitive-perceptual Pattern
7. Self-perception and self-control Pattern
8. Role-relationship Pattern
9. Sexuality-reproductive Pattern
10. Coping-stress tolerance Pattern
11. Value-belief Pattern
12. Emotional Pattern
13. Cultural Pattern
14. Recreation Pattern
15. Environment
16. Hygiene
17. Substance Used
Interpretation:
Analysis: (Provide end note Ex. Lana, 2019)
NOTE: Applied in each health pattern
NOTE: The following data must be presented in a tabulated format:
a. Nutrition & metabolic pattern
b. Elimination Pattern
c. Activity-Exercise Patterns
d. Sleep – rest pattern
e. Substance use/use of medications
Before Hospitalization During Hospitalization Analysis/inference References
VI. REVIEW OF SYSTEM (subjective complaints)
Case Study Format 1|P a g e
VII. PHYSICAL ASSESSMENT (all objective findings; indicate date performed; Head to Toe assessment
follow
IPPA sequence)
General Survey (Short Paragraph)
Vital Signs
BODY PART (Technique NORMAL ACTUAL INTERPRETATION/ ANALYSIS
used) FINDINGS FINDINGS With reference
Based on the pathophysiologic
analysis of the patients’ disease
process.
VIII. ANATOMY & PHYSIOLOGY
A. With anatomical figure
B. Include structure description
IX. DIAGNOSTIC/LABORATORY PROCEDURES
Date INDICATION NSG.CONSIDERATI NORMAL ACTUAL ANALYSIS/
(chronological) FOR THE ON VALUE/ RESULT/ INTERPRETATION
TEST/ BEFORE & AFTER FINDINGS/ FINDINGS/ (with Reference;
NAME OF TEST/ PROCEDUR THE PROCEDURE IMPRESSIO with pathophysiologic
PROCEDURE E N relevance)
X. SURGICAL PROCEDURE (Refer to Operative worksheet if applicable)
XI. PATHOPHYSIOLOGY (Present in Schematic Diagram; Concept/Mind mapping/ Obstetric Physiology
Analysis)
XII. DRUG STUDY/ IV INFUSIONS/ BLOOD TRANSFUSIONS, AND TREATMENTS
DATE TRADE/ PHARMA INDICATIO ADVERSE DESIRED NURSING
ORDERED/ BRAND COLOGI N AND EFFECTS ACTION ON RESPONSIBILITIES/PRE
STARTED NAME C CONTRAI OF THE CLIENT CAUTIONS
DRUG ORDER ACTION NDICATIO DRUG
(Generic name, OF NS (disease related)
dosage, route, DRUG
frequency) (disease
related)
INFUSION/ CLASSIFICATION INDICATION CONTRAINDICATIO NURSING RESPONSIBILITIES/
TREATMEN N PRECAUTIONS
T
XIII. COURSE IN THE WARD (narrative form)
Summary of day to day medical/nursing management from the date of admission up to the time
case study was done
Patient’s Status:
General condition of the client (LOC, VS, Subjective & Objective, complaint during the day)
Patient Condition & 4 D’s with inference/analysis:
o Drugs/IVF
o Diagnostics/Lab. Procedure
o Diet
o Disposition (special order, instruction)
XIV. PRIORITIZED LIST OF NURSING DIAGNOSES (Table)
Prioritized using ABC’s , Actual or Potential Problem, Maslow’s Hierarchy of Needs
Include 1st three priority diagnoses only
DATE NURSING PROBLEMS CUES JUSTIFICATION
IDENTIFIED
XV . NURSING CARE PLAN
Case Study Format 2|P a g e
ASSESSME NURSING BACKGROUND GOALS AND NURSING EVALUATION
NT DIAGNOSI KNOWLEDGE/ OBJECTIVES INTERVENTION (narrative form)
S (Problem ANALYSIS(Pathophys (include long and S AND
Subjective & Etiology) iology/ psychosocial short term RATIONALE Efficiency
Objective explanation or objectives) (with reference) Accuracy
Measureme consequences of the Is the problem:
nt nursing diagnosis) Independent met?
Dependent partially met?
Collaborative not met?
XVI. FINAL DIAGNOSIS (if for discharge)
XVII. PROPOSED/DISCHARGE PLAN (to be submitted by students whose patients are for discharge)
M – Medications to take at home
E – Exercises
T – Treatment
H – Health Teachings
O – Out - patient follow-up
D – Diet
S – Spiritual/Sexual activity (optional)
Writing Style & Format
1. Cover Page (see attachment)
2. Table of contents (small Roman Numeral pagination)
3. References (APA Format)
4. Legal Size
5. Page margination 1.5x1x1x1
6. Font Arial
7. Font Size 12
8. Double spaced (except for cover page, table of contents, references, NCP, Drug Study, and all in
tabular form).
9. Pagination – upper right
Prepare 4 sets of the manuscript (for panelist only).
10. Submit the manuscript to your adviser for proof reading 3 days before the schedule presentation.
End Stage Renal Disease
Case Study Format 3|P a g e
A case study
Presented to the faculty of Nursing
New Era University
In Partial fulfillment of the requirement for the Course _______, Concept of _________
Presented by:
BSN Level II, Group ____
Name of members
Date of Exposure
__________ Semester, AY ________________
Case Study Format 4|P a g e
You might also like
- Bids For Connection Quiz - GottmanDocument4 pagesBids For Connection Quiz - GottmanHollie123083% (6)
- Holes Lesson PlanDocument3 pagesHoles Lesson Planapi-270543697No ratings yet
- SOAPE TemplateDocument6 pagesSOAPE Templatemuhahss100% (1)
- Case Study Format 1Document4 pagesCase Study Format 1javenn mackenzieNo ratings yet
- Case Study FormatDocument4 pagesCase Study Formatjohn datuNo ratings yet
- Case Study FormatDocument4 pagesCase Study Formatjavenn mackenzieNo ratings yet
- Case Study FormatDocument2 pagesCase Study Formatgrandpa12No ratings yet
- Case Format 2024 RevisedDocument10 pagesCase Format 2024 RevisedGave gonzalesNo ratings yet
- NCS UpdatedDocument8 pagesNCS UpdatedwalaNo ratings yet
- Clinical Case Study Format General Ward 1Document3 pagesClinical Case Study Format General Ward 1Fita ClanNo ratings yet
- Case Study FormatDocument4 pagesCase Study FormatLuiezt BernardoNo ratings yet
- Nursing Process EBN Format OB PEDIADocument5 pagesNursing Process EBN Format OB PEDIAAnn Nicole UlitNo ratings yet
- Nursing Process EBN Format OB PEDIADocument5 pagesNursing Process EBN Format OB PEDIAChezka Orton Swift BolintiamNo ratings yet
- Brief Description of The Disease/statistical IncidenceDocument2 pagesBrief Description of The Disease/statistical IncidenceLeanne Princess Gamboa100% (1)
- Case Study Format 1Document4 pagesCase Study Format 1Michelle Rose RodaviaNo ratings yet
- Case Presentation Format 1Document4 pagesCase Presentation Format 1Ayessa Camelle DumileNo ratings yet
- Nursing Process EBN Format OB PEDIA NormalDocument5 pagesNursing Process EBN Format OB PEDIA Normalquesandara16No ratings yet
- Case Study FormatDocument9 pagesCase Study FormatALIZA BAKILNo ratings yet
- Case Study FormatDocument2 pagesCase Study FormatWendy Grace Yasay SantueleNo ratings yet
- Annex B.4 Sample Concept Mapping FormatDocument2 pagesAnnex B.4 Sample Concept Mapping FormatSen SioNo ratings yet
- Jhson Aham Prime Osce RubricDocument6 pagesJhson Aham Prime Osce RubricTony NguyenNo ratings yet
- Case Study FormatDocument4 pagesCase Study Formatapi-76740522No ratings yet
- Pedia Case Study FormatDocument4 pagesPedia Case Study FormatJohn Carlo B. Dungca100% (1)
- 2021 TDC Module Case Analysis GuidelinesDocument5 pages2021 TDC Module Case Analysis GuidelinesLeuqcar Ramos DonascoNo ratings yet
- Case Study Hospital FormatDocument3 pagesCase Study Hospital Formatsenyorakath0% (1)
- Grand Case Presentation FormatDocument7 pagesGrand Case Presentation FormatRENEROSE TORRESNo ratings yet
- Nursing Assessment Ii: Normal Pattern Before Hospitalization Clinical Appraisal Initial Day 1 Day 2 Day 3Document27 pagesNursing Assessment Ii: Normal Pattern Before Hospitalization Clinical Appraisal Initial Day 1 Day 2 Day 3DeejNo ratings yet
- PICO: Model For Clinical Questions: Evidence-Based Medicine August 2018Document3 pagesPICO: Model For Clinical Questions: Evidence-Based Medicine August 2018ShervieNo ratings yet
- Concept Mapping FormatDocument2 pagesConcept Mapping FormatL Rean Carmelle MAGALLONESNo ratings yet
- EPI 2.05 Overview of Analytic Observational StudiesDocument7 pagesEPI 2.05 Overview of Analytic Observational StudiesJoher MendezNo ratings yet
- Nursing Health History FormatDocument7 pagesNursing Health History FormatJasmine PonceNo ratings yet
- Nursing Health History FormatDocument7 pagesNursing Health History Formatgeraldine suarezNo ratings yet
- Case Analysis Format: Medical-Surgical & Maternal and Child Health Nursing ConceptsDocument4 pagesCase Analysis Format: Medical-Surgical & Maternal and Child Health Nursing ConceptsEmmy Flor ValmoriaNo ratings yet
- PRELIMS - NCMA216 TRANS - Nursing Process in PharmacologyDocument2 pagesPRELIMS - NCMA216 TRANS - Nursing Process in Pharmacologybnancajas7602valNo ratings yet
- 71 Principles of Patient ManagementDocument10 pages71 Principles of Patient ManagementAlluc Medical CentreNo ratings yet
- Case Study (HOSPITAL)Document4 pagesCase Study (HOSPITAL)Reyna Mee AhiyasNo ratings yet
- Far Eastern University Institute of Nursing: Individual/ Group Nursing Process FormatDocument7 pagesFar Eastern University Institute of Nursing: Individual/ Group Nursing Process FormatGamer DogeNo ratings yet
- St. Paul University Dumaguete College of Nursing Dumaguete CityDocument12 pagesSt. Paul University Dumaguete College of Nursing Dumaguete Cityzoie ziazzetteNo ratings yet
- Study DesignsDocument108 pagesStudy DesignsJobel FernandezNo ratings yet
- SCARE Checklist Topic Item Checklist Item Description Page NumberDocument3 pagesSCARE Checklist Topic Item Checklist Item Description Page NumberAhmad Fathira FitraNo ratings yet
- De Carvalho Nagliate Et Al - 2013 - Measures of Knowledge About Standard PrecautionsDocument6 pagesDe Carvalho Nagliate Et Al - 2013 - Measures of Knowledge About Standard PrecautionsBlake Toscani Apaza PerezNo ratings yet
- NCP and CNPDocument37 pagesNCP and CNPDen TupasNo ratings yet
- The Clinical and Research Question in Physiotherapy: The PICO AcronymDocument5 pagesThe Clinical and Research Question in Physiotherapy: The PICO Acronymसन्दिप पौडेलNo ratings yet
- Far Eastern University Institute of Nursing: Individual/ Group Nursing Process FormatDocument4 pagesFar Eastern University Institute of Nursing: Individual/ Group Nursing Process FormatDannielle EvangelistaNo ratings yet
- Evidence-Based Practice: Joslin John Assistant Professor Caritas College of NursingDocument30 pagesEvidence-Based Practice: Joslin John Assistant Professor Caritas College of NursingJOSLINNo ratings yet
- UTI Practicum Make-Up Assignment FINALDocument8 pagesUTI Practicum Make-Up Assignment FINALlmstar98No ratings yet
- Case Study Psyche Form 2023Document6 pagesCase Study Psyche Form 2023Hanniel Jufet GolosindaNo ratings yet
- Biostat Lec M1-8Document25 pagesBiostat Lec M1-8Mohammad MasacalNo ratings yet
- Clinical Research and Organization Sheet Bnur2901 For BBDocument4 pagesClinical Research and Organization Sheet Bnur2901 For BBcallytedford5No ratings yet
- Nusring Case Analysis FormatDocument6 pagesNusring Case Analysis Formatchazney casianoNo ratings yet
- Lecture IV - Cross Sectional - EPHD 320 - 2019Document40 pagesLecture IV - Cross Sectional - EPHD 320 - 2019Monique ChaayaNo ratings yet
- Lecture 1 - IntroductionDocument58 pagesLecture 1 - IntroductionJames LittleNo ratings yet
- HA Lab SAS26 Putting It All TogetherDocument9 pagesHA Lab SAS26 Putting It All TogetherMathewNo ratings yet
- Study Design in Medical ResearchDocument6 pagesStudy Design in Medical ResearchAngelo Jude CobachaNo ratings yet
- CNP FormatDocument20 pagesCNP FormatRhona Mae HernandezNo ratings yet
- Submodule4 Epid Exprmntl-StudiesDocument15 pagesSubmodule4 Epid Exprmntl-StudiesPowell TabogocNo ratings yet
- Case Pre Write Up Eval ToolDocument2 pagesCase Pre Write Up Eval ToolEspinoza AdrianNo ratings yet
- Format and NPI FormDocument4 pagesFormat and NPI FormPrince Rener PeraNo ratings yet
- Final Epidemiology ModuleDocument185 pagesFinal Epidemiology Moduleabdullahalshehri127No ratings yet
- Purpose: Characteristics of The Nursing ProcessDocument12 pagesPurpose: Characteristics of The Nursing ProcessVanessa Mae IlaganNo ratings yet
- Clinical Epidemiology DKA NOTESDocument22 pagesClinical Epidemiology DKA NOTESTris100% (1)
- Dimensional PsychopathologyFrom EverandDimensional PsychopathologyMassimo BiondiNo ratings yet
- Getting The Most Out of RootsMagic-7-BookDocument398 pagesGetting The Most Out of RootsMagic-7-Booksuntzu1869No ratings yet
- Hiponatremia Acute ApendicitisDocument13 pagesHiponatremia Acute ApendicitisDeliciousNo ratings yet
- Week 3-Tals: 1. The Student Learning MovementDocument5 pagesWeek 3-Tals: 1. The Student Learning MovementPrincess PauleNo ratings yet
- Sexology Lecture NotesDocument32 pagesSexology Lecture NotesanaNo ratings yet
- Grade-2-4th monthly-EXAM-2023Document20 pagesGrade-2-4th monthly-EXAM-2023Riza ReambonanzaNo ratings yet
- 1.4d Emergency Shower Eye Wash Inspection ChecklistDocument1 page1.4d Emergency Shower Eye Wash Inspection ChecklistShafie ZubierNo ratings yet
- Main Idea With Robots: Directions: Read Each Passage and Ask Yourself, "What Is The Author Doing in This Paragraph?"Document2 pagesMain Idea With Robots: Directions: Read Each Passage and Ask Yourself, "What Is The Author Doing in This Paragraph?"Cristine Bernadeth CruzNo ratings yet
- School Improvement Through Better Grading PracticesDocument5 pagesSchool Improvement Through Better Grading PracticesMortega, John RodolfNo ratings yet
- MatrixDocument105 pagesMatrixAsafAhmad100% (1)
- Documentação OpenpyxlDocument35 pagesDocumentação Openpyxlbottaluan20No ratings yet
- (Industrial Marketing) : Marketing Strategies Used by Conros Steel Pvt. LTDDocument5 pages(Industrial Marketing) : Marketing Strategies Used by Conros Steel Pvt. LTDpuranpoliNo ratings yet
- The Autocar HandbookDocument228 pagesThe Autocar HandbookRahul SinghNo ratings yet
- A For and Against Essay - Exercises 1Document4 pagesA For and Against Essay - Exercises 1vaisacrujirNo ratings yet
- UAS General English-2-2021Document12 pagesUAS General English-2-2021Putri Pradnya DewantiNo ratings yet
- CAN2 Power-Train (Engine Control and Pump Control) CAN2 Power-Train (Engine Control and Pump Control)Document18 pagesCAN2 Power-Train (Engine Control and Pump Control) CAN2 Power-Train (Engine Control and Pump Control)Boran CarmonaNo ratings yet
- (A Guide To Administering Distance Learning) Chapter 5 Theories and Frameworks For Online EducationDocument25 pages(A Guide To Administering Distance Learning) Chapter 5 Theories and Frameworks For Online EducationJohn Patrick Lare Cap-atanNo ratings yet
- Chapter 2 Vectors and Two Dim Motion - Gen - Med - All SectionsDocument60 pagesChapter 2 Vectors and Two Dim Motion - Gen - Med - All Sectionsnader siamNo ratings yet
- AmanDocument10 pagesAmanAmanVatsNo ratings yet
- Bimetal Dial ThermometerDocument2 pagesBimetal Dial ThermometerAnonymous edvYngNo ratings yet
- Cera DampproofDocument2 pagesCera DampproofAnwar HussainNo ratings yet
- مغامرة تحت الارض - مكتبة المغامرات - 2Document65 pagesمغامرة تحت الارض - مكتبة المغامرات - 2alaa alaaNo ratings yet
- Lubrication System C27Document4 pagesLubrication System C27insano008No ratings yet
- Passive Suppression of Nonlinear Panel Flutter Using Piezoelectric Materials With Resonant CircuitDocument12 pagesPassive Suppression of Nonlinear Panel Flutter Using Piezoelectric Materials With Resonant CircuitYonghui XUNo ratings yet
- Project ManagementDocument41 pagesProject ManagementOm Prakash SharmaNo ratings yet
- Week 3Document2 pagesWeek 3Jasmine Morante AntonioNo ratings yet
- Seca717,757 - Service ManualDocument17 pagesSeca717,757 - Service ManualSergio PérezNo ratings yet
- Isolve Sata: Product Features and BenefitsDocument2 pagesIsolve Sata: Product Features and BenefitsShah DhavalNo ratings yet
- UCOL Online Style GuideDocument8 pagesUCOL Online Style GuideucoledtechNo ratings yet