Professional Documents
Culture Documents
Pattern and Outcome of Dengue Fever in A
Pattern and Outcome of Dengue Fever in A
Uploaded by
Bambang SudjatmikoCopyright:
Available Formats
You might also like
- NarrativeReview - Fluid Management in Children With Severe DengueDocument14 pagesNarrativeReview - Fluid Management in Children With Severe DenguePamela JumpNo ratings yet
- Couden - Final Chikungunya Health Impact Framework PaperDocument15 pagesCouden - Final Chikungunya Health Impact Framework Paperapi-449016836100% (1)
- Kegawatdaruratan Emergency DBD AnakDocument2 pagesKegawatdaruratan Emergency DBD AnakTheresia ChesarNo ratings yet
- Original ArticleDocument6 pagesOriginal Articlethasim.evrNo ratings yet
- Zinc in RandomizedDocument6 pagesZinc in RandomizedSanti IskandarNo ratings yet
- Clinical and Laboratory Characteristics of Pediatric Dengue Fever Patients in A Tertiary Care HospitalDocument4 pagesClinical and Laboratory Characteristics of Pediatric Dengue Fever Patients in A Tertiary Care HospitalPratiwi UmbohNo ratings yet
- Karakteristik Infeksi Virus Dengue Pada Pasien Anak Di Poliklinik Anak Rumah Sakit Umum Pusat (Rsup) Sanglah, Denpasar Tahun 2016Document7 pagesKarakteristik Infeksi Virus Dengue Pada Pasien Anak Di Poliklinik Anak Rumah Sakit Umum Pusat (Rsup) Sanglah, Denpasar Tahun 2016Ananta Bryan Tohari WijayaNo ratings yet
- 838 3348 1 PBDocument7 pages838 3348 1 PBararapiaNo ratings yet
- Prognostic Factors of Severe Dengue Infections in ChildrenDocument11 pagesPrognostic Factors of Severe Dengue Infections in ChildrenDoraemon BiruNo ratings yet
- A Two-Year Review On Epidemiology and Clinical Characteristics of Dengue Deaths in Malaysia, 2013-2014Document16 pagesA Two-Year Review On Epidemiology and Clinical Characteristics of Dengue Deaths in Malaysia, 2013-2014ibnu malikNo ratings yet
- Clinical and Demographic Profile of Pediatric Patients With Dengue Fever Admitted in Three Hospitals in Tagbilaran City 2161 0665 1000332Document6 pagesClinical and Demographic Profile of Pediatric Patients With Dengue Fever Admitted in Three Hospitals in Tagbilaran City 2161 0665 1000332nailaNo ratings yet
- AsdsfDocument6 pagesAsdsfvirta andhikaNo ratings yet
- Etiologic and Epidemiologic Analysis of Hand FootDocument9 pagesEtiologic and Epidemiologic Analysis of Hand FootAisah AisahNo ratings yet
- Research Proposal A. Title Page Personal DataDocument4 pagesResearch Proposal A. Title Page Personal DataAfdaliaNo ratings yet
- Annotated Reading - DHF (Pedia)Document5 pagesAnnotated Reading - DHF (Pedia)Ma. Ferimi Gleam BajadoNo ratings yet
- Dengue Disease Spectrum Among Infants in The 2001 Dengue Epidemic in Chennai, Tamil Nadu, IndiaDocument3 pagesDengue Disease Spectrum Among Infants in The 2001 Dengue Epidemic in Chennai, Tamil Nadu, IndiaReju VijayandranNo ratings yet
- 35 Iajps35052018-1 PDFDocument4 pages35 Iajps35052018-1 PDFiajpsNo ratings yet
- Cureus 0015 00000048171Document9 pagesCureus 0015 00000048171Adistha Eka Noveyani,No ratings yet
- JFamMedPrimaryCare831022-3758081 102620Document6 pagesJFamMedPrimaryCare831022-3758081 102620miss.JEJENo ratings yet
- Pang Et Al 2014Document11 pagesPang Et Al 2014paiskopaxiew888No ratings yet
- 2 A Population Based Cohort Study On Chronic Comorbidity Risk Factors For Adverse Outcome in DengueDocument8 pages2 A Population Based Cohort Study On Chronic Comorbidity Risk Factors For Adverse Outcome in Denguerommelbasket08No ratings yet
- Severe Dengue in The Intensive Care UnitDocument18 pagesSevere Dengue in The Intensive Care UnitHitallo BezerraNo ratings yet
- Prevalence and Associated Risk Factors of Sepsis Among Neonates Admitted Into Neonatal Intensive Care Units of Public Hospitals in DhakaDocument12 pagesPrevalence and Associated Risk Factors of Sepsis Among Neonates Admitted Into Neonatal Intensive Care Units of Public Hospitals in DhakaAnonymous SMLzNANo ratings yet
- 1 s2.0 S0929664621003892 MainDocument8 pages1 s2.0 S0929664621003892 Mainrheynamaulidar rumoninNo ratings yet
- Direct Cost of Illness For Dengue in Hospitalized - 2019 - International JournalDocument4 pagesDirect Cost of Illness For Dengue in Hospitalized - 2019 - International JournalShelly TanNo ratings yet
- JFMPC 8 1022Document6 pagesJFMPC 8 1022SasbellaNo ratings yet
- Case Control ExDocument8 pagesCase Control ExmujahidatinstituteNo ratings yet
- Guo Et Al 2017Document11 pagesGuo Et Al 2017Ana Beatriz Vasquez RodriguezNo ratings yet
- Research Article: Does Comorbidity Increase The Risk of Dengue Hemorrhagic Fever and Dengue Shock Syndrome?Document6 pagesResearch Article: Does Comorbidity Increase The Risk of Dengue Hemorrhagic Fever and Dengue Shock Syndrome?Erena HairunisaNo ratings yet
- Varicella DengueDocument3 pagesVaricella DengueDian Fajar FebrianiNo ratings yet
- Research Imd 21 Section A: Topic: Dengue FeverDocument15 pagesResearch Imd 21 Section A: Topic: Dengue FeverAayush KhanvilkarNo ratings yet
- International Journal of Pediatric Research Ijpr 9 111Document6 pagesInternational Journal of Pediatric Research Ijpr 9 111VsbshNo ratings yet
- Dengue Typhoid Co-Infection: A New Threat: Case ReportDocument2 pagesDengue Typhoid Co-Infection: A New Threat: Case ReportJohn Bryan JamisonNo ratings yet
- Dengue Fever Case StudyDocument55 pagesDengue Fever Case StudyGlory Holmes67% (6)
- Dengue LancetDocument16 pagesDengue LancetJorge Ricardo Uchuya GómezNo ratings yet
- Complicaciones Neurológicas de Las Infecciones Por Rotavirus en Niños Ped Inf Dis 07 2023Document4 pagesComplicaciones Neurológicas de Las Infecciones Por Rotavirus en Niños Ped Inf Dis 07 2023ANNIX FERRERNo ratings yet
- Dengue Hemorrhagic Fever and Shock Syndromes : Suchitra Ranjit, MBBS, MD Niranjan Kissoon, MBBS, FAAP, FCCM, FACPEDocument11 pagesDengue Hemorrhagic Fever and Shock Syndromes : Suchitra Ranjit, MBBS, MD Niranjan Kissoon, MBBS, FAAP, FCCM, FACPEvalenzuelacastilloNo ratings yet
- Intensified Short Symptom Screening Program For Dengue Infection During Pregnancy, IndiaDocument6 pagesIntensified Short Symptom Screening Program For Dengue Infection During Pregnancy, IndiaJose Luis RChNo ratings yet
- Journal Pone 0190637Document15 pagesJournal Pone 0190637cooky maknaeNo ratings yet
- Tropicalmed 08 00086 v2Document24 pagesTropicalmed 08 00086 v2Radityo Ali MurtiNo ratings yet
- Estudio en Bangladesh 2022Document11 pagesEstudio en Bangladesh 2022ADAN CARLOS DANIEL GUERRERO MEDINANo ratings yet
- Dengue Fever: AssignmentDocument14 pagesDengue Fever: AssignmentRenx KhanNo ratings yet
- 44 RevDocument14 pages44 RevAsshiddiqie ColectionNo ratings yet
- Dengue Infection in Children in Ratchaburi, Thailand: A Cohort Study. II. Clinical ManifestationsDocument11 pagesDengue Infection in Children in Ratchaburi, Thailand: A Cohort Study. II. Clinical ManifestationsMey KhNo ratings yet
- Dengue Management in Triage Using Ultrasound in CHDocument11 pagesDengue Management in Triage Using Ultrasound in CHYuning tyas Nursyah FitriNo ratings yet
- Anak Bu HeniDocument10 pagesAnak Bu HeniVeronika IntanNo ratings yet
- Journal PNTD 0001244Document10 pagesJournal PNTD 0001244Zulia Ahmad BurhaniNo ratings yet
- Sciencedirect: Hong-Jie Kuo, Ing-Kit Lee, Jien-Wei LiuDocument9 pagesSciencedirect: Hong-Jie Kuo, Ing-Kit Lee, Jien-Wei LiuzihanNo ratings yet
- Dengue Hemorrhagic Fever e A Systemic Literature Review of Current Perspectives On Pathogenesis, Prevention and ControlDocument16 pagesDengue Hemorrhagic Fever e A Systemic Literature Review of Current Perspectives On Pathogenesis, Prevention and ControlMichael Jansen SulaimanNo ratings yet
- The Rise of Imported Dengue Infections in Victoria, Australia, 2010-2016Document11 pagesThe Rise of Imported Dengue Infections in Victoria, Australia, 2010-2016Satriya WibawaNo ratings yet
- Journal Pone 0138465Document16 pagesJournal Pone 0138465Indra IhsanNo ratings yet
- Dengue in Pregnancy: AbstractDocument3 pagesDengue in Pregnancy: AbstractsharenNo ratings yet
- Jurnal 1Document8 pagesJurnal 1aziskarnNo ratings yet
- Nguyen Minh Tuan 2013Document8 pagesNguyen Minh Tuan 2013libremdNo ratings yet
- DENGUE HEMORRHAGIC FEVER-final N ToDocument52 pagesDENGUE HEMORRHAGIC FEVER-final N ToRachel Ann CorpuzNo ratings yet
- Usg For DBDDocument5 pagesUsg For DBDhappy gummyNo ratings yet
- 1 s2.0 S2667100X23000567 MainDocument18 pages1 s2.0 S2667100X23000567 MainEnrique CastelanNo ratings yet
- Difyeri IndiaDocument5 pagesDifyeri IndiaDian Fajar FebrianiNo ratings yet
- Diagnosis and Treatment of Chronic CoughFrom EverandDiagnosis and Treatment of Chronic CoughSang Heon ChoNo ratings yet
- Infectious Diseases in the Intensive Care UnitFrom EverandInfectious Diseases in the Intensive Care UnitManish SonejaNo ratings yet
- Burn-Like Skin Necrosis in A Patient Following Infusion of Sodium BicarbonateDocument3 pagesBurn-Like Skin Necrosis in A Patient Following Infusion of Sodium BicarbonateViniFortunataNo ratings yet
- Dengue LancetDocument16 pagesDengue LancetJorge Ricardo Uchuya GómezNo ratings yet
- Snake Bite ManagementDocument92 pagesSnake Bite ManagementManoharNo ratings yet
- 2nd Webinar HighlightDocument5 pages2nd Webinar HighlightYS NateNo ratings yet
- Dengue Management Guideline 2020, Training Materials Top SheetDocument257 pagesDengue Management Guideline 2020, Training Materials Top Sheetdeepak das100% (1)
- Dengue Fever by LubnaDocument47 pagesDengue Fever by LubnaDr AnilNo ratings yet
- Materi DR Martin PDFDocument93 pagesMateri DR Martin PDFFajar Agustian Combachie Part IINo ratings yet
- DengueDocument70 pagesDengueVijay ArumugamNo ratings yet
- Dengue Guidelines For Electronic Circulation - CompressedDocument73 pagesDengue Guidelines For Electronic Circulation - CompressedakeelNo ratings yet
- Dengue Virus Infection - Prevention and Treatment - UpToDateDocument32 pagesDengue Virus Infection - Prevention and Treatment - UpToDateAnderson SilvaNo ratings yet
- Idiopathic Systemic Capillary Leak Syndrome - UpToDateDocument17 pagesIdiopathic Systemic Capillary Leak Syndrome - UpToDatenikos papamakariosNo ratings yet
- Revised National Guideline For Clinical Management of Dengue Syndrome 2018Document112 pagesRevised National Guideline For Clinical Management of Dengue Syndrome 2018rony ghoshNo ratings yet
- DengueDocument45 pagesDengueRachel AlbertNo ratings yet
- Revised Dengue Guideline 2020 PDFDocument98 pagesRevised Dengue Guideline 2020 PDFAbid Hasan ZiKonNo ratings yet
- Dengue 2Document56 pagesDengue 2Eliz Codilla-SyNo ratings yet
- Dengue Feve1Document10 pagesDengue Feve1Santhosh KumarNo ratings yet
- Disseminated Intravascular Coagulation Initial Score As A Predictor ofDocument6 pagesDisseminated Intravascular Coagulation Initial Score As A Predictor ofPriska ForceveeanaNo ratings yet
- History Taking For FeverDocument13 pagesHistory Taking For FeverAfiQsyazwan Abd RaniNo ratings yet
- Manajemen Cairan Pada Luka BakarDocument38 pagesManajemen Cairan Pada Luka Bakarwati suwartaNo ratings yet
- Dengue (Lancet)Document16 pagesDengue (Lancet)Roberth Mero100% (1)
- Dengue 2019Document79 pagesDengue 2019Nou ChannarithNo ratings yet
- National Guidelines On Clinical Management of Dengue Infection in Pregnancy Reprint Version - New PDFDocument78 pagesNational Guidelines On Clinical Management of Dengue Infection in Pregnancy Reprint Version - New PDFsarakg vathNo ratings yet
- Hyperferritinemia in Severe Dengue Infection .13Document8 pagesHyperferritinemia in Severe Dengue Infection .13rsthsn6z8xNo ratings yet
Pattern and Outcome of Dengue Fever in A
Pattern and Outcome of Dengue Fever in A
Uploaded by
Bambang SudjatmikoOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pattern and Outcome of Dengue Fever in A
Pattern and Outcome of Dengue Fever in A
Uploaded by
Bambang SudjatmikoCopyright:
Available Formats
Open Access Original
Article DOI: 10.7759/cureus.14164
Pattern and Outcome of Dengue Fever in a
Pediatric Tertiary Hospital: A Retrospective
Report
Wajid Hussain 1 , Mehmood Shaikh 2 , Muhammad Hanif 2 , Muhammad Ashfaq 1 , Habib Ahmed 1 , Bader-u-
Nisa 1
1. Pediatrics and Child Health, Jinnah Sindh Medical University, Karachi, PAK 2. Neonatal Intensive Care Unit, Jinnah
Sindh Medical University, Karachi, PAK
Corresponding author: Mehmood Shaikh, mehmood_shaikh78@yahoo.com
Abstract
Introduction
For Pakistan, dengue has been established as a public health problem. With superimposed factors such as
poor socioeconomic conditions, limited public health awareness, poor hygiene, and sanitation conditions,
the situation has become more severe and complications have become frequent. Almost 90% of all infections
occur in children of age less than 18 years. This is a three-year retrospective report of dengue fever in
Southern Pakistan.
Methods
In this retrospective analysis, all records of patients admitted to the National Institute of Child Health,
Karachi, from May 1, 2016, till April 30, 2019, diagnosed with dengue fever were recruited. Their
demographic, clinical, and biochemical records were assessed. The outcome was also recorded. Data
were entered and analyzed using Statistical Package for Social Sciences (SPSS) for Windows version 20.0
(IBM Corp., Chicago).
Results
Among 93 cases of dengue fever, there were 71 (76.3%) male and 22 (23.7%) female children. Their mean age
was 5.7 ± 3.07 years. The mean duration from onset of disease to hospitalization was 4.2 ± 2.1 days. The
mean platelet count was 47391.30 ± 41370.61 x 109/L. Fever (100%) and abdominal pain (35.5%) were
common presentations. Bleeding episodes were seen in 31% of children, rash in 15%, disseminated
intravascular coagulation in 3%, and 1% developed pleural effusion. There were no mortalities; 87 (93.5%)
were discharged and six (6.5%) children left against medical advice.
Conclusion
Review began 12/26/2020 Fever, abdominal pain, bleeding episodes, and rash were common presentations. Hematological,
Review ended 03/27/2021 hepatological, neurological, and pleural complications were not uncommon. The outcome of the disease was
Published 03/28/2021
adequate and there were no mortalities.
© Copyright 2021
Hussain et al. This is an open access
article distributed under the terms of the
Creative Commons Attribution License Categories: Pediatrics, Infectious Disease, Epidemiology/Public Health
CC-BY 4.0., which permits unrestricted Keywords: dengue fever/complications, children, dengue related hospitalization, dengue fever
use, distribution, and reproduction in any
medium, provided the original author and
source are credited. Introduction
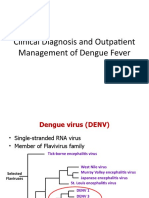
Dengue is an acute febrile arboviral illness. It is mainly endemic in tropical and subtropical areas as its
transmitting mosquito - Aedes genus - is primarily seen in both these areas. The average incubation period
is seven days (three to 14 days) [1]. The spectrum of dengue ranges from a non-severe febrile disease to a
severe systemic life-threatening illness [2].
World Health Organization (WHO), reported approximately 400 million cases of dengue fever annually and
the majority of cases of dengue fever are reported from Asian countries [3]. Dengue is now endemic in
Pakistan and a public health threat especially for children [4]. In Pakistan, superimposed factors such as poor
socioeconomic condition, limited public health awareness, poor hygiene, and sanitation conditions resulting
in a more severe form of dengue fever [5].
Dengue affects all age groups; however, 90% of dengue infections occur in children of age less than 18 years
[6]. Children have a 15-times higher risk of dying during a second episode compared to adults [7]. Fever
remains the most common presentation of dengue in children followed by vomiting, and abdominal pain [8].
Complications include severe shock, disseminated intravascular coagulation (DIC), acute respiratory distress
How to cite this article
Hussain W, Shaikh M, Hanif M, et al. (March 28, 2021) Pattern and Outcome of Dengue Fever in a Pediatric Tertiary Hospital: A Retrospective
Report. Cureus 13(3): e14164. DOI 10.7759/cureus.14164
syndrome (ARDS), and hepatic and neurological involvement [9].
Older outbreaks, particularly from northern Pakistan have been reported in detail in the literature; however,
there remains limited data depicting the situation in southern Pakistan [10-12].
Materials And Methods
For the retrospective analysis, all records of patients admitted at the National Institute of Child Health,
Karachi, from May 1, 2016, till April 30, 2019, that were diagnosed with dengue fever were recruited. After
taking permission from the hospital administration the records were recruited.
Data collection
Definition
Dengue fever: Dengue fever is an acute febrile illness defined by the presence of fever and two or more
headache, myalgia and/or bone pain, arthralgia, retro-orbital or ocular pain rash, hemorrhagic
manifestations (e.g., positive tourniquet test, petechiae, purpura/ecchymosis, epistaxis, gum bleeding, blood
in emesis, urine, or stool, or vaginal bleeding), or leukopenia.
Dengue hemorrhagic fever: It is characterized by the evidence of plasma leakage due to increased vascular
permeability, such as hemoconcentration, pleural effusion, or ascites in addition to the manifestation of
dengue fever.
Dengue shock syndrome: It consists of dengue hemorrhagic fever with marked plasma leakage that leads to
circulatory collapse (shock) as evidenced by narrowing pulse pressure or hypotension.
Admission Criteria
All those patients who visited the hospital, with a history of fever and or vomiting or rashes and according to
hospital policies sick enough requiring IV fluids.
Discharge Criteria
All dengue non-structural protein 1 (NS1) antigen or dengue serum immunoglobulin M (IgM) antibodies
against dengue positive whose platelets were more than 50 thousand, defervescence of fever for the last 24
hour, and child can take per oral without vomiting were included in the discharge criteria.
Exclusion Criteria
Patients with positive blood culture for any bacterial pathogen: Patients concomitant having B thalassemia
major, idiopathic thrombocytopenic purpura, acute leukemia, and aplastic anemia.
A semi-structured questionnaire was filled for data extraction. The variables were age and gender of the
child, date of onset of symptoms, date of hospital admission, clinical signs and symptoms and duration of
hospital stay, platelet count, dengue non-structural protein 1 (NS1), and dengue immunoglobulin M (dengue
IgM). The outcome was classified as discharge, death, and left against medical advice (LAMA).
Data analysis
All data were entered and analyzed using Statistical Package for Social Sciences (SPSS) for Windows version
20.0 (IBM Corp., Chicago). Continuous variables, such as age, duration of onset of symptoms, duration of
hospital stay, platelet count were presented as mean and standard deviation (SD) was calculated. Categorical
variables, such as gender, clinical sign, and symptoms, dengue (IgM) positive, and outcome, were presented
in frequency and percentages.
Results
Among 93 cases of dengue fever-related hospitalizations, there were 71 (76.3%) male children. The mean age
of the children was 5.7 ± 3.07 years (range: six months to 12 years). There were 15 (16.1%) hospitalizations
in 2019, 31 (33.3%) in 2018, and 47 (50.5%) in 2017 making an estimated 31 dengue-related hospital
admissions annually. Out of 93 patients, 64 (68.8%) were dengue fever, 26 (28%) were dengue hemorrhagic
fever, and three (3.22%) dengue shock syndrome.
The mean duration from onset of disease to hospitalization was 4.2 ± 2.1 days (range: two to eight days).
Demographic characteristics of enrolled patients are summarized in Table 1.
2021 Hussain et al. Cureus 13(3): e14164. DOI 10.7759/cureus.14164 2 of 6
Patient characteristics Frequency (%)
Gender
Male 71 (76.3%)
Female 22 (23.7%)
Age in years
≤5 45 (48.4%)
6-10 40 (43.0%)
≥ 11 years 8 (8.6%)
Mean ± SD 5.7 ± 3.07
Mean duration from onset of symptoms to hospital admission in days 4.2 ± 2.1
TABLE 1: Demographic characteristics of the patients (N=15)
Table 2 summarize the clinical and biochemical profile. All children had a fever and 29 (31.2%) had bleeding
from the nose, mouth, ears, or petechiae. Four (4.3%) children had hematuria. The mean platelet count was
47,391.30 ± 41,370.61 x 109/L (range: 2000-251,000 x 10 9/L).
2021 Hussain et al. Cureus 13(3): e14164. DOI 10.7759/cureus.14164 3 of 6
Patient characteristics Frequency (%)
Signs and symptoms
Fever 93(100%)
Generalized rash 14 (15.1%)
Abdominal pain 33(35.5%)
Joint pain 17 (18.3%)
Vomiting 11(11.8%)
Complications
Jaundice 9(9.6%)
Bleeding 29 (31.2%)
Petechiae 12 (12.9%)
Hematuria 4 (4.3%)
Disseminated intravascular coagulation 3 (3.2%)
Generalized/pedal edema 3(3.2%)
Pleural effusion 1 (1.1%)
Fits 1 (1.1%)
Laboratory tests
Mean platelet count x109/L at admission 47,391.30 ± 41,370.61
Only D IgM positive 34 (36.5%)
Both DNS1 and D IgM positive 12 (12.9%)
TABLE 2: Clinical characteristics of the patients (N=15)
D IgM: dengue immunoglobulin M; DNS1: dengue non-structural protein 1
Of all patients with dengue fever, 87 (93.5%) were discharged and six (6.5%) children left against medical
advice. No death was reported.
Discussion
In this analysis, it was found that the proportion of 50.5% hospitalizations due to dengue were high in 2017.
Fever, abdominal pain, and joint pain were common presentations. Bleeding, petechiae, and jaundice were
common complications. There was one case of pleural effusion and fits due to neurological involvement in
each. There were no mortalities.
Although a lot of literary work is being done to document the burden of dengue in both endemic and non-
endemic countries, the empirical data governing the pediatric population is still scarce. A large multi-center
study from India reported that 60% of children age five to 10 years had been infected with dengue at least
once (immunoglobulin G {IgG} seroprevalence positive). Upon multivariate analysis, the type of housing and
household water storage system were significant associations with seropositivity [13]. Reports from Passive
Dengue Surveillance System (PDSSS) in Puerto Rico reported more than 4000 cases of dengue in children of
age <18 months. Of all laboratory positive cases, 58% required hospitalization and 33% of hospitalized
children had severe dengue [14]. In a five-year-long study from India examining the blood samples of
suspected dengue patients age 15 years or less, 25% were positive for dengue. They were more common in
male children (58%) and children age 10-<15 years (46%) [15].
Despite the high prevalence and increasing severity with every outbreak, there still is lesser data explaining
the characteristics and outcomes of hospitalized severe cases of dengue as compared to the epidemiological
perspective of the illness. In a large cohort conducted across 10 Asian and Latin American countries, 10% of
all febrile episodes were serologically proven to be dengue; of these 11-19% were severe enough to require
hospitalization [16]. In almost all of these studies, fever, abdominal pain, vomiting, and skin rash were the
2021 Hussain et al. Cureus 13(3): e14164. DOI 10.7759/cureus.14164 4 of 6
common clinical presentation of dengue fever in children. Thrombocytopenia was also extremely common
[7,8]. The bleeding presentation was commonly reported in the form of petechiae, nose bleeds, hematuria,
hemoptysis, bleeding gums, hematemesis, melena, menorrhagia, and subconjunctival hemorrhages [6,9,17].
Among our children with dengue, only IgM was positive in 37%, and both IgM and DNS1 in 13%. Our results
are on the lower end. Comparatively, in Afroze et al., 87% of children were DNS1 positive and 15% were IgM
positive [7]. IgM was positive 41%, IgG in 24% while in 31 % of the children population both were found
positive [18]. The mean duration from onset of symptoms to hospital admission in our children was four days
which means that they were transitioning from acute to sub-acute and late phase of the disease. DNS1 alone
has been seen to be sufficient in the acute phase of the disease. None of our children had DNS1 alone
positive. A positive combination of DNS1 and IgM is highly sensitive in diagnosing both acute and late
phases of the disease [19].
The outcome of children hospitalized with dengue was very promising in our study. Only a few had severe
and life-threatening complications including DIC and pleural effusion and there were no mortalities.
Hepatorenal and neurological complications, respiratory distress, DIC, and severe shock have been reported
commonly in the literature and comprise of the common causes of death in these children [9,10,18]. In
suspecting severe dengue and studying disease progression, it is essential to comprehend the warning signs.
Hemodynamic instability is a crucial warning sign in these children. Lethargy presented 72 hours before the
onset of shock and dyspnea however 48 hours before in children with severe disease. Lethargy (adjusted
odds ratio {ORa}: 9.15), dyspnea (ORa: 8.24), and abdominal pain (ORa: 6.78) independently correlated with
the severity of dengue in these children [20].
Limitations
We identify key study limitations and suggest directions for future research on this topic: (1) this is a
retrospective study design and review of files. Prospective studies will be helpful for clinical spectrum; (2)
seasonal variations have not been considered. A longer duration of study is required to interpret accurately
for it; (3) a study comprised of a small number of patients larger sample may be a true representative.
Conclusions
Ninety-three cases of dengue fever were admitted over the three years period. Fever, abdominal pain, rash,
and bleeding episodes were common presentations. Hematological, hepatological, neurological, and pleural
complications were not uncommon. The outcome of the disease was adequate and there were no mortalities.
Additional Information
Disclosures
Human subjects: All authors have confirmed that this study did not involve human participants or tissue.
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the
following: Payment/services info: All authors have declared that no financial support was received from
any organization for the submitted work. Financial relationships: All authors have declared that they have
no financial relationships at present or within the previous three years with any organizations that might
have an interest in the submitted work. Other relationships: All authors have declared that there are no
other relationships or activities that could appear to have influenced the submitted work.
References
1. Kularatne SA: Dengue fever. BMJ. 2015, 351:4661. 10.1136/bmj.h4661
2. Laul A, Laul P, Merugumala V, Pathak R, Miglani U, Saxena P: Clinical profiles of dengue infection during an
outbreak in Northern India. J Trop Med. 2016, 2016:5917934. 10.1155/2016/5917934
3. Dengue and severe dengue. (2020). https://www.who.int/news-room/fact-sheets/detail/dengue-and-severe-
dengue.
4. Jahan F: Dengue fever (DF) in Pakistan . Asia Pac Fam Med. 2011, 10:1. 10.1186/1447-056X-10-1
5. Haider Z, Ahmad FZ, Mahmood A, et al.: Dengue fever in Pakistan: a paradigm shift; changing epidemiology
and clinical patterns. Perspect Public Health. 2015, 135:294-298. 10.1177/1757913915599019
6. Prasanna L, Jayaram G: Patho-clinical profile of dengue fever in hospitalized children . Int J Intg Med Sci.
2018, 5:700-704. 10.16965/ijims.2018.126
7. Afroze S, Shakur S, Wahab A, Shakur S: Clinical profile of dengue and predictors of its severity among
children. Am J Pediatr. 2019, 5:219-223. 10.11648/j.ajp.20190504.19
8. Jabeen U, Iftikhar A, Hamid MH, Chaudhry A: Comparison of characteristics of dengue hemorrhagic fever in
children during 2011 and 2013 outbreaks. Pak Pediatr J. 2018, 42:95-100.
9. Banerjee A, Barik KL, Bandyopadhyay A, Paul UK: A study on the clinical features of dengue virus infected
pediatric patients. Int J Contemp Pediatr. 2018 Mar, 5:368-371. 10.18203/2349-3291.ijcp20180437
10. Ahmed S, Arif F, Yahya Y, Rehman A, Abbas K, Ashraf S, Akram DS: Dengue fever outbreak in Karachi 2006-
-a study of profile and outcome of children under 15 years of age. J Pak Med Assoc. 2008, 58:4.
11. Sajid A, Ikram A, Ahmed M: Dengue fever outbreak 2011: clinical profile of children presenting at Madina
Teaching Hospital Faisalabad. J Univ Med Dent Coll. 2012, 3:42-47.
2021 Hussain et al. Cureus 13(3): e14164. DOI 10.7759/cureus.14164 5 of 6
12. Khan J, Khan I, Amin I: A comprehensive entomological, serological and molecular study of 2013 dengue
outbreak of Swat, Khyber Pakhtunkhwa, Pakistan. PLoS One. 2016, 11:0147416.
10.1371/journal.pone.0147416
13. Garg S, Chakravarti A, Singh R, et al.: Dengue serotype-specific seroprevalence among 5-to 10-year-old
children in India: a community-based cross-sectional study. Int J Infect Dis. 2017, 54:25-30.
10.1016/j.ijid.2016.10.030
14. Hause AM, Perez-Padilla J, Horiuchi K, et al.: Epidemiology of dengue among children aged< 18 months—
Puerto Rico, 1999-2011. Am J Trop Med Hyg. 2016, 94:404-408. 10.4269/ajtmh.15-0382
15. Mistry M, Chudasama RK, Goswami Y: Profile of dengue fever in hospitalized children in Saurashtra,
Gujarat, 2013-2017. Indian Pediatr. 2019, 56:123-125.
16. L’Azou M, Moureau A, Sarti E, et al.: Symptomatic dengue in children in 10 Asian and Latin American
countries. New Engl J Med. 2016, 374:1155-1166. 10.1056/NEJMoa1503877
17. Ahmed NU, Talha KA, Ibrahim MY, Selina F, Myint T, Ohn KM: Clinical presentation of dengue in a general
hospital in Bangladesh. Borneo J Med Sci. 2016, 10:60-66.
18. Alam S, Sadat S, Swapan Z, Ahmed A, Karim N, Paul HK, Zaman S: Clinical profile of dengue fever in
children. Bangladesh J Child Health. 2009, 33:55-58. 10.3329/bjch.v33i2.5678
19. Kumar D, Verma RK, Singh A, Kumar M, Singh DP, Pandey R, Krishnappa K: Evaluation of NS1, IgM ELISA
and RT-PCR in diagnosis of dengue fever. Int J Res Med Sci. 2018, 6:2440-2443. 10.18203/2320-
6012.ijrms20182832
20. Wakimoto MD, Camacho LA, Gonin ML, Brasil P: Clinical and laboratory factors associated with severe
dengue: a case-control study of hospitalized children. J Trop Pediatr. 2017, 64:373-381.
10.1093/tropej/fmx078
2021 Hussain et al. Cureus 13(3): e14164. DOI 10.7759/cureus.14164 6 of 6
You might also like
- NarrativeReview - Fluid Management in Children With Severe DengueDocument14 pagesNarrativeReview - Fluid Management in Children With Severe DenguePamela JumpNo ratings yet
- Couden - Final Chikungunya Health Impact Framework PaperDocument15 pagesCouden - Final Chikungunya Health Impact Framework Paperapi-449016836100% (1)
- Kegawatdaruratan Emergency DBD AnakDocument2 pagesKegawatdaruratan Emergency DBD AnakTheresia ChesarNo ratings yet
- Original ArticleDocument6 pagesOriginal Articlethasim.evrNo ratings yet
- Zinc in RandomizedDocument6 pagesZinc in RandomizedSanti IskandarNo ratings yet
- Clinical and Laboratory Characteristics of Pediatric Dengue Fever Patients in A Tertiary Care HospitalDocument4 pagesClinical and Laboratory Characteristics of Pediatric Dengue Fever Patients in A Tertiary Care HospitalPratiwi UmbohNo ratings yet
- Karakteristik Infeksi Virus Dengue Pada Pasien Anak Di Poliklinik Anak Rumah Sakit Umum Pusat (Rsup) Sanglah, Denpasar Tahun 2016Document7 pagesKarakteristik Infeksi Virus Dengue Pada Pasien Anak Di Poliklinik Anak Rumah Sakit Umum Pusat (Rsup) Sanglah, Denpasar Tahun 2016Ananta Bryan Tohari WijayaNo ratings yet
- 838 3348 1 PBDocument7 pages838 3348 1 PBararapiaNo ratings yet
- Prognostic Factors of Severe Dengue Infections in ChildrenDocument11 pagesPrognostic Factors of Severe Dengue Infections in ChildrenDoraemon BiruNo ratings yet
- A Two-Year Review On Epidemiology and Clinical Characteristics of Dengue Deaths in Malaysia, 2013-2014Document16 pagesA Two-Year Review On Epidemiology and Clinical Characteristics of Dengue Deaths in Malaysia, 2013-2014ibnu malikNo ratings yet
- Clinical and Demographic Profile of Pediatric Patients With Dengue Fever Admitted in Three Hospitals in Tagbilaran City 2161 0665 1000332Document6 pagesClinical and Demographic Profile of Pediatric Patients With Dengue Fever Admitted in Three Hospitals in Tagbilaran City 2161 0665 1000332nailaNo ratings yet
- AsdsfDocument6 pagesAsdsfvirta andhikaNo ratings yet
- Etiologic and Epidemiologic Analysis of Hand FootDocument9 pagesEtiologic and Epidemiologic Analysis of Hand FootAisah AisahNo ratings yet
- Research Proposal A. Title Page Personal DataDocument4 pagesResearch Proposal A. Title Page Personal DataAfdaliaNo ratings yet
- Annotated Reading - DHF (Pedia)Document5 pagesAnnotated Reading - DHF (Pedia)Ma. Ferimi Gleam BajadoNo ratings yet
- Dengue Disease Spectrum Among Infants in The 2001 Dengue Epidemic in Chennai, Tamil Nadu, IndiaDocument3 pagesDengue Disease Spectrum Among Infants in The 2001 Dengue Epidemic in Chennai, Tamil Nadu, IndiaReju VijayandranNo ratings yet
- 35 Iajps35052018-1 PDFDocument4 pages35 Iajps35052018-1 PDFiajpsNo ratings yet
- Cureus 0015 00000048171Document9 pagesCureus 0015 00000048171Adistha Eka Noveyani,No ratings yet
- JFamMedPrimaryCare831022-3758081 102620Document6 pagesJFamMedPrimaryCare831022-3758081 102620miss.JEJENo ratings yet
- Pang Et Al 2014Document11 pagesPang Et Al 2014paiskopaxiew888No ratings yet
- 2 A Population Based Cohort Study On Chronic Comorbidity Risk Factors For Adverse Outcome in DengueDocument8 pages2 A Population Based Cohort Study On Chronic Comorbidity Risk Factors For Adverse Outcome in Denguerommelbasket08No ratings yet
- Severe Dengue in The Intensive Care UnitDocument18 pagesSevere Dengue in The Intensive Care UnitHitallo BezerraNo ratings yet
- Prevalence and Associated Risk Factors of Sepsis Among Neonates Admitted Into Neonatal Intensive Care Units of Public Hospitals in DhakaDocument12 pagesPrevalence and Associated Risk Factors of Sepsis Among Neonates Admitted Into Neonatal Intensive Care Units of Public Hospitals in DhakaAnonymous SMLzNANo ratings yet
- 1 s2.0 S0929664621003892 MainDocument8 pages1 s2.0 S0929664621003892 Mainrheynamaulidar rumoninNo ratings yet
- Direct Cost of Illness For Dengue in Hospitalized - 2019 - International JournalDocument4 pagesDirect Cost of Illness For Dengue in Hospitalized - 2019 - International JournalShelly TanNo ratings yet
- JFMPC 8 1022Document6 pagesJFMPC 8 1022SasbellaNo ratings yet
- Case Control ExDocument8 pagesCase Control ExmujahidatinstituteNo ratings yet
- Guo Et Al 2017Document11 pagesGuo Et Al 2017Ana Beatriz Vasquez RodriguezNo ratings yet
- Research Article: Does Comorbidity Increase The Risk of Dengue Hemorrhagic Fever and Dengue Shock Syndrome?Document6 pagesResearch Article: Does Comorbidity Increase The Risk of Dengue Hemorrhagic Fever and Dengue Shock Syndrome?Erena HairunisaNo ratings yet
- Varicella DengueDocument3 pagesVaricella DengueDian Fajar FebrianiNo ratings yet
- Research Imd 21 Section A: Topic: Dengue FeverDocument15 pagesResearch Imd 21 Section A: Topic: Dengue FeverAayush KhanvilkarNo ratings yet
- International Journal of Pediatric Research Ijpr 9 111Document6 pagesInternational Journal of Pediatric Research Ijpr 9 111VsbshNo ratings yet
- Dengue Typhoid Co-Infection: A New Threat: Case ReportDocument2 pagesDengue Typhoid Co-Infection: A New Threat: Case ReportJohn Bryan JamisonNo ratings yet
- Dengue Fever Case StudyDocument55 pagesDengue Fever Case StudyGlory Holmes67% (6)
- Dengue LancetDocument16 pagesDengue LancetJorge Ricardo Uchuya GómezNo ratings yet
- Complicaciones Neurológicas de Las Infecciones Por Rotavirus en Niños Ped Inf Dis 07 2023Document4 pagesComplicaciones Neurológicas de Las Infecciones Por Rotavirus en Niños Ped Inf Dis 07 2023ANNIX FERRERNo ratings yet
- Dengue Hemorrhagic Fever and Shock Syndromes : Suchitra Ranjit, MBBS, MD Niranjan Kissoon, MBBS, FAAP, FCCM, FACPEDocument11 pagesDengue Hemorrhagic Fever and Shock Syndromes : Suchitra Ranjit, MBBS, MD Niranjan Kissoon, MBBS, FAAP, FCCM, FACPEvalenzuelacastilloNo ratings yet
- Intensified Short Symptom Screening Program For Dengue Infection During Pregnancy, IndiaDocument6 pagesIntensified Short Symptom Screening Program For Dengue Infection During Pregnancy, IndiaJose Luis RChNo ratings yet
- Journal Pone 0190637Document15 pagesJournal Pone 0190637cooky maknaeNo ratings yet
- Tropicalmed 08 00086 v2Document24 pagesTropicalmed 08 00086 v2Radityo Ali MurtiNo ratings yet
- Estudio en Bangladesh 2022Document11 pagesEstudio en Bangladesh 2022ADAN CARLOS DANIEL GUERRERO MEDINANo ratings yet
- Dengue Fever: AssignmentDocument14 pagesDengue Fever: AssignmentRenx KhanNo ratings yet
- 44 RevDocument14 pages44 RevAsshiddiqie ColectionNo ratings yet
- Dengue Infection in Children in Ratchaburi, Thailand: A Cohort Study. II. Clinical ManifestationsDocument11 pagesDengue Infection in Children in Ratchaburi, Thailand: A Cohort Study. II. Clinical ManifestationsMey KhNo ratings yet
- Dengue Management in Triage Using Ultrasound in CHDocument11 pagesDengue Management in Triage Using Ultrasound in CHYuning tyas Nursyah FitriNo ratings yet
- Anak Bu HeniDocument10 pagesAnak Bu HeniVeronika IntanNo ratings yet
- Journal PNTD 0001244Document10 pagesJournal PNTD 0001244Zulia Ahmad BurhaniNo ratings yet
- Sciencedirect: Hong-Jie Kuo, Ing-Kit Lee, Jien-Wei LiuDocument9 pagesSciencedirect: Hong-Jie Kuo, Ing-Kit Lee, Jien-Wei LiuzihanNo ratings yet
- Dengue Hemorrhagic Fever e A Systemic Literature Review of Current Perspectives On Pathogenesis, Prevention and ControlDocument16 pagesDengue Hemorrhagic Fever e A Systemic Literature Review of Current Perspectives On Pathogenesis, Prevention and ControlMichael Jansen SulaimanNo ratings yet
- The Rise of Imported Dengue Infections in Victoria, Australia, 2010-2016Document11 pagesThe Rise of Imported Dengue Infections in Victoria, Australia, 2010-2016Satriya WibawaNo ratings yet
- Journal Pone 0138465Document16 pagesJournal Pone 0138465Indra IhsanNo ratings yet
- Dengue in Pregnancy: AbstractDocument3 pagesDengue in Pregnancy: AbstractsharenNo ratings yet
- Jurnal 1Document8 pagesJurnal 1aziskarnNo ratings yet
- Nguyen Minh Tuan 2013Document8 pagesNguyen Minh Tuan 2013libremdNo ratings yet
- DENGUE HEMORRHAGIC FEVER-final N ToDocument52 pagesDENGUE HEMORRHAGIC FEVER-final N ToRachel Ann CorpuzNo ratings yet
- Usg For DBDDocument5 pagesUsg For DBDhappy gummyNo ratings yet
- 1 s2.0 S2667100X23000567 MainDocument18 pages1 s2.0 S2667100X23000567 MainEnrique CastelanNo ratings yet
- Difyeri IndiaDocument5 pagesDifyeri IndiaDian Fajar FebrianiNo ratings yet
- Diagnosis and Treatment of Chronic CoughFrom EverandDiagnosis and Treatment of Chronic CoughSang Heon ChoNo ratings yet
- Infectious Diseases in the Intensive Care UnitFrom EverandInfectious Diseases in the Intensive Care UnitManish SonejaNo ratings yet
- Burn-Like Skin Necrosis in A Patient Following Infusion of Sodium BicarbonateDocument3 pagesBurn-Like Skin Necrosis in A Patient Following Infusion of Sodium BicarbonateViniFortunataNo ratings yet
- Dengue LancetDocument16 pagesDengue LancetJorge Ricardo Uchuya GómezNo ratings yet
- Snake Bite ManagementDocument92 pagesSnake Bite ManagementManoharNo ratings yet
- 2nd Webinar HighlightDocument5 pages2nd Webinar HighlightYS NateNo ratings yet
- Dengue Management Guideline 2020, Training Materials Top SheetDocument257 pagesDengue Management Guideline 2020, Training Materials Top Sheetdeepak das100% (1)
- Dengue Fever by LubnaDocument47 pagesDengue Fever by LubnaDr AnilNo ratings yet
- Materi DR Martin PDFDocument93 pagesMateri DR Martin PDFFajar Agustian Combachie Part IINo ratings yet
- DengueDocument70 pagesDengueVijay ArumugamNo ratings yet
- Dengue Guidelines For Electronic Circulation - CompressedDocument73 pagesDengue Guidelines For Electronic Circulation - CompressedakeelNo ratings yet
- Dengue Virus Infection - Prevention and Treatment - UpToDateDocument32 pagesDengue Virus Infection - Prevention and Treatment - UpToDateAnderson SilvaNo ratings yet
- Idiopathic Systemic Capillary Leak Syndrome - UpToDateDocument17 pagesIdiopathic Systemic Capillary Leak Syndrome - UpToDatenikos papamakariosNo ratings yet
- Revised National Guideline For Clinical Management of Dengue Syndrome 2018Document112 pagesRevised National Guideline For Clinical Management of Dengue Syndrome 2018rony ghoshNo ratings yet
- DengueDocument45 pagesDengueRachel AlbertNo ratings yet
- Revised Dengue Guideline 2020 PDFDocument98 pagesRevised Dengue Guideline 2020 PDFAbid Hasan ZiKonNo ratings yet
- Dengue 2Document56 pagesDengue 2Eliz Codilla-SyNo ratings yet
- Dengue Feve1Document10 pagesDengue Feve1Santhosh KumarNo ratings yet
- Disseminated Intravascular Coagulation Initial Score As A Predictor ofDocument6 pagesDisseminated Intravascular Coagulation Initial Score As A Predictor ofPriska ForceveeanaNo ratings yet
- History Taking For FeverDocument13 pagesHistory Taking For FeverAfiQsyazwan Abd RaniNo ratings yet
- Manajemen Cairan Pada Luka BakarDocument38 pagesManajemen Cairan Pada Luka Bakarwati suwartaNo ratings yet
- Dengue (Lancet)Document16 pagesDengue (Lancet)Roberth Mero100% (1)
- Dengue 2019Document79 pagesDengue 2019Nou ChannarithNo ratings yet
- National Guidelines On Clinical Management of Dengue Infection in Pregnancy Reprint Version - New PDFDocument78 pagesNational Guidelines On Clinical Management of Dengue Infection in Pregnancy Reprint Version - New PDFsarakg vathNo ratings yet
- Hyperferritinemia in Severe Dengue Infection .13Document8 pagesHyperferritinemia in Severe Dengue Infection .13rsthsn6z8xNo ratings yet