Professional Documents
Culture Documents
Lead 4
Lead 4
Uploaded by
afamhbkOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Lead 4
Lead 4
Uploaded by
afamhbkCopyright:
Available Formats
Emerging Treatments and Technologies
O R I G I N A L A R T I C L E
Efficacy and Safety of the Human
Glucagon-Like Peptide-1 Analog
Liraglutide in Combination With Metformin
and Thiazolidinedione in Patients With
T ype 2 Diabetes (LEAD-4 MetⴙTZD)
T
BERNARD ZINMAN, MD1 PHILIP RASKIN, MD6 ype 2 diabetes is characterized by
JOHN GERICH, MD2 PAULA M. HALE, PHD7 insulin resistance and progressive
JOHN B. BUSE, MD, PHD3 MILAN ZDRAVKOVIC, PHD7 -cell failure. Treatment often must
ANDREW LEWIN, MD4 LAWRENCE BLONDE, MD8 be intensified over time, usually by a com-
Downloaded from http://diabetesjournals.org/care/article-pdf/32/7/1224/605411/zdc00709001224.pdf by guest on 03 October 2022
SHERWYN SCHWARTZ, MD5 THE LEAD-4 STUDY INVESTIGATORS*
bination of agents that address both insu-
lin resistance and -cell dysfunction
(1,2). However, several available thera-
OBJECTIVE — To determine the efficacy and safety of liraglutide (a glucagon-like peptide-1 pies increase the risk for hypoglycemia
receptor agonist) when added to metformin and rosiglitazone in type 2 diabetes. and weight gain, which may reduce pa-
RESEARCH DESIGN AND METHODS — This 26-week, double-blind, placebo- tient adherence and lead to poor glycemic
controlled, parallel-group trial randomized 533 subjects (1:1:1) to once-daily liraglutide (1.2 or control (3).
1.8 mg) or liraglutide placebo in combination with metformin (1 g twice daily) and rosiglitazone Glucagon-like peptide-1 (GLP-1) stim-
(4 mg twice daily). Subjects had type 2 diabetes, A1C 7–11% (previous oral antidiabetes drug ulates insulin secretion and suppression of
[OAD] monotherapy ⱖ3 months) or 7–10% (previous OAD combination therapy ⱖ3 months), glucagon secretion in a glucose-dependent
and BMI ⱕ45 kg/m2. manner, delays gastric emptying, and de-
creases appetite (4). GLP-1 is rapidly de-
RESULTS — Mean A1C values decreased significantly more in the liraglutide groups versus graded by dipeptidyl peptidase-4 (4).
placebo (mean ⫾ SE ⫺1.5 ⫾ 0.1% for both 1.2 and 1.8 mg liraglutide and ⫺0.5 ⫾ 0.1% for
placebo). Fasting plasma glucose decreased by 40, 44, and 8 mg/dl for 1.2 and 1.8 mg and
Liraglutide is a human GLP-1 analog with
placebo, respectively, and 90-min postprandial glucose decreased by 47, 49, and 14 mg/dl, 97% homology to native GLP-1 (5). Lira-
respectively (P ⬍ 0.001 for all liraglutide groups vs. placebo). Dose-dependent weight loss glutide has a half-life in humans of 13 h
occurred with 1.2 and 1.8 mg liraglutide (1.0 ⫾ 0.3 and 2.0 ⫾ 0.3 kg, respectively) (P ⬍ 0.0001) compared with 1–2 min for native GLP-1,
compared with weight gain with placebo (0.6 ⫾ 0.3 kg). Systolic blood pressure decreased by making liraglutide suitable as a once-daily
6.7, 5.6, and 1.1 mmHg with 1.2 and 1.8 mg liraglutide and placebo, respectively. Significant treatment for patients with type 2 diabetes
increases in C-peptide and homeostasis model assessment of -cell function and significant (6).
decreases in the proinsulin-to-insulin ratio occurred with liraglutide versus placebo. Minor In previously published phase 3 trials
hypoglycemia occurred more frequently with liraglutide, but there was no major hypoglycemia.
Gastrointestinal adverse events were more common with liraglutide, but most occurred early and
(the Liraglutide Effect and Action in Dia-
were transient. betes [LEAD] Program), treatment with
liraglutide produced substantial and clin-
CONCLUSIONS — Liraglutide combined with metformin and a thiazolidinedione is a well- ically significant reductions in A1C and
tolerated combination therapy for type 2 diabetes, providing significant improvements in gly- fasting and postprandial glucose (PPG)
cemic control. levels, with a low risk of hypoglycemia,
and moderate weight loss (7–10). Lira-
Diabetes Care 32:1224–1230, 2009 glutide treatment alone or in combination
with oral antidiabetes drugs (OADs) dem-
● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● onstrated significantly larger A1C re-
From the 1Samuel Lunenfeld Research Institute, Mount Sinai Hospital, Toronto, Ontario, Canada; the ductions compared with glimepiride
2
Department of Medicine, University of Rochester, Rochester, New York; the 3University of North Caro- (monotherapy) (7), rosiglitazone (in com-
lina, Chapel Hill, North Carolina; the 4National Research Institute, Los Angeles, California; the 5Diabetes bination with a sulfonylurea) (8), and in-
and Glandular Disease Center, San Antonio, Texas; the 6Department of Medicine, University of Texas, sulin glargine (in combination with
Dallas, Texas; 7Novo Nordisk, Copenhagen, Denmark; and the 8Ochsner Institute, New Orleans,
Louisiana. metformin and sulfonylurea) (10). When
Corresponding author: Bernard Zinman, zinman@lunenfeld.ca. initiated as monotherapy in a subgroup of
Received 8 December 2008 and accepted 8 March 2009. previously treatment-naïve patients with
Published ahead of print at http://care.diabetesjournals.org on 16 March 2009. DOI: 10.2337/dc08-2124. type 2 diabetes, a mean A1C reduction of
Clinical trial reg. no. NCT00333151, clinicaltrials.gov.
*A full list of the LEAD-4 Study Investigators is available in an online appendix at http://dx.doi. 1.6% was observed, with mean A1C val-
org/10.2337/dc08-2124. ues sustained below 7.0% over 52 weeks
© 2009 by the American Diabetes Association. Readers may use this article as long as the work is properly (7). In combination with metformin, lira-
cited, the use is educational and not for profit, and the work is not altered. See http://creativecommons. glutide reduced body weight by 2–3 kg,
org/licenses/by-nc-nd/3.0/ for details.
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby with the majority of the weight loss being
marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact. fat (11). In addition, a decrease in systolic
1224 DIABETES CARE, VOLUME 32, NUMBER 7, JULY 2009 care.diabetesjournals.org
Zinman and Associates
blood pressure (SBP) has been previously at the evening meal). Rosiglitazone was and subject-reported hypoglycemic epi-
demonstrated (7–10). No major hypo- started at 4 mg in the morning and in- sodes (plasma glucose ⬍56 mg/dl
glycemic events occurred during the ran- creased to 8 mg/day (4 mg in the morning [⬍3.1mmol/l]). A serious adverse event
domized treatment period when lira- and evening, the highest approved dose in was defined as an adverse event that re-
glutide was used as monotherapy or with the U.S. and Canada). Subjects who tol- sulted in death, hospitalization, disability,
metformin (7,9). The current study in- erated the final OAD doses and had fast- or a birth defect; was life threatening; or
vestigated liraglutide treatment in com- ing plasma glucose (FPG) values 135–230 required medical or surgical intervention
bination with metformin and a thiazo- mg/dl (7.5–12.8 mmol/l) after 6 weeks’ to prevent one of the other outcomes. Mi-
lidinedione (TZD) (rosiglitazone) as part treatment at the titrated doses were eligi- nor hypoglycemic episodes were defined
of the LEAD program. These three ble for randomization. At randomization, as those that could be self-treated; major
glucose-lowering agents are of particu- subjects initiated liraglutide or placebo episodes were defined as requiring third-
lar interest, as they have complementary treatment with 100-l injections corre- party assistance or medical intervention.
modes of action and are not generally sponding to a 0.6-mg dose and increased Nausea was patient reported.
associated with increased risk of to 1.2 mg/day (200 l injections) after 1
hypoglycemia. week and then to 1.8 mg/day (300 l in- Statistical analysis
jections) after an additional week for The analysis of efficacy end points was
Downloaded from http://diabetesjournals.org/care/article-pdf/32/7/1224/605411/zdc00709001224.pdf by guest on 03 October 2022
RESEARCH DESIGN AND those randomized to the highest dose. Li- based on the intent-to-treat population,
METHODS — Subjects with type 2 di- raglutide (active or placebo) was injected defined as subjects who were exposed to
abetes were screened and enrolled if they subcutaneously once daily at any time of at least one dose of trial product and had
were aged 18 – 80 years, had A1C be- the day in the upper arm, abdomen, or one postbaseline measurement of the pa-
tween 7 and 11% (prestudy OAD mono- thigh using a prefilled pen device. Sub- rameter. Each end point was analyzed us-
therapy for ⱖ3 months) or 7–10% jects were encouraged to use liraglutide ing an ANCOVA model with treatment,
(prestudy combination OAD therapy for during the same overall time period. The country, and previous antidiabetes treat-
ⱖ3 months), and had BMI ⱕ45 kg/m2. titration period was followed by a 24- ment as fixed effects and baseline as the
Subjects who used insulin during the pre- week maintenance period during which covariate. Missing data were imputed as
vious 3 months (except short-term treat- the doses of study drugs were to be the last observation carried forward. Sam-
ment) were excluded. The protocol was maintained. ple size calculations were based on show-
approved by local institutional review The primary outcome measure was ing A1C and body weight differences of
boards, and subjects provided written in- change in A1C from randomization to the 0.5 and 3%, respectively. The combined
formed consent before the initiation of end of the study. Secondary end points power (calculated as the product of the
any trial-related activities. The study was included changes in body weight; FPG; marginal powers for A1C and weight) was
conducted in accordance with the Decla- seven-point plasma glucose profiles; ⬎95%.
ration of Helsinki and Good Clinical Prac- -cell function based on fasting insulin, Superiority of glycemic control with
tice Guidelines (12). fasting C-peptide, and fasting proinsulin- liraglutide versus comparators was con-
This 26-week, double-blind, random- to-insulin ratio; the homeostasis model cluded if the upper limit of the two-sided
ized, placebo-control, parallel-group, mul- assessment (HOMA) for -cell function 95% CI for the treatment difference in
ticenter (96 sites), two-country (U.S. and (HOMA-B) and insulin resistance change in A1C was ⬍0%; equivalence
Canada) trial randomized subjects (1:1:1) (HOMA-IR) (13); and lipids. Laboratory was also tested. The proportion of sub-
to receive 1.2 or 1.8 mg of once-daily li- analyses were performed by a central lab- jects achieving A1C targets (American Di-
raglutide (Novo Nordisk, Bagsværd, Den- oratory (MDS Pharma Services in Canada abetes Association [ADA] target: ⬍7%;
mark) or liraglutide placebo (Novo and Switzerland). A1C was assayed by a American Association of Clinical Endocri-
Nordisk) injected subcutaneously by method certified by the National Glyco- nologists [AACE]/International Diabetes
subjects in combination with metformin hemoglobin Standardization Program. Federation [IDF] target: ⱕ6.5%) was
and rosiglitazone in all three treatment Subjects were provided with MediSense compared between treatments using a lo-
groups. Precision Xtra/MediSense Optium glu- gistic regression model with treatment
Randomization was carried out using cose meters (Abbott Laboratories, Abbott and baseline A1C as covariates. CIs for
a telephone- or Web-based randomiza- Park, IL) calibrated to plasma glucose to secondary end points were corrected us-
tion system. Before randomization, eligi- determine self-measured plasma glucose ing Dunnett’s test. Hypoglycemic epi-
ble subjects underwent a 6- to 9-week (SMPG) and were asked to record values sodes were analyzed using a general linear
metformin and rosiglitazone run-in and in their diaries. The seven-point SMPG model including treatment as a fixed ef-
dose-titration period. Prior treatment profile measurements were performed fect. The significance level was set at P ⬍
with OADs other than metformin and before and 90 min after meals and at bed- 0.05.
rosiglitazone were discontinued. Subjects time for 2 consecutive days at weeks 0
previously treated with pioglitazone un- (randomization), 12, and 26. Serum insu- RESULTS — A total of 821 subjects
derwent rosiglitazone titration (by trans- lin and C-peptide values were determined were enrolled in the study; 533 subjects
ferring to the corresponding rosiglitazone using a chemiluminescence immunoassay, were randomly assigned to liraglutide or
dose) or went directly to the maximum and proinsulin was measured in serum us- placebo treatment after the metformin
dose if they were on the maximum piogli- ing an enzyme-linked immunosorbent plus rosiglitazone run-in period (288
tazone dose. Metformin was started at assay. subjects were run-in failures due to FPG
500 mg at breakfast and increased weekly Safety variables included adverse values out of range [135–230 mg/dl; 7.5–
by increments of 500 mg to a final dose of events, vital signs, electrocardiogram, 12.8 mmol/l] or other reasons). Three
2,000 mg/day (1,000 mg at breakfast and biochemical and hematology measures, subjects were randomized but were with-
care.diabetesjournals.org DIABETES CARE, VOLUME 32, NUMBER 7, JULY 2009 1225
LEAD-4 study
Table 1—Characteristics of randomized population and subject disposition
1.2 mg Liraglutide 1.8 mg Liraglutide Placebo
Sex (%) (men/women) 57/43 51/49 62/38
Age (years) 55 ⫾ 10 55 ⫾ 11 55 ⫾ 10
Race (%) (C/B/A/I/O) 81/15/1/1/2 83/10/3/1/3 84/10/2/1/3
Ethnicity (Hispanic or Latino/not) 13/87 16/84 16/84
BMI (kg/m2) 33.2 ⫾ 5.4 33.5 ⫾ 5.1 33.9 ⫾ 5.2
Duration of diabetes (years) 9⫾6 9⫾6 9⫾6
Prestudy OAD treatment
Monotherapy 29 (16) 29 (16) 32 (18)
Combination therapy 149 (84) 149 (84) 145 (82)
A1C (%) 8.5 ⫾ 1.2 8.6 ⫾ 1.2 8.4 ⫾ 1.2
FPG 关mg/dl (mmol/l)兴 182 ⫾ 43 (10.1 ⫾ 2.4) 185 ⫾ 43 (10.3 ⫾ 2.4) 180 ⫾ 47 (10.0 ⫾ 2.6)
SBP (mmHg) 129 ⫾ 14.8 126 ⫾ 14.2 128 ⫾ 14.5
Downloaded from http://diabetesjournals.org/care/article-pdf/32/7/1224/605411/zdc00709001224.pdf by guest on 03 October 2022
DBP (mmHg) 75.8 ⫾ 9.0 75.2 ⫾ 8.4 76.2 ⫾ 9.2
Total cholesterol (mmol/l) 5.01 ⫾ 1.33 5.17 ⫾ 1.43 4.99 ⫾ 1.34
LDL cholesterol (mmol/l) 2.82 ⫾ 0.95 2.96 ⫾ 1.08 2.77 ⫾ 0.95
VLDL cholesterol (mmol/l) 0.74 ⫾ 0.38 0.76 ⫾ 0.38 0.71 ⫾ 0.36
HDL cholesterol (mmol/l) 1.26 ⫾ 0.32 1.27 ⫾ 0.31 1.25 ⫾ 0.28
Triglycerides (mmol/l) 2.41 ⫾ 2.24 2.39 ⫾ 1.88 2.74 ⫾ 2.80
Free fatty acids (mmol/l) 0.51 ⫾ 0.22 0.55 ⫾ 0.27 0.52 ⫾ 0.34
Randomized 178 178 177
Completers 153 (86) 133 (75) 121 (68)
Withdrawals 25 (14) 45 (25) 56 (32)
Adverse events* 11 (6) 27 (15) 6 (3)
Nausea/vomiting/diarrhea 5 (3) 19 (11) 0
Ineffective therapy 3 (2) 3 (2) 29 (16)
Noncompliance 4 (2) 4 (2) 5 (3)
Other 7 (4) 11 (6) 16 (9)
Data are means ⫾ SD or n (%) unless otherwise indicated. *The adverse events row includes nausea/vomiting/diarrhea. A, Asian; B, black; C, Caucasian; I, American
Indian; O, other.
drawn before receiving the study drug. groups achieved the ADA and AACE/IDF crease observed in the placebo group (⫺8
Baseline characteristics were balanced A1C goals compared with placebo (P ⬍ mg/dl [⫺0.4 mmol/l], P ⬍ 0.0001).
across treatment groups (Table 1). The 0.0001 for all comparisons of liraglutide Mean 90-min PPG (mean of three
majority (83%) of the randomized sub- to placebo for both A1C goals) (Fig. 1B). meals), from self-monitored seven-point
jects were treated with two or more OADs At the end of the study, 57.5 and 53.7% of plasma glucose measurements at the end
before the study. subjects in the 1.2 and 1.8 mg liraglutide/ of the study, decreased from baseline in
day groups, respectively, had an A1C all treatment groups by ⫺47 mg/dl (2.6
Efficacy ⬍7%, compared with 28.1% in the pla- mmol/l) for 1.2 mg liraglutide/day, ⫺49
At the end of the study, the mean A1C cebo group, with 37.3 and 36.2%, respec- mg/dl (2.7 mmol/l) for 1.8 mg liraglutide/
values for the overall population de- tively, reaching ⱕ6.5% compared with day, and ⫺14 mg/dl (0.8 mmol/l) for pla-
creased by (means ⫾ SE) 1.5 ⫾ 0.1% for 14.4% with placebo. cebo (P ⬍ 0.001 comparisons of all
both 1.2 and 1.8 mg/day liraglutide FPG values decreased within 2 weeks liraglutide groups to placebo). The post-
groups and 0.5 ⫾ 0.1% for the placebo prandial increment (postmeal value mi-
of randomization with liraglutide, re-
group. Liraglutide-treated subjects had nus premeal) was significantly reduced
maining relatively stable thereafter, while
superior glycemic control compared with over breakfast with liraglutide treatment
those in the placebo group (liraglutide 1.2 with placebo, smaller decreases occurred (⫺16, ⫺14, and ⫺5 mg/dl [⫺0.9, ⫺0.8,
mg/day vs. placebo: ⫺0.9% [95% CI (Fig. 1C). End-of-study FPG values were ⫺0.3 mmol/l], respectively; P ⬍ 0.05 for
⫺1.1 to ⫺0.8] and liraglutide 1.8 mg/day 139 ⫾ 49 mg/dl (7.7 ⫾ 2.7 mmol/l), both liraglutide treatment groups vs. pla-
vs. placebo: ⫺1.1% [⫺1.1 to ⫺0.8]). 137 ⫾ 41 mg/dl (7.6 ⫾ 2.3 mmol/l), and cebo) but not for lunch and dinner.
Within the first 12 weeks of the study, 171 ⫾ 54 mg/dl (9.5 ⫾ 3.0 mmol/l) in the Mean change in body weight over
mean A1C values decreased from baseline 1.2 and 1.8 mg liraglutide/day and pla- time is shown in Fig. 1D. Weight loss was
for the liraglutide-treated groups and cebo groups, respectively. The decreases observed in the liraglutide-treated groups
thereafter remained steady throughout in FPG from baseline for the liraglutide ([means ⫾ SE] 1.0 ⫾ 0.3 and 2.0 ⫾ 0.3 kg
the trial (Fig. 1A). groups (⫺40 mg/dl [⫺2.2 mmol/l] and from baseline for 1.2 and 1.8 mg lira-
A logistic regression analysis demon- ⫺44 mg/dl [⫺2.4 mmol/l] for 1.2 and 1.8 glutide/day groups, respectively) and was
strated that a significantly greater percent- mg liraglutide/day groups, respectively) significantly different (P ⬍ 0.0001) from
age of subjects in both of the liraglutide were significantly greater than the de- the weight gain in the placebo group
1226 DIABETES CARE, VOLUME 32, NUMBER 7, JULY 2009 care.diabetesjournals.org
Zinman and Associates
Downloaded from http://diabetesjournals.org/care/article-pdf/32/7/1224/605411/zdc00709001224.pdf by guest on 03 October 2022
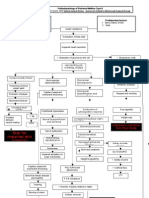
Figure 1—A: A1C over time for the study population. B: Percentage of subjects achieving ADA and AACE/IDF A1C goals at the end of the study. C:
FPG values over time. D: Change in body weight over time. E: SBP over time. F: Percentage of subjects with nausea by week. Data are intent to treat,
last observation carried forward for all postbaseline values, with the exception of F, which is data from the safety analysis set. Error bars shown in
A, C, D, and E are 2 ⫻ SE. **P ⫽ 0.0009; ***P ⬍ 0.0001.
(0.6 ⫾ 0.3 kg). The weight loss in the 1.8 treatment groups in diastolic blood pres- LDL cholesterol and triglycerides de-
mg liraglutide/day group was signifi- sure (DBP). Minor, but statistically signif- creased significantly more in the 1.2 mg
cantly greater than the 1.2 mg liraglutide/ icant, increases in pulse rate were liraglutide group than in the placebo
day group (P ⫽ 0.011). observed in the liraglutide-treated groups group.
The 1.2 and 1.8 mg liraglutide/day versus placebo (2 and 3 bpm for 1.2 mg The decreases in the proinsulin-to-
groups had significant reductions in mean (P ⫽ 0.0071) and 1.8 mg liraglutide (P ⫽ insulin ratio from baseline (baseline of 0.4
SBP compared with the placebo group 0.0001), respectively) with a decrease of across all groups) for the liraglutide
(Table 2) (Fig. 1E) (placebo-corrected dif- 0.5 bpm for placebo. Changes in lipids groups were significant (P ⬍ 0.05) com-
ference: 1.2 mg liraglutide/day: ⫺5.6 from baseline are presented in Table 2 pared with the placebo group, which in-
mmHg, P ⬍ 0.0001; 1.8 mg liraglutide/ showing that free fatty acid values de- creased from baseline (Table 2). The
day: ⫺4.5mmHg, P ⫽ 0.0009). There creased with liraglutide treatment as com- increase in C-peptide was significantly
were no significant differences between pared with an increase with placebo, and greater in the liraglutide groups (131 and
care.diabetesjournals.org DIABETES CARE, VOLUME 32, NUMBER 7, JULY 2009 1227
LEAD-4 study
Table 2—Other end points of interest/metabolic intermediates change from baseline to end of study
Liraglutide 1.2 mg Liraglutide 1.8 mg Placebo
Blood pressure (mmHg)
SBP ⫺6.7 ⫾ 1.1* ⫺5.6 ⫾ 1.1* ⫺1.1 ⫾ 1.2
DBP ⫺2.3 ⫾ 0.7 ⫺1.9 ⫾ 0.7 ⫺0.8 ⫾ 0.7
-Cell function
Insulin (pmol/l) 6.0 ⫾ 5.8 5.6 ⫾ 5.5 6.8 ⫾ 6.0
C-peptide (pmol/l) 131 ⫾ 32* 144 ⫾ 31* 51 ⫾ 34
Proinsulin-to-insulin ratio ⫺0.029 ⫾ 0.026* ⫺0.085 ⫾ 0.26* 0.036 ⫾ 0.029
-Cell function (%) (HOMA-B) 27 ⫾ 4.4* 27 ⫾ 4.2* 6 ⫾ 4.5
Insulin resistance (HOMA-IR) ⫺0.6 ⫾ 0.3 ⫺0.7 ⫾ 0.3 ⫺0.3 ⫾ 0.3
Proinsulin–to–C-peptide ratio ⫺0.007 ⫾ 0.001* ⫺0.008 ⫾ 0.001* ⫺0.002 ⫾ 0.001
Fasting glucagon (pg/ml) ⫺5.9 ⫾ 2.9 ⫺6.7 ⫾ 2.8 ⫺0.4 ⫾ 3.0
Lipids
Downloaded from http://diabetesjournals.org/care/article-pdf/32/7/1224/605411/zdc00709001224.pdf by guest on 03 October 2022
Total cholesterol (mmol/l) ⫺0.21 ⫾ 0.9 ⫺0.20 ⫾ 0.09 ⫺0.02 ⫾ 0.10
LDL cholesterol (mmol/l) ⫺0.28 ⫾ 0.07* ⫺0.23 ⫾ 0.07 ⫺0.10 ⫾ 0.07
VLDL cholesterol (mmol/l) 0.12 ⫾ 0.03 0.10 ⫾ 0.03 0.11 ⫾ 0.03
HDL cholesterol (mmol/l) ⫺0.03 ⫾ 0.02 ⫺0.04 ⫾ 0.02 ⫺0.03 ⫾ 0.02
Triglycerides (mmol/l) ⫺0.38 ⫾ 0.10* ⫺0.32 ⫾ 0.10 ⫺0.13 ⫾ 0.11
Free fatty acids (mmol/l) ⫺0.03 ⫾ 0.02* ⫺0.05 ⫾ 0.02* 0.02 ⫾ 0.02
Data are means ⫾ SE, unless otherwise noted. *P ⬍ 0.05 vs. placebo.
144 pmol/l for 1.2 and 1.8 mg liraglutide, 65 events in weeks 4 –26) (Fig. 1F). Dur- treatment differences were observed in
respectively) compared with an increase ing the first 8 weeks of treatment, 71– physical examination findings, laboratory
of 51 pmol/l for placebo (P ⬍ 0.05 for 84% of subjects in the liraglutide groups analyses (hematology and biochemistry
comparison of both liraglutide groups to and 98% of subjects in the placebo group analyses), electrocardiogram, or ophthal-
placebo). Both liraglutide treatment reported ⱕ7 days of nausea. Peripheral moscopy. There was no significant treat-
groups had significant improvements (in- edema was reported by 5.1, 1.7, and 8.0% ment effect with 1.8 mg liraglutide versus
crease of 27 absolute percentage points) in the 1.2 mg liraglutide, 1.8 mg lira- placebo on calcitonin. Geometric mean–
in HOMA-B for both groups from base- glutide, and placebo groups, respectively. estimated repeated-measurement analy-
line values of 34 to 37%, respectively, The percentages of subjects with- sis showed calcitonin levels of 0.89, 0.83,
compared with an improvement in the pla- drawn because of adverse events were and 0.75 ng/l for 1.2 mg liraglutide, 1.8
cebo group of 6 absolute percentage points greater in the liraglutide groups than in mg liraglutide, and placebo, respectively,
from a baseline of 40% (P ⬍ 0.0001 for the placebo group (Table 1). Nausea, at the end of the study (all values within
both groups vs. placebo). Insulin resistance vomiting, and/or diarrhea were the gas- the normal range). There was a significant
(measured by HOMA-IR) was reduced in all trointestinal events that lead to the with- increase for the 1.2 mg liraglutide group
three treatment groups but was not signifi- drawal of five subjects treated with 1.2 mg versus placebo group (P ⫽ 0.022) but no
cantly different between groups. No signif- liraglutide and 19 subjects treated with significant difference with the 1.8 mg li-
icant differences in the change-from- 1.8 mg liraglutide (Table 1). Most gastro- raglutide group. No difference in cardio-
baseline of HOMA-IR and fasting insulin intestinal adverse events resulting in vascular adverse events was reported
and glucagon values were observed be- withdrawal occurred during the first between the liraglutide groups and pla-
tween either of the liraglutide groups versus month of therapy. There were no episodes cebo (five events [five subjects] with lira-
the placebo group (Table 2). of pancreatitis, and no deaths occurred. glutide 1.2, three events [three subjects]
Serious adverse events were infrequent (8 with liraglutide 1.8, and four events [four
Safety subjects [8 total events] for 1.2 mg lira- subjects] with placebo). There were 4.1
Gastrointestinal disorders (including glutide, 7 subjects [10 events] for 1.8 mg and 6.7% of subjects treated with 1.2 and
nausea, vomiting, and diarrhea) were the liraglutide, and 12 subjects [13 events] for 1.8 mg liraglutide and positive for lira-
most frequently reported adverse events placebo). glutide antibodies at the end of the study
in the liraglutide groups and were re- Minor hypoglycemia occurred at low (versus none with placebo). Subjects with
ported by 45, 56, and 19% of the subjects incidence (9.0, 7.9, and 5.1% of subjects) antibodies did not have an attenuated
in the 1.2 and 1.8 mg liraglutide and pla- resulting in a low rate of reported minor A1C response.
cebo groups, respectively. One episode or hypoglycemia (0.4. 0.6, and 0.2 events
more of nausea was experienced by 29 per year) for the 1.2 mg liraglutide, 1.8 mg CONCLUSIONS — Liraglutide ther-
and 40% in the 1.2 and 1.8 mg liraglutide liraglutide, and placebo groups, respec- apy in combination with metformin and
groups, respectively, and vomiting was tively. The rate of minor hypoglycemia for TZD provided significant decreases in
experienced by 7 and 17%, respectively. the 1.8 mg liraglutide group was signifi- A1C, FPG, and PPG with weight loss; de-
The majority of nausea was transient, as it cantly higher than placebo (P ⫽ 0.004). No creases in SBP; and a low rate of minor
occurred in the first 4 weeks of liraglutide major hypoglycemic event was reported. hypoglycemia. In addition, there were in-
treatment (216 events in weeks 1– 4 vs. No clinically relevant between- dications of improvement in -cell func-
1228 DIABETES CARE, VOLUME 32, NUMBER 7, JULY 2009 care.diabetesjournals.org
Zinman and Associates
tion with liraglutide treatment compared weight decreased by 1.75 kg (vs. 0.24 kg Squibb, Calpis, Conjuchem, Daiichi Sankyo, De-
with placebo. While improvement in in the placebo group; P ⬍ 0.001), and poMed, Eli Lilly & Company, Elixir Pharmaceu-
-cell function may have been a conse- other measurements of glycemic control ticals, Essentialis, Forest Laboratories/Forest
quence of improved glucose control, it (FPG, mean SMPG, and mean postpran- Research Institute, Generex Pharmaceuticals,
GlaxoSmithKline, Hollis-Eden, Hoffmann-La
could well be a direct effect of liraglutide, dial SMPG values) all showed significant Roche, Incyte, InteKrin Therapeutics, Johnson
which is known to stimulate glucose- improvement with exenatide treatment. & Johnson, King Pharmaceuticals, Kowa Re-
dependent endogenous insulin secretion. These studies support the effectiveness of search Institute, Lilly ICOS, Merck & Com-
Gastrointestinal adverse events were re- this type of diabetes regimen, particularly pany, Metabasis, Metabolic Solutions,
ported more frequently with liraglutide as it is associated with modest weight loss Microbia, Novartis Pharmaceuticals, Novo Nor-
treatment, with most of the events occur- and low risk of hypoglycemia. disk, Pfizer, Pharmacopeia, Regeneron Pharma-
ring early in treatment. The glucose- The very significant change in SBP ceuticals, Reliant Pharmaceuticals, Sankyo
lowering effects of the two doses of observed in this study appears to be of Pharma Development/Sankyo USA, sanofi-
liraglutide were similar, although there larger magnitude than that observed in aventis, Schering-Plough, Sepracor, Takeda
were significantly more gastrointestinal the other LEAD studies. TZD treatment is Pharmaceuticals America, TAP Holdings, Tran-
sition Therapeutics, Tularik, VIVUS, and
adverse events with the higher dose. associated with a modest reduction in Wyeth-Ayerst. P.R. has attended advisory boards
However, it is likely that there is signifi- blood pressure but is also associated with
Downloaded from http://diabetesjournals.org/care/article-pdf/32/7/1224/605411/zdc00709001224.pdf by guest on 03 October 2022
for Novo Nordisk. P.H. and M.Z. are both em-
cant individual variation in the develop- fluid retention. There may be an interac- ployees of Novo Nordisk. L.B. has acted as an
ment of nausea and glycemic tion between the cardiovascular effects of investigator for Amylin Pharmaceuticals, Astra-
effectiveness. liraglutide and TZD. Further study would Zeneca, Boehringer-Ingelheim Pharmaceutical,
The underlying pathophysiology of be of obvious interest, particularly if there Bristol-Myers Squibb, Eli Lilly and Company,
type 2 diabetes is complex and involves was potential for long-term cardiovascu- MannKind Corporation, Merck & Company,
three main factors: a relative decrease in lar benefit. Novo Nordisk, Novartis, Pfizer, and sanofi-
-cell insulin secretory function; in- The specific mechanism(s) of SBP re- aventis; has been a speaker for Abbott, Amylin
creased glucose production by the liver, Pharmaceuticals, AstraZeneca, Bristol-Myers
duction and the slight increases in pulse
Squibb, Daiichi Sankyo, Eli Lilly & Company,
which is at least partially mediated by in- with liraglutide remain to be further stud- GlaxoSmithKline, LifeScan, Merck & Company,
appropriately increased glucagon levels; ied. Based on data with native GLP-1, it Novartis, Novo Nordisk, Pfizer, and sanofi-
and decreased glucose uptake by muscle. could be speculated that the effect on SBP aventis; and has acted as consultant for Boehr-
The triple therapy of metformin, TZD, relates to reduced renal sodium reabsorp- inger-Ingelheim Pharmaceutical and
and GLP-1 receptor agonists has the po- tion (16,17). Native GLP-1 has been Hazlozyme. No other potential conflicts of inter-
tential of addressing all three underlying shown to improve endothelial function in est relevant to this article were reported.
abnormalities and results in improved patients with type 2 diabetes and coronary The authors acknowledge the assistance of
glycemic control, potential weight loss, heart disease (18) and in vitro endothelial the LEAD-4 Met⫹TZD Study Group, their
and improvements in -cell function with cell models (19). The latter has also been staff, clinical trial personnel, and the subjects
minimal risk of hypoglycemia. The use of for participating in the study. The LEAD-4
shown for liraglutide (20). Potentially, the
Study Investigators are listed in online appen-
this triple therapy has demonstrated the slight increases in pulse observed with lira- dix 1. We also thank C.T. Chang for statistical
largest decreases in A1C and SBP values in glutide may be compensatory for the de- assistance and Angela M. Campbell and Jen-
the LEAD program. It should be noted creases in SBP. nifer M. Faleska for writing assistance (all from
that ⬃50% of the subjects initiated TZD In summary, this study demonstrated Novo Nordisk).
treatment during the run-in period, and that the triple combination of liraglutide,
doses of metformin and TZD were maxi- metformin, and TZD is an effective and
mized during this period, which may ac- safe treatment for patients with type 2 References
count for the improvements observed in diabetes. This combination significantly 1. Kahn SE, Haffner SM, Heise MA, Herman
the placebo arm of this study. improved glycemic control and other ef- WH, Holman RR, Jones NP, Kravitz BG,
Exenatide, a commercially available ficacy parameters, in addition to resulting Lachin JM, O’Neill MC, Zinman B, Viberti
GLP-1 receptor agonist, is a synthetic ver- in significant weight loss and improved G, the ADOPT Study Group. Glycemic
sion of exendin-4. Unlike liraglutide, durability of rosiglitazone, metformin, or
blood pressure.
glyburide monotherapy. N Engl J Med
which is dosed once daily independently 2006;355:2427– 43
of meals, exenatide is dosed twice daily 2. UKPDS Group. Intensive blood-glucose
within 60 min of breakfast and dinner Acknowledgments — B.Z. has attended advi- control with sulphonylureas or insulin
(14). The findings in this study support sory boards for Amylin, Eli Lilly, GSK, Merck, compared with conventional treatment
the findings of a previous study (15) in sanofi-aventis, and Servier and has received re- and risk of complications in patients with
which 233 subjects inadequately con- search support from GlaxoSmithKline, Merck, type 2 diabetes (UKPDS 33). UK Prospec-
trolled with a stable dose of TZD (rosigli- Novartis, and Novo Nordisk. J.B.B. has con- tive Diabetes Study (UKPDS) Group. Lan-
tazone ⱖ4 mg/day or pioglitazone ⱖ30 ducted clinical trials and provided consultation cet 1998;352:837–53
mg/day) with or without metformin treat- for Novo Nordisk, Amylin Pharmaceuticals, and 3. Green J, Feinglos M. Update on type 2
ment (79% were treated with metformin) Eli Lilly under contract with the University of diabetes mellitus: understanding changes
North Carolina; these relationships do not pro- in the diabetes treatment paradigm. Int
were randomized to add exenatide treat- vide him with direct financial benefit. A.L. has J Clin Pract 2007;61(Suppl. 154):3–11
ment (n ⫽ 121) or placebo (n ⫽ 112) for received research grants from 7TM Pharma, Ab- 4. Holst JJ. The physiology of glucagon-like
16 weeks of treatment. At the end of the bott Laboratories, ActivX Biosciences, Amylin peptide 1. Physiol Rev 2007;87:
study, A1C values decreased by 0.89%, Pharmaceuticals, AstraZeneca, Aura Laborato- 1409 –1439
compared with a slight increase of 0.09% ries, Aventis Pharmaceuticals, Boehringer In- 5. Knudsen LB, Nielsen PF, Huusfeldt PO,
in the placebo group (P ⬍ 0.001). Body gelheim Pharmaceuticals, Bristol-Myers Johansen NL, Madsen K, Pedersen FZ,
care.diabetesjournals.org DIABETES CARE, VOLUME 32, NUMBER 7, JULY 2009 1229
LEAD-4 study
Thøgersen H, Wilken M, Agersø H. Potent in combination with metformin, in type 2 15. Zinman B, Hoogwerf BJ, Durán García S,
derivatives of glucagon-like peptide-1 diabetes: the LEAD (liraglutide effect and Milton DR, Giaconia JM, Kim DD, Traut-
with pharmacokinetic properties suitable action in diabetes)-2 study. Diabetes Care mann ME, Brodows RG. The effect of add-
for once daily administration. J Med 2009;32:84 –90 ing exenatide to a thiazolidinedione in
Chem 2000;43:1664 –1669 10. Russell-Jones D, Vaag A, Schmitz O, Sethi suboptimally controlled type 2 diabetes.
6. Agerso H, Jensen LB, Elbrond B, Rolan P, B, Lalic NM, Antic S, Zdravkovic M, Ravn Ann Intern Med 2007;146:477– 485
Zdravkovic M. The pharmacokinetics, GM, Simo R. Significantly better glycae- 16. Gutzwiller JP, Tschopp S, Bock A, Ze-
pharmacodynamics, safety and tolerabil- mic control and weight reduction with li- hnder CE, Huber AR, Kreyenbuehl M,
ity of NN2211, a new long-acting GLP-1 raglutide, a once-daily human GLP-1 Gutmann H, Drewe J, Henzen C, Goeke
derivative, in healthy men. Diabetologia analog, compared with insulin glargine: B, Beglinger C. Glucagon-like peptide 1
2002;45:195–202 all as add-on to metformin and a sulpho- induces natriuresis in healthy subjects
7. Garber A, Henry R, Ratner R, Garcia-Her- nylurea in type 2 diabetes (Abstract). Di- and in insulin-resistant obese men. J Clin
nandez PA, Rodriguez-Pattzi H, Olvera- abetes 2008;57(Suppl. 1):A159 Endocrinol Metab 2004;89:3055–3061
Alvarez I, Hale PM, Zdravkovic M, Bode 11. Jendle J, Nauck MA, Matthews DR, Frid A, 17. Gutzwiller JP, Hruz P, Huber AR, Hamel
B, the LEAD-3 (Mono) Study Group. Hermansen K, During M, Zdravkovic M, C, Zehnder C, Drewe J, Gutmann H,
Liraglutide versus glimepiride mono- Strauss BJ. Liraglutide, a once-daily human Stanga Z, Vogel D, Beglinger C. Glucagon-
therapy for type 2 diabetes (LEAD-3 GLP-1 analog, reduces fat percentage, vis- like peptide-1 is involved in sodium and
Downloaded from http://diabetesjournals.org/care/article-pdf/32/7/1224/605411/zdc00709001224.pdf by guest on 03 October 2022
Mono): a randomised, 52-week, phase III, ceral and subcutaneous adipose tissue water homeostasis in humans. Digestion
double-blind, parallel-treatment trial. and hepatic steatosis compared with 2006;73:142–150
Lancet 2008;373:473– 481 glimepiride when added to metformin in 18. Nyström T, Gutniak MK, Zhang Q, Zhang
8. Marre M, Shaw J, Brändle M, Bebakar subjects with type 2 diabetes (Abstract). F, Holst JJ, Ahrén B, Sjöholm A. Effects of
WMW, Kamaruddin NA, Strand J, Diabetes 2008;57(Suppl. 1):A32 glucagon-like peptide-1 on endothelial
Zdravkovic M, Le Thi TD, Colagiuri S, 12. World Medical Association. Declaration of function in type 2 diabetes patients with
the LEAD-1 SU Study Group. Liraglutide, Helsinki: recommendations guiding physi- stable coronary artery disease. Am J
a once-daily human GLP-1 analogue, cians in biomedical research involving hu- Physiol Endocrinol Metab 2004;287:
added to a sulphonylurea over 26 weeks man subjects. JAMA 1997;277:925–926 1209 –1215
produces greater improvements in glycae- 13. Matthews DR, Hosker JP, Rudenski AS, 19. Liu H, Hu Y, Simpson RW, Dear AE. Glu-
mic and weight control compared with Naylor BA, Treacher DF, Turner RC. Ho- cagon-like peptide-1 attenuates tumour
adding rosiglitazone or placebo in sub- meostasis model assessment: insulin re- necrosis factor-alpha-mediated induction
jects with type 2 diabetes (LEAD-1 SU). sistance and beta-cell function from of plasmogen activator inhibitor-1 ex-
Diabet Med 2008;26:268 –278 fasting plasma glucose and insulin con- pression. J Endocrinol 2008;196:57– 65
9. Nauck M, Frid A, Hermansen K, Shah NS, centrations in man. Diabetologia 1985; 20. Liu H, Dear A, Knudsen L, Simpson R. A
Tankova T, Mitha IH, Zdravkovic M, Dür- 28:412– 419 long-acting GLP-1 analogue attenuates
ing M, Matthews DR, the LEAD-2 Study 14. Byetta (exenatide) [package insert]. Avail- induction of PAI-1 and vascular adhe-
Group. Efficacy and safety comparison of able from http://pi.lilly.com/us/byetta-pi. sion molecules. J Endocrinol 2009;201:
liraglutide, glimepiride, and placebo, all pdf. Accessed 27 October 2008 59 – 66
1230 DIABETES CARE, VOLUME 32, NUMBER 7, JULY 2009 care.diabetesjournals.org
You might also like
- Diabetes Self-Management Questionnaire (DSMQ)Document2 pagesDiabetes Self-Management Questionnaire (DSMQ)Wayan SugitaNo ratings yet
- Naplex Complete Study Outline A Topic-Wise Approach DiabetesFrom EverandNaplex Complete Study Outline A Topic-Wise Approach DiabetesRating: 4.5 out of 5 stars4.5/5 (3)
- DM Type 2 PathophysiologyDocument3 pagesDM Type 2 PathophysiologyuzumakiruleNo ratings yet
- The Role of Tirzepatide, Dual GIP and GLP-1 Receptor Agonist, in The Management of Type 2 Diabetes: The SURPASS Clinical TrialsDocument15 pagesThe Role of Tirzepatide, Dual GIP and GLP-1 Receptor Agonist, in The Management of Type 2 Diabetes: The SURPASS Clinical TrialsLilian Aracely Gaspar caceresNo ratings yet
- DM WordDocument14 pagesDM WordmasrorohNo ratings yet
- International Journal of Pharmaceutical Science Invention (IJPSI)Document10 pagesInternational Journal of Pharmaceutical Science Invention (IJPSI)inventionjournalsNo ratings yet
- Comparison of Efficacy and Safety Profile of Empagliflozin Versus Dapagliflozin As Add On Therapy in Type 2 Diabetic PatientsDocument5 pagesComparison of Efficacy and Safety Profile of Empagliflozin Versus Dapagliflozin As Add On Therapy in Type 2 Diabetic Patientsthomas albertNo ratings yet
- Glycemic and IRDocument10 pagesGlycemic and IRAyman AleemNo ratings yet
- Drug Evaluation Bashayir &sameraDocument10 pagesDrug Evaluation Bashayir &samerayara baNo ratings yet
- NauckDocument8 pagesNauckIqaNo ratings yet
- Ajhp 140168Document12 pagesAjhp 140168cherrygems99No ratings yet
- Incretin-Based Therapy For Diabetes: What A Cardiologist Needs To KnowDocument9 pagesIncretin-Based Therapy For Diabetes: What A Cardiologist Needs To KnowmdmmmNo ratings yet
- Ghosal 2021 GLP1RA DM MAFLDDocument8 pagesGhosal 2021 GLP1RA DM MAFLDnicnpNo ratings yet
- PMC4020327-jdi 12214Document11 pagesPMC4020327-jdi 12214anca irinaNo ratings yet
- Glucagon-Like Peptide 1-Based Therapies For The Treatment of Type 2 Diabetes Mellitus - UpToDateDocument45 pagesGlucagon-Like Peptide 1-Based Therapies For The Treatment of Type 2 Diabetes Mellitus - UpToDateWaseem UsmanNo ratings yet
- Practical Use of Glucagon-Like Peptide-1 Receptor Agonist Therapy in Primary CareDocument10 pagesPractical Use of Glucagon-Like Peptide-1 Receptor Agonist Therapy in Primary CareRidha Surya NugrahaNo ratings yet
- New Practice in Semaglutide On Type-2 Diabetes and Obesity: Clinical Evidence and ExpectationDocument8 pagesNew Practice in Semaglutide On Type-2 Diabetes and Obesity: Clinical Evidence and ExpectationBoris ThielmannNo ratings yet
- Drug Interaction DMT2Document12 pagesDrug Interaction DMT2Dhonat FlashNo ratings yet
- Incretin Mimetics and Dipeptidyl Peptidase-4 Inhibitors: Innovative Treatment Therapies For Type 2 DiabetesDocument11 pagesIncretin Mimetics and Dipeptidyl Peptidase-4 Inhibitors: Innovative Treatment Therapies For Type 2 DiabetesRidha Surya NugrahaNo ratings yet
- Comparison of Efficacy and Safety Profile of Empagliflozin Versus Dapagliflozin As Add On Therapy in Type 2 Diabetic PatientsDocument6 pagesComparison of Efficacy and Safety Profile of Empagliflozin Versus Dapagliflozin As Add On Therapy in Type 2 Diabetic Patientsthomas albertNo ratings yet
- Incretin PharmDocument3 pagesIncretin PharmSlim SaaryNo ratings yet
- Jdi 13126Document9 pagesJdi 13126Nirmal AliNo ratings yet
- Saxagliptin and Metformin in Fixed Combination For The Treatment of Type 2 Diabetes in AdultsDocument11 pagesSaxagliptin and Metformin in Fixed Combination For The Treatment of Type 2 Diabetes in AdultsLaura MelatiNo ratings yet
- Diabetes Disease Modified DrugsDocument103 pagesDiabetes Disease Modified Drugsbassam alharaziNo ratings yet
- Dapaglifozin A Review in Type 2 DiabetesDocument12 pagesDapaglifozin A Review in Type 2 DiabetesDaniel CastanNo ratings yet
- Dapagliflozin in Type 2 DiabetesDocument12 pagesDapagliflozin in Type 2 DiabetesLokesh KhuranaNo ratings yet
- GLP 1Document15 pagesGLP 1miguelalmenarezNo ratings yet
- Pharmacologic Approaches To Glycemic Treatment Standards of Medical Care in Diabetes-2018Document13 pagesPharmacologic Approaches To Glycemic Treatment Standards of Medical Care in Diabetes-2018ferrossanchezNo ratings yet
- A Review of GLP-1 Receptor Agonists in Type 2 DiabDocument11 pagesA Review of GLP-1 Receptor Agonists in Type 2 Diab이호원No ratings yet
- Tirzepatide Versus Semaglutide Once Weekly in Patients With Type 2 DiabetesDocument13 pagesTirzepatide Versus Semaglutide Once Weekly in Patients With Type 2 Diabetesmanish chaudharyNo ratings yet
- Zmeili 2014 IMDocument40 pagesZmeili 2014 IMscribdNo ratings yet
- (ALEMANIA, 2020) Quality of Life, Glycemic Control, Safety and TolerabilityDocument12 pages(ALEMANIA, 2020) Quality of Life, Glycemic Control, Safety and TolerabilityINVESTIGACIONES HEINZNo ratings yet
- Improving Glucagon-Like Peptide-1 Dynamics in Patients With Type 2 Diabetes MellitusDocument5 pagesImproving Glucagon-Like Peptide-1 Dynamics in Patients With Type 2 Diabetes MellitusscribdNo ratings yet
- Semaglutide Added To Basal Insulin in Type 2 Diabetes (SUSTAIN 5) : A Randomized, Controlled TrialDocument11 pagesSemaglutide Added To Basal Insulin in Type 2 Diabetes (SUSTAIN 5) : A Randomized, Controlled TrialIvan Dario Hernandez ErazoNo ratings yet
- The Effects of Licogliflozin, A Dual SGLT12 Inhibitor, On BodyDocument11 pagesThe Effects of Licogliflozin, A Dual SGLT12 Inhibitor, On BodyJose Mario HoyosNo ratings yet
- Vildagliptin Efficacy in Combination With Metformin Among Jordanian Patients With Type 2 Diabetes Mellitus Inadequately Controlled With MetforminDocument5 pagesVildagliptin Efficacy in Combination With Metformin Among Jordanian Patients With Type 2 Diabetes Mellitus Inadequately Controlled With MetforminAlbert EdoNo ratings yet
- The Kaohsiung J of Med Scie - 2024 - Chong - Recent Advances in The Treatment of Type 2 Diabetes Mellitus Using New DrugDocument9 pagesThe Kaohsiung J of Med Scie - 2024 - Chong - Recent Advances in The Treatment of Type 2 Diabetes Mellitus Using New DrugAnanda SalmaNo ratings yet
- Glucagon-Like Peptide 1 Receptor Agonists For The Treatment of Type 2 Diabetes Mellitus - UpToDateDocument53 pagesGlucagon-Like Peptide 1 Receptor Agonists For The Treatment of Type 2 Diabetes Mellitus - UpToDateRaúl MartínezNo ratings yet
- Incretin HealthyDocument12 pagesIncretin HealthyRoger CNo ratings yet
- Alogliptin - A Review of Its Use in Patients With Type 2 Diabetes MellitusDocument20 pagesAlogliptin - A Review of Its Use in Patients With Type 2 Diabetes Mellitus13201940No ratings yet
- Dipeptidyl Peptidase (DPP) - IV InhibitorDocument2 pagesDipeptidyl Peptidase (DPP) - IV InhibitorAndhi FahrurrojiNo ratings yet
- Incretin-Based Therapies: Joshua J. NeumillerDocument23 pagesIncretin-Based Therapies: Joshua J. NeumillerAbulHasan Idrus IstarNo ratings yet
- GLP-1 Paradigma DC 2017Document7 pagesGLP-1 Paradigma DC 2017Pablo SozaNo ratings yet
- Sustaine 10Document10 pagesSustaine 10Ivan Dario Hernandez ErazoNo ratings yet
- Comparison of Vildagliptin-Metformin and Glimepiride-Metformin Treatments in Type 2 Diabetic PatientsDocument7 pagesComparison of Vildagliptin-Metformin and Glimepiride-Metformin Treatments in Type 2 Diabetic PatientsGregory VeintimillaNo ratings yet
- Newer Drugs in The Management of Diabetes MellitusDocument8 pagesNewer Drugs in The Management of Diabetes MellitusAstri Faluna SheylavontiaNo ratings yet
- Dipeptidyl Peptidase-4 Inhibitors: Their Role in The Management of Type 2 DiabetesDocument3 pagesDipeptidyl Peptidase-4 Inhibitors: Their Role in The Management of Type 2 DiabetesRidha Surya NugrahaNo ratings yet
- Def RonzoDocument6 pagesDef RonzoLidyawati SabutNo ratings yet
- Defronzo2017 PDFDocument36 pagesDefronzo2017 PDFEsteban Martin Chiotti KaneshimaNo ratings yet
- Diabetes LinagliptinaDocument7 pagesDiabetes LinagliptinaFatimaNo ratings yet
- Efficacy of Semaglutide in A Subcutaneous and An Oral FormulationDocument11 pagesEfficacy of Semaglutide in A Subcutaneous and An Oral FormulationNewtonRibeiroNo ratings yet
- Linagliptin - Farmacology, Efficacy and SafetyDocument7 pagesLinagliptin - Farmacology, Efficacy and SafetyMisaelDominguezNo ratings yet
- Empagliflozin/Linagliptin in Type 2 Diabetes: ADocument11 pagesEmpagliflozin/Linagliptin in Type 2 Diabetes: Aalerta.bfcmNo ratings yet
- Glutathione Synthesis Is Diminished in Patients With Uncontrolled Diabetes and Restored by Dietary Supplementation With Cysteine and GlycineDocument6 pagesGlutathione Synthesis Is Diminished in Patients With Uncontrolled Diabetes and Restored by Dietary Supplementation With Cysteine and GlycineSusendren BalakrishnanNo ratings yet
- Surpass 1Document13 pagesSurpass 1Fernando DominguezNo ratings yet
- Clinical Trial Results of Glp-1-Related Agents: The Early EvidenceDocument5 pagesClinical Trial Results of Glp-1-Related Agents: The Early EvidenceRidha Surya NugrahaNo ratings yet
- Wei LinDocument9 pagesWei Linasma.almhsnNo ratings yet
- Pharmacodynamics, Efficacy and Safety of Sodium-Glucose Co-Transporter Type 2 (SGLT2) Inhibitors For The Treatment of Type 2 Diabetes MellitusDocument27 pagesPharmacodynamics, Efficacy and Safety of Sodium-Glucose Co-Transporter Type 2 (SGLT2) Inhibitors For The Treatment of Type 2 Diabetes MellituskoolaberNo ratings yet
- Efficacy and Safety Comparison of Liraglutide, Glimepiride, and Placebo, All in Combination With Metformin, in Type 2 DiabetesDocument7 pagesEfficacy and Safety Comparison of Liraglutide, Glimepiride, and Placebo, All in Combination With Metformin, in Type 2 DiabetesOzi ThingkingandactionNo ratings yet
- Yutaka SeinoDocument11 pagesYutaka Seinoasma.almhsnNo ratings yet
- Mitigating Effects of Vildagliptin in Experimental Diabetes With Metabolic SyndromeDocument9 pagesMitigating Effects of Vildagliptin in Experimental Diabetes With Metabolic Syndromerajesh sumanNo ratings yet
- 02 Ijpscr 123 23Document12 pages02 Ijpscr 123 23BRNSS Publication Hub InfoNo ratings yet
- Storage of Insulin: Idf Europe Awareness PaperDocument12 pagesStorage of Insulin: Idf Europe Awareness PaperIndri AuraliaNo ratings yet
- The Prevalence of Metabolic Syndrome in Latin AmerDocument13 pagesThe Prevalence of Metabolic Syndrome in Latin AmercarolinaNo ratings yet
- Diabetes Prediction ModelDocument7 pagesDiabetes Prediction ModelIJRASETPublicationsNo ratings yet
- Family Nursing Care Plan .Diabetes.Document2 pagesFamily Nursing Care Plan .Diabetes.Jerome GazmenNo ratings yet
- IDFATLAS9e-final-web PDFDocument176 pagesIDFATLAS9e-final-web PDFBala ChandiranNo ratings yet
- Ospe Case Discussion: Presenter - Dr. Salma Ahmed Dept. of BiochemistryDocument29 pagesOspe Case Discussion: Presenter - Dr. Salma Ahmed Dept. of BiochemistryManashi JalanNo ratings yet
- Diabetes Prevention: 5 Tips For Taking Control: 1. Get More Physical ActivityDocument2 pagesDiabetes Prevention: 5 Tips For Taking Control: 1. Get More Physical Activitymatindi galawanNo ratings yet
- WHO - Global Database On Body Mass IndexDocument1 pageWHO - Global Database On Body Mass IndexOwer AsvNo ratings yet
- Mounjaro MonographDocument13 pagesMounjaro Monographlu161513No ratings yet
- Diabetes Care Tasks at SchoolDocument17 pagesDiabetes Care Tasks at SchoolPrakash PrabhuNo ratings yet
- Wound CareDocument43 pagesWound CareIrma Rakhmawati Nur FatimahNo ratings yet
- Observational Registry of Basal Insulin Treatment in Patients With Type 2 Diabetes in China: Safety and Hypoglycemia PredictorsDocument10 pagesObservational Registry of Basal Insulin Treatment in Patients With Type 2 Diabetes in China: Safety and Hypoglycemia PredictorsDiana SamuezaNo ratings yet
- Report 1690018110488Document2 pagesReport 1690018110488Krishna ChaitanyaNo ratings yet
- Nur 105 Adult Health I: Diabetes MellitusDocument70 pagesNur 105 Adult Health I: Diabetes MellitusrikramNo ratings yet
- Self-Monitoring of Blood Glucose in Type 2 Diabetes Recent StudiesDocument11 pagesSelf-Monitoring of Blood Glucose in Type 2 Diabetes Recent StudiesSelaNo ratings yet
- Diabetes in PregnancyDocument38 pagesDiabetes in Pregnancybdzq3i12No ratings yet
- 592008000011: 59000720 03-Aug-20 08:49 AM: Mrs. Veena K Arora: 03-Aug-2020 08:49 AM: Dr. Self: 03-Aug-2020 12:47PM: 48 Y 06 M 12 D / F: 03-Aug-2020 01:12PMDocument2 pages592008000011: 59000720 03-Aug-20 08:49 AM: Mrs. Veena K Arora: 03-Aug-2020 08:49 AM: Dr. Self: 03-Aug-2020 12:47PM: 48 Y 06 M 12 D / F: 03-Aug-2020 01:12PMrajanarora72No ratings yet
- Revised Hypergly NCPDocument15 pagesRevised Hypergly NCPDacillo GailleNo ratings yet
- Insulin Degludec - Pharmacokinetic Properties in Subjects With Hepatic ImpairmentDocument7 pagesInsulin Degludec - Pharmacokinetic Properties in Subjects With Hepatic ImpairmentThúy Trang PhanNo ratings yet
- Rit ReportDocument4 pagesRit Reportadarshranjansingh1903No ratings yet
- Jurnal Diabetes MelitusDocument7 pagesJurnal Diabetes MelitusNova RosalinaNo ratings yet
- Diabetes Blood Sugar Chart Blood Glucose Chart DSMDocument1 pageDiabetes Blood Sugar Chart Blood Glucose Chart DSMBIRD MARKONo ratings yet
- OET Preparation Guide and Sample Corrections by DR Che PDF VersionDocument139 pagesOET Preparation Guide and Sample Corrections by DR Che PDF Versionrajashri patilNo ratings yet
- Select All That Apply Question Study TipsDocument2 pagesSelect All That Apply Question Study TipsjodymahmoudNo ratings yet
- Insulin Pump Therapy Vs InjectionsDocument6 pagesInsulin Pump Therapy Vs InjectionsHakan KüçükerNo ratings yet
- Diabetes & Technology: Dr. Emad HamedDocument49 pagesDiabetes & Technology: Dr. Emad HamedEmad HamedNo ratings yet
- Chapter 18 Homeostasis (Summary)Document2 pagesChapter 18 Homeostasis (Summary)橙歌、No ratings yet
- Aida - Final Assessment PresentationDocument16 pagesAida - Final Assessment PresentationaidaNo ratings yet