Professional Documents
Culture Documents
Blood Pharmacology by Dr. Mayur Sayta
Blood Pharmacology by Dr. Mayur Sayta
Uploaded by
sahilthakker2012Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Blood Pharmacology by Dr. Mayur Sayta
Blood Pharmacology by Dr. Mayur Sayta
Uploaded by
sahilthakker2012Copyright:
Available Formats
Blood- Pharmacology
Vitamin K
Vitamin K, a fat-soluble vitamin, is required for the synthesis of clotting
factors.
It exists in different forms:
Vitamin K1 (phytonadione) is from plant and animal source;
vitamin K2 (menaquinone) is produced by intestinal bacteria and is stored
in hepatic tissue,
vitamin K3 (menadione) is a synthetic form.
All three forms of vitamin K (K1, K2 and K3) are naphthoquinone
derivatives.
Dietary source:
Vitamin K is found in spinach, cabbage, caulifl ower and tomatoes.
It is also present in butter, meat, milk, liver.
The average daily intake for an adult is estimated to be 70–140 mcg/day.
Pharmacokinetics:
Vitamin K1 and K2 require the presence of bile for their absorption
while watersoluble forms can be absorbed in the absence of bile.
Vitamin K is transported along with low-density lipoprotein (LDL) and is
stored mainly in the liver.
It is metabolized by glucuronide and sulphate conjugation
Metabolites are excreted in bile and urine.
Actions:
Vitamin K acts as a cofactor for carboxylation of glutamic acid residues of
clotting factors (II, VII, IX and X).
Deficiency:
Vitamin K defi ciency may occur due to inadequate absorption (lack of bile
salts)
loss of vitamin (chronic diarrhoea) and administration of broad-spectrum
antibiotics (suppression of bacterial flora).
SMCI www.mayursayta.com M 9104448555 Page 1
Blood- Pharmacology
In vitamin K deficiency, there is an increased tendency to bleed—epistaxis,
haematuria, gastrointestinal bleeding and post-operative bleeding.
Preparations
Phytonadione (vitamin K1): It is available for oral, subcutaneous (s.c.),
intramuscular (i.m.) and intravenous (i.v.) administration.
Menadiol sodium diphosphate (vitamin K3): It is a water-soluble
preparation and is available for i.v., i.m. and oral administration.
Uses
1. For prevention and treatment of bleeding associated with vitamin K defi
ciency.
2. In obstructive jaundice with haemorrhagic symptoms, parenteral vitamin K1 is
preferred.
3. Vitamin K1 (1 mg phytonadione, i.m.) is given routinely to all neonates to
prevent bleeding, as the intestinal fl ora—which is necessary for the synthesis of
vitamin K—is not developed.
4. To control bleeding due to oral anticoagulant therapy, phytonadione is used.
5. Vitamin K1 is used in salicylate poisoning with haemorrhagic complications.
Adverse effects
Oral vitamin K is safe.
Intravenous injection may cause flushing, sweating, dyspnoea, hypotension,
cyanosis, collapse and anaphylactic reaction.
Administration of vitamin K through intramuscular and s.c. routes may
cause severe pain.
Menadione may cause haemolysis, hyperbilirubinaemia and kernicterus in
newborn, hence is not used.
SMCI www.mayursayta.com M 9104448555 Page 2
Blood- Pharmacology
Fibrinogen
It is obtained from human plasma.
It is used to control bleeding associated with hypofibrinogenaemia and is
infused intravenously.
Antihaemophilic factor
It contains coagulation factor VIII with von Willebrand’s factor.
It is used to control bleeding episodes in haemophiliacs.
It is administered as i.v. infusion.
Adverse effects include fever with chills, headache and skin rashes.
Ethamsylate
It is a haemostatic, available for oral, i.m. and i.v. administration.
It corrects abnormal platelet adhesionand also maintains the stability of
the capillary wall.
It is well absorbed after oral administration, secreted in breast milk and
excreted unchanged in urine.
It is used for prophylaxis and to control bleeding from small blood vessels
e.g. following tooth extraction, epistaxis, etc.
It may cause skin rashes, hypotension and headache.
SMCI www.mayursayta.com M 9104448555 Page 3
Blood- Pharmacology
Anticoagulants
Anticoagulants are drugs that prevent or reduce coagulability of blood.
Classification
1. Used in vitro:
Heparin
Sodium citrate Used in blood banks to store blood.
Sodium oxalate
Sodium edetate Used as an anticoagulant in laboratory
2. Used in vivo:
Parenteral anticoagulants
Heparin [unfractionated heparin (UFH)].
Low-molecular-weight heparins (LMWHs): Enoxaparin, dalteparin,
tinzaparin, ardeparin, reviparin.
Synthetic - Fondaparinux.
Direct thrombin inhibitors: Lepirudin, bivalirudin.
Oral anticoagulants
Coumarin derivatives- Warfarin, dicumarol.
Indandione derivatives- Phenindione.
Oral direct thrombin inhibitor-Dabigatran etexilate.
Parenteral Anticoagulants
Heparin (Unfractionated Heparin [UFH]
Heparin was discovered by a medical student, McLean. It was later isolated
identified by Howell as a sulphated mucopolysaccharide.
Because of its high concentration in liver, it was named heparin.
A strong electronegative compound, it is the strongest organic acid in the
body.
Commercially, heparin is obtained from ox lung and pig intestinal mucosa.
Mechanism of action
Heparin is an indirect thrombin inhibitor.
Heparin binds and accelerates the activity of plasma antithrombin III.
SMCI www.mayursayta.com M 9104448555 Page 4
Blood- Pharmacology
Heparin antithrombin III complex then inhibits activated clotting factors
Xa, IIa, IXa, XIa, XIIa and XIIIa by forming stable complexes with them.
At low concentration, heparin selectively inhibits the conversion of
prothrombin to thrombin.
Heparin thus prevents further thrombus formation.
Heparin in high doses has antiplatelet action and, thereby, prolongs the
bleeding time.
Heparin reduces the blood lipid level by releasing lipoprotein lipase from
vessel wall and tissues.
Pharmacokinetics
Heparin is not absorbed after oral administration because of its high
negative charge and large molecular size.
Therefore, it must be given parenterally—intravenously or
subcutaneously.
On i.v. administration, the anticoagulant effect starts immediately,
SMCI www.mayursayta.com M 9104448555 Page 5
Blood- Pharmacology
Through s.c. route, it takes 1–2 hours.
Heparin is highly protein bound.
It does not cross the blood–brain barrier or placental barrier and is safe
during pregnancy.
It is rapidly inactivated in the liver by heparinase and the metabolites are
excreted in urine.
Mode of administration
Heparin is administered by i.v. infusion and i.v. intermittent injection (for
treatment) or
s.c. route (for prophylaxis).
Administration of heparin intramuscularly may cause haematomas; hence, this
route should not be used.
During heparin therapy, activated partial thromboplastin time (aPTT)
monitoring is necessary
Adverse effects and contraindications
1. Bleeding:
Bleeding can occur in the urinary and gastrointestinal tract or anywhere in
the body.
it can be controlled rapidly by slow i.v. infusion of protamine sulphate
(heparin antagonist).
It is a strongly basic protein and hence rapidly neutralizes the
anticoagulant effect of heparin.
It is obtained from fish sperm.
One milligram of protamine sulphate approximately neutralizes 100 units of
heparin (chemical antagonism).
2. Heparin-induced thrombocytopenia (HIT)
3. Hypersensitivity. They are skin rashes, urticaria, fever, etc.
4. Osteoporosis
5. Reversible alopecia has been reported.
Heparin is contraindicated in haemophiliacs, patients with heparin-induced
thrombocytopenia (HIT), severe hypertension, intracranial haemorrhage,
bacterial endocarditis, active tuberculosis, peptic ulcer, threatened
abortion, cirrhosis, renal failure, etc.
SMCI www.mayursayta.com M 9104448555 Page 6
Blood- Pharmacology
Low-molecular-weight heparins (LMWHs)
Enoxaparin, dalteparin, tinzaparin, ardeparin, reviparin, etc. are LMWHs
and are isolated from standard heparin by various techniques.
LMWHs are indirect thrombin inhibitors—produce anticoagulant effect
mainly by inhibition of factor Xa through antithrombin.
Low-molecular-weight heparins are given subcutaneously.
The following are the advantages of LMWHs
1. They have a higher s.c. bioavailability as compared to UFH.
2. They have a longer duration of action.
3. They do not routinely require aPTT monitoring.
4. There is a lower incidence of thrombocytopaenia and osteoporosis.
(Uses, adverse effects and contraindications are same as other anticoagulants)
Fondaparinux
It is a synthetic parenteral anticoagulant.
It binds to antithrombin and selectively inhibits factor Xa (indirect thrombin
inhibitor).
It does not require routine laboratory monitoring.
Fondaparinux is administered subcutaneously.
It is useful in pulmonary embolism and deep vein thrombosis (DVT).
Incidence of thrombocytopaenia is lower with fondaparinux.
Direct thrombin inhibitors
Lepirudin and bivalirudin combine directly and inactivate thrombin
without binding to antithrombin III.
They are used in patients who are at risk of heparin induced
thrombocytopaenia.
SMCI www.mayursayta.com M 9104448555 Page 7
Blood- Pharmacology
Oral Anticoagulants
Among oral anticoagulants, coumarin derivatives are commonly used.
Oral anticoagulants act only in vivo.
They are vitamin K antagonists.
Mechanism of action (Fig. 9.2)
Clotting factors II, VII, IX and X are synthesized in liver as inactive proteins.
These factors are rich in glutamic acid residues and are carboxylated in
liver where active form of vitamin K acts as a cofactor.
Vitamin K is converted to inactive epoxide form by oxidation and is
regenerated to its active form by epoxide reductase enzyme.
Warfarin is a coumarin derivative and has a structure similar to that of
vitamin K.
Hence, warfarin competitively inhibits epoxide reductase enzyme, thus
inhibiting the synthesis of vitamin K-dependent biologically active factors—
II, VII, IX and X
and produces anticoagulant effect.
The onset and duration of anticoagulant effect of warfarin depends on the
half-lives (in hours) of clotting factors,
which are as follows: VII (6), IX (24), X (36) and II (50).
There is always a delay in the onset of anticoagulant effect because the
levels of clotting factors already present in plasma decline slowly over a
period of 1–3 days.
SMCI www.mayursayta.com M 9104448555 Page 8
Blood- Pharmacology
Pharmacokinetics
Warfarin is almost completely absorbed after oral administration.
It can also be given intravenously or rectally.
Food interferes with the absorption of warfarin.
It is highly bound to plasma proteins, freely crosses placental barrier, is
metabolized in liver and the inactive metabolites are excreted in urine and
stool.
It has a long half-life of about 40 hours, and the duration of action is 2–5
days.
Adverse effects
1. Bleeding
Bleeding can be controlled by oral or parenteral vitamin K1
Oral anticoagulant therapy is monitored by measuring international
normalized ratio (INR).
2. Teratogenic effect: Warfarin is contraindicated during pregnancy as it may
cause foetal CNS abnormalities, foetal haemorrhage, abortion or intrauterine
death.
3. Skin necrosis- The skin lesions are commonly seen on breast, buttocks,
abdomen and thighs.
4. Other rare side effects: These include diarrhoea, alopecia, urticaria,
dermatitis, abdominal cramps and anorexia.
Oral direct thrombin inhibitor
Dabigatran etexilate is a prodrug, which is converted to dabigatran.
No laboratory monitoring is required during dabigatran therapy.
SMCI www.mayursayta.com M 9104448555 Page 9
Blood- Pharmacology
Difference between heparin and warfarin
SMCI www.mayursayta.com M 9104448555 Page 10
Blood- Pharmacology
Therapeutic Uses of Anticoagulants
The main aim of anticoagulant therapy is to prevent formation of
intravascular thrombus or further extension of the already formed clot.
They do not dissolve the clot or thrombus once it is formed.
Treatment is initiated with an LMWH or UFH and continued for at least 4–
5 days.
An oral anticoagulant, warfarin, is usually started simultaneously as it has
a delayed onset of action.
1. Deep vein thrombosis and pulmonary embolism:
Venous thrombi are mainly formed of fibrin.
Anticoagulants are used for the treatment and prevention of
thromboembolism in high-risk cases, e.g. prolonged hospitalization,
prolonged immobilization, major surgery, major trauma, etc.
Anticoagulants are used along with low-dose aspirin to prevent
thromboembolism in patients undergoing haemodialysis and those with
prosthetic heart valves.
2. Myocardial infarction:
Anticoagulants (heparin, LMWH or fondaparinux) are used in patients with
a high risk of embolism
Anticoagulants help to prevent recurrent attacks of myocardial infarction
and stroke, especially when given in combination with low dose of aspirin.
Heparin is used during coronary angioplasty.
3. Unstable angina
4. Atrial fibrillation
5. disseminated intravascular coagulation.
SMCI www.mayursayta.com M 9104448555 Page 11
Blood- Pharmacology
Fibrinolytics (Thrombolytics)
Fibrinolytics promote the conversion of plasminogen to plasmin.
Plasmin degrades fibrin into fibrin degradation products and thus rapidly
dissolves the blood clot.
Streptokinase, urokinase, alteplase, reteplase and tenecteplase are
plasminogen activators
Reteplase and tenecteplase are obtained from DNA recombinant
technology. They have longer plasma half-lives than alteplase.
Uses of fibrinolytics
1. Acute MI:
The main aim of fibrinolytic therapy is to restore coronary artery patency.
Thrombolytic therapy is more effective if they are administered within 6–12
h of onset of symptoms.
2. Deep vein thrombosis: Thrombolytic therapy helps to prevent DVT.
3. Pulmonary embolism: Fibrinolytics are used to lyse the clot.
Contraindications
Recent trauma, recent surgery, recent abortion, recent stroke, severe
hypertension
Severe diabetes, severe liver damage, peptic ulcer and bleeding disorders.
SMCI www.mayursayta.com M 9104448555 Page 12
Blood- Pharmacology
SMCI www.mayursayta.com M 9104448555 Page 13
Blood- Pharmacology
Antifibrinolytics
Antifi brinolytics block the conversion of plasminogen to plasmin and thus inhibit
fibrinolytic activity
Epsilon amino-caproic acid (EACA)
It is administered orally or intravenously.
It is used mainly to control bleeding due to overdose of fibrinolytics
after tooth extraction and surgery in haemophiliacs.
It can also be used in haematuria and bleeding following obstetric
complications.
It rarely causes myopathy and muscle necrosis.
Tranexamic acid
It is available for oral, i.v. and topical administration.
It is more potent than EACA.
It is used to control bleeding due to excessive fibrinolytic activity and
following tooth extraction, tonsillectomy, prostatectomy, etc
In dentistry, tranexamic acid soaked gauze or mouthwash can be used to
reduce bleeding postoperatively in haemophiliacs and in patients on
anticoagulant therapy.
Its main side effects are nausea, vomiting, diarrhoea, headache, etc.
SMCI www.mayursayta.com M 9104448555 Page 14
Blood- Pharmacology
ANTIPLATELET DRUGS
Drugs that inhibit platelet aggregation are called antiplatelet drugs
Classification
1. Thromboxane (TXA2) synthesis inhibitor Low-dose aspirin.
2. Phosphodiesterase inhibitor Dipyridamole.
3. Thienopyridine derivatives Ticlopidine and clopidogrel.
4. Glycoprotein (GP)-IIb/IIIa-receptor antagonists: Abciximab, eptifibatide and
tirofiban.
SMCI www.mayursayta.com M 9104448555 Page 15
Blood- Pharmacology
Aspirin (TXA2 synthesis inhibitor)
Low-dose aspirin (50–325 mg) irreversibly acetylates platelet COX-I and
reduces the production of TXA2;
thus the antiplatelet effect lasts for the life-time of the platelets, i.e. 7–10
days.
In higher doses, aspirin inhibits both TXA2 and PGI2; hence efficacy is
reduced.
Common adverse effects are gastric irritation and bleeding.
Dipyridamole (phosphodiesterase inhibitor)
It is a vasodilator.
It inhibits phosphodiesterase and increases the concentration of cyclic
adenosine monophosphate (cAMP) levels, which inhibits platelet
aggregation.
It is occasionally used in combination with warfarin during postoperative
period in patients with prosthetic heart valves.
Ticlopidine and clopidogrel (thienopyridine derivatives)
They are prodrugs and structurally related.
They inhibit adenosine diphosphate (ADP)-mediated platelet aggregation.
Ticlopidine is well absorbed after oral administration and is converted to
an active metabolite in liver.
It has a long duration of antiplatelet effect.
Side effects are nausea, vomiting, diarrhoea, leucopaenia, agranulocytosis,
thrombocytopaenia and GI bleeding.
Clopidogrel
It is a congener of ticlopidine.
It is also given orally.
They produce synergistic effect when combined with aspirin or GP-IIb/IIIa
antagonists.
Clopidogrel produces fewer side effects than ticlopidine; and it rarely
produces neutropaenia and thrombocytopaenia.
SMCI www.mayursayta.com M 9104448555 Page 16
Blood- Pharmacology
Abciximab, eptifibatide and tirofi ban (GP IIb/IIIa receptor antagonists)
They block GP IIb/IIIa receptors for fibrinogen and von Willebrand’s factor
on platelet surface,
Thus inhibiting the final step in the process of platelet aggregation.
These drugs are administered parenterally.
Abciximab is a monoclonal antibody
Eptifibatide is a synthetic drug.
The main side effect of these drugs is bleeding.
Uses
Acute MI: Low-dose aspirin is most commonly used in high-risk individuals
to reduce the incidence of MI and in post-MI patients to prevent recurrent
attacks.
unstable angina,
Transient ischaemic attacks,
in patients with prosthetic heart valves
Periphheral artery Disease.
SMCI www.mayursayta.com M 9104448555 Page 17
Blood- Pharmacology
HAEMATINICS
Causes of anaemia
1. Decreased formation of RBCs: Defi ciency of essential nutrients—iron, vitamin
B12, folic acid, etc.
2. Increased destruction of RBCs: Haemolytic anaemias, sickle-cell anaemia.
3. Depression of bone marrow: Cytotoxic drugs, radiation, toxins.
4. Excessive blood loss: Due to hookworm infestation, bleeding from
gastrointestinal tract (GIT) and other sites.
Iron
Iron is an essential element of the body.
The important sources of iron are liver, fish, dry fruits, jaggery, spinach,
banana, meat, etc.
SMCI www.mayursayta.com M 9104448555 Page 18
Blood- Pharmacology
Factors affecting iron absorption
Iron absorption is facilitated by acidic pH of the stomach, ascorbic acid,
cysteine, etc.,
which reduces the ferric iron to ferrous form.
Iron-defi ciency states also increase the absorption of iron.
Iron absorption is inhibited by excess of phosphates, oxalates, phytates,
etc.
Milk, antacids and tetracyclines reduce iron absorption by forming
insoluble complexes.
Preparations of iron
Oral preparations:
1. Ferrous sulphate contains 20% (hydrated salt) and 32% (dried salt) elemental
iron.
It is the oldest and cheapest iron preparation.
2. Ferrous gluconate contains 12% elemental iron.
3. Ferrous fumarate contains 33% elemental iron.
4. Colloidal ferric hydroxide – 50%
5. Carbonyl iron – Purified metallic iron
Other are ferrous succinate, iron choline citrate, ferric ammonium citrate, etc.
Adverse effects of oral iron are - nausea, vomiting, epigastric discomfort,
dyspepsia, metallic taste, constipation or diarrhoea, and staining of teeth (mainly
with liquid preparation).
Parenteral preparations
1. Iron sorbitol citric acid complex (Jectofer): It is given intramuscularly, but
never intravenously.
2. Iron dextran complex (Imferon): It can be administered intravenously or
intramuscularly.
To prevent staining of the skin, intramuscular injection of iron preparations
into the buttock is made using Z-track technique.
3. Ferric carboxymaltose and ferrous sucrose are administered intravenously.
The risk of hypersensitivity reaction is much less with these preparations.
SMCI www.mayursayta.com M 9104448555 Page 19
Blood- Pharmacology
Indications for parenteral iron therapy
1. Intolerance to oral iron.
2. Severe malabsorption.
3. Non-compliance to oral iron.
4. Severe anaemia in the late stages of pregnancy.
5. Along with erythropoietin in patients with renal disease.
The total dose of parenteral iron is calculated by using the formula
Iron requirement (mg) = 4.4 × body weight (kg) × Hb deficit (g/dL)
(Normal Hb in men = 14–16 g%; women = 12–14 g%)
Adverse effects
The injections are painful,
May cause abscess and discolouration of the skin at the site of injection.
Thesystemic side effects are headache, pyrexia, nausea, vomiting,
arthralgia, lymphadenopathy, urticaria
anaphylactic reaction (Test dose of iron preparation should be
administered before giving full dose of parenteral iron).
Therapeutic uses of iron
1. To treat iron-defi ciency anaemia (microcytic hypochromic anaemia)
a. During pregnancy.
b. Due to blood loss.
c. Due to nutritional iron defi ciency.
d. Due to poor absorption of iron from the gut.
Most of the patients can be treated with oral iron.
For treatment of iron-defi ciency anaemia, 200 mg of elemental iron is
required per day.
Ferrous sulphate is the most commonly used preparation—200 mg of
ferrous sulphate (60 mg elemental iron) is given thrice daily after food.
Therapy should be continued till the Hb level returns to normal (4–8
weeks);
and later, iron should be continued for at least 3–6 months to replenish
iron stores.
The expected rise in Hb concentration after iron therapy is 0.7–1 g/100
mL/week.
SMCI www.mayursayta.com M 9104448555 Page 20
Blood- Pharmacology
2. Prophylaxis
Prophylactic iron therapy is usually indicated during pregnancy and infancy.
For prophylaxis, 100 mg of elemental iron is administered daily
Starting from the second trimester.
Folic acid 0.5 mg/day is given from the first trimester to prevent neural
tube defects.
Acute Iron Poisoning
It is seen frequently in young children.
The manifestations are nausea, vomiting, epigastric pain, bloody diarrhoea,
dehydration, cyanosis, drowsiness, hyperventilation, metabolic acidosis,
convulsions, coma and death.
Treatment
General measures
Supportive measures
Airway, Breathing, Circulation, Fluid and Electrolyte and acid–base balance
should be maintained.
Whole bowel irrigation to remove unabsorbed iron pills from the GIT.
Intravenous Diazepam to control convulsions.
Specific therapy
Desferrioxamine, a potent iron chelating agent
It is administered by i.v. infusion or intramuscularly depending on the
severity of poisoning.
It binds with iron in the blood and facilitates its excretion.
SMCI www.mayursayta.com M 9104448555 Page 21
You might also like
- Case 21Document45 pagesCase 21Mark GironNo ratings yet
- AnticoagulantDocument34 pagesAnticoagulantAslam Baltee100% (1)
- Drugs Used in Disorders of CoagulationDocument61 pagesDrugs Used in Disorders of CoagulationDUEÑAS, MARIELNo ratings yet
- Endocrine Pharmacology by DR - Mayur SaytaDocument27 pagesEndocrine Pharmacology by DR - Mayur Saytasahilthakker2012No ratings yet
- Anti EmeticsDocument29 pagesAnti EmeticsBezawit TsigeNo ratings yet
- 8 Fibrinolytic DrugsDocument41 pages8 Fibrinolytic DrugsIman SaksoukNo ratings yet
- Antibiotics 9Document11 pagesAntibiotics 9Beth Morales100% (1)
- Mu 002Document10 pagesMu 002chandanNo ratings yet
- Pharmacology of The GITDocument31 pagesPharmacology of The GITmarviecute22No ratings yet
- Histamine: Moderator: Dr. Pooja Shukla Resident: Fariha Fatima JR-2Document45 pagesHistamine: Moderator: Dr. Pooja Shukla Resident: Fariha Fatima JR-2;'SiLeNt';No ratings yet
- Agam Pharm CompressedDocument265 pagesAgam Pharm CompressedthisaiofficialNo ratings yet
- AntiemeticsDocument25 pagesAntiemeticsPridho GaziansyahNo ratings yet
- Git PharmacologyDocument73 pagesGit PharmacologyShehu Baba AbdullahiNo ratings yet
- PharmacologyDocument74 pagesPharmacologyKiara Denise Tamayo100% (1)
- Antimalarial Drug CologyDocument15 pagesAntimalarial Drug CologyManthan ChauhanNo ratings yet
- Organic Medicinal Chemistry: FunctionalizationDocument25 pagesOrganic Medicinal Chemistry: FunctionalizationPrincess RonsableNo ratings yet
- 2013 December Exam CompilationDocument7 pages2013 December Exam CompilationabbasyaqobiNo ratings yet
- Antibiotic Summary - DraftDocument10 pagesAntibiotic Summary - DraftStrept Pneumonia100% (1)
- Mechanism of Action For Each Class of AntiDocument146 pagesMechanism of Action For Each Class of AntiReynaldo RiveraNo ratings yet
- MalariaDocument61 pagesMalariaEscitalopram 5mgNo ratings yet
- Common DrugsDocument15 pagesCommon DrugsKate Penelope DalidNo ratings yet
- Table: Selected Antibacterial Antibiotics Antibiotics THAT . Mechanism of Action Names of Drugs Notes and ProblemsDocument4 pagesTable: Selected Antibacterial Antibiotics Antibiotics THAT . Mechanism of Action Names of Drugs Notes and ProblemsTJNo ratings yet
- APHA-Chapter-34 - Patient Assessment Laboratory: REVIEW OF SYSTEMS - Physical Assessment, Vital Signs& ObservationsDocument13 pagesAPHA-Chapter-34 - Patient Assessment Laboratory: REVIEW OF SYSTEMS - Physical Assessment, Vital Signs& ObservationsDrSamia El WakilNo ratings yet
- Drug Use During Pregnancy and LactationDocument50 pagesDrug Use During Pregnancy and LactationJuveria Fatima75% (4)
- Pharma MneomicsDocument30 pagesPharma MneomicselanthamizhmaranNo ratings yet
- Adrenocorticosteroids & Adrenocortical Antagonists: Namwase Hadijja KatabiraDocument77 pagesAdrenocorticosteroids & Adrenocortical Antagonists: Namwase Hadijja KatabiraSamson100% (1)
- Drug Interaction SaDocument3 pagesDrug Interaction SaShahabWassiNo ratings yet
- Pharmacology of The Antibiotics: Nurse Licensure Examination ReviewDocument27 pagesPharmacology of The Antibiotics: Nurse Licensure Examination ReviewSeth-Thomas TateNo ratings yet
- Tienam Leaflet Eng-102!12!03Document2 pagesTienam Leaflet Eng-102!12!03MikeNo ratings yet
- AntibioticsDocument36 pagesAntibioticsBen Paolo Cecilia RabaraNo ratings yet
- Antiarrhythmic Drugs-Test-2-QuestionsDocument7 pagesAntiarrhythmic Drugs-Test-2-QuestionsDrishya BioplannetNo ratings yet
- 39 Adrenocorticosteroids and Andrenocortical AntagonistsDocument5 pages39 Adrenocorticosteroids and Andrenocortical AntagonistsJENICCA GONo ratings yet
- Pharmacology Antimycobacterial DrugsDocument9 pagesPharmacology Antimycobacterial Drugsroyce charlieNo ratings yet
- IV PO Conversion CAPDocument3 pagesIV PO Conversion CAPdamondouglasNo ratings yet
- To The Point PharmacologyDocument5 pagesTo The Point PharmacologyDR AbidNo ratings yet
- Bioavailability Bioequivalance PDFDocument24 pagesBioavailability Bioequivalance PDFANJUM N. HASNAINNo ratings yet
- Drug Drug Interactions 2Document133 pagesDrug Drug Interactions 2joo saadNo ratings yet
- Review Notes For Diabetes MellitusDocument8 pagesReview Notes For Diabetes MellitusEditha LucasNo ratings yet
- Beta Lactam AntibioticsDocument94 pagesBeta Lactam AntibioticsHely PatelNo ratings yet
- MeningitisDocument5 pagesMeningitisliesel_12100% (1)
- Pharm All NotesDocument511 pagesPharm All NotesShoaib Ali100% (1)
- Drug Analysis: Submitted By: GALICINAO, Gretta Shalou GDocument9 pagesDrug Analysis: Submitted By: GALICINAO, Gretta Shalou GggalicinaoNo ratings yet
- Drug ListDocument2 pagesDrug ListhahahahaaaaaaaNo ratings yet
- Chapter 43 - Beta-LactamDocument7 pagesChapter 43 - Beta-LactamErika De JesusNo ratings yet
- Sem 5/unit-3 Autocoids & Related DrugsDocument28 pagesSem 5/unit-3 Autocoids & Related DrugsDARSHAN BhirudNo ratings yet
- Pharmacotherapeutics PDFDocument30 pagesPharmacotherapeutics PDFprazol shresthaNo ratings yet
- Anthelmintics 2020Document19 pagesAnthelmintics 2020RutinNo ratings yet
- Prescribing Medicine in Pregnancy, by Australian Drug Evaluation CommitteeDocument90 pagesPrescribing Medicine in Pregnancy, by Australian Drug Evaluation Committee徐承恩100% (1)
- Vancomycin Protocol RQHRDocument15 pagesVancomycin Protocol RQHRl1o2stNo ratings yet
- Dispensing Lab - Calculations and Practice of PharmacyDocument36 pagesDispensing Lab - Calculations and Practice of PharmacyJoyce VillanuevaNo ratings yet
- Presented By: (DR.) Vishnu.R.Nair, Pharm.D Intern (Amri Hospital Academic Trainee), National College of Pharmacy, Kozhikode, KeralaDocument92 pagesPresented By: (DR.) Vishnu.R.Nair, Pharm.D Intern (Amri Hospital Academic Trainee), National College of Pharmacy, Kozhikode, KeralaHarshit BhardwajNo ratings yet
- Warfarin Sodium: INR Levels 4.0 or Less Ok To Carry Out Procedure Test Atleast 72 Hrs Prior To ProcedureDocument6 pagesWarfarin Sodium: INR Levels 4.0 or Less Ok To Carry Out Procedure Test Atleast 72 Hrs Prior To ProcedureVimi GeorgeNo ratings yet
- Warfarin Mechanism of ActionDocument7 pagesWarfarin Mechanism of ActionIna GrigorasNo ratings yet
- SJDWHDJSDJSDDocument358 pagesSJDWHDJSDJSDwide mind hackerNo ratings yet
- Anticoagulants ParamedDocument20 pagesAnticoagulants ParamedManikanta GupthaNo ratings yet
- Anti Coagulatants: Presented By:-Mr - Gorishankar Nursing Tutor (Tantia University)Document10 pagesAnti Coagulatants: Presented By:-Mr - Gorishankar Nursing Tutor (Tantia University)yogesh kumarNo ratings yet
- Drugs Used To Affect in Blood Coagulation: Prajogo WibowoDocument44 pagesDrugs Used To Affect in Blood Coagulation: Prajogo WibowoIda Bagus Putu SwabawaNo ratings yet
- PHM - Hematologic DrugsDocument3 pagesPHM - Hematologic DrugsJeanne Rodiño100% (3)
- Anticoagulant TherapyDocument41 pagesAnticoagulant Therapyryan yovanNo ratings yet
- Coagulants and AnticoagulantsDocument29 pagesCoagulants and AnticoagulantsfdamissieNo ratings yet
- Anticoagulants May BeDocument5 pagesAnticoagulants May BeAmmar magdyNo ratings yet
- Handbook of Pediatric Hematology and Oncology 3rd Edition 2021Document492 pagesHandbook of Pediatric Hematology and Oncology 3rd Edition 2021pgginecologiahospirioNo ratings yet
- Iron Deficiency Anemia-HandoutDocument4 pagesIron Deficiency Anemia-HandoutCeleste Parin Procopia KardinNo ratings yet
- AnaemiaDocument25 pagesAnaemiaShubhendu ChattopadhyayNo ratings yet
- Anemia in ChildrenDocument9 pagesAnemia in ChildrenanishaNo ratings yet
- Iron Dextran Drug StudyDocument5 pagesIron Dextran Drug StudySofronio OmboyNo ratings yet
- Obs-UM - Paper - 1Document16 pagesObs-UM - Paper - 1Muhammad Abbas AliNo ratings yet
- Haematinics PPDocument37 pagesHaematinics PPLilaksha HasarangaNo ratings yet
- Heamatology Dr. Osama PDFDocument94 pagesHeamatology Dr. Osama PDFAnmar ZawahraNo ratings yet
- Anemia in PregnancyDocument11 pagesAnemia in PregnancyIcetea KokomNo ratings yet
- Assessment and Management of Patients With Hematologic DisordersDocument20 pagesAssessment and Management of Patients With Hematologic DisordersJhosita Flora LarocoNo ratings yet
- Anemia in Chronic Kidney DiseaseDocument38 pagesAnemia in Chronic Kidney DiseaseHemodialisa LindimaraNo ratings yet
- Comparative Study On Efficacy, Tolerability, and Cost of Different Iron Supplements Among Antenatal Women With Iron-Deficiency AnemiaDocument8 pagesComparative Study On Efficacy, Tolerability, and Cost of Different Iron Supplements Among Antenatal Women With Iron-Deficiency AnemiaAjay DNo ratings yet
- Estacion, England Dan C. - AnemiasDocument17 pagesEstacion, England Dan C. - AnemiasEngland Dan EstacionNo ratings yet
- VenoferDocument13 pagesVenoferLuciano H.Vivas M.No ratings yet
- Anemia in PregnancyDocument24 pagesAnemia in PregnancyAzwanie Ali100% (1)
- Sogp Anemia Highllight MedhomeDocument32 pagesSogp Anemia Highllight MedhomeMuhammad Farrukh ul IslamNo ratings yet
- Lipid Lowering Agents IDocument14 pagesLipid Lowering Agents IRALPH ELVIN MACANLALAYNo ratings yet
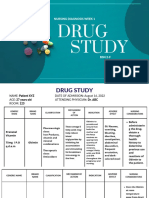
- Drug StudyDocument1 pageDrug StudyTHERESE YZABEL CLOMANo ratings yet
- Analytical Method Development and Validation For Iron and Ascorbic Acid in Ferrous Bisglycinate Effervescent Tablets by Colorimetry and Reverse Phase-High-performance Liquid ChromatographyDocument7 pagesAnalytical Method Development and Validation For Iron and Ascorbic Acid in Ferrous Bisglycinate Effervescent Tablets by Colorimetry and Reverse Phase-High-performance Liquid Chromatographyshoaib naqviNo ratings yet
- Misbah 2016-Tip AnswersDocument269 pagesMisbah 2016-Tip AnswersMahsa PourghasemNo ratings yet
- Assessment and Management of Patients With Hematologic DisordersDocument20 pagesAssessment and Management of Patients With Hematologic Disorderschristine mercado100% (1)
- Becadexamin PDFDocument14 pagesBecadexamin PDFakshay bhadauriaNo ratings yet
- DS Ferrous SulfateDocument3 pagesDS Ferrous SulfateKrizha Angela NicolasNo ratings yet
- Recreational Drugs DissertationDocument4 pagesRecreational Drugs DissertationProfessionalPaperWritersHartford100% (1)
- Hematopoietic Agents and Hematinics: PharmacologyDocument9 pagesHematopoietic Agents and Hematinics: PharmacologyAbi SulitNo ratings yet
- J1-T5 Anemia FerropénicaDocument12 pagesJ1-T5 Anemia FerropénicaGoblin HunterNo ratings yet
- CE Forceris Art N4 LRDocument7 pagesCE Forceris Art N4 LRLài LêNo ratings yet
- Iron Deficiency Anemia PregnancyDocument18 pagesIron Deficiency Anemia PregnancyKarleneNo ratings yet
- Study: Nursing Diagnosis Week 1Document9 pagesStudy: Nursing Diagnosis Week 122 - Fernandez, Lyza Mae D.No ratings yet