Professional Documents
Culture Documents
Safari - Feb 21, 2024 at 12:17 PM 3
Safari - Feb 21, 2024 at 12:17 PM 3
Uploaded by
syansyncCopyright:
Available Formats
You might also like
- Bone Development and Growth: Rosy Setiawati and Paulus RahardjoDocument20 pagesBone Development and Growth: Rosy Setiawati and Paulus Rahardjoputri aishe100% (1)
- Fracture Healing in Cortical and Cancellous BoneDocument63 pagesFracture Healing in Cortical and Cancellous BonePramod Thottimane0% (1)
- Bones As A Living Dynamic TissueDocument13 pagesBones As A Living Dynamic TissueSanish Basnet100% (1)
- Fracture Healing and BonegraftingDocument76 pagesFracture Healing and BonegraftingJio AmurNo ratings yet
- Stages of Bone HealingDocument2 pagesStages of Bone HealingArra Beatriz100% (1)
- Dr. Sassia Lecture Bone Histology Part II July 4 2023Document39 pagesDr. Sassia Lecture Bone Histology Part II July 4 2023Ali ELKARGHALYNo ratings yet
- Bone HealingDocument5 pagesBone HealingFadliArifNo ratings yet
- Lec. 4 Bone FractureDocument11 pagesLec. 4 Bone Fracturebtwlalbwdy16No ratings yet
- Distraction OsteogenesisDocument141 pagesDistraction OsteogenesisJohan Edward Franklin MarpaungNo ratings yet
- AO Surgery ReferenceDocument8 pagesAO Surgery ReferenceHurulaeniNo ratings yet
- Orthopaedics DocumentDocument131 pagesOrthopaedics DocumentRazvan NegritasNo ratings yet
- Alveolarbone Graftingand Reconstruction Procedurespriorto ImplantplacementDocument10 pagesAlveolarbone Graftingand Reconstruction Procedurespriorto ImplantplacementKranti PrajapatiNo ratings yet
- Fracture HealingDocument22 pagesFracture Healingsumitbhosale3No ratings yet
- Fracture Healing and FactorsDocument29 pagesFracture Healing and FactorsVivek ChNo ratings yet
- FRACTURESDocument85 pagesFRACTURESSteven OdhiamboNo ratings yet
- Bridging Technique and Science A Review of The Molecular Sig - 2022 - OrthoplasDocument7 pagesBridging Technique and Science A Review of The Molecular Sig - 2022 - OrthoplasAlex Rolando Suntaxi LlumiquingaNo ratings yet
- Principles of Bone GraftingDocument6 pagesPrinciples of Bone GraftingJayanth Perumal100% (2)
- Normal Bone Anatomy and Physiology: Go ToDocument11 pagesNormal Bone Anatomy and Physiology: Go TotariNo ratings yet
- Fix. Musculosceletal Anatomy (DR - Hendra)Document33 pagesFix. Musculosceletal Anatomy (DR - Hendra)rumah sakit daerahNo ratings yet
- 1 2009-Principles of Fracture Healing and Disorders of Bone UnionDocument7 pages1 2009-Principles of Fracture Healing and Disorders of Bone UnionRodrigo ValderramaNo ratings yet
- Week 6 Bone Case StudyDocument7 pagesWeek 6 Bone Case StudyAndriNo ratings yet
- What Is A FractureDocument4 pagesWhat Is A FracturemidskiescreamzNo ratings yet
- DR Himanshu Gaur: Consultant Orthopaedic, Joint Replacement & Arthroscopy (Sports Injury) Surgeon BCIMS, New DelhiDocument34 pagesDR Himanshu Gaur: Consultant Orthopaedic, Joint Replacement & Arthroscopy (Sports Injury) Surgeon BCIMS, New DelhiAnjani Kumar JhaNo ratings yet
- A Brief Introduction Into Orthopaedic ImplantsDocument20 pagesA Brief Introduction Into Orthopaedic ImplantsLuisAngelPonceTorresNo ratings yet
- TARI ReferensiDocument13 pagesTARI ReferensitariNo ratings yet
- Fractures and Fracture Healing Lecture 22422 Sept 2023Document25 pagesFractures and Fracture Healing Lecture 22422 Sept 2023Mofe OkoromaduNo ratings yet
- Lesson 3: Bone Growth, Remodeling, and Repair: Break A LegDocument8 pagesLesson 3: Bone Growth, Remodeling, and Repair: Break A LegEduardo SantosNo ratings yet
- Fracture Healing SsDocument2 pagesFracture Healing SsIndra SyafaatNo ratings yet
- Biology of Bone RepairDocument9 pagesBiology of Bone RepairdebbyrahmadiniNo ratings yet
- BSN1 Unit 5 Skeletal SystemDocument101 pagesBSN1 Unit 5 Skeletal SystemCherub Chua100% (1)
- Fracture HealingDocument40 pagesFracture Healingmohammad farhanNo ratings yet
- Normal Bone Anatomy and PhysiologyDocument9 pagesNormal Bone Anatomy and PhysiologyElsa GonçalvesNo ratings yet
- Skeletal SystemDocument3 pagesSkeletal SystemFrederick ManaigNo ratings yet
- Secondary Healing Occurs in Fractures Treated With Stress Sharing Devices Such As CastsDocument4 pagesSecondary Healing Occurs in Fractures Treated With Stress Sharing Devices Such As CastsYuva RajaNo ratings yet
- Ch6Bone StudentDocument66 pagesCh6Bone Studentbhattiareeba13No ratings yet
- Basic Bone BiologyDocument3 pagesBasic Bone BiologyRuxandra Maria100% (1)
- Bone Graft AssingmentDocument4 pagesBone Graft AssingmentNyein Chan AungNo ratings yet
- Ch6Bone StudentDocument67 pagesCh6Bone Studentbhattiareeba13No ratings yet
- Fractures and Bone HealingDocument39 pagesFractures and Bone HealingAndreas RendraNo ratings yet
- Anaphy AnalysisDocument6 pagesAnaphy AnalysisLuna ScorpiusNo ratings yet
- Fracture Healing: Dow University of Health SciencesDocument15 pagesFracture Healing: Dow University of Health SciencesZaheer KhanNo ratings yet
- Bone Injury and Fracture Healing Biology: ArticleDocument16 pagesBone Injury and Fracture Healing Biology: Articleali amerNo ratings yet
- Bone Graft RefrDocument58 pagesBone Graft RefrAchmadPrihadiantoNo ratings yet
- Pathological FracturesDocument48 pagesPathological FracturesHafidah RakhmatinaNo ratings yet
- Bone Growth and Factors That Associated With It1234Document7 pagesBone Growth and Factors That Associated With It1234Amanuel TarekegnNo ratings yet
- Ossification: Ossification (Or Osteogenesis) in Bone Remodeling Is TheDocument3 pagesOssification: Ossification (Or Osteogenesis) in Bone Remodeling Is TheAlan FosterNo ratings yet
- HANDOUTS Prelim CH 6Document40 pagesHANDOUTS Prelim CH 6Abia Annieson A. LorenzoNo ratings yet
- Bone RemodellingDocument8 pagesBone RemodellingAmaliaPermataBaharNo ratings yet
- Pathologic Bone FractureDocument5 pagesPathologic Bone FractureJaysellePuguonTabijeNo ratings yet
- ASYNCHRO1111Document5 pagesASYNCHRO1111Jan Vincent BallesterosNo ratings yet
- Week 6 Case StudyDocument5 pagesWeek 6 Case StudyElizabeth GithinjiNo ratings yet
- Bone Grafts, Bone Substitutes and OrthobiologicsDocument11 pagesBone Grafts, Bone Substitutes and Orthobiologicshaqqulmauludiyah_ict_ismkiNo ratings yet
- Skeletal System Lesson 2Document40 pagesSkeletal System Lesson 2Ella Nika FangonNo ratings yet
- Lo MSK 2-3Document6 pagesLo MSK 2-3FirmanHidayatNo ratings yet
- Fracture Healing: Presenter: DR Mugi Ortho ResidentDocument32 pagesFracture Healing: Presenter: DR Mugi Ortho ResidentPhoenix MerchantsNo ratings yet
- The Skeletal SystemDocument52 pagesThe Skeletal SystemrizzamaearancesNo ratings yet
- Skeletal - Break A LegDocument9 pagesSkeletal - Break A LegShannon SandersNo ratings yet
- LP 7 Connective Tissue BoneDocument3 pagesLP 7 Connective Tissue BoneAndrei TimofteNo ratings yet
- Advanced farriery knowledge: A study guide and AWCF theory course companionFrom EverandAdvanced farriery knowledge: A study guide and AWCF theory course companionNo ratings yet
- Safari - Feb 21, 2024 at 11:49 AM 2Document1 pageSafari - Feb 21, 2024 at 11:49 AM 2syansyncNo ratings yet
- Safari - Feb 21, 2024 at 12:01 PMDocument1 pageSafari - Feb 21, 2024 at 12:01 PMsyansyncNo ratings yet
- Safari - Feb 13, 2024 at 11:56 AMDocument1 pageSafari - Feb 13, 2024 at 11:56 AMsyansyncNo ratings yet
- Safari - Feb 21, 2024 at 12:16 PM 2Document1 pageSafari - Feb 21, 2024 at 12:16 PM 2syansyncNo ratings yet
- Safari - Feb 21, 2024 at 11:51 AMDocument1 pageSafari - Feb 21, 2024 at 11:51 AMsyansyncNo ratings yet
- Safari - Feb 21, 2024 at 11:58 AMDocument1 pageSafari - Feb 21, 2024 at 11:58 AMsyansyncNo ratings yet
- Safari - Feb 21, 2024 at 12:18 PM 4Document1 pageSafari - Feb 21, 2024 at 12:18 PM 4syansyncNo ratings yet
- Safari - Jan 10, 2024 at 12:25 AM PDFDocument1 pageSafari - Jan 10, 2024 at 12:25 AM PDFsyansyncNo ratings yet
- Safari - Feb 13, 2024 at 12:01 PMDocument1 pageSafari - Feb 13, 2024 at 12:01 PMsyansyncNo ratings yet
- Safari - Feb 21, 2024 at 11:56 AMDocument1 pageSafari - Feb 21, 2024 at 11:56 AMsyansyncNo ratings yet
- Safari - Feb 4, 2024 at 11:38 PMDocument1 pageSafari - Feb 4, 2024 at 11:38 PMsyansyncNo ratings yet
- Safari - Feb 21, 2024 at 11:48 AMDocument1 pageSafari - Feb 21, 2024 at 11:48 AMsyansyncNo ratings yet
- Safari - Feb 13, 2024 at 12:04 PMDocument1 pageSafari - Feb 13, 2024 at 12:04 PMsyansyncNo ratings yet
- Safari - Feb 21, 2024 at 12:17 PM 2Document1 pageSafari - Feb 21, 2024 at 12:17 PM 2syansyncNo ratings yet
- Safari - Jan 10, 2024 at 12:31 AM 2 PDFDocument1 pageSafari - Jan 10, 2024 at 12:31 AM 2 PDFsyansyncNo ratings yet
- Safari - Jan 10, 2024 at 12:31 AM PDFDocument1 pageSafari - Jan 10, 2024 at 12:31 AM PDFsyansyncNo ratings yet
- Safari - Jan 9, 2024 at 5:16 AM 3 PDFDocument1 pageSafari - Jan 9, 2024 at 5:16 AM 3 PDFsyansyncNo ratings yet
- Safari - Feb 4, 2024 at 11:39 PM 2Document1 pageSafari - Feb 4, 2024 at 11:39 PM 2syansyncNo ratings yet
- Safari - Feb 4, 2024 at 11:40 PM 3Document1 pageSafari - Feb 4, 2024 at 11:40 PM 3syansyncNo ratings yet
- Safari - Jan 10, 2024 at 12:30 AM PDFDocument1 pageSafari - Jan 10, 2024 at 12:30 AM PDFsyansyncNo ratings yet
- Safari - Jan 10, 2024 at 12:25 AM 3 PDFDocument1 pageSafari - Jan 10, 2024 at 12:25 AM 3 PDFsyansyncNo ratings yet
- Safari - Jan 10, 2024 at 12:01 AM 3 PDFDocument1 pageSafari - Jan 10, 2024 at 12:01 AM 3 PDFsyansyncNo ratings yet
- Safari - Jan 9, 2024 at 5:13 AM 3 PDFDocument1 pageSafari - Jan 9, 2024 at 5:13 AM 3 PDFsyansyncNo ratings yet
- Safari - Jan 9, 2024 at 5:19 AM 3 PDFDocument1 pageSafari - Jan 9, 2024 at 5:19 AM 3 PDFsyansyncNo ratings yet
- Safari - Jan 9, 2024 at 5:20 AM PDFDocument1 pageSafari - Jan 9, 2024 at 5:20 AM PDFsyansyncNo ratings yet
- Safari - Jan 9, 2024 at 5:18 AMDocument1 pageSafari - Jan 9, 2024 at 5:18 AMsyansyncNo ratings yet
- Safari - Jan 9, 2024 at 5:12 AM 2 PDFDocument1 pageSafari - Jan 9, 2024 at 5:12 AM 2 PDFsyansyncNo ratings yet
- Safari - Jan 9, 2024 at 5:13 AM PDFDocument1 pageSafari - Jan 9, 2024 at 5:13 AM PDFsyansyncNo ratings yet
- Safari - Jan 9, 2024 at 5:12 AM PDFDocument1 pageSafari - Jan 9, 2024 at 5:12 AM PDFsyansyncNo ratings yet
- Safari - Jan 9, 2024 at 5:18 AM 2 PDFDocument1 pageSafari - Jan 9, 2024 at 5:18 AM 2 PDFsyansyncNo ratings yet
- Upper Limb AnatomyDocument15 pagesUpper Limb AnatomyAjennyKinoNo ratings yet
- Session #16 SAS - AnaPhyDocument6 pagesSession #16 SAS - AnaPhyNicole Ken AgdanaNo ratings yet
- The Temporo - Mandibular Joint. AnatomyDocument41 pagesThe Temporo - Mandibular Joint. AnatomyZoita MandilaNo ratings yet
- Skeleton WorksheetDocument4 pagesSkeleton WorksheetNalendra UjiNo ratings yet
- GROW TALLER + Perfect Posture - Desired BodyDocument5 pagesGROW TALLER + Perfect Posture - Desired BodyJundi Abdurobih SalamNo ratings yet
- Introduction To The Human BodyDocument13 pagesIntroduction To The Human BodyDeroNo ratings yet
- Praktikum Anatomi 3 (Muscle of Head and NeckDocument36 pagesPraktikum Anatomi 3 (Muscle of Head and NeckPutriIffahNo ratings yet
- Skeletal System Study SheetsDocument6 pagesSkeletal System Study SheetsLisa P100% (1)
- Specific Osteology: Skeleton Axiale - Cranium (Skull) - Truncus (Trunk)Document46 pagesSpecific Osteology: Skeleton Axiale - Cranium (Skull) - Truncus (Trunk)Defi Sofianti AnnoNo ratings yet
- Joints of The Lower Limb DiagramsDocument39 pagesJoints of The Lower Limb Diagramssanullah123khan.13No ratings yet
- Tindakan Dan Istrument Yang DipakaiDocument3 pagesTindakan Dan Istrument Yang DipakaiToetik AryaniNo ratings yet
- Histogenesis of BoneDocument6 pagesHistogenesis of BoneAlya Putri KhairaniNo ratings yet
- Lesson Plan SKELETAL SYSTEMDocument11 pagesLesson Plan SKELETAL SYSTEMpoonamNo ratings yet
- Handouts in Skeletal SystemDocument6 pagesHandouts in Skeletal SystemShiela Mae EslumNo ratings yet
- Complete Guide To Core StabilityDocument212 pagesComplete Guide To Core StabilityLynseyNo ratings yet
- Summary of Head DR - Ihab - 3Document41 pagesSummary of Head DR - Ihab - 3ايمان عبد الشافى100% (1)
- Surgical Tips and Tricks For Distal Femur Plating.2Document10 pagesSurgical Tips and Tricks For Distal Femur Plating.2jojoNo ratings yet
- Prepared By:: Ma. Kristina G. CristobalDocument17 pagesPrepared By:: Ma. Kristina G. CristobalDiovy TahilanNo ratings yet
- OIA Muscles of The CatDocument3 pagesOIA Muscles of The CatAyee AtienzaNo ratings yet
- Lytic Bone Lesions - StatPearls - NCBI BookshelfDocument9 pagesLytic Bone Lesions - StatPearls - NCBI Bookshelfjuan ricardo carvajal alvaradoNo ratings yet
- Musculoskeletal SystemDocument316 pagesMusculoskeletal SystemPrincess Averin NavarroNo ratings yet
- Muscoloskeletal - System - Medical TerminologyDocument11 pagesMuscoloskeletal - System - Medical Terminologymaglit777No ratings yet
- ManualDocument95 pagesManualcristina_c_43No ratings yet
- ملزمة احياء جميع الفصولDocument178 pagesملزمة احياء جميع الفصولمحمدNo ratings yet
- Pilates For KyphosisDocument13 pagesPilates For KyphosisAnonymous NKGMQv9100% (1)
- Skeleton of The SharkDocument12 pagesSkeleton of The SharkJoachimNo ratings yet
- Ultrasound-Guided Lumbar Central Neuraxial Block 2016Document8 pagesUltrasound-Guided Lumbar Central Neuraxial Block 2016drkis20100% (1)
- Human Skeletal SystemDocument3 pagesHuman Skeletal Systemahmei100% (1)
- ArticulationsDocument36 pagesArticulationsLisaNo ratings yet
- AOS Injury Classification Systems Poster 20200327 SUBAXIALDocument1 pageAOS Injury Classification Systems Poster 20200327 SUBAXIALReyhan AristoNo ratings yet
Safari - Feb 21, 2024 at 12:17 PM 3
Safari - Feb 21, 2024 at 12:17 PM 3
Uploaded by
syansyncOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Safari - Feb 21, 2024 at 12:17 PM 3
Safari - Feb 21, 2024 at 12:17 PM 3
Uploaded by
syansyncCopyright:
Available Formats
Search Wikipedia
Bone healing
Article Talk
Bone healing, or fracture healing, is a proliferative physiological process in which the body facilitates
the repair of a bone fracture.
Generally, bone fracture treatment consists of a doctor reducing
(pushing) displaced bones back into place via relocation with or
without anaesthetic, stabilizing their position to aid union, and then
waiting for the bone's natural healing process to occur.
Adequate nutrient intake has been found to significantly affect the
integrity of the fracture repair.[1] Age, bone type, drug therapy and
pre-existing bone pathology are factors that affect healing. The role
of bone healing is to produce new bone without a scar as seen in
other tissues which would be a structural weakness or deformity.[2]
The process of the entire regeneration of the bone can depend on
the angle of dislocation or fracture. While the bone formation usually
spans the entire duration of the healing process, in some instances,
bone marrow within the fracture has healed two or fewer weeks
before the final remodelling phase.[citation needed]
Bone healing of a fracture by
While immobilization and surgery may facilitate healing, a fracture forming a callus as shown by X-ray.
ultimately heals through physiological processes. The healing
process is mainly determined by the periosteum (the connective tissue membrane covering the bone).
The periosteum is one source of precursor cells that develop into chondroblasts and osteoblasts that
are essential to the healing of bone. Other sources of precursor cells are the bone marrow (when
present), endosteum, small blood vessels, and fibroblasts.[3]
Contents
Primary healing
Contact healing
Gap healing
Secondary healing
Reaction
Repair
Remodelling
Obstructions
Complications
Gallery
Radiologic timeline in young children
Footnotes
References
Primary healing
Primary healing (also known as direct healing) requires a correct anatomical reduction which is stable,
without any gap formation. Such healing requires only the remodeling of lamellar bone, the Haversian
canals and the blood vessels without callus formation. This process may take a few months to a few
years.[4]
Contact healing
When the gap between the bone ends is less than 0.01 mm, and interfragmentary strain is less than
2%, contact healing can occur. In this case, cutting cones, which consists of osteoclasts, form across
the fracture lines, generating cavities at a rate of 50–100 µm/day. Osteoblasts fill up the cavities with
the Haversian system. This causes the formation of lamellar bone that orients longitudinally along the
long axis of the bone. Blood vessels form that penetrate the Haversian system. Remodelling of lamellar
bone results in healing without callus formation.[4]
Gap healing
If the fracture gap is 800 µm to 1 mm, the fracture is filled by osteoblasts and then by lamellar bone
oriented perpendicular to the axis of the bone. This initial process takes three to eight weeks.
Perpendicular orientation of lamellar bone is weak, thus a secondary osteonal reconstruction is
required to re-orient the lamellar bone longitudinally.[4]
Secondary healing
Secondary healing (also known as indirect fracture healing) is the most common form of bone healing.
It usually consists of only endochondral ossification. Sometimes, intramembranous ossification occurs
together with endochondral ossification. Intramembranous ossification, mediated by the periosteal
layer of bone, occurs with the formation of callus. For endochondral ossification, deposition of bone
only occurs after the mineralised cartilage.[citation needed] This process of healing occurs when the
fracture is treated conservatively using orthopaedic cast or immobilisation, external fixation, or
internal fixation.[4]
Reaction
After bone fracture, blood cells accumulate adjacent to the injury site. Soon after fracture, blood
vessels constrict, stopping further bleeding. Within a few hours, the extravascular blood cells form a
clot called a hematoma[5] that acts as a template for callus formation. These cells, including
macrophages, release inflammatory mediators such as cytokines (tumor necrosis factor alpha (TNFα),
interleukin-1 family (IL-1), interleukin 6 (IL-6), 11 (IL-11), and 18 (IL-18)) and increase blood capillary
permeability. Inflammation peaks by 24 hours and completes by seven days. Through tumor necrosis
factor receptor 1 (TNFR1) and tumor necrosis factor receptor 2, TNFα mediates the differentiation of
mesenchymal stem cell (originated from the bone marrow) into osteoblast and chondrocytes. Stromal
cell-derived factor 1 (SDF-1) and CXCR4 mediate recruitment of mesenchymal stem cells. IL-1 and IL-6
are the most important cytokines for bone healing. IL-1 promotes formation of callus and of blood
vessels. IL-6 promotes differentiation of osteoblasts and osteoclasts.[4] All cells within the blood clot
degenerate and die. Within this area, the fibroblasts replicate. Within 7–14 days, they form a loose
aggregate of cells, interspersed with small blood vessels, known as granulation tissue.[citation needed]
Osteoclasts move in to reabsorb dead bone ends, and other necrotic tissue is removed.[6]
Repair
Seven to nine days after fracture, the cells of the periosteum
replicate and transform. The periosteal cells proximal to (on the
near side of) the fracture gap develop into chondroblasts, which
form hyaline cartilage. The periosteal cells distal to (at the far end
of) the fracture gap develop into osteoblasts, which form woven
bone[citation needed] through bone resorption of calcified cartilage
and recruitment of bone cells and osteoclasts.[4] The fibroblasts
within the granulation tissue develop into chondroblasts which
also form hyaline cartilage. These two new tissues grow in size Radiolucency around a 12-day-old
until they unite with each other. These processes culminate in a scaphoid fracture that was initially
barely visible.[7]
new mass of heterogeneous tissue known as a fracture
callus[citation needed] Callus formation peaks at day 14 of fracture.[4] Eventually, the fracture gap is
bridged[citation needed]
The next phase is the replacement of the hyaline cartilage and woven bone with lamellar bone. The
replacement process is known as endochondral ossification with respect to the hyaline cartilage and
bony substitution with respect to the woven bone. Substitution of woven bone happens before
substitution of hyaline cartilage. The lamellar bone begins forming soon after the collagen matrix of
either tissue becomes mineralized[citation needed] At this stage, the process is induced by IL-1 and
TNFα.[4] The mineralized matrix is penetrated by microvessel and numerous osteoblasts. The
osteoblasts form new lamellar bone upon the recently exposed surface of the mineralized matrix. This
new lamellar bone is in the form of trabecular bone. Eventually, all of the woven bone and cartilage of
the original fracture callus is replaced by trabecular bone, restoring most of the bone's original
strength[citation needed]
Remodelling
Remodeling begins as early as three to four weeks after fracture and may take 3 to 5 years to
complete.[4] The process substitutes the trabecular bone with compact bone. The trabecular bone is
first resorbed by osteoclasts, creating a shallow resorption pit known as a "Howship's lacuna". Then
osteoblasts deposit compact bone within the resorption pit. Eventually, the fracture callus is
remodelled into a new shape which closely duplicates the bone's original shape and strength. This
process can be achieved by the formation of electrical polarity during partial weight bearing a long
bone;[citation needed] where electropositive convex surface and electronegative concave surface
activates osteoclasts and osteoblasts respectively.[4] This process can be enhanced by certain
synthetic injectable biomaterials, such as Cerament, which are osteoconductive and promote bone
healing[citation needed]
Obstructions
1. Poor blood supply which leads to the death of the osteocytes.
Bone cell death also depends on degree of fracture and
disruption to the Haversian system.
2. Condition of the soft tissues. Soft tissue between bone ends
restricts healing.
3. Nutrition and drug therapy. Poor general health reduces healing
rate. Drugs that impair the inflammatory response impede
healing also.
Femur (top) healed while improperly
4. Infection. Diverts the inflammatory response away from healing aligned
towards fighting off the infection.
5. Age. Young bone unites more rapidly than adult bone.
6. Pre-existing bone malignancy.
7. Mechanical factors such as the bone not being aligned, and too much or too little movement. Excess
mobility can disrupt the bridging callus, interfering with union; but slight biomechanical motion is seen
to improve callus formation.[6]
Complications
Complications of fracture healing include:
1. Infection: this is the most common complication of fractures and predominantly occurs in open
fractures. Post-traumatic wound infection is the most common cause of chronic osteomyelitis in
patients. Osteomyelitis can also occur following surgical fixation of a fracture.[8]
2. Non-union: no progression of healing within six months of a fracture occurring. The fracture pieces
remain separated and can be caused by infection and/or lack of blood supply (Ischaemia) to the
bone.[9] There are two types of non-union, atrophic and hypertrophic. Hypertrophic involves the
formation of excess callus leading to bone ends appearing sclerotic causing a radiological "Elephants
Foot" appearance[6] due to excessive fracture ends mobility but adequate blood supply.[4] Atrophic
non-union results in re-absorption and rounding of bone ends[6] due to inadequate blood supply and
excessive mobility of the bone ends.[4]
3. Mal-union: healing occurs but the healed bone has 'angular deformity, translation, or rotational
alignment that requires surgical correction'. This is most common in long bones such as the femur.[10]
4. Delayed union: healing times vary depending on the location of a fracture and the age of a patient.
Delayed union is characterised by 'persistence of the fracture line and a scarcity or absence of callus
formation' on x-ray. Healing is still occurring but at a much slower rate than normal.[9]
Gallery
Collagen fibers of woven Osteoclast displaying Light micrograph of
bone many nuclei within its decalcified cancellous
"foamy" cytoplasm. bone displaying
osteoblasts forming new
bone tissue, containing
two osteocytes, within a
resorption pit.
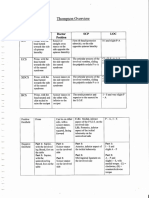
Radiologic timeline in young children
On medical imaging, secondary bone healing displays the following features over time in young
children:
Features and when they appear (and percentage of
individuals having the feature in that period or at that time
point)[11]
Resolution of soft tissues 7–10 days (or 2–21 days)
Gap widening 4–6 weeks (56%)
Periosteal reaction 7 days – 7 weeks
Marginal sclerosis 4–6 weeks (85%)
First callus 4–7 weeks (100%)
Radiodensity of callus > cortex 13 weeks (90%)
Bridging callus 2.6 – 13 weeks
Periosteal incorporation 14 weeks
Remodeling 9 weeks (50%)
Footnotes
1. ^ Karpouzos, A.; Diamantis, E.; Farmaki, P.;
8. ^ Rowbotham, Emma; Barron, Dominic (2009).
Savvanis, S.; Troupis, T. (2017). "Nutritional
"Radiology of fracture complications". Orthopaedics
Aspects of Bone Health and Fracture Healing" .
and Trauma. 23 (1): 52–60.
Journal of Osteoporosis. 2017: 1–10.
doi:10.1016/j.mporth.2008.12.008 .
doi:10.1155/2017/4218472 . PMC 5804294 .
PMID 29464131 . 9. ^ a b
Jahagirdar, Rajeev; Scammell, Brigitte E
(2008). "Principles of fracture healing and
2. ^ Gomez-Barrena E, Rosset P, Lozano D, Stanovici
disorders of bone union". Surgery. 27 (2): 63–69.
J, Ermthaller C, Gerbhard F. Bone fracture healing:
doi:10.1016/j.mpsur.2008.12.011 .
Cell therapy in delayed unions and nonunions.
Bone. 2015;70:93–101. 10. ^ Chen, Andrew T; Vallier, Heather A (2016).
"Noncontiguous and open fractures of the lower
3. ^ Ferretti C, Mattioli-Belmonte M. Periosteum
extremity: Epidemiology, complications, and
derived stem cells for regenerative medicine
unplanned procedures". Injury. 47 (3): 742–747.
proposals: Boosting current knowledge. World
doi:10.1016/j.injury.2015.12.013 .
Journal of Stem Cells. 2014;6(3):266-277.
PMID 26776462 .
doi:10.4252/wjsc.v6.i3.266.
11. ^ Unless otherwise specified in boxes, reference is:
4. ^ a b c d e f g h i j k l
Richard, Marsell; Thomas A,
- Prosser, Ingrid; Lawson, Zoe; Evans, Alison;
Einhorn (1 June 2012). "The biology of fracture
Harrison, Sara; Morris, Sue; Maguire, Sabine; Kemp,
healing" . Injury. 42 (6): 551–555.
Alison M. (2012). "A Timetable for the Radiologic
doi:10.1016/j.injury.2011.03.031 . PMC 3105171 .
Features of Fracture Healing in Young Children" .
PMID 21489527 .
American Journal of Roentgenology. 198 (5): 1014–
5. ^ "Overview of Bone Fractures" . The Lecturio 1020. doi:10.2214/AJR.11.6734 . ISSN 0361-
Medical Concept Library. Retrieved 26 August 2021. 803X . PMID 22528890 .
- Data is taken from scientific studies, notably Islam
6. ^ a b c d
Nyary Tamas, Scamell BE. (2015).
et al. where data is contradictory to radiology
Principles of bone and joint injuries and their
textbooks:
healing. Surgery(Oxford). 33 (1), p 7-14.
Islam, Omar; Soboleski, Don; Symons, S.; Davidson,
7. ^ Jarraya, Mohamed; Hayashi, Daichi; Roemer, L. K.; Ashworth, M. A.; Babyn, Paul (2000).
Frank W.; Crema, Michel D.; Diaz, Luis; Conlin, "Development and Duration of Radiographic Signs
Jane; Marra, Monica D.; Jomaah, Nabil; Guermazi, of Bone Healing in Children". American Journal of
Ali (2013). "Radiographically Occult and Subtle Roentgenology. 175 (1): 75–78.
Fractures: A Pictorial Review" . Radiology doi:10.2214/ajr.175.1.1750075 . ISSN 0361-
Research and Practice. 2013: 1–10. 803X . PMID 10882250 .
doi:10.1155/2013/370169 . ISSN 2090-1941 .
PMC 3613077 . PMID 23577253 . CC-BY 3.0
References
Brighton, Carl T. and Robert M. Hunt (1986), "Histochemical localization of calcium in the fracture callus
with potassium pyroantimonate: possible role of chondrocyte mitochondrial calcium in callus
calcification", Journal of Bone and Joint Surgery, 68-A (5): 703-715
Brighton, Carl T. and Robert M. Hunt (1991), "Early histologic and ultrastructural changes in medullary
fracture callus", Journal of Bone and Joint Surgery, 73-A (6): 832-847
Brighton, Carl T. and Robert M. Hunt (1997), "Early histologic and ultrastructural changes in microvessels
of periosteal callus", Journal of Orthopaedic Trauma, 11 (4): 244-253
Ham, Arthur W. and William R. Harris (1972), "Repair and transplantation of bone", The biochemistry and
physiology of bone, New York: Academic Press, p. 337-399
Last edited on 25 December 2023, at 02:45
Content is available under CC BY-SA 4.0 unless otherwise noted.
Terms of Use • Privacy policy • Desktop
:
You might also like
- Bone Development and Growth: Rosy Setiawati and Paulus RahardjoDocument20 pagesBone Development and Growth: Rosy Setiawati and Paulus Rahardjoputri aishe100% (1)
- Fracture Healing in Cortical and Cancellous BoneDocument63 pagesFracture Healing in Cortical and Cancellous BonePramod Thottimane0% (1)
- Bones As A Living Dynamic TissueDocument13 pagesBones As A Living Dynamic TissueSanish Basnet100% (1)
- Fracture Healing and BonegraftingDocument76 pagesFracture Healing and BonegraftingJio AmurNo ratings yet
- Stages of Bone HealingDocument2 pagesStages of Bone HealingArra Beatriz100% (1)
- Dr. Sassia Lecture Bone Histology Part II July 4 2023Document39 pagesDr. Sassia Lecture Bone Histology Part II July 4 2023Ali ELKARGHALYNo ratings yet
- Bone HealingDocument5 pagesBone HealingFadliArifNo ratings yet
- Lec. 4 Bone FractureDocument11 pagesLec. 4 Bone Fracturebtwlalbwdy16No ratings yet
- Distraction OsteogenesisDocument141 pagesDistraction OsteogenesisJohan Edward Franklin MarpaungNo ratings yet
- AO Surgery ReferenceDocument8 pagesAO Surgery ReferenceHurulaeniNo ratings yet
- Orthopaedics DocumentDocument131 pagesOrthopaedics DocumentRazvan NegritasNo ratings yet
- Alveolarbone Graftingand Reconstruction Procedurespriorto ImplantplacementDocument10 pagesAlveolarbone Graftingand Reconstruction Procedurespriorto ImplantplacementKranti PrajapatiNo ratings yet
- Fracture HealingDocument22 pagesFracture Healingsumitbhosale3No ratings yet
- Fracture Healing and FactorsDocument29 pagesFracture Healing and FactorsVivek ChNo ratings yet
- FRACTURESDocument85 pagesFRACTURESSteven OdhiamboNo ratings yet
- Bridging Technique and Science A Review of The Molecular Sig - 2022 - OrthoplasDocument7 pagesBridging Technique and Science A Review of The Molecular Sig - 2022 - OrthoplasAlex Rolando Suntaxi LlumiquingaNo ratings yet
- Principles of Bone GraftingDocument6 pagesPrinciples of Bone GraftingJayanth Perumal100% (2)
- Normal Bone Anatomy and Physiology: Go ToDocument11 pagesNormal Bone Anatomy and Physiology: Go TotariNo ratings yet
- Fix. Musculosceletal Anatomy (DR - Hendra)Document33 pagesFix. Musculosceletal Anatomy (DR - Hendra)rumah sakit daerahNo ratings yet
- 1 2009-Principles of Fracture Healing and Disorders of Bone UnionDocument7 pages1 2009-Principles of Fracture Healing and Disorders of Bone UnionRodrigo ValderramaNo ratings yet
- Week 6 Bone Case StudyDocument7 pagesWeek 6 Bone Case StudyAndriNo ratings yet
- What Is A FractureDocument4 pagesWhat Is A FracturemidskiescreamzNo ratings yet
- DR Himanshu Gaur: Consultant Orthopaedic, Joint Replacement & Arthroscopy (Sports Injury) Surgeon BCIMS, New DelhiDocument34 pagesDR Himanshu Gaur: Consultant Orthopaedic, Joint Replacement & Arthroscopy (Sports Injury) Surgeon BCIMS, New DelhiAnjani Kumar JhaNo ratings yet
- A Brief Introduction Into Orthopaedic ImplantsDocument20 pagesA Brief Introduction Into Orthopaedic ImplantsLuisAngelPonceTorresNo ratings yet
- TARI ReferensiDocument13 pagesTARI ReferensitariNo ratings yet
- Fractures and Fracture Healing Lecture 22422 Sept 2023Document25 pagesFractures and Fracture Healing Lecture 22422 Sept 2023Mofe OkoromaduNo ratings yet
- Lesson 3: Bone Growth, Remodeling, and Repair: Break A LegDocument8 pagesLesson 3: Bone Growth, Remodeling, and Repair: Break A LegEduardo SantosNo ratings yet
- Fracture Healing SsDocument2 pagesFracture Healing SsIndra SyafaatNo ratings yet
- Biology of Bone RepairDocument9 pagesBiology of Bone RepairdebbyrahmadiniNo ratings yet
- BSN1 Unit 5 Skeletal SystemDocument101 pagesBSN1 Unit 5 Skeletal SystemCherub Chua100% (1)
- Fracture HealingDocument40 pagesFracture Healingmohammad farhanNo ratings yet
- Normal Bone Anatomy and PhysiologyDocument9 pagesNormal Bone Anatomy and PhysiologyElsa GonçalvesNo ratings yet
- Skeletal SystemDocument3 pagesSkeletal SystemFrederick ManaigNo ratings yet
- Secondary Healing Occurs in Fractures Treated With Stress Sharing Devices Such As CastsDocument4 pagesSecondary Healing Occurs in Fractures Treated With Stress Sharing Devices Such As CastsYuva RajaNo ratings yet
- Ch6Bone StudentDocument66 pagesCh6Bone Studentbhattiareeba13No ratings yet
- Basic Bone BiologyDocument3 pagesBasic Bone BiologyRuxandra Maria100% (1)
- Bone Graft AssingmentDocument4 pagesBone Graft AssingmentNyein Chan AungNo ratings yet
- Ch6Bone StudentDocument67 pagesCh6Bone Studentbhattiareeba13No ratings yet
- Fractures and Bone HealingDocument39 pagesFractures and Bone HealingAndreas RendraNo ratings yet
- Anaphy AnalysisDocument6 pagesAnaphy AnalysisLuna ScorpiusNo ratings yet
- Fracture Healing: Dow University of Health SciencesDocument15 pagesFracture Healing: Dow University of Health SciencesZaheer KhanNo ratings yet
- Bone Injury and Fracture Healing Biology: ArticleDocument16 pagesBone Injury and Fracture Healing Biology: Articleali amerNo ratings yet
- Bone Graft RefrDocument58 pagesBone Graft RefrAchmadPrihadiantoNo ratings yet
- Pathological FracturesDocument48 pagesPathological FracturesHafidah RakhmatinaNo ratings yet
- Bone Growth and Factors That Associated With It1234Document7 pagesBone Growth and Factors That Associated With It1234Amanuel TarekegnNo ratings yet
- Ossification: Ossification (Or Osteogenesis) in Bone Remodeling Is TheDocument3 pagesOssification: Ossification (Or Osteogenesis) in Bone Remodeling Is TheAlan FosterNo ratings yet
- HANDOUTS Prelim CH 6Document40 pagesHANDOUTS Prelim CH 6Abia Annieson A. LorenzoNo ratings yet
- Bone RemodellingDocument8 pagesBone RemodellingAmaliaPermataBaharNo ratings yet
- Pathologic Bone FractureDocument5 pagesPathologic Bone FractureJaysellePuguonTabijeNo ratings yet
- ASYNCHRO1111Document5 pagesASYNCHRO1111Jan Vincent BallesterosNo ratings yet
- Week 6 Case StudyDocument5 pagesWeek 6 Case StudyElizabeth GithinjiNo ratings yet
- Bone Grafts, Bone Substitutes and OrthobiologicsDocument11 pagesBone Grafts, Bone Substitutes and Orthobiologicshaqqulmauludiyah_ict_ismkiNo ratings yet
- Skeletal System Lesson 2Document40 pagesSkeletal System Lesson 2Ella Nika FangonNo ratings yet
- Lo MSK 2-3Document6 pagesLo MSK 2-3FirmanHidayatNo ratings yet
- Fracture Healing: Presenter: DR Mugi Ortho ResidentDocument32 pagesFracture Healing: Presenter: DR Mugi Ortho ResidentPhoenix MerchantsNo ratings yet
- The Skeletal SystemDocument52 pagesThe Skeletal SystemrizzamaearancesNo ratings yet
- Skeletal - Break A LegDocument9 pagesSkeletal - Break A LegShannon SandersNo ratings yet
- LP 7 Connective Tissue BoneDocument3 pagesLP 7 Connective Tissue BoneAndrei TimofteNo ratings yet
- Advanced farriery knowledge: A study guide and AWCF theory course companionFrom EverandAdvanced farriery knowledge: A study guide and AWCF theory course companionNo ratings yet
- Safari - Feb 21, 2024 at 11:49 AM 2Document1 pageSafari - Feb 21, 2024 at 11:49 AM 2syansyncNo ratings yet
- Safari - Feb 21, 2024 at 12:01 PMDocument1 pageSafari - Feb 21, 2024 at 12:01 PMsyansyncNo ratings yet
- Safari - Feb 13, 2024 at 11:56 AMDocument1 pageSafari - Feb 13, 2024 at 11:56 AMsyansyncNo ratings yet
- Safari - Feb 21, 2024 at 12:16 PM 2Document1 pageSafari - Feb 21, 2024 at 12:16 PM 2syansyncNo ratings yet
- Safari - Feb 21, 2024 at 11:51 AMDocument1 pageSafari - Feb 21, 2024 at 11:51 AMsyansyncNo ratings yet
- Safari - Feb 21, 2024 at 11:58 AMDocument1 pageSafari - Feb 21, 2024 at 11:58 AMsyansyncNo ratings yet
- Safari - Feb 21, 2024 at 12:18 PM 4Document1 pageSafari - Feb 21, 2024 at 12:18 PM 4syansyncNo ratings yet
- Safari - Jan 10, 2024 at 12:25 AM PDFDocument1 pageSafari - Jan 10, 2024 at 12:25 AM PDFsyansyncNo ratings yet
- Safari - Feb 13, 2024 at 12:01 PMDocument1 pageSafari - Feb 13, 2024 at 12:01 PMsyansyncNo ratings yet
- Safari - Feb 21, 2024 at 11:56 AMDocument1 pageSafari - Feb 21, 2024 at 11:56 AMsyansyncNo ratings yet
- Safari - Feb 4, 2024 at 11:38 PMDocument1 pageSafari - Feb 4, 2024 at 11:38 PMsyansyncNo ratings yet
- Safari - Feb 21, 2024 at 11:48 AMDocument1 pageSafari - Feb 21, 2024 at 11:48 AMsyansyncNo ratings yet
- Safari - Feb 13, 2024 at 12:04 PMDocument1 pageSafari - Feb 13, 2024 at 12:04 PMsyansyncNo ratings yet
- Safari - Feb 21, 2024 at 12:17 PM 2Document1 pageSafari - Feb 21, 2024 at 12:17 PM 2syansyncNo ratings yet
- Safari - Jan 10, 2024 at 12:31 AM 2 PDFDocument1 pageSafari - Jan 10, 2024 at 12:31 AM 2 PDFsyansyncNo ratings yet
- Safari - Jan 10, 2024 at 12:31 AM PDFDocument1 pageSafari - Jan 10, 2024 at 12:31 AM PDFsyansyncNo ratings yet
- Safari - Jan 9, 2024 at 5:16 AM 3 PDFDocument1 pageSafari - Jan 9, 2024 at 5:16 AM 3 PDFsyansyncNo ratings yet
- Safari - Feb 4, 2024 at 11:39 PM 2Document1 pageSafari - Feb 4, 2024 at 11:39 PM 2syansyncNo ratings yet
- Safari - Feb 4, 2024 at 11:40 PM 3Document1 pageSafari - Feb 4, 2024 at 11:40 PM 3syansyncNo ratings yet
- Safari - Jan 10, 2024 at 12:30 AM PDFDocument1 pageSafari - Jan 10, 2024 at 12:30 AM PDFsyansyncNo ratings yet
- Safari - Jan 10, 2024 at 12:25 AM 3 PDFDocument1 pageSafari - Jan 10, 2024 at 12:25 AM 3 PDFsyansyncNo ratings yet
- Safari - Jan 10, 2024 at 12:01 AM 3 PDFDocument1 pageSafari - Jan 10, 2024 at 12:01 AM 3 PDFsyansyncNo ratings yet
- Safari - Jan 9, 2024 at 5:13 AM 3 PDFDocument1 pageSafari - Jan 9, 2024 at 5:13 AM 3 PDFsyansyncNo ratings yet
- Safari - Jan 9, 2024 at 5:19 AM 3 PDFDocument1 pageSafari - Jan 9, 2024 at 5:19 AM 3 PDFsyansyncNo ratings yet
- Safari - Jan 9, 2024 at 5:20 AM PDFDocument1 pageSafari - Jan 9, 2024 at 5:20 AM PDFsyansyncNo ratings yet
- Safari - Jan 9, 2024 at 5:18 AMDocument1 pageSafari - Jan 9, 2024 at 5:18 AMsyansyncNo ratings yet
- Safari - Jan 9, 2024 at 5:12 AM 2 PDFDocument1 pageSafari - Jan 9, 2024 at 5:12 AM 2 PDFsyansyncNo ratings yet
- Safari - Jan 9, 2024 at 5:13 AM PDFDocument1 pageSafari - Jan 9, 2024 at 5:13 AM PDFsyansyncNo ratings yet
- Safari - Jan 9, 2024 at 5:12 AM PDFDocument1 pageSafari - Jan 9, 2024 at 5:12 AM PDFsyansyncNo ratings yet
- Safari - Jan 9, 2024 at 5:18 AM 2 PDFDocument1 pageSafari - Jan 9, 2024 at 5:18 AM 2 PDFsyansyncNo ratings yet
- Upper Limb AnatomyDocument15 pagesUpper Limb AnatomyAjennyKinoNo ratings yet
- Session #16 SAS - AnaPhyDocument6 pagesSession #16 SAS - AnaPhyNicole Ken AgdanaNo ratings yet
- The Temporo - Mandibular Joint. AnatomyDocument41 pagesThe Temporo - Mandibular Joint. AnatomyZoita MandilaNo ratings yet
- Skeleton WorksheetDocument4 pagesSkeleton WorksheetNalendra UjiNo ratings yet
- GROW TALLER + Perfect Posture - Desired BodyDocument5 pagesGROW TALLER + Perfect Posture - Desired BodyJundi Abdurobih SalamNo ratings yet
- Introduction To The Human BodyDocument13 pagesIntroduction To The Human BodyDeroNo ratings yet
- Praktikum Anatomi 3 (Muscle of Head and NeckDocument36 pagesPraktikum Anatomi 3 (Muscle of Head and NeckPutriIffahNo ratings yet
- Skeletal System Study SheetsDocument6 pagesSkeletal System Study SheetsLisa P100% (1)
- Specific Osteology: Skeleton Axiale - Cranium (Skull) - Truncus (Trunk)Document46 pagesSpecific Osteology: Skeleton Axiale - Cranium (Skull) - Truncus (Trunk)Defi Sofianti AnnoNo ratings yet
- Joints of The Lower Limb DiagramsDocument39 pagesJoints of The Lower Limb Diagramssanullah123khan.13No ratings yet
- Tindakan Dan Istrument Yang DipakaiDocument3 pagesTindakan Dan Istrument Yang DipakaiToetik AryaniNo ratings yet
- Histogenesis of BoneDocument6 pagesHistogenesis of BoneAlya Putri KhairaniNo ratings yet
- Lesson Plan SKELETAL SYSTEMDocument11 pagesLesson Plan SKELETAL SYSTEMpoonamNo ratings yet
- Handouts in Skeletal SystemDocument6 pagesHandouts in Skeletal SystemShiela Mae EslumNo ratings yet
- Complete Guide To Core StabilityDocument212 pagesComplete Guide To Core StabilityLynseyNo ratings yet
- Summary of Head DR - Ihab - 3Document41 pagesSummary of Head DR - Ihab - 3ايمان عبد الشافى100% (1)
- Surgical Tips and Tricks For Distal Femur Plating.2Document10 pagesSurgical Tips and Tricks For Distal Femur Plating.2jojoNo ratings yet
- Prepared By:: Ma. Kristina G. CristobalDocument17 pagesPrepared By:: Ma. Kristina G. CristobalDiovy TahilanNo ratings yet
- OIA Muscles of The CatDocument3 pagesOIA Muscles of The CatAyee AtienzaNo ratings yet
- Lytic Bone Lesions - StatPearls - NCBI BookshelfDocument9 pagesLytic Bone Lesions - StatPearls - NCBI Bookshelfjuan ricardo carvajal alvaradoNo ratings yet
- Musculoskeletal SystemDocument316 pagesMusculoskeletal SystemPrincess Averin NavarroNo ratings yet
- Muscoloskeletal - System - Medical TerminologyDocument11 pagesMuscoloskeletal - System - Medical Terminologymaglit777No ratings yet
- ManualDocument95 pagesManualcristina_c_43No ratings yet
- ملزمة احياء جميع الفصولDocument178 pagesملزمة احياء جميع الفصولمحمدNo ratings yet
- Pilates For KyphosisDocument13 pagesPilates For KyphosisAnonymous NKGMQv9100% (1)
- Skeleton of The SharkDocument12 pagesSkeleton of The SharkJoachimNo ratings yet
- Ultrasound-Guided Lumbar Central Neuraxial Block 2016Document8 pagesUltrasound-Guided Lumbar Central Neuraxial Block 2016drkis20100% (1)
- Human Skeletal SystemDocument3 pagesHuman Skeletal Systemahmei100% (1)
- ArticulationsDocument36 pagesArticulationsLisaNo ratings yet
- AOS Injury Classification Systems Poster 20200327 SUBAXIALDocument1 pageAOS Injury Classification Systems Poster 20200327 SUBAXIALReyhan AristoNo ratings yet