Professional Documents
Culture Documents
Safari - Feb 21, 2024 at 12:04 PM
Safari - Feb 21, 2024 at 12:04 PM
Uploaded by
syansyncCopyright:
Available Formats
You might also like
- Fitzpatricks Dermatology in General Medicine 8edDocument3,190 pagesFitzpatricks Dermatology in General Medicine 8edFauzul Azmi96% (74)
- Flexi Master Series Mock-1 SolutionDocument96 pagesFlexi Master Series Mock-1 SolutionYugal0% (1)
- Antiaging Efficacy of A Retinaldehyde-Based Cream Compared With Glycolic Acid Peel Sessions: A Randomized Controlled StudyDocument8 pagesAntiaging Efficacy of A Retinaldehyde-Based Cream Compared With Glycolic Acid Peel Sessions: A Randomized Controlled Studypermen_lollypopzNo ratings yet
- Wnofns 43 (2022) 11-37Document27 pagesWnofns 43 (2022) 11-37Dennis StwnNo ratings yet
- Anatomy, Skin (Integument) - StatPearls - NCBI BookshelfDocument4 pagesAnatomy, Skin (Integument) - StatPearls - NCBI Bookshelfputri aisheNo ratings yet
- Safari - Feb 21, 2024 at 11:56 AMDocument1 pageSafari - Feb 21, 2024 at 11:56 AMsyansyncNo ratings yet
- Skin Examination 1Document17 pagesSkin Examination 1Daffa AmaliaNo ratings yet
- Structure of SkinDocument129 pagesStructure of SkinDeepak BaliyanNo ratings yet
- Chapter 4: Examination of The Skin, Coat and Associated StructuresDocument19 pagesChapter 4: Examination of The Skin, Coat and Associated StructuresZekarias GetachewNo ratings yet
- Canine Ichthyosis and Related Disorders of CornificationDocument9 pagesCanine Ichthyosis and Related Disorders of CornificationPaolaNo ratings yet
- Modul 1 (No: 1-3) Anggota KelompokDocument33 pagesModul 1 (No: 1-3) Anggota KelompokfrostedsurgeonNo ratings yet
- Tissue Integrity Outline Spring 2023Document25 pagesTissue Integrity Outline Spring 2023morganstorey0No ratings yet
- Project Topic: Skin Prepared By: (1) Ankita Chavda (2) Krupali Tandel (F.Y. B.PT. Students)Document55 pagesProject Topic: Skin Prepared By: (1) Ankita Chavda (2) Krupali Tandel (F.Y. B.PT. Students)shivaniNo ratings yet
- The Integumentary SystemDocument4 pagesThe Integumentary SystemKhan Hayudini SaliNo ratings yet
- The Integumentary System Activity No. 12Document4 pagesThe Integumentary System Activity No. 12Khan Hayudini SaliNo ratings yet
- 2017 - Tecnología CosméticaDocument54 pages2017 - Tecnología CosméticaCésar Rosado Avila ToñoNo ratings yet
- Integumentary SystemDocument13 pagesIntegumentary Systemleih jsNo ratings yet
- Integumentary System: Chapter OutlineDocument7 pagesIntegumentary System: Chapter OutlineRiy KimNo ratings yet
- Safari - Feb 21, 2024 at 11:48 AMDocument1 pageSafari - Feb 21, 2024 at 11:48 AMsyansyncNo ratings yet
- Dissertation LeucodermaDocument90 pagesDissertation LeucodermaRashmi Mishra100% (1)
- GENOVE, ERICKA IS-Module2Document11 pagesGENOVE, ERICKA IS-Module2Ericka GenoveNo ratings yet
- IJCRT2310623Document18 pagesIJCRT2310623roseNo ratings yet
- Mechanisms and Causes of Scalp ScalingDocument5 pagesMechanisms and Causes of Scalp ScalingAdrianeNo ratings yet
- Superficial and Medium-Depth Chemical PeelsDocument10 pagesSuperficial and Medium-Depth Chemical PeelsFenni Oktoberry100% (1)
- Isi RefreshingDocument73 pagesIsi RefreshingKarina Sandra AmiliaNo ratings yet
- Assessing and Managing Vulnerable Periwound SkinDocument6 pagesAssessing and Managing Vulnerable Periwound SkinPaty Antuña YarzaNo ratings yet
- Tinea VersicolorDocument4 pagesTinea Versicolorparand2003No ratings yet
- Dr. Igwe DISEASE OF THE SKIN - Doc-1Document11 pagesDr. Igwe DISEASE OF THE SKIN - Doc-1Jake MillerNo ratings yet
- WrinkleDocument2 pagesWrinkleNuRhidayah Syarifuddin Wijaya'odeNo ratings yet
- Elastosis: TalengiastaeaDocument2 pagesElastosis: TalengiastaeaNuRhidayah Syarifuddin Wijaya'odeNo ratings yet
- ANAPHY Integumentary SystemDocument3 pagesANAPHY Integumentary SystemNina JasminNo ratings yet
- Skin Care With ExDocument5 pagesSkin Care With ExnurinkdewiNo ratings yet
- Anatomy and Physiology ReviewDocument10 pagesAnatomy and Physiology Reviewrahtu suzi ameliaNo ratings yet
- The Natural Outer Layer of Tissue That Covers The Body of A Person or AnimalDocument7 pagesThe Natural Outer Layer of Tissue That Covers The Body of A Person or AnimalFebrianNo ratings yet
- ANAPHY Lec Session #4 - SAS (Agdana, Nicole Ken)Document10 pagesANAPHY Lec Session #4 - SAS (Agdana, Nicole Ken)Nicole Ken AgdanaNo ratings yet
- The Cornea: Gross Anatomy Corneal DiametersDocument25 pagesThe Cornea: Gross Anatomy Corneal DiametersDrmhdh DrmhdhNo ratings yet
- MainDocument11 pagesMainMuhammad Nur Ardhi LahabuNo ratings yet
- 2nd Half Microbiology For Allied Health StudentsDocument404 pages2nd Half Microbiology For Allied Health StudentsFjornNo ratings yet
- Integumentary SystemDocument59 pagesIntegumentary SystemJihaifa AjidùNo ratings yet
- Disorders of Abnormal KeratinizationDocument36 pagesDisorders of Abnormal KeratinizationdayangNo ratings yet
- Structure of SkinDocument31 pagesStructure of Skinshaiknafisa1255No ratings yet
- World's Largest Science, Technology & Medicine Open Access Book PublisherDocument33 pagesWorld's Largest Science, Technology & Medicine Open Access Book Publisherlenn chandNo ratings yet
- Integumentary SystemDocument17 pagesIntegumentary SystemNurani AtikasariNo ratings yet
- Tecnologí A Cosmé Tica 2020Document56 pagesTecnologí A Cosmé Tica 2020HAIDY FRANCONo ratings yet
- 2000 Ocular PathDocument26 pages2000 Ocular Pathdeta hamidaNo ratings yet
- Dr. Kurniati - Eliminating Dead Skin Cell Face and Body 0kt 2022Document27 pagesDr. Kurniati - Eliminating Dead Skin Cell Face and Body 0kt 2022wiwinNo ratings yet
- Skincarewith ExDocument4 pagesSkincarewith ExmissphidelisNo ratings yet
- Atopic Dermatitis Eczema NotesDocument12 pagesAtopic Dermatitis Eczema Notes돼끼빈No ratings yet
- ANAPHY Lec Session #4 - SASDocument10 pagesANAPHY Lec Session #4 - SASFherry Mae UsmanNo ratings yet
- Collodion Baby: Presented byDocument10 pagesCollodion Baby: Presented byNoor AhamedNo ratings yet
- Unit 2Document9 pagesUnit 2Aaron Clarence CalimagNo ratings yet
- Collodion Baby: eISSN 1307 - 394XDocument5 pagesCollodion Baby: eISSN 1307 - 394XMimi FatinNo ratings yet
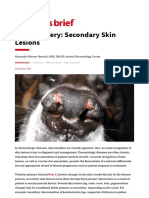
- Image Gallery - Secondary Skin Lesions - Clinician's BriefDocument9 pagesImage Gallery - Secondary Skin Lesions - Clinician's BriefMabe AguirreNo ratings yet
- Organs of The Integumentary SystemDocument4 pagesOrgans of The Integumentary SystemShyeNo ratings yet
- Integumentary System: By: Tim Barclay, PHD Medically Reviewed By: Stephanie Curreli, MD, PHD Jul 16, 2019Document12 pagesIntegumentary System: By: Tim Barclay, PHD Medically Reviewed By: Stephanie Curreli, MD, PHD Jul 16, 2019Caereel LopezNo ratings yet
- SDL IntegumentaryDocument4 pagesSDL IntegumentaryMonique Eloise GualizaNo ratings yet
- Common Cutaneous Disorders in ElderlyDocument6 pagesCommon Cutaneous Disorders in Elderlyirvinaldi9No ratings yet
- ENT216 - Lecture 5 Integument MoultingDocument33 pagesENT216 - Lecture 5 Integument MoultingkaraboletheNo ratings yet
- Kamus ManusiaDocument822 pagesKamus ManusiaAhmad Abdullah100% (1)
- Biomolecules 13 01614Document16 pagesBiomolecules 13 01614river771No ratings yet
- Skin Sense!: A Dermatologist's Guide to Skin and Facial Care; Third EditionFrom EverandSkin Sense!: A Dermatologist's Guide to Skin and Facial Care; Third EditionRating: 5 out of 5 stars5/5 (12)
- Safari - Feb 21, 2024 at 11:49 AM 2Document1 pageSafari - Feb 21, 2024 at 11:49 AM 2syansyncNo ratings yet
- Safari - Feb 21, 2024 at 12:01 PMDocument1 pageSafari - Feb 21, 2024 at 12:01 PMsyansyncNo ratings yet
- Safari - Feb 21, 2024 at 11:51 AMDocument1 pageSafari - Feb 21, 2024 at 11:51 AMsyansyncNo ratings yet
- Safari - Feb 21, 2024 at 12:16 PM 2Document1 pageSafari - Feb 21, 2024 at 12:16 PM 2syansyncNo ratings yet
- Safari - Feb 21, 2024 at 12:17 PM 2Document1 pageSafari - Feb 21, 2024 at 12:17 PM 2syansyncNo ratings yet
- Safari - Feb 21, 2024 at 11:56 AMDocument1 pageSafari - Feb 21, 2024 at 11:56 AMsyansyncNo ratings yet
- Safari - Feb 21, 2024 at 11:48 AMDocument1 pageSafari - Feb 21, 2024 at 11:48 AMsyansyncNo ratings yet
- Safari - Feb 21, 2024 at 11:58 AMDocument1 pageSafari - Feb 21, 2024 at 11:58 AMsyansyncNo ratings yet
- Safari - Feb 21, 2024 at 12:17 PM 3Document1 pageSafari - Feb 21, 2024 at 12:17 PM 3syansyncNo ratings yet
- Safari - Feb 13, 2024 at 11:56 AMDocument1 pageSafari - Feb 13, 2024 at 11:56 AMsyansyncNo ratings yet
- Safari - Feb 13, 2024 at 12:01 PMDocument1 pageSafari - Feb 13, 2024 at 12:01 PMsyansyncNo ratings yet
- Safari - Feb 13, 2024 at 12:04 PMDocument1 pageSafari - Feb 13, 2024 at 12:04 PMsyansyncNo ratings yet
- Safari - Feb 21, 2024 at 12:18 PM 4Document1 pageSafari - Feb 21, 2024 at 12:18 PM 4syansyncNo ratings yet
- Safari - Jan 9, 2024 at 5:16 AM 3 PDFDocument1 pageSafari - Jan 9, 2024 at 5:16 AM 3 PDFsyansyncNo ratings yet
- Safari - Feb 4, 2024 at 11:38 PMDocument1 pageSafari - Feb 4, 2024 at 11:38 PMsyansyncNo ratings yet
- Safari - Jan 10, 2024 at 12:31 AM PDFDocument1 pageSafari - Jan 10, 2024 at 12:31 AM PDFsyansyncNo ratings yet
- Safari - Feb 4, 2024 at 11:39 PM 2Document1 pageSafari - Feb 4, 2024 at 11:39 PM 2syansyncNo ratings yet
- Safari - Jan 10, 2024 at 12:25 AM 3 PDFDocument1 pageSafari - Jan 10, 2024 at 12:25 AM 3 PDFsyansyncNo ratings yet
- Safari - Feb 4, 2024 at 11:40 PM 3Document1 pageSafari - Feb 4, 2024 at 11:40 PM 3syansyncNo ratings yet
- Safari - Jan 10, 2024 at 12:31 AM 2 PDFDocument1 pageSafari - Jan 10, 2024 at 12:31 AM 2 PDFsyansyncNo ratings yet
- Safari - Jan 9, 2024 at 5:12 AM 2 PDFDocument1 pageSafari - Jan 9, 2024 at 5:12 AM 2 PDFsyansyncNo ratings yet
- Safari - Jan 9, 2024 at 5:13 AM 3 PDFDocument1 pageSafari - Jan 9, 2024 at 5:13 AM 3 PDFsyansyncNo ratings yet
- Safari - Jan 9, 2024 at 5:20 AM PDFDocument1 pageSafari - Jan 9, 2024 at 5:20 AM PDFsyansyncNo ratings yet
- Safari - Jan 10, 2024 at 12:30 AM PDFDocument1 pageSafari - Jan 10, 2024 at 12:30 AM PDFsyansyncNo ratings yet
- Safari - Jan 10, 2024 at 12:25 AM PDFDocument1 pageSafari - Jan 10, 2024 at 12:25 AM PDFsyansyncNo ratings yet
- Safari - Jan 9, 2024 at 5:12 AM PDFDocument1 pageSafari - Jan 9, 2024 at 5:12 AM PDFsyansyncNo ratings yet
- Safari - Jan 9, 2024 at 5:18 AMDocument1 pageSafari - Jan 9, 2024 at 5:18 AMsyansyncNo ratings yet
- Safari - Jan 9, 2024 at 5:19 AM 3 PDFDocument1 pageSafari - Jan 9, 2024 at 5:19 AM 3 PDFsyansyncNo ratings yet
- Safari - Jan 9, 2024 at 5:13 AM PDFDocument1 pageSafari - Jan 9, 2024 at 5:13 AM PDFsyansyncNo ratings yet
- Safari - Jan 9, 2024 at 5:18 AM 2 PDFDocument1 pageSafari - Jan 9, 2024 at 5:18 AM 2 PDFsyansyncNo ratings yet
- Sar SkinradDocument8 pagesSar SkinradEmf RefugeeNo ratings yet
- Dokumen - Tips - Croda Europe LTD Cosmetic Ingredient Expert Panel Meeting 17 Croda EuropeDocument36 pagesDokumen - Tips - Croda Europe LTD Cosmetic Ingredient Expert Panel Meeting 17 Croda Europechi nguyenNo ratings yet
- Bathing Tips For Dry Skin Relief InfographicDocument1 pageBathing Tips For Dry Skin Relief InfographicRella ShaNo ratings yet
- Diagnosis and Treatment of PsoriasisDocument36 pagesDiagnosis and Treatment of PsoriasisLeony_octaviasNo ratings yet
- BIO2OO - Introduction Tissues, Classification of Living Things & Ecology 1.1.0 Animal TissueDocument19 pagesBIO2OO - Introduction Tissues, Classification of Living Things & Ecology 1.1.0 Animal TissueMark SullivanNo ratings yet
- 17-Biotoxins-Poisnous Glands in FishesDocument34 pages17-Biotoxins-Poisnous Glands in FishesIqra AnwarNo ratings yet
- Dengue Hemorrhagic Fever Case BookDocument105 pagesDengue Hemorrhagic Fever Case BookMarianne Daphne Guevarra100% (1)
- Vitiligo TreatmentDocument3 pagesVitiligo TreatmentAnonymous d9GP3q5Z8PNo ratings yet
- New Microsoft Word DocumentDocument7 pagesNew Microsoft Word DocumentBiancaPascuNo ratings yet
- Wmsu-Vpaa-Fr-33.00 Templates For The Independent Learning PacketDocument3 pagesWmsu-Vpaa-Fr-33.00 Templates For The Independent Learning PacketBeng LunaNo ratings yet
- BURNS GeneralDocument59 pagesBURNS GeneralValluri MukeshNo ratings yet
- Cyspera FrontDocument1 pageCyspera FrontkriswantiNo ratings yet
- Exilis Ultra 360 Catalogue 6hFRZpjsQ2iiiLJDocument13 pagesExilis Ultra 360 Catalogue 6hFRZpjsQ2iiiLJJohn LuNo ratings yet
- Kamedis Business Development BrochureDocument8 pagesKamedis Business Development Brochurepanji respatiNo ratings yet
- N64.4 Mastodynia: C73 Malignant Neoplasm of Thyroid GlandDocument1 pageN64.4 Mastodynia: C73 Malignant Neoplasm of Thyroid Glanddebby nirmasariNo ratings yet
- 03 Relevant and Irrelevant DetailsDocument5 pages03 Relevant and Irrelevant DetailsKaki KitaiNo ratings yet
- Sany Truck Crane Stc250s5 Parts BookDocument22 pagesSany Truck Crane Stc250s5 Parts Bookrobertflynn180290sdg100% (65)
- BULLOUS PEMPHIGOID-anto-1Document21 pagesBULLOUS PEMPHIGOID-anto-1Nur RifqahNo ratings yet
- Test Bank For Accompany Saladin Human Anatomy 6th Edition Eric Wise DownloadDocument35 pagesTest Bank For Accompany Saladin Human Anatomy 6th Edition Eric Wise Downloadstevenmccallcdrjybmage100% (27)
- A00314 LINEFACTOR C - Marketing BrochureDocument11 pagesA00314 LINEFACTOR C - Marketing BrochureparomanikNo ratings yet
- CystsDocument5 pagesCystsranindita maulyaNo ratings yet
- Data Upload ShopeeDocument28 pagesData Upload Shopeebanyakmauu borNo ratings yet
- Physiological Effects of MassageDocument1 pagePhysiological Effects of MassagehannahNo ratings yet
- Animal Tissue - 1Document3 pagesAnimal Tissue - 1Kb AshishNo ratings yet
- Biomaterials Assignments2Document34 pagesBiomaterials Assignments2Mohâmmed Ä. ÃlFakihNo ratings yet
- Basic Facials and Treatments: Topic 1: Facial Treatment BenefitsDocument6 pagesBasic Facials and Treatments: Topic 1: Facial Treatment Benefitsrobert100% (1)
- Doctor Brochure Stylage Bi Soft 2018Document36 pagesDoctor Brochure Stylage Bi Soft 2018薛凯No ratings yet
Safari - Feb 21, 2024 at 12:04 PM
Safari - Feb 21, 2024 at 12:04 PM
Uploaded by
syansyncOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Safari - Feb 21, 2024 at 12:04 PM
Safari - Feb 21, 2024 at 12:04 PM
Uploaded by
syansyncCopyright:
Available Formats
Search Wikipedia
Desquamation
Article Talk
This article is about the medical condition. For the meaning in material sciences, see spalling. For onion skin
weathering of rocks, see Onion-skin weathering.
Desquamation occurs when the outermost layer of a tissue, such as the skin, is shed. The term is
from Latin desquamare 'to scrape the scales off a fish'.
Contents Desquamation
Physiologic desquamation Other names Skin peeling
Abnormal desquamation
Eyes
See also
References
External links
Specialty Dermatology
Physiologic desquamation
Keratinocytes are the predominant cells of the epidermis, the outermost layer of the skin. Living
keratinocytes reside in the basal, spinous, or granular layers of the epidermis. The outermost layer of
the epidermis is called the stratum corneum and it is composed of terminally differentiated
keratinocytes, the corneocytes. In the absence of disease, desquamation occurs when corneocytes
are individually shed unnoticeably from the surface of the skin.[1] Typically the time it takes for a
corneocyte to be formed and then shed is about 14 weeks but this time can vary depending on the
anatomical location that the skin is covering. For example, desquamation occurs more slowly at acral
(palm and sole) surfaces and more rapidly where the skin is thin, such as the eyelids. Normal
desquamation can be visualized by immersing skin in warm or hot water. This induces the outermost
layer of corneocytes to shed, such as is the case after a hot shower or bath.[citation needed]
Corneocytes are held together by corneodesmosomes. In order for desquamation to occur these
corneodesmosome connections must be degraded.[1] Keratinocytes residing in the stratum
granulosum produce corneodesmosome-degrading kallikrein family members, especially KLK1, KLK5,
and KLK7.[2] Kallikreins are serine proteases. They are packaged within lamellar bodies and released
into the intercellular space between the keratinocytes as they transition into becoming corneocytes.[1]
To prevent premature desquamation, granular layer keratinocytes also produce kallikrein-inhibitory
proteins.[2] At acral surfaces, desquamation occurs more slowly because granular layer keratinocytes
downregulate expression of KLK1 and KLK7 and upregulate expression of protease inhibitors, including
the KLK5-specific SPINK9 and the cysteine protease inhibitors CSTA and CST3.[2] Slowing the process
of corneocyte desquamation allows acral (palm and sole) skin to form a thick protective stratum
corneum.[2]
Abnormal desquamation
Scale forms on the skin surface in various disease settings, and is the result of abnormal
desquamation. In pathologic desquamation, such as that seen in X-linked ichthyosis, the stratum
corneum becomes thicker (hyperkeratosis), imparting a "dry" or scaly appearance to the skin, and
instead of detaching as single cells, corneocytes are shed in clusters, which forms visible scales.[1]
Desquamation of the epidermis may result from disease or injury of the skin. For example, once the
rash of measles fades, there is desquamation. Skin peeling typically follows healing of a first degree
burn or sunburn. Toxic shock syndrome, a potentially fatal immune system reaction to a bacterial
infection such as Staphylococcus aureus,[3] can cause severe desquamation; so can mercury
poisoning. Other serious skin diseases involving extreme desquamation include Stevens–Johnson
syndrome and toxic epidermal necrolysis (TEN).[4] Radiation can cause dry or moist desquamation.[5]
Desquamation is also abnormal in patients with immune-mediated skin diseases such as psoriasis and
atopic dermatitis.[2] Abnormal desquamation often results in scale formation on the skin's surface.[2]
Lipid composition alterations in scale have been used to construct diagnostic models for human skin
disease.[2]
Desquamation of skin on Desquamation of skin on Desquamation of skin on
hands, caused by scarlet fingertips, caused by the finger, caused by the
fever infection scarlet fever popping of an acute
paronychia
Eyes
Certain eye tissues, including the conjunctiva and cornea, may undergo pathological desquamation in
diseases such as dry eye syndrome.[6] The anatomy of the human eye makes desquamation of the
lens impossible.[7]
See also
Desquamative gingivitis
Exfoliation joint
Moist desquamation
Pityriasis—flaking of the skin
Spalling
Sunburn
References
1. ^ a b c d Jackson, Simon M.; Williams, Mary L.; Feingold, Kenneth R.; Elias, Peter M. (1993). "Pathobiology of the
Stratum Corneum" . The Western Journal of Medicine. 158 (3): 279–85. PMC 1311754 . PMID 8460510 .
2. ^ a b c d e f g Merleev, Alexander A.; Le, Stephanie T.; Alexanian, Claire; Toussi, Atrin; Xie, Yixuan; Marusina, Alina I.;
Watkins, Steven M.; Patel, Forum; Billi, Allison C.; Wiedemann, Julie; Izumiya, Yoshihiro; Kumar, Ashish; Uppala,
Ranjitha; Kahlenberg, J. Michelle; Liu, Fu-Tong (2022-08-22). "Biogeographic and disease-specific alterations in
epidermal lipid composition and single-cell analysis of acral keratinocytes" . JCI Insight. 7 (16): e159762.
doi:10.1172/jci.insight.159762 . ISSN 2379-3708 . PMC 9462509 . PMID 35900871 .
3. ^ Dinges, MM; Orwin, PM; Schlievert, PM (January 2000). "Exotoxins of Staphylococcus aureus" . Clinical
Microbiology Reviews. 13 (1): 16–34, table of contents. doi:10.1128/cmr.13.1.16 . PMC 88931 .
PMID 10627489 .
4. ^ Parillo, Steven J; Parillo, Catherine V. (2010-05-25). "Stevens-Johnson Syndrome" . eMedicine. Medcape.
Retrieved 2010-09-06.
5. ^ Centers for Disease Control and Prevention (2005-06-30). "Cutaneous Radiation Injury" . CDC. Retrieved 2011-
05-15.
6. ^ Gilbard, Jeffrey P. (November 1, 2003). "Dry Eye: Natural History, Diagnosis and Treatment" . Wolters Kluwer
Pharma Solutions. Archived from the original on January 30, 2013. Retrieved February 3, 2012.
7. ^ Lynnerup, Niels; Kjeldsen, Henrik; Heegaard, Steffen; Jacobsen, Christina; Heinemeier, Jan (2008). Gazit, Ehud
(ed.). "Radiocarbon Dating of the Human Eye Lens Crystallines Reveal Proteins without Carbon Turnover throughout
Life" . PLOS ONE. 3 (1): e1529. Bibcode:2008PLoSO...3.1529L . doi:10.1371/journal.pone.0001529 .
PMC 2211393 . PMID 18231610 .
External links
Wikimedia Commons has media
related to Desquamation.
Last edited on 11 January 2024, at 15:19
Content is available under CC BY-SA 4.0 unless otherwise noted.
Terms of Use • Privacy policy • Desktop
:
You might also like
- Fitzpatricks Dermatology in General Medicine 8edDocument3,190 pagesFitzpatricks Dermatology in General Medicine 8edFauzul Azmi96% (74)
- Flexi Master Series Mock-1 SolutionDocument96 pagesFlexi Master Series Mock-1 SolutionYugal0% (1)
- Antiaging Efficacy of A Retinaldehyde-Based Cream Compared With Glycolic Acid Peel Sessions: A Randomized Controlled StudyDocument8 pagesAntiaging Efficacy of A Retinaldehyde-Based Cream Compared With Glycolic Acid Peel Sessions: A Randomized Controlled Studypermen_lollypopzNo ratings yet
- Wnofns 43 (2022) 11-37Document27 pagesWnofns 43 (2022) 11-37Dennis StwnNo ratings yet
- Anatomy, Skin (Integument) - StatPearls - NCBI BookshelfDocument4 pagesAnatomy, Skin (Integument) - StatPearls - NCBI Bookshelfputri aisheNo ratings yet
- Safari - Feb 21, 2024 at 11:56 AMDocument1 pageSafari - Feb 21, 2024 at 11:56 AMsyansyncNo ratings yet
- Skin Examination 1Document17 pagesSkin Examination 1Daffa AmaliaNo ratings yet
- Structure of SkinDocument129 pagesStructure of SkinDeepak BaliyanNo ratings yet
- Chapter 4: Examination of The Skin, Coat and Associated StructuresDocument19 pagesChapter 4: Examination of The Skin, Coat and Associated StructuresZekarias GetachewNo ratings yet
- Canine Ichthyosis and Related Disorders of CornificationDocument9 pagesCanine Ichthyosis and Related Disorders of CornificationPaolaNo ratings yet
- Modul 1 (No: 1-3) Anggota KelompokDocument33 pagesModul 1 (No: 1-3) Anggota KelompokfrostedsurgeonNo ratings yet
- Tissue Integrity Outline Spring 2023Document25 pagesTissue Integrity Outline Spring 2023morganstorey0No ratings yet
- Project Topic: Skin Prepared By: (1) Ankita Chavda (2) Krupali Tandel (F.Y. B.PT. Students)Document55 pagesProject Topic: Skin Prepared By: (1) Ankita Chavda (2) Krupali Tandel (F.Y. B.PT. Students)shivaniNo ratings yet
- The Integumentary SystemDocument4 pagesThe Integumentary SystemKhan Hayudini SaliNo ratings yet
- The Integumentary System Activity No. 12Document4 pagesThe Integumentary System Activity No. 12Khan Hayudini SaliNo ratings yet
- 2017 - Tecnología CosméticaDocument54 pages2017 - Tecnología CosméticaCésar Rosado Avila ToñoNo ratings yet
- Integumentary SystemDocument13 pagesIntegumentary Systemleih jsNo ratings yet
- Integumentary System: Chapter OutlineDocument7 pagesIntegumentary System: Chapter OutlineRiy KimNo ratings yet
- Safari - Feb 21, 2024 at 11:48 AMDocument1 pageSafari - Feb 21, 2024 at 11:48 AMsyansyncNo ratings yet
- Dissertation LeucodermaDocument90 pagesDissertation LeucodermaRashmi Mishra100% (1)
- GENOVE, ERICKA IS-Module2Document11 pagesGENOVE, ERICKA IS-Module2Ericka GenoveNo ratings yet
- IJCRT2310623Document18 pagesIJCRT2310623roseNo ratings yet
- Mechanisms and Causes of Scalp ScalingDocument5 pagesMechanisms and Causes of Scalp ScalingAdrianeNo ratings yet
- Superficial and Medium-Depth Chemical PeelsDocument10 pagesSuperficial and Medium-Depth Chemical PeelsFenni Oktoberry100% (1)
- Isi RefreshingDocument73 pagesIsi RefreshingKarina Sandra AmiliaNo ratings yet
- Assessing and Managing Vulnerable Periwound SkinDocument6 pagesAssessing and Managing Vulnerable Periwound SkinPaty Antuña YarzaNo ratings yet
- Tinea VersicolorDocument4 pagesTinea Versicolorparand2003No ratings yet
- Dr. Igwe DISEASE OF THE SKIN - Doc-1Document11 pagesDr. Igwe DISEASE OF THE SKIN - Doc-1Jake MillerNo ratings yet
- WrinkleDocument2 pagesWrinkleNuRhidayah Syarifuddin Wijaya'odeNo ratings yet
- Elastosis: TalengiastaeaDocument2 pagesElastosis: TalengiastaeaNuRhidayah Syarifuddin Wijaya'odeNo ratings yet
- ANAPHY Integumentary SystemDocument3 pagesANAPHY Integumentary SystemNina JasminNo ratings yet
- Skin Care With ExDocument5 pagesSkin Care With ExnurinkdewiNo ratings yet
- Anatomy and Physiology ReviewDocument10 pagesAnatomy and Physiology Reviewrahtu suzi ameliaNo ratings yet
- The Natural Outer Layer of Tissue That Covers The Body of A Person or AnimalDocument7 pagesThe Natural Outer Layer of Tissue That Covers The Body of A Person or AnimalFebrianNo ratings yet
- ANAPHY Lec Session #4 - SAS (Agdana, Nicole Ken)Document10 pagesANAPHY Lec Session #4 - SAS (Agdana, Nicole Ken)Nicole Ken AgdanaNo ratings yet
- The Cornea: Gross Anatomy Corneal DiametersDocument25 pagesThe Cornea: Gross Anatomy Corneal DiametersDrmhdh DrmhdhNo ratings yet
- MainDocument11 pagesMainMuhammad Nur Ardhi LahabuNo ratings yet
- 2nd Half Microbiology For Allied Health StudentsDocument404 pages2nd Half Microbiology For Allied Health StudentsFjornNo ratings yet
- Integumentary SystemDocument59 pagesIntegumentary SystemJihaifa AjidùNo ratings yet
- Disorders of Abnormal KeratinizationDocument36 pagesDisorders of Abnormal KeratinizationdayangNo ratings yet
- Structure of SkinDocument31 pagesStructure of Skinshaiknafisa1255No ratings yet
- World's Largest Science, Technology & Medicine Open Access Book PublisherDocument33 pagesWorld's Largest Science, Technology & Medicine Open Access Book Publisherlenn chandNo ratings yet
- Integumentary SystemDocument17 pagesIntegumentary SystemNurani AtikasariNo ratings yet
- Tecnologí A Cosmé Tica 2020Document56 pagesTecnologí A Cosmé Tica 2020HAIDY FRANCONo ratings yet
- 2000 Ocular PathDocument26 pages2000 Ocular Pathdeta hamidaNo ratings yet
- Dr. Kurniati - Eliminating Dead Skin Cell Face and Body 0kt 2022Document27 pagesDr. Kurniati - Eliminating Dead Skin Cell Face and Body 0kt 2022wiwinNo ratings yet
- Skincarewith ExDocument4 pagesSkincarewith ExmissphidelisNo ratings yet
- Atopic Dermatitis Eczema NotesDocument12 pagesAtopic Dermatitis Eczema Notes돼끼빈No ratings yet
- ANAPHY Lec Session #4 - SASDocument10 pagesANAPHY Lec Session #4 - SASFherry Mae UsmanNo ratings yet
- Collodion Baby: Presented byDocument10 pagesCollodion Baby: Presented byNoor AhamedNo ratings yet
- Unit 2Document9 pagesUnit 2Aaron Clarence CalimagNo ratings yet
- Collodion Baby: eISSN 1307 - 394XDocument5 pagesCollodion Baby: eISSN 1307 - 394XMimi FatinNo ratings yet
- Image Gallery - Secondary Skin Lesions - Clinician's BriefDocument9 pagesImage Gallery - Secondary Skin Lesions - Clinician's BriefMabe AguirreNo ratings yet
- Organs of The Integumentary SystemDocument4 pagesOrgans of The Integumentary SystemShyeNo ratings yet
- Integumentary System: By: Tim Barclay, PHD Medically Reviewed By: Stephanie Curreli, MD, PHD Jul 16, 2019Document12 pagesIntegumentary System: By: Tim Barclay, PHD Medically Reviewed By: Stephanie Curreli, MD, PHD Jul 16, 2019Caereel LopezNo ratings yet
- SDL IntegumentaryDocument4 pagesSDL IntegumentaryMonique Eloise GualizaNo ratings yet
- Common Cutaneous Disorders in ElderlyDocument6 pagesCommon Cutaneous Disorders in Elderlyirvinaldi9No ratings yet
- ENT216 - Lecture 5 Integument MoultingDocument33 pagesENT216 - Lecture 5 Integument MoultingkaraboletheNo ratings yet
- Kamus ManusiaDocument822 pagesKamus ManusiaAhmad Abdullah100% (1)
- Biomolecules 13 01614Document16 pagesBiomolecules 13 01614river771No ratings yet
- Skin Sense!: A Dermatologist's Guide to Skin and Facial Care; Third EditionFrom EverandSkin Sense!: A Dermatologist's Guide to Skin and Facial Care; Third EditionRating: 5 out of 5 stars5/5 (12)
- Safari - Feb 21, 2024 at 11:49 AM 2Document1 pageSafari - Feb 21, 2024 at 11:49 AM 2syansyncNo ratings yet
- Safari - Feb 21, 2024 at 12:01 PMDocument1 pageSafari - Feb 21, 2024 at 12:01 PMsyansyncNo ratings yet
- Safari - Feb 21, 2024 at 11:51 AMDocument1 pageSafari - Feb 21, 2024 at 11:51 AMsyansyncNo ratings yet
- Safari - Feb 21, 2024 at 12:16 PM 2Document1 pageSafari - Feb 21, 2024 at 12:16 PM 2syansyncNo ratings yet
- Safari - Feb 21, 2024 at 12:17 PM 2Document1 pageSafari - Feb 21, 2024 at 12:17 PM 2syansyncNo ratings yet
- Safari - Feb 21, 2024 at 11:56 AMDocument1 pageSafari - Feb 21, 2024 at 11:56 AMsyansyncNo ratings yet
- Safari - Feb 21, 2024 at 11:48 AMDocument1 pageSafari - Feb 21, 2024 at 11:48 AMsyansyncNo ratings yet
- Safari - Feb 21, 2024 at 11:58 AMDocument1 pageSafari - Feb 21, 2024 at 11:58 AMsyansyncNo ratings yet
- Safari - Feb 21, 2024 at 12:17 PM 3Document1 pageSafari - Feb 21, 2024 at 12:17 PM 3syansyncNo ratings yet
- Safari - Feb 13, 2024 at 11:56 AMDocument1 pageSafari - Feb 13, 2024 at 11:56 AMsyansyncNo ratings yet
- Safari - Feb 13, 2024 at 12:01 PMDocument1 pageSafari - Feb 13, 2024 at 12:01 PMsyansyncNo ratings yet
- Safari - Feb 13, 2024 at 12:04 PMDocument1 pageSafari - Feb 13, 2024 at 12:04 PMsyansyncNo ratings yet
- Safari - Feb 21, 2024 at 12:18 PM 4Document1 pageSafari - Feb 21, 2024 at 12:18 PM 4syansyncNo ratings yet
- Safari - Jan 9, 2024 at 5:16 AM 3 PDFDocument1 pageSafari - Jan 9, 2024 at 5:16 AM 3 PDFsyansyncNo ratings yet
- Safari - Feb 4, 2024 at 11:38 PMDocument1 pageSafari - Feb 4, 2024 at 11:38 PMsyansyncNo ratings yet
- Safari - Jan 10, 2024 at 12:31 AM PDFDocument1 pageSafari - Jan 10, 2024 at 12:31 AM PDFsyansyncNo ratings yet
- Safari - Feb 4, 2024 at 11:39 PM 2Document1 pageSafari - Feb 4, 2024 at 11:39 PM 2syansyncNo ratings yet
- Safari - Jan 10, 2024 at 12:25 AM 3 PDFDocument1 pageSafari - Jan 10, 2024 at 12:25 AM 3 PDFsyansyncNo ratings yet
- Safari - Feb 4, 2024 at 11:40 PM 3Document1 pageSafari - Feb 4, 2024 at 11:40 PM 3syansyncNo ratings yet
- Safari - Jan 10, 2024 at 12:31 AM 2 PDFDocument1 pageSafari - Jan 10, 2024 at 12:31 AM 2 PDFsyansyncNo ratings yet
- Safari - Jan 9, 2024 at 5:12 AM 2 PDFDocument1 pageSafari - Jan 9, 2024 at 5:12 AM 2 PDFsyansyncNo ratings yet
- Safari - Jan 9, 2024 at 5:13 AM 3 PDFDocument1 pageSafari - Jan 9, 2024 at 5:13 AM 3 PDFsyansyncNo ratings yet
- Safari - Jan 9, 2024 at 5:20 AM PDFDocument1 pageSafari - Jan 9, 2024 at 5:20 AM PDFsyansyncNo ratings yet
- Safari - Jan 10, 2024 at 12:30 AM PDFDocument1 pageSafari - Jan 10, 2024 at 12:30 AM PDFsyansyncNo ratings yet
- Safari - Jan 10, 2024 at 12:25 AM PDFDocument1 pageSafari - Jan 10, 2024 at 12:25 AM PDFsyansyncNo ratings yet
- Safari - Jan 9, 2024 at 5:12 AM PDFDocument1 pageSafari - Jan 9, 2024 at 5:12 AM PDFsyansyncNo ratings yet
- Safari - Jan 9, 2024 at 5:18 AMDocument1 pageSafari - Jan 9, 2024 at 5:18 AMsyansyncNo ratings yet
- Safari - Jan 9, 2024 at 5:19 AM 3 PDFDocument1 pageSafari - Jan 9, 2024 at 5:19 AM 3 PDFsyansyncNo ratings yet
- Safari - Jan 9, 2024 at 5:13 AM PDFDocument1 pageSafari - Jan 9, 2024 at 5:13 AM PDFsyansyncNo ratings yet
- Safari - Jan 9, 2024 at 5:18 AM 2 PDFDocument1 pageSafari - Jan 9, 2024 at 5:18 AM 2 PDFsyansyncNo ratings yet
- Sar SkinradDocument8 pagesSar SkinradEmf RefugeeNo ratings yet
- Dokumen - Tips - Croda Europe LTD Cosmetic Ingredient Expert Panel Meeting 17 Croda EuropeDocument36 pagesDokumen - Tips - Croda Europe LTD Cosmetic Ingredient Expert Panel Meeting 17 Croda Europechi nguyenNo ratings yet
- Bathing Tips For Dry Skin Relief InfographicDocument1 pageBathing Tips For Dry Skin Relief InfographicRella ShaNo ratings yet
- Diagnosis and Treatment of PsoriasisDocument36 pagesDiagnosis and Treatment of PsoriasisLeony_octaviasNo ratings yet
- BIO2OO - Introduction Tissues, Classification of Living Things & Ecology 1.1.0 Animal TissueDocument19 pagesBIO2OO - Introduction Tissues, Classification of Living Things & Ecology 1.1.0 Animal TissueMark SullivanNo ratings yet
- 17-Biotoxins-Poisnous Glands in FishesDocument34 pages17-Biotoxins-Poisnous Glands in FishesIqra AnwarNo ratings yet
- Dengue Hemorrhagic Fever Case BookDocument105 pagesDengue Hemorrhagic Fever Case BookMarianne Daphne Guevarra100% (1)
- Vitiligo TreatmentDocument3 pagesVitiligo TreatmentAnonymous d9GP3q5Z8PNo ratings yet
- New Microsoft Word DocumentDocument7 pagesNew Microsoft Word DocumentBiancaPascuNo ratings yet
- Wmsu-Vpaa-Fr-33.00 Templates For The Independent Learning PacketDocument3 pagesWmsu-Vpaa-Fr-33.00 Templates For The Independent Learning PacketBeng LunaNo ratings yet
- BURNS GeneralDocument59 pagesBURNS GeneralValluri MukeshNo ratings yet
- Cyspera FrontDocument1 pageCyspera FrontkriswantiNo ratings yet
- Exilis Ultra 360 Catalogue 6hFRZpjsQ2iiiLJDocument13 pagesExilis Ultra 360 Catalogue 6hFRZpjsQ2iiiLJJohn LuNo ratings yet
- Kamedis Business Development BrochureDocument8 pagesKamedis Business Development Brochurepanji respatiNo ratings yet
- N64.4 Mastodynia: C73 Malignant Neoplasm of Thyroid GlandDocument1 pageN64.4 Mastodynia: C73 Malignant Neoplasm of Thyroid Glanddebby nirmasariNo ratings yet
- 03 Relevant and Irrelevant DetailsDocument5 pages03 Relevant and Irrelevant DetailsKaki KitaiNo ratings yet
- Sany Truck Crane Stc250s5 Parts BookDocument22 pagesSany Truck Crane Stc250s5 Parts Bookrobertflynn180290sdg100% (65)
- BULLOUS PEMPHIGOID-anto-1Document21 pagesBULLOUS PEMPHIGOID-anto-1Nur RifqahNo ratings yet
- Test Bank For Accompany Saladin Human Anatomy 6th Edition Eric Wise DownloadDocument35 pagesTest Bank For Accompany Saladin Human Anatomy 6th Edition Eric Wise Downloadstevenmccallcdrjybmage100% (27)
- A00314 LINEFACTOR C - Marketing BrochureDocument11 pagesA00314 LINEFACTOR C - Marketing BrochureparomanikNo ratings yet
- CystsDocument5 pagesCystsranindita maulyaNo ratings yet
- Data Upload ShopeeDocument28 pagesData Upload Shopeebanyakmauu borNo ratings yet
- Physiological Effects of MassageDocument1 pagePhysiological Effects of MassagehannahNo ratings yet
- Animal Tissue - 1Document3 pagesAnimal Tissue - 1Kb AshishNo ratings yet
- Biomaterials Assignments2Document34 pagesBiomaterials Assignments2Mohâmmed Ä. ÃlFakihNo ratings yet
- Basic Facials and Treatments: Topic 1: Facial Treatment BenefitsDocument6 pagesBasic Facials and Treatments: Topic 1: Facial Treatment Benefitsrobert100% (1)
- Doctor Brochure Stylage Bi Soft 2018Document36 pagesDoctor Brochure Stylage Bi Soft 2018薛凯No ratings yet