Professional Documents
Culture Documents
Report f642c 1704009629273
Report f642c 1704009629273
Uploaded by
Er Sumit SiwatchCopyright:
Available Formats
You might also like
- Exegesis Paper On 1 Corinthians 13Document11 pagesExegesis Paper On 1 Corinthians 13Elisa Medina AlbinoNo ratings yet
- Laboratory Test Report: Test Name Result Biological Reference Interval Uric AcidDocument5 pagesLaboratory Test Report: Test Name Result Biological Reference Interval Uric AcidBalraj EnjamuriNo ratings yet
- OSS Double-Agent Operations in World War IIDocument12 pagesOSS Double-Agent Operations in World War IIoscarherradonNo ratings yet
- Bullet Trajectory Reconstruction On Vehicles JFIDocument8 pagesBullet Trajectory Reconstruction On Vehicles JFIManolo BermeoNo ratings yet
- Report 190a3 1695110951228Document13 pagesReport 190a3 1695110951228Mohd Jaffer ShareefNo ratings yet
- Report bc90b 1710052260449Document11 pagesReport bc90b 1710052260449muralinaiduNo ratings yet
- Report Eaaf4 1695467677147Document16 pagesReport Eaaf4 1695467677147Mohd Jaffer ShareefNo ratings yet
- Subhra Pattnaik ReportDocument4 pagesSubhra Pattnaik ReportSubhra pattnaikNo ratings yet
- Nilesh Karani 13295 29-10-2023 20231029084151 StationerypdfmergedDocument22 pagesNilesh Karani 13295 29-10-2023 20231029084151 StationerypdfmergedsteelblackNo ratings yet
- CombinepdfDocument28 pagesCombinepdfNEETFIXNo ratings yet
- Po3979242722 431Document8 pagesPo3979242722 431NEETFIXNo ratings yet
- Report 9c0fcfa7Document3 pagesReport 9c0fcfa7Shivam SharmaNo ratings yet
- Biochemistry: Investigation Observed Value Unit Biological Reference IntervalDocument15 pagesBiochemistry: Investigation Observed Value Unit Biological Reference IntervalAshutoshNo ratings yet
- LFT (Liver Function Test) : Biological Reference Results Units Test NameDocument4 pagesLFT (Liver Function Test) : Biological Reference Results Units Test Namemetepraju0210No ratings yet
- Quadra Medical Services Pvt. LTD.: Department of PathologyDocument1 pageQuadra Medical Services Pvt. LTD.: Department of PathologyRiyaa SahaNo ratings yet
- Uetquwiuj 912083949Document4 pagesUetquwiuj 912083949TzvineZNo ratings yet
- YourDocument1 pageYourYashdeep Singh.kNo ratings yet
- N8 R 9 W3 Pupeyo RF RTWB 42 BRDocument2 pagesN8 R 9 W3 Pupeyo RF RTWB 42 BRPrashant KumarNo ratings yet
- Date 24/dec/2022 08:32AM 03/dec/22 09:33AM 26/nov/22 09:05AM Unit Bio Ref IntervalDocument11 pagesDate 24/dec/2022 08:32AM 03/dec/22 09:33AM 26/nov/22 09:05AM Unit Bio Ref IntervalAmit SinghNo ratings yet
- 1-Liver Function Test - PO3921596584-773 - 230517 - 125136Document4 pages1-Liver Function Test - PO3921596584-773 - 230517 - 125136Moksh GujjarNo ratings yet
- Date 16/feb/2020 02:12PM Unit Bio - Ref.Range: Laboratory Investigation ReportDocument1 pageDate 16/feb/2020 02:12PM Unit Bio - Ref.Range: Laboratory Investigation ReportBhupender SinghNo ratings yet
- Clinical Biochemistry: Test Report Reg - No Age Name::: Reg - Date Collection:: Received: 15-Jul-2019 / 09:25 AMDocument8 pagesClinical Biochemistry: Test Report Reg - No Age Name::: Reg - Date Collection:: Received: 15-Jul-2019 / 09:25 AMAnuradha KommojuNo ratings yet
- Department of Biochemistry Test Name Result Unit Bio. Ref. RangeDocument5 pagesDepartment of Biochemistry Test Name Result Unit Bio. Ref. RangeSudhanshuNo ratings yet
- PR1546497Document2 pagesPR1546497basavajsalagar1No ratings yet
- Report 8b3a3101Document11 pagesReport 8b3a3101Pooja AgarwalNo ratings yet
- ReportDocument3 pagesReportPawan MadhesiyaNo ratings yet
- Lab Report - ShivanandhamDocument7 pagesLab Report - ShivanandhamPO, ITDA BhadrachalamNo ratings yet
- Uk007 2223 006609Document3 pagesUk007 2223 006609Arpit KumarNo ratings yet
- Biochemistry Test Name Result Bio. Ref. Range Method: C-Reactive Protein 0-5 Immuno Turbidometric AssayDocument10 pagesBiochemistry Test Name Result Bio. Ref. Range Method: C-Reactive Protein 0-5 Immuno Turbidometric AssayAnkur DeyNo ratings yet
- LIVER PROFILE LFT Test Report Format Example Sample Template Drlogy Lab ReportDocument1 pageLIVER PROFILE LFT Test Report Format Example Sample Template Drlogy Lab ReportM ShafiqNo ratings yet
- Report ViewerDocument1 pageReport ViewermuhammadmoazmaalikNo ratings yet
- Patient Name Mr. Umesh Jain Uhid Lab No Sample Date Receiving Date 03/04/2021 11:40AMDocument1 pagePatient Name Mr. Umesh Jain Uhid Lab No Sample Date Receiving Date 03/04/2021 11:40AMAkshay ChaudhryNo ratings yet
- Ap Land Titling ActDocument7 pagesAp Land Titling ActmurtyaretyNo ratings yet
- PranithaDocument15 pagesPranithaKumar VijayNo ratings yet
- SnehaDocument3 pagesSneharazeena salamNo ratings yet
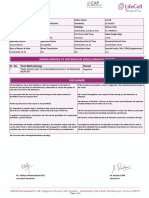
- Inborn Errors of Metabolism (Iem) Summary Report: Sr. No. Test Methodology Result Test TypeDocument2 pagesInborn Errors of Metabolism (Iem) Summary Report: Sr. No. Test Methodology Result Test TypeMallikharjunaRao medaNo ratings yet
- Document 4Document5 pagesDocument 4mehtanagina682No ratings yet
- PdfText - 2023-12-12T152233.242Document2 pagesPdfText - 2023-12-12T152233.242joshipriya208No ratings yet
- Biochemistry CDCL CDCL-14403 17-18Document1 pageBiochemistry CDCL CDCL-14403 17-18Ashutosh SinghNo ratings yet
- Biochemistry CDCL CDCL-14403 17-18 PDFDocument1 pageBiochemistry CDCL CDCL-14403 17-18 PDFAshutosh SinghNo ratings yet
- Liver Function Test (Lft-A)Document4 pagesLiver Function Test (Lft-A)ce mgnregsNo ratings yet
- Report GNDocument3 pagesReport GNPawan MadhesiyaNo ratings yet
- Mrs Nandhinidevi.M 04007180: Sid No. Patient ID 0400005449Document2 pagesMrs Nandhinidevi.M 04007180: Sid No. Patient ID 040000544911F10 RUCHITA MAARANNo ratings yet
- LabReportNew - 2023-09-08T160827.328Document3 pagesLabReportNew - 2023-09-08T160827.328viraj kshirsagarNo ratings yet
- PdfText - 2024-03-15T191650.936Document1 pagePdfText - 2024-03-15T191650.936jayanthmahesh0403No ratings yet
- Haematology: Investigation Observed Value Unit Biological Reference IntervalDocument9 pagesHaematology: Investigation Observed Value Unit Biological Reference Intervalsunita hoskotiNo ratings yet
- LabTest 30nov2023Document5 pagesLabTest 30nov2023Ritu SinghNo ratings yet
- Mrs Sonali Upadhiya: Interpretation: Interpretation For Hba1C% As Per American Diabetes Association (Ada)Document3 pagesMrs Sonali Upadhiya: Interpretation: Interpretation For Hba1C% As Per American Diabetes Association (Ada)CHINMAY UPADHYAYA X-DNo ratings yet
- Department of Chemical Pathology: Liver Function TestsDocument3 pagesDepartment of Chemical Pathology: Liver Function TestsbabarchuhanNo ratings yet
- Apollo247 249052700 LabreportDocument7 pagesApollo247 249052700 LabreportASHWAQ JAANNo ratings yet
- EGAC0401Document5 pagesEGAC0401bhanuprasadbkNo ratings yet
- Chandan Diagnostic Centre: Department of BiochemistryDocument2 pagesChandan Diagnostic Centre: Department of BiochemistryRupal RupalNo ratings yet
- Lab ReportDocument7 pagesLab Reportabdulsamad202000No ratings yet
- Lab ReportDocument1 pageLab ReportPreyashNo ratings yet
- Smart Full Body Checkup: Test Description Value(s) Unit(s) Reference RangeDocument13 pagesSmart Full Body Checkup: Test Description Value(s) Unit(s) Reference RangeShamsher SiddiqueNo ratings yet
- LFT ReportDocument3 pagesLFT Reportacer.tsk007No ratings yet
- District Civil Hospital, Panchkula, Department of LaboratoryDocument1 pageDistrict Civil Hospital, Panchkula, Department of LaboratoryGh WaniNo ratings yet
- PDF TextDocument3 pagesPDF TextPratyush SinghNo ratings yet
- LabReportNew - 2024-03-18T184949.154Document1 pageLabReportNew - 2024-03-18T184949.154desarajit72No ratings yet
- ReportDocument14 pagesReportWaseem FarooqNo ratings yet
- File - Report (1689931082736)Document6 pagesFile - Report (1689931082736)Inderjeet KaurNo ratings yet
- Test Report: Investigation Observed Value Unit Biological Ref. Interval SpecimenDocument2 pagesTest Report: Investigation Observed Value Unit Biological Ref. Interval SpecimensumaNo ratings yet
- Injury To The Colon and RectumDocument40 pagesInjury To The Colon and RectumLilibeth Tenorio De LeonNo ratings yet
- Magic Tee As An IsolatorDocument7 pagesMagic Tee As An IsolatorkrNo ratings yet
- 4 Huge Benefits of Meditation (And How To Get Started Today)Document16 pages4 Huge Benefits of Meditation (And How To Get Started Today)Jia Huay Chang (MY)No ratings yet
- English Grammar Test With AnswersDocument39 pagesEnglish Grammar Test With Answersmehari kirosNo ratings yet
- Master of Business Administration-MBA Semester 1 MB0048 - Operations Research - 4 Credits (Book ID: B1631) Assignment Set - 1 (60 Marks)Document7 pagesMaster of Business Administration-MBA Semester 1 MB0048 - Operations Research - 4 Credits (Book ID: B1631) Assignment Set - 1 (60 Marks)Vikas WaliaNo ratings yet
- Java Bca SlipsDocument30 pagesJava Bca SlipsNikhil GoudNo ratings yet
- Pangasinan State UniveristyDocument8 pagesPangasinan State UniveristyCha ChaNo ratings yet
- ChallengesDocument2 pagesChallengesChinmae XanthineNo ratings yet
- Scientific Paradigms and Economics - An Introduction Gerald E. PeabodyDocument16 pagesScientific Paradigms and Economics - An Introduction Gerald E. Peabody杜零No ratings yet
- Final Exam BriefingDocument9 pagesFinal Exam BriefingCatherine ChoiNo ratings yet
- My First Writing - Workbook 2 - Answer Key (E-Future)Document26 pagesMy First Writing - Workbook 2 - Answer Key (E-Future)Mona MohamedelsayedNo ratings yet
- Problem Set 1Document2 pagesProblem Set 1Tanzy SNo ratings yet
- Biasing in Magnetic Tape RecordingDocument4 pagesBiasing in Magnetic Tape RecordingkirillNo ratings yet
- 6.law and Morality Mr. Hitesh Agrawal PDFDocument18 pages6.law and Morality Mr. Hitesh Agrawal PDFjuhiNo ratings yet
- Activity of Artemisia Annua Capsules Versus Artemeter Lumefantrine On Uncomplicated MalariaDocument9 pagesActivity of Artemisia Annua Capsules Versus Artemeter Lumefantrine On Uncomplicated MalariaajmrdNo ratings yet
- How To Close A Loop in CAEPIPEDocument7 pagesHow To Close A Loop in CAEPIPEalmustanir_903004759No ratings yet
- Hill Criterion and Von MisesDocument10 pagesHill Criterion and Von MisesSiva PrasadNo ratings yet
- Identifying and Overcoming The Challenges of Implementing A Project Management OfficeDocument19 pagesIdentifying and Overcoming The Challenges of Implementing A Project Management OfficeLuis Enrique Palomino CañahueriNo ratings yet
- Taguig City UniversityDocument48 pagesTaguig City UniversityJayson CalbanNo ratings yet
- English7 Q3 M5Document15 pagesEnglish7 Q3 M5Mary Rose ReyesNo ratings yet
- Revised Neurophysiology of Pain QuestionnaireDocument2 pagesRevised Neurophysiology of Pain QuestionnaireivanNo ratings yet
- Jadwal Sholat Lima Waktu Masjid Al-Ikhlas Juni 2023Document1 pageJadwal Sholat Lima Waktu Masjid Al-Ikhlas Juni 2023febri agustian100% (1)
- Impacts of Imports, Exports and Foreign Direct Investment On The Gross Domestic Product (GDP) GrowthDocument2 pagesImpacts of Imports, Exports and Foreign Direct Investment On The Gross Domestic Product (GDP) Growthzee3000No ratings yet
- Introduction To Business ManagementDocument15 pagesIntroduction To Business ManagementSandhiya SureshNo ratings yet
- American Cinematographer - 2017 - 03Document96 pagesAmerican Cinematographer - 2017 - 03lucioNo ratings yet
- 1.for Print Handout - Encounter With JesusDocument3 pages1.for Print Handout - Encounter With JesusFeds Gula Jr.No ratings yet
- 8 Steps To Perfect English AccentDocument5 pages8 Steps To Perfect English Accentadhe hildaNo ratings yet
Report f642c 1704009629273
Report f642c 1704009629273
Uploaded by
Er Sumit SiwatchOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Report f642c 1704009629273
Report f642c 1704009629273
Uploaded by
Er Sumit SiwatchCopyright:
Available Formats
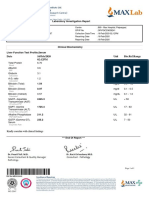
Name : Mr.
Sumit Siwatch Age / Sex : 31 Year(s) / Male Collected On : 31/12/2023 11:00 AM
Patient ID : OHPXWD5C619468 Ref. Doctor : Received On : 31/12/2023 11:40 AM
Visit No. : GG11746801 Client : Getvisit TPA Reported On : 31/12/2023 01:12 PM
Test Results Units Biological Reference Interval
BIOCHEMISTRY
Fasting Glucose 89 mg/dL Normal Fasting Glucose: 70-100
F- fluoride plasma,GOD-POD
Page 1 / 16
Dr. Radhika Puri Dr. Sanchit Singhal
MD Pathologist
MBBS, MD (Pathologist)
Consultant Pathologist
Name : Mr. Sumit Siwatch Age / Sex : 31 Year(s) / Male Collected On : 31/12/2023 11:00 AM
Patient ID : OHPXWD5C619468 Ref. Doctor : Received On : 31/12/2023 11:40 AM
Visit No. : GG11746801 Client : Getvisit TPA Reported On : 31/12/2023 01:12 PM
Test Results Units Biological Reference Interval
LFT - LIVER FUNCTION TEST
Serum
Total Bilirubin 0.9 mg/dL Adult: 0.2-1.3
Diazo Method Neonate: 1.0-10.5
Direct Bilirubin 0.10 mg/dL Neonate: 0.0-0.6
Calculated Adult: 0.0-0.3
Indirect Bilirubin 0.80 mg/dL Adult: 0.0-1.1
Spectrophotometry Neonate: 0.6-10.5
Aspartate Transaminase(AST/ 39 U/L 17-49
SGOT)
IFCC method
Alanine Transaminase(ALT/ 56 U/L < 50
SGPT)
IFCC method
Alkaline Phosphatase 122 U/L 38-126
IFCC method
Gamma-Glutamyl Transferase 44 U/L 15-73
(GGT)
Szasz method
Total Protein 7.2 g/dL 6.3-8.2
Cholesterol Oxidase
Albumin 4.5 g/dL 3.5-5.0
Bromo-Cresol Green
Globulin 2.7 g/dL 2.3-3.5
Calculated
A/G ratio 1.7 1.1-1.8
Calculated
Page 2 / 16
Dr. Radhika Puri Dr. Sanchit Singhal
MD Pathologist
MBBS, MD (Pathologist)
Consultant Pathologist
Name : Mr. Sumit Siwatch Age / Sex : 31 Year(s) / Male Collected On : 31/12/2023 11:00 AM
Patient ID : OHPXWD5C619468 Ref. Doctor : Received On : 31/12/2023 11:40 AM
Visit No. : GG11746801 Client : Getvisit TPA Reported On : 31/12/2023 01:12 PM
Test Results Units Biological Reference Interval
SGOT/SGPT- RATIO 0.7 0.7-1.4
Calculated
Total bilirubin is invariably increased in jaundice. Causes of jaundice are prehepatic, resulting from various hemolytic diseases; hepatic, resulting
from hepatocellular injury or obstruction; and posthepatic, resulting from obstruction of the hepatic or common bile ducts.
Aspartate aminotransferase is present in high activity in heart, skeletal muscle, and liver. Increased serum AST activity commonly follows
myocardial infarction, pulmonary emboli, skeletal muscle trauma, alcoholic cirrhosis, viral hepatitis, and drug-induced hepatitis.
Alanine aminotransferase is present in high activity in liver, skeletal muscle, heart, and kidney. Serum ALT increases rapidly in liver cell necrosis,
hepatitis, hepatic cirrhosis, liver tumours, obstructive jaundice, Reye’s syndrome, extensive trauma to skeletal muscle, myositis, myocarditis, and
myocardial infarction.
Alkaline phosphatase is elevated in fever and increased bone metabolism, for example, in adolescents and during the healing of a fracture;
primary and secondary hyperparathyroidism; Paget’s disease of bone; carcinoma metastatic to bone; osteogenic sarcoma; and Hodgkin’s disease if
bones are invaded. Hepatobiliary diseases involving cholestasis, inflammation, or cirrhosis increased ALP activity; also increased in renal infarction
and failure and in the complications of pregnancy. Low ALP activity may occasionally be seen in hypothyroidism.
Serum GGT is a sensitive indicator of hepatobiliary disease and is useful in the diagnosis of obstructive jaundice and chronic alcoholic liver
disease, in the follow-up of chronic alcoholics undergoing treatment, and in the detection of hepatotoxicity. GGT is more responsive to biliary
obstruction than AST, ALT, or ALP.
Total serum protein levels can be used for evaluation of nutritional status. Causes of high total serum protein concentration include dehydration,
Waldenström’s macroglobulinemia, multiple myeloma, hyperglobulinemia, granulomatous diseases, and some tropical diseases. Causes of low
total serum protein concentration include pregnancy, excessive intravenous fluid administration, cirrhosis or other liver diseases, chronic
alcoholism, heart failure, nephrotic syndrome, glomerulonephritis, neoplasia, protein-losing enteropathies, malabsorption, and severe malnutrition.
Page 3 / 16
Dr. Radhika Puri Dr. Sanchit Singhal
MD Pathologist
MBBS, MD (Pathologist)
Consultant Pathologist
Name : Mr. Sumit Siwatch Age / Sex : 31 Year(s) / Male Collected On : 31/12/2023 11:00 AM
Patient ID : OHPXWD5C619468 Ref. Doctor : Received On : 31/12/2023 11:40 AM
Visit No. : GG11746801 Client : Getvisit TPA Reported On : 31/12/2023 01:12 PM
Test Results Units Biological Reference Interval
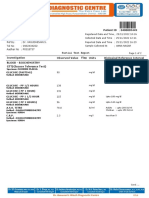
Kidney Function Test Mini
Serum
Urea 22 mg/dL 19-42
Urease
Creatinine 1.0 mg/dL 0.66-1.25
Twopoint Rate - Creatinine
Aminohydrolase
Blood Urea Nitrogen (BUN) 10.3 mg/dL 9.0-20.0
Calculated Newborn: 3.0-12.0
BUN Creatinine Ratio 10.3 0-24
Calculated
Uric Acid 6.6 mg/dL 3.5-8.5
Uricase
Calcium 9.1 mg/dL 8.4-10.2
Arsenazo Method
eGFR 103 ml/min/1.73 sq Normal: >= 90
Calculated m Mild decrease: 60-89
Mild moderate decrease: 45-59
Moderate to severe decrease: 30
-44
Severe decrese: 15-29
Kidney failure: < 15
Page 4 / 16
Dr. Radhika Puri Dr. Sanchit Singhal
MD Pathologist
MBBS, MD (Pathologist)
Consultant Pathologist
Name : Mr. Sumit Siwatch Age / Sex : 31 Year(s) / Male Collected On : 31/12/2023 11:00 AM
Patient ID : OHPXWD5C619468 Ref. Doctor : Received On : 31/12/2023 11:40 AM
Visit No. : GG11746801 Client : Getvisit TPA Reported On : 31/12/2023 01:12 PM
Test Results Units Biological Reference Interval
Lipid Profile with calculated LDL
Serum
Total Cholesterol 182 mg/dl < 200
CHOD-POD
Triglycerides 114 mg/dL < 150
GPO-POD
HDL Cholesterol 33 mg/dL > 50
Direct
Non-HDL Cholesterol 149 mg/dL < 130
Calculated
LDL Cholesterol 126 mg/dL < 100
Calculated
VLDL Cholesterol 23 mg/dL < 30
Calculated
Cholesterol / HDL Ratio 5.5 3.3-4.4
Calculated
LDL:HDL Ratio 4.0 0.5-3.0
Calculated
HDL/LDL RATIO 0.3 > 0.4
Calculated
Page 5 / 16
Dr. Radhika Puri Dr. Sanchit Singhal
MD Pathologist
MBBS, MD (Pathologist)
Consultant Pathologist
Name : Mr. Sumit Siwatch Age / Sex : 31 Year(s) / Male Collected On : 31/12/2023 11:00 AM
Patient ID : OHPXWD5C619468 Ref. Doctor : Received On : 31/12/2023 11:40 AM
Visit No. : GG11746801 Client : Getvisit TPA Reported On : 31/12/2023 01:12 PM
Test Results Units Biological Reference Interval
REMARKS TOTAL CHOLESTEROL(mg/dL) TRIGLYCERIDE(mg/dL) LDL CHOLESTEROL(mg/dL)
Optimal <200 <150 <100
Above Optimal - - 100-129
Borderline 200-239 150-199 130-159
High >=240 200-499 160-189
Very High - >=500 >=190
Lipid profile is a group test consisting of various lipids. Lipid profiles are generally collected with overnight fasting. However, Recent guidelines have
recommended non fasting samples for lipid profile for assessment of cardiovascular risk. The details for the study can be checked at
https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2733560
In certain instances measurements in the same patient can show physiological and analytical variations. In such cases three serial samples at an interval of 1
week each are recommended for Total cholesterol, TG, HDL and LDL.
Cholesterol levels are increased in primary hypercholesterolemia; secondary hyperlipoproteinemia, including nephrotic syndrome; primary biliary cirrhosis;
hypothyroidism; and in some cases, diabetes mellitus. Low cholesterol levels may be found in malnutrition, malabsorption, advanced malignancy, and
hyperthyroidism.
Triglyceride levels are used in the diagnosis and treatment of patients with diabetes mellitus, nephrosis, liver obstruction, other diseases involving lipid
metabolism, or various endocrine disorders.
High Density Lipoprotein (HDL) cholesterol levels is used to evaluate the risk of developing coronary heart disease (CHD). The risk of CHD increases with
lower HDL cholesterol concentrations.
LDL (low-density lipoprotein) cholesterol level, sometimes called “bad” cholesterol, makes up most of our body’s cholesterol. High levels of LDL cholesterol
raise your risk for heart disease and stroke.
Very-low-density lipoprotein (VLDL) cholesterol is produced in the liver and released into the bloodstream to supply body tissues with triglycerides. High
levels of VLDL cholesterol have
been associated with the development of plaque deposits on artery walls, which narrow the passage and restrict blood flow.
Page 6 / 16
Dr. Radhika Puri Dr. Sanchit Singhal
MD Pathologist
MBBS, MD (Pathologist)
Consultant Pathologist
Name : Mr. Sumit Siwatch Age / Sex : 31 Year(s) / Male Collected On : 31/12/2023 11:00 AM
Patient ID : OHPXWD5C619468 Ref. Doctor : Received On : 31/12/2023 11:40 AM
Visit No. : GG11746801 Client : Getvisit TPA Reported On : 31/12/2023 01:12 PM
Test Results Units Biological Reference Interval
IMMUNOLOGY
TSH-Thyroid Stimulating 1.363 µIU/mL 0.400-4.049
Hormone
Serum,ECLIA
Thyroid Stimulating Hormone (TSH), also called Thyrotropin is a hormone secreted into the blood by the Pituitary gland (a gland present in the
brain)). It signals the thyroid gland to make and release the thyroid hormones (T3 & T4) into the blood.
High TSH level indicates that the thyroid gland is not making enough thyroid hormone (primary hypothyroidism).
Low TSH level usually indicates that the thyroid is producing too much thyroid hormone (hyperthyroidism).
Factors influencing TSH levels:
Fasting: TSH level shows a significant decline after meal intake in comparison to fasting values. This may have clinical implications in the
diagnosis and management of hypothyroidism, especially Subclinical hypothyroidism.1
Circadian Rhythm: TSH levels follow a circadian variation, reaching peak levels between Morning 2 – 4 am and at a minimum between Evening 6-
10 pm. The variation is of the order of 50%. hence time of sample collection during a day can significantly influence on the measured serum TSH
concentrations.2
Other Factors: Genetics, Poisonous substances and radiation exposure, Inflammation of the thyroid gland, Deficiency or excess of iodine in the
diet, Pregnancy, Certain medications – antidepressants, cholesterol lowering drugs, chemotherapy drugs, steroids, Thyroid cancer.
References:
1. Indian Journal of Endocrinology and Metabolism 18(5):p 705-707, Sep–Oct 2014.)
2. efaidnbmnnnibpcajpcglclefindmkaj/http://www.pnei-it.com/1/upload/thyrotropin_secretion_patterns_i n_health_and_disease.pdf
In pregnant females the reference range of TSH differs. Please refer the table below for the same:-
PREGNANCY TSH REFERENCE RANGE(uIU/ML)
1st Trimester 0.100-2.500
2nd Trimester 0.200-3.00
3rd Trimester 0.300-3.00
Page 7 / 16
Dr. Radhika Puri
MBBS, MD (Pathologist)
Consultant Pathologist
Name : Mr. Sumit Siwatch Age / Sex : 31 Year(s) / Male Collected On : 31/12/2023 11:00 AM
Patient ID : OHPXWD5C619468 Ref. Doctor : Received On : 31/12/2023 11:40 AM
Visit No. : GG11746801 Client : Getvisit TPA Reported On : 31/12/2023 01:12 PM
Test Results Units Biological Reference Interval
Vitamin D (25 OH 33.4 ng/mL Deficient: < 20
Cholecalciferol) Insufficient: 20-30
Serum,ECLIA Sufficient: 30-100
Potential Toxicity: > 100
For diagnosis of vitamin D deficiency it is recommended to have clinical correlation with serum 25
(OH)vitamin D, serum calcium, serum PTH & serum alkaline phosphatase. During monitoring of oral vitamin
D therapy- suggested testing of serum 25(OH)vitamin D is after 12 weeks or 3 moths of treatment. However,
the required dosage of vitamin D supplements & time to achieve sufficient vitamin D levels show significant
seasonal (especially winter) & individual variability depending on age, body fat, sun exposure, physical
activity ,genetic factors (especially variable vitamin D receptor responses), associated liver or renal disease,
mal-absorption syndromes and calcium or magnesium deficiency influencing the vitamin D metabolism.
Page 8 / 16
Dr. Radhika Puri
MBBS, MD (Pathologist)
Consultant Pathologist
Name : Mr. Sumit Siwatch Age / Sex : 31 Year(s) / Male Collected On : 31/12/2023 11:00 AM
Patient ID : OHPXWD5C619468 Ref. Doctor : Received On : 31/12/2023 11:40 AM
Visit No. : GG11746801 Client : Getvisit TPA Reported On : 31/12/2023 01:12 PM
Test Results Units Biological Reference Interval
HEMATOLOGY
Complete Blood Count with ESR
Whole Blood
RBC count 5.36 mill/mm3 4.5-5.5
DC Impedance method
Haemoglobin (Hb) 16.6 g/dL 13.0-17.0
Cyanide-free SLS method
Haematocrit(PCV) 51.2 % 40-50
DC Impedance method
Mean Corpuscular Volume 95.6 fL 83-101
(MCV)
Calculated
Mean Corpuscular 31.0 pg 27-32
Haemoglobin(MCH)
Calculated
Mean Corpuscular 32.4 g/dL 31.5-34.5
Haemoglobin Concentration
(MCHC)
Calculated
Red cell distribution width 15.2 % 11.6-14.0
(RDW)
Calculated
Mentzer Index 18 Beta Thalassemia trait: < 14
Calculated Iron deficiency anemia: >= 14
Sehgal index 1705.1 Iron deficiency anemia: >= 972
Calculated Beta Thalassemia trait: < 972
Page 9 / 16
Dr. Radhika Puri
MBBS, MD (Pathologist)
Consultant Pathologist
Name : Mr. Sumit Siwatch Age / Sex : 31 Year(s) / Male Collected On : 31/12/2023 11:00 AM
Patient ID : OHPXWD5C619468 Ref. Doctor : Received On : 31/12/2023 11:40 AM
Visit No. : GG11746801 Client : Getvisit TPA Reported On : 31/12/2023 01:12 PM
Test Results Units Biological Reference Interval
Total WBC count - TC 3450 cells/cu.mm 4000-10000
Flow Cytometry
Comment Kindly correlate clinically and suggest follow-up.
Differential Leucocyte Count - DC
Flow Cytometry
Neutrophils 65.2 % 40-80
Lymphocytes 27.3 % 20-40
Monocytes 6.2 % 2-10
Eosinophils 0.4 % 1-6
Basophils 0.9 % 0-2
Absolute Neutrophil Count 2249 / cu.mm 2000-7000
Calculated
Absolute Lymphocyte Count 942 /cu.mm 1000-3000
Calculated
Absolute Monocyte Count 214 /cu.mm 200-1000
Calculated
Absolute Eosinophil Count 14 /cu.mm 20-500
Calculated
Absolute Basophil Count 31 /cu.mm 0-100
Calculated
Page 10 / 16
Dr. Radhika Puri
MBBS, MD (Pathologist)
Consultant Pathologist
Name : Mr. Sumit Siwatch Age / Sex : 31 Year(s) / Male Collected On : 31/12/2023 11:00 AM
Patient ID : OHPXWD5C619468 Ref. Doctor : Received On : 31/12/2023 11:40 AM
Visit No. : GG11746801 Client : Getvisit TPA Reported On : 31/12/2023 01:12 PM
Test Results Units Biological Reference Interval
Neutrophil Lymphocyte Ratio 2.4 Ratio 1.0-3.0
(NLR)
Calculated
Platelet count 160 10^3/ul 150-450
DC Impedance method
Mean Platelet Volume 9.8 fL 7-13
Calculated
Platelet haematocrit 0.16 % 0.2-0.5
Calculated
Erythrocyte Sedimentation 7 mm/hr 0-10
Rate
Quantitative Capillary Photometry
1. Reference Ranges are in accordance with Dacie & Lewis Practical Hematology International Edition (12th).
2. As per International Council for Standardization in Hematology's recommendations Differential Leucocyte counts are additionally reported in
Absolute numbers in each cell per unit volume of blood.
Page 11 / 16
Dr. Radhika Puri
MBBS, MD (Pathologist)
Consultant Pathologist
Name : Mr. Sumit Siwatch Age / Sex : 31 Year(s) / Male Collected On : 31/12/2023 11:00 AM
Patient ID : OHPXWD5C619468 Ref. Doctor : Received On : 31/12/2023 11:40 AM
Visit No. : GG11746801 Client : Getvisit TPA Reported On : 31/12/2023 01:12 PM
Test Results Units Biological Reference Interval
Glycosylated Haemoglobin - (HbA1c)
Whole Blood
Glycosylated Haemoglobin 5.4 % Normal: < 5.7
(HbA1c) Pre-Diabetes: 5.7-6.4
HPLC Diabetes: >= 6.5
Mean Blood Glucose 108.00
HbA1C:
HbA1C is used to monitor fluctuations in blood glucose concentration in the past 8 to 12 week’s period.
The reference interval defined as per American Diabetes Association guidelines 2016:
a) Less than 5.7% : Non Diabetic
b) 5.7 to 6.4% : at increased risk of developing diabetes in the future
c) More than 6.5% : Diabetic
d) Therapeutic glycemic target:
i. Adults: less than 7%
ii. Children with Type 1 diabetes : less than 7 %
e) Pregnant diabetic patients : less than 6.5%
Note:
• Targets may be individualized based on: Age/life expectancy, Comorbid conditions, Diabetes duration , Hypoglycemia status,
Individual patient considerations
Reference: American Diabetes Association. Standards of medical care in diabetes—2021.
Mean Blood Glucose is average Blood glucose which directly correlates with A1C, reported in the same units as blood sugar levels
(mg/dl). Thus it reflects the average glucose concentration in the past 8 to 12 weeks period. This should not be compared with
Fasting or Post prandial or random blood sugar which measures glucose concentration at that point of time of testing.
Page 12 / 16
Dr. Radhika Puri
MBBS, MD (Pathologist)
Consultant Pathologist
Name : Mr. Sumit Siwatch Age / Sex : 31 Year(s) / Male Collected On : 31/12/2023 11:00 AM
Patient ID : OHPXWD5C619468 Ref. Doctor : Received On : 31/12/2023 11:40 AM
Visit No. : GG11746801 Client : Getvisit TPA Reported On : 31/12/2023 01:12 PM
Test Results Units Biological Reference Interval
CLINICAL PATHOLOGY
Urine Complete Analysis
Stool/Urine
PHYSICAL EXAMINATION
Volume 30 ml
Colour Pale yellow Pale Yellow
Manual
Appearance clear Clear
Manual
CHEMICAL EXAMINATION
pH 8.0 5.0-8.0
Double indicator method
Specific gravity 1.015 1.001-1.035
Refractive Index
Protein Nil Nil
Protein error of pH indicator
Glucose Nil Nil
Enzyme method GOD POD
Ketone bodies Nil Nil
Dipstick
Bilirubin Nil Nil
Azo coupling method
Page 13 / 16
Dr. Radhika Puri Dr. Sanchit Singhal
MD Pathologist
MBBS, MD (Pathologist)
Consultant Pathologist
Name : Mr. Sumit Siwatch Age / Sex : 31 Year(s) / Male Collected On : 31/12/2023 11:00 AM
Patient ID : OHPXWD5C619468 Ref. Doctor : Received On : 31/12/2023 11:40 AM
Visit No. : GG11746801 Client : Getvisit TPA Reported On : 31/12/2023 01:12 PM
Test Results Units Biological Reference Interval
Blood Negative Negative
Peroxidase activity
Urobilinogen Normal Normal
Dipstick
Leucocyte Esterase Negative Negative
Granulocyte esterase method
Nitrites Negative Negative
Griess method
MICROSCOPY EXAMINATION
Pus cells 0-1 /hpf 0-5
Flow digital Imaging
Epithelial cells 0-1 /hpf Occasional
Fixed point immuno-rate
RBCs Nil /hpf 0-2
Flow digital Imaging
Uric acid Crystals Nil Nil
Flow digital Imaging
Phosphate Crystals Nil Nil
Flow digital Imaging
Calcium Oxalate Crystals Nil Nil
Flow digital Imaging
Granular Casts Nil Nil
Flow digital Imaging
Hyaline Casts Nil Nil
Flow digital Imaging
Page 14 / 16
Dr. Radhika Puri Dr. Sanchit Singhal
MD Pathologist
MBBS, MD (Pathologist)
Consultant Pathologist
Name : Mr. Sumit Siwatch Age / Sex : 31 Year(s) / Male Collected On : 31/12/2023 11:00 AM
Patient ID : OHPXWD5C619468 Ref. Doctor : Received On : 31/12/2023 11:40 AM
Visit No. : GG11746801 Client : Getvisit TPA Reported On : 31/12/2023 01:12 PM
Test Results Units Biological Reference Interval
Amorphous urates Nil Nil
Amorphous phosphates Nil Nil
Flow digital Imaging
Yeast Nil Nil
Flow digital Imaging
Bacteria Nil Nil
Flow digital Imaging
Parasites Nil Nil
Mucus Nil Nil
Flow digital Imaging
Page 15 / 16
Dr. Radhika Puri Dr. Sanchit Singhal
MD Pathologist
MBBS, MD (Pathologist)
Consultant Pathologist
Name : Mr. Sumit Siwatch Age / Sex : 31 Year(s) / Male Collected On : 31/12/2023 11:00 AM
Patient ID : OHPXWD5C619468 Ref. Doctor : Received On : 31/12/2023 11:40 AM
Visit No. : GG11746801 Client : Getvisit TPA Reported On : 31/12/2023 01:12 PM
Test Results Units Biological Reference Interval
Urine examination:
Increased protein in urine is seen in dehydration, kidney disorders, heart failure and transplant rejection. 24 hour urine protein and
Protein/creatinine ratio in a random urine sample recommended if increased.
Glucosuria can be seen in kidney disorders, uncontrolled diabetes mellitus, hormonal disorders, and pregnancy. To be correlated
with plasma glucose levels.
Ketonuria is seen in physical exercise, starvation, severe vomiting, exposure to cold, uncontrolled diabetes (diabetic ketoacidosis)
Increased bilirubin levels should be followed up with Liver function tests and indicates conjugated hyperbilirubinemia.
Increased urobilinogen can be seen due to haemolysis, megaloblastic anaemia and haemorrhage in tissues. Urobilinogen is
absent or reduced in obstructive liver disease and antibiotic therapy.
RBCs in urine (Haematuria) can be seen in anticoagulant therapy, bleeding diathesis and traumatic catheterization history to be
looked into. Dysmorphic RBCs suggestive of glomerular pathology. Non glomerular diseases line calculus, infections, tumours,
after strenuous exercise and diseases of the prostate.
Increase in pus cells are elevated in cases of UTI, to be correlated with urine culture, if clinically indicated. Infection can be in
either the upper or lower urinary tract or with acute glomerulonephritis, tubule interstitial nephritis. Leucocyte esterase detects
esterase enzyme released from the granules of leucocytes.
Infected urine may contain considerable amounts of nitrite as a result of bacterial nitrate reductase activity, and detection of nitrite
in urine is routinely used in the diagnosis of bacterial cystitis. It is indicative of the requirement of Urine culture and sensitivity
testing for identification and treatment of UTI.
Hyaline casts are seen normally (not associated with disease states); seen after strenuous exercise and with non renal diseases,
such as dehydration.
Granular casts can be seen in acute glomerulonephritis and pyelonephritis.
-- End of Report --
Tests marked with NABL symbol are accredited by NABL vide Certificate no MC-3278
Page 16 / 16
Dr. Radhika Puri Dr. Sanchit Singhal
MD Pathologist
MBBS, MD (Pathologist)
Consultant Pathologist
You might also like
- Exegesis Paper On 1 Corinthians 13Document11 pagesExegesis Paper On 1 Corinthians 13Elisa Medina AlbinoNo ratings yet
- Laboratory Test Report: Test Name Result Biological Reference Interval Uric AcidDocument5 pagesLaboratory Test Report: Test Name Result Biological Reference Interval Uric AcidBalraj EnjamuriNo ratings yet
- OSS Double-Agent Operations in World War IIDocument12 pagesOSS Double-Agent Operations in World War IIoscarherradonNo ratings yet
- Bullet Trajectory Reconstruction On Vehicles JFIDocument8 pagesBullet Trajectory Reconstruction On Vehicles JFIManolo BermeoNo ratings yet
- Report 190a3 1695110951228Document13 pagesReport 190a3 1695110951228Mohd Jaffer ShareefNo ratings yet
- Report bc90b 1710052260449Document11 pagesReport bc90b 1710052260449muralinaiduNo ratings yet
- Report Eaaf4 1695467677147Document16 pagesReport Eaaf4 1695467677147Mohd Jaffer ShareefNo ratings yet
- Subhra Pattnaik ReportDocument4 pagesSubhra Pattnaik ReportSubhra pattnaikNo ratings yet
- Nilesh Karani 13295 29-10-2023 20231029084151 StationerypdfmergedDocument22 pagesNilesh Karani 13295 29-10-2023 20231029084151 StationerypdfmergedsteelblackNo ratings yet
- CombinepdfDocument28 pagesCombinepdfNEETFIXNo ratings yet
- Po3979242722 431Document8 pagesPo3979242722 431NEETFIXNo ratings yet
- Report 9c0fcfa7Document3 pagesReport 9c0fcfa7Shivam SharmaNo ratings yet
- Biochemistry: Investigation Observed Value Unit Biological Reference IntervalDocument15 pagesBiochemistry: Investigation Observed Value Unit Biological Reference IntervalAshutoshNo ratings yet
- LFT (Liver Function Test) : Biological Reference Results Units Test NameDocument4 pagesLFT (Liver Function Test) : Biological Reference Results Units Test Namemetepraju0210No ratings yet
- Quadra Medical Services Pvt. LTD.: Department of PathologyDocument1 pageQuadra Medical Services Pvt. LTD.: Department of PathologyRiyaa SahaNo ratings yet
- Uetquwiuj 912083949Document4 pagesUetquwiuj 912083949TzvineZNo ratings yet
- YourDocument1 pageYourYashdeep Singh.kNo ratings yet
- N8 R 9 W3 Pupeyo RF RTWB 42 BRDocument2 pagesN8 R 9 W3 Pupeyo RF RTWB 42 BRPrashant KumarNo ratings yet
- Date 24/dec/2022 08:32AM 03/dec/22 09:33AM 26/nov/22 09:05AM Unit Bio Ref IntervalDocument11 pagesDate 24/dec/2022 08:32AM 03/dec/22 09:33AM 26/nov/22 09:05AM Unit Bio Ref IntervalAmit SinghNo ratings yet
- 1-Liver Function Test - PO3921596584-773 - 230517 - 125136Document4 pages1-Liver Function Test - PO3921596584-773 - 230517 - 125136Moksh GujjarNo ratings yet
- Date 16/feb/2020 02:12PM Unit Bio - Ref.Range: Laboratory Investigation ReportDocument1 pageDate 16/feb/2020 02:12PM Unit Bio - Ref.Range: Laboratory Investigation ReportBhupender SinghNo ratings yet
- Clinical Biochemistry: Test Report Reg - No Age Name::: Reg - Date Collection:: Received: 15-Jul-2019 / 09:25 AMDocument8 pagesClinical Biochemistry: Test Report Reg - No Age Name::: Reg - Date Collection:: Received: 15-Jul-2019 / 09:25 AMAnuradha KommojuNo ratings yet
- Department of Biochemistry Test Name Result Unit Bio. Ref. RangeDocument5 pagesDepartment of Biochemistry Test Name Result Unit Bio. Ref. RangeSudhanshuNo ratings yet
- PR1546497Document2 pagesPR1546497basavajsalagar1No ratings yet
- Report 8b3a3101Document11 pagesReport 8b3a3101Pooja AgarwalNo ratings yet
- ReportDocument3 pagesReportPawan MadhesiyaNo ratings yet
- Lab Report - ShivanandhamDocument7 pagesLab Report - ShivanandhamPO, ITDA BhadrachalamNo ratings yet
- Uk007 2223 006609Document3 pagesUk007 2223 006609Arpit KumarNo ratings yet
- Biochemistry Test Name Result Bio. Ref. Range Method: C-Reactive Protein 0-5 Immuno Turbidometric AssayDocument10 pagesBiochemistry Test Name Result Bio. Ref. Range Method: C-Reactive Protein 0-5 Immuno Turbidometric AssayAnkur DeyNo ratings yet
- LIVER PROFILE LFT Test Report Format Example Sample Template Drlogy Lab ReportDocument1 pageLIVER PROFILE LFT Test Report Format Example Sample Template Drlogy Lab ReportM ShafiqNo ratings yet
- Report ViewerDocument1 pageReport ViewermuhammadmoazmaalikNo ratings yet
- Patient Name Mr. Umesh Jain Uhid Lab No Sample Date Receiving Date 03/04/2021 11:40AMDocument1 pagePatient Name Mr. Umesh Jain Uhid Lab No Sample Date Receiving Date 03/04/2021 11:40AMAkshay ChaudhryNo ratings yet
- Ap Land Titling ActDocument7 pagesAp Land Titling ActmurtyaretyNo ratings yet
- PranithaDocument15 pagesPranithaKumar VijayNo ratings yet
- SnehaDocument3 pagesSneharazeena salamNo ratings yet
- Inborn Errors of Metabolism (Iem) Summary Report: Sr. No. Test Methodology Result Test TypeDocument2 pagesInborn Errors of Metabolism (Iem) Summary Report: Sr. No. Test Methodology Result Test TypeMallikharjunaRao medaNo ratings yet
- Document 4Document5 pagesDocument 4mehtanagina682No ratings yet
- PdfText - 2023-12-12T152233.242Document2 pagesPdfText - 2023-12-12T152233.242joshipriya208No ratings yet
- Biochemistry CDCL CDCL-14403 17-18Document1 pageBiochemistry CDCL CDCL-14403 17-18Ashutosh SinghNo ratings yet
- Biochemistry CDCL CDCL-14403 17-18 PDFDocument1 pageBiochemistry CDCL CDCL-14403 17-18 PDFAshutosh SinghNo ratings yet
- Liver Function Test (Lft-A)Document4 pagesLiver Function Test (Lft-A)ce mgnregsNo ratings yet
- Report GNDocument3 pagesReport GNPawan MadhesiyaNo ratings yet
- Mrs Nandhinidevi.M 04007180: Sid No. Patient ID 0400005449Document2 pagesMrs Nandhinidevi.M 04007180: Sid No. Patient ID 040000544911F10 RUCHITA MAARANNo ratings yet
- LabReportNew - 2023-09-08T160827.328Document3 pagesLabReportNew - 2023-09-08T160827.328viraj kshirsagarNo ratings yet
- PdfText - 2024-03-15T191650.936Document1 pagePdfText - 2024-03-15T191650.936jayanthmahesh0403No ratings yet
- Haematology: Investigation Observed Value Unit Biological Reference IntervalDocument9 pagesHaematology: Investigation Observed Value Unit Biological Reference Intervalsunita hoskotiNo ratings yet
- LabTest 30nov2023Document5 pagesLabTest 30nov2023Ritu SinghNo ratings yet
- Mrs Sonali Upadhiya: Interpretation: Interpretation For Hba1C% As Per American Diabetes Association (Ada)Document3 pagesMrs Sonali Upadhiya: Interpretation: Interpretation For Hba1C% As Per American Diabetes Association (Ada)CHINMAY UPADHYAYA X-DNo ratings yet
- Department of Chemical Pathology: Liver Function TestsDocument3 pagesDepartment of Chemical Pathology: Liver Function TestsbabarchuhanNo ratings yet
- Apollo247 249052700 LabreportDocument7 pagesApollo247 249052700 LabreportASHWAQ JAANNo ratings yet
- EGAC0401Document5 pagesEGAC0401bhanuprasadbkNo ratings yet
- Chandan Diagnostic Centre: Department of BiochemistryDocument2 pagesChandan Diagnostic Centre: Department of BiochemistryRupal RupalNo ratings yet
- Lab ReportDocument7 pagesLab Reportabdulsamad202000No ratings yet
- Lab ReportDocument1 pageLab ReportPreyashNo ratings yet
- Smart Full Body Checkup: Test Description Value(s) Unit(s) Reference RangeDocument13 pagesSmart Full Body Checkup: Test Description Value(s) Unit(s) Reference RangeShamsher SiddiqueNo ratings yet
- LFT ReportDocument3 pagesLFT Reportacer.tsk007No ratings yet
- District Civil Hospital, Panchkula, Department of LaboratoryDocument1 pageDistrict Civil Hospital, Panchkula, Department of LaboratoryGh WaniNo ratings yet
- PDF TextDocument3 pagesPDF TextPratyush SinghNo ratings yet
- LabReportNew - 2024-03-18T184949.154Document1 pageLabReportNew - 2024-03-18T184949.154desarajit72No ratings yet
- ReportDocument14 pagesReportWaseem FarooqNo ratings yet
- File - Report (1689931082736)Document6 pagesFile - Report (1689931082736)Inderjeet KaurNo ratings yet
- Test Report: Investigation Observed Value Unit Biological Ref. Interval SpecimenDocument2 pagesTest Report: Investigation Observed Value Unit Biological Ref. Interval SpecimensumaNo ratings yet
- Injury To The Colon and RectumDocument40 pagesInjury To The Colon and RectumLilibeth Tenorio De LeonNo ratings yet
- Magic Tee As An IsolatorDocument7 pagesMagic Tee As An IsolatorkrNo ratings yet
- 4 Huge Benefits of Meditation (And How To Get Started Today)Document16 pages4 Huge Benefits of Meditation (And How To Get Started Today)Jia Huay Chang (MY)No ratings yet
- English Grammar Test With AnswersDocument39 pagesEnglish Grammar Test With Answersmehari kirosNo ratings yet
- Master of Business Administration-MBA Semester 1 MB0048 - Operations Research - 4 Credits (Book ID: B1631) Assignment Set - 1 (60 Marks)Document7 pagesMaster of Business Administration-MBA Semester 1 MB0048 - Operations Research - 4 Credits (Book ID: B1631) Assignment Set - 1 (60 Marks)Vikas WaliaNo ratings yet
- Java Bca SlipsDocument30 pagesJava Bca SlipsNikhil GoudNo ratings yet
- Pangasinan State UniveristyDocument8 pagesPangasinan State UniveristyCha ChaNo ratings yet
- ChallengesDocument2 pagesChallengesChinmae XanthineNo ratings yet
- Scientific Paradigms and Economics - An Introduction Gerald E. PeabodyDocument16 pagesScientific Paradigms and Economics - An Introduction Gerald E. Peabody杜零No ratings yet
- Final Exam BriefingDocument9 pagesFinal Exam BriefingCatherine ChoiNo ratings yet
- My First Writing - Workbook 2 - Answer Key (E-Future)Document26 pagesMy First Writing - Workbook 2 - Answer Key (E-Future)Mona MohamedelsayedNo ratings yet
- Problem Set 1Document2 pagesProblem Set 1Tanzy SNo ratings yet
- Biasing in Magnetic Tape RecordingDocument4 pagesBiasing in Magnetic Tape RecordingkirillNo ratings yet
- 6.law and Morality Mr. Hitesh Agrawal PDFDocument18 pages6.law and Morality Mr. Hitesh Agrawal PDFjuhiNo ratings yet
- Activity of Artemisia Annua Capsules Versus Artemeter Lumefantrine On Uncomplicated MalariaDocument9 pagesActivity of Artemisia Annua Capsules Versus Artemeter Lumefantrine On Uncomplicated MalariaajmrdNo ratings yet
- How To Close A Loop in CAEPIPEDocument7 pagesHow To Close A Loop in CAEPIPEalmustanir_903004759No ratings yet
- Hill Criterion and Von MisesDocument10 pagesHill Criterion and Von MisesSiva PrasadNo ratings yet
- Identifying and Overcoming The Challenges of Implementing A Project Management OfficeDocument19 pagesIdentifying and Overcoming The Challenges of Implementing A Project Management OfficeLuis Enrique Palomino CañahueriNo ratings yet
- Taguig City UniversityDocument48 pagesTaguig City UniversityJayson CalbanNo ratings yet
- English7 Q3 M5Document15 pagesEnglish7 Q3 M5Mary Rose ReyesNo ratings yet
- Revised Neurophysiology of Pain QuestionnaireDocument2 pagesRevised Neurophysiology of Pain QuestionnaireivanNo ratings yet
- Jadwal Sholat Lima Waktu Masjid Al-Ikhlas Juni 2023Document1 pageJadwal Sholat Lima Waktu Masjid Al-Ikhlas Juni 2023febri agustian100% (1)
- Impacts of Imports, Exports and Foreign Direct Investment On The Gross Domestic Product (GDP) GrowthDocument2 pagesImpacts of Imports, Exports and Foreign Direct Investment On The Gross Domestic Product (GDP) Growthzee3000No ratings yet
- Introduction To Business ManagementDocument15 pagesIntroduction To Business ManagementSandhiya SureshNo ratings yet
- American Cinematographer - 2017 - 03Document96 pagesAmerican Cinematographer - 2017 - 03lucioNo ratings yet
- 1.for Print Handout - Encounter With JesusDocument3 pages1.for Print Handout - Encounter With JesusFeds Gula Jr.No ratings yet
- 8 Steps To Perfect English AccentDocument5 pages8 Steps To Perfect English Accentadhe hildaNo ratings yet