Professional Documents
Culture Documents
Cronion2018 Vírus e Síndrome
Cronion2018 Vírus e Síndrome
Uploaded by
beatriceandrade97Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cronion2018 Vírus e Síndrome
Cronion2018 Vírus e Síndrome
Uploaded by
beatriceandrade97Copyright:
Available Formats
POSTER VIEWING I Tuesday 1 May 2018 iii43
Tuesday 1 May 2018
POSTER VIEWING I
suppressing IL-1b, IL-6 and IL-23-releasing antigen-presenting cells,
disrupting induction of Th17 cells. Corticosteroids are however
POSTER ABSTRACT SESSION associated with significant morbidity including osteoporosis, diabetes
mellitus, hypertension and infection. At least two distinct CD4 T-cell
subsets promote vascular inflammation in GCA and as a consequence
a number of cytokines have been implicated in the pathogenesis of the
001 SUCCESSFUL TREATMENT OF EPSTEIN BARR VIRUS- disease including TNF-a, IL-1 and IL-6, IFN-g and IL-17. Trials looking
TRIGGERED MACROPHAGE ACTIVATION SYNDROME IN A at TNF-a inhibitors have been disappointing whilst trials of IL-1, IL-6
PATIENT WITH SYSTEMIC JUVENILE IDIOPATHIC ARTHRITIS and IL-23 blockade are ongoing. In light of this, we report a case of a
patient with a background of psoriatic arthritis treated with adalimu-
Owen Cronin1, Euan McRorie1 and Mohini Gray1,2
1 mab (anti-TNF-a) who developed GCA and has subsequently been
Rheumatic Diseases Unit, Western General Hospital, Edinburgh,
managed successfully with the IL-17 inhibitor secukinumab, licensed
UNITED KINGDOM, and 2MRC Centre for Inflammation Research,
for use in psoriatic arthritis, psoriasis and ankylosing spondylitis.
The University of Edinburgh, Edinburgh, UNITED KINGDOM
Downloaded from https://academic.oup.com/rheumatology/article/57/suppl_3/key075.225/4971125 by guest on 22 January 2024
Methods: A 70 year old male was admitted with a one week history of
Background: Macrophage activation syndrome (MAS) is a potentially fever, dry cough, and occipital headache. Past medical history
life-threatening complication of inflammatory rheumatic disorders, included psoriatic arthritis, diagnosed in 2013, and managed with
most commonly occurring in patients with systemic-onset juvenile fortnightly 40mg subcutaneous injections of adalimumab since
idiopathic arthritis (JIA). It is characterised by an inappropriate, February 2015 with remission achieved shortly after its introduction.
aggressive cascade of pro-inflammatory cytokine release from innate Results: On admission investigations showed a CRP of 233mg/L, a
immune cells, driven by dysfunctional activation and uncontrolled WBC of 14.2 x109/L. (3.5-11.0) and negative blood cultures. His chest
expansion of macrophages and T-lymphocytes. Recognition of the x-ray, T-spot and sputum culture were normal. He was started on
clinical features of MAS is the first step in preventing mortality. broad spectrum antibiotics for sepsis of unknown origin but had no
Mortality rates in patients with JIA are in the region of 8%. Episodes of clinical response and the temperature and CRP remained elevated.
MAS triggered by host infection pose challenging therapeutic Further investigations including a CT scan of his head, chest, abdomen
dilemmas for the treating clinician, including careful consideration of and pelvis, and lumbar puncture with CSF analysis were carried out
the balance between effective pharmacological blockade of immune and did not demonstrate any source of sepsis. A left temporal artery
over-stimulation, and avoidance of excessive immunosuppression in biopsy was performed and the histological features were characteristic
the face of pathogenic microbial threat. of GCA. He was started on 40mg of oral prednisolone, and his fevers
Methods: We performed a retrospective case review of the success- and inflammatory markers settled within 48 hours. He remained on
ful management of MAS triggered by significant Epstein Barr virus adalimumab but his psoriatic arthritis flared and corticosteroid
(EBV) infection, in a patient with systemic JIA in the rheumatic diseases requirement for the GCA remained high. Three months later adalimu-
unit, Edinburgh. mab was stopped and he was started on secukinumab (anti-IL-17). At
Results: We report a case of a 22-year-old male with JIA, presenting review four months later both the psoriatic arthritis and GCA were in
with unremitting high fevers, widespread lymphadenopathy and remission and his CRP had normalised on low dose corticosteroids.
splenomegaly. Preceding history suggested a viral prodrome prior to Nine months after presentation with GCA, this man remains well on low
presentation to the emergency department. Laboratory abnormalities dose corticosteroids and secukinumab.
on presentation including thrombocytopenia (platelet count of 69 Conclusion: There is evidence to suggest that IL-17 is implicated in
x109), hyperferritinemia (15,433 mg/l), hypertriglyceridemia (2.1mmol/ the pathogenesis of GCA along with other cytokines. Whether the
L), and low fibrinogen levels (1.2g/L), led to a diagnosis of MAS in remission is sustained when corticosteroids are stopped remains to be
accordance with the 2016 ACR/EULAR classification criteria. A seen.
thorough diagnostic work-up was performed revealing extremely Disclosures: The authors have declared no conflicts of interest.
elevated titres of EBV DNA (titre ¼ 28,746 IU/L) in the peripheral
blood. Clinical concerns of an EBV-associated lymphoma were
eliminated following bone marrow biopsy and axillary lymph node 003 CARDIAC SARCOIDOSIS IDENTIFIED ON MRI OR
sampling that revealed the presence of EBV-positive cells but no PET-CT
evidence of an EBV-associated lymphoproliferative disorder. In this Ella Daniels1, Lucia Chen1, Catherine Hughes1, Shirish Sangle1 and
case, the patient’s usual immunosuppression was withheld on David D’Cruz1
presentation (weekly oral methotrexate (5mg) and subcutaneous 1
Rheumatology, Guy’s and St Thomas’ NHS Foundation Trust,
injections of the humanised anti-IL-6 receptor monoclonal antibody, London, UNITED KINGDOM
tocilizumab). The patient was treated with intravenous methylpredni-
solone (3 pulses of 1000mg) and one dose of intravenous immunoglo- Background: Sarcoidosis is a multisystemic non-caseating granulo-
bulin (2g/kg). He was monitored as an inpatient for six days with matous disorder of unknown aetiology. Clinical manifestations of
supportive care including IV fluids and analgesia. Over the course of cardiac sarcoidosis vary depending on the location and extent of
eight weeks EBV DNA viral load reduced without the need for anti-viral granulomatous inflammation. It can occur insidiously, present with
treatment and our patient made a full recovery. Usual immunosup- conduction abnormalities, heart failure or sudden cardiac death.
pression was recommenced at five weeks post-presentation. Only 5-10% of cases present with serious cardiac dysfunction,
Conclusion: Epstein Barr virus is an acknowledged trigger for macro- whereas up to 50% of patients can be asymptomatic.
phage activation syndrome in patients with autoimmune rheumatic For these reasons cardiac sarcoidosis remains a diagnostic challenge.
disease. In this case MAS was successfully treated with intravenous Diagnosis relies on Positron Emission Tomography - Computed
immunoglobulin with concurrent cessation of immunosuppression Tomography (PET-CT), cardiac Magnetic Resonance Imaging (MRI),
following identification of the causative organism. We propose that or histopathology. This poster will compare two cases of cardiac
treatment of MAS in rheumatic disorders may be stratified based on the involvement identified on cardiac MRI and PET-CT in patients with
precipitating cause e.g. viral, bacterial infection or others. known sarcoidosis.
Disclosures: The authors have declared no conflicts of interest. Methods: This is a case report describing two cases. Full informed
written patient consent was obtained.
Results: Case one is a 48 year old female with pulmonary sarcoidosis,
002 BIOPSY PROVEN GIANT CELL ARTERITIS IN A PATIENT who presented with a new rash, intermittent pyrexia and a vague
WITH PSORIATIC ARTHRITIS ON TNF-ALPHA INHIBITOR history of unexplained arrhythmias. ACE was elevated at 146. She
TREATED WITH HIGH DOSE PREDNISOLONE AND A SWITCH underwent a PET-CT scan, which demonstrated focal diffuse uptake
TO SECUKINUMAB (ANTI IL-17) within the myocardium. This was in keeping with active myocarditis
Luke Sammut1, Anna Litwic1, Richard Smith1 and Sarah Bartram1 secondary to sarcoidosis. There were no specific abnormalities
1
Rheumatology, Salisbury NHS Foundation Trust, Salisbury, UNITED identified on her cardiac MRI.
KINGDOM Case two is a 56 year old female with lupus and sarcoid overlap. She
presented with weight loss and breathlessness with a dramatic
Background: Corticosteroids remain the mainstay of treatment in troponin and BNP rise. PET-CT findings were non-specific, however
giant cell arteritis (GCA). Corticosteroids treat GCA by selectively cardiac MRI found focal epicardial fibrosis in the basal anterolateral
You might also like
- Government Departments Contact Emails/Phone Numbers EtcDocument149 pagesGovernment Departments Contact Emails/Phone Numbers EtcPaul Smith0% (1)
- Gateway-and-Apple 1111Document5 pagesGateway-and-Apple 1111Khulan Tsetsegmaa100% (3)
- Detailed Lesson Plan in TLE VIIDocument3 pagesDetailed Lesson Plan in TLE VIIJose Nilo Pastorall70% (10)
- SS Number State CodesDocument5 pagesSS Number State CodesCharles Kimbrough Sr.0% (1)
- "The Mammogram Myth" by Rolf HeftiDocument3 pages"The Mammogram Myth" by Rolf HeftiRolf HeftiNo ratings yet
- Offshore Engineer-February 2015Document84 pagesOffshore Engineer-February 2015ilkerkozturk100% (2)
- Spotify Strategig Possining and Product Life Cycle Four Basic Stages.Document5 pagesSpotify Strategig Possining and Product Life Cycle Four Basic Stages.Jorge YeshayahuNo ratings yet
- Evan Syndrome A Case ReportDocument3 pagesEvan Syndrome A Case ReportEditor IJTSRDNo ratings yet
- Respiratory and Pulmonary Medicine: ClinmedDocument3 pagesRespiratory and Pulmonary Medicine: ClinmedGrace Yuni Soesanti MhNo ratings yet
- Management of HemophagocyticDocument10 pagesManagement of HemophagocyticAlexander CanoNo ratings yet
- Purpura y PfizerDocument9 pagesPurpura y PfizerGerardo de Gyves AvilaNo ratings yet
- Article Koskina ArchDocument8 pagesArticle Koskina ArchElli SymeonidouNo ratings yet
- COVID-19 Related Acute Necrotizing Encephalopathy Presenting in The Early Postoperative PeriodDocument8 pagesCOVID-19 Related Acute Necrotizing Encephalopathy Presenting in The Early Postoperative PeriodElli SymeonidouNo ratings yet
- Mycobacterium Avium-Intracellulare Complex Pleurisy in A Patient With Lupus-Dermatomyositis Overlap SyndromeDocument3 pagesMycobacterium Avium-Intracellulare Complex Pleurisy in A Patient With Lupus-Dermatomyositis Overlap SyndromeSergio David Foronda ZuletaNo ratings yet
- Haemophagocytic Lymphohistiocytosis Associated With Dengue Fever - A Case SeriesDocument5 pagesHaemophagocytic Lymphohistiocytosis Associated With Dengue Fever - A Case Seriesdrmurad321No ratings yet
- Nej Mo A 2107051Document9 pagesNej Mo A 2107051bagholderNo ratings yet
- Adjunct Immune Globulin For Vaccine-Induced Immune Thrombotic ThrombocytopeniaDocument9 pagesAdjunct Immune Globulin For Vaccine-Induced Immune Thrombotic ThrombocytopeniaNi'ma NurmagfirahNo ratings yet
- A Case Report of Invasive Aspergillosis in A Patient Treated With RuxolitinibDocument3 pagesA Case Report of Invasive Aspergillosis in A Patient Treated With RuxolitinibJongga SiahaanNo ratings yet
- Covid Asociado A CoagulopatiaDocument2 pagesCovid Asociado A CoagulopatiaNahui IcatlNo ratings yet
- Cardiac Leptospirosis: Iralphuaborque Md14thbatch Hds DocharlabardaDocument15 pagesCardiac Leptospirosis: Iralphuaborque Md14thbatch Hds DocharlabardaJr. CesingNo ratings yet
- Ijam-3775 CDocument3 pagesIjam-3775 Carunkumar kumararunNo ratings yet
- Labmed36 0419 PDFDocument5 pagesLabmed36 0419 PDFRahul K. JagaNo ratings yet
- Clinical ImmunologyDocument5 pagesClinical ImmunologyiuventasNo ratings yet
- A Case of Covaxin-Induced Focal Sclerosing Glomerulonephritis (Collapsing Variety)Document4 pagesA Case of Covaxin-Induced Focal Sclerosing Glomerulonephritis (Collapsing Variety)bijgimNo ratings yet
- Nej Mo A 2308917Document14 pagesNej Mo A 2308917mnf6bb2tckNo ratings yet
- Genet 1996Document1 pageGenet 1996Araceli Enríquez OvandoNo ratings yet
- COVID-19 Presentation in Association With Myasthenia Gravis. ADocument4 pagesCOVID-19 Presentation in Association With Myasthenia Gravis. Aarenasgrecia1No ratings yet
- Meller FUODocument6 pagesMeller FUOJohannes MellerNo ratings yet
- Revista Clínica EspañolaDocument3 pagesRevista Clínica EspañolaJuan Alonso Leon-AbarcaNo ratings yet
- IVIG Treatment in HIVDocument2 pagesIVIG Treatment in HIVovirosNo ratings yet
- COVID-19-associated Immune ThrombocytopeniaDocument7 pagesCOVID-19-associated Immune ThrombocytopeniaDr Varshil ShahNo ratings yet
- Wright Et Al. 2016 - Ankylosing Spondylitis Patients Display Altered Den ... Hogenic Roles For The-AnnotatedDocument13 pagesWright Et Al. 2016 - Ankylosing Spondylitis Patients Display Altered Den ... Hogenic Roles For The-AnnotatedmuamarrayNo ratings yet
- Adult Still's Disease and Respiratory Failure in A 74 Year Old WomanDocument3 pagesAdult Still's Disease and Respiratory Failure in A 74 Year Old WomanEduardo Romero StéfaniNo ratings yet
- Junal PyodermaDocument6 pagesJunal PyodermaJares Clinton Saragih SimarmataNo ratings yet
- CeaaDocument3 pagesCeaaAlfi RahmatikaNo ratings yet
- Case Report: Severe Hyperbilirubinemia: A Rare Complication of Lyme DiseaseDocument4 pagesCase Report: Severe Hyperbilirubinemia: A Rare Complication of Lyme DiseaseDhruva PatelNo ratings yet
- American J Hematol - 1999 - Grumbeck - Macrocytic Anemia and Thrombocytosis Associated With Thymoma A Case ReportDocument4 pagesAmerican J Hematol - 1999 - Grumbeck - Macrocytic Anemia and Thrombocytosis Associated With Thymoma A Case ReportVengky UtamiNo ratings yet
- Lupus SeverDocument3 pagesLupus SeverdeliaNo ratings yet
- Importancia de Las Imágenes y El Diagnóstico Etiológico en El Paciente Inmunocomprometido Con Afección Del SNCDocument9 pagesImportancia de Las Imágenes y El Diagnóstico Etiológico en El Paciente Inmunocomprometido Con Afección Del SNCFranciely GarridoNo ratings yet
- AACE Clinical Case Reports: Manthan Pandya, MD, Geethika Thota, MD, Xiangbing Wang, MD, Hongxiu Luo, MDDocument3 pagesAACE Clinical Case Reports: Manthan Pandya, MD, Geethika Thota, MD, Xiangbing Wang, MD, Hongxiu Luo, MDSameerNo ratings yet
- 58 - 18015erdheim ChesterDocument5 pages58 - 18015erdheim ChesterGerman HaroNo ratings yet
- PIIS2213260020302678Document9 pagesPIIS2213260020302678kayegi8666No ratings yet
- International Journal of Infectious DiseasesDocument2 pagesInternational Journal of Infectious DiseasesAtikaNo ratings yet
- Granulomatose Eosinophilique Avec Polyangeite: Presentations Inhabituelles. Eosinophilic Granulomatosis With Polyangiitis: Unusual PresentationsDocument5 pagesGranulomatose Eosinophilique Avec Polyangeite: Presentations Inhabituelles. Eosinophilic Granulomatosis With Polyangiitis: Unusual PresentationsIJAR JOURNALNo ratings yet
- An Atypical Presentation of Kikuchi-Fujimoto Disease Mimicking Systemic Lupus Erythematosus: Case Report and Literature ReviewDocument5 pagesAn Atypical Presentation of Kikuchi-Fujimoto Disease Mimicking Systemic Lupus Erythematosus: Case Report and Literature Reviewzulfikar adiNo ratings yet
- Cryptococcal Postinfectious Inflammatory Response Syndrome in An Immunocompetent HostDocument3 pagesCryptococcal Postinfectious Inflammatory Response Syndrome in An Immunocompetent HostinfectogoNo ratings yet
- Endocard BartonDocument4 pagesEndocard BartonKrull TTTeamNo ratings yet
- Lupus Dupa InterferonDocument3 pagesLupus Dupa InterferondeliaNo ratings yet
- Tuberculous Pericarditis Leading To Cardiac Tamponade Importance of Screening Prior To ImmunosuppressionDocument3 pagesTuberculous Pericarditis Leading To Cardiac Tamponade Importance of Screening Prior To ImmunosuppressionLink BuiNo ratings yet
- Severe Hyponatremia Triggered by Immune Checkpoint Inhibi - 2024 - AACE ClinicalDocument4 pagesSevere Hyponatremia Triggered by Immune Checkpoint Inhibi - 2024 - AACE ClinicalronaldwquezadaNo ratings yet
- Artigo Neuromeningeal Cryptococcosis in A Patient Not Infected With HumanDocument4 pagesArtigo Neuromeningeal Cryptococcosis in A Patient Not Infected With HumanRENATA SANTOS ASSUNCAONo ratings yet
- Leptospirosis Presenting As Severe Cardiogenic Shock: A Case ReportDocument3 pagesLeptospirosis Presenting As Severe Cardiogenic Shock: A Case ReportFirdha GitaNo ratings yet
- 10 Relato de Caso Acute CoronaryDocument4 pages10 Relato de Caso Acute CoronaryAsis FitrianaNo ratings yet
- Secondary Hemophagocytic Lymphohistiocytosis: A Rare Case ReportDocument5 pagesSecondary Hemophagocytic Lymphohistiocytosis: A Rare Case ReportivanNo ratings yet
- Successful Treatment of Vaccine-Induced Prothrombotic Immune Thrombocytopenia (VIPIT)Document4 pagesSuccessful Treatment of Vaccine-Induced Prothrombotic Immune Thrombocytopenia (VIPIT)Ravi KumarNo ratings yet
- Unusual Cause of Fever in A 35-Year-Old Man: ECP YuenDocument4 pagesUnusual Cause of Fever in A 35-Year-Old Man: ECP YuenhlNo ratings yet
- Gangi Et Al 2021 Imaging and Hematologic Findings in Thrombosis and Thrombocytopenia After Chadox1 Ncov 19Document8 pagesGangi Et Al 2021 Imaging and Hematologic Findings in Thrombosis and Thrombocytopenia After Chadox1 Ncov 19Valentina EnacheNo ratings yet
- A Case of Vaccine-Associated Myocarditis Following Pneumococcal Immunization Leading To Acute Mitral RegurgitationDocument8 pagesA Case of Vaccine-Associated Myocarditis Following Pneumococcal Immunization Leading To Acute Mitral RegurgitationAlina Elisabeta Tiniuc căs LehaciNo ratings yet
- 25 Kawasaki DiseaseDocument13 pages25 Kawasaki DiseaseVictor PazNo ratings yet
- PIIS1198743X14652605Document3 pagesPIIS1198743X14652605Gerald NacoNo ratings yet
- Casos Medicina InternaDocument219 pagesCasos Medicina Internazara galiciaNo ratings yet
- Could COVID-19 Induce Remission of Acute LeukemiaDocument5 pagesCould COVID-19 Induce Remission of Acute LeukemiaAhmed RichiNo ratings yet
- ECR01 FullDocument2 pagesECR01 FullJUAN MARTIN REYNOSO RAMIREZNo ratings yet
- 2 +Severe+LeptospirosisDocument6 pages2 +Severe+LeptospirosisYhuzz Toma5No ratings yet
- Acute Meningitis Complicated by Transverse Myelitis: Case ReportDocument2 pagesAcute Meningitis Complicated by Transverse Myelitis: Case ReportSeptian TheaNo ratings yet
- ArticuloDocument6 pagesArticuloWillyPeñaNo ratings yet
- Steamshovel Press Issue 04Document60 pagesSteamshovel Press Issue 04liondog1No ratings yet
- For StatDocument47 pagesFor StatLyn VeaNo ratings yet
- ED6008Document4 pagesED6008VolvoxdjNo ratings yet
- Proforma Invoice: TOTAL:300000 Meters $3,900,000Document3 pagesProforma Invoice: TOTAL:300000 Meters $3,900,000Eslam A. AliNo ratings yet
- Addiction Is A Family IllnessDocument21 pagesAddiction Is A Family IllnessMarla100% (1)
- Mathematics: Quarter 3 - Module 5: Independent & Dependent EventsDocument19 pagesMathematics: Quarter 3 - Module 5: Independent & Dependent EventsAlexis Jon NaingueNo ratings yet
- Zero Moment Point ZMP Elysium LabsDocument3 pagesZero Moment Point ZMP Elysium LabsKaren DuarteNo ratings yet
- The Eternal VeritiesDocument81 pagesThe Eternal VeritiesDr Jacquelyn PY SooNo ratings yet
- How To Install The Data Protector License KeyDocument4 pagesHow To Install The Data Protector License KeyHillary Johnson0% (1)
- International Capital BudgetingDocument29 pagesInternational Capital BudgetingSaadat ShaikhNo ratings yet
- Ebook Contemporary Issues in Accounting 2Nd Edition Rankin Solutions Manual Full Chapter PDFDocument53 pagesEbook Contemporary Issues in Accounting 2Nd Edition Rankin Solutions Manual Full Chapter PDFfideliamaximilian7pjjf100% (11)
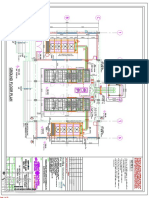
- Dg-1 (Remote Radiator) Above Control Room Slab: 05-MAR-2018 Atluri Mohan Krishna (B845)Document32 pagesDg-1 (Remote Radiator) Above Control Room Slab: 05-MAR-2018 Atluri Mohan Krishna (B845)Shaik AbdullaNo ratings yet
- Earth and Lice Science Quarter 2 BrochureDocument2 pagesEarth and Lice Science Quarter 2 BrochureCamille NavorNo ratings yet
- Activity 4 - TR-WPS OfficeDocument2 pagesActivity 4 - TR-WPS OfficeJed JaquecaNo ratings yet
- Annotated BibliographyDocument7 pagesAnnotated Bibliographyapi-340711045No ratings yet
- English Essay 2Document6 pagesEnglish Essay 2api-280146957No ratings yet
- To-Do List FormulaDocument1 pageTo-Do List FormulaPre MANo ratings yet
- 1 SMDocument12 pages1 SMasdNo ratings yet
- Self - Assessment Guide: Can I? YES NODocument3 pagesSelf - Assessment Guide: Can I? YES NOJohn Castillo100% (1)
- Triangle BreakoutDocument3 pagesTriangle BreakoutHarun MamatNo ratings yet
- Major Item Wise Export 2020Document1 pageMajor Item Wise Export 2020RoshniNo ratings yet
- Notice: Agency Information Collection Activities Proposals, Submissions, and ApprovalsDocument2 pagesNotice: Agency Information Collection Activities Proposals, Submissions, and ApprovalsJustia.comNo ratings yet
- Furniture For The 21st CenturyDocument178 pagesFurniture For The 21st Centurytajanan7240100% (4)