Professional Documents
Culture Documents
SMFM 2016 Implementation of The Use of Antenatal Corticosteroids in The Late Preterm Birth Period in Women at Risk For Preterm Delivery
SMFM 2016 Implementation of The Use of Antenatal Corticosteroids in The Late Preterm Birth Period in Women at Risk For Preterm Delivery
Uploaded by
Angela FernandezCopyright:
Available Formats
You might also like
- USMLE Step 3 Lecture Notes 2021-2022: Internal Medicine, Psychiatry, EthicsFrom EverandUSMLE Step 3 Lecture Notes 2021-2022: Internal Medicine, Psychiatry, EthicsRating: 5 out of 5 stars5/5 (9)
- Practice Bulletin: Management of Preterm LaborDocument10 pagesPractice Bulletin: Management of Preterm LaborXimena OrtegaNo ratings yet
- NVBSP BMR Forms (BM 01-10) - Revised2022Document23 pagesNVBSP BMR Forms (BM 01-10) - Revised2022lynore sandovalNo ratings yet
- Pituitary Tumors: A Clinical CasebookFrom EverandPituitary Tumors: A Clinical CasebookLisa B. NachtigallNo ratings yet
- Ajog AcsDocument3 pagesAjog AcsAndre PutraNo ratings yet
- Pi Is 0002937816004750Document3 pagesPi Is 0002937816004750Taufik RizalNo ratings yet
- 10 1016@j Ajog 2016 03 013Document7 pages10 1016@j Ajog 2016 03 013Fernando CruzNo ratings yet
- Provider Resources Obstetrics Late Preterm Steroids July2016Document10 pagesProvider Resources Obstetrics Late Preterm Steroids July2016Pediatrics SLCM-WHQMNo ratings yet
- Antenatal Betamethasone For WomenDocument10 pagesAntenatal Betamethasone For WomenMarcela Garzon O VelezNo ratings yet
- Antenatal Betamethasone For Women at RiskDocument10 pagesAntenatal Betamethasone For Women at RiskThapakorn JalearnyingNo ratings yet
- App y CorticoesteroidesDocument7 pagesApp y CorticoesteroidesMichelle ArenasNo ratings yet
- Parto Prematuro ACOGDocument10 pagesParto Prematuro ACOGAngela_Maria_M_7864No ratings yet
- Induction of Labor With Misoprostol For Premature Rupture of Membranes Beyond Thirty-Six Weeks' GestationDocument6 pagesInduction of Labor With Misoprostol For Premature Rupture of Membranes Beyond Thirty-Six Weeks' GestationFebrinata MahadikaNo ratings yet
- 10.1111@jog.13193 2 PDFDocument5 pages10.1111@jog.13193 2 PDFgandongmiziNo ratings yet
- Sibai PDFDocument2 pagesSibai PDFAdriana PajueloNo ratings yet
- Synopsis For Foley Plus Miso Vs Miso Alone in Induction of LabourDocument5 pagesSynopsis For Foley Plus Miso Vs Miso Alone in Induction of LabourAshish TomarNo ratings yet
- PPROM GuidelinesDocument2 pagesPPROM GuidelinesLaiza JubyNo ratings yet
- Misoprostol Vaginal Insert and Time To Vaginal.4Document9 pagesMisoprostol Vaginal Insert and Time To Vaginal.4Afiqah So JasmiNo ratings yet
- Evaluation of The Effect of Antenatal Betamethasone On Neonatal Respiratory Morbidities in Late Preterm Deliveries (34-37 Weeks)Document9 pagesEvaluation of The Effect of Antenatal Betamethasone On Neonatal Respiratory Morbidities in Late Preterm Deliveries (34-37 Weeks)Rizka RamadaniNo ratings yet
- The Effects of Betamethasone On Clinical Outcome of The Late Preterm Neonates Born Between 34 and 36 Weeks of GestationDocument17 pagesThe Effects of Betamethasone On Clinical Outcome of The Late Preterm Neonates Born Between 34 and 36 Weeks of GestationjeffyNo ratings yet
- Antenatal Corticosteroids Beyond 34 Weeks Gestation: What Do We Do Now?Document8 pagesAntenatal Corticosteroids Beyond 34 Weeks Gestation: What Do We Do Now?XIMENAGILDANo ratings yet
- Management of Premature Rupture of The Fetal Membranes at TermDocument6 pagesManagement of Premature Rupture of The Fetal Membranes at TermFrancisco Javier Gayoso DhagaNo ratings yet
- Use of Mifepristone For Termination of Intrauterine Fetal DemiseDocument4 pagesUse of Mifepristone For Termination of Intrauterine Fetal DemiseRizky AMNo ratings yet
- Figo Maduracion PumonarDocument5 pagesFigo Maduracion PumonarSoy PatoNo ratings yet
- Thesis PaperDocument5 pagesThesis PaperbhalNo ratings yet
- Pematangan ParuDocument8 pagesPematangan ParuMuthia NadhiraNo ratings yet
- Premature Rupture of Membrane at Term: Early Induction Versus Expectant ManagementDocument5 pagesPremature Rupture of Membrane at Term: Early Induction Versus Expectant ManagementIntan Permata Sari IpsNo ratings yet
- Ijgo 13836Document5 pagesIjgo 13836Christian YzaguirreNo ratings yet
- Ijgo 12998Document7 pagesIjgo 12998el_dani_ellNo ratings yet
- Conservative Management of Early-Onset Severe Preeclampsia: Comparison Between Randomized and Observational Studies A Systematic ReviewDocument13 pagesConservative Management of Early-Onset Severe Preeclampsia: Comparison Between Randomized and Observational Studies A Systematic ReviewCorey WoodsNo ratings yet
- 34784898_ The effects of betamethasone on clinical outcome of the late preterm neonates born between 34 and 36 weeks of gestatioDocument5 pages34784898_ The effects of betamethasone on clinical outcome of the late preterm neonates born between 34 and 36 weeks of gestatioaurimeryNo ratings yet
- Skor Tokolitik PDFDocument5 pagesSkor Tokolitik PDFrahayu muhsiNo ratings yet
- Review: Expert Committee Member MISOPROSTOL (Low Dose For Labour Induction at Term) Author: Lenita WannmacherDocument13 pagesReview: Expert Committee Member MISOPROSTOL (Low Dose For Labour Induction at Term) Author: Lenita WannmacherTri YuliasihNo ratings yet
- Corticoides PrenatalesDocument13 pagesCorticoides PrenatalesGraciela FissoreNo ratings yet
- 3.1 Pprom ShangrilaDocument31 pages3.1 Pprom Shangrilaintan.obgNo ratings yet
- Current Concepts in The Management of Premature Rupture of The MembranesDocument21 pagesCurrent Concepts in The Management of Premature Rupture of The MembranesWike UbayNo ratings yet
- Pesario - SMFMDocument3 pagesPesario - SMFMDaniela Franco HNo ratings yet
- Sectio Pada Preeclampsia BeratDocument4 pagesSectio Pada Preeclampsia BeratJosepb SimarmataNo ratings yet
- Omj D 09 00101Document6 pagesOmj D 09 00101DewinsNo ratings yet
- Tocolytics (Also Called Anti-Contraction Medications or Labor Represents) AreDocument2 pagesTocolytics (Also Called Anti-Contraction Medications or Labor Represents) AreEric RothNo ratings yet
- 9 Antenatal Corticosteroid Green Top PDFDocument13 pages9 Antenatal Corticosteroid Green Top PDFangela_karenina_1No ratings yet
- Comparative Study of Nifedipine and Isoxpurine As Tocolytics For Preterm LaborDocument4 pagesComparative Study of Nifedipine and Isoxpurine As Tocolytics For Preterm LaborMeitika Wahyu Wedha WatiNo ratings yet
- January 2003: East African Medical Journal 51Document5 pagesJanuary 2003: East African Medical Journal 51simoncktNo ratings yet
- Early Amniotomy After Vaginal Misoprostol For Induction of Labor: A Randomized Clinical TrialDocument5 pagesEarly Amniotomy After Vaginal Misoprostol For Induction of Labor: A Randomized Clinical Trialbidan22No ratings yet
- OB - 02 - Outcomes of Multifetal ReductionDocument6 pagesOB - 02 - Outcomes of Multifetal Reductionram4a5No ratings yet
- Aborto Manejo Medico Primer Trimestre ACOG'14Document18 pagesAborto Manejo Medico Primer Trimestre ACOG'14CIRUGIA GENERAL HRAEZNo ratings yet
- Tocolisis by NejmDocument11 pagesTocolisis by NejmalbertoNo ratings yet
- Jurnal KB Inggg 1Document4 pagesJurnal KB Inggg 1HidayahNo ratings yet
- Shrader2011 Updates in Hormonal Emergency ContraceptionDocument9 pagesShrader2011 Updates in Hormonal Emergency ContraceptionAdityaWijayaNo ratings yet
- Induction of LabourDocument51 pagesInduction of LabourvaleriaNo ratings yet
- Antenatal CorticosteroidsDocument17 pagesAntenatal CorticosteroidsRolando DiazNo ratings yet
- WNHS Og Corticosteroids UseofDocument9 pagesWNHS Og Corticosteroids UseofADRIANA FERNANDA MENESES AYALANo ratings yet
- Premature Rupture of Membrane at Term: Early Induction Versus Expectant ManagementDocument5 pagesPremature Rupture of Membrane at Term: Early Induction Versus Expectant ManagementSyaifullahNo ratings yet
- Aggressive Intervention of Previable Preterm Premature Rupture of MembranesDocument8 pagesAggressive Intervention of Previable Preterm Premature Rupture of MembranesVanessa Riaño GodoyNo ratings yet
- Conservative Management of Early-Onset Severe Preeclampsia: Comparison Between Randomized and Observational Studies A Systematic ReviewDocument9 pagesConservative Management of Early-Onset Severe Preeclampsia: Comparison Between Randomized and Observational Studies A Systematic ReviewCorey WoodsNo ratings yet
- ACOG 2009 Induction of LaborDocument12 pagesACOG 2009 Induction of LaborRiantiara PutrizaNo ratings yet
- Facchinetti 2005Document5 pagesFacchinetti 2005Sri HariNo ratings yet
- Preterm Prelabor Rupture of Membranes - Management and Outcome - UpToDateDocument29 pagesPreterm Prelabor Rupture of Membranes - Management and Outcome - UpToDateDương Danh CườngNo ratings yet
- Isoxuprine VS Terbutaline in Pre-Term Labor TocolysisDocument29 pagesIsoxuprine VS Terbutaline in Pre-Term Labor TocolysisGarry Kin CamarilloNo ratings yet
- Diminished Ovarian Reserve and Assisted Reproductive Technologies: Current Research and Clinical ManagementFrom EverandDiminished Ovarian Reserve and Assisted Reproductive Technologies: Current Research and Clinical ManagementOrhan BukulmezNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 10: ObstetricsFrom EverandComplementary and Alternative Medical Lab Testing Part 10: ObstetricsNo ratings yet
- SMFM Hepatitis B in Pregnancy Updated GuidelinesDocument10 pagesSMFM Hepatitis B in Pregnancy Updated GuidelinesAngela FernandezNo ratings yet
- The Assessment of Intrapartum Transperineal Ultrasonographic Parameters For Their Effectiveness in Evaluation of Progress of Labor and Prediction of Mode of Delivery in Egyptian WomenDocument7 pagesThe Assessment of Intrapartum Transperineal Ultrasonographic Parameters For Their Effectiveness in Evaluation of Progress of Labor and Prediction of Mode of Delivery in Egyptian WomenAngela FernandezNo ratings yet
- SLE Management in PregnancyDocument13 pagesSLE Management in PregnancyAngela FernandezNo ratings yet
- SMFM Maternal SepsisDocument18 pagesSMFM Maternal SepsisAngela FernandezNo ratings yet
- Pharmaceutical ManagementDocument23 pagesPharmaceutical ManagementAngela FernandezNo ratings yet
- BONENT CPDN Exam Content PDFDocument6 pagesBONENT CPDN Exam Content PDFVashistmohan A.P.No ratings yet
- I. Nursing Assessment: Date/Time of Admission: July 2, 2010, 8:12 AmDocument17 pagesI. Nursing Assessment: Date/Time of Admission: July 2, 2010, 8:12 AmYami PinedaNo ratings yet
- 1 s2.0 S1930043321003083 MainDocument5 pages1 s2.0 S1930043321003083 MainSandra ArellanoNo ratings yet
- PH 36 Anterior Cruciate Ligament Reconstruction Advice Booklet v1 WebDocument12 pagesPH 36 Anterior Cruciate Ligament Reconstruction Advice Booklet v1 WebPushpa NNo ratings yet
- Nursing Management of Patient With BurnsDocument30 pagesNursing Management of Patient With BurnsjsoalNo ratings yet
- Residency Survival Guide: Canadian Association of General Surgeons Residents CommitteeDocument53 pagesResidency Survival Guide: Canadian Association of General Surgeons Residents CommitteeIrina MincuNo ratings yet
- ADocument2 pagesASrinivasareddy OgiralaNo ratings yet
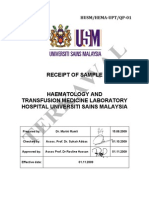
- Receipt of Sample: HUSM/HEMA - UPT/QP - 01Document10 pagesReceipt of Sample: HUSM/HEMA - UPT/QP - 01zakwanmustafaNo ratings yet
- Hemostaza Kao Fiziološki Mehanizam Pozitivne Povratne SpregeDocument10 pagesHemostaza Kao Fiziološki Mehanizam Pozitivne Povratne SpregeCrvena LoknicaNo ratings yet
- Postural Deviations: Kinesiology RHS 341 Dr. Einas Al-EisaDocument40 pagesPostural Deviations: Kinesiology RHS 341 Dr. Einas Al-EisaStephanie GuevaraNo ratings yet
- ENT Practice MCQs With Key 4th Year MBBSDocument7 pagesENT Practice MCQs With Key 4th Year MBBSPatrick BatemanNo ratings yet
- Survival GuideDocument4 pagesSurvival Guideeclipse1130No ratings yet
- A Case of Suspected Illegal Abortion: How Clinicians May Assist The Forensic PathologistDocument43 pagesA Case of Suspected Illegal Abortion: How Clinicians May Assist The Forensic Pathologistjeremy ludwigNo ratings yet
- Dr. Jaime T. Cruz v. Dr. Agas, Jr. - G.R. No. 204095 - June 15, 2015 - DigestDocument3 pagesDr. Jaime T. Cruz v. Dr. Agas, Jr. - G.R. No. 204095 - June 15, 2015 - DigestAaron Ariston100% (2)
- Effectiveness of Demonstration Method On Knowledge Regarding Paediatric Advanced Life Support Among GNM Final Year Students Studying in Selected School of Nursing BagalkotDocument3 pagesEffectiveness of Demonstration Method On Knowledge Regarding Paediatric Advanced Life Support Among GNM Final Year Students Studying in Selected School of Nursing BagalkotInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Nurse Duties and Medical Equipment in OperatingDocument10 pagesNurse Duties and Medical Equipment in OperatingFita DinarNo ratings yet
- Case Study 416Document34 pagesCase Study 416jennifer_crumm100% (1)
- Basic SuturingDocument17 pagesBasic SuturingWahyu HidayatNo ratings yet
- Allium Species Poisoning in Dogs and CatsDocument9 pagesAllium Species Poisoning in Dogs and CatsKmii TspNo ratings yet
- Acantosis Nigricans PDFDocument4 pagesAcantosis Nigricans PDFCarlosYovadSaldamandoCruzNo ratings yet
- Front PageDocument11 pagesFront PageJake PaduaNo ratings yet
- Atlas of Intraoperative Transesophageal EchocardiographyDocument416 pagesAtlas of Intraoperative Transesophageal EchocardiographyDelia Acsinte100% (1)
- Andrew Solomon Case Study - EditedDocument5 pagesAndrew Solomon Case Study - EditedJefferson KagiriNo ratings yet
- EBN Diarrhea OrasolDocument8 pagesEBN Diarrhea Orasolcharm_peñaNo ratings yet
- Disorders of Potassium Metabolism PresentationDocument20 pagesDisorders of Potassium Metabolism PresentationSolomon Fallah Foa SandyNo ratings yet
- Wound Essentials 8 1 Debridement Consensus Recommendations For PracticeDocument5 pagesWound Essentials 8 1 Debridement Consensus Recommendations For PracticeAndaz MortinNo ratings yet
- NEW-EVLT Phlebology LaserDocument5 pagesNEW-EVLT Phlebology LaserJesús JoveNo ratings yet
- Resume - 2 ProjectDocument2 pagesResume - 2 Projectapi-357163581No ratings yet
- G12 - HS - Food Borne - RevisionDocument6 pagesG12 - HS - Food Borne - RevisionEbtisam AlmenhaliNo ratings yet
SMFM 2016 Implementation of The Use of Antenatal Corticosteroids in The Late Preterm Birth Period in Women at Risk For Preterm Delivery
SMFM 2016 Implementation of The Use of Antenatal Corticosteroids in The Late Preterm Birth Period in Women at Risk For Preterm Delivery
Uploaded by
Angela FernandezOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
SMFM 2016 Implementation of The Use of Antenatal Corticosteroids in The Late Preterm Birth Period in Women at Risk For Preterm Delivery
SMFM 2016 Implementation of The Use of Antenatal Corticosteroids in The Late Preterm Birth Period in Women at Risk For Preterm Delivery
Uploaded by
Angela FernandezCopyright:
Available Formats
SMFM Statement
smfm.org
Implementation of the use of antenatal
corticosteroids in the late preterm birth period
in women at risk for preterm delivery
Society for Maternal-Fetal Medicine (SMFM) Publications Committee
The practice of medicine continues to evolve, and individual circumstances will vary. This publication reflects information
available at the time of its submission for publication and is neither designed nor intended to establish an exclusive standard
of perinatal care. This publication is not expected to reflect the opinions of all members of the Society for Maternal-Fetal
Medicine.
L ate preterm birth is defined as delivery between
34 weeks 0 days through 36 weeks 6 days of gestation
and accounts for 70% of all preterm births.1 Late preterm
were likely to deliver within 12 hours (eg, if they were
deemed unstable, presented with active bleeding or non-
reassuring status requiring delivery), had previously
neonates are at risk for signficant morbidities, including received a course of betamethasone, or had pregestational
respiratory distress syndrome because pulmonary matura- diabetes, chorioamnionitis, or any other contraindication to
tion continues through the late preterm period into early betamethasone.
childhood.2 The primary outcome of the study was a composite
Although the use of antenatal corticosteroids prior to endpoint describing the need for respiratory support within
34 weeks of gestation is standard practice for women at 72 hours after birth and 1 or more of the following: the use of
high risk for delivery in the next 7 days,3 such treatment has continuous positive airway pressure or high-flow nasal
not been recommended for women during late preterm cannula for at least 2 consecutive hours, supplemental
period birth because of the lack of supportive data from oxygen with a fraction of inspired oxygen of at least 0.30
randomized controlled trials. for at least 4 continuous hours, extracorporeal membrane
The purpose of this document is to review the findings of a oxygenation, or mechanical ventilation.
recently conducted randomized controlled trial evalating the The study involved treatment with either 2 doses of
use of antental corticosteroids in late preterm pregnancies betamethasone (12 mg intramuscularly) 24 hours apart or a
and to provide guidance for implementation into clinical matching placebo. Tocolysis was not used as a part of the
practice. protocol, and clinical management decisions after study
The Antenatal Late Preterm Steroids trial was conducted drug administration were at the discretion of the provider.
by the Eunice Kennedy Shriver National Institute of Child The most common indication for enrollment was preterm
Health and Human Development, Maternal-Fetal Medicine labor (28%), followed by delivery for gestational hyperten-
Units Network.4 This double-blind, placebo-controlled sion or preeclampsia (26%) and ruptured membranes
randomized controlled trial was conducted at 17 Maternal- (22%). There were no differences between groups in the
Fetal Medicine Units centers across the United States time from randomization to delivery; approximately 60% of
from 2010 to 2015. Women with a singleton gestation at the women in the betamethasone group received 2 doses of
high risk for preterm delivery between 34 weeks 0 days study medication.
through 36 weeks 5 days of gestation were eligible if they The study found a significant decrease in the primary
presented in preterm labor with a cervix that was at least outcome, which was the need for respiratory support
3 cm dilated or 75% effaced, if they had preterm premature within the first 72 hours (14.4% in the placebo group vs
rupture of the membranes, or if a planned delivery was 11.6% in the betamethasone group; relative risk, 0.80,
scheduled in the late preterm period, with the indication at 95% confidence interval, 0.66e0.97, P ¼ .02). There were
the discretion of the provider. also significant decreases in the rates of severe respiratory
Women with obstetric or medical complications and morbidity (a composite outcome of continuous positive
anticipation for worsening status leading to a high likelihood airway pressure or high-flow nasal cannula for at least 12
for late preterm delivery between 24 hours and 7 days were continuous hours, supplemental oxygen with a fraction of
eligible (eg, oligohydramnios, fetal growth restriction, or inspired oxygen of at least 0.30 for at least at least 24
preeclampsia). Women were considered ineligible if they continuous hours, extracorporeal membrane oxygenation
AUGUST 2016 B13
SMFM Statement smfm.org
or mechanical ventilation, stillbirth, or neonatal death gestation. Thus, in the absence of new data, the use of
within 72 hours after delivery), bronchopulmonary betamethasone administration in the late preterm period
dysplasia, transient tachypnea of the newborn, the need should not include an attempt to delay delivery such
for resuscitation at birth, and the need for postnatal as with tocolysis or expectant management for pre-
surfactant. eclampsia with severe features or premature rupture of
There were no differences in maternal outcomes such as membranes.
mode of delivery, clinical chorioamnionitis, or endometritis. Another important aspect of the Antenatal Late Preterm
With respect to the newborn, hypoglycemia (glucose <40 Steroids study was that preterm labor was strictly defined
mg/dL) was increased with betamethasone (24.0% vs in that the cervix was required to be at least 3 cm dilated
14.9%; relative risk, 1.61, 95% confidence interval, or 75% effaced. Utilization of similar criteria for preterm
1.38e1.88); other adverse neonatal outcomes were not labor is recommended to decrease the potential risk of
different between groups. The rates of hypoglycemia overtreatment of women who ultimately would deliver at
reported in the betamethasone group were similar to those term.
expected in late preterm neonates.5 Outcomes for women in the late preterm period who were
Antenatal Late Preterm Steroids is the largest randomized not included in the Antenatal Late Preterm Steroids study
controlled trial to date (N ¼ 2831 subjects) evaluating the remain unknown (eg, women with multiple gestations, those
benefits and harms of antenatal betamethasone in the late who had previously been treated with betamethasone prior
preterm period. Two small randomized controlled trials to 34 weeks of gestation, those with pregestational dia-
involving antenatal corticosteroids in late preterm preg- betes, or those with scheduled cesarean deliveries at or
nancies have been published,6,7 but the largest comparable beyond 37 weeks of gestation).
study was the Antenatal Steroids for Term Elective Additional data are needed prior to the use of betame-
Caesarean Section trial,8 which included 998 women who thasone in the late preterm period for these indications. For
were to undergo scheduled cesarean delivery at term. these reasons, institutions should utilize standard guide-
Infants of women who received betamethasone had lower lines for the implementation of the Antenatal Late Preterm
rates of NICU admission because of respiratory complica- Steroids study into routine clinical practice.
tions (relative risk, 0.46; 95% confidence interval, 0.2e0.93)
as compared with controls. SMFM recommendations
The findings of the Antenatal Late Preterm Steroids study 1. In women with a singleton pregnancy between 34 weeks
are consistent with multiple other randomized controlled 0 days and 36 weeks 6 days of gestation who are at high
trials of antenatal corticosteroids administered at <34 risk for preterm birth within the next 7 days (but before
weeks of gestation.3 The rationale to implement the Ante- 37 weeks of gestation), we recommend treatment with
natal Late Preterm Steroids protocol into clinical practice betamethasone (2 doses of 12 mg intramuscularly
includes its relatively large sample size, the fact that it 24 hours apart).
included a study cohort generalizable to the US population, 2. In women with preterm labor symptoms in the late
and that it involved a methodologically rigorous study preterm period, we recommend waiting for evidence of
design and protocol that enhances its internal validity. preterm labor, such as a cervical dilatation of at least
Outcomes data from Antenatal Late Preterm Steroids are 3 cm or effacement of at least 75%, before treatment
restricted at this time to the newborn period, and the lack of with betamethasone.
long-term information is a current limitation of this ran- 3. In women with late preterm pregnancies receiving
domized controlled trial. betamethasone, we recommend against the use of
Follow-up data on preterm newborns who received a tocolysis in an attempt to delay delivery to complete the
single course of antenatal corticosteroids do not suggest steroid course because it is unclear whether the benefits
any increased risk for long-term adverse effects.9,10 of betamethasone administration are outweighed by the
Concern has been raised about the potential increased risks of attempts to delay delivery.
risks associated with neonatal hypoglycemia, but these 4. In women with late preterm pregnancies with a potential
should be minimized by the utilization of routine testing for medical indication for delivery, we recommend beta-
all late preterm newborns, as advocated by the Committee methasone not be given unless there is a definitive plan
on Fetus and Newborn of the American Academy of for late preterm delivery.
Pediatrics.11 5. We recommend that institutions utilize standard guide-
There is always the potential for unintended conse- lines for the assessment and management of neonatal
quences with any change in clinical practice. The Ante- hypoglycemia in late preterm newborns.
natal Late Preterm Steroids protocol did not attempt to 6. We recommend against implementation of the Antenatal
change clinical management of late preterm pregnancies Late Preterm Steroids protocol for conditions not
other than to administer betamethasone. Greater than studied in the randomized controlled trial unless per-
80% of women in the trial delivered prior to 37 weeks of formed as part of research or quality improvement. n
B14 AUGUST 2016
smfm.org SMFM Statement
REFERENCES 11. Committee on Fetus and Newborn, Adamkin DH. Postnatal glucose
1. Martin JA, Hamilton BE, Osterman MJ, Curtin SC, Matthews TJ. Births: homeostasis in late-preterm and term infants. Pediatrics 2011;127:
final data for 2013. Natl Vital Stat Rep 2015;64:1-65. 575-9.
2. Consortium on Safe Labor, Hibbard JU, Wilkins I, et al. Respiratory
morbidity in late preterm births. JAMA 2010;304:419-25.
3. Roberts D, Dalziel S. Antenatal corticosteroids for accelerating fetal lung
maturation for women at risk of preterm birth. Review. Cochrane Database
All authors and Committee members have filed a conflict of
Syst Rev 2006:CD004454.
interest disclosure delineating personal, professional, and/or
4. Gyamfi-Bannerman C, Thom EA, Blackwell SC, et al. Antenatal
business interests that might be perceived as a real or potential
betamethasone for women at risk for late preterm delivery. N Engl J Med
conflict of interest in relation to this publication. Any conflicts
2016.
have been resolved through a process approved by the Exec-
5. Harris DL, Weston PJ, Harding JE. Incidence of neonatal hypoglycemia
utive Board. The Society for Maternal-Fetal Medicine has neither
in babies identified as at risk. J Pediatr 2012;161:787-91.
solicited nor accepted any commercial involvement in the
6. Porto AM, Coutinho IC, Correia JB, Amorim MM. Effectiveness of
development of the content of this publication.
antenatal corticosteroids in reducing respiratory disorders in late preterm
infants: randomised clinical trial. BMJ 2011;342:d1696. This document has undergone an internal peer review through a
7. Balci O, Ozdemir S, Mahmoud AS, Acar A, Colakoglu MC. The effect of multi-level committee process within the Society for Maternal
antenatal steroids on fetal lung maturation between the 34th and 36th Fetal Medicine (SMFM). This review involves critique and feed-
week of pregnancy. Gynecol Obstet Invest 2010;70:95-9. back from the SMFM Publications and Risk Management
8. Stutchfield P, Whitaker R, Russell I; Antenatal Steroids for Term Elective Committees and final approval by the SMFM Executive Com-
Caesarean Section Research Team. Antenatal betamethasone and inci- mittee. SMFM accepts sole responsibility for document content.
dence of neonatal respiratory distress after elective caesarean section: SMFM publications do not undergo editorial and peer review by
pragmatic randomised trial. BMJ 2005;331:662. the American Journal of Obstetrics & Gynecology. The SMFM
9. Sotiriadis A, Tsiami A, Papatheodorou S, Baschat AA, Sarafidis K, Publications Committee reviews publications every 18-24
Makrydimas G. Neurodevelopmental outcome after a single course of months and issues updates as needed. Further details
antenatal steroids in children born preterm: a systematic review and regarding SMFM Publications can be found at www.smfm.org/
meta-analysis. Obstet Gynecol 2015;125:1385-96. publications. All questions or comments regarding the docu-
10. Dalziel SR, Lim VK, Lambert A, et al. Antenatal exposure to betame- ment should be referred to the SMFM Publications committee at
thasone: psychological functioning and health related quality of life 31 pubs@smfm.org.
years after inclusion in randomised controlled trial. BMJ 2005;331:665.
ª 2016 Elsevier Inc. All rights reserved. http://dx.doi.org/10.1016/j.ajog.2016.03.013 AUGUST 2016 B15
You might also like
- USMLE Step 3 Lecture Notes 2021-2022: Internal Medicine, Psychiatry, EthicsFrom EverandUSMLE Step 3 Lecture Notes 2021-2022: Internal Medicine, Psychiatry, EthicsRating: 5 out of 5 stars5/5 (9)
- Practice Bulletin: Management of Preterm LaborDocument10 pagesPractice Bulletin: Management of Preterm LaborXimena OrtegaNo ratings yet
- NVBSP BMR Forms (BM 01-10) - Revised2022Document23 pagesNVBSP BMR Forms (BM 01-10) - Revised2022lynore sandovalNo ratings yet
- Pituitary Tumors: A Clinical CasebookFrom EverandPituitary Tumors: A Clinical CasebookLisa B. NachtigallNo ratings yet
- Ajog AcsDocument3 pagesAjog AcsAndre PutraNo ratings yet
- Pi Is 0002937816004750Document3 pagesPi Is 0002937816004750Taufik RizalNo ratings yet
- 10 1016@j Ajog 2016 03 013Document7 pages10 1016@j Ajog 2016 03 013Fernando CruzNo ratings yet
- Provider Resources Obstetrics Late Preterm Steroids July2016Document10 pagesProvider Resources Obstetrics Late Preterm Steroids July2016Pediatrics SLCM-WHQMNo ratings yet
- Antenatal Betamethasone For WomenDocument10 pagesAntenatal Betamethasone For WomenMarcela Garzon O VelezNo ratings yet
- Antenatal Betamethasone For Women at RiskDocument10 pagesAntenatal Betamethasone For Women at RiskThapakorn JalearnyingNo ratings yet
- App y CorticoesteroidesDocument7 pagesApp y CorticoesteroidesMichelle ArenasNo ratings yet
- Parto Prematuro ACOGDocument10 pagesParto Prematuro ACOGAngela_Maria_M_7864No ratings yet
- Induction of Labor With Misoprostol For Premature Rupture of Membranes Beyond Thirty-Six Weeks' GestationDocument6 pagesInduction of Labor With Misoprostol For Premature Rupture of Membranes Beyond Thirty-Six Weeks' GestationFebrinata MahadikaNo ratings yet
- 10.1111@jog.13193 2 PDFDocument5 pages10.1111@jog.13193 2 PDFgandongmiziNo ratings yet
- Sibai PDFDocument2 pagesSibai PDFAdriana PajueloNo ratings yet
- Synopsis For Foley Plus Miso Vs Miso Alone in Induction of LabourDocument5 pagesSynopsis For Foley Plus Miso Vs Miso Alone in Induction of LabourAshish TomarNo ratings yet
- PPROM GuidelinesDocument2 pagesPPROM GuidelinesLaiza JubyNo ratings yet
- Misoprostol Vaginal Insert and Time To Vaginal.4Document9 pagesMisoprostol Vaginal Insert and Time To Vaginal.4Afiqah So JasmiNo ratings yet
- Evaluation of The Effect of Antenatal Betamethasone On Neonatal Respiratory Morbidities in Late Preterm Deliveries (34-37 Weeks)Document9 pagesEvaluation of The Effect of Antenatal Betamethasone On Neonatal Respiratory Morbidities in Late Preterm Deliveries (34-37 Weeks)Rizka RamadaniNo ratings yet
- The Effects of Betamethasone On Clinical Outcome of The Late Preterm Neonates Born Between 34 and 36 Weeks of GestationDocument17 pagesThe Effects of Betamethasone On Clinical Outcome of The Late Preterm Neonates Born Between 34 and 36 Weeks of GestationjeffyNo ratings yet
- Antenatal Corticosteroids Beyond 34 Weeks Gestation: What Do We Do Now?Document8 pagesAntenatal Corticosteroids Beyond 34 Weeks Gestation: What Do We Do Now?XIMENAGILDANo ratings yet
- Management of Premature Rupture of The Fetal Membranes at TermDocument6 pagesManagement of Premature Rupture of The Fetal Membranes at TermFrancisco Javier Gayoso DhagaNo ratings yet
- Use of Mifepristone For Termination of Intrauterine Fetal DemiseDocument4 pagesUse of Mifepristone For Termination of Intrauterine Fetal DemiseRizky AMNo ratings yet
- Figo Maduracion PumonarDocument5 pagesFigo Maduracion PumonarSoy PatoNo ratings yet
- Thesis PaperDocument5 pagesThesis PaperbhalNo ratings yet
- Pematangan ParuDocument8 pagesPematangan ParuMuthia NadhiraNo ratings yet
- Premature Rupture of Membrane at Term: Early Induction Versus Expectant ManagementDocument5 pagesPremature Rupture of Membrane at Term: Early Induction Versus Expectant ManagementIntan Permata Sari IpsNo ratings yet
- Ijgo 13836Document5 pagesIjgo 13836Christian YzaguirreNo ratings yet
- Ijgo 12998Document7 pagesIjgo 12998el_dani_ellNo ratings yet
- Conservative Management of Early-Onset Severe Preeclampsia: Comparison Between Randomized and Observational Studies A Systematic ReviewDocument13 pagesConservative Management of Early-Onset Severe Preeclampsia: Comparison Between Randomized and Observational Studies A Systematic ReviewCorey WoodsNo ratings yet
- 34784898_ The effects of betamethasone on clinical outcome of the late preterm neonates born between 34 and 36 weeks of gestatioDocument5 pages34784898_ The effects of betamethasone on clinical outcome of the late preterm neonates born between 34 and 36 weeks of gestatioaurimeryNo ratings yet
- Skor Tokolitik PDFDocument5 pagesSkor Tokolitik PDFrahayu muhsiNo ratings yet
- Review: Expert Committee Member MISOPROSTOL (Low Dose For Labour Induction at Term) Author: Lenita WannmacherDocument13 pagesReview: Expert Committee Member MISOPROSTOL (Low Dose For Labour Induction at Term) Author: Lenita WannmacherTri YuliasihNo ratings yet
- Corticoides PrenatalesDocument13 pagesCorticoides PrenatalesGraciela FissoreNo ratings yet
- 3.1 Pprom ShangrilaDocument31 pages3.1 Pprom Shangrilaintan.obgNo ratings yet
- Current Concepts in The Management of Premature Rupture of The MembranesDocument21 pagesCurrent Concepts in The Management of Premature Rupture of The MembranesWike UbayNo ratings yet
- Pesario - SMFMDocument3 pagesPesario - SMFMDaniela Franco HNo ratings yet
- Sectio Pada Preeclampsia BeratDocument4 pagesSectio Pada Preeclampsia BeratJosepb SimarmataNo ratings yet
- Omj D 09 00101Document6 pagesOmj D 09 00101DewinsNo ratings yet
- Tocolytics (Also Called Anti-Contraction Medications or Labor Represents) AreDocument2 pagesTocolytics (Also Called Anti-Contraction Medications or Labor Represents) AreEric RothNo ratings yet
- 9 Antenatal Corticosteroid Green Top PDFDocument13 pages9 Antenatal Corticosteroid Green Top PDFangela_karenina_1No ratings yet
- Comparative Study of Nifedipine and Isoxpurine As Tocolytics For Preterm LaborDocument4 pagesComparative Study of Nifedipine and Isoxpurine As Tocolytics For Preterm LaborMeitika Wahyu Wedha WatiNo ratings yet
- January 2003: East African Medical Journal 51Document5 pagesJanuary 2003: East African Medical Journal 51simoncktNo ratings yet
- Early Amniotomy After Vaginal Misoprostol For Induction of Labor: A Randomized Clinical TrialDocument5 pagesEarly Amniotomy After Vaginal Misoprostol For Induction of Labor: A Randomized Clinical Trialbidan22No ratings yet
- OB - 02 - Outcomes of Multifetal ReductionDocument6 pagesOB - 02 - Outcomes of Multifetal Reductionram4a5No ratings yet
- Aborto Manejo Medico Primer Trimestre ACOG'14Document18 pagesAborto Manejo Medico Primer Trimestre ACOG'14CIRUGIA GENERAL HRAEZNo ratings yet
- Tocolisis by NejmDocument11 pagesTocolisis by NejmalbertoNo ratings yet
- Jurnal KB Inggg 1Document4 pagesJurnal KB Inggg 1HidayahNo ratings yet
- Shrader2011 Updates in Hormonal Emergency ContraceptionDocument9 pagesShrader2011 Updates in Hormonal Emergency ContraceptionAdityaWijayaNo ratings yet
- Induction of LabourDocument51 pagesInduction of LabourvaleriaNo ratings yet
- Antenatal CorticosteroidsDocument17 pagesAntenatal CorticosteroidsRolando DiazNo ratings yet
- WNHS Og Corticosteroids UseofDocument9 pagesWNHS Og Corticosteroids UseofADRIANA FERNANDA MENESES AYALANo ratings yet
- Premature Rupture of Membrane at Term: Early Induction Versus Expectant ManagementDocument5 pagesPremature Rupture of Membrane at Term: Early Induction Versus Expectant ManagementSyaifullahNo ratings yet
- Aggressive Intervention of Previable Preterm Premature Rupture of MembranesDocument8 pagesAggressive Intervention of Previable Preterm Premature Rupture of MembranesVanessa Riaño GodoyNo ratings yet
- Conservative Management of Early-Onset Severe Preeclampsia: Comparison Between Randomized and Observational Studies A Systematic ReviewDocument9 pagesConservative Management of Early-Onset Severe Preeclampsia: Comparison Between Randomized and Observational Studies A Systematic ReviewCorey WoodsNo ratings yet
- ACOG 2009 Induction of LaborDocument12 pagesACOG 2009 Induction of LaborRiantiara PutrizaNo ratings yet
- Facchinetti 2005Document5 pagesFacchinetti 2005Sri HariNo ratings yet
- Preterm Prelabor Rupture of Membranes - Management and Outcome - UpToDateDocument29 pagesPreterm Prelabor Rupture of Membranes - Management and Outcome - UpToDateDương Danh CườngNo ratings yet
- Isoxuprine VS Terbutaline in Pre-Term Labor TocolysisDocument29 pagesIsoxuprine VS Terbutaline in Pre-Term Labor TocolysisGarry Kin CamarilloNo ratings yet
- Diminished Ovarian Reserve and Assisted Reproductive Technologies: Current Research and Clinical ManagementFrom EverandDiminished Ovarian Reserve and Assisted Reproductive Technologies: Current Research and Clinical ManagementOrhan BukulmezNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 10: ObstetricsFrom EverandComplementary and Alternative Medical Lab Testing Part 10: ObstetricsNo ratings yet
- SMFM Hepatitis B in Pregnancy Updated GuidelinesDocument10 pagesSMFM Hepatitis B in Pregnancy Updated GuidelinesAngela FernandezNo ratings yet
- The Assessment of Intrapartum Transperineal Ultrasonographic Parameters For Their Effectiveness in Evaluation of Progress of Labor and Prediction of Mode of Delivery in Egyptian WomenDocument7 pagesThe Assessment of Intrapartum Transperineal Ultrasonographic Parameters For Their Effectiveness in Evaluation of Progress of Labor and Prediction of Mode of Delivery in Egyptian WomenAngela FernandezNo ratings yet
- SLE Management in PregnancyDocument13 pagesSLE Management in PregnancyAngela FernandezNo ratings yet
- SMFM Maternal SepsisDocument18 pagesSMFM Maternal SepsisAngela FernandezNo ratings yet
- Pharmaceutical ManagementDocument23 pagesPharmaceutical ManagementAngela FernandezNo ratings yet
- BONENT CPDN Exam Content PDFDocument6 pagesBONENT CPDN Exam Content PDFVashistmohan A.P.No ratings yet
- I. Nursing Assessment: Date/Time of Admission: July 2, 2010, 8:12 AmDocument17 pagesI. Nursing Assessment: Date/Time of Admission: July 2, 2010, 8:12 AmYami PinedaNo ratings yet
- 1 s2.0 S1930043321003083 MainDocument5 pages1 s2.0 S1930043321003083 MainSandra ArellanoNo ratings yet
- PH 36 Anterior Cruciate Ligament Reconstruction Advice Booklet v1 WebDocument12 pagesPH 36 Anterior Cruciate Ligament Reconstruction Advice Booklet v1 WebPushpa NNo ratings yet
- Nursing Management of Patient With BurnsDocument30 pagesNursing Management of Patient With BurnsjsoalNo ratings yet
- Residency Survival Guide: Canadian Association of General Surgeons Residents CommitteeDocument53 pagesResidency Survival Guide: Canadian Association of General Surgeons Residents CommitteeIrina MincuNo ratings yet
- ADocument2 pagesASrinivasareddy OgiralaNo ratings yet
- Receipt of Sample: HUSM/HEMA - UPT/QP - 01Document10 pagesReceipt of Sample: HUSM/HEMA - UPT/QP - 01zakwanmustafaNo ratings yet
- Hemostaza Kao Fiziološki Mehanizam Pozitivne Povratne SpregeDocument10 pagesHemostaza Kao Fiziološki Mehanizam Pozitivne Povratne SpregeCrvena LoknicaNo ratings yet
- Postural Deviations: Kinesiology RHS 341 Dr. Einas Al-EisaDocument40 pagesPostural Deviations: Kinesiology RHS 341 Dr. Einas Al-EisaStephanie GuevaraNo ratings yet
- ENT Practice MCQs With Key 4th Year MBBSDocument7 pagesENT Practice MCQs With Key 4th Year MBBSPatrick BatemanNo ratings yet
- Survival GuideDocument4 pagesSurvival Guideeclipse1130No ratings yet
- A Case of Suspected Illegal Abortion: How Clinicians May Assist The Forensic PathologistDocument43 pagesA Case of Suspected Illegal Abortion: How Clinicians May Assist The Forensic Pathologistjeremy ludwigNo ratings yet
- Dr. Jaime T. Cruz v. Dr. Agas, Jr. - G.R. No. 204095 - June 15, 2015 - DigestDocument3 pagesDr. Jaime T. Cruz v. Dr. Agas, Jr. - G.R. No. 204095 - June 15, 2015 - DigestAaron Ariston100% (2)
- Effectiveness of Demonstration Method On Knowledge Regarding Paediatric Advanced Life Support Among GNM Final Year Students Studying in Selected School of Nursing BagalkotDocument3 pagesEffectiveness of Demonstration Method On Knowledge Regarding Paediatric Advanced Life Support Among GNM Final Year Students Studying in Selected School of Nursing BagalkotInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Nurse Duties and Medical Equipment in OperatingDocument10 pagesNurse Duties and Medical Equipment in OperatingFita DinarNo ratings yet
- Case Study 416Document34 pagesCase Study 416jennifer_crumm100% (1)
- Basic SuturingDocument17 pagesBasic SuturingWahyu HidayatNo ratings yet
- Allium Species Poisoning in Dogs and CatsDocument9 pagesAllium Species Poisoning in Dogs and CatsKmii TspNo ratings yet
- Acantosis Nigricans PDFDocument4 pagesAcantosis Nigricans PDFCarlosYovadSaldamandoCruzNo ratings yet
- Front PageDocument11 pagesFront PageJake PaduaNo ratings yet
- Atlas of Intraoperative Transesophageal EchocardiographyDocument416 pagesAtlas of Intraoperative Transesophageal EchocardiographyDelia Acsinte100% (1)
- Andrew Solomon Case Study - EditedDocument5 pagesAndrew Solomon Case Study - EditedJefferson KagiriNo ratings yet
- EBN Diarrhea OrasolDocument8 pagesEBN Diarrhea Orasolcharm_peñaNo ratings yet
- Disorders of Potassium Metabolism PresentationDocument20 pagesDisorders of Potassium Metabolism PresentationSolomon Fallah Foa SandyNo ratings yet
- Wound Essentials 8 1 Debridement Consensus Recommendations For PracticeDocument5 pagesWound Essentials 8 1 Debridement Consensus Recommendations For PracticeAndaz MortinNo ratings yet
- NEW-EVLT Phlebology LaserDocument5 pagesNEW-EVLT Phlebology LaserJesús JoveNo ratings yet
- Resume - 2 ProjectDocument2 pagesResume - 2 Projectapi-357163581No ratings yet
- G12 - HS - Food Borne - RevisionDocument6 pagesG12 - HS - Food Borne - RevisionEbtisam AlmenhaliNo ratings yet