Professional Documents
Culture Documents
Short Note
Short Note
Uploaded by
mulugetaOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Short Note
Short Note
Uploaded by
mulugetaCopyright:
Available Formats
Competence Based Practical
short note for Nursing
[COMPETENCE BASED PRACTICAL SHORT NOTE FOR NURSING ] April 29, 2020
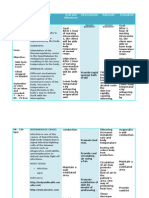
Perioperative period Vital sign: - a cardinal sign which
Indicate any alteration of the Human
Definition: - the Entire span of the total physiology.
Episodes of Surgical procedure thus Include
the time prior to operative period, the time Component of vital sign
spent during the actual surgery and the time
1. Body temperature
after the surgery is completed.
2. Pulse rate
3. Respiratory rate
Sub classification
4. Blood Pressure
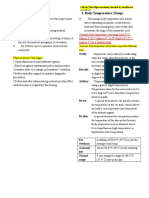
Body Temperature: - the Balance B/n
Perioperativeperiods have three main phases
they are Heat gain And Heatloss.
The average Healthy person Body
1. Pre-operative period temperature is B/n 36.5 – 37.2 0C.
2. Intra operative period
3. Post-operative period Common site
1. Pre-operative period: -A time line which A. Axillary:- taking Body temperature
starts from when the surgeon decide to make from the space between The arm pit
surgical procedure until transferring the pt to And Normal Range is B/n 35.5 –
the operating table. 37.50C.
Contraindications
Pre-operative Nursing Cares: - A
Nursing activity which is given before a
Emaciated
surgical procedure is done. It may be Axillary Surgery
Educative or procedural. Upper extremity amputation
Purpose Convulsion
Children less than 5yrs old
1. To prepare the pt psychologically and
physically N:Bit’s the Most Convenient site to Measure
2. To prevent Intra andpost-operative body temperature
complication
3. Tofacilitate Recovery from Anaesthesia B. Oral:- taking Body temperature
4. To control pain through Mouth And Normal Range is
B/n 36.5 – 38.50c
Nursing Task during pre-operative period Contraindications
1.
Informed consent
Childrenless than five years old.
2.
Monitor vital sign Convulsive (seizurept.)
3.
Provide cleansing Enema Psychotic pt.
4.
Provide NG Tube Insertion
5.
Provide Catheterization
Nausea and vomiting
6.
Secure IV line. Oro Nasopharyngeal tube
7.
Skin preparation. Insertion.
8.
Keep the pt NPO.
N: B the Most accessible site to Measure Body
1. Informed consent:- it is a states that
temperature
the pt has been inform about the
procedure to be done the alternative
C. Rectal:- taking Body temperatures
treatments and Risk involved, And that
through the anus and Normal Range
the pt agree to the procedure
is B/n 37.5 – 39.50c.
Contraindications
2. Monitor vital sign: - it refers to
Measurements of the clients Body
-anal surgery
temperature, pulse Rate, Respiratory rate, Haemorrhoid
and Blood pressure. Congestive Heart failure
Imperforated Anus
©: Solomon Tegegne 2012 E.c Page 1
[COMPETENCE BASED PRACTICAL SHORT NOTE FOR NURSING ] April 29, 2020
N:B the Most accuratesite and used Blood pressure: - a force Exerted by the Blood
to measure the core or central Body against the wall of the arteries measured in
Temperature. Millimetres of Mercury (mmHg) and it
described as systolic and diastolic Manner
Pulserate: - A Number of Heart beat per a
minute. 1. Systolic BP: -A pressure occurs during
the contraction of ventricle and it’s
Pulse: a wave of Blood generated by ranged B/n 100 – 140 mmHg.
contraction of ventricles. 2. Diastolic BP: - A pressure that occur
during the Relaxation of ventricle and its
Type of pulse pressureMeasured B/n 60 – 90 mmHg.
1. Peripheralpulse:- located in peripheral site2. Procedure for Body temperature
Apical pulse:- located in central site onthe
Apex of heart. 1. Wear disposable glove and assess the site of
measurement.
Common pulse site
2. Rinse the thermometer in antiseptic
1. Radial pulse: - It found the place where the solution for at least 15 – 30 minutes.
radial artery runs along the radial bone on the
tomb side of the Inner aspects of the wrist. 3. Clean with normal saline solution from Bulb
to steam then dry
It commonly used for Adult (60 –
90/100 bpm) 4. Make sure that the thermometer below 350c
if it is not,shaking until it’s Become below
2. Apical pulse: - It the contraction of the 350c.
Heart rate riches also can be palpated with the
Hand or auscultated with stethoscopes placed 5. Clean the site of Insertion and put
over the area of the ventricle at 4th and5th ICS thermometer on the proper place
It commonly used for Infant and 6. Wait for 2-3 mint for rectal, 5min for Orals,
Children (120 – 160 bpm) 5 -10 mint for Axillary
N: B the Rate of Pulse is Expressed in Beats 7. Clean thermometer from steam to bulb then
per minutes Read the findings by held up the thermometer
on the Eye level.
3. Respiration Rate;- A Number of
Respirations a person takes per minute. 8. Clean thermometer with normal saline
Normal Respiration Rate solution and Immerse in antiseptic solution.
Birth – 2 month - 30 - 60 Bpm
2 month – 12month 26 – 50 Bpm 9. Documentation.
1- 6 year 20 – 40 Bpm
Provide Cleansing Enema
6 – 10 year 18 – 24 Bpm
Adolescent 16 – 24 Bpm
Enema: - A process of Introducing a fluid or
Adult 12 – 20 Bpm
Solution through Rectum to colon to be
Returned or Retained.
Focus
Purpose
Count Respiration for one full minute
if the Rate is Abnormal or Rhythm is To Empty the colon
Irregular. To soften impacted stool or to relieve
Wait for 5 -10 mint before assessing constipation.
Respiration if pt had been active. To prepare the Pt. for surgery (pre
operatively)
To administer medication.
To visualizing the Intestine during
radiotherapy.
©: Solomon Tegegne 2012 E.c Page 2
[COMPETENCE BASED PRACTICAL SHORT NOTE FOR NURSING ] April 29, 2020
Type of Enema Infant 14 – 18fr
1. Cleansing Contraindications
2. Retention
3. Rectal wash out Haemorrhage
4. Flatus tube insertion Appendicitis
Colon obstruction
Common Solution for Enema Acute Renal failure (ARF)
Congestive Heart failure (CHF)
1. Hypertonic solution :- Sodium phosphate Haemorrhoid
2. Isotonic solution: - physiologic saline. Obstetric problem(APH)
3. Hypotonic solution: - tap water.
Rectal wash out ;-A process of washing a
Classification of Returned or Retention colon and Rectum through a process of
Enema Enema.
1. Returned (Evacuative) Enema Purpose
To Empty the Rectum.
A. Cleansing Enema To prepare the Pt. for Rectal Surgery
B. Helminthic Enema To remove any debris from the Rectum.
C. Ice (cold) Enema
2. Retention Enema -N:B –The procedure for rectal wash
A. Anaesthetic Enema. out always Proceed 1hr after
B. Nutritive Enema.
cleansing Enema
C. Sedative Enema.
D. Oil Enema.
Precaution
Cleansing Enema: - a sub division of
Returned Enema that mainly used for It should be washuntil clean water is
cleaning the Rectum or colon. Returned.
While perform Rectal wash out use a
There are two classifications
funnelor y- shaped Instrument
1. High cleansing Enema.(≥ 45 cm)
Insertion of flatustube ;-A process of
inserting a tube to relief abdominaldistension
2. Low cleansing Enema. (≤ 35 cm)
as result of Excess accumulation of gas.
Common position for Enema
Purpose
1. Left lateral position (sim’s) for Adult
To Relief Abdominal distension
2. Dorsal Recumbent for child
To provide comfort
3. Lithotomic position for Infant
To Aid peristaltic movement
Amount of Solution for Enema
Site of tube
750 - 1000 ml for Adult.
20 – 22 fr
500 – 750 ml for Adollcent
14 – 15 fr
300 – 500 ml for School Age
250 – 300 ml for toddler
N:B Before Inserting the tube in to anal Orifice
150 – 250 ml for infant
submerge the tube part in to water (siled in
water) to prevent the Entrance of air.
Temperature of solution
Precautions for enema
Adult 41.5 – 43.50c
Infant child: - Equals to their Body to
1. Befor administering fluid Remove the air
(370c – 380c)
from Enema Cane.
Size of Rectal tube for Enema
2. If the Pt.complains of cramping or has
difficulty retaining Solution
Adult 24 – 28fr
Child 18 – 20/24fr
©: Solomon Tegegne 2012 E.c Page 3
[COMPETENCE BASED PRACTICAL SHORT NOTE FOR NURSING ] April 29, 2020
immediately for a few secondand continue the
procedure.
a. slow administration rate
10. After administer the fluid Instruct the pt.
b. Temporally stop flow to hold deep breath and remove tubing gently
with supporting of the anus.
c. Encourage slow deep Breathing through
mouth for a few seconds. 11. Wait for 10 – 15 mint and offer bed pan or
tell the pt. to go to toilet.
3. Be for administer Enema assess the
contraindications and take the actions N: Bwhile offering Bed pan if the pt. is weak
assist him positioning on bed pan.
4. While administering Enema Maintain the
length of inserting tube 12 Provide documentation.
7.5 -10cm for adult Document
7.5 cm for child
3.7 cm for Infant *colour of stool
5 While Administering Enema lubricate
5cm of the rectal tube In order to *Amount of fluid Return
prevent soft tissue damage.
* Content and consistently of returned fluid
Complication of Enema
* Odour
Abdominal distension
Soft tissue damage Nasogastric tube Insertion
Pain and discomfort
DEFINITION;-A process of administering a
Peritonitis
nasogastric tube through the nostril in to the
PROCEDURE FOR CLEANCING ENEMA stomach.
1. Prepare the solution and cheek temperature Purpose
of fluid.
to feed the pt. post operatively (gavage)
2. Rise Enema cane, Release clamper and to provide gastric wash out (lavage)
allow solution to flow inthe tubing In order to to Aspirate gastric content
remove the air. to provide medications
To prevent Nausea and vomiting after
3. Clamp tubing and wear disposable glove surgery by decompressing the
and provide water proof pad (Mackintosh) stomach.
4. Position pt. in left lateral with right leg flex. Measuring the tube length
5. Prepare KY jelly on the gauze 1from tip of nose -> Earlobe ->xyphoied
process for Adult
6. Support the two fold of buttock with non-
dominant hand and clear with tissue paper. 2 from Ear lobes -> tip of Nose ->xyphoied
process for child
7. Lubricate rectal tube and instruct the pt. to
take deep breath. 3. from tip of Nose to umbilicus for Infant.
8. Insert tube smoothly in circular motion and For orogastric Insertion
remove clamper.
Measure From corner of mouth to ear lobe
9. Observe the pt. facial Expression Intra then to xyphoied process
procedurally.
Position for NGT
N.B if the pt. complain or develop
abdominal cramp, clamp the tubing Semi fowler position: - it help to
prevent aspiration during insertion and
facilitate the opening of oesophagus.
©: Solomon Tegegne 2012 E.c Page 4
[COMPETENCE BASED PRACTICAL SHORT NOTE FOR NURSING ] April 29, 2020
Confirmation methods Purpose
to Reduce Bladder distension
1. Communication symbol. to prevent Incontinency
2. Gastric content aspiration to collect sterile urine specimen
3. Bubbling motion to provide bladder irrigation
4. Whooshing sound over EpigastriaRegion Type of catheter
5. Chest – X – ray.
N:B During Aspiration 1. Plain catheter(single lumen catheter)
* Clean watery colourindicates tube is in 2. Folly catheter (double and triple limen
trachea. catheter)
* Dark brown colour indicate tube is in 3 condom catheter
stomach
Type of catheterization
* If the aspirating content changes blue
litmus paper in to Red the tube is in 1. Intermittent (straight):- A single use
stomach. straight catheter introduced in to
bladder for a short period to drain the
Procedure for NGT urine 5 – 10 minute
.Purpose
1. Place the pt. in semi siting position and put to relive bladder distension
towel over the chest. to empty bladder prior to
delivery
2. Assess the nostril and clean with cotton
tipped applicator 2.Indwelling (Retention or folly):- used to
stay in place for urine drainage
3 Measure the length of tube and mark on the
maximally it wait for 7 -10 days.
exact point.
Purpose
4. Insert the tube properly to prevent Incontinency
To prevent urine contact on
N:B when you Rich on the nasopharynx area the incision site after
cheek back of throat with spatula and perennial surgery
flashlight to see, if coiling has occurred. Positions
For females:- Dorsal Recumbent with
5. Give straw water and Instruct the pt. to slight knee flexed
follow your order to take shallow. For Males :- Supine position with thigh
slight Abduction
NB: pt. should take straw water during
Insertion to facilitate the iteranceof NG tube. Site and length of Insertion
6. After insertion of tube clamp immediately Male 18 – 22 fr and 16 -25 cm
and start to cheek the placement Female 14 – 16 fr and 4 – 6 cm
For children 10 – 12 fr
N: Btakes 10 cc/ml of air and inflates through
the tubing in to the stomach. If whooshing Precaution
sound is heard over the Epigastric Region with
the help of stethoscope the tube is in stomach. 1. While Inserting catheter Avoid force
full application.
7. If the placement confirmed on the exact site
Apply adhering tape (plaster) 2. Follow strict aseptic technique to
prevent urinary tract infection
Provide catheterization
3. Keep the pt. relaxed by providing
Definition: -A process of administering privacy and Explaining the sequence
catheter through urethra in to the bladder. of the procedure.
©: Solomon Tegegne 2012 E.c Page 5
[COMPETENCE BASED PRACTICAL SHORT NOTE FOR NURSING ] April 29, 2020
4. Administer 5 – 10 cc/ml of distal 11. Support labia with non-dominant hand
water to secure the catheter in to start cleaning with bethadinSolution then dry.
Bladder. 12. Lubricate the catheter and instruct the pt
to take deep Breath then insert.
Complications
13. Clump immediately after urine return and
Soft tissue trauma. give avance push
Urinary tract infection
Haematuria 14. Inflate distil water and cheek the security.
Pain
15. Remove fenestrated towel and connect
PROCEDURE FOR CATHETERIZATION catheter with urine bag
1. Wear disposable glove and positioning the 16. Document all about the procedure.
pt.
Provide Intravenous fluid Infusion
2. Place water proof pad under the Buttock
Intravenous Infusion;-A process of
3. Offer Bed pan and other needed Equipment administering a large volume of fluid
in to circulation through vein
4. Purring water at centre – far – near
PURPOSE
5. Start cleaning with Cotton Ball 1 from
minspubis to simphussis pubis to maintain fluid & Electrolyte
to introduce medication
1. far growing to provide caloric when the pt is NPO
2. near growing to maintain acid base balance
3. far labia major and minor Type of solution
4. near labia major and minor 1. Isotonic Soln:- a fluid that have the
5. from clitoris to vagina same Osmolality with that of the Body
6. from clitoris to anus plasma
Eg.Normal saline (0.9%)
6 Againpurring water from far – near – centre. Dextrose water (5%)
Ringer Lactate (RL)
7. Dry with the same sequence and remove
Plasma and albumin (5%)
bed pan
2. Hypotonic Soln:- a fluid that have
less Osmolality than that of the Body
8. Put the pt side lying position and dry the
Plasma
Buttock with tissue paper
Eg.NS (0.45 and 0.33%)
9. Follow the 5: 2 principles. 3. Hypertonic Soln:- a fluid that have
high Osmolality than that of the body
5 clean preparation Plasma
1. Apply KYjelly on sterile gauze Eg. DW 10 & 20%
2. Cut plaster Common vein site
3. Prepare solutions 1. Cephalic vein
4. Adhere (attach) urine bag on bed. 2. Bacilic vein
5. Prepare pt position 3. Medial vein
2Sterile preparation 4. Dorsal Network vein
1 wears one hand surgical glove and 5. Scalp vein
prepares distil water Precautions
2 check the functionality of catheter 1. Remove air from the IV line
2. Start securing from distal to proximal
3. Do Not secure the IV line on joint area
Drop= Total fluid Volume x Drop Factor
4. Check the Expiry date
Total time taken x 60 mint
Common flow rate formula
10. Prepare sterile filed on the pts genital area
and transfer Equipment to the site. N;BDF = 15 or 20
15for Blood
©: Solomon Tegegne 2012 E.c Page 6
[COMPETENCE BASED PRACTICAL SHORT NOTE FOR NURSING ] April 29, 2020
20 for solutions 2 Infection:- an invasion of photogenic
Microorganism in to the body may be due to
1. To fined the volume of fluid to be contamination of Infusion size or solution
administer per hour
CLINICAL MANIFESTATION
ML/hr = ML of fluid to be infused
-fever sort after infection
No of hr. To be infused
-Back or Head ach
-Increase PR & RR
2. To fined volume of fluid to be
-Nausea and Vomiting
administer per minute
diarrhoea
ML/min = ML/hr (TFV/hr)
Septicaemic shock & death
60min/hr
3. To fined the number of drop Management
gtt =ML/min x DF -disconnect the IV line
-culture the cannula and Treat the cause
EX. Administer 2000ml of RL within 6hr -Establish other IV line
3 Phlebitis:-an inflammation of vein related to
Soln = gtt = TFV x DF mechanical irritation from Needle or chemical.
TTr x 60min Clinical manifestation
Gtt =2000ml x 2040000= 111,1drop/mit local acute tenderness
6 x60min 360 -Redness,
warmth
OR ML/hr = 2000/6 = 333.3ML/mit -slight Oedema over the insertion site
ML/min = 333.3/60 = 5.5ml/mit Management
gtt =5.5 x 20 = 111,1dro/mit Discontinue the drainage and change
the life
Factor influencing flow rate
Warm hot compress over the area
1. Position of the arm
4 Hematoma:-when blood leak into the
2. Position & potency of the tubing
surrounding tissue
3. The Height of Infusion bag
4. Possible Infiltration of fluid leakage CLINICAL MANIFESTATION
COMPLICATION
1. Air Embolism:- foreign Body or air in Immediate swelling
the Blood Blood leaking out side
Cause:- air inter through the infusion line Management
Clinical manifestation Remove the needle
Apply ice then Heat compress
dyspnoea
Lin consciousness 5 FLUIDS OVER LOAD
Hypotension
Back or shoulder pain Cause:-
Weak & Rapid Plus
Increase Infusion rate
Management Renal or cardinal disease
Disconnect the line immediately CLINICAL MANIFESTATION
Place the PtTrendiler Burg position
with lift side Monitor Vital sign and Oedema
assess Breath sound Dyspnoea
Provide O2 therapy(of Necessary) weight gain
©: Solomon Tegegne 2012 E.c Page 7
[COMPETENCE BASED PRACTICAL SHORT NOTE FOR NURSING ] April 29, 2020
shallow & increased Respiration Procedure
1. Place towel or water prove pad under
Management body part to be shoved
2. Drape patient with towel, leaving only
decrease the Rate the area to be shaved atone times
place High fowler position& assess exposed.
Breath sound 3. Cut long Hair short with scissor,
Monitor vital sign lather skin with gauze sponges dipped
in antiseptic soap
Procedure for Intravenous
4. Shave small area at a time
1. Cheek the physician Ordered and
N.B with non-dominate hand hold gauze
explain procedure sponge to stabilize skin. Then hold razor
2. Collect an necessary Equipment at 45 degree angle in dominate Hand and
shave in the direction of hair growth.
3. Cheek the Expiry date of the fluid
4. Connect the Iv set and remove the air. 5. Rinse and dry the size
5. Place mackintosh and prepare plaster
N.B during skin preparation cleans with
6. Apply tourniquet and wear surgical
cotton tipped applicators or cotton Balls
glove dipped in anti-septic Solution if the site is over
7. Clean the site and put on sterile gauze body crevices Eg. Umbilicus or groin
8. Insert the cannula to the size
INTRA OPRATIVEPERIOD
N.B immediately remove tourniquet, if the
A time line starting with transferring the pt to
blood is observed (naked eye) in the top of the operating Table and ends when the Pt goes
the cannula. to post anaesthesia care unit (PACU)
9. Remove Needle and connect with IV set Members of surgical team
10. Cheek the sign of Infiltration and apply Surgical team:- A group of Highly Trend and
plaster educated professionals who Cordiant there
effort to assure the welfare & safety of the
11. Adjust flow rate and provide label
client.
12. Documentation
amount of solution although the specifics of each types of
surgical procedure may rare certain key
drop rate per minute
players must always be present such as
added medication 1. surgeon
2. assistance surgeon
SKINE PREPARATION 3. scrub nurse
4. circulatory nurse
A preoperative procedure performed to 5. anaesthesiologist
decontaminate and reduce the number or
Others
organisms on skin, to eliminate the
transference of such organisms in to the 6. pathologist
7. radiologist
Incision site. 8. perfusionist
1. surgeon:- heads(leads) the surgical
Purpose team and make decision, concerning
the surgical procedure
To remove hair from well-defined skin
area N.B depends on the surgical procedure to
To prevent round infection perform a second surgeon or special trained
postoperatively nurse serves as Assistance.
©: Solomon Tegegne 2012 E.c Page 8
[COMPETENCE BASED PRACTICAL SHORT NOTE FOR NURSING ] April 29, 2020
2. Circulation Nurse:- A Nurse who -providing suturing
circulating in the operating room to monitor
the procedure N.B Assistant surgeon (Registered Nurse first
Assistant) must work with a surgeon and are
N.B The circulating role is a major one for not independent practitioners.
perioperative nurse
Operating room areas
Responsibility of circulating Nurse
1. Satirize operating field
Assess the patient preoperational ( eg. 2. Non sterile area
CVS, Vital sign, Nutrition) Intra Operative Nursing period:- A
Ensuring all equipment is working Nursing are a given under intra
properly operative period
guarantying sterility of instrument &
supplies Purpose:-
Transporting the Pt to operating room.
-to minimize cross contamination
Assist the Pt transferring to Operating
To prevent intra& postoperative
table& positioning
complication
Performing surgical skin preparation
General Nursing task
N.B. Circulatory Nurse can coordinate all
personnel with in the operating room. Assist with Pt position
Prepare the Pt skin
3.Scrub Nurse:- A registered Nurse who assist Managing surgical specimen
in surgical procedures by setting up the room Assist surgeon as needed throughout
before the operation, working with surgeon the procedure
during surgery and prepare the Pt for move to Monitor intra-operative complications
recovery room Document intra-operative events
Common scrub Nurse Task
Responsibility of scrub Nurse
1. Surgical scrub:- the process of removing
as many micro-organism as possible from
1. Before surgery
the hands and arms by mechanical
Ensure the operating room is clean &
washing and chemical antisepsis before
ready to be set up
participating in surgical procedure
Prepare the instrument and equipment
2. Gowning: - a process of worn A robe or
need for surgery
smoke in operating rooms and others
Count all sponges, instruments, and
parts of hospitals as guard against
needle and preserve the sterile
contamination.
environment by "scrubbing" which
3. Gloving:-A process of donning sterile
require washing hands with special
Rubber gloves in such a way to preserve
soap& potting on sterile garments.
asepsis of the operator before each
2. During Surgery
surgical procedure.
Selecting and passing instrument to
the surgeon Methods of growing:- 1. Close gloving
3. After surgery 2. Open Gloving
Count all instrument, sponges and
others tools Preparation for surgical scrub
Apply dressing to the surgical site
Transport the Pt to recovery area 1. The skin and nail should clean &
Assistant Surgeon Activities Intact
2. Finger Nail should be short and avoid
Some of the activities are:- - polishing
3. All jewellery should be removed
provide exposure of surgical area 4. all Hairy area should be covered
-Using instrument to hold and Cut
-Retracting and handling tissue
-providing haemostasis Ex IV infusion
©: Solomon Tegegne 2012 E.c Page 9
[COMPETENCE BASED PRACTICAL SHORT NOTE FOR NURSING ] April 29, 2020
General Instruction for surgical Hand D rinse (wet) hands& arms then dry with
washing sterile to
1. When wash the Hands, they are held 4. Apply gowning & Gloving
above the level of Elbows
2. The water should run from least -maintaining sterility of the gown while
contaminated to more contaminated preparing for application the fingers remain in
area(Hand Elbow)
the cuffs to protect the sterility of the gown
3. A sterile towel is used to wipe the
hands and arms(starting from the and prepare for closed gloving
palm to the Elbow)
4. Prior to surgical scrubs, it will be Post –Operative period
necessary to put on the head caps and
masks.
Atime line begin with transfer the pt to the
Intra- Operative procedures surgical recovery area and ends with recovery
1. Apply Medical Hand washing from surgery
A. Remove all jewellery from the Hands
Nursing activities (care) which is given
B. Stand in front of sink& Turn on water
C. Rinse(wet) hands starting 5cm above after surgery is called post-operative
wrist Nursing cares. Under post-operative
D. Apply soap or antiseptics
period Nurses are play a critical role in
E. Wash hand using phenyl of lather and
friction returning the Pt to optimal level of
Rub palms and back of hands then finger functioning.
nail with circular motion
Purpose of Nursing care
To decrease(reduce) post-operative
F. Rinse Hand& wrist thoroughly keeping
Hands down and Elbow up complications
To facilitate recovery or wound healing
G. Turn off water by using towel
process
H. Dry hand thoroughly from finger to wrist To assess patient physiological status
and forearm
Post-operative period can be divided in two
2. Wear medical gown and mask then cap
sub phase
3. Apply surgical Hand washing
1. Immediate post-operative
A. wet (Rinse) hands and Arms 2. Later post-operative
B. Apply soap to make good lathers
1. Immediate post-operative:- is the
first few hours after surgery when the
C. scrub with Brush so that every areareceives
clients is recovering from the effect of
15 stork for fingertip, 10 for palm and 5 for
aesthesia.
forearms.
Immediate Nursing activities
Scrubbing technique
1. Patient transferring from Streature to bed
1. Scrubbing finger tips and nails
2. Patient positioning
2. Scrub each side of fingers and web space 3. Assessing wound(incision)site
3. Scrub palmer surface 4. Assessing drainage tubs
4. Scrub dorsal surface 5. Monitoring vital signs
6. Provide suctioning& 02 therapy(if
5. Scrub exterior side if firearm
Necessary)
6. Scrub interior side of forearms 2. Late post-Operative:- its period that
staring with a complete recovery from
anaesthesia
©: Solomon Tegegne 2012 E.c Page 10
[COMPETENCE BASED PRACTICAL SHORT NOTE FOR NURSING ] April 29, 2020
Later post-operative Nursing activities very 15minutes the first hours, every
30 minutes the next two hours every
1. Suctioning
2. Oxygen therapy hour for four hours and finally every
3. Wound care 4hours.
4. Nasogastric tube feeding
5. Post-operative Exercises 7. Give setting priority
General task under post-operative
A. suctioning
1. Prepare Anaesthetic Bed
Definition:-A process of aspirating secretion
It is a type of bed prepared for receiving the Pt from respiratory tract by using a Negative
from operation room. pressure
Purpose Purpose
to facilitate circulation To facilitate ventilation
to prevent chillness To remove secretion
To prevent infection
to provide comfort
2. Transferring patient from strature to bed Indication
While transferring pt use the Visible secretion in the air way
following two methods Coarse & Noisy Breath sound
1. Caring methods Type of suctioning
2. Sheet transferring Methods 1. Oro-pharyngeal suctioning (Approximately
13 cm )
N: Bstrature should stand perpendicular for
caring Methods and parallel for sheet Use when Pt is able to cough effectively but is
transferring Methods. unable to clear secretions by expectorating or
swallowing
2. Positioning
-immediately after transferred pt to bed 2 Naso-pharengialsuctioning (14-16cm)
nurses must be prepare Pt position in to
supine with Head turn to left side. This When the Pt with pulmonary secretions is
position wills help to prevent Aspiration unable to cough and does not have an
Artificial air way.
4. Check derange tubes (connection
tube) 3Tracheal suctioning
Check the functionality of catheter, Iv line and It Accomplished through in artificial
NG tube air way
5. Assess wound size It may be through
-Observe wound size for bleeding or
leakage of suture A. Endotracheal tube (12-14 cm)
B. Tracheostomy tube (10-13 cm)
N.B if the Bleeding is easy to control use a Suctioning technique
strictsatirize technique and try to control but If 1. Rotation for mouth suctioning
it is much and heavy bleeding immediately 2. In and out for Nasal and other
informed to the physician. suctioning
Position for suctioning
6 Monitor vital sign 1. Semi fowler for conscious Pt
2. Flat position with Head towards
Vital sign should monitor frequently. you for unconscious Pt
Assessment order may vary, but usual
frequency includes taking vital signs
©: Solomon Tegegne 2012 E.c Page 11
[COMPETENCE BASED PRACTICAL SHORT NOTE FOR NURSING ] April 29, 2020
Precaution colour and any Odour of secretions
pre & post respiratory status
1. The Negative pressure of suction
machine should be adjust B/n 80-
B. Oxygen administration
120mmhg. But if the suction machine
Definition;- process of Administration of
is portable adjust b/n 7-15 mm Hg
Oxygen greater than that found in the
2. Before and after provide suctioning
atmospheric air (>21%)
give hyper ventilation or hyper
oxygenation Oxygen therapy:-process of Administering
Oxygen as a medical intervention
N.Buse Manual restatingAmbubag connected
to an oxygen source to provide hyper Purpose
oxygenation
To maintain Blood& tissue 02
Hyper-oxygenation 10-15 L/mint for 30 concentration
seconds To sustain life and mental function
Hyper-ventilation 3-6 cycle with Ambubag To rise arterial blood gas level back to
3. Give suctioning for 10-15 second and normal
rest for 30-60 second in one cycle
Indication
N:Bsectioning should be given for 4 to 5 cycle
Hypoxia and Hypoxemia
Complications Cardiac arrest
Hypoxia/Hypoxemia COPD( chronic Obstructive pulmonary
Tracheal and bronchial disease)
trauma Atelectasis
Pulmonary haemorrhage Anaemia
Bronchospasm
Dysrhythmia and Brady card Methods of O2 Administration
Procedure for suctioning 1. Nasal Cannula:- it used when low O2
concentration are needed
1. Place the Pt on preferable position
N:B:- It is relatively simple and comfortable
2. Open sterile field and adjust solutions
way to talk, cough and eat with therapy
3. Give hyperventilation or oxygenations
4. Wear surgical glove and put draping Oxygen concentration
over the chest
5. Transfer kidney dish to the chest(on One litre 24-25%
sterile drips) Two litre27-29%
6. Clean the tip of suction machine and Three litre 32-33%
connect with suction catheter. Four litre33-37%
7. Check the functionality of suction Five litre 36-41%
machine and lubricate the catheter Six litre39-45%
8. Provide suctioning for proper duration
N:B During administering of O2 with cannula
N.B. suction (10-15 sec) method never administer greater
than 45 or 50%
Rest for (30-60 sec) Do for 4 to 5 cycle
2. Face mask delivery;-It cover the client
9. After all sucking out Normal saline Nose & Mouth used for o2 Administration
solution form kidney dish and return and generally deliver adequate
all equipment to the proper place warm(Humidified)Oxygen.
N:B Do Not forge to give Hyper ventilation Type of facemask
or Oxygenation after procedures.
A. Simple facemask:- it deliver 40-60% 02
10 Documentation concentration
amount of secretion
consistency
©: Solomon Tegegne 2012 E.c Page 12
[COMPETENCE BASED PRACTICAL SHORT NOTE FOR NURSING ] April 29, 2020
B. Partial Re-breath face mask:- It Factor affecting the Onset and severity of
deliver 60-90% of o2 concentration with the O2 toxicity
a flow rate of 6 to 10 lit/mint
1. Concentration of the gas used
N:B - it have reserve bag 2. Duration of exposure
3. Susceptibility of the Individual
C. Non- Rebreathe facemask:- it deliver person
95-100% of O2 concentration with a
flow rate of 10 to 15 lit/mint Clinical manifestation
D. Venture(ventricular) face mask:-Oxygen
concentration vary from 24 to 40 & sub sternal chest pain
50% at flow rate of 4 to 10 Lt/mint fatigue
3. Face tent delivery:-it can replace O2 cough with tracheal irritation
mask when mask are poorly tolerated by Inspiratory pain
the Pt. dyspnoea and restlessness
It provide 30-50% of oxygen concentration
at 4 to 8 Lit/mint Management
Position for O2 Administration N:B. Treatment is being purely symptomatic,
prevent on and early recognition of the
1. Semi fowler position for conscious toxicity is of primary importance.
2. Flat position for un conscious
Typical sign of Hypoxia 1. Early prevention
Tachycardia Limitation of prolonged exposure
Tachypinea to high concentration of Oxygen
Rest lessens 2. After Exposure
Cough Disconnect administration
Shortness of breathing Allow the Pt to performpositive
Irritability continuous air way
pressure(PCAP) and positive End
Special consideration Expiratory pressure (PEEP)
Put the Pt in High fowler
1. Never administer more then 2-3L/mint of position
O2 to the Pt with chronic obstructive
pulmonary disease(COPD) Precautions (O2 Administration )
2. Flow rate is depends on Pt condition
3. O2 is medication& Except in Emergency 1. Post NOSMOKING sign on the client’s
situation it should administer when the bed, door and cylinder
physician prescribed 2. Avoid any volatile substance
4. Assess Blood gas level after administered 3. Fire extinguisher must be available
O2 4. Electrical substance should be
grounded
Complications 5. Avoid line and suite clothe
6. The Nurse should always cheek the O2
1. Oxygen toxicity level of portable tank before
2. Oxygen Induced Hypoventilation transporting to ensure that there is
3. Dryness of respiratory mucosa enough remaining in the tank.
Oxygen toxicity:- associated with
long term exposure to high Procedure for O2 Administration
inspired oxygen concentration
1. Positioning the Pt.
Cause 2. Clean the nostril with cotton typed
applicator
Friction of inspired O2 (FIO2) > 60%
3. Refill the Humidifier Bottle with sterile
more than 2-3 days
water until maximum level
4. Connect the cannula to the out let
5. Open the gate valve and regulate the flow
rate
©: Solomon Tegegne 2012 E.c Page 13
[COMPETENCE BASED PRACTICAL SHORT NOTE FOR NURSING ] April 29, 2020
6. Cheek the functionality and delivers to the Purpose
Pt.
7. If you use the Nasal cannula put Gauzes to facilitate wound Healing process
over ear lobes to prevent damage of skin to prevent Infection.
and to provide comfort to Maintain skin Integrity
Method of cleansing
N.B always before Administering O2 post No 1. . Aseptic wound:- clean from Inside to
smoking sign on the cylinder, On the Pt. bed and on outside.
the door 2. Septic wound:- clean from outside to
8. Wound care Inside.
3. Surgical wound:- clean from top to
Wound: - A disruption in the continuity of bottom.
cells or tissues.
Principle of wound care
Wound classification
1. While provide wound care often clean
Wound may be classified in two different ways from least contaminated area to more
contaminated area.
1. Based on to mechanism of Injury 2. Avoid, using cotton Ball because they
2. Based on degree of contamination. may shed fibres in to the wound.
3. Used each gauze pad only for one
1. Mechanism of Injury: - wound may be
stroke.
described as incised, contused lacerated or
4. Clean at least 2.5 cm beyond the end
puncture.
of new dressing.
A. Incised wound: - made by clean cut with
Common solutions used to clean wound
sharp instrumentsEx surgical wound
1. Normal saline.
N.B It usually closed by suture.
2. Hydrogen peroxide.
B. Contused wounds: - made by blunt 3. Sodium hypochlorite.
force and are characterised by considerable 4. Providing Iodine.
injury of the soft part, Haemorrhage and 5. Acetic acid.
swelling.
N: B:- Antiseptic solution such as acetic acid,
C. Lacerated wound: - these are with sodium Hypochlorite and povidine Iodine’s
tagged irregular Edges may damage tissue and delays wound healing
process so that they must give with A special
D. puncture wound: - this result in cautions.
small openings in the skin.
Dressing:- aprocess of covering the wound site
E. Avulsion: - these are with separation by using a strict sterile technique.
or torn off tissue from body
Purpose
2. Degree of contamination
to prevent pathogens from entering of the
Clean wound (Aseptic wound) wound
Contaminated (infected) or septic to prevent further Injury.
wound. to promote comfort of the pt.
to promote wound healing process
Complication of wound to absorb drainage of discharge.
Scar Type of dressing
Dehiscence
keloids 1. Dry (non – antiseptic) dressing
Necrosis
Contracture - Sterileunmediated dressing used for fresh
Cellulitis wound
Wound care: - A process of cleaning and
providing dressing.
©: Solomon Tegegne 2012 E.c Page 14
[COMPETENCE BASED PRACTICAL SHORT NOTE FOR NURSING ] April 29, 2020
2. Wet (Antiseptic) dressing Position
Sterile moisten dressing used for infected Placept on semi siting (semi fowler)
wound and also used to supply heat to the position.
tissue.
Procedure (for Gavage)
3 Pressure dressing
1. Put the pt on recommended position.
A thick sterile pad made of gauze or gauze and 2. Cheek for tube placement
cellulose applied with a firm bandage used 3. Cheek peristalses movement.
when there is danger of bleeding.
NB: while you monitor peristalsis
Procedure for wound care movement place stethoscope for 2 minute
on each quadrant of the abdomen (RUQ ->
1 assesses the wound site and placemackintosh RLQ -> LLQ -> LUQ) and in order to say no
peristalses movement wait for at least 5
2 open sterile filled and prepare the solution minute on each Quadrants.
3 drape the old dressing with normal saline Remember if the RUQ have pain
solution and remove smoothly start cheeking from RLQ.
4. Measure the Residual Amount
4 assess the skin condition and suture site
N: B If the Residual amount is < 100
5 remove disposable glove and wear surgical glove
provide feeding
6 clean the wound site with recommended
If the residual Amount is > 100 wait for 4hr
solutions and cleaning techniques
5. Return the Residual Amount in to
7 dry the site and apply dressing
gastric and give 10 – 50 ml of clean
8 make the patient in comfortable position water in order to Irrigate the tube
6. Provide feeding through funnel
N;B if ordered medication is available give to the
patient without breaking sterility N: B do not give much Amount of food
it.should be B/n 250 – 500 ml.
9. Nasogastric tube feeding (Gavage)
7. Again give 100ml of clean water and
Definition: A process of Administering dress the tip of tubing
Nutrition feeding through NG tube. 8. Documenting
Amount of food
Purpose Pt. condition
Time of feeding.
to maintain acid base balance
to provide caloric (Nutrition’s) N: Balways after giving feeding let the pt. on
To promote pt. health. semi fowler position for 20 – 30 minutes.
Type of NG tube feeding Complications
Abdominal cramp
1. Blouse form. Gastric distension.
2. Continuous form vomiting
Aspiration
Precaution
10. Post-operative Exercise
1. The food must be liquid and warm
2. Cheek tube placement A. Deep Breath and cough Exercise
3. Cheek peristalsis movement and
bowel sound Purpose
4. Cheek residual amount
5. Do not allow the air inter to stomach facilitate Respiratory functioning by
through tubing. increasing lung Expansion
prevent alveolar collapse
©: Solomon Tegegne 2012 E.c Page 15
[COMPETENCE BASED PRACTICAL SHORT NOTE FOR NURSING ] April 29, 2020
Encourage Expectoration of mucus Type of ROM
secretion
1. Active ROM:- performed by the pt
Precaution (Before procedure) himself
2. Passive ROM:- performed with the
1 assess Quality, Rate and depth of Help of other person.
Respiration General principles for ROM
1. Never do ROM exercise beyond the
2 Assess placement of Incision Evaluate whiter capacity of the individual
or not It Interferes with chest Expansion 2. While performing ROM move the Body
part smoothly slowly and
3 Evaluate ability to assume fowler’s position.
rhythmically.
3. While performing ROM, stop the mov’t
temporarily, if the muscle spasticity
Provider (Deep Breath) occurs.
4. Provide passive ROM Exercise two
1. Assist the client to fowlers or sitting times a day.
position 5. While performing ROM use support
2. Have the client place hands palm measuring technique to prevent
down, with middle fingers touching, muscle straining or Injury during
along power of rib cage. ROM exercise.
3. Ask client In hale slowly through the 6. Avoid any tight cloth and jewellery
nose, felling middle fingers separate, during ROM exercise.
Hold breath for 2 or 3 second
4. Have the client Exhale slowly through Procedure
mouth.repeat three to five times.
1. Explain the procedure to the pt
Procedure (cough exercise) how and when it’s performing.
2. Remove all jewellery from the site.
1. Instruct the pt to keep his/her 3. Prepare the comfortable bed
position on fowler position and start ROM.
2. If the client has an Abdominal or A. Neck
chest incision that will cause pain Flexion
during coughing, Instruct the Extension
client to Hold pillow firmly over Hyper Extension
the Incision when coughing Lateral flexion
3. Have client take deep Breath, hold Rotation
for 3 seconds and cough deeply
two or three times. Then Allow
client to Rest.
B. shoulder
N:B Instruct, Reinforce and supervise
deep Breathing and cough exercise Flexion
Every 2 to 3hr post operatively. Extension
Internal Rotation
B. providing Range of Motion Exercise Hyper Extension
Abduction
ROM: - Mobilize all joints through their full Adduction
Range of Motion. Circumduction
Internal Rotation
Purpose
C. Trunk
1. To increased muscle strength
2. To increased joint flexibility Flexion
3. To prevent contracture lateral flexion
4. To Improve physical activity Extension
Rotation
Hyperextension
©: Solomon Tegegne 2012 E.c Page 16
[COMPETENCE BASED PRACTICAL SHORT NOTE FOR NURSING ] April 29, 2020
Adduction
D. Elbow
Flexion 4. Positioning the patient in a comfortable
pronation place.
Extension
Supination 5. Wash the hand and documentation.
E Forearm Terminology
pronation 1. Flexion:- decreasing the angel at a
supination joint
2. Extension:- increasing the angel at
F. wrist joint
3. Abduction: - moves a bone a way from
Flexion middle line.
Lateral Radial 4. Adduction:- moves a bone closer to the
flexion middle line.
Extension 5. Supination:- turning the palm up
lateral ulnas ward mov’t
flexion 6. Pronation:- turn the plum down ward
Hyperextension 7. Rotation:- Move the bone along
longitudinal is axis
G. Hand 8. Circumduction:- circular mov’t of a
part
Flexion 9. Dorsiflexion:- Bending the foot back
Abduction ward
Extension 10 Planter flexion :- Bending the foot
Adduction back ward
Hyperextension 11 Planter: - concerning the sole of the
circumduction of tomb foot.
H. Hip .INSTRUCTING THE PATIENT TO CRUTCH
WALK
Flexion
Extension &Hyper There are five ways of waking with
extension crutches
Abduction &adduction 1- Four – point gait
2- Three – point gait
I. Knee
3- Two – point gait
Flexion 4- Sowing – through gait.
Extension 5- Swing to gait.
J. Ankle and Foot
1 FOUR POINT GAIT
Ankle
1. Patient assumes tripod position
planter flexion 2. Move tight crutch for ward
dorsiflexion 3. Move left foot for ward
4. Move left crutch for ward
Foot 5. Move right foot for ward
Everson 2 THREE- POINT GALT
Inversion
1. Patient assumes tripod position
K. Toes 2. Move walk leg & crutches forward.
3. Bear & balance weight on both crutches
Flexion 4. Advance strong leg.
Abduction
Extension 3 TWO – POINT GAIT
©: Solomon Tegegne 2012 E.c Page 17
[COMPETENCE BASED PRACTICAL SHORT NOTE FOR NURSING ] April 29, 2020
1. Patient assumes tripod position. M:-Change in to Necessary Chemical form
2. Advance right foot & left crutch (Metabolism)
together.
3. Advance left foot & right crutch E:-Elimination of the waste drug content from
together the body via Renal, Biliaryand pulmonary
process (Excretion).
4 SWING – THROUGH GAIT
FACTOR AFFECTING DRUG ACTION
1. Patients assumes tripod position
2. Advance both crutches together. 1. Drug to drug Interaction
3. Lift & swing body through by
supporting weight on hand grips & A. Addictive Effect:- occurs when two
crutches drugs with similar actions areTaken
together.
MEDICATION ADMINISTRATION B. Synergism (potentiating):-a total effect
of two similar drugs that isgreater than
Drug:-Any substance that when taken in to the sum of the effect if each is taken
living organism may modify one or more of its separately.
function C. Interference: - when one drug interferes
Medication:- A drug that administered for its with the metabolism or elimination of
therapeutic effects. Thus, all medication are second drug resulting in intensification
drugs but all drugs are not medications. of the second drug.
Pharmacology D. Displacement: - Occurs when one drugs
is displaced from a plasma protein
A science which studies the origins, nature, binding site by a second, causing an
and chemistry, effects of drug & how they increased effect of the displaced drug.
exert their effect. E. Antagonism:- a decrease in the effect of
drug caused by the action of one on the
Sub-division of pharmacology other.
2. Personal factors:- age , weight, sex
1. Pharmachoginosis:- deals with the
origin, chemistry and physical property 3. Physiologic factor:- state of Health, acid
of drug with animal and plant base & fluid electrolyte balance, permeability,
service.“Gnosis means knowledge” circulatory capability.
2. Pharmacokinetics:- Effect of the body 4. Psychological consideration:- attitudes
on the drug“Kinetics means movement” and expectations influence Patient response
3. Pharmacodynamics:- the Effect of the (Eg. anxiety candecrees effects of analgesics).
drug on the body 5. Route and time of Administration
4. Pharmachotherapeutic:- positive Effect
of the drug Type of drug preparation
5. Toxicology:- Toxic Effect of the drug on Drugs are available in many forms or
the Body preparations like, pills, powder, and liquid,
inject able, supposition, clean, in halation,
Pharmacokinetic concept ointment. So from in w/c the drug is prepared
A pharmacokinetic process which follows a determines the rout. The most desirable form
given dosageRegimen can be described by of medication from any given pt is determined
“LADME” scheme. by
L: - Exit of drug from dosage (Liberations) The disease process being treated
Age and ability of pt to swallow
A: - Enter to Blood circulation (Absorption) The amount of medication that must
be delivered.
D: Mov’t to the target body tissue
(Distribution) Medication Administration:-A process of
administering a right medication To the right
©: Solomon Tegegne 2012 E.c Page 18
[COMPETENCE BASED PRACTICAL SHORT NOTE FOR NURSING ] April 29, 2020
patient, at the right time, with the right dose 1. Solid preparation tablets, capsule, pills.
bythe right route.
Principle of medication Administration 2. Liquid preparation, suspensions, syrup.
1. While giving medication concentrate Precautions
on the task to avoid error.
2. Never charting the medication before 1. Never give if the solutions are discoloured.
giving it
Contraindications
3. Don’t give a medication prepared by
other. Unconscious pt
4. Medications are not to be left as the Pt who is unable to swallow
bed side table. Nothing per oral pt
5. Don’t give the medication if they have Gastric Irritation
illegible label container. When drugs are inactivated by
gastric juice
Safety precautions
1 Respiratory Administration: - Medication
Check the label container three times.
Introduced in to the deeper Passages of the
respiratory track provides a large surface area
1. When you reach the container
for drug Absorption.
2. Immediately prior to pouring the medication 2Topical administration:- refers to the drugs
applied to the skin and mucous membrane
3. When replace the container too the drawer principally have local effect.
on shelf or discarded 3.Parental Administration:- giving A
medication by a route through injection in to
Right of medication body tissues.
-This involves four major types of Injection
1. Right pt: - that medication is given to the
pt for whom its Intended. 1. Subcutaneous: - Just below the dermis of
2. Right medication:- that the medication the skin
given is the medication that Was ordered
and that is appropriate for the pt. 2. Intradermal: - Just under the Epidermis
3. Right dosage:- that the medication is
given in the dose ordered and That the 3. Intramuscular: -Injection in to muscle body
dose ordered is appropriate for the pt.
4. Intravenous: - Injection in to vein.
4. Right route:- that the medication is given
by the dose ordered and that the ordered
N: B the other types of parental routes used in
route is safe and appropriate for the pt
certain circumstances are as follow
5. Right time:- that the medication is given
with the correct fervency and at the time Intracranial (Intra spinal)
ordered according to agency policy. Intra cordial
6. Right charting or documentation Intra pleural
Intra arterial
Methods of medication Administration Intra articular
1. Oral Administration: - It is the easiest and 1 Intra dermal Medication Administration
the most commonly used in which drugs are
given by mouth and swallowed. A process of Administering medication
between Epidermis and dermis layer of the
Purpose skin by holding the needle 10 -150
to provide a safe effective & economical Purpose
Administration
to provide a sustained drug action with For Diagnostic Ex TAT (0.1 ml)
minimal discomfort For therapeutic Ex BCG (0.05 ml)
Type oral medication Dose to be Administer;-Always the dose
should be maintain B/n 0.01-0.1ml
©: Solomon Tegegne 2012 E.c Page 19
[COMPETENCE BASED PRACTICAL SHORT NOTE FOR NURSING ] April 29, 2020
1. Greatertrochanter
2. Anterior superior iliac crust
3. our hand
Common site N:B place palm of left hand on right greater
trochanter so that the Index finger points
Inner aspects of lower arm
Upper chest toward anterior superior iliac spine; spread
Between scapula. first and middle fingers to form a "V" shape
and injection site is the middle of the "V"
N: B. Do not massages the site after Injection.
Contraindication Dose to be Administer on ventrogluteal
is often B/n 2-3 mL
A know allergic Pt.
HIV Pt for BCG
2 Subcutaneous injection(Sq/sc):- an 3 Dorso-gluteal (DG);-Use the following
administration of medication between anatomical hand mark
dermis and Muscle by holding the Needle
450 or 900 1 angle of scapula
Purpose
2 greater trochanteror
For therapeutic purpose
1Sacro coccygeal Joint
Ex Anti rabies
Insulin
Adrenaline 2 Posterior superior ileaccrust
Dose to be AdministerOften between 0.5- 1ml
N.B draw an Imaginary line from angle of
Common site scapula to the Bottom of Buttock and again
from sacro coccygeal joint to Greater
All Im site
trochanter; then Injection site is outer upper
Around the umbilicus
Quadrant
Beneath of the scapula
Dos to be administer is often B/n 4-5 ml
3 Intramuscular Injection (IM):- an
4 Vistas lateralise – safest site for infant &
introduction of medication deep in to the
children
muscle by holding the needle 900
To Find The Exact site follow the
Common site
following anatomical hand mark
1. DeltoidMsc(D.M)
1 Hip Joint
Use the following anatomical and mark
2knee joint
Acromion process or 1 Acromion process
N:B Injection site is middle third of anterior
Axillary line 2 Our fingers
lateral aspect usual dose is often 2 mL
N:B. Located lateral side of the
Precautions for IM Medications
Humours from three finger width below
the acromion process. 1. Ask the Pt for allergy before administering
2. Assess the injection site, if the site has
Dose to be administer on deltoid is often
scar, infection or abscess change to other
B/n 0.5-1 mL
site.
3. Cheek 3x after inject the needle in to the
2. Ventroglutiale (VG)(safest site for Adult)
Muscle before introducing medication
- use the following Anatomical hand mark
©: Solomon Tegegne 2012 E.c Page 20
[COMPETENCE BASED PRACTICAL SHORT NOTE FOR NURSING ] April 29, 2020
4. Instruct thePt to wait for 20-30mit after 2. Clark’s Rule:- is method of determining
injection medication dosage for children based on
Childs weight in pound. The formula is
N:B some medications are cause for based on the assumption the average
syncope(feinting) adult weight is 150 pound
5. Use "Z" tract motion for obsess and Child dose=weight of child in pound X UAD
pinching Method for those who are tine. 150 pound
Complication of 1M
N:B 1kg =2.2lb or pound
Nerve(vessel) damage (paralysis)
Allergic Rx n ( Anaphylactic) 3. Friends formula:- used for children
Abscess less than 11 months
Tissue damage
Infection and Bleeding Child dose:-Infant age in Month X UAD
N:B. Anaphylaxis:- severe allergic reaction 150
involving cardio vascular and respiratory
N:B. used for those age is B/n 0-11 month
systems; may be life-threatening.
IM Procedure
Common drugs
1 Cheek the physician Order and wash your
Procaine penicillin fortified(PPF) hand
4,000,000 IU diluted with 10mL
Benzantin Penicillin(BP) 2 Explain the procedure to the Pt.
2,400,000 IU diluted with 8 mL
1.200,000 IU diluted with 4mL 3 Assess the site of injection
N:B PPF& BP are A group of natural 4 Collect all necessary equipment
penicillin that against gram +vebacteria
particularly staphylococci & streptococci and 5 Monitor vital sign (Esp. Blood Pressure)
from gram-ve they are effective against
6 Prepare medications
meningococcal infection.
7 Wear disposable glove and positioning the
PPF and BP can Not resist acids
Pt.
Gentamicin =>80 mg/2mL
diclofenac =>75mg/3mL 8 Administer medication
Ceftriaxone=>1gm/10mL
N: B first cleans with alcohols swab second
Common Drug formula infect the Needle by using
:- desired dose (D) x Quantity (Q) "Z" track or pinching methods then check 3x
Dose on hand (H) before administering
Eg .Administer 2,000,000 IU of PPF
if the blood is return to the medication
A = 2,000,000 x 10 20/4= 5mL
4,000,000 immediately dustcart and prepare other
Paediatric Calculation
9 Instruct the Pt to wait 20-30min if the talk
1. Young’s rule:- method of determining
dosage for children Based on age of child penicillin
in year
10 Document about medication type, amount,
Child dose=age of child in year x UAD route of administration, time of
administration and Pt response
Age of child +12 11 Provide comfort
N:B. Used for children those age B/n 1-12yers
©: Solomon Tegegne 2012 E.c Page 21
[COMPETENCE BASED PRACTICAL SHORT NOTE FOR NURSING ] April 29, 2020
Up – Back ward for Adult
Down-Back word for Infant
Medication form
Eye Medication Administration
Used drop form only
Defn:- an installation of medication in to the
Eye Precaution
Purpose 1. at least wait for 2-3 mint to Administer
medication to the left side after
To lubricate the eye socket administering in Right side of the ear.
To prevent infection 2. the medication should be warmed
To dilate the pupil before administering in to the Ear
Precautions
DIABETES MALLITUS
Use each medication for each Pt. Definition: a metabolic disorder characterized
Before administer discard the first drop by an elevation of blood glucose level above the
normal range (>120 mg/dl) and result from
Form of eye medication defective insulin production, secretion and
utilization.
A. Ointment
B. Drop Coues:-
Common word on Eye Medications Idiopathic (Unknown)
OD = Right Eye RISK RACTORS:-
OS:- Left Eye
OU:- both Eye Genetics
hs:- at bed time Obesity
Od:- every each other day Age
Gt:- One drop Some diseases
Gtt:- two drop
TYPES OF DIABETUS MALITUS
Position of Pt
Generally diabetes mellitus can be divided
sitting(up Right) with full Extension of
based on the severity of the disease progress
head and neck
and the cause of the disease. The main
lying position with head full extension
common types are
Method of Administration
1 TYPE 1 (Insulin dependent diabetes
Ψ Make cup form for drop mellitus)
Ψ Make retract form for Ointment 2 TYPE2(Non-insulindependent diabetes
mellitus)
3 Gestational diabetes mellitus
4 Diabetes associated with others
Installation of Ear Medication
TYPE 1 (JUVENILE DM/IDDM)
Definition ;-An administering of medication in It most commonly occur at the age of
to the ear juvenile (child hood) or early adult hood
(<30 yrs)
Purpose - to soften the wax Most probably they are tine
- To treat infections They need insulin to survive
-to relief pain& local swelling They have no good response for oral
Contraindication hypoglycaemic agent
Rupture of Tympanic membrane
ETIOLOGY
Ear Position for assessment
©: Solomon Tegegne 2012 E.c Page 22
[COMPETENCE BASED PRACTICAL SHORT NOTE FOR NURSING ] April 29, 2020
With idiopathic reasons the destructions Increase glucose production due to
of beta cell abnormal glucose production
RISK FACTORES N: B diabetic ketoacidosis does not typically
occur in type 2 DM
Molecular mimicry
Autoimmune system 3. Gestational DM: - it occur in the pregnant
Congenital loss of beta cell women and it may be disappear after delivery
1. What does it mean molecular mimicry? 4. Diabetic mellitus associated with other
The trigger agent which is called Ψ Drug: - corticosteroids
coxsackie virus and the enzyme
Which is found in the beta cell - Thiazide
which is called Glutamic
AcidDecarboxylase have the same - Oestrogens
chemical structure.
- Phenytoin
When the trigger agent get in to the
body and cause for infection, the
Ψ Disease: -pancritis
immune systems detect the
antigens and the beta cells - Cushing’s syndrome
together.
Then immune systems will destruct - Huntington’s chorea
the virus and the beta cells and
remove out from the body through -Acromegaly
west removal mechanism. Then
step by step the insulin production Diagnosis
goes down.
1 FASTING BLOODS GLUCOSE LEVEL
2. Auto immune system destructions- Its TESTE (FBGLT)
occurs when the immune system recognise
First keep the patient nothing per oral for 8
their own cell as Antigen mistakenly and start
hrs and monitor his/her blood glucose level.
to destroy then remove from the body.
If it is between 70 –110 mg/dl its normal.
3. Congenital loss of beta cell - When the
child born without beta cell due to congenital 2 RANDOME BLOOD GLUCOSE LEVEL
Abnormality he/she has a chance to develop TESTE (RBGLT)
diabetes mellitus.
Monitor the patient’s blood glucose level
2Adult onset (type 2/non-insulin randomly and
dependentDM)
if the patient score between 160 – 200
It occur late in adult hood (>40 yrs) mg/dl it’s normal.
They are most probably obese
They have good response for oral 3 ORAL GLUCOSE TORELANCE TEST (OGTT)
hypoglycaemic agent
The no need insulin to survive Give 75mg of glucose tab per oral and instruct
the patient to wheat for 30mit and Monitor
Cause blood glucose level.
a.Insulin resistance;-Decrease tissue if the result below 200 mg/dl its normal.
responsiveness for insulin as result of
post receptor defect CLINICAL MANIFEATATION
b. .impaired insulin action
Decrease glucose utilization:- over 1 CARDINAL SIGN
production of insulin in early phase, but
Polyuria
eventually decrease secretion of the
insulin from beta cell. Polyphagia
Polydipsia
©: Solomon Tegegne 2012 E.c Page 23
[COMPETENCE BASED PRACTICAL SHORT NOTE FOR NURSING ] April 29, 2020
It’s the corner stone of diabetes
management
2. Visual deficits:-
4 PHARMACHOLOGICAL MANEGEMENTES
3. Weaknesses:-
Two type of glucose lowering agent used in the
4. Weight losses treatment of DM,theye are insulin and oral
hypoglycaemic agent
5. Dryness of the skin:-
Insulin
6. Delayed wound healing process
1. Short (fast) acting insulin:- it cover
7. Abdominal pain only 4 – 6hr ex Regular insulin
2. Inter mediate acting insulin:- it cover
8. Tingling and numbness sensation
12 – 16hr ex Lent insulin
MANAGEMENTES 3. Long acting insulin:- it cover 24hrs ex
ultra-lent insulin
GOAL
Oral hypoglycaemic agent
To equalised the blood glucose level.
To prevent the acute complications OHGAs increase sensitivity to receptors on
To the improvements of overall health sensitive tissue. They also reduce hepatic
through optimal nutrition. glucose production.
To prevent or delay the chronic
Ex sulfonylurea’s like
complication
Ψ tolbuzamide (orinase)
COMPONENTES OF DLABETES
Ψ Acetohexamide (dymelor)
MALLITUS MANAGEMENTE
Ψ tolazamide (tolinase)
1 NUTRITIONAL MANAGEMENTE Ψ Chloropropamide (diabinese)
5 EDUCATIONAL MANEGEMENTE
Principles of nutritional management
Teach the patient about
1. The patient should have to know which food
is recommended and restricted. 1. Self-care:- bathing, foot and Neal care
2. Self-infection:- teach the pt how to inject
2. Eat according to the prescribe meal plan. insulin
N:B commonly insulin given through
Increase the frequency of meal per a day subcutaneously on upper arm, around the
(5-6 time pre a day)
umbilicus, on vests lateralise muscle, beneath
3. Never skip meals particularly for the pt who of the scapula.
take insulin and OHGA
3. Dagger sign of DM:- like blurred vision,
4. Learn to recognise appropriate food portion. palpitation, tingling and numbness
sensation, headache, delayed wound
2EXERCISE MANEGEMENTE 4. The problems relate with insulin therapy:-
insulin allergy, tissue lipodistrophy,
Regular scheduled exercise to promote the smoggy effect and down phenomenon.
utilization of carbohydrate, assist with weight
control, enhance the action of insulin and COMPLICATION
improve the cardio vascular fitness.
Acute complications
N;BAdvice the pt to perform aerobic exercises
for 20 – 30mit 2- 3 times within a week and 1 hypoglycaemia:- decrease blood glucose
avoid strenuous type of exercise level below the normal range (<60mg/dI)
2 BLOOD GLUCOSE MONITORING Coues
Loss of meals
©: Solomon Tegegne 2012 E.c Page 24
[COMPETENCE BASED PRACTICAL SHORT NOTE FOR NURSING ] April 29, 2020
Insulin over dose Perform correct hand washing technique
strenuous exercise Perform correct procedures in bed bathing
Occupied Bed making
Clinical manifestation Perennial care
Perform the for stroke in back massage
Cold and sweat skin Wound care
Palpitations Teaching about Diet. Medication Injection
Blurred vision Inform complication. Danger sing and
Starvation precautions
Headache
Termer Procedure
Confusion
1. Wash your hand and explain the
Management procedure to the pt why, How & when it is
done.
40% of glucose through IV 2. Collect all necessary Equ’t step wisely
Glucagon 1 mg sc if the ptcannot 3. Take necessary vital sign that used for the
ingest a sugar treatment procedure
Encourage the pt to carry a portable 4. Ask the pt that she need to be use the bed
treatment at all time. pan.
2Diabetic ketoacidosisthe acute HAIR CARE
complication of DM characterised by
hyperglycaemia, ketoneuria, dehydration. 5. Prepare the solution and measure the
(BGL is between 300 – 1000 mg/dI) temperature of water
6. Make the pt position diagonally (move the
Cause pt’s head to the Edge of the Bed)
7. Place pillow under the shoulder so that the
Sever deficiency of insulin
head is slightlyTilted backwards. (Make
Clinical manifestation sure that the pillow cover with
mackintosh)
Fatigue 8. Put towel under the neck
Malaise 9. Make through with rubber sheet or use a
Drowsiness Kelly’s pad to allow dirty water to flow in to
Abdominal pain the bucket.
Kussmaul respiration 10. Plug the Ear with cotton Ball & place the
Hypotension wash towel over the Eye.
Week pulse 11. Start cleaning first rinse than rub with
Acetous breath (fruity) shampoo and massaging the scalp well.
Stupor and coma 12. Remove shampoo with clean water then
squeeze off water from the hair and dry
Management 13. Remove the cotton ball from the Ear and
wash towel from the Eye.
IV fluids and electrolyte replacement to 14. Cover the hair with towel which hasbeen
treat dehydration put under the Neck.
Remove all used materials and comfort the
IV insulin drip 15.
pt properly.
Chronic complications
“BED BATH”
Retinopathy
16. Prepare the solution and measure the
Neuropathy
temperature of water
Nephropathy
17. Remove the pt’s cloth if she wear then
Project ;- Provide a Nursing care for a change the top sheet with bath blanket
female Diabetes mellitus patient who is bed step wisely.
Ridden and has wound on her right toe 18. Start washing from the Eye
Main task
©: Solomon Tegegne 2012 E.c Page 25
[COMPETENCE BASED PRACTICAL SHORT NOTE FOR NURSING ] April 29, 2020
N:B wash pt.’s Eyes using separate corners of 2. Petri sage:- grasping tissue B/n
the bath mitt for each Eye and wipe from inner your tumb and fingers then knead
canthus to outer canthus. upward from buttock to shoulder.
3. Appointment:- tapping mov’t from
19. Wash, Rinse and dry pt’s face, Nose, Ear buttock to shoulder with medial
then neck. Aspects of hands.
20. Wash hand and Arms, Rinse, Apply soap,
wash and dry by using long stocks from BED MAKING
distal to proximal Area.
29. Make an occupied bed or change the
N:B use mackintosh to prevent bed from bottom sheet then put the pt dorsal position.
soiling.
Focus:- Don’t mess Bed making principles.
21. Change the water
22. Rinse apply soap wash then dry chest and Perennial care
abdomen with giving a special attention to
skin ford under breast (Esp. females) 30 positioning the patient (dorsal recumbent
23. Rinse, apply soapand wash then dry legs with knee flex and spread legs apart)
by using long stocks from distal to
31 place water proof pad under the site
proximal.
32 open sterile field and prepare the solutions
N:B - use mackintosh to prevent Bed from
that used for cleansing
soiling
33 wear surgical glove and place
- do not wash the dressing site to prevent
fenestratedtowel over the area
infection.
34 separate the labia with sterile gauze and
24. Change the water
start cleansing from distal labia (3x) proximal
25. Turn the pt to side lying position and
labia (3x) then Centre (3x)
exposed back area.
26. Rinse, Apply soap, wash & dry by using
35 dry with the same sequence
long firm stroke from shoulder to buttocks.
N:B start from the upper portion of back. 36 remove all used equipment then make
comfort
BACK RUB
N:B do not use the cotton ball in order to
27. Remove the glove and Assess the skin clean the site
condition then make decision to be used either
powder or lotion Wound care
N:B do not use lotion on moist and wet skin in 37 place mackintosh under the wound site
order to prevent skin maceration.
38 open sterile filed the prepare the solution
Powder for moist skin&Lotion for dry skin
39 wear surgical glove and put fenestratedtowel over
28. Apply massaging starting with Effleurage, the wound site
friction Rub, petricege then tappointment.
40 remove old dressing andmeasure the depth of the
N:B 1. Effleurage:- by using a palm of your wound to determine how to clean
hands strokeupward from the buttock to
shoulder. 41 take a specimen sample for lab investigation
Do not take the Hand-off from the pt back 42 start cleansing
until the procedure ends.
1. Friction Rub:- by using a tumb Ψ If the wound is superficial clean the
finger make a motion to clockwise site as usual with hydrogen per oxide
direction from buttock to shoulder. Ψ If the wound is deep use hydrogen per
oxide with pressure
43 dry and dress the wound site
©: Solomon Tegegne 2012 E.c Page 26
[COMPETENCE BASED PRACTICAL SHORT NOTE FOR NURSING ] April 29, 2020
N;B do note adhere the plaster on the skin part Over dry wound Indicate Dehydration
Wound with swollen Edge suggest
44 remove all used equipment and make a comforts. cellulites’
Wound with powder suggest fungal
infection
Providing Burn care N:BHealthy granulation tissue appears clean
pinkish faintly shiny and free of exudates.
Burn: - An injury of skin and its underlying
Complication
tissue result from heat, chemical, radiation
and electrics.
Infection
Shock
Type of Burn
Scar formation
Burn can be categorized based on its cause, Burn Management
Extent and Depth
General Goal of Burn Management
Based on cause To maintain physiologic stability
To restore skin Integrity
Heat Burn To prevent Infection
Chemical Burn To promote psychological Health
Radiation Burn
Based On Electrical Burn Components of Burn Management
Based on extent 1. Provide fluid Resastation
First degree burn Commonly 2nd& 3rd degree Burns are need
Second degree burn fluid Resastation In order to equalize body
Third degree burn fluid and electrolyte.
Based on depth N: B to provide adequate fluid follow rule of
nine (9) then calculate totalbodysurface area
Superficial Burn by using park and/ or consciences formula
Deep Burn
Rule of Nine
N:B Burn is the most common cause for
Hemodynamic compromise, smoke in halation, Head and Neck................. 9%
Multi organ damage and laterally scar Upper front Trunk............ 9%
formation. Lower front Trunk............ 9%
Upper Back Trunk............ 9%
Lower Back trunk............. 9%
Clinical Manifestation
Upper Right Leg................ 9%
Burning pain Lower right Leg................. 9%
Blister formation Upper Left Leg.................. 9%
Red Melted Appearance Lower Left Leg.................. 9%
es PR and Respiratory rate Right Hand...................... 9%
Unconsciousness Left Hand......................... 9%
Sweating Genitalia.......................... 1%
Discolouration of skin
100%
Shock (Hypovolemic
&Anaphylactic) Consciences Formula
Hypothermia
Sign of Dehydration 2mL or 4mL X TBSA X wt(kg)/24hr
Nursing Consideration 2ml for <50% burned area
4ml for > 50% burned area
Assess the wound site
If purulent wound & green grey exudates Park Land:-
present on the site of Burn Indicate
Infection 4ml X TBSA X wt (kg) /24hr
©: Solomon Tegegne 2012 E.c Page 27
[COMPETENCE BASED PRACTICAL SHORT NOTE FOR NURSING ] April 29, 2020
N: B. Greater than 20% Burned area need In order to promote the wound healing
fluid resastation for 2nd degree Burn &< 20% process advice the Pt to take proteins,
Burned area also need fluid resastation in case vitamin
of 3rd degree Burn. N: B it should be started the day after
surgery
The most common and preferable fluid is To provide nutrition follow the following
ranger lactate and adequate resastation formula
measured by clinical parameters like
Urineout Put& Blood pleasure. ( Urine out 25 kcal/kg + 40kcaL/total Burned surface area
Put should be between 30-50mL /hr)
Give Total fluid Volume within 24 hr by Procedure
using drop Rate formula
1. collect all necessary Equipment
Total fluid Volume X Drop factor 2. assess the wound site
Total time taken X 60mit 3. check vital sign
4. secure IV line
5. remove close from the wound site
2 wound care 6. offer draw sheet and rubber sheet then
open sterile filled
-It has three steps 7. wear surgical glove
8. clean the wound site with wet gauze then
A. cleaning the wound site-while cleaning the
dry
wound do not use cotton Ball.
9. prepare medication and apply over the
B. ProvideMedications wound
10. 10. Dress by roller bandage
- A, Broad spectrum Antibiotics (BSA) 11. Give TAT
- B, decicants:- to substitute the function of
Blister
Providing Antenatal
N:B.Silver sulfadiazine, mafinied acetate,
Nitroforatone is the best decicants that used to care (ANC)
substitute the function of blister but among
those silver sulfadiazine is most preferable and Definition:- a care given during pregnancy or
popularly used. before delivery
C. Provide Dressing Purpose
To promote physical and mental
Rule of dressing
health of mother
1. Dressing should be applied from distal to To prepare women for labour,
paroxysmal lactation & subsequent car of baby
To identify actual and potential
2. Dressing should be over lap problem of mother&foetus in order
to take action
3. Start dressing by letting 2.5cm above the To provide TT immunization
wound site
ANC Visit
3. Provide Anti pain
1. First visit at 16wks
- Before 20 mints of starting the care you 2. Second visit B/n 24-28 wks.
should administer Anti pain 3. Third visit at 32wks
4. Fourth visit B/n 36-38wks
4. Proved tetanus anti toxoid (TAT)
Components of ANC
- To prevent tetanus toxoid give 3000 IV I’m
1. Risk assessment
5. Provide Nutrition 2. Health promotion
3. Care provision
©: Solomon Tegegne 2012 E.c Page 28
[COMPETENCE BASED PRACTICAL SHORT NOTE FOR NURSING ] April 29, 2020
1. Risk Assessment:- It help to Identify all ΨSevere Headache
risks and problems involving the mother ΨFever
and foetus. ΨEpigastria pain or abdominal
Risk assessment also have sub- pain
component Ψ Blurred vision
A. History taking Ψ Absence or Reduction of fatal
B. Physical examination Movement
C. Lab investigation Ψ Profuse vaginal discharge
Ψ Persist ant vomiting
A. History taking Minor problem during pregnancy
1. Biographic data Heart burn
Nausea & vomiting
Name ,age, sex, religion, Occupation, Address 4. Past Obstetric History
2. Elaboration of chief complain ;- It helps Ask mother about History of previous
to identify what the mother’s brought to pregnancy
Hospital
3. History of present pregnancy A. Length of gestation
B. Onset of Labour Spontaneous or induced
Ask Mother about C. Mode of delivery
Spontaneous vaginal delivery
Gravidity Forceps or vacuum delivery
Destructive delivery
-Abortion Caesarean section
-stillbirth
D.foetalout come
-parity
-Number of children alive Alive
-Last manenustrational period Dead
Sex
-Gestational age (GA) Weight
-Expected date of delivery (EDD) malformation
N.B. To fined gestational age use the following E Medical Hx related to previous pregnancy
formula
GA= VD-LNMP Gestational diabetes Mellitus
7 DAY Hypertension (pre-Eclampsia&eclmpsia)
To fined expected date of delivery follow Anaemia
the following formula Antepartum Haemorrhage
A. Naegale’s Rule 5. Gynaecological History
NLMP – 3Month + 7 days Ask Mother About
B. Ethiopian Calendars A. Family planning
Type
Ψ NLMP + 9 month + 10 days if not
passedpagume Duration
Ψ NLMP + 9month + 5 days of Side effect
passedpagume
B sexual history
Condition of pregnancy
Planed Risk for STI and HIV/AIDS
Unplanned
Supported C gynaecological operation
unsupported
Female genital mutilation(FGM)
Manual vacuum aspiration(MVA)
Ask mother-about danger sign of
Evacuation and curettage(E&C)
pregnancy
Ψ Vaginal Bleeding
©: Solomon Tegegne 2012 E.c Page 29
[COMPETENCE BASED PRACTICAL SHORT NOTE FOR NURSING ] April 29, 2020
D Menstrual history second trimester due to Hormonal
vasodilatation Effect
Age of menarche
Menstrual cycle N:B. Maternal position defect readings,
Amount( always between 10- Brachial BP is Highest when the
80ml) women is sitting, lowest when she is
Colour (dark red ) lying in lateral Recumbent position,
6 past medical and surgical history and intermediate when she is supine.
There-fore the same maternal position
A medical Hx and the same arm are used at each
visit.
diabetes mellitus
hypertension Respiratory Rate:- Increase Maternal
congestive heart failure Respiration Rate about 2-4 Bpm
Weight and Height ;-It helps to identify
B surgical Hx high Risk mother
3. HEENT
caesarean section
Emphasis on –
laparotomy and other
head and hair condition
7 personal, social and family history
Abscess on the Head
HABITIS
Conductivities
Smoking
Palecolour
Alcoholism
Infection of Ear
Drug abused
Hearing ability (Bone &air
Others
conduction)
OCCUPATION
Breathing pattern
EDUCATIONAL STATUSS
Polyps in the Nostril
FAMILLIY HISTOR
Mouth condition
Diabetes mellitus
Tonsillitis
Hypertension
4. Lympho-glandular system;-Examining
Twines pregnancy
Breast and Thyroid gland
other
Ψ Thyroid gland assessment
Inspection – If the Goitre is visible
B Physical Examination
Inspection and palpation:- if the Goitre is
Invisible
a process of Examining Mother’s Body
Physically
N:B Give something to swallow or instruct to
swallow her own saliva In order to visualised
Methods of P/E on pregnant mother
invisible goitre.
1. Inspection
2. Palpation Ψ Breast Assessment
3. Auscultation Inspection
Size of Breast
1. General Appearance Colour
Well looking Areola part
Sick looking Nipple(Inversion, cracking)
2. Monitoring Vital Sign
Palpation
During pregnancy the Mother vital sign have
Methods 1. Circular Motion palpation
slightly difference from X lone pregnant
Mother 2. Stroke (divisional) palpation
Body temperature
5 Abdominal examinations
Pulse Rate:- increased by 10-15 bpm
Blood pressure:- Mothers blood pressure
equal when she is at first and third Inspection;- assesse for 4s’
trimester and decreased by 5-10mmHg at
Skin;- linenigra, streagravidrum
©: Solomon Tegegne 2012 E.c Page 30
[COMPETENCE BASED PRACTICAL SHORT NOTE FOR NURSING ] April 29, 2020
Scar;- c/s N;B use one hand to grasp the lower portion of
Shape ;- oval or round abdomen
Size;- Huge or bulky
4 pelvic palpation (4th leopard manoeuvre)
N;B oval abdominal shape indicate
primigravida and round abdominal shape purpose
indicate multigravida
used to measure the extent of
decent
Palpation;- to determine the presenting part on
the pelvic
1 Fundal palpation (1st leopard manoeuvre)
N;B if the presenting part hard and round the
Purpose find out will be occiputo prominence or
sinciputal prominence.
Used to determine what parts of
the foetus occupy on the fundus 6 Genito urinary system
Used to measure gestational age
7 Extremity
and fundal height
Check for oedema
Pathological oedema
N;B to measured GA follow the following
Physiological oedema
measures
Tape measuring technique C LABORATORY EXAMIATION
Finger measuring technique
To identify normal with abnormal and
1finger above umbilicus = 2wks treat abnormal tings accordingly
Blood
1finger bellow umbilicus = 1 wk VDRL
RH factor
2 lateral palpation (2nd leopard manoeuvre) Stool
Urine for infection and protein
Purpose
Haematocrits (HCT)
to determine foetal lie Haemoglobin(Hgb)
PIHCT(personal initiative
Eg oblique humane counselling test)
3 HEALTH PROMOTIONS
Longitudinal
Related with nutritional and educational
therapy
Transfers
Educate mother about
to determine the foetus side Life style modification
Eg anterior or posterior Pregnancy condition
to monitor foetal heart rate Activities
SITE OF AUSCULTATION Health and nutrition education during
pregnancy
Cephalic presentation below umbilicus
Breech presentation above umbilicus Coarse of pregnancy
Oblique presentation on flank region Bleeding
Labour sign
3 paw licks grip (3rd leopard manoeuvre) Fever
Diet and nitration
Purpose Substance abuse and drug
Traditional belief and practice
Used to determine the presenting Preparation for deliver and BF
parte and its mobility
Used to assess the engagement
4 Care provision
A minimum care that should be provide at
each visits are
©: Solomon Tegegne 2012 E.c Page 31
[COMPETENCE BASED PRACTICAL SHORT NOTE FOR NURSING ] April 29, 2020
Provide treatment for problem and Brest feeding
complaints Way to reduce risk of MTCT
Arrange for support if no social support 1. Safe delivery practice
2. Counselling the mother about HIV and
nitration
3. Antiretroviral based on viral load
Preventing HIV transmission from HIV (prophylaxis of RX)
infected women to their infant 4. Infant feeding counselling for safe feeding
Objective: to identify HIV infected pregnant practice
women and to provide effective intervention to
reduce General information about the risk and benefit
of infant feeding option
MTCT
1. Mother to child transmission of HI/v 1 Exclusive Brest feeding by HIV positive
infection. (MTCT) women
MTCT...... vertical or prenatal
2 Exclusive Brest feeding by HIV negative
transmission
MTCT of HIV can occur during mother,
Pregnancy and labour 3 Expressing and heating Brest milk of
Child birth and Brest HIV positive women (20-30 mint at 54-
feeding
56oc)
Risk factor for HIV transmission
Maternal viral lode 4 Replacement feeding
Sexually transmitted infection
E.g. commercial or home-made formula
Maternal malnutrition
Maternal other d/se If the mother decides to BF then
exclusive BF should encouraged,
infectionE.g. malaria placenta
followed by early weans 4-6 month
infection If the mother decide not BF
Duration of Brest feeding educate replace (formula) feeding
Early mixed feeding Mixed feeding (BF + formula)
discouraged.
Rupture of membrane more
than 4 hour Nursing process
Specific intervention to reduce HIV
transmission from mother to child 1 ASSESSMENTE
Antiretroviral prophylaxis and
Objective and subjective data
treatment
Safe delivery practice 2 DIAGNOSIS
Anxiety related to poor understanding of
Safe infant feeding practice
HIV /AIDS and it is the mood of
Safe sex practice during transmission from mother to child as
pregnancy evidenced by verbal expression
Risk to infection related to decrease
How these intervention works
immunity
1. Reduce maternal viral lode
Altered nutrition less than body
2. Reduce infant exposure to the requirement related it nausea and
virus during vomiting
Pregnancy Fatigue related to physiologic change of
pregnancy
Labour 3 PLANING
Delivery To decreaseanxiety
To increase immunity
©: Solomon Tegegne 2012 E.c Page 32
[COMPETENCE BASED PRACTICAL SHORT NOTE FOR NURSING ] April 29, 2020
To provide sufficient knowledge A. Positioning the New Born (Neonate, Baby
about the disease process on its Back with the Head looking straight
up . this will usually provide for good air
flow
B. Provide suctioning first from Orophanex
then from Nasopharnex with suction Bulb
or syringe
4 IMPLIMENTATION
C. Keep the neonate warm to Avoid Hypoxia
Provide teaching about the Because of increase O2 demand
transmission of HIV/AIDS during D. If the neonate is in distress Oxygen
prenatal ,intranatal and postnatal therapy with tight fitting mark can be
Providing a initiated.
Advice or council about nutrition 3. Give Eye prophylaxis ;-Administering
supplement prophylactic antibiotic ointment like,1%
Educate about the pregnancy Tetracycline, 0.5%Erytromicin and 1%
Educate the mother for infant safe silvernitrate Ointment within one hrs after
breast feeding practice with full Birth in order to
option preventeoptalmianeonatrum.
4. Provide Vitamin K (A quamephyton)
5 EVALUATIONS
In order to initiate clotting factor and to
GOAL IS MEETED control vitamin K deficiency Bleeding.
It
New Born Care can be given through oral or
Intramuscular, How Ever the Expert
Agree that giving Vitk by injection is
Definition;-Care given for A new Born baby is the most effective and Efficient way
called new Born Care of protecting Babies from VKDB
Aim /Goal/ Dose
to maintain and stabilizing body Through Oral delivery, vitK has its own
temperature of New-born regimen. It the first Wks of Baby’s life two dose
are given. And another dose when the body get
to maintain and support Respiration one month old.
to Identify Actual and potential
problem that may require immediate That mean 2mg at birth followed by
a second 2mg oral dos B/n day 2 &
action
7 and the rest 2mg after one month.
Task under New Born Care INTRA MESCULAR VITAMIN K DOSE
1. immediately after delivery the baby should During the first few hours following
cover properly& keep dry delivery A single injection of 0.5 to1.0mg of
2. Maintaining respiration: - respiration Natural vit K can Help prevent VKDB.
must be maintained at Birth for this the N:B first Milk(colostrum) are Rich in Vit K
child must begin cry lustily periodically.
5 Provide Cord care
Failure to cry may be due to several
causes. The most common cause is air Ǽ Keep the cord stump clean and Dry
way obstruction By mucous Ǽ After delivery the cord has to be tied or
If the child Not spontaneously clamp to preventBleeding that clamped
Begin Breathing due to different cord develop dry gangrene and fail off with
condition follow the following in 5 to 10 days and the Base Heals with in
step few weeks.
©: Solomon Tegegne 2012 E.c Page 33
[COMPETENCE BASED PRACTICAL SHORT NOTE FOR NURSING ] April 29, 2020
6 Provide polio and BCG Vaccine
Polio vaccine to prevent poliomalitis
Score
(2 drop per Oral)
BCG vaccine to prevent Tuberculosis <3 Asphyxia
(0.05mL ID RUA) 4-6 Moderate
7-10 Normality
7 Measure Head and chest Circumference
Breast feeding
- The average head circumference of term
baby is around 35 cm and greater than A process of feeding Breast Milk After delivery
from chest circumference at Birth in order to provide Immunological, nutritional
- Chest circumference is less than the Head and psychosocial advantage
by two cm at Birth
- Average term baby weight is b/n 2.5-4kg Purpose
and length is 50 cm
For normal growth and development of
Infant
APGAR score Enhance bonding and attachment
Help to develop child Immunity
It is A quantitative method of assessing the
New Born condition.
Have contraceptive Benefit
To prevent cancer
APGAR test usually given to a baby twice,
Ǽ
Help to Return Mother’s uterus to its
once at 1 minute after Birth and again at 5
Normal size and shape
minutes after Birth sometimes if there are
concerns about the baby’s condition or the
Stages of Breast Milk
score at 5 minutes is low. The test may be
1. Colostrum:- first Milk of Mother and very
scored for a third time at 10 minutes after
concentrated and high in protein, uniquely
Birth.
suited to providing Nutrition during this
transition to life outside the womb.
APGAR Refers to as an Acronymfor :-
A:- Appearance (skin coloration) Type
P:- Pulse (Heart Rate)
A. Early colostrum:-hard, shiny and Ranges
G:- Grimace (Reflex Irritability )
in colour from very pale to bright yellow.
A:- Activity (MSc tone)
R:- Respiration(Breathing Rate & Effort) B. Late colostrum:- similar to early colostrum
has a thin Translucent outer Ring
Five factors are used to evaluate the baby’s
condition and each factor is scored on a scale 2 Transitional Milk:- It Replace colostrum
of) to 2, with2being the best score. and lasts Until about a Wks of post-partum
APGAR Scoring Type – Early transitional milk
-late transitional Milk
3. Mature Milk:- three rings, but it is hard to
see the canter ring which is almost the same
Activity 0 1 2 colour as the middle ring.
Appearance All Trunk pink All over
over pale Extremity pink Positioning during Breast Milk
pale
1. Foot Ball
Pulse Absent <100 >100
2. Cradling
Grimace Absent Grimace Sneezing 3. Lying down(side lying)
cough
Activity Flaccid(flopp Some Active Body
y) flexion mov’t
Respiration Absent Weak cry Good Cry
©: Solomon Tegegne 2012 E.c Page 34
[COMPETENCE BASED PRACTICAL SHORT NOTE FOR NURSING ] April 29, 2020
1 Football Holding 4. Low Client teaching during Breast
feeding
1. Hold the baby’s back and
shoulders in the palm of your Client teaching during Breast feeding
hand
2. Tuck the baby up under your arm, 1. Properly wash the Hand and Nipple
keeping the baby’s Ear, shoulder with warm water
and hip in straight line 2. Placing finger in corner of Baby mouth
3. Support the breast. Once the In order
baby’s mouth is open wide, pull 3. Burp baby after feeding
the baby quickly to you 4. Your New born is feeding about eight
4. Continue to hold your Breast until times in 24 hrs for 30-40 minutes at
the baby feeds easily each feeding.
5. You feel a tug, but not pain, when the
2 CRADLLING baby sucks.
1. Cradle the baby in the arm closest
Procedure for New Born Care
to the breast, with the baby’s
Head in the crook of your arm 1 Assemble all necessary equipment for this
2. Have your baby’s body facing you, procedure
2 Prepare the solution and wear personal
tummy to tummy
protective
3. Use your opposite hand to support
3 Put on surgical glove and take sterile towel
the Breast
then be ready to receive the child from the
3 Lying down (side lying) midwife.
4 After receiving the child cover immediately
1. Lie on your side with pillow at your
and dry
back, and lay the baby so you are
N:B. Do not exposed the new born’s head
facing each other.
to prevent excessive heat loss
2. To start, prop you self-up on your
5 Put the child on flat position and often the
elbow and support your breast with
suction equipment to the working place
that hand
then start suctioning
3. Pull the baby close to your, lining up
the baby mouth with your nipple. N:B. Suctioning should be starts from Oral
4. Once the baby is feeling well, lie back and then from Nasal
down
6 Clean the Eye by using socked cotton Ball
N:B Hold your breast with the opposite
in Normal saline
hand
N:B. Cleaning should be from Inner cantus to
Sign of good a attachment
outer cantus
1. Wide opened mouth of the baby
2. Chine of the Baby touché the Mother 7 Retract the eye lied and apply TTC
Breast Ointment in order to prevent Neonatal
3. More a record is visible above the Optima
baby’s mouth than below 8 Clean the injection site for vitamin "K" by
using N/S solution and give the injection
©: Solomon Tegegne 2012 E.c Page 35
[COMPETENCE BASED PRACTICAL SHORT NOTE FOR NURSING ] April 29, 2020
in to the proper site (V/L) with Holding the 22 give the child for the mother and give
syringe 900 advice about breast feeding, cord care
9 Check the New Barn’s plus Rate on the
,hygienic care.
Apical Area.
N.B. Do not forget counting the APGGR HOW TO APPLY CPR FOR THE NEW BORN
score B/n the procedure
Put the child in flat position insert small
10 Change the used towel then remove old
towel or pillow under the neck
glove and put on the New
11 Exposed the cord area and Hold up the Apply suctioning from the mouth then
cord by using Non dominate Hand
from the nose
12 Start cleaning from Bottom to top
including the Base Check the Breathing system by using LLF
protocolor apgar score.
N.B. first start cleaning by Alcohol and
following by Betadin solution If there is no breathing, Give One Rescue
13 Apply “V” shaped gauze Over the cored Breath and check the pulse on the apical
Area site. Then if it is weak or absent give
three compressions
14 Measure the cored and clamp then tie
N:BCPR should be given for 5 cycle
N.B. clamp the cord two fingers from the
Base and two fingersfrom the first clamper
then Cut above 2cm of the second clamper. After five cycle check the breathing
and circulatory system. If the child’s
If the cord tie is long, make it short after recovered then goes to the Next step
tied
as usual.
15 Squeeze the tip of cord by Gauze and
remove the clamper
Performing A cardiopulmonary
16 Clean the cord from top to Bottom Resuscitation (CPR)
Defn:- A process of stimulating the heart by
N:Bfirst by Betadine then by Alcohol
External chest compression and lung by
artificial ventilation(Respiration)
17 Remove the old "V "shaped gauze and
Replace by New Purpose
18 Apply abdominal Binder to cover the cord -to restore circulation and respiration
site Indication
Respiratory arrest
N:B do not attached the abdominal binder ton Cardiac arrest
the body by plaster instead, attached the ABCD Protocols
A:- air way
plaster gauze to gauze
B:- Breathing
C:- circulation
19 give polio vaccine D :_ definitive therapy
20 give BCG vaccine
Air way Opening technique
1. Head tilt chine lift Maneuverer
N:B do not rube the site after injecting 2. Jaw trust maneuverer (for spinal &
Neck injury)
21 take the anthropometric measurement
Breathing and compression Ratio
2;30 for adult
1;3 for neonate
©: Solomon Tegegne 2012 E.c Page 36
[COMPETENCE BASED PRACTICAL SHORT NOTE FOR NURSING ] April 29, 2020
CPR should be done for 5 cycle CHARACTERSTIC OF BLEEDING
1. Between the two Nipples (for Adult)Draw
imaginary line from Trachea to Abdomen Type Pressure Colour
and again from one Nipple to the other.the Arterial Heavy Bleeding Bright Red
space where the two imaginary lines Venial Medium Dark Red
connected is the site of compression. Bleeding
2. 4-6 cm Above xyphoid process (for Capillary Minor Bleeding Dark Bright
Adult) Red
First put two fingers on the xyphoid
process and place the Heel of your
Bleeding Control Mechanism
palm Above the fingers
3. 2-4 cm bellow the line of two nipple for 1. Apply Direct pressure
neonate 2. Elevate above the heart level
Depth 3. Apply pressure bandage
Adult 1 ½ - 2 Inch with two Hand 4. Apply pressure point or torniquating
Child 1 - 1½ Inch with One Hand
Infant ½ - 1 Inch with two fingers N:B:- if the bleeding site have fracture do not
use elevation technique to control Bleeding
When to stop CPR
1. Return of spontaneous circulation
2. Arrival of arrest team or medical Help While you use Bleeding control
3. If the rescuer become exhausted technique follow strict sterile
4. When death is confirmed technique.
5. When there is unsafe condition
SUTURING
Complications Related with CPR
1. Ribs fracture Definition; - process of sewing together the
2. Gastric distant ion(the most common) edge of the injurered tissue
3. Vital Organ injury
PURPOSE
Bleeding control
To facilitate wound healing process
Definition;- Process of controlling the Escaped
Blood from the site.
To prevent infection
To promote skin integrity
Bleeding:- Oozing (Escape)of Blood from the
Blood Vessel TYPE OF SUTURING
Plain interrupted
Coues:- -
Plain continuous
Motor vehicle accident
Mattress interrupted
Sharp instrument injury
Mattress continuous
Intentional surgical procedures
Type of Bleeding TYPE OF SUTUR MATERIAL
1. Internal Bleeding Silk;- non absorbable suture material and
used for repairing outer tissue part
2. External Bleeding Cut gut ;- absorbable suturing material
and used for repairing internal tissues like
Source of Bleeding
muscle cartilages
1. Arterial :-Bleeding fromthe Arteries
CONTRA INDICATION
2. Venial: Bleeding fromthe veins
3. Capillary:- Bleeding from capillary Wound >12hr
Dog and humane bite
Gun shoot
©: Solomon Tegegne 2012 E.c Page 37
[COMPETENCE BASED PRACTICAL SHORT NOTE FOR NURSING ] April 29, 2020
5. Growth retardation
Portion Energy
6. Wasting of fat and muscle tissue
Malnutrition 7. Monkey face (old man face)
Definition:- A form of malnutrition result from 3.Marasmickwashi:- A marked protein and
a diet that lack of sufficient portion and /or caloric adequacy characterised by
Energy extremely weight loss, Oedema and other
symptom that combined with marasmus &
Coues/Ethology kwashiorkor
1. Primary cause:- directly related with food Diagnosis
supply limitation 1. Clinical manifestation
Ex. Poverty 2. Anthropometric measurement
2. Secondary course:- malnutrition
secondary to disease process Anthropometric measurement often done in
the following classification
Ex. diarrheal, infection, malaria
Gomez classification
Forms of protein Energy malnutrition it not considered Oedema
used to compare and contrast the
1. Kwashiorkor percentile of Wt for Age according to
2. Marasmus Gomez classification the result will be
3. Marasmic-kwashi described as follow
1. Kwashiorkor (wet-malnutrition) :- a
sever deficiency of protein and other
related nutrients. It commonly occur at Percentile of wt Result
the Age B/n 1-4 year and after for age
Breastfeeding is discontinued >90% Well Nourished
76-90% Grade 1or mild
malnutrition
Clinical Manifestation
60-75% Grade 2 or moderate
malnutrition
The child being diagnosed in this category
<60% Grade 3 or sever
shows the following sign and symptoms
malnutrition
mainly.
Welcome classification
They are
it considered Oedema and also Comair
1. Oedema weight for age
2. Poor appetite (Anorexia)
3. Apathetic:- poor feeling(calm) Percentile Result
60-80% With Kwashiorkor
4. Skin Infection mainly dermatitis
Oedema
5. Moon face
Without Under nutrition
6. Hair Colour Change Oedema
7. Ulcer development <60% With Maralmic&kwashi
8. Hepatomegaly Oedema
9. Calm Without Marasmus
10. Skin become pale Oedema
2. Marasmus (dry-malnutrition) :- long term
lack of protein energy and carbohydrate Management
deficiency. It commonly occur at the age
B/n 6-18 month Goal – to promote child Health status
Clinical Manifestation - to provide adequate caloric
1. Old man face(monkey face) - to prevent Infection
2. Extremely weight loss
3. Have appetite -to prevent future complication
4. Irritable/restlessness)
©: Solomon Tegegne 2012 E.c Page 38
[COMPETENCE BASED PRACTICAL SHORT NOTE FOR NURSING ] April 29, 2020
according to their cause the treatment 580 gm of F75 diluted with 420ml
criteria have two phase of clean water and provide 5-
1. Rehabilitation phase:- direct 10ml/kg ever 2 hr for 6-7 days
treatment of PEM
2. Acute stabilization phase:- A B. Transitional phase
process that used to treat the
underlying cause. Phase that used to prepare the patent for
1. Rehabilitation Phase phase 2
1. Protein food (kwashi Transition criteria
Milk)
2. Fortified 75(F-75) and 1. Return of appetite
fortified 100(F-100) 2. Beginning of loss of Oedema
3. 6gm weight gain per day
To provide fortified therapy a care giver 4. No IV line & NG Tube
should classified in to three sub-phase
N:B use F 100 for 1-2 days but remember 130
A. Phase One ml of f100 should have 100 kcal and the
preparation the same as phase one
Apt who has poor appetite and major medical
complication are initially admitted to an Criteria to move back from transition to
inpatient facility phase1
Admission criteria for phase 1 1. 10gm weight gain per day
2. Increased bilateral oedema
1. Bilateral Oedema (pitting Oedema) 3. If NG tube feed is needed
2. Open skin lesion 4. If the Pt develop medical complication
3. Reduced mid upper arm Ex. -Abdominal distension
circumference (MUAC) -pneumonia
11.5 cm or 110 mm with > 65cm -diarrhoea & vomiting
5. If the child who does not have Oedema,
for Infant and Adolescent
18.5cm or 180mm with recent wt develop Oedema
loss (BMI<6) or underlying chronic
Inness for adult
C. Phase two
4. Sever form of medical complication
It is given in outpatient facility
Ex. Severe anaemia, vomiting
Any condition that require an Formula that used to give is F100
infusion of NG tube feeding
Preparation
N:B. The aboveadmission criteria
recommends forall agegroups 1. 130mL of F100 x kg
6-8feed /24hrs
Formula feed during this phase is fortified N:B 130 ml of F100 should contain 130 kcal
75(F-75)
2. According to packet preparation580
Preparation gm of F100diluted with 540 ml of
clean water and provide
1. 130ml of F75 x kg
5-10mL/kg every, 4 hr for,12-14 days
6-8 feed / 24hr
Criteria to move back from phase two to
130ml of F75 = 100kcal
phase one
N:B410gm of F-75 diluted with 2 litre of clean 1. Failure of appetite test
water 2. Increased Oedema
3. Development of diarrheal sufficient to
2. According to packet preparation lead weight loss
4. Failure to respond to treatment
©: Solomon Tegegne 2012 E.c Page 39
[COMPETENCE BASED PRACTICAL SHORT NOTE FOR NURSING ] April 29, 2020
N:Bkwash Milk preparation:-to prepare 2. Some (moderate) dehydration:- two of
&kwashi Milk use the following formula the following clinical manifestation will
indicate that there is some DHN.
Nido + KCL + Oil + Sugar + Mgso4 (Antacid)
Irritable or restlessness
600ml of kwash milk given within 24 hr Eger to drink
Routine Medicine Skin goes back slowly
1. Vitamin A:- a fat soluble vitamin and Sunken eye
help for treatment of Avitaminosis (Vit A
deficiency) N:Bto check the turgor pressure pinch the
abdominal area vertical not horizontally
Dose 100,000 IV given B/n 6-11month
The treatment given under plan B
200,000 IV given for the child who is B/n 12-
59 month 3. No dehydration (mild); there is not
enough sign symptom to classify
Sx/sxy of vitA deficiency
the dehydration but there is a good
1. Dryness of eye (xerosis)or risk factor.
(xeroptalmia)
2. Desquamation of sclera Plan A
Management It should be given at home and plan
components are
1st dose of Vit A 200,000IV 1st day at any
time when the child comes to your 1 GICE EXTRA FLIID
Hospital
2nd dose give after month ORs + BF only if the child age is < 6month
3rd dose better given after month or ORs + BF + FBF if the child age is >6 month
2month
Oral rehydration salt (ORs) preparation
DEHYDRATION
The sever forms of body fluid deficiency or the Up to 2 yr from 50-100 ml after each stool
reduction off fluid and electrolytes in the body loss or vomiting
2-5 yrs from 100-200 ml after each stool
CAUSE
loss or vomiting
.....Diarrhoea, vomiting, haemorrhage,
burn...etc
2 Give zinc supplement
Type of dehydration
Zinc supplement always given based on the
Dehydration can be classified based on its child’s age
severity,
If the child age below 6 month give
half tab or 10 mg/ day for 10days
They are:-
If the child age is above 6 month give
1. Saver dehydration:- two of the following one tab/day for 10days
clinical manifestation indicate that 3 Continues feeding
there is a sever DHN
If the child once exposed for dehydration you
Lethargic(unconsciousness) should have to give extra feeding so these
Poor to drink extra feeding will provide by giving breast
Skin goes back very slowly feeding and food based fluids with additional
Sunken eye nutritional supplement.
The treatment should be given under the 4 When to return to the hospital
If the child get worse
planeC
If the child manifested sever forms of
fever
©: Solomon Tegegne 2012 E.c Page 40
[COMPETENCE BASED PRACTICAL SHORT NOTE FOR NURSING ] April 29, 2020
If the diarrhoea is not stop If the child age is between 1-5yrthe
Other manifestation related with fluid should be ended within 3hr (30
dehydration minute & 150 minute)
Plan “B” Poste partumhaemorrhage
It always given at hospital within the first four Definition;- sever bleeding during 3rd stage of
hours and the treatment component should labour or within 24hr after expulsion of
have ORs + BF + Clean water placenta. (>1000ml)
Couse
N;BThe clean water must be boiled
before provide for the child Uterineatony
Retained placenta
ORs can be given based on the child age Genitaltract laceration
and weight Blood coagulation dis order
Based on Age Clinical manifestation
Up to 4 month 200-400 ml Vaginal bleeding
4-12month 400-700 ml Big and boggyuterus
1-2year 700 – 900 ml Rapidand weak pulse
2-5 year 900-1400ml Pallor
Hypotension
Based on weight Shock
Dehydration
75ml x kg(wt) = amount of solution
Management
Assessment after the first four hour
Determine the Couse
If the child is recover put on planA Fell for the uterus and asses its tone
If the child is not recover repeat plan
B for the next four hour N;B if soft and not well contracted it is
uterineatony
Assessment after the next four hour
Inspect lower genitalia tract(Cx,Vx and
If the child is recover put on planA perineum)
If the child is not recovered put on
PLAN C .:. If laceration is seen the cause is laceration
Do manual explanation of uterus
Plan “C”
If fragment is found the cause is retained
It always given at hospital for sever form of placenta and if uterus tear is found the cause
dehydration and The treatment component will is rupture of uterus
be
Treat accordingly the Couse
IV/NGT + ORs(5ml/kg/hr) Massaging the uterus for uterineatony
Put the pt in obstetric position
Expel any clots and give ergometriane or
The best and the preferable fluid to be oxytocin 2ml IM
Repairer if it is CxVxperennial laceration
administered is RINGER LACTET 100ml/kg
Do evacuation and curettage for retained
(30ml/kg + 70ml/kg)
placenta
The flow rate always based on the child age Provide fluid resastasion and
continuous assessmen
If the child age is less than 12 month
the fluid should be end within 6hr. (l
hr& 5hr)
©: Solomon Tegegne 2012 E.c Page 41
You might also like
- Always Breathe Correctly E Book PDFDocument62 pagesAlways Breathe Correctly E Book PDFFilipe Boiler100% (1)
- TCB ChecklistDocument3 pagesTCB ChecklistStephanie LiauNo ratings yet
- Low Birth WeightDocument22 pagesLow Birth Weightエド パジャロン100% (4)
- NCP LeptospirosisDocument2 pagesNCP LeptospirosisLouise Anne Asuncion OclimaNo ratings yet
- Chemistry Project 2Document13 pagesChemistry Project 2Manish Chaudhary86% (83)
- 2) Vital SignsDocument7 pages2) Vital SignsJudy JalbunaNo ratings yet
- Ncma121 Lec MidtermsDocument4 pagesNcma121 Lec MidtermsAlyanna TiglaoNo ratings yet
- Module 2 VITAL SIGNSDocument15 pagesModule 2 VITAL SIGNSSHANE VALERIE DIEZNo ratings yet
- Vital SignsDocument5 pagesVital SignsSandara Delas PenasNo ratings yet
- Vital SignsDocument16 pagesVital SignsNj PagdawanNo ratings yet
- Abbreviation of MedicalDocument34 pagesAbbreviation of Medicalfw4yfycp87No ratings yet
- Vital SignsDocument63 pagesVital SignsAlvin JavierNo ratings yet
- Vitals Sign HandoutsDocument13 pagesVitals Sign HandoutsAce ClaireNo ratings yet
- MedED Portal Case ExampleDocument8 pagesMedED Portal Case Examplea6909330No ratings yet
- Vital SignsDocument14 pagesVital SignsDesai NehaNo ratings yet
- Cues Nursing Diagnosis Scientific Explanation Planning Intervention Rationale EvaluationDocument6 pagesCues Nursing Diagnosis Scientific Explanation Planning Intervention Rationale EvaluationApril Ann PonceNo ratings yet
- Department of Education: Republic of The PhilippinesDocument68 pagesDepartment of Education: Republic of The Philippinesma.fatima ravalo rabulanNo ratings yet
- Vitalsigns PDFDocument36 pagesVitalsigns PDFSuneel Kumar PrajapatiNo ratings yet
- Haad Mle FundaDocument20 pagesHaad Mle FundaGreggy Francisco LaraNo ratings yet
- Assessment Nursing Diagnosis Planning Implementation Rationale EvaluationDocument3 pagesAssessment Nursing Diagnosis Planning Implementation Rationale EvaluationChloie Marie RosalejosNo ratings yet
- Chapter 21: Measuring Vital Signs Test Bank: Multiple ChoiceDocument16 pagesChapter 21: Measuring Vital Signs Test Bank: Multiple ChoiceNurse UtopiaNo ratings yet
- Lahore School of Nursing The University of Lahore Nursing Care PlanDocument2 pagesLahore School of Nursing The University of Lahore Nursing Care PlanAyesha ImtiazNo ratings yet
- ACLS ChecklistDocument9 pagesACLS ChecklistEllayza OperanaNo ratings yet
- Vital Sign Lecture 2013 PDFDocument86 pagesVital Sign Lecture 2013 PDFknotstm100% (1)
- Vital Signs MeasurementDocument17 pagesVital Signs MeasurementEly TalledoNo ratings yet
- NCM 103 Rle NotesDocument8 pagesNCM 103 Rle Notesgallardo.bettinarose.iNo ratings yet
- VITAL SIGNS (Word)Document21 pagesVITAL SIGNS (Word)Jennifer B. GarciaNo ratings yet
- Radtech Vital SignsDocument49 pagesRadtech Vital SignsGEORGIE JANE LORENANo ratings yet
- Fundamentals in Nursing NotesDocument6 pagesFundamentals in Nursing NotesKarol De La CruzNo ratings yet
- UNIT II in HEALTH9 - Injury Prevention Safety and First Aid Unintentional - STUDENTS LectureDocument7 pagesUNIT II in HEALTH9 - Injury Prevention Safety and First Aid Unintentional - STUDENTS Lectureitsmefuntassy100% (1)
- Hyperthermia NCPDocument3 pagesHyperthermia NCPkaylejordan_29100% (2)
- VITAL SIGNS and Patient AssessmentDocument8 pagesVITAL SIGNS and Patient AssessmentHANNAH ANIVERSARIONo ratings yet
- Assessment Explanation of The Problem Objectives Nursing Interventions Rationale EvaluationDocument3 pagesAssessment Explanation of The Problem Objectives Nursing Interventions Rationale EvaluationAlyssa Moutrie Dulay Arabe100% (1)
- Vital SignsDocument7 pagesVital SignsEmeroot RootNo ratings yet
- FON Question BankDocument5 pagesFON Question Bankramzan aliNo ratings yet
- 8vital SignsDocument15 pages8vital SignsVaniegrace Angel BalagonNo ratings yet
- SubjectiveDocument2 pagesSubjectiveMicalyn R. EspinosaNo ratings yet
- Community Health Nursing and Pharmacology Course Task #4Document3 pagesCommunity Health Nursing and Pharmacology Course Task #4Michelle Angela AlombroNo ratings yet
- HyperthermiaDocument6 pagesHyperthermiaBerlyn FelicianoNo ratings yet
- Multiple TraumaDocument5 pagesMultiple TraumaChristabel EdithNo ratings yet
- Vital Signs (Lecture)Document15 pagesVital Signs (Lecture)ALLYSON GENE GULANESNo ratings yet
- Concept MapDocument13 pagesConcept MapIssa RomaNo ratings yet
- Module 7 Taking Vital SignsDocument7 pagesModule 7 Taking Vital SignsMary Joy CejalboNo ratings yet
- Nursing Care PlanDocument6 pagesNursing Care PlanKaguraNo ratings yet
- Vitalsigns 180617200506Document34 pagesVitalsigns 180617200506Maricris Tac-an Calising-PallarNo ratings yet
- Vital Signs Vital Signs: Importance: ImportanceDocument6 pagesVital Signs Vital Signs: Importance: ImportanceTyron KristianNo ratings yet
- Lab Manual - Human Anatomy and Physiology IIDocument23 pagesLab Manual - Human Anatomy and Physiology IIosm paglaNo ratings yet
- Vital SignsDocument15 pagesVital Signsgennemayguzman2004No ratings yet
- Post Operative PhaseDocument5 pagesPost Operative PhaseKaren May HontiverosNo ratings yet
- Vital SignsDocument5 pagesVital SignsJazminCabagnotNo ratings yet
- January 29 DiscussionDocument11 pagesJanuary 29 DiscussionA CNo ratings yet
- March 2023 Duty NavDocument5 pagesMarch 2023 Duty NavKyle Mitzie SengcoNo ratings yet
- Virginia Avenel HendersonDocument109 pagesVirginia Avenel HendersonSimranpreetkaur SimranNo ratings yet
- Vital Signs Cardinal SignsDocument6 pagesVital Signs Cardinal SignsHNo ratings yet
- 10663-26 CH26 PDFDocument37 pages10663-26 CH26 PDFHermanNo ratings yet
- Emergency Drugs (LEAD)Document8 pagesEmergency Drugs (LEAD)RayePrudenteNo ratings yet
- Vital Signs HandoutsDocument4 pagesVital Signs Handoutsjoemel gregoriNo ratings yet
- Disaster Nursing ReviewerDocument45 pagesDisaster Nursing ReviewerYor ForgerNo ratings yet
- Health Assessment Handout 2Document15 pagesHealth Assessment Handout 2ApRil Anne BalanonNo ratings yet
- Heart of the Field "Refresher & Nha Certification Quick Notes"From EverandHeart of the Field "Refresher & Nha Certification Quick Notes"No ratings yet
- Predicting Creativity: Interactive Effects of Openness To Experience and Emotion Regulation AbilityDocument8 pagesPredicting Creativity: Interactive Effects of Openness To Experience and Emotion Regulation Abilitynoah0firthNo ratings yet
- Katrin Barnard Theory PciDocument34 pagesKatrin Barnard Theory PciArum NingtiasNo ratings yet
- Pollution Prevention Management Plan MajorDocument30 pagesPollution Prevention Management Plan MajorAlbatool ElsayedNo ratings yet
- EnterobiasisDocument5 pagesEnterobiasiszairaconcoNo ratings yet
- 12 Advantages and Disadvantages of Animal Testing On CosmeticsDocument3 pages12 Advantages and Disadvantages of Animal Testing On CosmeticsElo RubioNo ratings yet
- Accuracy and Reliability of Knee Goniometry Methods: Research Open AccessDocument6 pagesAccuracy and Reliability of Knee Goniometry Methods: Research Open AccessAdil HidayatNo ratings yet
- Negative ReinforcementDocument16 pagesNegative Reinforcementcibrown12No ratings yet
- Lanyard - Business ProposalDocument4 pagesLanyard - Business ProposalPaul SuicoNo ratings yet
- Role of Pharmacists in The IndustryDocument10 pagesRole of Pharmacists in The IndustryGerald Limo Arap ChebiiNo ratings yet
- Best Practice Paper 1 Postpartum Family PlanningDocument17 pagesBest Practice Paper 1 Postpartum Family PlanningGia DuyNo ratings yet
- P. Research 2 Prelims Edited 2Document5 pagesP. Research 2 Prelims Edited 2Marichu CayabyabNo ratings yet
- Organisational Dynamics: Term 1Document14 pagesOrganisational Dynamics: Term 1Gudia ManmeetNo ratings yet
- Women's Era TP August 2021Document116 pagesWomen's Era TP August 2021NancyShahNo ratings yet
- Module 3 The FamilyDocument98 pagesModule 3 The FamilyJoycee BoNo ratings yet
- Ucs102 Entrepreneurship in Asia Assignment-sept20-SuryatiDocument16 pagesUcs102 Entrepreneurship in Asia Assignment-sept20-SuryatiNUR HABIBAH BT YUSUFNo ratings yet
- School Counselor InterviewDocument1 pageSchool Counselor InterviewJhonmarkNo ratings yet
- NCM 3260 - Gastro - Intestinal ObstructionDocument36 pagesNCM 3260 - Gastro - Intestinal ObstructionCherish Marie HurbodaNo ratings yet
- Pharmacology Exam COHORT 8Document9 pagesPharmacology Exam COHORT 8Lesley Liavoga SandeNo ratings yet
- The Origin of Comfort TheoryDocument6 pagesThe Origin of Comfort Theoryibrahimaldarawi34No ratings yet
- DNB Family Medicine Question BankDocument157 pagesDNB Family Medicine Question BankEpun B. Dissanayake100% (1)
- Drtbalu'S Otolaryngology Online: Vocal NoduleDocument2 pagesDrtbalu'S Otolaryngology Online: Vocal NoduleAnish RajNo ratings yet
- Ultrasound For Detection of Ascites and For Guidan PDFDocument18 pagesUltrasound For Detection of Ascites and For Guidan PDFEstu Paramadina PratamaNo ratings yet
- ProstataDocument26 pagesProstatasidney souzaNo ratings yet
- Shallow and Flat Anterior ChamberDocument8 pagesShallow and Flat Anterior Chamberjudah samuelNo ratings yet
- KF - 07 - Blood Grouping 2019 - 03 - enDocument4 pagesKF - 07 - Blood Grouping 2019 - 03 - enSurta DevianaNo ratings yet
- BG of The StudyDocument2 pagesBG of The StudySbs Nhanxzkie Jountey MushroomxzNo ratings yet
- Thyroid QuizDocument3 pagesThyroid QuizĐặng Quỳnh ANNo ratings yet
- Tab9 PDFDocument7 pagesTab9 PDFGokul GoNo ratings yet