Professional Documents
Culture Documents
Menzies 2015
Menzies 2015
Uploaded by
kosikevinonuOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Menzies 2015
Menzies 2015
Uploaded by
kosikevinonuCopyright:
Available Formats
REVIEWS
Compromised autophagy and
neurodegenerative diseases
Fiona M. Menzies1, Angeleen Fleming1,2 and David C. Rubinsztein1
Abstract | Most neurodegenerative diseases that afflict humans are associated with the
intracytoplasmic deposition of aggregate-prone proteins in neurons and with
mitochondrial dysfunction. Autophagy is a powerful process for removing such proteins and
for maintaining mitochondrial homeostasis. Over recent years, evidence has accumulated
to demonstrate that upregulation of autophagy may protect against neurodegeneration.
However, autophagy dysfunction has also been implicated in the pathogenesis of various
diseases. This Review summarizes the progress that has been made in our understanding of
how perturbations in autophagy are linked with neurodegenerative diseases and the
potential therapeutic strategies resulting from the modulation of this process.
Tauopathies
Intracytoplasmic protein misfolding and aggregation Investigations into the function of these genes have iden-
A group of neurodegenerative are features of many late-onset neurodegenerative dis- tified multiple intersections with the autophagy path-
diseases that are characterized eases called proteinopathies. These proteinopathies way. In this Review, we examine the role of autophagy
by the prominent accumulation include Alzheimer disease (AD), Parkinson disease — in particular, macroautophagy — in neurodegenera-
of tau protein in the CNS.
(PD), tauopathies and the neurodegenerative diseases tion. We begin by briefly reviewing the core aspects of
Ubiquitin–proteasome caused by (CAG)n trinucleotide tract expansions that autophagy biology, before focusing on studies from the
system encode abnormally long polyglutamine (polyQ) tracts, past 2 years that have revealed the diversity of autophagy
A cellular protein degradation such as Huntington disease (HD). In many of these components that can be hijacked by disease-causing
system in which proteins diseases, the proteins that accumulate are thought to lesions and how this process may be manipulated to
tagged with ubiquitin, a small
regulatory protein that is
be toxic. This concept is supported by overexpression protect against neurodegeneration.
covalently attached to a target mouse models of HD, the occurrence of autosomal
protein, are broken down by an dominant tauopathies that are caused by mutations in the The autophagy machinery
enzyme complex called the gene encoding tau, and PD that is caused by triplication Autophagy, literally meaning ‘self-eating’, is an intra-
proteasome.
of the α‑synuclein (SNCA) locus (reviewed in REFS 1,2). cellular degradation pathway that is responsible for
Accordingly, reductions in the steady-state levels of these the digestion and recycling of nutrients via autophago-
proteins may be beneficial in targeting the root cause of somes. These intracellular double-membraned struc-
these diseases. Recent data suggest that the lifetime of tures engulf cytoplasmic proteins and organelles and
mutant huntingtin (mHTT), the protein that accumu- deliver them to the lysosome for degradation (FIG. 1).
lates in and causes HD, may be a superior predictor of The process is essential for cell survival during nutrient
1
Department of Medical neuronal toxicity compared with its steady-state levels3, starvation, as it provides cellular energy 10. Autophagy is
Genetics, University of
Cambridge, Cambridge
supporting strategies that aim to enhance the clearance also a major pathway for the degradation of intracellu-
Institute for Medical of such proteins. lar organelles and aggregate-prone proteins11. Through
Research, Addenbrooke’s Although inducing clearance of intracytoplasmic both the recycling of nutrients and the degradation of
Hospital, Hills Road, aggregate-prone proteins may represent a therapeutic protein oligomers and damaged organelles, autophagy
Cambridge CB2 0XY, UK.
strategy, compromised clearance may exacerbate or con- serves a vital role in maintaining homeostasis within
2
Department of Physiology,
Development and tribute to disease by increasing levels of key substrates the cell.
Neuroscience, University of such as aggregate-prone proteins4,5 and dysfunctional
Cambridge, Downing Street, mitochondria6; enhancing susceptibility to cell death7,8; Initiation of autophagy. The initial step in the forma-
Cambridge CB2 3EG, UK. and perturbing flux through the ubiquitin–proteasome tion of autophagosomes is the fusion of vesicles that
Correspondence to D.C.R.
system 9. The genomics era has revealed many genes have been proposed to arise from a variety of membrane
e‑mail: dcr1000@hermes.
cam.ac.uk associated with neurodegenerative diseases, either sources, including plasma membrane-derived endoso-
doi:10.1038/nrn3961 as causative mutations or as risk factors for disease. mal intermediates12, the endoplasmic reticulum (ER)13,14,
NATURE REVIEWS | NEUROSCIENCE VOLUME 16 | JUNE 2015 | 345
© 2015 Macmillan Publishers Limited. All rights reserved
REVIEWS
H+ pH
ATP13A2 (PD) and PS1 (AD)
Trafficking
Degradation
ATG5–ATG12–ATG16L Cystatins (LSDs) and
LC3-II glucocerebrosidase
Receptor (LSDs and PD)
Recycling
Autophagic cargo Spastizin and Biogenesis
spatacsin (HSP) TFEB (multiple)
Initiation
Alsin (ALS), ATG7 (HD)
and spastizin (HSP) Precursor Pre-autophagosomal Autophagosome Lysosome Autolysosome
vesicle structures
VPS34
Beclin 1
Precursor formation Receptors
VPS35 and α-synuclein (PD), p62 and optineurin (ALS) Maturation of autophagosomes and lysosomes
PICALM (AD) and WIPI4 (BPAN) and HTT (HD) PICALM (AD), CHMP2B (CMT2) and SIGMAR1 (ALS)
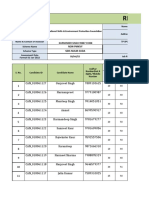
Figure 1 | Overview of the autophagy pathway and the sites of action of disease-associated proteins.| Neuroscience
Nature Reviews This diagram
shows a simplified version of autophagy. Initiation of autophagy is signalled via the activity of the vacuolar protein
sorting 34 (VPS34) complex. Precursor vesicles fuse to form pre-autophagosomal structures that grow to eventually
become double-membraned autophagosomes. Substrates for degradation by autophagy are engulfed by these growing
membranes or may be sequestered into the forming structure by receptor proteins. The completed autophagosomes are
then trafficked to fuse with lysosomes. The acidic environment inside the lysosomes is maintained by ATPases. This low pH
is required for the correct function of the lysosomal degradative enzymes (depicted as scissors) and, therefore, the
breakdown of the autophagy substrates. Perturbations throughout the pathway, from initiation of autophagosome
formation to degradation in the autolysosomes, have been suggested to be involved in neurodegenerative diseases; some
disease-associated proteins function at multiple points in the process. The key points in the pathway and the selected
disease-associated proteins that are thought to act at these points are highlighted in boxes; the relevant disease is
indicated in parentheses. AD, Alzheimer disease; ALS, amyotrophic lateral sclerosis; ATG, autophagy protein; ATP13A2,
ATPase type 13A2; BPAN, β‑propeller protein-associated neurodegeneration; CHMP2B, charged multivesicular body
protein 2B; CMT2, Charcot–Marie–Tooth disease type 2; HD, Huntington disease; HSP, hereditary spastic paraplegia; HTT,
huntingtin; LC3, microtubule-associated protein 1 light chain 3; LSD, lysosomal storage disease; PD, Parkinson disease;
PICALM, phosphatidylinositol-binding clathrin assembly protein; PS1, presenilin 1; SIGMAR1, sigma non-opioid
intracellular receptor 1; TFEB, transcription factor EB; WIPI4, WD repeat domain phosphoinositide-interacting protein 4.
the Golgi15,16 and mitochondria17. These vesicles coalesce is first cleaved by ATG4B to form LC3‑I, which is then
to form a flattened membrane sac called a phagophore. conjugated to phosphatidylethanolamine by ATG7 and
The fusion of additional vesicles results in the forma- ATG3 to form LC3‑II19. As the phagophore enlarges
tion of a cup-shaped double membrane that surrounds and approaches closure, the ATG5–ATG12–ATG16L1
and eventually engulfs portions of cytoplasm as the two complex dissociates from the outer membrane,
edges of the structure come together and fuse (FIG. 1). whereas LC3‑II remains associated with the completed
Various autophagy (ATG) proteins are essential autophagosome. Following closure, autophagosomes
for the formation of autophagosomes. The vesicles are trafficked by dynein motors along microtubules20 to
that give rise to the phagophore contain a complex the perinuclear region where they fuse with the lyso-
of ATG5–ATG12–ATG16L1, the formation of which some and their contents are degraded. SNAREs (solu-
requires the catalytic activities of ATG7 and ATG10. ble NSF attachment protein receptors) have a critical
Risk factors In addition, the phagophore membrane contains role in autophagosome formation and degradation.
Factors (in this article, ATG9, the only multipass transmembrane protein in The primary function of these proteins is to facilitate
alterations in DNA sequences) the ATG family. Recently, it was shown that ATG9- and vesicle fusion, and different members of the SNARE
that may increase the chance
ATG16L1‑containing vesicles arise independently via family are critical for various steps of the process.
of developing a disease.
clathrin-mediated endocytosis but subsequently fuse in For example, vesicle-associated membrane protein 3
Lysosome the recycling endosome18. (VAMP3)18 is important for ATG9–ATG16L1 vesicle
An intracellular A second enzyme cleavage and conjugation pathway fusion; VAMP7, syntaxin 7 and syntaxin 8 (REF. 21) are
membrane-bound organelle that is essential to autophagosome biogenesis involves important for phagophore elongation; and VAMP7,
containing hydrolytic enzymes
that are capable of breaking
the processing of microtubule-associated protein 1 light VAMP8 and VTI1B (vesicle transport through interac-
down proteins and other chain 3 (LC3). LC3 is a protein that has been proposed tion with t‑SNAREs homologue 1B)22,23 are involved in
cellular components. to recruit membrane to the developing phagophore. LC3 autophagosome–lysosome fusion.
346 | JUNE 2015 | VOLUME 16 www.nature.com/reviews/neuro
© 2015 Macmillan Publishers Limited. All rights reserved
REVIEWS
Control over the initiation of autophagy is mediated receptor complex and components of the autophagosome
through a protein complex comprising ULK1 or ULK2, membrane (for example, ATG5 and PtdIns3P36) (FIG. 1).
ATG13, ATG101 and the focal adhesion kinase family Autophagy-linked FYVE protein (ALFY) may function
interacting protein of 200 kDa (FIP200)24. This ULK1/ in this way. ALFY is localized to the nuclear envelope
ULK2–ATG13–FIP200 complex serves as both an initiator under basal conditions but redistributes to colocalize
of autophagy and a sensor for upstream signalling through with ubiquitin-positive cytoplasmic structures upon pro-
three major pathways: the mTOR complex 1 (mTORC1), teasome inhibition, and with ATG5 or LC3‑positive cyto-
adenosine monophosphate (AMP)-activated protein plasmic puncta under amino acid starvation conditions37.
kinase (AMPK) and p53 pathways24,25. Phosphorylation of The FYVE domain of ALFY is able to bind to PtdIns3P,
ULK1 or ULK2 and ATG13 by mTORC1 inactivates this but it also contains additional domains, notably five
complex, whereas AMPK activates autophagy through the WD40 repeats, which are required for its interaction with
direct phosphorylation of ULK1 at sites that are distinct Atg5 (REF. 38), and a pleckstrin homology‑like domain
from those targeted by mTORC1. p53 can also control and a BEACH domain, which together interact with p62
autophagy through transcriptional regulation. Activated (REF. 39). These interactions suggest that ALFY has a scaf-
p53 transcriptionally upregulates pro-autophagic proteins folding role in the formation of p62‑labelled aggregates,
such as ULK1, ULK2, AMPK and tuberous sclerosis 2 which can then be targeted to autophagosomes.
protein (TSC2)25, whereas transcriptionally inactive, cyto- Additional autophagy proteins have been implicated
plasmic p53 negatively regulates autophagy through direct in the selective degradation of mitochondria (for example,
binding with FIP200 (REF. 26), which may block formation BNIP3L (BCL‑2/adenovirus E1B 1 19 kDa protein-inter-
of the ULK complex. acting protein 3‑like), Atg32 and p62) and peroxisomes
The ULK1/ULK2–ATG13–FIP200 complex controls (for example, Atg30 and p62). Although Atg32 and Atg30
the initiation of autophagy through the PI3K complex, have only been characterized in yeast and it is unclear
which comprises the vacuolar protein sorting 34 (VPS34; whether mammalian homologues of these proteins exist,
also known as PIK3C3) and its accessory partners VPS15 BNIP3L, a mitochondrial membrane protein contain-
(also known as PIK3R4), beclin 1 and ATG14L (also ing a LC3‑interacting region motif, has been shown in
known as barkor). Activation of ULK1 results in the phos- mammalian cells to play a part in the targeted clearance of
phorylation of beclin 1 and a subsequent increase in the damaged mitochondria40,41 (see BOX 1 and FIG. 2 for further
activity of the VPS34 complex 27. This complex is required details on mitophagy and neurodegeneration).
for the formation of phosphatidylinositol 3‑phosphate
(PtdIns3P) on nascent autophagosomes, which facilitates Autophagosome trafficking and degradation. The mat-
the recruitment of PtdIns3P‑binding proteins such as uration of autophagosomes and the final steps of the
WD repeat domain phosphoinositide-interacting pro- autophagic pathway have been the subject of a recent
tein 1 (WIPI1) and WIPI2 (both of which are mammalian expert review 42. Once formed, autophagosomes are
orthologues of yeast Atg18) to autophagosome mem- transported along microtubules to the lysosome-rich
branes. The recruitment of ATG16L1 to these structures perinuclear region. In neurons, autophagosomes formed
appears to occur through binding to WIPI proteins28. at the distal tip of axons are transported towards the
ULK1 also regulates the recruitment of the transmem- cell body by dynein-mediated retrograde transport 43.
brane protein ATG9 to the phagophore29,30. Recent data Autophagosomes may fuse with vesicles from the endocytic
suggest that PtdIns5P can substitute for the functions of pathway (early or late endosomes) to form amphisomes,
PtdIns3P in autophagosome biogenesis31. which subsequently fuse with lysosomes, or they may fuse
directly with lysosomes. This final step of the autophagy
Autophagy receptors. Until recently, autophagy was process is mediated by VAMP7, VAMP8 and VTI1B,
thought to be a non-selective degradation pathway, but members of the SNARE family of proteins (reviewed in
an emerging field of research has revealed a series of REF. 44). Efficient degradation of autophagy substrates
receptor proteins (which have sometimes been referred can only occur if the acidic lysosomal pH is correctly
to as adaptor proteins; for clarification on terminology, maintained and the degrading enzymes are functioning
see REF. 32) that confer substrate specificity on this pro- correctly. Sufficient lysosomes must also be available for
cess. These receptor proteins bind to a diverse range of fusion with autophagosomes because this process con-
cargoes including bacteria and viruses; however, more sumes the lysosomes. They can be regenerated through
pertinently, they have also been shown to bind to aggre- lysosomal reformation, in which tubules formed on auto
gated proteins33–35. Receptor proteins — such as p62 (also lysosomes mature into new lysosomes45. Transcription
known as sequestosome 1), next to BRCA1 gene 1 pro- factor EB (TFEB) has been identified as a master regula-
tein (NBR1), nuclear domain 10 protein 52 (NDP52; also tor for lysosomal biogenesis46; as such, this protein has an
known as CALCOCO2) and optineurin — are able to important role in the control of autophagy 47.
bind to their cargo selectively. For example, such proteins
may recognize ubiquitylated proteins (the cargoes) via Autophagy failure in neurodegeneration
Endocytic pathway ubiquitin-binding domains and bind to LC3 family mem- The vast majority of neurodegenerative diseases, includ-
A general term to describe the bers on autophagosomes through their LC3‑interacting ing sporadic forms of such diseases, have a genetic
vesicle trafficking routes by
which cells internalize
region motifs36 (FIG. 1). Selective targeting of autophagic component, and the assessment of the cellular func-
molecules from the plasma cargoes can also be mediated by autophagy recep- tions of these genes has implicated autophagic dys-
membrane. tors that form a bridge between the cargo–autophagy function in their pathogenesis. These findings have
NATURE REVIEWS | NEUROSCIENCE VOLUME 16 | JUNE 2015 | 347
© 2015 Macmillan Publishers Limited. All rights reserved
REVIEWS
Box 1 | Mitophagy in neurodegenerative disease
Mitochondria have long been studied as key organelles in the depolarization, and it is not clear how relevant this process is to
pathogenesis of many neurodegenerative diseases, particularly Parkinson disease progression. However, recent work has shown that
disease (PD). Recently, much of this research has focused on the potential endogenous parkin enables mitochondrial clearance157. This is further
contribution of altered clearance of dysfunctional mitochondria by supported by work using mt‑KR, a photoactivatable protein that
autophagy (termed mitophagy). This research has centred on two genes produces local increases in reactive oxygen species. Using this
that are the major causes of autosomal recessive PD, namely parkin construct to damage mitochondria in the distal axons of cultured
(PARK2) and phosphatase and tensin homologue-induced putative neurons, it was observed that the PINK1–parkin pathway induced
kinase 1 (PINK1; also known as PARK6), which have been shown in autophagy of these damaged mitochondria in the axons160.
Drosophila melanogaster to act via the same pathway146–148. An alternative mechanism controlling mitophagy is the externalization
In functional mitochondria, which are able to maintain their of cardiolipin, a phospholipid that is normally only present on the
mitochondrial membrane potential, PINK1 is imported via the translocase mitochondrial inner membrane. Cardiolipin is able to bind to microtubule-
of the outer membrane (TOM) complex and the translocase of the inner associated protein 1 light chain 3 (LC3)161, thereby promoting autophagy.
membrane (TIM23) complex (FIG. 2). It is then cleaved by mitochondrial However, this effect has only been observed in cells treated with
processing peptide (MPP) and presenilins-associated rhomboid-like mitochondrial toxins such as rotenone and 6‑hydroxydopamine, which
protein (PARL) before being translocated back to the cytoplasm for did not cause the same increase in PINK1 levels that are seen after CCCP
degradation by the proteasome149–151. However, in the absence of treatment. This suggests that different causes of mitochondrial damage
a mitochondrial membrane potential, PINK1 accumulates on the may result in mitophagy via different mechanisms.
mitochondrial outer membrane where it recruits parkin152–155, resulting in When considering the role of mitophagy in PD, it must be asked how
the targeting of mitochondria for degradation by autophagy. The exact mutations in PINK1 or PARK2, which account for only a small proportion
mechanism by which mitophagy is promoted downstream of parkin of PD cases, relate to other forms of the disease. A recent study has
recruitment has yet to be established (reviewed in REF. 156). A major addressed this, suggesting that sterol regulatory element-binding
hypothesis for the mechanism is that parkin ubiquitylates a number of transcription factor 1 (SREBF1), a gene identified by a genome-wide
mitochondrial outer membrane proteins, such as voltage-dependent association study as a risk factor for PD162, has a role in parkin recruitment
anion-selective channel protein 1 (VDAC1), TOM20 and mitochondrial to damaged mitochondria and mitophagy163 and could thus represent a
RHO GTPase 1 (MIRO1)152,157, which then recruit p62 to the mitochondrial link between mitophagy and sporadic PD.
outer membrane where autophagsomes subsequently form, although this Mitophagy might have further disease relevance because xeroderma
role for VDAC1 has been disputed158. PINK1 and parkin are also reported pigmentosum group A, a DNA repair disorder associated with
to have roles in mitochondrial fission and fusion, as well as in neurodegeneration, has also been linked to defective mitophagy that is
mitochondrial trafficking (reviewed in REF. 159). These roles could associated with increased cleavage of PINK1 (REF. 164). Importantly,
represent either mechanisms by which PINK1 and parkin act to ultimately impaired autophagy flux will also affect mitophagy and perturb the
control mitophagy or independent processes that affect mitochondrial clearance of dysfunctional mitochondria, which may increase the cellular
health and function. levels of reactive oxygen species and the propensity to caspase activation.
Investigations into the role for the PINK1–parkin pathway in Although mitophagy is not the focus of this Review (and has been the
mitophagy have mostly been carried out in non-neuronal cultured subject of a recent excellent review156), these consequences are important
cells overexpressing parkin and treated with carbonyl cyanide to consider as pathogenic mechanisms in the diseases in which autophagy
m‑chlorophenylhydrazone (CCCP) to induce mitochondrial is compromised.
been complemented by studies showing that autophagy neurodegenerative diseases. Instead, we aim to highlight it
markers are perturbed in post-mortem tissue in many as a common aspect of these complex diseases and discuss
neurodegenerative diseases. However, in many cases, the the new information coming to light about the intersec-
molecular mechanisms have yet to be determined, and tion of autophagy and neurodegeneration.
it remains to be ascertained whether this truly repre-
sents dysfunctional autophagy or whether compromised Mutations in core autophagy genes. Loss-of-function
autophagy contributes to disease progression. mutations have been identified in the gene encoding the
Here, we do not discuss the evidence for altered β‑propeller scaffold protein WIPI4 (WDR45) in BPAN49.
autophagy disease-by‑disease as we have done previously48 WDR45 is a core autophagy gene, encoding one of four
but, rather, consider how recent research has revealed a homologues of yeast Atg18, involved in autophago-
number of key points in the autophagic pathway that can some formation. Parents or siblings of patients with
be affected by disease-causing mutations. To date, there WDR45 mutations do not share the mutation, suggest-
has only been one disease — β‑propeller protein-associ- ing that such mutations occur de novo50. Lymphoblastoid
ated neurodegeneration (BPAN; also known as neuro cell lines derived from these patients have reduced
degeneration with brain iron accumulation 5 (see below)) autophagic activity 50, which may result from disrupted
— in which the causal mutation occurs in a gene that is ATG9A vesicle translocation at the autophagosome for-
proposed to function solely in autophagy (although other mation site owing to altered WIPI4 activity 51.
Polymorphisms functions of this gene may emerge with further research). Given the importance of autophagy in cellular func-
The existence of multiple Indeed, most of the proteins discussed in this Review have tion, mutations in core autophagy genes are likely to have
variants of a DNA sequence functions beyond a role in autophagy. Many of these func- severe consequences. Thus, it is perhaps unlikely that
that occur within different tions may be pertinent to the pathogenesis of neurodegen- late-onset neurodegenerative diseases will be caused by
individuals in the population,
with no sequence being
erative disease but are, for the most part, not discussed recessive mutations in autophagy genes, and it is more
regarded as the standard here. We do not suggest that autophagy dysfunction is likely that polymorphisms in these genes contribute to the
sequence. the single mechanism underlying the pathogenesis of age of onset and disease progression of such disorders.
348 | JUNE 2015 | VOLUME 16 www.nature.com/reviews/neuro
© 2015 Macmillan Publishers Limited. All rights reserved
REVIEWS
is observed55. In turn, RHES has been demonstrated
PINK1
to enhance autophagy via its interaction with beclin 1,
Proteasome
blocking the inhibitory interaction of beclin 1 with
BCL‑2. Importantly, mHTT prevents this autophagy
TOM Mitochondrion activation56.
TIM23
Beclin 1 is also involved in the maturation of
MPP PARL autophagosomes through its role in the ultraviolet radia-
tion resistance-associated gene protein (UVRAG)–
H+ Cardiolipin
rubicon–beclin 1 complex. Beclin 1 also interacts with
spastizin57 (encoded by ZFYVE26, which is mutated
in hereditary spastic paraplegia (HSP) type 15), and
disease-associated mutations disrupt this interaction58.
Autophagosomes accumulate in cells lacking spastizin or
expressing mutant forms of this protein58. This accumula-
tion has been proposed to result from loss of function of
MIRO1 Phagopore the UVRAG–rubicon–beclin 1 complex 58 but may also be
due to defects in lysosomal function (see below).
Ubiquitin
VDAC1
Parkin LC3-II Mutations in genes involved in trafficking. Membrane
ATG5–ATG12–ATG16L trafficking is a vital element of autophagy, and the
Figure 2 | Initiation signals for mitophagy. In mitochondria that are able to maintain identification of proteins involved in such trafficking
Nature
their membrane potential (as shown in the upper half of the Reviews
diagram), | Neuroscience
phosphatase and is currently an area of intensive research. Many neuro
tensin homologue-induced putative kinase 1 (PINK1) is imported across the degenerative disease-causing mutations have been iden-
mitochondrial membrane by the translocase of the outer membrane (TOM) complex tified in genes that can be classed as trafficking genes,
and the translocase of the inner membrane (TIM23) complex before being cleaved by and an attractive hypothesis for the pathogenic mecha-
mitochondrial processing peptidase (MPP) and presenilins-associated rhomboid-like nism of late-onset neurodegenerative diseases is that the
protein (PARL) and then targeted for degradation by the proteasome. In the absence of
mutations are likely to impair autophagy efficiency.
a membrane potential (lower half of the diagram), PINK1 cannot be transported across
the membrane and instead recruits parkin to the membrane, resulting in the Phosphatidylinositol-binding clathrin assembly
ubiquitylation of other mitochondrial outer membrane proteins (such as protein (PICALM) was identified through genome-
voltage-dependent anion-selective channel protein 1 (VDAC1) and mitochondrial RHO wide association studies to be associated with AD59,60.
GTPase 1 (MIRO1)), phagophore formation and subsequent degradation. Alternatively, Moreover, PICALM has been reported to be abnormally
externalization of cardiolipin onto the outer membrane following mitochondrial cleaved in the brains of patients with AD, resulting in
depolarization has also been reported to result in phagophore formation. ATG, a decreased level of the full-length protein61. PICALM
autophagy protein; LC3, microtubule-associated protein 1 light chain 3. is required for the endocytosis of VAMP2 and VAMP3,
which are necessary for autophagosome formation,
and VAMP8, which is important for autophagosome–
Support for this assertion can be found in HD. The age lysosome fusion. In the absence of PICALM, decreased
of onset of HD is closely correlated with the polyQ repeat fusion of autophagosome precursor vesicles is observed
length, which accounts for 70% of the variance; however, (VAMP2- and VAMP3‑dependent processes), leading
other genetic factors have been proposed to contribute to impaired autophagosome biogenesis, along with a
to age of onset. One such gene is ATG7: the V471A poly- decrease in the fusion of autophagosomes with lyso
morphism has been associated with an earlier onset of somes (a VAMP8‑dependent process), resulting in an
disease by 4–6 years in certain populations52,53. However, overall reduction in autophagic flux 62. These defects
it has yet to be demonstrated whether this polymorphism contribute to the accumulation of tau, an autophagy
has functional importance in terms of autophagic activity. substrate and a probable contributor to AD pathology.
The small GTPase RAB protein family comprises
Beclin 1 interactions. As noted above, beclin 1 is req well-known regulators of membrane trafficking and
uired for the early steps of autophagosome formation. fusion events. Mutations in RAB7, which encodes a
Neurodegeneration-associated proteins are now coming late endosomal RAB protein known to be involved in
to light that may affect the interactions of beclin 1 with autophagy (reviewed in REF. 63), have been reported
its protein partners and influence its ability to medi- to cause Charcot–Marie–Tooth type 2B disease 64.
ate autophagy. Overexpression of the E46K variant of Similarly, the gene encoding alsin (ALS2) is mutated
α‑synuclein, which causes a rare autosomal dominant in some cases of recessive amyotrophic lateral sclerosis
form of PD, leads to decreased levels of phosphorylated (ALS)65. Alsin is an activator of RAB5 (REF. 66), which is
BCL‑2, which then enhances the interaction between required for the clearance of aggregate-prone proteins
beclin 1 and BCL‑2 and therefore results in autophagy by autophagy 67. Missense mutations in ALS2 result in
inhibition54. Regulation of the beclin 1–BCL‑2 inter- mislocalization of the protein and a decreased fusion
action has also been suggested to be compromised in of autophagosomes with endosomes68. Hexanucleotide-
HD. HTT has been demonstrated to interact with Ras repeat expansions in a non-coding region of chromo-
homologue enriched in striatum (RHES), which is selec- some 9 open reading frame 72 (C9ORF72) have been
tively expressed in the striatum, where HD pathology reported as a major genetic factor in patients with ALS
NATURE REVIEWS | NEUROSCIENCE VOLUME 16 | JUNE 2015 | 349
© 2015 Macmillan Publishers Limited. All rights reserved
REVIEWS
Multivesicular bodies and in patients with frontotemporal dementia (FTD). is disrupted, resulting in the inhibition of the early
A type of late endosome Recently, C9ORF72 has been suggested to have a stages of autophagosome formation and decreased
containing internal vesicles. role in endosomal trafficking, and it contains DENN α‑synuclein clearance75. The ATG9 mislocalization that
(differentially expressed in normal and neoplastic results from VPS35-D620N is reminiscent of that seen
Lewy bodies
Protein aggregates found
cells) domains, which are normally associated with to result from increased levels of α-synuclein77, the pro-
within neurons in patients with RABGEFs, activators of endocytic RAB proteins69. In tein that accumulates in Lewy bodies in PD. Increased
certain neurodegenerative neuronal cell lines, C9ORF72 colocalizes with several levels of α‑synuclein are sufficient to cause PD78, and
diseases, including Parkinson RAB proteins, and small interfering RNA (siRNA)- this protein has been shown to inhibit RAB1A79, lead-
disease and Lewy body
mediated knockdown of C9ORF72 inhibited shiga toxin ing to an alteration of ATG9 localization and decreased
dementia.
trafficking from the plasma membrane to the Golgi and autophagosome formation in cell culture and in vivo77.
endocytosis of tropomyosin-related kinase B (TRKB), The identification of the autophagy defect caused by
as well as increased the levels of LC3‑II70. However, the VPS35-D620N could be a mechanistic feature that
importance of these mechanisms in the pathogenesis of is shared by other neurodegenerative diseases. For
ALS is unclear. This is because mutations in C9ORF72 example, mutations in the gene encoding strumpellin
are found in non-coding regions, and it is considered (KIAA0196; a WASH complex subunit) have been iden-
that repeat associated non-ATG-mediated translation tified in some cases of HSP80, and mutations in the gene
(RAN) of arginine-rich dipeptides are the toxic entities encoding SWIP (also known as KIAA1033; another
in the case of this mutation71. WASH complex subunit) have been associated with
Mutations in charged multivesicular body pro- autosomal recessive intellectual disability 81. Moreover,
tein 2B (CHMP2B) can cause FTD72. CHMP2B is part of another gene mutated in PD, DNAJC13 (also known
the ESCRT-III (endosomal secretory complex required as RME8)82, encodes a protein that associates with the
for transport III) complex, and CHMP2B mutations WASH complex through binding to the same subunit as
result in disruption of this complex, causing defects in does VPS35 (REF. 80).
the endosome–lysosome pathway. Overexpression of Mutations in the 3ʹ untranslated region and the cod-
mutant CHMP2B has been demonstrated to result in ing region of sigma non-opioid intracellular receptor 1
the accumulation of autophagosomes, suggesting that (SIGMAR1) can cause forms of ALS and FTD83,84, and
their maturation is blocked73. This finding is also con- levels of SIGMAR1 are decreased in the spinal cord of
sistent with the role of ESCRT-III in the formation of patients with sporadic ALS85. Loss of Sigmar1 in mice
multivesicular bodies, which can fuse with autophago- results in motor deficits86, and treatment with a SIGMAR1
somes before the fusion of autophagosomes with agonist improves motor function and survival in a mutant
lysosomes. superoxide dismutase 1 (SOD1) ALS mouse model87.
VPS35 is a component of retromer, which mediates SIGMAR1 is a chaperone that is located at the ER–mito-
endosome-to‑Golgi trafficking (reviewed in REF. 74). chondria interface and has many functions, including
Retromer is also required for the endosomal recruit- a role in trafficking. Knockdown of SIGMAR1 impairs
ment of the actin nucleation-promoting WAS protein vesicle trafficking from the ER to the Golgi and results in a
family homologue (WASH) complex that is required for decrease in the fusion of autophagosomes with lysosomes
the formation of actin patches and efficient protein sort- and therefore a reduction in the degradation of autophagy
ing 75. Recently, the D620N substitution in VPS35 has substrates88.
been identified as causing autosomal dominant PD76,
and this mutation impairs binding of the WASH com- Lysosomal defects in neurodegenerative diseases.
plex to endosomes. As a consequence, ATG9 trafficking Lysosomal storage disorders (LSDs) are the most com-
mon neurodegenerative diseases of childhood and com-
prise more than 50 diseases. The clinical phenotypes
Box 2 | Chaperone-mediated autophagy of these diseases vary; however, they frequently show
Chaperone-mediated autophagy (CMA) is a form of lysosomal degradation in which progressive CNS defects. Because the final step in the
substrates are delivered directly to the lysosome rather than being trafficked via autophagic process is the fusion of autophagic vesicles
autophagosomes as occurs in macroautophagy. CMA substrates are recognized by a with lysosomes and the degradation of the contents of
pentapeptide motif based on the charge of the amino acids, allowing a motif to also be these autolysosomes, lysosomal defects are highly likely
generated by post-translational modifications. Proteins to be degraded are bound by to affect the autophagic capacity of the cell (reviewed in
the heat shock protein HSC70 and are targeted to the lysosome, where they interact REF. 89), both in terms of macroautophagy, as we discuss
with a multiprotein complex, which includes lysosomal-associated membrane
here, and in terms of chaperone-mediated autophagy
glycoprotein 2 (LAMP2). They are unfolded and translocated directly across the
(BOX 2). Although the defects causing LSDs can vary
lysosomal membrane. This process is not the focus of this Review and has been
reviewed elsewhere165–167; however, it is important to note that CMA dysfunction has widely from one type of LSD to another (LSDs may
also been implicated in the pathogenesis of neurodegenerative diseases. CMA is able to arise as a consequence of defects in lysosomal enzymes,
degrade proteins associated with neurodegeneration, such as α-synuclein168, lysosomal membrane-associated proteins or even non-
leucine-rich repeat serine/threonine-protein kinase 2 (LRRK2)169 and tau170, and lysosomal-associated enzymes), all cases studied to
disease-associated mutant versions of these proteins are less efficiently degraded by date show impaired autophagy, suggesting that this
CMA and in fact block the degradation of other substrates by CMA168,169. It is also is the common pathogenic mechanism in these dis-
important to note that the defects in lysosomal function outlined in this Review are eases. A LSD that has been widely studied in terms of
equally likely to affect CMA and macroautophagy and may thus contribute to its autophagic characteristics is Niemann–Pick disease
neurodegeneration by perturbation in CMA.
type C1 (BOX 3).
350 | JUNE 2015 | VOLUME 16 www.nature.com/reviews/neuro
© 2015 Macmillan Publishers Limited. All rights reserved
REVIEWS
Box 3 | Niemann–Pick disease type C1 — excessive or defective autophagy?
derived from patients with ATP13A2 mutations show
increased lysosomal pH and reduced processing of lyso-
The study of the role of autophagy in Niemann–Pick disease type C1 (NPC1) highlights somal proteases from their precursor to mature forms.
not only the difficulties associated with interpreting the contribution of autophagy This results in decreased protease activity 97 and an
function and dysfunction to a disease but also the challenges of understanding the increase in the number of autophagic vesicles owing to a
potential of autophagy modulation as a therapeutic approach. NPC1 is caused by
block in fusion with lysosomes. Mutations in presenilin 1
mutations in NPC1, which result in the loss of correct trafficking of cholesterol within
the cell and the accumulation of unesterified cholesterol and glycosphingolipids in
(PS1) in AD can also result in an increase in lysosomal
lysosomes and late endosomes (which would normally be trafficked on to the Golgi and pH owing to the role of the presenilin holoprotein (rather
endoplasmic reticulum for further processing). This mislocalization disrupts both than the cleaved form that is active in the γ‑secretase
lysosomes and endosomes, as well as other membrane compartments, which do not complex) in the glycosylation of the lysosomal v‑ATPase
receive the cholesterol they require for their correct membrane composition171. subunit V0a1, which results in decreased autophagic
A role for autophagy in NPC1 was first suggested after autophagosomes were found turnover 98,99. Although the exact mechanism that leads
to accumulate in degenerating Purkinje cells in mice with mutant NPC1 (REF. 172), and to this decrease in turnover is unclear 100,101, there does
autophagy was initially thought to be upregulated in this disease (reviewed in REF. 171). seem to be a consensus regarding the idea that PS1 has a
However, with improved knowledge of the autophagic pathway and how to measure role in autophagic clearance98,99,102,103.
autophagy activity, such as the use of tandem red fluorescent protein–GFP-tagged
TFEB enhances both lysosomal biogenesis and
microtubule-associated protein 1 light chain 3 (LC3)173, it has become clear that
autophagy is defective in this disease, leading to the proposal that autophagy was
autophagosome formation46,47. Mutant forms of the andro-
both induced and defective174,175. These studies suggested that treatment with either gen receptor, which cause the polyQ disorder spinobul-
cholesterol-depleting drugs (such as cyclodextrin) or autophagy inhibitors (such as bar muscular atrophy (SBMA; also known as Kennedy
3‑methyladenine) may be beneficial. Cyclodextrin was suggested to decrease the disease), interact with and inhibit TFEB, with conse-
accumulation of autophagosomes as it restored autophagic function175. However, more quent effects on the autophagy–lysosome pathway 104.
recent studies have argued against the evidence for any upregulation of autophagy in A role for altered TFEB activity has also been suggested
NPC1 (REFS 176–178), demonstrating that the increase in autophagic markers is solely a in PD because α‑synuclein has been reported to inter-
result of decreased maturation of autophagosomes. Furthermore, it was suggested that act with TFEB; in dopaminergic neurons from patients
cyclodextrin treatment in fact inhibits autophagy. A proposed therapeutic strategy for with PD, TFEB seems to be sequestered in the cytoplasm
this disease involved treatment with low-dose cyclodextrin to alleviate the cholesterol
(away from its target of action in the nucleus)105. In AD,
build‑up, along with autophagy inducers such as rapamycin177 or carbamazepine176.
enhanced levels of acid sphingomyelinase, one of a group
of sphingomyelin-metabolizing enzymes, have been
The LSD Gaucher disease is caused by homozygous shown in fibroblasts, brain and plasma of patients106.
mutations in glucocerebrosidase (GBA). Heterozygosity This increase in acid sphingomyelinase causes a decrease
for GBA mutations (Gaucher disease carrier status) is in TFEB levels. The genetic reduction of acid sphingo
the most common known genetic risk factor associated myelinase in heterozygous knockout mice, or pharma-
with PD90. Loss of GBA results in lysosomal dysfunction cological inhibition of this enzyme with amitriptyline,
owing to the accumulation of its substrate, glucocere- protected against disease development in the APP/PS1
broside. Mice lacking Gba have defective autophagy mouse model of AD, reducing the accumulation of LC3‑II
and accumulation of potential autophagy substrates and p62 that is observed in this model106.
in the brain, such as p62, monomeric and oligomeric Finally, two genes in which mutations have been iden-
forms of α‑synuclein, and ubiquitylated proteins, along tified in autosomal recessive HSP are implicated in the
with decreased mitochondrial function and decreased regeneration of lysosomes. The genes encode spastizin
mitophagy 91. Patients with sporadic PD have decreased (ZFYVE26) and spatacsin (SPG11), which act together in
levels of GBA in affected regions of the brain, along with a complex that is required for the initiation of lysosomal
increased levels of α-synuclein92,93. reformation. Loss or mutation of either gene results in a
Lysosomal membrane permeabilization (LMP) may decrease in lysosomal number and an accumulation of
also cause lysosomal dysfunction in LSDs (reviewed in autolyososomes107.
REF. 94). LMP leads to a release of cathepsins into the
cytoplasm, which has been associated with calpain acti- Autophagy receptors for aggregate-prone proteins. p62
vation and apoptotic cell death, and may also lead to a and other autophagy receptors are components of neu-
block in autophagy. For example, in Niemann–Pick dis- ronal protein aggregates in various neurodegenerative
ease type A, which is caused by mutations in the gene diseases33,108–110. p62 and LC3 were shown to colocalize
encoding acid sphingomyelinase, increases in sphingo- within a shell formed around mHTT aggregates in vitro,
myelin levels lead to LMP and a concomitant decrease and knockdown of p62 enhanced mHTT toxicity, provid-
in autophagosome degradation95. Although there is clear ing the first evidence for its role in the selective clearance
evidence for a defect in autophagy in LSDs, the specific of mHTT aggregates33. Indeed, in Drosophila melanogaster
contribution of autophagy defects versus lysosomal dys- models of neurodegeneration, loss of p62 exacerbates
function has not been parsed out. In addition to clas- the degeneration of the eye caused by overexpression
sical LSDs, it is now becoming evident that lysosomal of mHTT, a truncated form of ataxin 3 containing an
dysfunction may play a part in other neurodegenerative expanded polyQ repeat (MJDtr‑Q78; associated with
diseases. another polyQ disease, spinocerebellar ataxia type 3) or
Kufor–Rakeb syndrome and some early-onset forms TAR DNA-binding protein 43 (TDP43; associated with
of PD are associated with mutations in the gene encoding ALS)111. However, these observations have not trans-
lysosomal ATPase type 13A2 (ATP13A2)96. Fibroblasts lated simply into vertebrate models. In a mouse model
NATURE REVIEWS | NEUROSCIENCE VOLUME 16 | JUNE 2015 | 351
© 2015 Macmillan Publishers Limited. All rights reserved
REVIEWS
of SBMA in which a polyQ-expanded androgen recep- act as a scaffold for selective autophagy by interacting
tor was overexpressed, knockout of p62 enhanced the with p62 and facilitating its association with LC3 and
disease phenotype, whereas p62 overexpression was ubiquitylated substrates119. Wild-type HTT was also
protective112. However, p62 overexpression, rather than shown to be involved in autophagy initiation: domains
enhancing clearance of the mutant protein, converted it of the protein distinct from those shown to interact with
from a soluble to an insoluble form, thereby increasing p62 are able to interact with ULK1, which reduces the
the number of nuclear inclusions observed in the brain112. inhibitory interaction of ULK1 with mTOR and leads to
Furthermore, depletion of p62 in mouse models of HD autophagy activation119.
has been shown to ameliorate rather than enhance disease Mutations in the genes encoding p62 and another
signs113. Although the number of nuclear mHTT aggre- receptor protein, optineurin, have been associated with
gates was decreased in p62-knockout mice expressing ALS110,120, along with other diseases such as Paget dis-
mHTT, there was an increase in the levels of cytoplasmic ease of bone and open-angle glaucoma. The proposed
aggregates and no apparent change in total HTT levels in functions for p62 and optineurin in the clearance of
the brain113. aggregate-prone proteins suggest a clear pathogenic
Another autophagy receptor implicated in the clear- mechanism for forms of ALS; however, mutations in
ance of mHTT aggregates is ALFY, which co‑immuno the genes encoding p62 and optineurin are located
precipitates with p62, ATG5 and LC3 within mHTT throughout the genes, affecting multiple domains121.
aggregates in mammalian cells expressing exon 1 of HTT Although mutations affecting the ubiquitin-binding
or in fibroblasts from patients with HD38. Furthermore, or LC3‑interacting domain of optineurin have been
in mammalian cells expressing mHTT, knockdown demonstrated to inhibit its function as a receptor 122, it
and overexpression of ALFY led to an accumulation of has yet to be established whether mutations affecting
aggregates and a reduction in the number of aggregates, other regions of the proteins have the same functional
respectively, and similar effects were observed in vivo in a consequences.
D. melanogaster model of polyQ toxicity 38. Together, these
findings provide good functional evidence that ALFY Autophagy as a therapeutic target
plays a part in facilitating autophagic clearance of polyQ In recent years, numerous studies have demonstrated
protein aggregates. that the aggregate-prone proteins at the heart of neuro-
Recently, a new class of receptors, the Cue5–TOLLIP degenerative disease toxicity are autophagy substrates
proteins (CUET proteins; also known as CUE-domain and that pharmacological upregulators of autophagy
targeting adaptors), were identified in yeast from a can be beneficial in both cell and animal models of
screen for novel ubiquitin–Atg8 (LC3) interactors114. these diseases, in which they are able to reduce both
Of these, Cue5 has a putative mammalian homologue, intracytoplasmic aggregates and associated cell death
namely Toll-interacting protein (TOLLIP). TOLLIP (reviewed in REF. 123). However, understanding the
was observed to colocalize with LC3 in mammalian exact mechanisms by which autophagy may be com-
cells, and its overexpression enhanced the clearance of promised in neurodegeneration is vital in the quest
mHTT, suggesting that this protein and maybe other for therapeutics that act on the pathway. In the pres-
yet‑to‑be‑identified CUET homologues act as mam- ence of a defect, pharmacological upregulators acting
malian autophagy receptors. Although both p62 and upstream would not enhance aggregate-prone protein
CUET proteins contain ubiquitin-binding domains, clearance, and where autophagosome clearance is dis-
ubiquitylation is not the only signal for selective recog- rupted, enhancing formation may exacerbate rather
nition. p62 can also bind to non-ubiquitylated protein than ameliorate pathology. Increasing our knowledge
aggregates and target these for autophagic degrada- of the function and dysfunction of autophagy in neu-
tion115. In addition, NDP52, already known as a selec- rodegenerative disease will facilitate the design of
tive autophagy receptor from work in bacteria116, has therapeutic interventions that can bypass a block in the
recently been shown to co‑immunoprecipitate with autophagic pathway, should it exist. Achieving this goal
human tau through its SKICH domain. Although it is feasible given the diverse mechanisms of action of
contains a Lim‑L domain that is capable of binding the autophagy-modulating agents that have so far been
ubiquitylated targets, this domain was not required for identified and the existence of others for which the
its interaction with phosphorylated tau. NDP52 expres- mechanisms are not yet completely understood.
sion is upregulated in response to nuclear factor eryth- The mTOR inhibitor rapamycin was the first drug
roid 2‑related factor 2 (NRF2) activation, which leads to to be identified as an autophagy inducer and, as such,
enhanced clearance of phosphorylated tau both in vitro has been at the forefront of studies establishing the role
and in vivo, providing good evidence that NDP52 can of autophagy upregulation as a therapeutic strategy
mediate selective autophagic clearance of phosphorylated for neurodegeneration, along with more soluble ana-
tau in response to NRF2 activation117. logues (rapalogues) such as temsirolimus (previously
Another protein that has been shown to have a role known as CCI‑779)124–128. However, mTOR has diverse
as an autophagy receptor is HTT itself. In the presence autophagy-independent functions, and its inhibition
of mHTT, autophagosomes are able to form but seem has adverse effects in patients, including immuno
to lack content, suggesting a failure in the sequestration suppression and impaired wound healing. Efforts have
of substrates118. Further investigation of this phenom- therefore been made to identify mTOR-independent
enon led to the discovery that wild-type HTT is able to upregulators of autophagy.
352 | JUNE 2015 | VOLUME 16 www.nature.com/reviews/neuro
© 2015 Macmillan Publishers Limited. All rights reserved
REVIEWS
Several compounds have been identified that regu- The combined evidence from different compounds
late autophagy via the cAMP–EPAC (exchange fac- and different models of neurodegeneration strongly sup-
tor directly activated by cAMP 1)–phospholipase Cε port the idea that upregulation of autophagy is a valid
(PLCε)–inositol‑1,4,5‑trisphosphate (Ins(1,4,5)P3) path- therapeutic strategy for neurodegenerative disease.
way and the Ca2+–calpain–Gsα pathway129. One of these However, upregulating autophagosome biogenesis is
compounds, rilmenidine, which acts via Gi‑coupled imi- unlikely to be suitable or safe for all neurodegenerative
dazoline receptors, was subsequently shown to decrease diseases. For example, in diseases in which autophago-
aggregate load and disease signs in a transgenic mouse some degradation is slowed owing to lysosomal lesions,
model of HD130 and is now in safety trials in patients with increasing autophagosome formation will result in largely
this disease (European Clinical Trials Database number: unproductive formation of autophagosomes that are not
2009‑018119‑14). Several other drugs that act on these properly cleared and therefore a marked increase in
pathways have since been shown to be effective in mam- autophagosomes, which may be deleterious. It has been
malian models of neurodegeneration. Lithium acts to suggested that one approach to ameliorate lysosomal
induce autophagy by reducing Ins(1,4,5)P3 levels through function in some of these diseases is to enhance the
the inhibition of inositol monophosphatase131 and is activity of TFEB. Viral transduction of TFEB has dem-
protective in mouse models of tauopathy 132, whereas onstrated promising results in mouse models of LSDs140,
carbamazepine, which inhibits inositol synthesis, has PD105 and tauopathies141. Another strategy for the treat-
been shown to be protective in mouse models of AD133. ment of LSDs may be to reduce the activity of cystatins,
Additionally, inhibitors of calpain activation, such as which are endogenous inhibitors of lysosomal cathepsin
calpastatin, are able to promote the clearance of aggre- proteases. This strategy has also yielded promising results
gate-prone proteins by autophagy and are protective in in mouse models of AD142.
mouse and D. melanogaster models of HD and tauopa-
thy 134. Another mTOR-independent autophagy regula- Future challenges
tor, the disaccharide trehalose, acts through unknown As our understanding of the autophagic process
mechanisms to promote autophagy 135. Trehalose is increases, we are beginning to identify new areas that
neuroprotective in mouse models of tauopathy 136,137 and will be important to investigate in the quest to under-
prolongs lifespan in mouse models of ALS138,139. stand the role of autophagy in neurodegenerative dis-
ease (BOX 4). One of the major difficulties in studying
autophagic processes in the brain in vivo is to define
Box 4 | New concepts and areas for investigation flux on the basis of ‘snapshot’ data. For example, if
Glial autophagy a study finds that there are increased numbers of
Although much of the focus of the field so far has been on neuronal autophagy, recent autophagosomes in the brain in a mouse model or an
studies suggest that autophagy in glia may be similarly important in maintaining individual with a particular disease, this does not mean
neuronal health and in the pathogenesis of neurodegenerative diseases. Many that autophagy is increased. An increase in autophago-
neurological diseases are associated with inflammatory responses, and autophagy is some numbers could be due to increased formation
required for the maintenance of mitochondrial architecture during inflammation in (which can lead to increased delivery to lysosomes of
astrocytes179. Studies in the Long–Evans shaker rat, a model of demyelinating disease180, substrates) or could be due to impaired lysosomal deg-
show that autophagy can protect vulnerable oligodendrocytes. In humans, duplications
radation or trafficking of completed autophagosomes
of or point mutations in the gene encoding peripheral myelin protein 22 (PMP22) in
Schwann cells cause the progressive demyelinating disease Charcot–Marie–Tooth
(as occurs in LSDs). In mice, at least, good progress has
disease type 1A (CMT1A). The levels of the aberrant PMP22 and Schwann cell health been made in adapting methods to differentiate between
appear to be regulated by autophagy in mouse models of CMT1A, and autophagy these scenarios. Hetz and colleagues143 performed intra-
upregulation may be a suitable strategy to consider for this class of diseases181. ventricular injections of adenoviruses encoding mono-
In lysosomal storage disorders, astrocytic autophagy may be important for neuronal meric tandem mCherry–GFP–LC3, which were then
health. Astrocyte-specific loss of the enzyme impaired in multiple sulfatase deficiency expressed in central and peripheral neurons. Before
causes a defect in autophagosome maturation. As the ability of these astrocytes to lysosome fusion, the LC3 vesicles were autophago-
support normal neurons is compromised, it is interesting to speculate whether this non- somes and exhibited both red and green fluorescence,
cell-autonomous mechanism can be partially attributed to the autophagy defect182. but after fusion, the vesicles were autolysosomes and
Autophagy and secretion of proteins exhibited red fluorescence only (as GFP was more rap-
Recent studies have highlighted the ways in which autophagy may regulate various idly quenched in the acidic environment). Assessing the
secretory processes183. This concept may be of relevance to neurodegenerative diseases, numbers of the two types (colours) of vesicles enabled a
particularly those in which cell‑to‑cell spreading of toxic proteins such as tau and
more reliable assessment of autophagic flux.
α‑synuclein have been implicated184. However, the current status of this field is complex.
In Parkinson disease, it seems that lysosomal impairment or defective autophagosome–
Another important issue relates to the interpretation
lysosome fusion causes increased exosomal α‑synuclein release, which can be of whether autophagy is causing cell death in certain
reconciled with the resulting increased pool of autophagosomes185–187. However, in the diseases in which increased numbers of autophago-
context of Alzhiemer disease, the situation appears to be different. In mouse studies, the somes are observed. First, one needs to know whether
secretion of amyloid‑β and the extracellular plaque load were reduced when autophagy there is increased formation of autophagosomes or
was blocked by deletion of Atg7 in relevant neurons. However, the authors suggest that decreased degradation. If there is increased formation,
this was associated with increased intracellular amyloid‑β levels and enhanced then one needs to use a number of genetic manipu-
pathology188. This study reiterates the possibility that intracellular amyloid‑β may be a lations of autophagy genes to perturb autophagy in
major toxic entity. However, it is important to note that in all these cases the secretory– order to test whether the increased autophagy is caus-
excretory route has not been precisely defined189.
ally involved in the toxic process. This is preferable to
NATURE REVIEWS | NEUROSCIENCE VOLUME 16 | JUNE 2015 | 353
© 2015 Macmillan Publishers Limited. All rights reserved
REVIEWS
chemical strategies because all the drugs currently used will not only be helpful for understanding disease patho-
to inhibit (or induce) autophagy have off-target effects. genesis but also serve as a powerful tool for monitoring
One also needs to consider that manipulations of some target engagement in therapeutic trials.
autophagy genes may have consequences unrelated to
autophagy (for example, beclin 1 indirectly regulates p53 Conclusions
levels144). Recent data suggest additional non-autophagy There are now substantial data showing how autophagy
roles of beclin 1 in retromer trafficking and phagocytosis may be compromised in various neurodegenerative
of amyloid‑β in microglia, and this appears to be disease- diseases and extensive preclinical support for the use of
relevant because reduced beclin 1 and retromer levels autophagy inducers in certain neurodegenerative dis-
have been observed in AD brains145. ease models. Further understanding of the basic biology
These challenges are difficult enough to negotiate in of autophagy will provide additional insights into how
cell culture and mouse experiments. However, ultimately, disease-causing protein variants may affect this critical
we need to understand human diseases, many of which degradation pathway. Similarly, further drug discovery
are complex and cannot be faithfully modelled in animals. efforts coupled with the development of relevant bio-
Thus, a major challenge for the future will be to develop markers will facilitate the testing of whether autophagy
markers that enable inferences regarding autophagic flux induction can affect the genesis or progression of some
in vivo and in post-mortem samples. Such new methods neurodegenerative diseases.
1. Imarisio, S. et al. Huntington’s disease: from 17. Hailey, D. W. et al. Mitochondria supply membranes 34. Kirkin, V. et al. A role for NBR1 in autophagosomal
pathology and genetics to potential therapies. for autophagosome biogenesis during starvation. degradation of ubiquitinated substrates. Mol. Cell 33,
Biochem. J. 412, 191–209 (2008). Cell 141, 656–667 (2010). 505–516 (2009).
2. Rubinsztein, D. C. The roles of intracellular protein- 18. Puri, C., Renna, M., Bento, C. F., Moreau, K. & 35. Pankiv, S. et al. p62/SQSTM1 binds directly to Atg8/
degradation pathways in neurodegeneration. Nature Rubinsztein, D. C. Diverse autophagosome membrane LC3 to facilitate degradation of ubiquitinated protein
443, 780–786 (2006). sources coalesce in recycling endosomes. aggregates by autophagy. J. Biol. Chem. 282,
3. Tsvetkov, A. S. et al. Proteostasis of polyglutamine Cell 154, 1285–1299 (2013). 24131–24145 (2007).
varies among neurons and predicts 19. Kabeya, Y. et al. LC3, a mammalian homologue of 36. Rogov, V., Dotsch, V., Johansen, T. & Kirkin, V.
neurodegeneration. Nature Chem. Biol. 9, 586–592 yeast Apg8p, is localized in autophagosome Interactions between autophagy receptors and
(2013). membranes after processing. EMBO J. 19, ubiquitin-like proteins form the molecular basis for
4. Hara, T. et al. Suppression of basal autophagy in 5720–5728 (2000). selective autophagy. Mol. Cell 53, 167–178 (2014).
neural cells causes neurodegenerative disease in mice. 20. Ravikumar, B. et al. Dynein mutations impair 37. Simonsen, A. et al. Alfy, a novel FYVE-domain-
Nature 441, 885–889 (2006). autophagic clearance of aggregate-prone proteins. containing protein associated with protein granules
5. Komatsu, M. et al. Loss of autophagy in the central Nature Genet. 37, 771–776 (2005). and autophagic membranes. J. Cell Sci. 117,
nervous system causes neurodegeneration in mice. 21. Moreau, K., Ravikumar, B., Renna, M., Puri, C. & 4239–4251 (2004).
Nature 441, 880–884 (2006). Rubinsztein, D. C. Autophagosome precursor 38. Filimonenko, M. et al. The selective macroautophagic
References 4 and 5 were the first to demonstrate maturation requires homotypic fusion. Cell 146, degradation of aggregated proteins requires the
the importance of autophagy for neuronal health 303–317 (2011). PI3P‑binding protein Alfy. Mol. Cell 38, 265–279 (2010).
(knockout of Atg5 or Atg7 in neurons resulted in a 22. Fader, C. M., Sanchez, D. G., Mestre, M. B. & 39. Clausen, T. H. et al. p62/SQSTM1 and ALFY interact
neurodegenerative phenotype in mice). Colombo, M. I. TI‑VAMP/VAMP7 and VAMP3/ to facilitate the formation of p62 bodies/ALIS and
6. Kim, I. & Lemasters, J. J. Mitophagy selectively cellubrevin: two v‑SNARE proteins involved in their degradation by autophagy. Autophagy 6,
degrades individual damaged mitochondria after specific steps of the autophagy/multivesicular body 330–344 (2010).
photoirradiation. Antioxid. Redox Signal. 14, pathways. Biochim. Biophys. Acta 1793, 40. Novak, I. et al. Nix is a selective autophagy receptor
1919–1928 (2011). 1901–1916 (2009). for mitochondrial clearance. EMBO Rep. 11, 45–51
7. Boya, P. et al. Inhibition of macroautophagy triggers 23. Furuta, N. & Amano, A. Cellular machinery to fuse (2010).
apoptosis. Mol. Cell. Biol. 25, 1025–1040 (2005). antimicrobial autophagosome with lysosome. 41. Schwarten, M. et al. Nix directly binds to GABARAP: a
8. Ravikumar, B., Berger, Z., Vacher, C., O’Kane, C. J. & Commun. Integr. Biol. 3, 385–387 (2010). possible crosstalk between apoptosis and autophagy.
Rubinsztein, D. C. Rapamycin pre-treatment protects 24. Alers, S., Loffler, A. S., Wesselborg, S. & Stork, B. Role Autophagy 5, 690–698 (2009).
against apoptosis. Hum. Mol. Genet. 15, 1209–1216 of AMPK–mTOR–Ulk1/2 in the regulation of 42. Shen, H. M. & Mizushima, N. At the end of the
(2006). autophagy: cross talk, shortcuts, and feedbacks. Mol. autophagic road: an emerging understanding of
9. Korolchuk, V. I., Mansilla, A., Menzies, F. M. & Cell. Biol. 32, 2–11 (2012). lysosomal functions in autophagy. Trends Biochem.
Rubinsztein, D. C. Autophagy inhibition compromises 25. Fullgrabe, J., Klionsky, D. J. & Joseph, B. The return of Sci. 39, 61–71 (2014).
degradation of ubiquitin–proteasome pathway the nucleus: transcriptional and epigenetic control of 43. Wong, Y. C. & Holzbaur, E. L. The regulation of
substrates. Mol. Cell 33, 517–527 (2009). autophagy. Nature Rev. Mol. Cell Biol. 15, 65–74 autophagosome dynamics by huntingtin and HAP1 is
10. Tsukada, M. & Ohsumi, Y. Isolation and (2014). disrupted by expression of mutant huntingtin, leading
characterization of autophagy-defective mutants of 26. Morselli, E. et al. p53 inhibits autophagy by to defective cargo degradation. J. Neurosci.
Saccharomyces cerevisiae. FEBS Lett. 333, 169–174 interacting with the human ortholog of yeast Atg17, 34, 1293–1305 (2014).
(1993). RB1CC1/FIP200. Cell Cycle 10, 2763–2769 (2011). 44. Moreau, K., Renna, M. & Rubinsztein, D. C.
11. Mizushima, N., Levine, B., Cuervo, A. M. & 27. Russell, R. C. et al. ULK1 induces autophagy by Connections between SNAREs and autophagy. Trends
Klionsky, D. J. Autophagy fights disease through cellular phosphorylating Beclin‑1 and activating VPS34 lipid Biochem. Sci. 38, 57–63 (2013).
self-digestion. Nature 451, 1069–1075 (2008). kinase. Nature Cell Biol. 15, 741–750 (2013). 45. Yu, L. et al. Termination of autophagy and reformation
12. Ravikumar, B., Moreau, K., Jahreiss, L., Puri, C. & 28. Dooley, H. C. et al. WIPI2 links LC3 conjugation with of lysosomes regulated by mTOR. Nature 465,
Rubinsztein, D. C. Plasma membrane contributes to PI3P, autophagosome formation, and pathogen 942–946 (2010).
the formation of pre-autophagosomal structures. clearance by recruiting Atg12‑5‑16L1. Mol. Cell 55, 46. Sardiello, M. et al. A gene network regulating lysosomal
Nature Cell Biol. 12, 747–757 (2010). 238–252 (2014). biogenesis and function. Science 325, 473–477 (2009).
13. Hayashi-Nishino, M. et al. A subdomain of the 29. Mack, H. I., Zheng, B., Asara, J. M. & Thomas, S. M. 47. Settembre, C. et al. TFEB links autophagy to lysosomal
endoplasmic reticulum forms a cradle for AMPK-dependent phosphorylation of ULK1 biogenesis. Science 332, 1429–1433 (2011).
autophagosome formation. Nature Cell regulates ATG9 localization. Autophagy 8, 48. Frake, R. A., Ricketts, T., Menzies, F. M. &
Biol. 11, 1433–1437 (2009). 1197–1214 (2012). Rubinsztein, D. C. Autophagy and neurodegeneration.
14. Yla-Anttila, P., Vihinen, H., Jokitalo, E. & 30. Papinski, D. et al. Early steps in autophagy depend on J. Clin. Invest. 125, 65–75 (2015).
Eskelinen, E. L. 3D tomography reveals connections direct phosphorylation of Atg9 by the Atg1 kinase. 49. Haack, T. B., Hogarth, P., Gregory, A., Prokisch, H. &
between the phagophore and endoplasmic reticulum. Mol. Cell 53, 471–483 (2014). Hayflick, S. J. BPAN: the only X‑linked dominant NBIA
Autophagy 5, 1180–1185 (2009). 31. Vicinanza, M. et al. PI(5)P regulates autophagosome disorder. Int. Rev. Neurobiol. 110, 85–90 (2013).
15. van der Vaart, A., Griffith, J. & Reggiori, F. Exit from biogenesis. Mol. Cell 57, 219–234 (2015). 50. Saitsu, H. et al. De novo mutations in the autophagy
the Golgi is required for the expansion of the 32. Stolz, A., Ernst, A. & Dikic, I. Cargo recognition and gene WDR45 cause static encephalopathy of
autophagosomal phagophore in yeast Saccharomyces trafficking in selective autophagy. Nature Cell Biol. 16, childhood with neurodegeneration in adulthood.
cerevisiae. Mol. Biol. Cell 21, 2270–2284 (2010). 495–501 (2014). Nature Genet. 45, 445–449 (2013).
16. Yen, W. L. et al. The conserved oligomeric Golgi 33. Bjorkoy, G. et al. p62/SQSTM1 forms protein This paper shows that static encephalopathy of
complex is involved in double-membrane vesicle aggregates degraded by autophagy and has a childhood with neurodegeneration in adulthood
formation during autophagy. J. Cell Biol. 188, protective effect on huntingtin-induced cell death. (SENDA; also known as BPAN) results from
101–114 (2010). J. Cell Biol. 171, 603–614 (2005). mutations in WDR45.
354 | JUNE 2015 | VOLUME 16 www.nature.com/reviews/neuro
© 2015 Macmillan Publishers Limited. All rights reserved
REVIEWS
51. Orsi, A. et al. Dynamic and transient interactions of 73. Lee, J. A., Beigneux, A., Ahmad, S. T., Young, S. G. & 96. Ramirez, A. et al. Hereditary parkinsonism with
Atg9 with autophagosomes, but not membrane Gao, F. B. ESCRT-III dysfunction causes autophagosome dementia is caused by mutations in ATP13A2,
integration, are required for autophagy. Mol. Biol. Cell accumulation and neurodegeneration. Curr. encoding a lysosomal type 5 P‑type ATPase. Nature
23, 1860–1873 (2012). Biol. 17, 1561–1567 (2007). Genet. 38, 1184–1191 (2006).
52. Metzger, S. et al. Age at onset in Huntington’s disease 74. Seaman, M. N. The retromer complex — endosomal 97. Dehay, B. et al. Loss of P‑type ATPase ATP13A2/
is modified by the autophagy pathway: implication of protein recycling and beyond. J. Cell Sci. 125, PARK9 function induces general lysosomal deficiency
the V471A polymorphism in Atg7. Hum. Genet. 128, 4693–4702 (2012). and leads to Parkinson disease neurodegeneration.
453–459 (2010). 75. Zavodszky, E. et al. Mutation in VPS35 associated with Proc. Natl Acad. Sci. USA 109, 9611–9616 (2012).
53. Metzger, S. et al. The V471A polymorphism in Parkinson’s disease impairs WASH complex 98. Lee, J. H. et al. Lysosomal proteolysis and autophagy
autophagy-related gene ATG7 modifies age at onset association and inhibits autophagy. Nature Commun. require presenilin 1 and are disrupted by Alzheimer-
specifically in Italian Huntington disease patients. 5, 3828 (2014). related PS1 mutations. Cell 141, 1146–1158 (2010).
PLoS ONE 8, e68951 (2013). 76. Zimprich, A. et al. A mutation in VPS35, encoding a 99. Avrahami, L. et al. Inhibition of glycogen synthase
54. Yan, J. Q. et al. Overexpression of human E46K subunit of the retromer complex, causes late-onset kinase‑3 ameliorates β-amyloid pathology and
mutant α-synuclein impairs macroautophagy via Parkinson disease. Am. J. Hum. Genet. 89, 168–175 restores lysosomal acidification and mammalian target
inactivation of JNK1–Bcl‑2 pathway. Mol. Neurobiol. (2011). of rapamycin activity in the Alzheimer disease mouse
50, 685–701 (2014). 77. Winslow, A. R. et al. α-synuclein impairs model: in vivo and in vitro studies. J. Biol. Chem.
55. Subramaniam, S., Sixt, K. M., Barrow, R. & macroautophagy: implications for Parkinson’s disease. 288, 1295–1306 (2013).
Snyder, S. H. Rhes, a striatal specific protein, mediates J. Cell Biol. 190, 1023–1037 (2010). 100. Zhang, X. et al. A role for presenilins in autophagy
mutant-huntingtin cytotoxicity. Science 324, 78. Singleton, A. B. et al. α-synuclein locus triplication revisited: normal acidification of lysosomes in cells
1327–1330 (2009). causes Parkinson’s disease. Science 302, 841 (2003). lacking PSEN1 and PSEN2. J. Neurosci. 32,
56. Mealer, R. G., Murray, A. J., Shahani, N., 79. Cooper, A. A. et al. α-synuclein blocks ER–Golgi traffic 8633–8648 (2012).
Subramaniam, S. & Snyder, S. H. Rhes, a striatal- and Rab1 rescues neuron loss in Parkinson’s models. 101. Coen, K. et al. Lysosomal calcium homeostasis defects,
selective protein implicated in Huntington disease, Science 313, 324–328 (2006). not proton pump defects, cause endo-lysosomal
binds beclin‑1 and activates autophagy. J. Biol. Chem. 80. Freeman, C., Seaman, M. N. & Reid, E. The hereditary dysfunction in PSEN-deficient cells. J. Cell Biol. 198,
289, 3547–3554 (2014). spastic paraplegia protein strumpellin: 23–35 (2012).
The results from this paper suggest a possible characterisation in neurons and of the effect of disease 102. Wilson, C. A. et al. Degradative organelles containing
mechanism for the selective vulnerability of striatal mutations on WASH complex assembly and function. mislocalized α- and β-synuclein proliferate in
cells in HD. Biochim. Biophys. Acta 1832, 160–173 (2013). presenilin‑1 null neurons. J. Cell Biol. 165, 335–346
57. Sagona, A. P. et al. A tumor-associated mutation of 81. Ropers, F. et al. Identification of a novel candidate (2004).
FYVE-CENT prevents its interaction with Beclin 1 and gene for non-syndromic autosomal recessive 103. Neely, K. M., Green, K. N. & LaFerla, F. M. Presenilin is
interferes with cytokinesis. PLoS ONE 6, e17086 intellectual disability: the WASH complex member necessary for efficient proteolysis through the
(2011). SWIP. Hum. Mol. Genet. 20, 2585–2590 (2011). autophagy-lysosome system in a γ-secretase-
58. Vantaggiato, C. et al. Defective autophagy in spastizin 82. Vilarino-Guell, C. et al. DNAJC13 mutations in independent manner. J. Neurosci. 31, 2781–2791
mutated patients with hereditary spastic paraparesis Parkinson disease. Hum. Mol. Genet. 23, 1794–1801 (2011).
type 15. Brain 136, 3119–3139 (2013). (2014). 104. Cortes, C. J. et al. Polyglutamine-expanded androgen
59. Harold, D. et al. Genome-wide association study 83. Al‑Saif, A., Al‑Mohanna, F. & Bohlega, S. A mutation in receptor interferes with TFEB to elicit autophagy
identifies variants at CLU and PICALM associated with sigma‑1 receptor causes juvenile amyotrophic lateral defects in SBMA. Nature Neurosci. 17, 1180–1189
Alzheimer’s disease. Nature Genet. 41, 1088–1093 sclerosis. Ann. Neurol. 70, 913–919 (2011). (2014).
(2009). 84. Luty, A. A. et al. Sigma nonopioid intracellular 105. Decressac, M. et al. TFEB-mediated autophagy
60. Jun, G. et al. Meta-analysis confirms CR1, CLU, and receptor 1 mutations cause frontotemporal lobar rescues midbrain dopamine neurons from α-synuclein
PICALM as Alzheimer disease risk loci and reveals degeneration–motor neuron disease. Ann. Neurol. 68, toxicity. Proc. Natl Acad. Sci. USA 110,
interactions with APOE genotypes. Arch. Neurol. 639–649 (2010). E1817–E1826 (2013).
67, 1473–1484 (2010). 85. Prause, J. et al. Altered localization, abnormal This study shows that overexpression of α‑synuclein
61. Ando, K. et al. Clathrin adaptor CALM/PICALM is modification and loss of function of Sigma receptor‑1 in rat midbrain results in a mislocalization of TFEB
associated with neurofibrillary tangles and is cleaved in amyotrophic lateral sclerosis. Hum. Mol. Genet. and the degeneration of dopaminergic neurons.
in Alzheimer’s brains. Acta Neuropathol. 125, 22, 1581–1600 (2013). This degeneration could be rescued by inducing
861–878 (2013). 86. Mavlyutov, T. A., Epstein, M. L., Andersen, K. A., autophagy via overexpression of TFEB or treatment
62. Moreau, K. et al. PICALM modulates autophagy Ziskind-Conhaim, L. & Ruoho, A. E. The sigma‑1 with the rapamycin analogue CCI‑779.
activity and tau accumulation. Nature Commun. 5, receptor is enriched in postsynaptic sites of C‑terminals 106. Lee, J. K. et al. Acid sphingomyelinase modulates the
4998 (2014). in mouse motoneurons. An anatomical and behavioral autophagic process by controlling lysosomal
63. Szatmari, Z. & Sass, M. The autophagic roles of Rab study. Neuroscience 167, 247–255 (2010). biogenesis in Alzheimer’s disease. J. Exp. Med.
small GTPases and their upstream regulators: a 87. Mancuso, R. et al. Sigma‑1R agonist improves motor 211, 1551–1570 (2014).
review. Autophagy 10, 1154–1166 (2014). function and motoneuron survival in ALS mice. 107. Chang, J., Lee, S. & Blackstone, C. Spastic paraplegia
64. Verhoeven, K. et al. Mutations in the small GTP-ase Neurotherapeutics 9, 814–826 (2012). proteins spastizin and spatacsin mediate autophagic
late endosomal protein RAB7 cause Charcot–Marie– 88. Vollrath, J. T. et al. Loss of function of the ALS protein lysosome reformation. J. Clin. Invest. 124,
Tooth type 2B neuropathy. Am. J. Hum. Genet. 72, SigR1 leads to ER pathology associated with defective 5249–5262 (2014).
722–727 (2003). autophagy and lipid raft disturbances. Cell Death Dis. This paper presents a newly identified process in
65. Yang, Y. et al. The gene encoding alsin, a protein with 5, e1290 (2014). autophagy, in which lysosomes are replenished,
three guanine-nucleotide exchange factor domains, is 89. Lieberman, A. P. et al. Autophagy in lysosomal storage involving two proteins in which mutations have
mutated in a form of recessive amyotrophic lateral disorders. Autophagy 8, 719–730 (2012). been identified in HSP.
sclerosis. Nature Genet. 29, 160–165 (2001). 90. Swan, M. & Saunders-Pullman, R. The association 108. Zatloukal, K. et al. p62 is a common component of
66. Topp, J. D., Gray, N. W., Gerard, R. D. & between β‑glucocerebrosidase mutations and cytoplasmic inclusions in protein aggregation diseases.
Horazdovsky, B. F. Alsin is a Rab5 and Rac1 guanine parkinsonism. Curr. Neurol. Neurosci. Rep. 13, 368 Am. J. Pathol. 160, 255–263 (2002).
nucleotide exchange factor. J. Biol. Chem. 279, (2013). 109. Mori, F. et al. Optineurin immunoreactivity in neuronal
24612–24623 (2004). 91. Osellame, L. D. et al. Mitochondria and quality control nuclear inclusions of polyglutamine diseases
67. Ravikumar, B., Imarisio, S., Sarkar, S., O’Kane, C. J. & defects in a mouse model of Gaucher disease — links (Huntington’s, DRPLA, SCA2, SCA3) and intranuclear
Rubinsztein, D. C. Rab5 modulates aggregation and to Parkinson’s disease. Cell. Metabolism 17, 941–953 inclusion body disease. Acta Neuropathol. 123,
toxicity of mutant huntingtin through macroautophagy (2013). 747–749 (2012).
in cell and fly models of Huntington disease. J. Cell 92. Mazzulli, J. R. et al. Gaucher disease 110. Maruyama, H. et al. Mutations of optineurin in
Sci. 121, 1649–1660 (2008). glucocerebrosidase and α-synuclein form a amyotrophic lateral sclerosis. Nature 465, 223–226
68. Otomo, A., Kunita, R., Suzuki-Utsunomiya, K., bidirectional pathogenic loop in synucleinopathies. (2010).
Ikeda, J. E. & Hadano, S. Defective relocalization of Cell 146, 37–52 (2011). 111. Saitoh, Y. et al. p62 plays a protective role in the
ALS2/alsin missense mutants to Rac1‑induced This paper identifies the molecular link between PD autophagic degradation of polyglutamine protein
macropinosomes accounts for loss of their cellular and heterozygous mutations in GBA. oligomers in polyglutamine disease model flies. J. Biol.
function and leads to disturbed amphisome formation. Glucosylceramide, which accumulates in Gaucher Chem. 290, 1442–1453 (2015).
FEBS Lett. 585, 730–736 (2011). disease caused by homozygous mutations in GBA, 112. Doi, H. et al. p62/SQSTM1 differentially removes the
69. Levine, T. P., Daniels, R. D., Gatta, A. T., Wong, L. H. & compromises lysosomal function and leads to an toxic mutant androgen receptor via autophagy and
Hayes, M. J. The product of C9orf72, a gene strongly accumulation of α‑synuclein; conversely, α‑synuclein inclusion formation in a spinal and bulbar muscular
implicated in neurodegeneration, is structurally inhibits GBA, resulting in an increase in atrophy mouse model. J. Neurosci. 33, 7710–7727
related to DENN Rab-GEFs. Bioinformatics 29, glucosylceramide. (2013).
499–503 (2013). 93. Murphy, K. E. et al. Reduced glucocerebrosidase is 113. Kurosawa, M. et al. Depletion of p62 reduces nuclear
70. Farg, M. A. et al. C9ORF72, implicated in amytrophic associated with increased α-synuclein in sporadic inclusions and paradoxically ameliorates disease
lateral sclerosis and frontotemporal dementia, Parkinson’s disease. Brain 137, 834–848 (2014). phenotypes in Huntington’s model mice. Hum. Mol.
regulates endosomal trafficking. Hum. Mol. Genet. 23, 94. Boya, P. & Kroemer, G. Lysosomal membrane Genet. 24, 1092–1105 (2014).
3579–3595 (2014). permeabilization in cell death. Oncogene 27, 114. Lu, K., Psakhye, I. & Jentsch, S. Autophagic clearance
71. Mizielinska, S. et al. C9orf72 repeat expansions cause 6434–6451 (2008). of polyQ proteins mediated by ubiquitin‑Atg8
neurodegeneration in Drosophila through arginine-rich 95. Gabande-Rodriguez, E., Boya, P., Labrador, V., adaptors of the conserved CUET protein family.
proteins. Science 345,1192–1194 (2014). Dotti, C. G. & Ledesma, M. D. High sphingomyelin Cell 158, 549–563 (2014).
72. Skibinski, G. et al. Mutations in the endosomal levels induce lysosomal damage and autophagy This paper describes an entirely new class of
ESCRTIII-complex subunit CHMP2B in frontotemporal dysfunction in Niemann Pick disease type A. Cell autophagy receptor proteins that have a specific
dementia. Nature Genet. 37, 806–808 (2005). Death Differ. 21, 864–875 (2014). role in the clearance of aggregate-prone proteins.
NATURE REVIEWS | NEUROSCIENCE VOLUME 16 | JUNE 2015 | 355
© 2015 Macmillan Publishers Limited. All rights reserved
REVIEWS
115. Watanabe, Y. & Tanaka, M. p62/SQSTM1 in 137. Schaeffer, V. et al. Stimulation of autophagy reduces 160. Ashrafi, G., Schlehe, J. S., LaVoie, M. J. &
autophagic clearance of a non-ubiquitylated neurodegeneration in a mouse model of human Schwarz, T. L. Mitophagy of damaged mitochondria
substrate. J. Cell Sci. 124, 2692–2701 (2011). tauopathy. Brain 135, 2169–2177 (2012). occurs locally in distal neuronal axons and requires
116. Thurston, T. L., Ryzhakov, G., Bloor, S., von 138. Castillo, K. et al. Trehalose delays the progression of PINK1 and Parkin. J. Cell Biol. 206, 655–670 (2014).
Muhlinen, N. & Randow, F. The TBK1 adaptor and amyotrophic lateral sclerosis by enhancing 161. Chu, C. T. et al. Cardiolipin externalization to the outer
autophagy receptor NDP52 restricts the proliferation autophagy in motoneurons. Autophagy 9, mitochondrial membrane acts as an elimination signal
of ubiquitin-coated bacteria. Nature 1308–1320 (2013). for mitophagy in neuronal cells. Nature Cell
Immunol. 10, 1215–1221 (2009). 139. Zhang, X. et al. MTOR-independent, autophagic Biol. 15, 1197–1205 (2013).
117. Jo, C. et al. Nrf2 reduces levels of phosphorylated enhancer trehalose prolongs motor neuron survival This paper describes an alternative mitophagy
tau protein by inducing autophagy adaptor protein and ameliorates the autophagic flux defect in a activation signal differing from that involving Parkin
NDP52. Nature Commun. 5, 3496 (2014). mouse model of amyotrophic lateral sclerosis. and PINK1, in which cardiolipin, a lipid normally
118. Martinez-Vicente, M. et al. Cargo recognition failure Autophagy 10, 588–602 (2014). localized to the mitochondrial inner membrane, is
is responsible for inefficient autophagy in 140. Medina, D. L. et al. Transcriptional activation of externalized.
Huntington’s disease. Nature Neurosci. 13, lysosomal exocytosis promotes cellular clearance. Dev. 162. Do, C. B. et al. Web-based genome-wide association
567–576 (2010). Cell 21, 421–430 (2011). study identifies two novel loci and a substantial
119. Rui, Y. N. et al. Huntingtin functions as a scaffold for This study demonstrates that TFEB can promote genetic component for Parkinson’s disease. PLoS
selective macroautophagy. Nature Cell Biol. 17, fusion of lysosomes with the plasma membrane Genet. 7, e1002141 (2011).
262–275 (2015). and the release of their contents. This process is 163. Ivatt, R. M. et al. Genome-wide RNAi screen identifies
120. Fecto, F. et al. SQSTM1 mutations in familial and protective in mouse models of the lysosomal the Parkinson disease GWAS risk locus SREBF1 as a
sporadic amyotrophic lateral sclerosis. Arch. Neurol. storage disorder multiple sulfatase deficiency. regulator of mitophagy. Proc. Natl Acad. Sci. USA 111,
68, 1440–1446 (2011). 141. Polito, V. A. et al. Selective clearance of aberrant tau 8494–8499 (2014).
121. Teyssou, E. et al. Mutations in SQSTM1 encoding p62 proteins and rescue of neurotoxicity by transcription 164. Fang, E. F. et al. Defective mitophagy in XPA via
in amyotrophic lateral sclerosis: genetics and factor EB. EMBO Mol. Med. 6, 1142–1160 (2014). PARP‑1 hyperactivation and NAD+/SIRT1 reduction.
neuropathology. Acta Neuropathol. 125, 511–522 142. Yang, D. S. et al. Reversal of autophagy dysfunction in Cell 157, 882–896 (2014).
(2013). the TgCRND8 mouse model of Alzheimer’s disease 165. Cuervo, A. M. & Wong, E. Chaperone-mediated
122. Wong, Y. C. & Holzbaur, E. L. Optineurin is an ameliorates amyloid pathologies and memory deficits. autophagy: roles in disease and aging. Cell Res. 24,
autophagy receptor for damaged mitochondria in Brain 134, 258–277 (2011). 92–104 (2014).
parkin-mediated mitophagy that is disrupted by an 143. Castillo, K. et al. Measurement of autophagy flux in 166. Wang, G. & Mao, Z. Chaperone-mediated autophagy:
ALS-linked mutation. Proc. Natl Acad. Sci. USA 111, the nervous system in vivo. Cell Death Dis. 4, e917 roles in neurodegeneration. Transl. Neurodegener.
E4439–E4448 (2014). (2013). 3, 20 (2014).
123. Harris, H. & Rubinsztein, D. C. Control of autophagy 144. Liu, J. et al. Beclin1 controls the levels of p53 by 167. Xilouri, M. & Stefanis, L. Chaperone mediated
as a therapy for neurodegenerative disease. Nature regulating the deubiquitination activity of USP10 and autophagy to the rescue: a new-fangled target for the
Rev. Neurol. 8, 108–117 (2012). USP13. Cell 147, 223–234 (2011). treatment of neurodegenerative diseases. Mol. Cell.
124. Rodriguez-Muela, N., Germain, F., Marino, G., 145. Lucin, K. M. et al. Microglial beclin 1 regulates Neurosci. http://dx.doi.org/10.1016/j.
Fitze, P. S. & Boya, P. Autophagy promotes survival of retromer trafficking and phagocytosis and is mcn.2015.01.003 (2015).
retinal ganglion cells after optic nerve axotomy in impaired in Alzheimer’s disease. Neuron 79, 168. Cuervo, A. M., Stefanis, L., Fredenburg, R.,
mice. Cell Death Differ. 19, 162–169 (2012). 873–886 (2013). Lansbury, P. T. & Sulzer, D. Impaired degradation of
125. Ravikumar, B. et al. Inhibition of mTOR induces 146. Clark, I. E. et al. Drosophila pink1 is required for mutant α-synuclein by chaperone-mediated
autophagy and reduces toxicity of polyglutamine mitochondrial function and interacts genetically with autophagy. Science 305, 1292–1295 (2004).
expansions in fly and mouse models of Huntington parkin. Nature 441, 1162–1166 (2006). This landmark paper is the first to suggest the
disease. Nature Genet. 36, 147. Park, J. et al. Mitochondrial dysfunction in Drosophila possibility of dysfunction in CMA as a factor in the
585–595 (2004). PINK1 mutants is complemented by parkin. Nature pathogenesis of PD.
Using rapamycin to treat animal models of HD, this 441, 1157–1161 (2006). 169. Orenstein, S. J. et al. Interplay of LRRK2 with
study was the first to demonstrate that 148. Narendra, D., Tanaka, A., Suen, D. F. & Youle, R. J. chaperone-mediated autophagy. Nature Neurosci. 16,
upregulation of autophagy can have a beneficial Parkin is recruited selectively to impaired 394–406 (2013).
effect in in vivo models of the disease. mitochondria and promotes their autophagy. J. Cell 170. Wang, Y. et al. Tau fragmentation, aggregation and
126. Menzies, F. M. et al. Autophagy induction reduces Biol. 183, 795–803 (2008). clearance: the dual role of lysosomal processing. Hum.
mutant ataxin‑3 levels and toxicity in a mouse model This pioneering paper linked Parkin to mitophagy Mol. Genet. 18, 4153–4170 (2009).
of spinocerebellar ataxia type 3. Brain 133, 93–104 for the first time and led to the subsequent surge 171. Pacheco, C. D. & Lieberman, A. P. The pathogenesis of
(2010). in understanding of the potential roles of certain Niemann–Pick type C disease: a role for autophagy?
127. Spilman, P. et al. Inhibition of mTOR by rapamycin genes that are mutated in PD. Expert Rev. Mol. Med. 10, e26 (2008).
abolishes cognitive deficits and reduces amyloid-β 149. Becker, D., Richter, J., Tocilescu, M. A., 172. Ko, D. C. et al. Cell-autonomous death of cerebellar
levels in a mouse model of Alzheimer’s disease. PLoS Przedborski, S. & Voos, W. Pink1 kinase and its Purkinje neurons with autophagy in Niemann–Pick
ONE 5, e9979 (2010). membrane potential (Deltapsi)-dependent cleavage type C disease. PLoS Genet. 1, 81–95 (2005).
128. Jiang, T. et al. Temsirolimus promotes autophagic product both localize to outer mitochondrial 173. Kimura, S., Noda, T. & Yoshimori, T. Dissection of the
clearance of amyloid-β and provides protective effects membrane by unique targeting mode. J. Biol. Chem. autophagosome maturation process by a novel
in cellular and animal models of Alzheimer’s disease. 287, 22969–22987 (2012). reporter protein, tandem fluorescent-tagged LC3.
Pharmacol. Res. 81, 54–63 (2014). 150. Greene, A. W. et al. Mitochondrial processing Autophagy 3, 452–460 (2007).
129. Williams, A. et al. Novel targets for Huntington’s peptidase regulates PINK1 processing, import and 174. Elrick, M. J., Yu, T., Chung, C. & Lieberman, A. P.
disease in an mTOR-independent autophagy Parkin recruitment. EMBO Rep. 13, 378–385 Impaired proteolysis underlies autophagic dysfunction
pathway. Nature Chem. Biol. 4, (2012). in Niemann–Pick type C disease. Hum. Mol. Genet.
295–305 (2008). 151. Jin, S. M. et al. Mitochondrial membrane potential 21, 4876–4887 (2012).
130. Rose, C. et al. Rilmenidine attenuates toxicity of regulates PINK1 import and proteolytic destabilization 175. Ordonez, M. P. et al. Disruption and therapeutic
polyglutamine expansions in a mouse model of by PARL. J. Cell Biol. 191, 933–942 (2010). rescue of autophagy in a human neuronal model of
Huntington’s disease. Hum. Mol. Genet. 19, 152. Geisler, S. et al. PINK1/Parkin-mediated mitophagy is Niemann Pick type C1. Hum. Mol. Genet. 21,
2144–2153 (2010). dependent on VDAC1 and p62/SQSTM1. Nature Cell 2651–2662 (2012).
131. Sarkar, S. et al. Lithium induces autophagy by Biol. 12, 119–131 (2010). 176. Maetzel, D. et al. Genetic and chemical correction of
inhibiting inositol monophosphatase. J. Cell 153. Matsuda, N. et al. PINK1 stabilized by mitochondrial cholesterol accumulation and impaired autophagy in
Biol. 170, 1101–1111 (2005). depolarization recruits Parkin to damaged hepatic and neural cells derived from Niemann-Pick
132. Shimada, K. et al. Long-term oral lithium treatment mitochondria and activates latent Parkin for type C patient-specific iPS cells. Stem Cell Rep.
attenuates motor disturbance in tauopathy model mitophagy. J. Cell Biol. 189, 211–221 (2010). 2, 866–880 (2014).
mice: implications of autophagy promotion. 154. Narendra, D. P. et al. PINK1 is selectively stabilized on 177. Sarkar, S. et al. Impaired autophagy in the lipid-
Neurobiol. Dis. 46, 101–108 (2012). impaired mitochondria to activate Parkin. PLoS Biol. storage disorder Niemann–Pick type C1 disease. Cell
133. Li, L. et al. Autophagy enhancer carbamazepine 8, e1000298 (2010). Rep. 5, 1302–1315 (2013).
alleviates memory deficits and cerebral amyloid-β 155. Vives-Bauza, C. et al. PINK1‑dependent recruitment of This paper attempts to clarify previous
pathology in a mouse model of Alzheimer’s disease. Parkin to mitochondria in mitophagy. Proc. Natl Acad. contentions in the role of autophagy in NPC1 and
Curr. Alzheimer Res. 10, 433–441 (2013). Sci. USA 107, 378–383 (2010). demonstrates a decrease in autophagic function in
134. Menzies, F. M. et al. Calpain inhibition mediates 156. de Vries, R. L. & Przedborski, S. Mitophagy and the disease.
autophagy-dependent protection against Parkinson’s disease: be eaten to stay healthy. Mol. 178. Meske, V., Erz, J., Priesnitz, T. & Ohm, T. G. The
polyglutamine toxicity. Cell Death Differ. 22, Cell. Neurosci. 55, 37–43 (2013). autophagic defect in Niemann-Pick disease type C
433–444 (2014). 157. Bingol, B. et al. The mitochondrial deubiquitinase neurons differs from somatic cells and reduces
135. Sarkar, S., Davies, J. E., Huang, Z., Tunnacliffe, A. & USP30 opposes parkin-mediated mitophagy. Nature neuronal viability. Neurobiol. Dis. 64, 88–97
Rubinsztein, D. C. Trehalose, a novel mTOR- 510, 370–375 (2014). (2014).
independent autophagy enhancer, accelerates the 158. Narendra, D., Kane, L. A., Hauser, D. N., 179. Motori, E. et al. Inflammation-induced alteration of
clearance of mutant huntingtin and α-synuclein. Fearnley, I. M. & Youle, R. J. p62/SQSTM1 is required astrocyte mitochondrial dynamics requires autophagy
J. Biol. Chem. 282, 5641–5652 (2007). for Parkin-induced mitochondrial clustering but not for mitochondrial network maintenance. Cell.
136. Rodriguez-Navarro, J. A. et al. Trehalose mitophagy; VDAC1 is dispensable for both. Autophagy Metab. 18, 844–859 (2013).
ameliorates dopaminergic and tau pathology in 6, 1090–1106 (2010). 180. Smith, C. M., Mayer, J. A. & Duncan, I. D. Autophagy
parkin deleted/tau overexpressing mice through 159. Scarffe, L. A., Stevens, D. A., Dawson, V. L. & promotes oligodendrocyte survival and function
autophagy activation. Neurobiol. Dis. 39, 423–438 Dawson, T. M. Parkin and PINK1: much more than following dysmyelination in a long-lived myelin mutant.
(2010). mitophagy. Trends Neurosci. 37, 315–324 (2014). J. Neurosci. 33, 8088–8100 (2013).
356 | JUNE 2015 | VOLUME 16 www.nature.com/reviews/neuro
© 2015 Macmillan Publishers Limited. All rights reserved
REVIEWS
181. Rangaraju, S. et al. Rapamycin activates autophagy therapeutic strategies. Neurotherapeutics 10, Acknowledgements
and improves myelination in explant cultures from 371–382 (2013). The authors are grateful for funding from a Wellcome Trust
neuropathic mice. J. Neurosci. 30, 11388–11397 185. Danzer, K. M. et al. Exosomal cell‑to‑cell transmission Principal Research Fellowship (D.C.R.), a Wellcome Trust and
(2010). of alpha synuclein oligomers. Mol. Neurodegener. Medical Research Council (MRC) Strategic Grant on neuro
182. Di Malta, C., Fryer, J. D., Settembre, C. & Ballabio, A. 7, 42 (2012). degeneration, a Wellcome Trust Strategic Award to the
Astrocyte dysfunction triggers neurodegeneration in a 186. Ejlerskov, P. et al. Tubulin polymerization-promoting Cambridge Institute for Medical Research, the Alzheimer’s
lysosomal storage disorder. Proc. Natl Acad. Sci. protein (TPPP/p25α) promotes unconventional disease National Institute for Health Research (NIHR)
USA 109, E2334–E2342 (2012). secretion of α-synuclein through exophagy by Biomedical Research Unit at Addenbrooke’s Hospital, the Tau
This paper demonstrates that astrocyte-specific impairing autophagosome–lysosome fusion. J. Biol. Consortium and Alzheimer’s Research UK.
deletion of Sumf1 in mice, a gene associated with Chem. 288, 17313–17335 (2013).
multiple sulfatase deficiency, results in the loss of 187. Lee, H. J. et al. Autophagic failure promotes the Competing interests statement
autophagy function in astrocytes and degeneration exocytosis and intercellular transfer of α-synuclein. The authors declare competing interests: see Web version for
of cortical neurons. Exp. Mol. Med. 45, e22 (2013). details.
183. Deretic, V., Jiang, S. & Dupont, N. Autophagy 188. Nilsson, P. et al. Aβ secretion and plaque formation
intersections with conventional and unconventional depend on autophagy. Cell Rep. 5,
secretion in tissue development, remodeling and 61–69 (2013). DATABASES
inflammation. Trends Cell Biol. 22, 397–406 189. Nixon, R. A. Alzheimer neurodegeneration, autophagy, European Clinical Trials Database: https://eudract.ema.
(2012). and Abeta secretion: the ins and outs (comment on europa.eu/index.html
184. Kaufman, S. K. & Diamond, M. I. Prion-like DOI 10.1002/bies.201400002). Bioessays 36, 547 ALL LINKS ARE ACTIVE IN THE ONLINE PDF
propagation of protein aggregation and related (2014).
NATURE REVIEWS | NEUROSCIENCE VOLUME 16 | JUNE 2015 | 357
© 2015 Macmillan Publishers Limited. All rights reserved
You might also like
- Neurodegenerative Diseases Multifactorial ConformationalDocument9 pagesNeurodegenerative Diseases Multifactorial ConformationalLala FemNo ratings yet
- Late-Onset Alzheimers Disease Is Associated WithDocument13 pagesLate-Onset Alzheimers Disease Is Associated WithAlix AliNo ratings yet
- Targeting Whole Body Metabolism and Mitochondrial Bioener - 2022 - Acta PharmaceDocument21 pagesTargeting Whole Body Metabolism and Mitochondrial Bioener - 2022 - Acta PharmaceMohammed Shuaib AhmedNo ratings yet
- Adipose Tissue As A Target For Second-Generation (Atypical) AntipsychoticsDocument14 pagesAdipose Tissue As A Target For Second-Generation (Atypical) AntipsychoticsAgustin NunezNo ratings yet
- Metabolic Products of Soluble Epoxide Hydrolase Are Essential For Monocyte Chemotaxis To MCP-1 in Vitro and in VivoDocument12 pagesMetabolic Products of Soluble Epoxide Hydrolase Are Essential For Monocyte Chemotaxis To MCP-1 in Vitro and in VivoghhhNo ratings yet
- Molecules: - Amyloid and The Pathomechanisms of Alzheimer's Disease: A Comprehensive ViewDocument32 pagesMolecules: - Amyloid and The Pathomechanisms of Alzheimer's Disease: A Comprehensive ViewdianawilcoxNo ratings yet
- Dhami Et Al-2019-Journal of Neurochemistry PDFDocument18 pagesDhami Et Al-2019-Journal of Neurochemistry PDFJawad A. KhanNo ratings yet
- Journal of Neurochemistry - 2016 - Jalewa - Novel Incretin Analogues Improve Autophagy and Protect From MitochondrialDocument13 pagesJournal of Neurochemistry - 2016 - Jalewa - Novel Incretin Analogues Improve Autophagy and Protect From Mitochondrialjalewa.jaishreeNo ratings yet
- Beyond Adiponectin and LeptinDocument50 pagesBeyond Adiponectin and Leptintasneemh2308No ratings yet
- De La Rosa 2015Document12 pagesDe La Rosa 2015yasmin matterNo ratings yet
- Acetaminophen-Induced Liver Injury: From Animal Models To HumansDocument8 pagesAcetaminophen-Induced Liver Injury: From Animal Models To HumansMiguel Adrian GaonaNo ratings yet
- Spektro Uv VisDocument7 pagesSpektro Uv VisNadaNo ratings yet
- Life Sciences: Haocheng Ao, Haichun Li, Xiujuan Zhao, Bingqian Liu, Lin LuDocument15 pagesLife Sciences: Haocheng Ao, Haichun Li, Xiujuan Zhao, Bingqian Liu, Lin LuPaoloMafaldoNo ratings yet
- PRD 89 59Document24 pagesPRD 89 59vrht2xyvsdNo ratings yet
- Review Article: The Bewildering Effect of AMPK Activators in Alzheimer's Disease: Review of The Current EvidenceDocument18 pagesReview Article: The Bewildering Effect of AMPK Activators in Alzheimer's Disease: Review of The Current EvidenceJoshNo ratings yet
- Perspective Is Therapeutic Plasma Exchange A Viable Option For TreatingDocument11 pagesPerspective Is Therapeutic Plasma Exchange A Viable Option For TreatingRaul Rios RitterNo ratings yet
- 1 s2.0 S0891584922006220 Main - CompressedDocument24 pages1 s2.0 S0891584922006220 Main - CompressedPauBlack 13No ratings yet
- The Awesome Lysosome: Louis-Jeantet Prize Winner: PerspectiveDocument4 pagesThe Awesome Lysosome: Louis-Jeantet Prize Winner: Perspectivexoco xocoNo ratings yet
- 1 s2.0 S092544391300327X MainDocument8 pages1 s2.0 S092544391300327X Main邢振凯No ratings yet
- Or 22 1 215 PDFDocument7 pagesOr 22 1 215 PDFLandcel Clarence ArcedoNo ratings yet
- Role of ROS in Metabolic Diseases and ChronicDocument9 pagesRole of ROS in Metabolic Diseases and ChronicFian AldyNo ratings yet
- Activation of mTOR: A Culprit of Alzheimer's Disease?: Neuropsychiatric Disease and Treatment DoveDocument16 pagesActivation of mTOR: A Culprit of Alzheimer's Disease?: Neuropsychiatric Disease and Treatment Dovemr dexterNo ratings yet
- Oroxylin A Promotes Pgc 1%Ce%B1 Mfn2 Signaling To Attenuate Hepatocyte Pyroptosis Via Blocking Mitochondrial Ros In Alcoholic Liver Disease Jun Kai Xiang Yang Zhimin Wang Feixia Wang Yan Jia full chapter pdf docxDocument39 pagesOroxylin A Promotes Pgc 1%Ce%B1 Mfn2 Signaling To Attenuate Hepatocyte Pyroptosis Via Blocking Mitochondrial Ros In Alcoholic Liver Disease Jun Kai Xiang Yang Zhimin Wang Feixia Wang Yan Jia full chapter pdf docxgottiagapov100% (6)
- Au Top HagiaDocument48 pagesAu Top HagiaJorge CamargoNo ratings yet
- Modeling Alzheimer's...Document35 pagesModeling Alzheimer's...clfp25No ratings yet
- Organelle-Specific Autophagy in Inflammatory Diseases A Potential Therapeutic Target Underlying The Quality Control of Multiple OrganellesDocument18 pagesOrganelle-Specific Autophagy in Inflammatory Diseases A Potential Therapeutic Target Underlying The Quality Control of Multiple OrganelleseNo ratings yet
- Neuropharmacology: Sciverse SciencedirectDocument8 pagesNeuropharmacology: Sciverse SciencedirectShawnNo ratings yet
- Migdalska-Richards Et Al-2016-Journal of NeurochemistryDocument14 pagesMigdalska-Richards Et Al-2016-Journal of Neurochemistryjazz castañedaNo ratings yet
- Journal of Pharmaceutical and Biomedical AnalysisDocument8 pagesJournal of Pharmaceutical and Biomedical AnalysisUday BaruahNo ratings yet
- Lysosomal Impairment in Parkinson's Disease: ReviewDocument8 pagesLysosomal Impairment in Parkinson's Disease: ReviewRara Aulia IINo ratings yet
- Austin ProteomicsDocument6 pagesAustin ProteomicsAustin Publishing GroupNo ratings yet
- A Multi-Systemic Mitochondrial Disorder Due To A Dominant p.Y955H Disease Variant in DNA Polymerase GammaDocument16 pagesA Multi-Systemic Mitochondrial Disorder Due To A Dominant p.Y955H Disease Variant in DNA Polymerase GammaMihai LazarNo ratings yet
- Biomedicine & Pharmacotherapy: ReviewDocument14 pagesBiomedicine & Pharmacotherapy: Reviewmr dexterNo ratings yet
- Cell Death 2011Document15 pagesCell Death 2011Paula Contreras MezaNo ratings yet
- IA - Molecular Biology of Pharmacology 160908Document39 pagesIA - Molecular Biology of Pharmacology 160908Susi RutmalemNo ratings yet
- Autophagy and Its Usefulness in Chemical BiologyDocument10 pagesAutophagy and Its Usefulness in Chemical BiologyGourav DasNo ratings yet
- Mitochondrial DDocument17 pagesMitochondrial DIt's MeNo ratings yet
- 5 PBDocument17 pages5 PBAisha MurtazaNo ratings yet
- Mitochondrial Dysfunction and Mitophagy in Parkinson's: From Familial To Sporadic DiseaseDocument11 pagesMitochondrial Dysfunction and Mitophagy in Parkinson's: From Familial To Sporadic DiseaseKaycsa AdrianaNo ratings yet
- Emerging Alternative Proteinases in APP Metabolism and Alzheimer Disease Pathogenesis-A Focus On MT1-MMP and MT5-MMPDocument19 pagesEmerging Alternative Proteinases in APP Metabolism and Alzheimer Disease Pathogenesis-A Focus On MT1-MMP and MT5-MMPRaynNo ratings yet
- HanooDocument8 pagesHanoomr samoNo ratings yet
- Weber 1999Document8 pagesWeber 1999prism1702No ratings yet
- Thioredoxin Is Implicated in The Anti Apoptotic Effects of Grape Seed Proanthocyanidin Extract During HyperglycemiaDocument7 pagesThioredoxin Is Implicated in The Anti Apoptotic Effects of Grape Seed Proanthocyanidin Extract During HyperglycemiaDevendra PathakNo ratings yet
- Golgi NCA LC3-IIDocument12 pagesGolgi NCA LC3-IIPetit PasNo ratings yet
- Journal Club: Paolo Dametto January 2013Document42 pagesJournal Club: Paolo Dametto January 2013Олег ЕвсюковNo ratings yet
- MainDocument15 pagesMainDamian KlóskaNo ratings yet
- Mitochondrial Hydrogen Peroxide Activates PTEN and Inactivates Akt Leading To Autophagy Inhibition Dependent Cell Death in Neuronal Models of Parkinson's DiseaseDocument20 pagesMitochondrial Hydrogen Peroxide Activates PTEN and Inactivates Akt Leading To Autophagy Inhibition Dependent Cell Death in Neuronal Models of Parkinson's DiseaseyusranurparlakNo ratings yet
- Nutritionandalzheimer Disease: Shirley Steffany Muñoz Fernández,, Sandra Maria Lima RibeiroDocument21 pagesNutritionandalzheimer Disease: Shirley Steffany Muñoz Fernández,, Sandra Maria Lima RibeiroReindeer MerkaatsNo ratings yet
- Ijms 24 09067Document42 pagesIjms 24 09067Carlos CalderonNo ratings yet
- Acido ValproicoDocument10 pagesAcido ValproicopreedtooneNo ratings yet
- Autophagy in Cardiovascular BiologyDocument10 pagesAutophagy in Cardiovascular Biologygaetano confortoNo ratings yet
- The Role of STAT3 in AutophagyDocument12 pagesThe Role of STAT3 in AutophagyeNo ratings yet
- 10 1016@j Pharmthera 2020 107521 PDFDocument112 pages10 1016@j Pharmthera 2020 107521 PDFSyedNo ratings yet
- Respuesta de Proteinas-0216Document8 pagesRespuesta de Proteinas-0216Daniela HNo ratings yet
- Serum Markers of Neurodegeneration in Maple Syrup Urine DiseaseDocument11 pagesSerum Markers of Neurodegeneration in Maple Syrup Urine DiseaseMatheus PioNo ratings yet
- Manuscript Mini-ReviewDocument7 pagesManuscript Mini-ReviewProviderNo ratings yet
- Lipid Signaling and Lipotoxicity in Metaflammation Indications For Metabolic Disease Pathogenesis and TreatmentDocument16 pagesLipid Signaling and Lipotoxicity in Metaflammation Indications For Metabolic Disease Pathogenesis and TreatmentSherin KhodierNo ratings yet
- Shared and Distinct Patterns of Oligodendroglial Response in A - Synucleinopathies and TauopathiesDocument10 pagesShared and Distinct Patterns of Oligodendroglial Response in A - Synucleinopathies and TauopathiesTibor SzénásiNo ratings yet
- NIH Public Access: Author ManuscriptDocument18 pagesNIH Public Access: Author Manuscriptنوره نورNo ratings yet
- Baldwin 1971Document3 pagesBaldwin 1971kosikevinonuNo ratings yet
- Varshavsky 1991Document3 pagesVarshavsky 1991kosikevinonuNo ratings yet
- Tucker 2018Document8 pagesTucker 2018kosikevinonuNo ratings yet
- Mckenna 2017Document3 pagesMckenna 2017kosikevinonuNo ratings yet
- Brissos 2007Document1 pageBrissos 2007kosikevinonuNo ratings yet
- Topiol 2009Document10 pagesTopiol 2009kosikevinonuNo ratings yet
- Result SheetDocument8 pagesResult SheetsumanNo ratings yet
- CS-CSA Centrifugal PumpsDocument60 pagesCS-CSA Centrifugal PumpsFelix Rodriguez Lira100% (1)
- HarvestlandDocument687 pagesHarvestlandJanetNo ratings yet
- ROCK Fill Specifiation & StandardsDocument17 pagesROCK Fill Specifiation & StandardsibrahimNo ratings yet
- Hall - Panikkar Trusting The OtherDocument23 pagesHall - Panikkar Trusting The OtherOscar Emilio Rodríguez CoronadoNo ratings yet
- DC DC: Table 5.13: Overhead Line Conductor - Hard Drawn CopperDocument8 pagesDC DC: Table 5.13: Overhead Line Conductor - Hard Drawn CopperVino VinoNo ratings yet
- 02nd To 04th December 2023 International Cotton Advisory Committee - 81st Plenary Meeting 2023Document11 pages02nd To 04th December 2023 International Cotton Advisory Committee - 81st Plenary Meeting 2023sabirNo ratings yet
- Computational Fluid Dynamics Prof. Dr. Suman Chakraborty Department of Mechanical Engineering Indian Institute of Technology, KharagpurDocument18 pagesComputational Fluid Dynamics Prof. Dr. Suman Chakraborty Department of Mechanical Engineering Indian Institute of Technology, Kharagpurk krishna chaitanyaNo ratings yet
- MHT CET 2023 Cutoff Round 2 Maharashtra CandidatesDocument1,365 pagesMHT CET 2023 Cutoff Round 2 Maharashtra Candidatestodankarpratham15No ratings yet
- Chapter-2 RERDocument20 pagesChapter-2 RERMahmoud TarekNo ratings yet
- Bosch Tune Up Parts PDFDocument9 pagesBosch Tune Up Parts PDFdwebs262No ratings yet
- Renewable Energy CertificatesDocument3 pagesRenewable Energy CertificatesVaradarajan SrinivasanNo ratings yet
- Painting and GlazingDocument56 pagesPainting and GlazingWilliam PeterNo ratings yet
- Barudan-Bens PDFDocument103 pagesBarudan-Bens PDFJoseph KimNo ratings yet
- Power of MantraDocument15 pagesPower of Mantraphani1978100% (1)
- Knife Gate Valve: Product DescriptionDocument2 pagesKnife Gate Valve: Product DescriptionTamil SelvanNo ratings yet
- Nursing Care PlanDocument25 pagesNursing Care PlanIndah MardianiNo ratings yet
- NN ST661 (CPH)Document42 pagesNN ST661 (CPH)Patrice PaulNo ratings yet
- GALLO-SCYTHIANS - Celtic Ukraine (By Mac Congail)Document22 pagesGALLO-SCYTHIANS - Celtic Ukraine (By Mac Congail)Toma100% (1)
- Bonn & Gaston 2005 Richness Ecosystem Conserv SAfDocument18 pagesBonn & Gaston 2005 Richness Ecosystem Conserv SAfKellyta RodriguezNo ratings yet
- The History of Moral and Social Philosophy A Professional Perspective - 2Document24 pagesThe History of Moral and Social Philosophy A Professional Perspective - 2rmm0415No ratings yet
- Advancing Physics B A2 CourseworkDocument5 pagesAdvancing Physics B A2 Courseworkbotav1nakak3100% (2)
- UD11379B - Baseline - Quick Start Guide of Turbo HD DVR - V3.4.89 - 20180823Document43 pagesUD11379B - Baseline - Quick Start Guide of Turbo HD DVR - V3.4.89 - 20180823NicolasNo ratings yet
- Revised Holiday HomeDocument4 pagesRevised Holiday HomerashmichemistryNo ratings yet
- Potential of Non-Conventional Source of Energy and Associated Environmental Issue: An Indian ScenarioDocument6 pagesPotential of Non-Conventional Source of Energy and Associated Environmental Issue: An Indian ScenarioSanchit PatilNo ratings yet
- Datasheet VisiTouch-Pac V1.3 ENDocument8 pagesDatasheet VisiTouch-Pac V1.3 ENDavid CalderonNo ratings yet
- A New Classification Scheme For Periodontal and Peri and Conditions - Introduction and Key Changes From The 1999 ClassificationDocument8 pagesA New Classification Scheme For Periodontal and Peri and Conditions - Introduction and Key Changes From The 1999 ClassificationOner Man0% (1)
- Boot Camp Workbook (Solutions)Document17 pagesBoot Camp Workbook (Solutions)Ujjwal VasishtNo ratings yet
- Light Mild Brown Girl in Glasses Sales Brochuryye (Yyyyyyyyyyyy1)Document2 pagesLight Mild Brown Girl in Glasses Sales Brochuryye (Yyyyyyyyyyyy1)Althea KimNo ratings yet
- RB Cagmat Review Center: Central Mindanao University, CMU, Musuan, BukidnonDocument6 pagesRB Cagmat Review Center: Central Mindanao University, CMU, Musuan, BukidnonshakiraNo ratings yet