Professional Documents
Culture Documents
Phos2 2019-07 v9 1
Phos2 2019-07 v9 1
Uploaded by
ammarhp23Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Phos2 2019-07 v9 1
Phos2 2019-07 v9 1
Uploaded by
ammarhp23Copyright:
Available Formats
0003183793122c501V9.
PHOS2
Phosphate (Inorganic) ver.2
Order information
Analyzer(s) on which cobas c pack(s) can be used
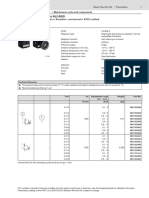
03183793 122 Phosphate (Inorganic) ver.2 (250 tests) System‑ID 07 6614 3 Roche/Hitachi cobas c 311, cobas c 501/502
10759350 190 Calibrator f.a.s. (12 x 3 mL) Code 401
10759350 360 Calibrator f.a.s. (12 x 3 mL, for USA) Code 401
12149435 122 Precinorm U plus (10 x 3 mL) Code 300
12149435 160 Precinorm U plus (10 x 3 mL, for USA) Code 300
12149443 122 Precipath U plus (10 x 3 mL) Code 301
12149443 160 Precipath U plus (10 x 3 mL, for USA) Code 301
05117003 190 PreciControl ClinChem Multi 1 (20 x 5 mL) Code 391
05947626 190 PreciControl ClinChem Multi 1 (4 x 5 mL) Code 391
05947626 160 PreciControl ClinChem Multi 1 (4 x 5 mL, for USA) Code 391
05117216 190 PreciControl ClinChem Multi 2 (20 x 5 mL) Code 392
05947774 190 PreciControl ClinChem Multi 2 (4 x 5 mL) Code 392
05947774 160 PreciControl ClinChem Multi 2 (4 x 5 mL, for USA) Code 392
04489357 190 Diluent NaCl 9 % (50 mL) System‑ID 07 6869 3
English Test principle5
System information Molybdate UV.
For cobas c 311 analyzer: Inorganic phosphate forms an ammonium phosphomolybdate complex
having the formula (NH4)3[PO4(MoO3)12] with ammonium molybdate in the
PHOS2: ACN 714 (serum/plasma) presence of sulfuric acid.
SPHO2: ACN 675 (STAT, reaction time: 7: serum/plasma)
PHO2U: ACN 716 (urine) H2SO4
SPH2U: ACN 656 (STAT, reaction time: 7: urine) Phosphate + ammonium phosphomolybdate
For cobas c 501 analyzer: ammonium molybdate
PHOS2: ACN 714 (serum/plasma/urine) The concentration of phosphomolybdate formed is directly proportional to
SPHO2: ACN 675 (STAT, reaction time: 7: serum/plasma/urine) the inorganic phosphate concentration and is measured photometrically.
For cobas c 502 analyzer: Reagents - working solutions
PHOS2: ACN 8714 (serum/plasma) R1 Sulfuric acid: 0.36 mol/L; detergent
SPHO2: ACN 8675 (STAT, reaction time: 7: serum/plasma)
R2 Ammonium molybdate: 3.5 mmol/L; sulfuric acid: 0.36 mol/L;
PHO2U: ACN 8716 (urine) sodium chloride: 150 mmol/L
SPH2U: ACN 8656 (STAT, reaction time: 7: urine)
R1 is in position B and R2 is in position C.
Intended use
Precautions and warnings
In vitro test for the quantitative determination of phosphorus in human
serum, plasma and urine on Roche/Hitachi cobas c systems. For in vitro diagnostic use.
Exercise the normal precautions required for handling all laboratory
Summary1,2,3,4,5 reagents.
88 % of the phosphorus contained in the body is localized in bone in the Disposal of all waste material should be in accordance with local guidelines.
form of calcium phosphate as the apatite Ca2+[Ca3(PO4)2]32-. The remainder Safety data sheet available for professional user on request.
is involved in intermediary carbohydrate metabolism and in physiologically For USA: Caution: Federal law restricts this device to sale by or on the
important substances such as phospholipids, nucleic acids and ATP. order of a physician.
Phosphorus occurs in blood in the form of inorganic phosphate and in
organically bound phosphoric acid. The small amount of extracellular This kit contains components classified as follows in accordance with the
organic phosphorus is found almost exclusively in the form of Regulation (EC) No. 1272/2008:
phospholipids.
The ratio of phosphate to calcium in the blood is approximately 6:10. An
increase in the level of phosphorus causes a decrease in the calcium level.
The mechanism is influenced by interactions between parathormone and
vitamin D. Hypoparathyroidism, vitamin D intoxication and renal failure with
decreased glomerular phosphate filtration give rise to hyperphosphatemia. Warning
Hypophosphatemia occurs in rickets, hyperparathyroidism and Fanconi's
syndrome. H290 May be corrosive to metals.
The preferred method for the determination of inorganic phosphorus is
based on the formation of ammonium phosphomolybdate with subsequent Prevention:
reduction to molybdenum blue. Reagent stability problems often occur with P234 Keep only in original packaging.
this method. The method presented here is based on the reaction of
phosphate with ammonium molybdate to form ammonium Response:
phosphomolybdate without reduction. The addition of an accelerator gives
rise to a more rapid rate of reaction and the application of sample blanking P390 Absorb spillage to prevent material damage.
yields more precise results. Product safety labeling follows EU GHS guidance.
Contact phone: all countries: +49-621-7590, USA: 1-800-428-2336
2019-07, V 9.0 English 1/5
0003183793122c501V9.0
PHOS2
Phosphate (Inorganic) ver.2
Reagent handling Wavelength (sub/main) 700/340 nm
Ready for use Reaction direction Increase
Storage and stability Units mmol/L (mg/dL, mg/L)
PHOS2 Reagent pipetting Diluent (H2O)
Shelf life at 2‑8 °C: See expiration date R1 90 µL 28 µL
on cobas c pack R2 38 µL –
label.
On‑board in use and refrigerated on the analyzer: 12 weeks
Sample volumes Sample Sample dilution
Diluent NaCl 9 %
Sample Diluent (NaCl)
Shelf life at 2‑8 °C: See expiration date
on cobas c pack Normal 2.5 µL – –
label. Decreased 12.5 µL 15 µL 135 µL
On‑board in use and refrigerated on the analyzer: 12 weeks Increased 2.5 µL – –
Specimen collection and preparation cobas c 501 test definition
For specimen collection and preparation only use suitable tubes or
collection containers. Assay type 2‑Point End
Only the specimens listed below were tested and found acceptable. Reaction time / Assay points 10 / 10‑47 (STAT 7 / 10‑47)
Serum Wavelength (sub/main) 700/340 nm
Plasma: Li‑heparin and K2‑EDTA plasma
The sample types listed were tested with a selection of sample collection Reaction direction Increase
tubes that were commercially available at the time of testing, i.e. not all Units mmol/L (mg/dL, mg/L)
available tubes of all manufacturers were tested. Sample collection systems
from various manufacturers may contain differing materials which could Reagent pipetting Diluent (H2O)
affect the test results in some cases. When processing samples in primary R1 90 µL 28 µL
tubes (sample collection systems), follow the instructions of the tube
manufacturer. R2 38 µL –
Urine
Collect in detergent‑free containers. Acidify with hydrochloric acid after Sample volumes Sample Sample dilution
collection (pH < 3).6,7
Sample Diluent (NaCl)
Stability in serum/plasma:8 24 hours at 15‑25 °C Normal 2.5 µL – –
4 days at 2‑8 °C Decreased 12.5 µL 15 µL 135 µL
1 year at (-15)‑(-25) °C Increased 2.5 µL – –
Stability in urine:6,7 6 months at 2‑8 °C (when acidified)
cobas c 502 test definition
24‑hour urine: Store cooled during collection.
Assay type 2‑Point End
Centrifuge samples containing precipitates before performing the assay.
Reaction time / Assay points 10 / 10‑47 (STAT 7 / 10‑47)
See the limitations and interferences section for details about possible
sample interferences. Wavelength (sub/main) 700/340 nm
Sample stability claims were established by experimental data by the Reaction direction Increase
manufacturer or based on reference literature and only for the
temperatures/time frames as stated in the method sheet. It is the Units mmol/L (mg/dL, mg/L)
responsibility of the individual laboratory to use all available references Reagent pipetting Diluent (H2O)
and/or its own studies to determine specific stability criteria for its
laboratory. R1 90 µL 28 µL
Materials provided R2 38 µL –
See “Reagents – working solutions” section for reagents.
Materials required (but not provided) Sample volumes Sample Sample dilution
▪ See “Order information” section Sample Diluent (NaCl)
▪ General laboratory equipment Normal 2.5 µL – –
Assay
Decreased 12.5 µL 15 µL 135 µL
For optimum performance of the assay follow the directions given in this
document for the analyzer concerned. Refer to the appropriate operator’s Increased 5 µL – –
manual for analyzer‑specific assay instructions. Application for urine
The performance of applications not validated by Roche is not warranted
and must be defined by the user. cobas c 311 test definition
Application for serum and plasma Assay type 2‑Point End
cobas c 311 test definition Reaction time / Assay points 10 / 6‑32 (STAT 7 / 6‑32)
Assay type 2‑Point End Wavelength (sub/main) 700/340 nm
Reaction time / Assay points 10 / 6‑32 (STAT 7 / 6‑32) Reaction direction Increase
2/5 2019-07, V 9.0 English
0003183793122c501V9.0
PHOS2
Phosphate (Inorganic) ver.2
Units mmol/L (mg/dL, mg/L) Calibration interval may be extended based on acceptable verification of
calibration by the laboratory.
Reagent pipetting Diluent (H2O)
Traceability: This method has been standardized against NERL primary
R1 90 µL 28 µL reference material.
R2 38 µL – For USA: This method has been standardized against NIST traceable
primary reference material.
Quality control
Sample volumes Sample Sample dilution Serum/plasma
Sample Diluent (NaCl) For quality control, use control materials as listed in the "Order information"
Normal 2.5 µL 15 µL 150 µL section.
In addition, other suitable control material can be used.
Decreased 2.5 µL 8 µL 168 µL
Urine
Increased 2.5 µL 15 µL 150 µL Quantitative urine controls are recommended for routine quality control.
cobas c 501 test definition The control intervals and limits should be adapted to each laboratory’s
individual requirements. Values obtained should fall within the defined
Assay type 2‑Point End limits. Each laboratory should establish corrective measures to be taken if
Reaction time / Assay points 10 / 10‑47 (STAT 7 / 10‑47) values fall outside the defined limits.
Follow the applicable government regulations and local guidelines for
Wavelength (sub/main) 700/340 nm quality control.
Reaction direction Increase Calculation
Units mmol/L (mg/dL, mg/L) Roche/Hitachi cobas c systems automatically calculate the analyte
concentration of each sample.
Reagent pipetting Diluent (H2O)
R1 90 µL 28 µL Conversion factors: mmol/L x 3.10 = mg/dL
R2 38 µL – mmol/L x 31 = mg/L
mg/L x 0.0323 = mmol/L
Sample volumes Sample Sample dilution Limitations - interference6
Sample Diluent (NaCl) Criterion: Recovery within ± 10 % of initial value at a phosphate
concentration of 0.87 mmol/L (2.7 mg/dL).
Normal 2.5 µL 15 µL 150 µL Serum/plasma
Decreased 2.5 µL 8 µL 168 µL Icterus:9 No significant interference up to an I index of 40 for conjugated
Increased 2.5 µL 15 µL 150 µL and 60 for unconjugated bilirubin (approximate conjugated bilirubin
concentration: 684 µmol/L or 40 mg/dL and approximate unconjugated
cobas c 502 test definition bilirubin concentration: 1026 µmol/L or 60 mg/dL).
Hemolysis:9 No significant interference up to an H index of 300
Assay type 2‑Point End (approximate hemoglobin concentration: 186 µmol/L or 300 mg/dL).
Reaction time / Assay points 10 / 10‑47 (STAT 7 / 10‑47) Note: This interference results from inorganic phosphates produced by the
Wavelength (sub/main) 700/340 nm action of phosphatases on organic phosphates, both of which are released
from the red cells upon hemolysis.
Reaction direction Increase Lipemia (Intralipid):9 No significant interference up to an L index of 1250.
Units mmol/L (mg/dL, mg/L) There is poor correlation between the L index (corresponds to turbidity) and
triglycerides concentration.
Reagent pipetting Diluent (H2O)
Drugs: No interference was found at therapeutic concentrations using
R1 90 µL 28 µL common drug panels.10,11
R2 38 µL – Exception: Phospholipids contained in liposomal drug formulations
(eg AmBisome) may be hydrolyzed in the test due to the acidic reaction pH
and thus lead to elevated phosphate results.12
Sample volumes Sample Sample dilution In very rare cases, gammopathy, in particular type IgM (Waldenström’s
macroglobulinemia), may cause unreliable results.13
Sample Diluent (NaCl)
Urine
Normal 2.5 µL 15 µL 150 µL
Drugs: No interference was found at therapeutic concentrations using
Decreased 2.5 µL 8 µL 168 µL common drug panels.11
Increased 5 µL 15 µL 150 µL Criterion: Recovery within ± 10 % of initial value at a phosphate
concentration of 13 mmol/L (40.3 mg/dL).
Calibration Urea: No significant interference from urea up to a concentration of
Calibrators S1: H2O 1500 mmol/L (9009 mg/dL).
For diagnostic purposes, the results should always be assessed in
S2: C.f.a.s. conjunction with the patient’s medical history, clinical examination and other
Calibration mode Linear findings.
ACTION REQUIRED
Calibration frequency 2‑point calibration Special Wash Programming: The use of special wash steps is mandatory
• after reagent lot change when certain test combinations are run together on Roche/Hitachi
• as required following quality control cobas c systems. The latest version of the carry‑over evasion list can be
procedures found with the NaOHD-SMS-SmpCln1+2-SCCS Method Sheets. For further
instructions refer to the operator’s manual. cobas c 502 analyzer: All
2019-07, V 9.0 English 3/5
0003183793122c501V9.0
PHOS2
Phosphate (Inorganic) ver.2
special wash programming necessary for avoiding carry‑over is available Precision
via the cobas link, manual input is required in certain cases. Precision was determined using human samples and controls in an internal
Where required, special wash/carry‑over evasion programming must protocol.
be implemented prior to reporting results with this test. Serum/plasma:
Limits and ranges Repeatability (n = 21), intermediate precision (3 aliquots per run, 1 run per
Measuring range day, 21 days);
Serum/plasma Urine:
0.10‑6.46 mmol/L (0.31‑20.0 mg/dL) Repeatability (n = 21), intermediate precision (3 aliquots per run, 1 run per
day, 10 days).
Determine samples having higher concentrations via the rerun function.
Dilution of samples via the rerun function is a 1:2 dilution. Results from The following results were obtained:
samples diluted using the rerun function are automatically multiplied by a
factor of 2. Serum/plasma
Urine
1.1‑92 mmol/L (3.4‑285 mg/dL) Repeatability Mean SD CV
Determine samples having higher concentrations via the rerun function. mmol/L (mg/dL) mmol/L (mg/dL) %
Dilution of samples via the rerun function is a 1:2 dilution. Results from
samples diluted using the rerun function are automatically multiplied by a Precinorm U 1.24 (3.84) 0.01 (0.03) 0.7
factor of 2. Precipath U 2.05 (6.36) 0.01 (0.03) 0.6
Lower limits of measurement Human serum 1 2.68 (8.31) 0.02 (0.06) 0.6
Lower detection limit of the test
Human serum 2 1.56 (4.84) 0.01 (0.03) 0.7
Serum/plasma
0.10 mmol/L (0.31 mg/dL) Intermediate precision Mean SD CV
The lower detection limit represents the lowest measurable analyte level mmol/L (mg/dL) mmol/L (mg/dL) %
that can be distinguished from zero. It is calculated as the value lying
3 standard deviations above that of the lowest standard (standard 1 + 3 SD, Precinorm U 1.23 (3.81) 0.02 (0.06) 1.4
repeatability, n = 21). Precipath U 2.04 (6.32) 0.02 (0.06) 1.2
Urine
Human serum 3 2.67 (8.28) 0.04 (0.12) 1.4
1.1 mmol/L (3.4 mg/dL)
The lower detection limit represents the lowest measurable analyte level Human serum 4 1.55 (4.81) 0.02 (0.06) 1.4
that can be distinguished from zero. It is calculated as the value lying
3 standard deviations above that of the lowest standard (standard 1 + 3 SD, Urine
repeatability, n = 21).
Expected values Repeatability Mean SD CV
Serum/plasma mmol/L (mg/dL) mmol/L (mg/dL) %
Adults:14 Control Level 1 10.2 (31.6) 0.1 (0.3) 1.4
0.81‑1.45 mmol/L (2.5‑4.5 mg/dL)
Control Level 2 19.9 (61.7) 0.2 (0.6) 1.2
Children:15
Human urine 1 40.9 (127) 0.4 (1) 1.0
Age Male Female
Human urine 2 6.25 (19.4) 0.08 (0.2) 1.2
mmol/L (mg/dL) mmol/L (mg/dL)
1–30 d 1.25–2.25 (3.9–6.9) 1.40–2.50 (4.3–7.7) Intermediate precision Mean SD CV
1–12 m 1.15–2.15 (3.5–6.6) 1.20–2.10 (3.7–6.5) mmol/L (mg/dL) mmol/L (mg/dL) %
1–3 y 1.00–1.95 (3.1–6.0) 1.10–1.95 (3.4–6.0) Control Level 1 10.0 (31.0) 0.2 (0.6) 1.6
4–6 y 1.05–1.80 (3.3–5.6) 1.05–1.80 (3.2–5.5) Control Level 2 19.6 (60.8) 0.3 (0.9) 1.7
7–9 y 0.95–1.75 (3.0–5.4) 1.00–1.80 (3.1–5.5) Human urine 3 40.4 (125) 0.5 (2) 1.3
10–12 y 1.05–1.85 (3.2–5.7) 1.05–1.70 (3.3–5.3) Human urine 4 6.23 (19.3) 0.12 (0.4) 2.0
13–15 y 0.95–1.65 (2.9–5.1) 0.90–1.55 (2.8–4.8) Method comparison
16–18 y 0.85–1.60 (2.7–4.9) 0.80–1.55 (2.5–4.8) Inorganic phosphate values for human serum, plasma and urine samples
obtained on a Roche/Hitachi cobas c 501 analyzer (y) were compared with
Roche has not evaluated reference ranges in a pediatric population. those determined using the corresponding reagent on a Roche/Hitachi 917
analyzer (x).
Urine Serum/plasma
1st morning urine16 13‑44 mmol/L (40‑136 mg/dL) Sample size (n) = 150
24‑hour urine6 13‑42 mmol/d (0.4‑1.3 g/d)
Passing/Bablok17 Linear regression
Each laboratory should investigate the transferability of the expected values
to its own patient population and if necessary determine its own reference y = 1.022x + 0.000 mmol/L y = 1.023x - 0.002 mmol/L
ranges. τ = 0.978 r = 1.000
Specific performance data The sample concentrations were between 0.62 and 5.54 mmol/L (1.92 and
Representative performance data on the analyzers are given below. 17.2 mg/dL).
Results obtained in individual laboratories may differ.
Urine
Sample size (n) = 145
4/5 2019-07, V 9.0 English
0003183793122c501V9.0
PHOS2
Phosphate (Inorganic) ver.2
Passing/Bablok17 Linear regression FOR US CUSTOMERS ONLY: LIMITED WARRANTY
y = 0.976x - 0.053 mmol/L y = 0.974x - 0.047 mmol/L Roche Diagnostics warrants that this product will meet the specifications
stated in the labeling when used in accordance with such labeling and will
τ = 0.967 r = 0.999 be free from defects in material and workmanship until the expiration date
The sample concentrations were between 1.61 and 91.5 mmol/L (4.99 and printed on the label. THIS LIMITED WARRANTY IS IN LIEU OF ANY
284 mg/dL). OTHER WARRANTY, EXPRESS OR IMPLIED, INCLUDING ANY IMPLIED
References WARRANTY OF MERCHANTABILITY OR FITNESS FOR PARTICULAR
1 Külpmann WR, Stummvoll HK, Lehmann P. Elektrolyte, Klinik und PURPOSE. IN NO EVENT SHALL ROCHE DIAGNOSTICS BE LIABLE
Labor. Heidelberg: Verlag Klinisches Labor 1993. FOR INCIDENTAL, INDIRECT, SPECIAL OR CONSEQUENTIAL
2 Tietz NW, ed. Fundamentals of Clinical Chemistry Philadelphia, PA: DAMAGES.
WB Saunders Company 1976;901. COBAS, COBAS C, PRECICONTROL, PRECINORM and PRECIPATH are trademarks of Roche.
All other product names and trademarks are the property of their respective owners.
3 Fiske CH, Subbarow Y. The colorimetric determination of phosphorus. Additions, deletions or changes are indicated by a change bar in the margin.
J Biol Chem 1925;66:375-400.
© 2019, Roche Diagnostics
4 Taussky HH, Schoor EA. A microcolorimetric method for the
determination of inorganic phosphorus. J Biol Chem 1953;202:675.
5 Henry R ed. Clinical Chemistry: Principles and Technics, 2nd ed. New
York, NY: Harper & Row 1974;723. Roche Diagnostics GmbH, Sandhofer Strasse 116, D-68305 Mannheim
www.roche.com
6 Tietz NW, ed. Clinical Guide to Laboratory Tests, 4th ed.
Philadelphia.WB Saunders Co 2006;852-855. Distribution in USA by:
Roche Diagnostics, Indianapolis, IN
7 NCCLS GP-16A2, Urineanalysis and Collection, Transportation and US Customer Technical Support 1-800-428-2336
Preservation of Urine specimens, 2nd edition 2001.
8 Use of Anticoagulants in Diagnostic Laboratory Investigations. WHO
Publication WHO/DIL/LAB/99.1 Rev. 2: Jan 2002.
9 Glick MR, Ryder KW, Jackson SA. Graphical Comparisons of
Interferences in Clinical Chemistry Instrumentation. Clin Chem
1986;32:470-475.
10 Breuer J. Report on the Symposium “Drug effects in Clinical Chemistry
Methods”. Eur J Clin Chem Clin Biochem 1996;34:385-386.
11 Sonntag O, Scholer A. Drug interference in clinical chemistry:
recommendation of drugs and their concentrations to be used in drug
interference studies. Ann Clin Biochem 2001;38:376-385.
12 Lane JW, Rehak NN, Hortin GL, et al. Pseudohyperphosphatemia
associated with high-dose liposomal amphotericin B therapy. Clin Chim
Acta 2008;387:145-149.
13 Bakker AJ, Mücke M. Gammopathy interference in clinical chemistry
assays: mechanisms, detection and prevention.
Clin Chem Lab Med 2007;45(9):1240-1243.
14 Burtis CA, Ashwood ER, Bruns DE (eds.). Tietz Textbook of Clinical
Chemistry and Molecular Diagnostics, 4th ed. St Louis, Missouri;
Elsevier Saunders 2006;2290.
15 Soldin JS, Brugnara C, Wong EC. Pediatric Reference Intervals. AACC
Press. 2005, 5th ed., p. 153.
16 Krieg M, Gunsser KJ, Steinhagen-Thiessen E, et al. Vergleichende
quantitative Analytik klinisch-chemischer Kenngrößen im 24-Stunden-
Urin und Morgenurin. J Clin Chem Clin Biochem 1986
Nov;24(11):863-869.
17 Bablok W, Passing H, Bender R, et al. A general regression procedure
for method transformation. Application of linear regression procedures
for method comparison studies in clinical chemistry, Part III. J Clin
Chem Clin Biochem 1988 Nov;26(11):783-790.
A point (period/stop) is always used in this Method Sheet as the decimal
separator to mark the border between the integral and the fractional parts of
a decimal numeral. Separators for thousands are not used.
Symbols
Roche Diagnostics uses the following symbols and signs in addition to
those listed in the ISO 15223‑1 standard (for USA: see
https://usdiagnostics.roche.com for definition of symbols used):
Contents of kit
Volume after reconstitution or mixing
GTIN Global Trade Item Number
2019-07, V 9.0 English 5/5
You might also like
- MSDS Bolidt Primer Pu-Lp 2580 (01 B en GHS)Document11 pagesMSDS Bolidt Primer Pu-Lp 2580 (01 B en GHS)BradyNo ratings yet
- BP s25 Wwta-DataDocument20 pagesBP s25 Wwta-DatajnmanivannanNo ratings yet
- AISI Steel Plate Engineering Data Vol1&2 2012 PDFDocument134 pagesAISI Steel Plate Engineering Data Vol1&2 2012 PDFJose Felix AcevedoNo ratings yet
- Insert ALP2 0003333752190c501 V8 enDocument4 pagesInsert ALP2 0003333752190c501 V8 enAnonymous F50PFE3No ratings yet
- ALPDocument4 pagesALPRastu KaryanaNo ratings yet
- c311 ALP2 enDocument3 pagesc311 ALP2 endr. SheryarOrakzaiNo ratings yet
- Magnesium CobasDocument5 pagesMagnesium CobasMarcellia AngelinaNo ratings yet
- TP2 501Document4 pagesTP2 501hairiNo ratings yet
- Ua 702Document5 pagesUa 702hairiNo ratings yet
- Co2 LDocument3 pagesCo2 LARIF AHAMMED P100% (1)
- Lact2 2018-11 v12Document4 pagesLact2 2018-11 v12Kouame FrancisNo ratings yet
- Urea 501Document5 pagesUrea 501hairiNo ratings yet
- Apobt: Nacl Diluent 9%Document3 pagesApobt: Nacl Diluent 9%Yunita RapaNo ratings yet
- Tpuc 501Document4 pagesTpuc 501hairiNo ratings yet
- APOAT enDocument3 pagesAPOAT enYunita RapaNo ratings yet
- Determination of Phosphate in Clinical SamplesDocument3 pagesDetermination of Phosphate in Clinical SamplesDaria VîrticNo ratings yet
- Ua 501Document5 pagesUa 501hairiNo ratings yet
- Alb2 BCG 2015-03 v10 0Document4 pagesAlb2 BCG 2015-03 v10 0KOUAME EDYMAIN FRANCISNo ratings yet
- PI e BICARB 16Document2 pagesPI e BICARB 16Jaydev DegloorkarNo ratings yet
- ALB2Document4 pagesALB2Jonalyn SalandoNo ratings yet
- PI e BICARB 15Document2 pagesPI e BICARB 15Khuon BunthaNo ratings yet
- CalciumDocument5 pagesCalciumDrAlaa ZidanNo ratings yet
- Lab Policies Alkaline Phosphatase C311 Lab 8803Document4 pagesLab Policies Alkaline Phosphatase C311 Lab 8803Valdez Francis ZaccheauNo ratings yet
- CalibradorDocument4 pagesCalibradorjuanNo ratings yet
- Insert PREA 0108252645190c503 V4 enDocument3 pagesInsert PREA 0108252645190c503 V4 enVegha NedyaNo ratings yet
- Ureal 2020-01 v13 0Document5 pagesUreal 2020-01 v13 0Kouame FrancisNo ratings yet
- Inserto Gluc3 HK RocheDocument4 pagesInserto Gluc3 HK RocheBruno ValeraNo ratings yet
- Common Buffers, Media, and Stock SolutionsDocument13 pagesCommon Buffers, Media, and Stock SolutionsRedondoself100% (3)
- AN 280 IC Carbohydrates Coffee HPAE PAD AN70231 - EDocument12 pagesAN 280 IC Carbohydrates Coffee HPAE PAD AN70231 - EgramdagpinNo ratings yet
- AN 280 IC Carbohydrates Coffee HPAE PAD AN70231 ENDocument12 pagesAN 280 IC Carbohydrates Coffee HPAE PAD AN70231 ENjoann bNo ratings yet
- 11 CholesterolDocument8 pages11 CholesterolAzhar Clinical Laboratory TubeNo ratings yet
- Ureal: GLDH 4 2Document8 pagesUreal: GLDH 4 2CarinaVillasantiNo ratings yet
- Acid Phosphatase: Orthophosphoric - Monoester Phospho-HydrolaseDocument1 pageAcid Phosphatase: Orthophosphoric - Monoester Phospho-HydrolaseMaherNo ratings yet
- Bitertanol 2Document4 pagesBitertanol 2SureshCoolNo ratings yet
- Alkaline Phosphatase FS : Order Information SpecimenDocument3 pagesAlkaline Phosphatase FS : Order Information SpecimenmnemonicsNo ratings yet
- Bilt3 2017-08 v7Document4 pagesBilt3 2017-08 v7Kouame FrancisNo ratings yet
- Amyl2: A) PNP P Nitrophenol B) G GlucoseDocument5 pagesAmyl2: A) PNP P Nitrophenol B) G Glucosesinghranjanr5748No ratings yet
- Roche GlucoseDocument4 pagesRoche GlucoseDiep LeNo ratings yet
- CreaDocument5 pagesCreaKouame Francis0% (1)
- UA2 enDocument4 pagesUA2 enhilmayuniarNo ratings yet
- Insert TRIGB 0011877771216c501 V7 enDocument5 pagesInsert TRIGB 0011877771216c501 V7 enGuneyden GuneydenNo ratings yet
- 10 AlciumDocument9 pages10 AlciumAzhar Clinical Laboratory TubeNo ratings yet
- PI e AST 2Document3 pagesPI e AST 2Cindy Mae A. PogoyNo ratings yet
- Namratha FinalDocument56 pagesNamratha FinalAkhil KattamuriNo ratings yet
- AAT2 enDocument3 pagesAAT2 enSyahdie FahledieNo ratings yet
- 562ue 2014-06Document55 pages562ue 2014-06vijayramaswamyNo ratings yet
- Alkaline Phosphatase ALP Reagent ENDocument2 pagesAlkaline Phosphatase ALP Reagent ENكن مع اللهNo ratings yet
- Kit Insert CK-NAC (IFCC) Single VialDocument2 pagesKit Insert CK-NAC (IFCC) Single VialsindiNo ratings yet
- Ck-Nac: IFCC Single VialDocument2 pagesCk-Nac: IFCC Single VialFariz KasyidiNo ratings yet
- Ck-Nac FsDocument2 pagesCk-Nac Fsadamalay wardiwiraNo ratings yet
- USP-NF Acetaminophen and Codeine Phosphate Oral SolutionDocument3 pagesUSP-NF Acetaminophen and Codeine Phosphate Oral SolutionStalin VacaNo ratings yet
- Application Note: Determination of C2-C12 Aldehydes in Water by SPME On-Fiber Derivatiza-Tion and GC/MSDocument6 pagesApplication Note: Determination of C2-C12 Aldehydes in Water by SPME On-Fiber Derivatiza-Tion and GC/MSAli AhmedNo ratings yet
- Sodium: Enzymatic MethodDocument2 pagesSodium: Enzymatic MethodFariz KasyidiNo ratings yet
- En - Alkaline PhosphataseDocument4 pagesEn - Alkaline PhosphatasecarineNo ratings yet
- EN LIPASE BAOSR6x30Document3 pagesEN LIPASE BAOSR6x30محمد عبدالواسعNo ratings yet
- Alkaline Phosphatase Stable LiquidDocument1 pageAlkaline Phosphatase Stable LiquidRakib Hossain 3A-159No ratings yet
- Calcium P FSDocument2 pagesCalcium P FSKang SoloNo ratings yet
- Application Note: A Cleaning Validation Swab Recovery Study Using A UV/Persulfate AnalyzerDocument4 pagesApplication Note: A Cleaning Validation Swab Recovery Study Using A UV/Persulfate AnalyzerPrianurraufikachmadNo ratings yet
- TG 702Document4 pagesTG 702hairiNo ratings yet
- Fluoraldehyde OPA Reag Solution UG8!31!17Document2 pagesFluoraldehyde OPA Reag Solution UG8!31!17AROMAL NATHNo ratings yet
- US10113060Document22 pagesUS10113060jituniNo ratings yet
- CCW - Common Cooling System ProblemsDocument59 pagesCCW - Common Cooling System Problemszerocool86No ratings yet
- Laser Vapour Deposition & Plasma Enhanced DepositionDocument21 pagesLaser Vapour Deposition & Plasma Enhanced DepositionPradeep76448No ratings yet
- CPCB NormsDocument95 pagesCPCB NormssurendharNo ratings yet
- Thickening and Gelling AgentsDocument10 pagesThickening and Gelling AgentsHemasriNo ratings yet
- Market and Legislation: Essential OilsDocument10 pagesMarket and Legislation: Essential OilsKarina Ariana MariniNo ratings yet
- AGRIC SC P1 QP GR11 NOV 2018 - English 1Document16 pagesAGRIC SC P1 QP GR11 NOV 2018 - English 1reconcilemalele3No ratings yet
- Rapid Detection of Milk ConstituentsDocument12 pagesRapid Detection of Milk ConstituentsNihal AhmadNo ratings yet
- OM For MES Sulfonation Plant Rev 0Document184 pagesOM For MES Sulfonation Plant Rev 0Harits Eka FebriyantoNo ratings yet
- Asphalt Mix Design-Marshall Method: Rajib Chattaraj Astt. Chief Engineer, NH, PW (R) DDocument42 pagesAsphalt Mix Design-Marshall Method: Rajib Chattaraj Astt. Chief Engineer, NH, PW (R) DPriyadarshini Saha Chowdhury100% (1)
- Product Information Sheet: Synthite Industries Private LimitedDocument2 pagesProduct Information Sheet: Synthite Industries Private LimitedMaurice Dan GeroyNo ratings yet
- CHEM Laboratory ManualDocument164 pagesCHEM Laboratory ManualCarlos José Lacava FernándezNo ratings yet
- Ffe - Weekly - Monthly Maintenance & Inspection PG.1Document2 pagesFfe - Weekly - Monthly Maintenance & Inspection PG.1Gerome Eugenio100% (1)
- Lecture1 CH317 2020 Fall Statistics Part4 GGclasssDocument21 pagesLecture1 CH317 2020 Fall Statistics Part4 GGclasssshanicejames7867No ratings yet
- Alucobest Aluminum Composite Panel For Architectural & BuildingDocument12 pagesAlucobest Aluminum Composite Panel For Architectural & BuildingAli ZhangNo ratings yet
- Binders For: Architectural CoatingsDocument8 pagesBinders For: Architectural CoatingsAPEX SON100% (1)
- Mohdsalehuddin 2021Document13 pagesMohdsalehuddin 2021mihovilNo ratings yet
- Mesbah - 2022 - Industrial Biotechnology Based On Enzymes From Extreme EnvironmentsDocument16 pagesMesbah - 2022 - Industrial Biotechnology Based On Enzymes From Extreme EnvironmentsFrancisco Luciano Issotta ContardoNo ratings yet
- Amberlyst 15 Dry H Form CAS NO 39389-20-3: Material Safety Data Sheet Sds/MsdsDocument6 pagesAmberlyst 15 Dry H Form CAS NO 39389-20-3: Material Safety Data Sheet Sds/MsdsMuhammad Dion ArfiNo ratings yet
- Pengaruh Penambahan Etanol Dan Lama Fermentasi Lanjutan Cairan Pulpa Hasil Samping Fermentasi Biji Kakao Terhadap Karakteristik Cuka KakaoDocument11 pagesPengaruh Penambahan Etanol Dan Lama Fermentasi Lanjutan Cairan Pulpa Hasil Samping Fermentasi Biji Kakao Terhadap Karakteristik Cuka KakaoAgus PurnamaNo ratings yet
- EnzymesDocument11 pagesEnzymesJustine UrbanNo ratings yet
- Technical: Data SheetDocument2 pagesTechnical: Data SheetTan Yann JiunNo ratings yet
- Job Clean Supplies Official Price List 1Document4 pagesJob Clean Supplies Official Price List 1Lee GonzalgoNo ratings yet
- QTnhNlaP WMnh2Document7 pagesQTnhNlaP WMnh2choilicious0816No ratings yet
- Pressure Regulator, Series NL2-RGSDocument3 pagesPressure Regulator, Series NL2-RGSHuynh Duc TriNo ratings yet
- 2Document2 pages2Mohamad YasinNo ratings yet
- Mineral Fillers in RubberDocument47 pagesMineral Fillers in RubberDarshan ShahNo ratings yet
- Ganga - SlideDocument39 pagesGanga - Slideompoultryfirm3No ratings yet