Professional Documents
Culture Documents
0 ratings0% found this document useful (0 votes)
11 viewsEmergency Severity Index LEC MLT 2 10 24
Emergency Severity Index LEC MLT 2 10 24
Uploaded by
SJane FeriaThis document discusses the Emergency Severity Index (ESI), which is used to prioritize patients in emergency departments. The ESI was developed in the 1990s to [1] prioritize incoming patients, [2] identify those who cannot wait to be seen, and [3] help determine how long a patient can safely wait for treatment. It categorizes patients into 5 levels based on acuity and resource needs, with Level 1 being the most urgent/acute patients requiring immediate lifesaving intervention. The ESI aims to maximize appropriate allocation of resources and get patients to the right level of care in a timely manner.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You might also like
- OSCE Preconception CounsellingDocument2 pagesOSCE Preconception Counsellinglatiffidalila100% (7)
- Triage in The Emergency Department With PostersDocument27 pagesTriage in The Emergency Department With PostersSoleh RamlyNo ratings yet
- Para-Cleanse P65 PDFDocument10 pagesPara-Cleanse P65 PDFAntonija100% (1)
- ESI ER CompleteDocument45 pagesESI ER Completetammy2121No ratings yet
- Early Warning Score For Patient Safety Measures - Mohd Said NurumalDocument50 pagesEarly Warning Score For Patient Safety Measures - Mohd Said NurumalAiko himeNo ratings yet
- Implementation Guidelines For The Canadian Emergency Department Triage & Acuity Scale (CTAS)Document27 pagesImplementation Guidelines For The Canadian Emergency Department Triage & Acuity Scale (CTAS)Jery JsNo ratings yet
- TriageDocument40 pagesTriagemody94546No ratings yet
- Newly Revise Emergency Nursing 1Document65 pagesNewly Revise Emergency Nursing 1Mikee PaningbatanNo ratings yet
- Assessment of The Severity of The ConditionDocument26 pagesAssessment of The Severity of The ConditioncrazieelorraNo ratings yet
- Emergency Severity Index: Adlyn Bea A. Bernaldez, MD Second Year Family Medicine BihmiDocument35 pagesEmergency Severity Index: Adlyn Bea A. Bernaldez, MD Second Year Family Medicine BihmiAdlyn Bea Albesa-BernaldezNo ratings yet
- Introduction To Ews (Early Warning Scores) : DR Rachael Lucas Teaching Fellow Focp 2016 at SRHDocument30 pagesIntroduction To Ews (Early Warning Scores) : DR Rachael Lucas Teaching Fellow Focp 2016 at SRHPetros Akin-NibosunNo ratings yet
- Triage in Emergency Department: Triage Waiting Room Team LeaderDocument27 pagesTriage in Emergency Department: Triage Waiting Room Team LeaderJerry AbleNo ratings yet
- Triage (Emergency Department)Document24 pagesTriage (Emergency Department)AnnNo ratings yet
- Mass Casualty Incident (MCI) ResponseDocument25 pagesMass Casualty Incident (MCI) ResponseMary Joy GarciaNo ratings yet
- Early Warning Score & Rapid Response TeamDocument26 pagesEarly Warning Score & Rapid Response TeamAsim IdreesNo ratings yet
- Emergency Nursing: By: Keverne Jhay P. ColasDocument61 pagesEmergency Nursing: By: Keverne Jhay P. ColasGaras AnnaBerniceNo ratings yet
- Triage in Emergency DepartmentDocument25 pagesTriage in Emergency DepartmentLourdelina Techap100% (1)
- Triage Level 5Document78 pagesTriage Level 5DanielKnows100% (1)
- Triage AkhirDocument40 pagesTriage AkhirputuNo ratings yet
- ESI Triage by Dr. Ryan MiranoDocument34 pagesESI Triage by Dr. Ryan MiranoEarl Kristoffer PiranteNo ratings yet
- TRIAGE Skills LabDocument8 pagesTRIAGE Skills Labczeremar chanNo ratings yet
- A Triage Scale PDFDocument13 pagesA Triage Scale PDFQueeiin NeeshaNo ratings yet
- Examples of Triage ConditionsDocument9 pagesExamples of Triage ConditionsDevi Christina Damanik (Papua medical School)No ratings yet
- Module1 Emergency BasicDocument3 pagesModule1 Emergency Basicmitchie riveraNo ratings yet
- The Canadian Triage and Acuity Scale: Education Manual: Version 2.5, 2012Document38 pagesThe Canadian Triage and Acuity Scale: Education Manual: Version 2.5, 2012abdullahmushlihNo ratings yet
- Early Recognittion of The Critically Ill PatientsDocument26 pagesEarly Recognittion of The Critically Ill PatientsDeviana HidayatiNo ratings yet
- Emergency NursingDocument52 pagesEmergency NursingJohnryl Francisco100% (1)
- Upana Critical Care TrialDocument15 pagesUpana Critical Care TrialScribdTranslationsNo ratings yet
- 2 Critical Care UnitDocument59 pages2 Critical Care UnitPALMA , JULIA A.No ratings yet
- ESI TRIAGEDocument31 pagesESI TRIAGEbpdh.nursingserviceNo ratings yet
- Triaging Seminar: Pesenter:Dr Balemlay Hailu (Eccm R1 Moderator:Dr Yonas (Assistant Professor of EccmDocument36 pagesTriaging Seminar: Pesenter:Dr Balemlay Hailu (Eccm R1 Moderator:Dr Yonas (Assistant Professor of EccmBalemlay HailuNo ratings yet
- Emergency Nursing TeachingDocument32 pagesEmergency Nursing TeachingBrian Jay Enriquez CalibotNo ratings yet
- TriageDocument6 pagesTriageWindyNo ratings yet
- Triage in Emergency DepartmentDocument139 pagesTriage in Emergency DepartmentEddy Liem100% (2)
- Extended and Expanded Role of Nurse in EmergencyDocument23 pagesExtended and Expanded Role of Nurse in Emergencyankita guptaNo ratings yet
- QDocument541 pagesQAmeer Youseff MarotoNo ratings yet
- Printed 9Document63 pagesPrinted 9Melodia Turqueza GandezaNo ratings yet
- Critical Care NursingDocument41 pagesCritical Care NursingAbirajan50% (2)
- COP Care of PatientsDocument48 pagesCOP Care of PatientsDr. Vijay Desai QualityNo ratings yet
- Emergency Nursing Practice in Hospital FacilitiesDocument33 pagesEmergency Nursing Practice in Hospital FacilitiesDidz BalibayNo ratings yet
- Nursing Care of Clients in Emergency Situation 1Document120 pagesNursing Care of Clients in Emergency Situation 1Mary Joy FrancoNo ratings yet
- Emergency Care in NursingDocument32 pagesEmergency Care in NursingPauline Añes100% (1)
- Triage Lecture DR F Mesa GaerlanDocument55 pagesTriage Lecture DR F Mesa Gaerlanapi-19431894100% (1)
- Prelims 118 SkillsDocument17 pagesPrelims 118 SkillsKrizzia Angela BacotocNo ratings yet
- Emergency and Disasater NursingDocument96 pagesEmergency and Disasater Nursingblacknurse100% (3)
- Harley L. Dela Cruz, RN LecturerDocument110 pagesHarley L. Dela Cruz, RN LecturerHarley Justiniani Dela CruzNo ratings yet
- Emergency Nursing2Document34 pagesEmergency Nursing2Nina Oaip100% (1)
- EmergancyDocument60 pagesEmergancyKhalid KhairyNo ratings yet
- Triage 1546Document26 pagesTriage 1546Santosh ThapaNo ratings yet
- TRIAGE Lecture + Scenarios (2Document27 pagesTRIAGE Lecture + Scenarios (2aliNo ratings yet
- Tertiary AssessmentDocument14 pagesTertiary AssessmentAngelie PantajoNo ratings yet
- Esi Validacion EuropaDocument6 pagesEsi Validacion EuropaPaullette SanjuanNo ratings yet
- Emergency Nursing PDFDocument39 pagesEmergency Nursing PDFJustin John NavarroNo ratings yet
- Esi Triage by DR Ryan MiranoDocument33 pagesEsi Triage by DR Ryan MiranofadiNo ratings yet
- BencanaDocument5 pagesBencanazakyNo ratings yet
- Clinical case in the emergency room of a patient with an ischemic strokeFrom EverandClinical case in the emergency room of a patient with an ischemic strokeNo ratings yet
- Textbook of Urgent Care Management: Chapter 39, Ensuring Patient SafetyFrom EverandTextbook of Urgent Care Management: Chapter 39, Ensuring Patient SafetyNo ratings yet
- Developing Advanced Assessment Skills: Patients with Long Term ConditionsFrom EverandDeveloping Advanced Assessment Skills: Patients with Long Term ConditionsNo ratings yet
- Head and NeckDocument41 pagesHead and NeckSJane FeriaNo ratings yet
- LAWS AND REGULATIONS DISASTER NURSING REVIEWERDocument2 pagesLAWS AND REGULATIONS DISASTER NURSING REVIEWERSJane FeriaNo ratings yet
- Chapter 3 Module Therapeutic CommunicationDocument6 pagesChapter 3 Module Therapeutic CommunicationSJane FeriaNo ratings yet
- ACE AND ARBs PRACTICE QUESTIONS HIghlightedDocument2 pagesACE AND ARBs PRACTICE QUESTIONS HIghlightedSJane FeriaNo ratings yet
- 1ST Term SummaryDocument5 pages1ST Term SummarySJane FeriaNo ratings yet
- 3 Acid Base ImbalanceDocument5 pages3 Acid Base ImbalanceSJane FeriaNo ratings yet
- 4 - CoparDocument4 pages4 - CoparSJane FeriaNo ratings yet
- 4 Neurologic Nursing DisordersDocument4 pages4 Neurologic Nursing DisordersSJane FeriaNo ratings yet
- Disaster Preparedness 1Document10 pagesDisaster Preparedness 1SJane FeriaNo ratings yet
- CD Cheat Sheet CompleteDocument6 pagesCD Cheat Sheet CompleteSJane FeriaNo ratings yet
- Endo SummarizedDocument8 pagesEndo SummarizedSJane FeriaNo ratings yet
- Neurologic NursingDocument3 pagesNeurologic NursingSJane FeriaNo ratings yet
- TRANSCULTURALDocument5 pagesTRANSCULTURALSJane FeriaNo ratings yet
- Chem and Hazmat MCI 2 13 24Document50 pagesChem and Hazmat MCI 2 13 24SJane FeriaNo ratings yet
- MicroPara LabDocument2 pagesMicroPara LabSJane FeriaNo ratings yet
- Urinary System1Document4 pagesUrinary System1SJane FeriaNo ratings yet
- Four Basic Models of Health CareDocument2 pagesFour Basic Models of Health CareAazeen memonNo ratings yet
- Proposal For Mental HealthDocument5 pagesProposal For Mental HealthKristine CastroNo ratings yet
- Exploring Concerns of Children With CancerDocument7 pagesExploring Concerns of Children With CancerVanessa SilvaNo ratings yet
- CORTEZ LoaloaDocument12 pagesCORTEZ LoaloaLouisa Marie Miranda100% (1)
- FINALDocument35 pagesFINALMark Justine ComendadorNo ratings yet
- Nbme Medicine Shelf Review Session 2Document142 pagesNbme Medicine Shelf Review Session 2Swisskelly1100% (1)
- Technology and Livelihood Education: Quarter 1 - Module 4: CaregivingDocument20 pagesTechnology and Livelihood Education: Quarter 1 - Module 4: CaregivingIrine Irine100% (1)
- StabilityDocument3 pagesStabilitykinsonprabuNo ratings yet
- Cryptococcosis: Dr.C.Meenakshisundaram.Document16 pagesCryptococcosis: Dr.C.Meenakshisundaram.Meenakshisundaram CNo ratings yet
- Faith Ezekiel College of Health IdahDocument43 pagesFaith Ezekiel College of Health IdahZedek PeterNo ratings yet
- TFN MidtermDocument7 pagesTFN MidtermDimple Lexiry GloriaNo ratings yet
- Assessing Body Temperatur1Document2 pagesAssessing Body Temperatur1juancristoNo ratings yet
- 페이지 포함 파일 - (변형 1부) 2023년 6월 고2 모의고사 (대의파악, 내용일치)Document11 pages페이지 포함 파일 - (변형 1부) 2023년 6월 고2 모의고사 (대의파악, 내용일치)히부No ratings yet
- Xavier University Gen Biology 1 Performance Task: Instructor: Mr. EdgarDocument4 pagesXavier University Gen Biology 1 Performance Task: Instructor: Mr. EdgarChin T. OndongNo ratings yet
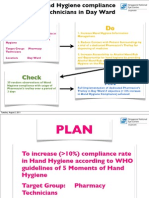
- PDCA ProjectDocument5 pagesPDCA ProjectAlan LeeNo ratings yet
- AyurvedaDocument2 pagesAyurvedaNizamuddin AhmadNo ratings yet
- Adult Early Warning Score Observation Chart For Cardiology UnitDocument1 pageAdult Early Warning Score Observation Chart For Cardiology UnitalexipsNo ratings yet
- 2021 08 21 07-03-33 AmDocument1 page2021 08 21 07-03-33 AmMohammad Masum HosenNo ratings yet
- Dr. Med. Reinhard Smettan Dr. Med. Heike Smettan: GemeinschaftspraxisDocument46 pagesDr. Med. Reinhard Smettan Dr. Med. Heike Smettan: GemeinschaftspraxiselrhavNo ratings yet
- LFD Ob WardDocument2 pagesLFD Ob WardMaria Althea Najorra100% (1)
- The Tanzania Food, Drugs and Cosmetics Act, 2003Document89 pagesThe Tanzania Food, Drugs and Cosmetics Act, 2003ananthNo ratings yet
- HayeSep Q Packed GC ColumnDocument10 pagesHayeSep Q Packed GC ColumnSpyr TourNo ratings yet
- Identifying Clients at RiskDocument5 pagesIdentifying Clients at RiskMaryela Maceda GalozoNo ratings yet
- Labor Code Book IVDocument17 pagesLabor Code Book IVJestoni PabiaNo ratings yet
- Shining The Light On Wound Care Symposium: March 15-16, 2020Document12 pagesShining The Light On Wound Care Symposium: March 15-16, 2020Nidhin JoseNo ratings yet
- UntitledDocument9 pagesUntitledfirda ningsiNo ratings yet
- Mmir 2020 04 14 PDFDocument16 pagesMmir 2020 04 14 PDFwrite2ameyNo ratings yet
- Rest Readiness Checklist: Child and Family Suitability QuestionsDocument1 pageRest Readiness Checklist: Child and Family Suitability QuestionsgurriaaliNo ratings yet
Emergency Severity Index LEC MLT 2 10 24
Emergency Severity Index LEC MLT 2 10 24
Uploaded by
SJane Feria0 ratings0% found this document useful (0 votes)
11 views27 pagesThis document discusses the Emergency Severity Index (ESI), which is used to prioritize patients in emergency departments. The ESI was developed in the 1990s to [1] prioritize incoming patients, [2] identify those who cannot wait to be seen, and [3] help determine how long a patient can safely wait for treatment. It categorizes patients into 5 levels based on acuity and resource needs, with Level 1 being the most urgent/acute patients requiring immediate lifesaving intervention. The ESI aims to maximize appropriate allocation of resources and get patients to the right level of care in a timely manner.
Original Description:
Original Title
Emergency-Severity-Index-LEC-mlt-2-10-24
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document discusses the Emergency Severity Index (ESI), which is used to prioritize patients in emergency departments. The ESI was developed in the 1990s to [1] prioritize incoming patients, [2] identify those who cannot wait to be seen, and [3] help determine how long a patient can safely wait for treatment. It categorizes patients into 5 levels based on acuity and resource needs, with Level 1 being the most urgent/acute patients requiring immediate lifesaving intervention. The ESI aims to maximize appropriate allocation of resources and get patients to the right level of care in a timely manner.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
11 views27 pagesEmergency Severity Index LEC MLT 2 10 24
Emergency Severity Index LEC MLT 2 10 24
Uploaded by
SJane FeriaThis document discusses the Emergency Severity Index (ESI), which is used to prioritize patients in emergency departments. The ESI was developed in the 1990s to [1] prioritize incoming patients, [2] identify those who cannot wait to be seen, and [3] help determine how long a patient can safely wait for treatment. It categorizes patients into 5 levels based on acuity and resource needs, with Level 1 being the most urgent/acute patients requiring immediate lifesaving intervention. The ESI aims to maximize appropriate allocation of resources and get patients to the right level of care in a timely manner.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 27
Emergency Severity Index
Arranged by: MLTominez
Purpose
• Prioritize in coming patient in the Emergency
Department
• Identify those who cannot wait to be seen
• Brief focused assessment
• How long can patient safely wait for a medical
screening
• In 2008 there were 123.8 million visits of patients in the ED’s (USA)
• CDC data – only 18% of patients were seen within 15 min, leaving
majority of the patients in the waiting room
• Worsening crisis
• Worldwide problem
• Leaves the patient for worsening conditions
BRIEF HISTORY
• Develop by two ED Physicians (Richard Wuerz and David
Eitel)
• Who should be seen first?
• How long can a patient safely wait?
• Became the traditional foundation of initially evaluating
patient urgency.
• Maximize getting the right patient to the right resources at
right place and the right time.
RESEARCH
•ESI proved that it easier to be used by
practicing nurses and it had a faster turn
– over of patients to other units
whatever the case of the patient is.
BENEFITS
• Rapid identification of patients that need immediate
attention
• Level 1 and level 2 patients can be treated in the high
dependency units of the ED.
• Determination of patients do not need to be seen in
the main ED. (ESI level 4 and 5)
Emergency Severity Index (ESI) Levels
A. Immediate life-saving intervention required:
airway, emergency medications, or other hemodynamic
interventions (IV, supplemental O2, monitor, ECG
or labs DO NOT count);
• and/or any of the following clinical conditions: intubated, ap
neic,
• pulseless, severe respiratory distress, SPO2<90, acute mental
status changes, or unresponsive.
Unresponsiveness is defined as a patient that is either:
(1) nonverbal and not following commands (acutely); or
(2) requires noxious stimulus.
B. High risk situation -
is a patient you would put in your last
open bed.
• Severe pain/distress is determined by cli
nical observation and/or patient rating of
greater than or equal
to 7 on 0-10 pain scale.
• C. Resources:
• Count the number of different types of re
sources, not the individual
• tests or x-rays
• Examples: CBC, electrolytes and coags equ
als one resource.
• CBC plus chest x-ray equals two resources.
POCT as: “testing that is
performed near or at the
site of a patient with the
result leading to possible
change in the care of the
patient
blood glucose testing,
blood gas and
electrolytes analysis,
rapid coagulation testing,
rapid cardiac markers
diagnostics, drugs of
abuse screening, urine
strips testing
D. Danger Zone Vital Signs
• Consider up
triage to ESI 2 if any vital sign criterion is exceeded.
Pediatric Fever Considerations
• 1 to 28 days of age: assign at least ESI 2 if temp >3
8.0 C (100.4F)
• 1-3 months of age: consider assigning ESI 2 if temp
• >38.0 C (100.4F)
• 3 months to 3 yrs of age: consider assigning ESI 3 if:
temp >39.0 C (102.2 F),
• or incomplete immunizations, or no obvious source of
fever
Decision Point A: Does the Patient Require Immediate
Life-Saving Intervention?
•If the answer is YES. The triage process is
complete and the patient is automatically
triaged as ESI LEVEL 1
•If NO the patient is put to the next step
ESI LEVEL 1
Examples of patients having ESI level 1
• Cardiac arrest
• Respiratory arrest
• Severe respiratory distress
• SP02 <90%
• Critically injured trauma patent who present unresponsive
• Overdose with RR of 6
• ASRDS gasping pt
• Shock
Decision Point B: Should the Patient Wait?
• The nurse needs to decide whether the patient should
not wait to be seen.
• ESI level 2
3 Broad Questions are used to determine if
the patients meets ESI level 2
• Is this a high – risk situation?
• Is the patient confused,
lethargic or disoriented?
• Is the patient in severe pain or
distress?
ESI LEVEL 2
• The nurse must obtain pertinent
subjective and objective information.
• The patient can develop sudden
deterioration.
• They are required time sensitive
treatment
Examples of ESI Level 2
• Active excruciating pain
• ACS
• Signs of stroke
• Ectopic pregnancy
• Blunt trauma and peritonitis
• Child is sleeping all the time
Decision Point C: Resource Needs
END
You might also like
- OSCE Preconception CounsellingDocument2 pagesOSCE Preconception Counsellinglatiffidalila100% (7)
- Triage in The Emergency Department With PostersDocument27 pagesTriage in The Emergency Department With PostersSoleh RamlyNo ratings yet
- Para-Cleanse P65 PDFDocument10 pagesPara-Cleanse P65 PDFAntonija100% (1)
- ESI ER CompleteDocument45 pagesESI ER Completetammy2121No ratings yet
- Early Warning Score For Patient Safety Measures - Mohd Said NurumalDocument50 pagesEarly Warning Score For Patient Safety Measures - Mohd Said NurumalAiko himeNo ratings yet
- Implementation Guidelines For The Canadian Emergency Department Triage & Acuity Scale (CTAS)Document27 pagesImplementation Guidelines For The Canadian Emergency Department Triage & Acuity Scale (CTAS)Jery JsNo ratings yet
- TriageDocument40 pagesTriagemody94546No ratings yet
- Newly Revise Emergency Nursing 1Document65 pagesNewly Revise Emergency Nursing 1Mikee PaningbatanNo ratings yet
- Assessment of The Severity of The ConditionDocument26 pagesAssessment of The Severity of The ConditioncrazieelorraNo ratings yet
- Emergency Severity Index: Adlyn Bea A. Bernaldez, MD Second Year Family Medicine BihmiDocument35 pagesEmergency Severity Index: Adlyn Bea A. Bernaldez, MD Second Year Family Medicine BihmiAdlyn Bea Albesa-BernaldezNo ratings yet
- Introduction To Ews (Early Warning Scores) : DR Rachael Lucas Teaching Fellow Focp 2016 at SRHDocument30 pagesIntroduction To Ews (Early Warning Scores) : DR Rachael Lucas Teaching Fellow Focp 2016 at SRHPetros Akin-NibosunNo ratings yet
- Triage in Emergency Department: Triage Waiting Room Team LeaderDocument27 pagesTriage in Emergency Department: Triage Waiting Room Team LeaderJerry AbleNo ratings yet
- Triage (Emergency Department)Document24 pagesTriage (Emergency Department)AnnNo ratings yet
- Mass Casualty Incident (MCI) ResponseDocument25 pagesMass Casualty Incident (MCI) ResponseMary Joy GarciaNo ratings yet
- Early Warning Score & Rapid Response TeamDocument26 pagesEarly Warning Score & Rapid Response TeamAsim IdreesNo ratings yet
- Emergency Nursing: By: Keverne Jhay P. ColasDocument61 pagesEmergency Nursing: By: Keverne Jhay P. ColasGaras AnnaBerniceNo ratings yet
- Triage in Emergency DepartmentDocument25 pagesTriage in Emergency DepartmentLourdelina Techap100% (1)
- Triage Level 5Document78 pagesTriage Level 5DanielKnows100% (1)
- Triage AkhirDocument40 pagesTriage AkhirputuNo ratings yet
- ESI Triage by Dr. Ryan MiranoDocument34 pagesESI Triage by Dr. Ryan MiranoEarl Kristoffer PiranteNo ratings yet
- TRIAGE Skills LabDocument8 pagesTRIAGE Skills Labczeremar chanNo ratings yet
- A Triage Scale PDFDocument13 pagesA Triage Scale PDFQueeiin NeeshaNo ratings yet
- Examples of Triage ConditionsDocument9 pagesExamples of Triage ConditionsDevi Christina Damanik (Papua medical School)No ratings yet
- Module1 Emergency BasicDocument3 pagesModule1 Emergency Basicmitchie riveraNo ratings yet
- The Canadian Triage and Acuity Scale: Education Manual: Version 2.5, 2012Document38 pagesThe Canadian Triage and Acuity Scale: Education Manual: Version 2.5, 2012abdullahmushlihNo ratings yet
- Early Recognittion of The Critically Ill PatientsDocument26 pagesEarly Recognittion of The Critically Ill PatientsDeviana HidayatiNo ratings yet
- Emergency NursingDocument52 pagesEmergency NursingJohnryl Francisco100% (1)
- Upana Critical Care TrialDocument15 pagesUpana Critical Care TrialScribdTranslationsNo ratings yet
- 2 Critical Care UnitDocument59 pages2 Critical Care UnitPALMA , JULIA A.No ratings yet
- ESI TRIAGEDocument31 pagesESI TRIAGEbpdh.nursingserviceNo ratings yet
- Triaging Seminar: Pesenter:Dr Balemlay Hailu (Eccm R1 Moderator:Dr Yonas (Assistant Professor of EccmDocument36 pagesTriaging Seminar: Pesenter:Dr Balemlay Hailu (Eccm R1 Moderator:Dr Yonas (Assistant Professor of EccmBalemlay HailuNo ratings yet
- Emergency Nursing TeachingDocument32 pagesEmergency Nursing TeachingBrian Jay Enriquez CalibotNo ratings yet
- TriageDocument6 pagesTriageWindyNo ratings yet
- Triage in Emergency DepartmentDocument139 pagesTriage in Emergency DepartmentEddy Liem100% (2)
- Extended and Expanded Role of Nurse in EmergencyDocument23 pagesExtended and Expanded Role of Nurse in Emergencyankita guptaNo ratings yet
- QDocument541 pagesQAmeer Youseff MarotoNo ratings yet
- Printed 9Document63 pagesPrinted 9Melodia Turqueza GandezaNo ratings yet
- Critical Care NursingDocument41 pagesCritical Care NursingAbirajan50% (2)
- COP Care of PatientsDocument48 pagesCOP Care of PatientsDr. Vijay Desai QualityNo ratings yet
- Emergency Nursing Practice in Hospital FacilitiesDocument33 pagesEmergency Nursing Practice in Hospital FacilitiesDidz BalibayNo ratings yet
- Nursing Care of Clients in Emergency Situation 1Document120 pagesNursing Care of Clients in Emergency Situation 1Mary Joy FrancoNo ratings yet
- Emergency Care in NursingDocument32 pagesEmergency Care in NursingPauline Añes100% (1)
- Triage Lecture DR F Mesa GaerlanDocument55 pagesTriage Lecture DR F Mesa Gaerlanapi-19431894100% (1)
- Prelims 118 SkillsDocument17 pagesPrelims 118 SkillsKrizzia Angela BacotocNo ratings yet
- Emergency and Disasater NursingDocument96 pagesEmergency and Disasater Nursingblacknurse100% (3)
- Harley L. Dela Cruz, RN LecturerDocument110 pagesHarley L. Dela Cruz, RN LecturerHarley Justiniani Dela CruzNo ratings yet
- Emergency Nursing2Document34 pagesEmergency Nursing2Nina Oaip100% (1)
- EmergancyDocument60 pagesEmergancyKhalid KhairyNo ratings yet
- Triage 1546Document26 pagesTriage 1546Santosh ThapaNo ratings yet
- TRIAGE Lecture + Scenarios (2Document27 pagesTRIAGE Lecture + Scenarios (2aliNo ratings yet
- Tertiary AssessmentDocument14 pagesTertiary AssessmentAngelie PantajoNo ratings yet
- Esi Validacion EuropaDocument6 pagesEsi Validacion EuropaPaullette SanjuanNo ratings yet
- Emergency Nursing PDFDocument39 pagesEmergency Nursing PDFJustin John NavarroNo ratings yet
- Esi Triage by DR Ryan MiranoDocument33 pagesEsi Triage by DR Ryan MiranofadiNo ratings yet
- BencanaDocument5 pagesBencanazakyNo ratings yet
- Clinical case in the emergency room of a patient with an ischemic strokeFrom EverandClinical case in the emergency room of a patient with an ischemic strokeNo ratings yet
- Textbook of Urgent Care Management: Chapter 39, Ensuring Patient SafetyFrom EverandTextbook of Urgent Care Management: Chapter 39, Ensuring Patient SafetyNo ratings yet
- Developing Advanced Assessment Skills: Patients with Long Term ConditionsFrom EverandDeveloping Advanced Assessment Skills: Patients with Long Term ConditionsNo ratings yet
- Head and NeckDocument41 pagesHead and NeckSJane FeriaNo ratings yet
- LAWS AND REGULATIONS DISASTER NURSING REVIEWERDocument2 pagesLAWS AND REGULATIONS DISASTER NURSING REVIEWERSJane FeriaNo ratings yet
- Chapter 3 Module Therapeutic CommunicationDocument6 pagesChapter 3 Module Therapeutic CommunicationSJane FeriaNo ratings yet
- ACE AND ARBs PRACTICE QUESTIONS HIghlightedDocument2 pagesACE AND ARBs PRACTICE QUESTIONS HIghlightedSJane FeriaNo ratings yet
- 1ST Term SummaryDocument5 pages1ST Term SummarySJane FeriaNo ratings yet
- 3 Acid Base ImbalanceDocument5 pages3 Acid Base ImbalanceSJane FeriaNo ratings yet
- 4 - CoparDocument4 pages4 - CoparSJane FeriaNo ratings yet
- 4 Neurologic Nursing DisordersDocument4 pages4 Neurologic Nursing DisordersSJane FeriaNo ratings yet
- Disaster Preparedness 1Document10 pagesDisaster Preparedness 1SJane FeriaNo ratings yet
- CD Cheat Sheet CompleteDocument6 pagesCD Cheat Sheet CompleteSJane FeriaNo ratings yet
- Endo SummarizedDocument8 pagesEndo SummarizedSJane FeriaNo ratings yet
- Neurologic NursingDocument3 pagesNeurologic NursingSJane FeriaNo ratings yet
- TRANSCULTURALDocument5 pagesTRANSCULTURALSJane FeriaNo ratings yet
- Chem and Hazmat MCI 2 13 24Document50 pagesChem and Hazmat MCI 2 13 24SJane FeriaNo ratings yet
- MicroPara LabDocument2 pagesMicroPara LabSJane FeriaNo ratings yet
- Urinary System1Document4 pagesUrinary System1SJane FeriaNo ratings yet
- Four Basic Models of Health CareDocument2 pagesFour Basic Models of Health CareAazeen memonNo ratings yet
- Proposal For Mental HealthDocument5 pagesProposal For Mental HealthKristine CastroNo ratings yet
- Exploring Concerns of Children With CancerDocument7 pagesExploring Concerns of Children With CancerVanessa SilvaNo ratings yet
- CORTEZ LoaloaDocument12 pagesCORTEZ LoaloaLouisa Marie Miranda100% (1)
- FINALDocument35 pagesFINALMark Justine ComendadorNo ratings yet
- Nbme Medicine Shelf Review Session 2Document142 pagesNbme Medicine Shelf Review Session 2Swisskelly1100% (1)
- Technology and Livelihood Education: Quarter 1 - Module 4: CaregivingDocument20 pagesTechnology and Livelihood Education: Quarter 1 - Module 4: CaregivingIrine Irine100% (1)
- StabilityDocument3 pagesStabilitykinsonprabuNo ratings yet
- Cryptococcosis: Dr.C.Meenakshisundaram.Document16 pagesCryptococcosis: Dr.C.Meenakshisundaram.Meenakshisundaram CNo ratings yet
- Faith Ezekiel College of Health IdahDocument43 pagesFaith Ezekiel College of Health IdahZedek PeterNo ratings yet
- TFN MidtermDocument7 pagesTFN MidtermDimple Lexiry GloriaNo ratings yet
- Assessing Body Temperatur1Document2 pagesAssessing Body Temperatur1juancristoNo ratings yet
- 페이지 포함 파일 - (변형 1부) 2023년 6월 고2 모의고사 (대의파악, 내용일치)Document11 pages페이지 포함 파일 - (변형 1부) 2023년 6월 고2 모의고사 (대의파악, 내용일치)히부No ratings yet
- Xavier University Gen Biology 1 Performance Task: Instructor: Mr. EdgarDocument4 pagesXavier University Gen Biology 1 Performance Task: Instructor: Mr. EdgarChin T. OndongNo ratings yet
- PDCA ProjectDocument5 pagesPDCA ProjectAlan LeeNo ratings yet
- AyurvedaDocument2 pagesAyurvedaNizamuddin AhmadNo ratings yet
- Adult Early Warning Score Observation Chart For Cardiology UnitDocument1 pageAdult Early Warning Score Observation Chart For Cardiology UnitalexipsNo ratings yet
- 2021 08 21 07-03-33 AmDocument1 page2021 08 21 07-03-33 AmMohammad Masum HosenNo ratings yet
- Dr. Med. Reinhard Smettan Dr. Med. Heike Smettan: GemeinschaftspraxisDocument46 pagesDr. Med. Reinhard Smettan Dr. Med. Heike Smettan: GemeinschaftspraxiselrhavNo ratings yet
- LFD Ob WardDocument2 pagesLFD Ob WardMaria Althea Najorra100% (1)
- The Tanzania Food, Drugs and Cosmetics Act, 2003Document89 pagesThe Tanzania Food, Drugs and Cosmetics Act, 2003ananthNo ratings yet
- HayeSep Q Packed GC ColumnDocument10 pagesHayeSep Q Packed GC ColumnSpyr TourNo ratings yet
- Identifying Clients at RiskDocument5 pagesIdentifying Clients at RiskMaryela Maceda GalozoNo ratings yet
- Labor Code Book IVDocument17 pagesLabor Code Book IVJestoni PabiaNo ratings yet
- Shining The Light On Wound Care Symposium: March 15-16, 2020Document12 pagesShining The Light On Wound Care Symposium: March 15-16, 2020Nidhin JoseNo ratings yet
- UntitledDocument9 pagesUntitledfirda ningsiNo ratings yet
- Mmir 2020 04 14 PDFDocument16 pagesMmir 2020 04 14 PDFwrite2ameyNo ratings yet
- Rest Readiness Checklist: Child and Family Suitability QuestionsDocument1 pageRest Readiness Checklist: Child and Family Suitability QuestionsgurriaaliNo ratings yet