Professional Documents
Culture Documents
A Population-Based Analysis of Incidence, Mortality, and Stage-Specific Survival of Cervical Cancer Patients in Hong Kong - 1997-2006
A Population-Based Analysis of Incidence, Mortality, and Stage-Specific Survival of Cervical Cancer Patients in Hong Kong - 1997-2006
Uploaded by
chenjiecdcCopyright:
Available Formats
You might also like
- Nurse Role in Intravenous TherapyDocument53 pagesNurse Role in Intravenous Therapyapi-300218860100% (2)
- A Systematic and Integrative Model For Mental Health Assessment and Treatment PlanningDocument35 pagesA Systematic and Integrative Model For Mental Health Assessment and Treatment PlanningCharleneKronstedt100% (2)
- Case Reflection FormatDocument9 pagesCase Reflection Formatanusarannya100% (5)
- Craniopharyngioma 2 PDFDocument9 pagesCraniopharyngioma 2 PDFBea NufuarNo ratings yet
- Original ArticleDocument7 pagesOriginal ArticleDain 2IronfootNo ratings yet
- Conditional Survival in Head and Neck Squamous Cell CarcinomaDocument13 pagesConditional Survival in Head and Neck Squamous Cell CarcinomaJoana KellenNo ratings yet
- J Amjoto 2019 102279Document5 pagesJ Amjoto 2019 102279Gisela LalitaNo ratings yet
- Incidence and Clinical Outcome of Primary Carcinomas of The Major Salivary Glands - 10-Year Data From A Population-Based State Cancer Registry in GermanyDocument11 pagesIncidence and Clinical Outcome of Primary Carcinomas of The Major Salivary Glands - 10-Year Data From A Population-Based State Cancer Registry in Germanymakif18651No ratings yet
- 394 FullDocument7 pages394 FullkemashabibiNo ratings yet
- Matsuo 2018Document14 pagesMatsuo 2018Mahmudur Rahman27No ratings yet
- Laryngoscope 2009 p1542Document8 pagesLaryngoscope 2009 p1542IRANo ratings yet
- Melanoma Incidence, Recurrence, and Mortality in An Integrated Healthcare System: A Retrospective Cohort StudyDocument9 pagesMelanoma Incidence, Recurrence, and Mortality in An Integrated Healthcare System: A Retrospective Cohort StudyPande Agung MahariskiNo ratings yet
- Survival Analysis of Nasopharyngeal Carcinoma in Hasan Sadikin HospitalDocument4 pagesSurvival Analysis of Nasopharyngeal Carcinoma in Hasan Sadikin HospitalRobert ChristevenNo ratings yet
- Prognostic JournalDocument6 pagesPrognostic JournalElpida WNo ratings yet
- Survival Analysis of Nasopharyngeal Carcinoma in Hasan Sadikin HospitalDocument4 pagesSurvival Analysis of Nasopharyngeal Carcinoma in Hasan Sadikin Hospitalairin shabrinaNo ratings yet
- Faecal Occult Blood Screening Reduced The Incidence of Colorectal CancerDocument1 pageFaecal Occult Blood Screening Reduced The Incidence of Colorectal CancerAgus PraktyasaNo ratings yet
- Bluethmann2016 PDFDocument9 pagesBluethmann2016 PDFramangNo ratings yet
- Trends in Incidence and Mortality of Esophageal Cancer in China 1990-2019 A Joinpoint and Age-Period-Cohort AnalysisDocument11 pagesTrends in Incidence and Mortality of Esophageal Cancer in China 1990-2019 A Joinpoint and Age-Period-Cohort Analysisstevenwang08No ratings yet
- Global Cancer Incidence and Mortality Rates and Trends - An UpdateDocument12 pagesGlobal Cancer Incidence and Mortality Rates and Trends - An UpdateVitória LeiteNo ratings yet
- Survival of Patients With Colorectal Cancer in A Cancer CenterDocument6 pagesSurvival of Patients With Colorectal Cancer in A Cancer CenterMuhammad bayu fernandaNo ratings yet
- Cancer Epidemiology-IARC. Original. HL Burden in CSA. ArgentinaDocument10 pagesCancer Epidemiology-IARC. Original. HL Burden in CSA. ArgentinaDiana Paola Valencia CamachoNo ratings yet
- Adolescents and Young Adult (AYA)Document13 pagesAdolescents and Young Adult (AYA)yunike M KesNo ratings yet
- Atm 07 05 100Document10 pagesAtm 07 05 100Farhan IrhamsyahNo ratings yet
- Nonsteroidal Anti-Inflammatory Drugs and Endometrial Carcinoma Mortality and RecurrenceDocument10 pagesNonsteroidal Anti-Inflammatory Drugs and Endometrial Carcinoma Mortality and RecurrencegraciaNo ratings yet
- Favorable Female NPCDocument6 pagesFavorable Female NPChi-lineNo ratings yet
- v07p0681 PDFDocument6 pagesv07p0681 PDFAzizaNo ratings yet
- 3454-Article Text-11501-1-10-20200318Document4 pages3454-Article Text-11501-1-10-20200318NuruljannahNo ratings yet
- Rakha Et Al. 2006 Prognostic Markers in Triple Negative Breast CancerDocument8 pagesRakha Et Al. 2006 Prognostic Markers in Triple Negative Breast CancerdanishNo ratings yet
- The Laryngoscope - 2018 - Farhood - Does Anatomic Subsite Influence Oral Cavity Cancer Mortality A SEER Database Analysis PDFDocument7 pagesThe Laryngoscope - 2018 - Farhood - Does Anatomic Subsite Influence Oral Cavity Cancer Mortality A SEER Database Analysis PDFJorge JaraNo ratings yet
- Nihms 281267Document27 pagesNihms 281267yohanasmjtNo ratings yet
- Sex Differences in Cancer Risk and Survival: A Swedish Cohort StudyDocument11 pagesSex Differences in Cancer Risk and Survival: A Swedish Cohort Studyfiora.ladesvitaNo ratings yet
- PIIS0959804918307081Document7 pagesPIIS0959804918307081nimaelhajjiNo ratings yet
- Xiaoli HuDocument12 pagesXiaoli HuYohanes AdhityaNo ratings yet
- Comparative Study of Fine Needle Aspiration Cytology and Histopathology in Grading Breast CarcinomaDocument5 pagesComparative Study of Fine Needle Aspiration Cytology and Histopathology in Grading Breast CarcinomaMafazi RifqiNo ratings yet
- Cancer GinjalDocument6 pagesCancer GinjalTutut setiowatiNo ratings yet
- Cancer Burden in China: A Bayesian Approach: Researcharticle Open AccessDocument10 pagesCancer Burden in China: A Bayesian Approach: Researcharticle Open AccessY YNo ratings yet
- Cancer-Specific Survival Outcome in Early-Stage Young Breast Cancer: Evidence From The SEER Database AnalysisDocument10 pagesCancer-Specific Survival Outcome in Early-Stage Young Breast Cancer: Evidence From The SEER Database Analysismahmud.meftahNo ratings yet
- Editorial: Lung Cancer: Prevalent Trends & Emerging ConceptsDocument3 pagesEditorial: Lung Cancer: Prevalent Trends & Emerging Conceptsjeevan georgeNo ratings yet
- 1 s2.0 S2405844020304485 MainDocument5 pages1 s2.0 S2405844020304485 MainSome LaNo ratings yet
- Santos2001 PDFDocument6 pagesSantos2001 PDFRoberto PazNo ratings yet
- Estimating The Net Survival of Patients With Gastric Cancer in Iran in A Relative Survival FrameworkDocument7 pagesEstimating The Net Survival of Patients With Gastric Cancer in Iran in A Relative Survival FrameworkRoja behnamiNo ratings yet
- Nihms 764091Document18 pagesNihms 764091Sheshang KamathNo ratings yet
- A Review of Lung Cancer Research in MalaysiaDocument9 pagesA Review of Lung Cancer Research in MalaysiaCahrun CarterNo ratings yet
- Tendências Na Incidência e Fatores de Risco Associados À Mortalidade Por Suicídio Entre Pacientes Com Câncer de MamaDocument7 pagesTendências Na Incidência e Fatores de Risco Associados À Mortalidade Por Suicídio Entre Pacientes Com Câncer de MamaLeonardo CarvalhoNo ratings yet
- Primary Tracheal Tumors: Review of 37 CasesDocument4 pagesPrimary Tracheal Tumors: Review of 37 CasesGordana PuzovicNo ratings yet
- Prognostic Biomarkers For Survival in Nasopharyngeal Carcinoma - A Systematic Review of The LiteratureDocument14 pagesPrognostic Biomarkers For Survival in Nasopharyngeal Carcinoma - A Systematic Review of The LiteratureWening Dewi HapsariNo ratings yet
- Gland CarcinomaDocument6 pagesGland CarcinomaVicko PratamaNo ratings yet
- Rosen 2011Document6 pagesRosen 2011Evelynππ θσυNo ratings yet
- Survival Outcomes For Different Subtypes of Epithelial Ovarian CancerDocument7 pagesSurvival Outcomes For Different Subtypes of Epithelial Ovarian CancerasclepiuspdfsNo ratings yet
- 6880-Article Text-54409-3-10-20231020Document12 pages6880-Article Text-54409-3-10-20231020Selma Mutiara HaniNo ratings yet
- Pretreatment Neutrophilto Lymphocyte Ratio Is Associatedwith Poor Survival in Patients With Stage I-III Non-Small Cell Lung CancerDocument16 pagesPretreatment Neutrophilto Lymphocyte Ratio Is Associatedwith Poor Survival in Patients With Stage I-III Non-Small Cell Lung CancerWilliamRayCassidyNo ratings yet
- Clinical Burden of Preoperative Albumin Globulin Rat - 2017 - The American JournDocument8 pagesClinical Burden of Preoperative Albumin Globulin Rat - 2017 - The American JournFlorin AchimNo ratings yet
- 20 ESMO E Learning Oesophageal CancerDocument55 pages20 ESMO E Learning Oesophageal CancerNatalindah Jokiem Woecandra T. D.No ratings yet
- 2016 Bradshaw Cardiovascular Disease Mortality Among BrCaDocument16 pages2016 Bradshaw Cardiovascular Disease Mortality Among BrCaAngélica Fernández PérezNo ratings yet
- Survival and Factors Affecting On Nasopharyngeal Carcinoma Patients in Hasan Sadikin General Hospital Bandung IndonesiaDocument1 pageSurvival and Factors Affecting On Nasopharyngeal Carcinoma Patients in Hasan Sadikin General Hospital Bandung IndonesiaDevi DaryaningsihNo ratings yet
- Metastatic Hepatocellular Carcinoma Diagnosed by Fine Needle Aspiration: A Clinical and Cytologic StudyDocument6 pagesMetastatic Hepatocellular Carcinoma Diagnosed by Fine Needle Aspiration: A Clinical and Cytologic StudyMara PitrezNo ratings yet
- Colorectal Cancer in The Young: Clinicopathologic Features and Prognostic Factors From A Cancer Institute in PeruDocument8 pagesColorectal Cancer in The Young: Clinicopathologic Features and Prognostic Factors From A Cancer Institute in PeruCristhian MejiaNo ratings yet
- Wessels 1996Document5 pagesWessels 1996Araceli Enríquez OvandoNo ratings yet
- Systemic Therapy For Advanced Appendiceal Adenocarcinoma: An Analysis From The NCCN Oncology Outcomes Database For Colorectal CancerDocument8 pagesSystemic Therapy For Advanced Appendiceal Adenocarcinoma: An Analysis From The NCCN Oncology Outcomes Database For Colorectal Canceralberto cabelloNo ratings yet
- Colon Cancer Clinical Macroscopic and MiDocument10 pagesColon Cancer Clinical Macroscopic and MiElena CaterevNo ratings yet
- Patterns in Lung Cancer Incidence Rates and Trends by Histologic Type in The United States, 2004-2009Document7 pagesPatterns in Lung Cancer Incidence Rates and Trends by Histologic Type in The United States, 2004-2009maleticjNo ratings yet
- 2018 - Article - 6627 SurvivalDocument10 pages2018 - Article - 6627 SurvivalMario OrtizNo ratings yet
- Lynch Syndrome: Molecular Mechanism and Current Clinical PracticeFrom EverandLynch Syndrome: Molecular Mechanism and Current Clinical PracticeNaohiro TomitaNo ratings yet
- Obstetric Ultrasound: What Is Obstetrical Ultrasound Imaging?Document6 pagesObstetric Ultrasound: What Is Obstetrical Ultrasound Imaging?Activity ManagerNo ratings yet
- CBC ReportDocument1 pageCBC ReportPranay BhosaleNo ratings yet
- KalaazarDocument44 pagesKalaazarJUNKY DOCTORNo ratings yet
- Confronting and Coping With Multidrug-Resistant TuDocument9 pagesConfronting and Coping With Multidrug-Resistant TuDWI HERU CAHYONONo ratings yet
- Surgical Treatment of Distal Femur Fracture Using Locking Reconstruction Plate in A DogDocument2 pagesSurgical Treatment of Distal Femur Fracture Using Locking Reconstruction Plate in A DogHari Krishna Nunna V VNo ratings yet
- Radiation Protection in Medical Radiography 8th Edition Sherer Test BankDocument6 pagesRadiation Protection in Medical Radiography 8th Edition Sherer Test Bankbeatrixkhuyen9rm100% (30)
- Effects of Physical Therapy On Mental Function in Patients With StrokeDocument6 pagesEffects of Physical Therapy On Mental Function in Patients With StrokeTeuku FadhliNo ratings yet
- Case Study (DM)Document28 pagesCase Study (DM)Jai - Ho100% (1)
- Special Chemistry: Test Name Current Result Previous Result Unit Normal RangeDocument1 pageSpecial Chemistry: Test Name Current Result Previous Result Unit Normal RangeSyed Muhammad Rafay AhmedNo ratings yet
- L&D PDFDocument2 pagesL&D PDFChandace JanineNo ratings yet
- LeukocytosisDocument2 pagesLeukocytosisNeoMedicaNo ratings yet
- Endoworld 19 Laparoscopy and Thoracoscopy in Small Animal PracticeDocument16 pagesEndoworld 19 Laparoscopy and Thoracoscopy in Small Animal PracticeCENEMEM ANDRADENo ratings yet
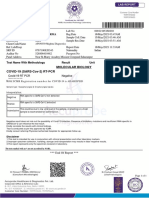
- Molecular Biology COVID-19 (SARS-Cov-2) RT-PCR: 80994699 Mr.I C SharmaDocument1 pageMolecular Biology COVID-19 (SARS-Cov-2) RT-PCR: 80994699 Mr.I C SharmaMohd YasarNo ratings yet
- Nithesh Pinto - Project-BioconDocument88 pagesNithesh Pinto - Project-BioconMohammed Thousif36No ratings yet
- Mucosta Drug Interactions - MIMS MalaysiaDocument4 pagesMucosta Drug Interactions - MIMS MalaysiaEsy LNo ratings yet
- Cervical CancerDocument52 pagesCervical CancerCiiezz BunciiezzNo ratings yet
- Aiapget 2018 QPDocument50 pagesAiapget 2018 QPGanesh RadhakrishnanNo ratings yet
- PIIS1201971220305294Document3 pagesPIIS1201971220305294kristina dewiNo ratings yet
- Pacientes OncológicosDocument12 pagesPacientes Oncológicosmelnutridiet8No ratings yet
- FOURTH YEAR BSC NURSING Course Plan - For MergeDocument33 pagesFOURTH YEAR BSC NURSING Course Plan - For MergeBHUKYA USHARANI50% (2)
- GeneticsDocument189 pagesGeneticstolgaonayNo ratings yet
- GMC Policy Benefits ChartDocument3 pagesGMC Policy Benefits ChartpankajgujjarNo ratings yet
- Global Health InitiativesDocument31 pagesGlobal Health InitiativesDaisy Joy SalanNo ratings yet
- Noy 192Document10 pagesNoy 192Cleysser Antonio Custodio PolarNo ratings yet
- Imbalanced NutritionDocument2 pagesImbalanced NutritionRizza 이 동해 Ocampo100% (1)
- DynaMed Plus - Premature Rupture of Membranes at Term (Term PROM)Document16 pagesDynaMed Plus - Premature Rupture of Membranes at Term (Term PROM)LudwinNo ratings yet
- Approach To Neonate With Low Birth WeightDocument40 pagesApproach To Neonate With Low Birth Weightnirajan khanalNo ratings yet
A Population-Based Analysis of Incidence, Mortality, and Stage-Specific Survival of Cervical Cancer Patients in Hong Kong - 1997-2006
A Population-Based Analysis of Incidence, Mortality, and Stage-Specific Survival of Cervical Cancer Patients in Hong Kong - 1997-2006
Uploaded by
chenjiecdcOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
A Population-Based Analysis of Incidence, Mortality, and Stage-Specific Survival of Cervical Cancer Patients in Hong Kong - 1997-2006
A Population-Based Analysis of Incidence, Mortality, and Stage-Specific Survival of Cervical Cancer Patients in Hong Kong - 1997-2006
Uploaded by
chenjiecdcCopyright:
Available Formats
A population-based analysis of incidence, mortality,
O R I G I N A L
A R T I C L E and stage-specific survival of cervical cancer patients
in Hong Kong: 1997-2006
CME
FY Cheung 張寬耀
Oscar WK Mang 孟偉剛
Objectives To determine the trends in incidence and mortality of cervical
Stephen CK Law 羅振基
cancer patients diagnosed during 1997 to 2006, and to describe
stage-specific survival using population-based cancer registry
data.
Design Retrospective, population-based study.
Setting Hong Kong.
Patients All patients diagnosed with cervical cancer between 1997 and
2006. Patients eligible for survival analysis were followed up till
31 December 2007.
Main outcome measures Age-standardised incidence and mortality rates and average
annual percent changes in these parameters were calculated
using the Poisson regression model. Survival was expressed as
relative survival rate using a period approach. Hazard ratios of
mortality including 95% confidence intervals for certain variables
were estimated using the Cox proportional hazards model.
Results During the 10-year period of the study, overall annual incidence
and mortality rates decreased by 4.2% and 6.0%, respectively.
Significant rates of reduction were observed in all age-groups
except those younger than 45 years. The reduction in incidence
of squamous cell carcinoma (3.6% annually) was less than that
of adenocarcinoma (5.2%) and other histological types (6.8%).
In all, 3807 (86.4%) of the patients were included in survival
analysis. The overall 5-year relative survival rate was 71.3% (95%
confidence interval, 69.5-73.1%), while the values for stages I,
II, III, and IV were 90.9%, 71.0%, 41.7%, and 7.8%, respectively.
Age, stage, and histology were independent prognostic factors.
Survival of stage IA patients was as good as that of the general
population.
Conclusions As in other industrialised countries, the incidence and mortality
rate of cervical cancer were decreasing. Stage-specific population-
based cancer survival was available for the first time, and was
useful as an indicator of cancer control. Collaboration between
public and private sectors to further improve the follow-up data
could provide more comprehensive surveillance information.
Key words
Epidemiologic studies; Incidence; Introduction
Prevalence; Survival analysis; Uterine
In 2007, cervical cancer was the third most common gynaecological cancer and the eighth
cervical neoplasms
most common women’s cancer in Hong Kong.1 The median age at diagnosis was 52 years.
Hong Kong Med J 2011;17:89-95 Squamous cell carcinoma (SCC) was the most common, followed by adenocarcinoma
(ADC) [including adenosquamous carcinoma], each accounting for 74.4% and 15.5% of all
Hong Kong Cancer Registry, R Block,
cases, respectively.
1/F, Queen Elizabeth Hospital, The Hong Kong Cancer Registry (HKCaR) is a population-based registry established
Kowloon, Hong Kong
FY Cheung, FRCRin 1963, and covered the entire population in the region. The collected data attained the
quality and completeness criteria for inclusion in the last six volumes of “Cancer Incidence
OWK Mang, MSc, C.Stat
SCK Law, FRCR in Five Continents” edited by the International Agency for Research on Cancer.2 Basic data
Correspondence to: Dr FY Cheung like demographics, the anatomical site, and the pathology of cancer were recorded. Cancer
Email: cheungfy@ha.org.hk death data were also included. Completeness of the coverage was demonstrated by the
Hong Kong Med J Vol 17 No 2 # April 2011 # www.hkmj.org 89
# Cheung et al #
to obtaining valid survival estimates on a population-
1997至2006年香港子宮頸癌患者的發病率、死 based level are that the follow-up data should be
complete and of high quality.4 The majority of such
亡率和癌症分期存活率:以人口為基礎的研究 information was available from either the electronic
目的 透過涵蓋全港人口為本的癌症登記資料庫數據,檢視 Patient Record system of the public health care
1997至2006年期間確診子宮頸癌患者的發病率和死 system (containing information on over 90% of
亡率的趨勢,並描述患者的分期存活率。 cancer patients in Hong Kong), or from routine record
設計 回顧性、以人口為基礎的研究。 linkage of data on all deceased persons provided by
the Government’s Births and Deaths General Register
安排 香港。 Office.
患者 1997至2006年期間所有確診子宮頸癌患者,並跟進
The purpose of the current study was to
合乎存活分析的患者至2007年12月31日。
estimate for the first time, the incidence and mortality
主要結果測量 年齡標準化發病率和死亡率,及利用卜瓦松(Pois- rates, as well as stage-specific population-based
son)迴歸模型計算年度平均百分比變化。患者存活 survival rates of patients with cervical cancer in Hong
率則按癌症分期的相對存活率顯示。部份變數的死亡 Kong. The study also examined survival patterns of
率風險比及其95%置信區間則以Cox比例風險模型估 different patient groups according to age, stage,
計。 and histology. These data could provide valuable
結果 在進行研究的10年期間,整體年度發病率和死亡率分 information for future planning and evaluation of
interventions against cervical cancer, such as those
別減低4.2%和6.0%。除45歲以下的年齡組別,其他
resulting from implementation of the mass Cervical
組別的上述比率均顯著減低。鱗狀細胞癌發病率減低
Screening Programme provided by the Department
的幅度(每年3.6%)不及腺癌(5.2%)和其他類型癌
of Health in 2004.
腫(6.8%)。研究共為3807名(86.4%)患者進行存
活分析。整體5年的相對存活率為71.3%(95%置信區
間:69.5-73.1%),而各階段的存活率如下:第I期 Methods
90.9%、第II期71.0%、第III期41.7%、第IV期7.8%。
This retrospective study was limited to individuals
年齡、癌症分期和癌腫類型是獨立預後因素。第IA期
newly diagnosed to have cervical cancer and
患者存活率理想,跟一般人口相若。
registered in the HKCaR from 1997 to 2006,
結論 香港子宮頸癌的發病率和死亡率正逐漸改善,情況跟 because this facilitated retrieval of relevant details;
其他工業化國家相若。這是首個以全港人口為基礎 information on death from causes other than cancer
及按癌症分期的存活率研究,並可視作癌症控制的指 was not available prior to that time. Apart from patient
標。公營和私營機構的合作可進一步強化隨訪期數 demographic characteristics, the following data were
據,提供更加全面的監測信息。 collected/verified: date of diagnosis (accurate to the
month), tumour site, histological type (according
to the International Classification of Diseases for
Oncology), and tumour staging as per the Federation
very low (<1%) rate of ‘death-certificate only’ cases
Internationale de Gynecologie et d’Obstetrique
in recent years. For some cancers including cervical
(FIGO), and the International Union Against Cancer
cancer, stage information was collected since 2001.
6th edition.5 For histological types, cases were divided
The aim of the Registry was to identify, as completely
into SCC (large-cell nonkeratinising type, large-cell
and accurately as possible, all newly diagnosed
keratinising type SCCs), ADC (adenocarcinoma and
cases of cancer in the territory. The Registry obtains
adenosquamous carcinoma) and others. Patients
information from: (1) reports on patients referred to were divided into the following age-groups for
oncology or radiotherapy centres in both public and analysis: younger than 45, 45-59, 60-74, and 75 years
private hospitals; (2) pathology reports from all public or older.
and most private hospitals; (3) electronic in-patient
and out-patient records from all public hospitals; (4) A total of 4407 patients with invasive cervical
death certificates kept by the Government; and (5) cancer were registered during the study period, of
whom 97.8% were verified microscopically; 2.1% were
voluntary notification from medical practitioners.
clinically diagnosed and less than 0.1% were based
A quarter-century collection of population-based
on death certification only. The annual incidence
cancer statistical information on incidence and
and mortality rates were standardised by the direct
mortality is readily accessible on the internet.
method using the world standard population.6 Trends
While the public hospital information was relatively
in incidence and mortality over 10-year periods were
comprehensive and easily accessible, private practice
analysed for the four age-groups and each histological
follow-up data were based on voluntary notification
type (if known). The annual percent change was
and subject to private practice agreement.
calculated using the Poisson regression model, by
Survival information has long been recognised fitting a regression line to the natural logarithm of
as an important indicator for monitoring the success the annual standardised rates, using calendar year as
of cancer-control activities.3 Important prerequisites a regressor variable (ie y = mx + b in which y = ln (rate)
90 Hong Kong Med J Vol 17 No 2 # April 2011 # www.hkmj.org
# Population-based analysis of cervical cancer #
and x = calendar year). The estimated annual percent using the Statistical Package for the Social Sciences
change (EAPC) was then equal to 100* (em–1). (Windows version 15.0; SPSS Inc, Chicago [IL], US).
All tests were two-sided and P values of less than 0.05
Of the 4407 incident cases, 600 (13.6%) were
were considered statistically significant.
excluded from the survival analysis for the following
reasons: other pre-existing or coexisting primary
malignancies; diagnosis based on death certificate Results
only; unknown age at diagnosis; aged ≥100 years;
Incidence and mortality
and loss to follow-up. Survival analyses were based
on the cohort of the remaining 3807 (86.4%) patients Between 1997 and 2006, there were on average 441
followed up until 31 December 2007. The end-point women diagnosed with cervical cancer each year
of each analysis was: (1) the date of death; (2) the (4.5% of all cancers in women). The crude rates of
censored date of last follow-up, or (3) termination of incidence and mortality were 12.8 and 3.8 per 100 000
the study. women, respectively. Stage distribution was: I, 42.0%;
II, 27.7%; III, 16.8%; IV, 4.7%; and unstaged, 8.8%.
In order to allow for deaths due to other Average annual rates by age-groups, histological
causes, survival was expressed as a relative survival types, and calendar year of diagnosis are shown in
rate, which is the ratio between observed survival Table 1. Overall, age-standardised incidence rates
and expected survival. Hence, the probability of decreased annually by 4.2% (P<0.001) and 6.0% in
surviving was compared with a group of the general mortality (P=0.001) during the period. There were
population with same age distribution and birth significant decreases in both incidence and mortality
cohort. Expected survival rates were estimated in almost all age-groups, except those diagnosed
according to the Hakulinen’s method,7 using Hong when younger than 45 years. There was a greater
Kong population life tables.8 The calculations were decrease in mortality than incidence in almost all
carried out using the SURV3 analysis programme.9 age-groups, except in those diagnosed aged 75 years
The Multivariate Cox proportional hazards model10 or older. The greatest drop in incidence rates was in
was then used to assess the impact of covariates patients 75 years or older, while it was static in the
on survival and estimate adjusted relative risks and youngest age-group. Figure 1 shows the change in
95% confidence intervals (CIs), after adjusting for age-specific incidence rates over the three periods.
other covariates. These calculations were performed For the most recent period, the age-specific incidence
TABLE 1. Cervical cancer incidence and mortality per 100 000 women in Hong Kong, 1997-2006
Categories No. of new cases 1997-1999 2000-2002 2003-2006 EAPC (%)* P value
Mean annual incidence
Age-group (years)
<45 1273 5.7 5.6 5.5 -0.6 0.353
45-59 1320 24.7 22.4 18.4 -4.4 0.004
60-74 1157 40.3 31.6 29.6 -4.3 0.005
≥75 653 47.1 38.9 27.6 -7.4 0.001
All ages †
4407 ‡
10.9 9.2 8.1 -4.2 <0.001
Histology§
SCC 3277 7.9 6.9 6.1 -3.6 0.008
ADC 683 1.7 1.5 1.2 -5.2 <0.001
Others 447 1.2 0.8 0.8 -6.8 0.006
No. of deaths Mean annual mortality
Age-group (years)
<45 182 0.9 0.8 0.7 -2.0 0.170
45-59 328 7.3 4.7 4.5 -5.8 0.039
60-74 399 15.2 10.7 9.4 -6.5 0.005
≥75 409 26.4 23.3 19.6 -4.2 0.005
All ages† 1318 3.4 2.4 2.1 -6.0 0.001
* EAPC denotes estimated annual percent change over the 10-year period
†
Rates were age-adjusted to the world standard population
‡
Includes four cases with unknown age
§
SCC denotes squamous cell carcinoma, and ADC adenocarcinoma
Hong Kong Med J Vol 17 No 2 # April 2011 # www.hkmj.org 91
# Cheung et al #
curve shows a peak at 65-69 years, which was 10 years of cervical cancer patients according to stage and
earlier than in previous periods. There were also histology. The overall 5-year relative survival rate of
changes in the proportion of these various cervical all patients was 71.3% (95% CI, 69.5-73.1%). Relative
cancers with respect to the histological diagnosis; survival rates at 5 years according to FIGO staging
the incidence being significantly decreased for SCC were: 90.9%, 71.0%, 41.7%, and 7.8% for stages I, II,
(EAPC, -3.6%; P=0.008), ADC (EAPC, -5.2%; P<0.001) III, and IV, respectively. There were considerable
and other rare tumours (EAPC, -6.8%; P=0.006). differences in survival rates among different
substages (Fig 2). The prognosis of patients with
stage IA was nearly the same as that of the general
Survival population and the survival of those with stage IIA
Among the 3807 incident cases of cervical cancer and IIB cancers were similar. The multivariate Cox
patients selected for the survival analysis, 28.6% were proportional hazards model also confirmed that age-
aged below 45 years and 14.3% were aged 75 years or group, stage, and histology had a significant impact
above. There was no significant difference in stage on survival (Table 3).
distribution between those in the survival analysis
group and those who were excluded. The mean
follow-up time was 51 months (range, 1-132 months). Discussion
Table 2 summarises the 5-year relative survival rates This study was the first report based on the HKCaR
60 1997-1999
2000-2002
50 2003-2006
Rates per 100 000 women
40
30
20
10
0
0- 10- 20- 30- 40- 50- 60- 70- 80-
Age-group (years)
FIG 1. Age-specific incidence rates for cervical cancer in Hong Kong
TABLE 2. Survival of patients with cervical cancer according to stage and histology
Categories No. Survival rate (%) 95% Confidence interval
for 5-year survival
1 Year 2 Years 3 Years 4 Years 5 Years
All 3807 90.6 81.0 76.6 73.2 71.3 69.5-73.1
Stage
I 1598 98.3 95.1 93.4 91.7 90.9 89.0-92.7
II 1062 95.1 83.7 78.3 74.5 71.0 67.5-74.5
III 643 81.6 63.1 52.7 44.4 41.7 36.9-46.4
IV 179 39.9 18.9 14.5 9.8 7.8 2.8-12.9
Unstaged 325 83.8 72.0 67.5 65.6 63.6 56.2-69.1
Histology*
SCC 2978 91.8 82.6 78.0 74.6 72.6 70.6-74.6
ADC 533 90.3 80.0 75.9 72.7 70.5 66.0-75.1
Others 296 79.8 67.7 63.7 60.4 60.0 53.4-66.5
* SCC denotes squamous cell carcinoma, and ADC adenocarcinoma
92 Hong Kong Med J Vol 17 No 2 # April 2011 # www.hkmj.org
# Population-based analysis of cervical cancer #
rates in other developed countries (Table 411-16). The
on incidence, mortality, and stage-specific survival
rates for cervical cancer. The strength of this study
5-year survival rate for Hong Kong patients (71.3%)
is that it is population-based, comprising virtually all
was higher than that of Singapore (64.7%), United
cases in Hong Kong and covering different hospitals,
Kingdom (65.2%), and Sweden (71.0%), but slightly
districts, and social classes. lower than that of Japan (71.5%), the US (73.3%), and
The 5-year relative survival rate of cervical Australia (73.6%). These results, however, should be
cancer in Hong Kong appears comparable to reported interpreted with caution due to differences in the
100%
90%
80%
70% Ia
Ib
60%
IIa
Survival
50% IIb
IIIa
40%
IIIb
30% IVa
IVb
20%
10%
0%
0 1 2 3 4 5
Years after diagnosis
FIG 2. Survival of patients with cervical cancer in Hong Kong according to their FIGO substage
FIGO denotes Federation Internationale de Gynecologie et d’Obstetrique
TABLE 3. Univariate and multivariate analyses of overall survival for cervical cancer patients
Categories No. of cases Univariate* Multivariate†
Hazard ratio 95% Confidence Hazard ratio 95% Confidence
interval interval
Age-group (years)
<45 1089 1 Reference 1 Reference
45-59 1163 1.60 1.33-1.93 1.21 1.01-1.47
60-74 1008 2.37 1.98-2.83 1.61 1.34-1.94
≥75 547 5.42 4.52-6.49 3.06 2.52-3.71
Stage
I 1598 1 Reference 1 Reference
II 1062 3.35 2.80-4.01 2.87 2.39-3.46
III 643 7.58 6.34-9.06 6.24 5.17-7.53
IV 179 26.47 21.29-32.92 21.14 16.90-26.45
Unstaged 325 4.32 3.46-5.40 3.72 2.97-4.65
Histology ‡
SCC 2978 1 Reference 1 Reference
ADC 533 0.99 0.84-1.17 1.72 1.41-2.10
Others 296 1.59 1.31-1.92 2.64 2.14-3.25
* Use of Cox regression on single covariate
†
Use of Cox proportional hazards model adjusted for all other factors in the table
‡
SCC denotes squamous cell carcinoma, and ADC adenocarcinoma
Hong Kong Med J Vol 17 No 2 # April 2011 # www.hkmj.org 93
# Cheung et al #
TABLE 4. Comparisons with international reports of 5-year survival from cervical the other hand, the observed drop in incidence
cancer could also have been related to an increase in
Country or population Year of diagnosis 5-Year relative survival opportunistic screening that mainly identified pre-
rate (%) cancerous lesions. Subsequent organised screening,
Hong Kong 1997-2006 71.3 if successful, could lead to a steeper fall in incidence
Korea11 1998-2002 80.4 rates in the ensuing years. Thus, the present incidence
Japan12 1997-1999 71.5 data could serve as a baseline for future comparison.
Singapore 13
1998-2002 64.7 The steadily decreasing incidence and mortality
Australia, NSW14 1999-2003 73.6
of cervical cancer in Hong Kong was consistent with
trends in other industrialised countries.18 Various
UK, England 15
1995-1999 65.2
studies revealed that widespread use of cervical
Sweden15 1995-1999 71.0 screening has been associated with the substantial
US 16
1995-2001 73.3 reduction in incidence and mortality rates of cervical
cancer.19-24 Iceland, Finland, Sweden, and parts of
Denmark25,26 achieved almost complete coverage
of the target populations, resulting in sharp falls
periods studied and standardisation methods.
in incidence and mortality. The increasing survival
Extent of disease at diagnosis is the most from cervical cancer was at least partly due to the
important determinant of survival, implying that nationwide programme.27 However, as cervical cancer
early detection is a more important outcome than incidence in Hong Kong has already dropped to a
improvement in the treatment modality. The very very low level compared to other western developed
high survival in early-stage disease suggests that countries even before the implementation of
early presentation and rapid referral are essential. organised mass screening, the merit of any mass
Survival of cervical cancer patients varies with age. screening programme towards further decrease of
After multivariate adjustment, patients with ADC cervical cancer incidence is indeed questionable.
had a worse prognosis than those with SCC. This
This study provides the first population-
may indicate that women with cervical ADC have an
based investigation of stage-specific survival of a
inherently worse prognosis than women with SCC.
major cancer—cervical cancer—in the territory. As a
There was continuous significant reduction in baseline, it would provide an effective and econom-
the incidence and mortality of patients with cervical ical method of evaluating the impact of the organised
cancer over the study period, with unadjusted 5-year screening programme through observation of the
relative rate improved from 69.6% in 1997-1999 to future changes in cervical cancer incidence, mortality
73.2% in 2000-2002 before the implementation of an and survival at community level. Further analyses
organised screening programme by the Department with longer follow-up periods will also enrich the
of Health in 2004. The overall reduction in incidence information for planning or evaluation of actions
in these earlier years might be attributed to period against this disease. Closer collaboration with private
and cohort effects17 and lower incidences might practice on follow-up data would certainly perfect
eventually be translated into reduced mortality. On the staging and surveillance data.
References
1. Hong Kong cancer stat 2007. Hong Kong Cancer Registry, (1950-1957). Sendai, Japan: Tohuku University of Medicine;
Hospital Authority website: http://www.ha.org.hk/cancereg. 1960.
Accessed 17 May 2010. 7. Brenner H, Hakulinen T. Up-to-date long-term survival
2. Curado MP, Edwards B, Shin HR, editors. Cancer incidence curves of patients with cancer by period analysis. J Clin
in five Continents. Vol. IX. IARC scientific publications no. Oncol 2002;20:826-32.
160. Lyon: IARC; 2007. 8. Hong Kong life tables. Hong Kong: Demographic Statistics
3. World Health Organization. National cancer control Section, Census and Statistics Department; 2004.
programmes: policies and managerial guidelines. 2nd ed. 9. Dickman P, Hakulinen T, Voutilainen E. Surv3 relative
Geneva: WHO; 2002. survival analysis program version 3.00b2. Helsinki, Finland:
4. Capocaccia R, Gatta G, Roazzi P, et al. The EUROCARE-3 Finnish Cancer Registry; 2002.
database: methodology of data collection, standardisation, 10. Cox DR. Regression models and life tables. J Royal Stat Soc
quality control and statistical analysis. Ann Oncol 2003;14 B 1972;34:187-200.
Suppl 5:v14-27. 11. Jung KW, Yim SH, Kong HJ, et al. Cancer survival in Korea
5. Sobin LH, Wittekind C. TNM classification of malignant 1993-2002: a population-based study. J Korean Med Sci
tumors. 6th ed. Geneva, Switzerland: UICC International 2007;22 Suppl: S5-S10.
Union Against Cancer; 2002. 12. Cancer statistics in Japan 2008. National Cancer Center website:
6. Segi M. Cancer mortality for selected sites in 24 countries http://ganjoho.ncc.go.jp/public/statistics/backnumber/
94 Hong Kong Med J Vol 17 No 2 # April 2011 # www.hkmj.org
# Population-based analysis of cervical cancer #
2008_en.html. Accessed 10 May 2010. Evaluation of the effectiveness of cervical cancer screening:
13. Wong CS, Chow KY, Lim GH, Bhalla V, Lee HP, Chia KS. a case-control study in Miyagi, Japan. Tohoku J Exp Med
Cancer survival in Singapore 1968-2002. Singapore: 1995;175:171-8.
Singapore Cancer Registry, National Registry of Diseases 21. Quinn M, Babb P, Jones J, Allen J. Effect of screening on
Office; 2010. incidence of and mortality from cancer of cervix in England:
14. Tracey E, Barraclough H, Chen W, editors. Survival from evaluation based on routinely collected statistics. BMJ
cancer in NSW: 1980 to 2003. Sydney: Cancer Institute 1999;318:904-8.
NSW; 2007. 22. Ronco G, Pilutti S, Patriarca S, et al. Impact of the
15. Capocaccia R, Gavin A, Hakulinen T, Lutz JM, Sant M. introduction of organised screening for cervical cancer in
Survival of cancer patients in Europe, 1995-2002: The Turin, Italy: cancer incidence by screening history 1992-98.
EUROCARE-4 study. Eur J Cancer 2009;45:901-1094. Br J Cancer 2005;93:376-8.
16. Jemal A, Seigel R, Ward E, et al. Cancer statistics, 2006. CA 23. Lynge E, Madsen M, Engholm G. Effect of organized
Cancer J Clin 2006;56:106-30. screening on incidence and mortality of cervical cancer in
17. Leung GM, Woo PP, McGhee SM, et al. Age-period-cohort Denmark. Cancer Res 1989;49:2157-60.
analysis of cervical cancer incidence in Hong Kong from 24. Laara E, Day NE, Hakama M. Trends in mortality from
1972 to 2001 using maximum likelihood and Bayesian cervical cancer in the Nordic countries: association with
methods. J Epidemiol Community Health 2006;60:712- organised screening programmes. Lancet 1987;1:1247-9.
20. 25. Hakama M, Louhivuori K. A screening programme for
18. Bray F, Loos AH, McCarron P, et al. Trends in cervical cervical cancer that worked. Cancer Surv 1988;7:403-16.
squamous cell carcinoma incidence in 13 European 26. Sigurdsson K. Effect of organized screening on the risk of
countries: changing risk and the effects of screening. Cancer cervical cancer. Evaluation of screening activity in Iceland,
Epidemiol Biomarkers Prev 2005;14:677-86. 1964-1991. Int J Cancer 1993;54:563-70.
19. Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 27. Ioka A, Tsukuma H, Ajiki W, Oshima A. Influence of age
2002. CA Cancer J Clin 2005;55:74-108. on cervical cancer survival in Japan. Jpn J Clin Oncol
20. Makino H, Sato S, Yajima A, Komatsu S, Fukao A. 2005;35:464-9.
Hong Kong Med J Vol 17 No 2 # April 2011 # www.hkmj.org 95
You might also like
- Nurse Role in Intravenous TherapyDocument53 pagesNurse Role in Intravenous Therapyapi-300218860100% (2)
- A Systematic and Integrative Model For Mental Health Assessment and Treatment PlanningDocument35 pagesA Systematic and Integrative Model For Mental Health Assessment and Treatment PlanningCharleneKronstedt100% (2)
- Case Reflection FormatDocument9 pagesCase Reflection Formatanusarannya100% (5)
- Craniopharyngioma 2 PDFDocument9 pagesCraniopharyngioma 2 PDFBea NufuarNo ratings yet
- Original ArticleDocument7 pagesOriginal ArticleDain 2IronfootNo ratings yet
- Conditional Survival in Head and Neck Squamous Cell CarcinomaDocument13 pagesConditional Survival in Head and Neck Squamous Cell CarcinomaJoana KellenNo ratings yet
- J Amjoto 2019 102279Document5 pagesJ Amjoto 2019 102279Gisela LalitaNo ratings yet
- Incidence and Clinical Outcome of Primary Carcinomas of The Major Salivary Glands - 10-Year Data From A Population-Based State Cancer Registry in GermanyDocument11 pagesIncidence and Clinical Outcome of Primary Carcinomas of The Major Salivary Glands - 10-Year Data From A Population-Based State Cancer Registry in Germanymakif18651No ratings yet
- 394 FullDocument7 pages394 FullkemashabibiNo ratings yet
- Matsuo 2018Document14 pagesMatsuo 2018Mahmudur Rahman27No ratings yet
- Laryngoscope 2009 p1542Document8 pagesLaryngoscope 2009 p1542IRANo ratings yet
- Melanoma Incidence, Recurrence, and Mortality in An Integrated Healthcare System: A Retrospective Cohort StudyDocument9 pagesMelanoma Incidence, Recurrence, and Mortality in An Integrated Healthcare System: A Retrospective Cohort StudyPande Agung MahariskiNo ratings yet
- Survival Analysis of Nasopharyngeal Carcinoma in Hasan Sadikin HospitalDocument4 pagesSurvival Analysis of Nasopharyngeal Carcinoma in Hasan Sadikin HospitalRobert ChristevenNo ratings yet
- Prognostic JournalDocument6 pagesPrognostic JournalElpida WNo ratings yet
- Survival Analysis of Nasopharyngeal Carcinoma in Hasan Sadikin HospitalDocument4 pagesSurvival Analysis of Nasopharyngeal Carcinoma in Hasan Sadikin Hospitalairin shabrinaNo ratings yet
- Faecal Occult Blood Screening Reduced The Incidence of Colorectal CancerDocument1 pageFaecal Occult Blood Screening Reduced The Incidence of Colorectal CancerAgus PraktyasaNo ratings yet
- Bluethmann2016 PDFDocument9 pagesBluethmann2016 PDFramangNo ratings yet
- Trends in Incidence and Mortality of Esophageal Cancer in China 1990-2019 A Joinpoint and Age-Period-Cohort AnalysisDocument11 pagesTrends in Incidence and Mortality of Esophageal Cancer in China 1990-2019 A Joinpoint and Age-Period-Cohort Analysisstevenwang08No ratings yet
- Global Cancer Incidence and Mortality Rates and Trends - An UpdateDocument12 pagesGlobal Cancer Incidence and Mortality Rates and Trends - An UpdateVitória LeiteNo ratings yet
- Survival of Patients With Colorectal Cancer in A Cancer CenterDocument6 pagesSurvival of Patients With Colorectal Cancer in A Cancer CenterMuhammad bayu fernandaNo ratings yet
- Cancer Epidemiology-IARC. Original. HL Burden in CSA. ArgentinaDocument10 pagesCancer Epidemiology-IARC. Original. HL Burden in CSA. ArgentinaDiana Paola Valencia CamachoNo ratings yet
- Adolescents and Young Adult (AYA)Document13 pagesAdolescents and Young Adult (AYA)yunike M KesNo ratings yet
- Atm 07 05 100Document10 pagesAtm 07 05 100Farhan IrhamsyahNo ratings yet
- Nonsteroidal Anti-Inflammatory Drugs and Endometrial Carcinoma Mortality and RecurrenceDocument10 pagesNonsteroidal Anti-Inflammatory Drugs and Endometrial Carcinoma Mortality and RecurrencegraciaNo ratings yet
- Favorable Female NPCDocument6 pagesFavorable Female NPChi-lineNo ratings yet
- v07p0681 PDFDocument6 pagesv07p0681 PDFAzizaNo ratings yet
- 3454-Article Text-11501-1-10-20200318Document4 pages3454-Article Text-11501-1-10-20200318NuruljannahNo ratings yet
- Rakha Et Al. 2006 Prognostic Markers in Triple Negative Breast CancerDocument8 pagesRakha Et Al. 2006 Prognostic Markers in Triple Negative Breast CancerdanishNo ratings yet
- The Laryngoscope - 2018 - Farhood - Does Anatomic Subsite Influence Oral Cavity Cancer Mortality A SEER Database Analysis PDFDocument7 pagesThe Laryngoscope - 2018 - Farhood - Does Anatomic Subsite Influence Oral Cavity Cancer Mortality A SEER Database Analysis PDFJorge JaraNo ratings yet
- Nihms 281267Document27 pagesNihms 281267yohanasmjtNo ratings yet
- Sex Differences in Cancer Risk and Survival: A Swedish Cohort StudyDocument11 pagesSex Differences in Cancer Risk and Survival: A Swedish Cohort Studyfiora.ladesvitaNo ratings yet
- PIIS0959804918307081Document7 pagesPIIS0959804918307081nimaelhajjiNo ratings yet
- Xiaoli HuDocument12 pagesXiaoli HuYohanes AdhityaNo ratings yet
- Comparative Study of Fine Needle Aspiration Cytology and Histopathology in Grading Breast CarcinomaDocument5 pagesComparative Study of Fine Needle Aspiration Cytology and Histopathology in Grading Breast CarcinomaMafazi RifqiNo ratings yet
- Cancer GinjalDocument6 pagesCancer GinjalTutut setiowatiNo ratings yet
- Cancer Burden in China: A Bayesian Approach: Researcharticle Open AccessDocument10 pagesCancer Burden in China: A Bayesian Approach: Researcharticle Open AccessY YNo ratings yet
- Cancer-Specific Survival Outcome in Early-Stage Young Breast Cancer: Evidence From The SEER Database AnalysisDocument10 pagesCancer-Specific Survival Outcome in Early-Stage Young Breast Cancer: Evidence From The SEER Database Analysismahmud.meftahNo ratings yet
- Editorial: Lung Cancer: Prevalent Trends & Emerging ConceptsDocument3 pagesEditorial: Lung Cancer: Prevalent Trends & Emerging Conceptsjeevan georgeNo ratings yet
- 1 s2.0 S2405844020304485 MainDocument5 pages1 s2.0 S2405844020304485 MainSome LaNo ratings yet
- Santos2001 PDFDocument6 pagesSantos2001 PDFRoberto PazNo ratings yet
- Estimating The Net Survival of Patients With Gastric Cancer in Iran in A Relative Survival FrameworkDocument7 pagesEstimating The Net Survival of Patients With Gastric Cancer in Iran in A Relative Survival FrameworkRoja behnamiNo ratings yet
- Nihms 764091Document18 pagesNihms 764091Sheshang KamathNo ratings yet
- A Review of Lung Cancer Research in MalaysiaDocument9 pagesA Review of Lung Cancer Research in MalaysiaCahrun CarterNo ratings yet
- Tendências Na Incidência e Fatores de Risco Associados À Mortalidade Por Suicídio Entre Pacientes Com Câncer de MamaDocument7 pagesTendências Na Incidência e Fatores de Risco Associados À Mortalidade Por Suicídio Entre Pacientes Com Câncer de MamaLeonardo CarvalhoNo ratings yet
- Primary Tracheal Tumors: Review of 37 CasesDocument4 pagesPrimary Tracheal Tumors: Review of 37 CasesGordana PuzovicNo ratings yet
- Prognostic Biomarkers For Survival in Nasopharyngeal Carcinoma - A Systematic Review of The LiteratureDocument14 pagesPrognostic Biomarkers For Survival in Nasopharyngeal Carcinoma - A Systematic Review of The LiteratureWening Dewi HapsariNo ratings yet
- Gland CarcinomaDocument6 pagesGland CarcinomaVicko PratamaNo ratings yet
- Rosen 2011Document6 pagesRosen 2011Evelynππ θσυNo ratings yet
- Survival Outcomes For Different Subtypes of Epithelial Ovarian CancerDocument7 pagesSurvival Outcomes For Different Subtypes of Epithelial Ovarian CancerasclepiuspdfsNo ratings yet
- 6880-Article Text-54409-3-10-20231020Document12 pages6880-Article Text-54409-3-10-20231020Selma Mutiara HaniNo ratings yet
- Pretreatment Neutrophilto Lymphocyte Ratio Is Associatedwith Poor Survival in Patients With Stage I-III Non-Small Cell Lung CancerDocument16 pagesPretreatment Neutrophilto Lymphocyte Ratio Is Associatedwith Poor Survival in Patients With Stage I-III Non-Small Cell Lung CancerWilliamRayCassidyNo ratings yet
- Clinical Burden of Preoperative Albumin Globulin Rat - 2017 - The American JournDocument8 pagesClinical Burden of Preoperative Albumin Globulin Rat - 2017 - The American JournFlorin AchimNo ratings yet
- 20 ESMO E Learning Oesophageal CancerDocument55 pages20 ESMO E Learning Oesophageal CancerNatalindah Jokiem Woecandra T. D.No ratings yet
- 2016 Bradshaw Cardiovascular Disease Mortality Among BrCaDocument16 pages2016 Bradshaw Cardiovascular Disease Mortality Among BrCaAngélica Fernández PérezNo ratings yet
- Survival and Factors Affecting On Nasopharyngeal Carcinoma Patients in Hasan Sadikin General Hospital Bandung IndonesiaDocument1 pageSurvival and Factors Affecting On Nasopharyngeal Carcinoma Patients in Hasan Sadikin General Hospital Bandung IndonesiaDevi DaryaningsihNo ratings yet
- Metastatic Hepatocellular Carcinoma Diagnosed by Fine Needle Aspiration: A Clinical and Cytologic StudyDocument6 pagesMetastatic Hepatocellular Carcinoma Diagnosed by Fine Needle Aspiration: A Clinical and Cytologic StudyMara PitrezNo ratings yet
- Colorectal Cancer in The Young: Clinicopathologic Features and Prognostic Factors From A Cancer Institute in PeruDocument8 pagesColorectal Cancer in The Young: Clinicopathologic Features and Prognostic Factors From A Cancer Institute in PeruCristhian MejiaNo ratings yet
- Wessels 1996Document5 pagesWessels 1996Araceli Enríquez OvandoNo ratings yet
- Systemic Therapy For Advanced Appendiceal Adenocarcinoma: An Analysis From The NCCN Oncology Outcomes Database For Colorectal CancerDocument8 pagesSystemic Therapy For Advanced Appendiceal Adenocarcinoma: An Analysis From The NCCN Oncology Outcomes Database For Colorectal Canceralberto cabelloNo ratings yet
- Colon Cancer Clinical Macroscopic and MiDocument10 pagesColon Cancer Clinical Macroscopic and MiElena CaterevNo ratings yet
- Patterns in Lung Cancer Incidence Rates and Trends by Histologic Type in The United States, 2004-2009Document7 pagesPatterns in Lung Cancer Incidence Rates and Trends by Histologic Type in The United States, 2004-2009maleticjNo ratings yet
- 2018 - Article - 6627 SurvivalDocument10 pages2018 - Article - 6627 SurvivalMario OrtizNo ratings yet
- Lynch Syndrome: Molecular Mechanism and Current Clinical PracticeFrom EverandLynch Syndrome: Molecular Mechanism and Current Clinical PracticeNaohiro TomitaNo ratings yet
- Obstetric Ultrasound: What Is Obstetrical Ultrasound Imaging?Document6 pagesObstetric Ultrasound: What Is Obstetrical Ultrasound Imaging?Activity ManagerNo ratings yet
- CBC ReportDocument1 pageCBC ReportPranay BhosaleNo ratings yet
- KalaazarDocument44 pagesKalaazarJUNKY DOCTORNo ratings yet
- Confronting and Coping With Multidrug-Resistant TuDocument9 pagesConfronting and Coping With Multidrug-Resistant TuDWI HERU CAHYONONo ratings yet
- Surgical Treatment of Distal Femur Fracture Using Locking Reconstruction Plate in A DogDocument2 pagesSurgical Treatment of Distal Femur Fracture Using Locking Reconstruction Plate in A DogHari Krishna Nunna V VNo ratings yet
- Radiation Protection in Medical Radiography 8th Edition Sherer Test BankDocument6 pagesRadiation Protection in Medical Radiography 8th Edition Sherer Test Bankbeatrixkhuyen9rm100% (30)
- Effects of Physical Therapy On Mental Function in Patients With StrokeDocument6 pagesEffects of Physical Therapy On Mental Function in Patients With StrokeTeuku FadhliNo ratings yet
- Case Study (DM)Document28 pagesCase Study (DM)Jai - Ho100% (1)
- Special Chemistry: Test Name Current Result Previous Result Unit Normal RangeDocument1 pageSpecial Chemistry: Test Name Current Result Previous Result Unit Normal RangeSyed Muhammad Rafay AhmedNo ratings yet
- L&D PDFDocument2 pagesL&D PDFChandace JanineNo ratings yet
- LeukocytosisDocument2 pagesLeukocytosisNeoMedicaNo ratings yet
- Endoworld 19 Laparoscopy and Thoracoscopy in Small Animal PracticeDocument16 pagesEndoworld 19 Laparoscopy and Thoracoscopy in Small Animal PracticeCENEMEM ANDRADENo ratings yet
- Molecular Biology COVID-19 (SARS-Cov-2) RT-PCR: 80994699 Mr.I C SharmaDocument1 pageMolecular Biology COVID-19 (SARS-Cov-2) RT-PCR: 80994699 Mr.I C SharmaMohd YasarNo ratings yet
- Nithesh Pinto - Project-BioconDocument88 pagesNithesh Pinto - Project-BioconMohammed Thousif36No ratings yet
- Mucosta Drug Interactions - MIMS MalaysiaDocument4 pagesMucosta Drug Interactions - MIMS MalaysiaEsy LNo ratings yet
- Cervical CancerDocument52 pagesCervical CancerCiiezz BunciiezzNo ratings yet
- Aiapget 2018 QPDocument50 pagesAiapget 2018 QPGanesh RadhakrishnanNo ratings yet
- PIIS1201971220305294Document3 pagesPIIS1201971220305294kristina dewiNo ratings yet
- Pacientes OncológicosDocument12 pagesPacientes Oncológicosmelnutridiet8No ratings yet
- FOURTH YEAR BSC NURSING Course Plan - For MergeDocument33 pagesFOURTH YEAR BSC NURSING Course Plan - For MergeBHUKYA USHARANI50% (2)
- GeneticsDocument189 pagesGeneticstolgaonayNo ratings yet
- GMC Policy Benefits ChartDocument3 pagesGMC Policy Benefits ChartpankajgujjarNo ratings yet
- Global Health InitiativesDocument31 pagesGlobal Health InitiativesDaisy Joy SalanNo ratings yet
- Noy 192Document10 pagesNoy 192Cleysser Antonio Custodio PolarNo ratings yet
- Imbalanced NutritionDocument2 pagesImbalanced NutritionRizza 이 동해 Ocampo100% (1)
- DynaMed Plus - Premature Rupture of Membranes at Term (Term PROM)Document16 pagesDynaMed Plus - Premature Rupture of Membranes at Term (Term PROM)LudwinNo ratings yet
- Approach To Neonate With Low Birth WeightDocument40 pagesApproach To Neonate With Low Birth Weightnirajan khanalNo ratings yet