Professional Documents
Culture Documents
Feb 24 2024 Gastrointestinal System Review
Feb 24 2024 Gastrointestinal System Review
Uploaded by
Jezzabel Kyra BadayosOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Feb 24 2024 Gastrointestinal System Review
Feb 24 2024 Gastrointestinal System Review
Uploaded by
Jezzabel Kyra BadayosCopyright:
Available Formats
GASTROINTESTINAL SYSTEM ○ Heartburn “pyrosis” - relieved by medicine; aggravated by
acidic food
Hiatal hernia “Diaphragmatic Hernia” ○ Regurgitation
● Protrusion of the stomach through the esophageal hiatus of the ○ Chest pain (without heaviness) , Dysphagia, Dyspnea, N&V
diaphragm into the thorax ○ Clients may be asymptomatic
● Two types: Sliding and rolling hernias
○ Sliding hernias:
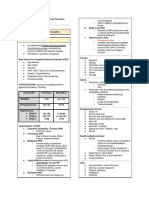
SLIDING ROLLING
■ Most common type (90%)
■ Hernia moves freely and slides into and out of the ● Heartburn ● Feeling of fullness after
thorax during changes in position or changes ● Regurgitation eating
intraabdominal pressure ● Chest pain ● Breathlessness after
■ Due to muscle weakening in the esophageal hiatus, ● Dysphagia eating
which loosens the esophageal supports and permits ● Belching ● Feeling of suffocation
the lower portion of the esophagus to rise in the thorax ● Chest Pain that mimics
angina
■ Other causes:
● Worsening
● Aging process manifestations in
● Congenital weakness recumbent position
● Trauma
● Obesity
● Incidence: affects more in women than men
● Surgery
● GERD, PEPTIC ULCER, HIATAL HERNIA - possible condition related
● Prolonged increase in abdominal pressure
to the symptoms mentioned above
■ Major concern: Esophageal Reflux
● Dx tests:
○ Paraesophageal “Rolling” hernias:
○ Barium swallow & fluoroscopy - most specific diagnostic test
■ The fundus roll through the esophageal hiatus and into
■ After procedure: Increase oral fluid intake/ give
the thorax beside the esophagus
laxatives
■ Causes: anatomic defect; previous esophageal
○ Esophagogastroduodenoscopy
surgeries
■ Prep: NPO for 8 hours; sedation
■ Reflux: not a major concern
● Management:
■ IDA is common
○ Meds: PPI, CaCO3, KremilS (antacids)
● Manifestation:
■ Note: Antacid should be given 30-45 mins after meal
○ Primary symptoms: associated with reflux
○ Diet therapy:
Transcribed by: Emelyn T. Anicoy
■ Avoid eating late evening & avoid foods associated ● Pantoprazole 40 mg in 90
with reflux ml PNSS X5 hours x 72
■ Modify diet to reduce body weight, obesity, increase hours
abdominal pressure ● For bleeding: 100 mcg
○ LIFESTYLE MODIFICATION: Octreotide (bolus) (to
■ Sleep at night with HOB elevated at 6 inches decrease blood volume in
■ Remain upright after eating GI)
■ Avoid straining or excessive vigorous exercise ● 100 mcg octreotide in
■ Refrain wearing tight clothes 100 ml PNSS x4 hrs x 5
○ Surgical management: days
■ Fundoplication (wrapping a portion of stomach) ● Diagnostic evaluation:
■ Laparoscopic Nissen Fundoplication ○ Upper GI endoscopy
○ SIDE NOTES: ○ Serum liver function test
■ Liver cirrhosis: associated with esophageal varices ● Nursing interventions:
● Dilated tortuous veins usually found in the ○ Monitor VS strictly, LOC
submucosa of the lower esophagus ○ Maintain NPO, monitor blood studies
● Causes: Portal hypertension secondary to liver ○ Administer O2, BT, Vasopressin
cirrhosis ○ Assist in NGT and Sengstaken-
● Assessment findings: Blakemore Tube
○ Hematemesis ■ Never leave patient unattended
■ Pt should be NPO immediately ■ Closely monitor lumen pressure
○ Melena ■ Check v/s q30 mins
○ Hepatomegaly ■ Monitor for signs of respiratory
○ Splenomegaly distress
○ Jaundice ● Pinch the tube at the
■ Icteric sclera (yellowish patient’s nose and cut it
discoloration of sclera) with scissors
○ Ascites ■ Deflate the balloon for about 30
○ Signs of SHOCK! minutes every 8-12 hrs
■ Mgt:: ■ Provide mouth and nose care
● Tranexamic acid (bolus) ● Surgical mgt:
○ Endoscopic sclerotherapy
Transcribed by: Emelyn T. Anicoy
○ Endoscopic variceal ligation ○ Endoscopy (EGD) - confirmatory test
○ Shunt procedures ○ Esophageal manometry “motility testing”
● Nursing intervention:
GastroEsophageal Reflux Disease ○ Diet therapy: limit chocolate, fatty foods, caffeinated
● Problem in sphincter beverages, alcohol)
● Backward flow of stomach contents ○ Lifestyle changes: sleep in the left lateral (aiide-lying) position
● High risk for esophageal cancer if the pt has esophageal varices ● Surgical mgt:
● Hallmark of GERD: reflux esophagitis ○ Nissen fundoplication
● CAUSES:
○ INAPPROPRIATE RELAXATION OF LES/ CARDIAC PEPTIC ULCER DISEASE
SPHINCTER ● An open sore that occurs in the protective lining of the stomach or
○ GASTRIC VOLUME IS ELEVATED duodenum
○ DELAYED GASTRIC EMPTYING ● Break in the mucosal barrier
○ ABNORMAL ESOPHAGEAL CLEARANCE ○ Mucus and bicarbonate secretion (1st line of defense in pH
○ IRRITATION FROM REFLUX MATERIAL maintenance)
● ASSESSMENT FINDINGS: ○ Gastric Mucosal PH (increase barrier resistance to ulceration)
■ Heartburn (mimic angina radiating to neck, jaw, back) ○ Inadequate blood supply
■ Regurgitation ● H.pylori infection
■ Hypersalivation ○ Mgt: Amoxicillin and clarithromycin x14 days
■ Dysphagia ● Pyloric sphincter dysfunction
■ Odynophagia (painful swallowing) ● DUODENAL ULCER:
■ Barrett's epithelium - high risk for cancer ○ Prone to perforation
■ Considered premalignant in clients with prolonged ○ Melena
GERD ○ Young adult - 30-60 yo
■ Others: ○ Weight gain
● Chronic cough especially at night, asthma ● GASTRIC CANCER:
● Eructation ○ Prone to hemorrhage
● Flatulence ○ Prone to cancer
● Bloating after eating ○ Elderly - 60 and above
● Nausea and vomiting ○ Weight loss
● DX TEST: ○ Hematemesis
○ Most accurate method: 24 hour ambulatory pH Monitoring ● Delayed gastric emptying
Transcribed by: Emelyn T. Anicoy
● Risk factor: ● Possible complication:
○ Type A personality ○ Pernicious anemia
○ Blood type O ■ Mgt: Vit B12
○ NSAIDS (ibuprofen, aspirin (antiplatelet)) ○ Dumping syndrome (rapid gastric
○ Cigarette smoking emptying) - common after billroth 2
○ Chronic anxiety ■ Occur within 30 mins
● Complications: ■ Early Symptoms: vertigo,
○ Hemorrhage (usually indicates upper GI bleeding) tachycardia, syncope, sweating,
■ +coffee ground = instruct pt for NPO (usually for 3 pallor, palpitations, desire to lie
days); insert NGT; down
■ Bland diet = low residue +low fat diet ■ Late symptoms:
○ Perforation - Surgical EMERGENCY ‼️ ● Hyperglycemia
⬇️
● Laboratory assessment: ● Rebound hypoglycemia
○ hgb/hct ● Lightheadedness
■ Mgt: Blood transfusion (gauge 18- 22 (smallest)) ● Confusion
○ + occult blood ■ Mgt: don't take meals with fluid
■ No red-beefy food prior to the procedure ● High protein, high fat,
○ Endoscopy (EGD) - reveals ulceration low- to -moderate carbs
○ Gastric analysis diet
● Medical/nursing Mgt: CROHN'S DISEASE
○ Supportive (rest, bland diet, stress managemetn) ● An idiopathic inflammatory disease of the small intestine (60%), the
○ Drug therapy: colon (20%), or both
■ Antacids ● A.k.a. “Regional enteritis”
■ H2 receptor antagonists ● Terminal ileum : the site most often affected
■ PPI ○ Terminal ileum to transverse colon: Crohn's disease
■ Anticholinergics ■ Cobblestone appearance - (endoscopy)
■ Antibiotic ■ String sign - barium swallow
○ Surgery: ● Causes:
■ Billroth 1 (gastroduodenostomy) - distal end of stomach ○ Unknown, thought to be autoimmune
is removed and is anastomosed to duodenum ○ M. Paratuberculosis
■ Billroth 2 (gastrojejunostomy) - distal end of stomach is ○ Genetic predisposition
removed and is anastomosis to jejunum ● Pathology:
Transcribed by: Emelyn T. Anicoy
○ Deep fissures ures & ulceration develops - bowel fistulas - ■ Ileostomy - 12 to 18 inches elevated above the stoma
diarrhea & malabsorption in irrigation and 3-4 inches deep
● Clinical manifestations: ● Prone to dehydration
○ Diarrhea (steatorrhea is common & sometimes bloody) ■ Pencil shape stool - pt with colon cancer
■ Prone to hypokalemia
○ Constant abdominal pain APPENDICITIS
○ Abdominal distention ● Inflammation of the vermiform appendix Due to fecalith
○ Low-grade fever ● Pain “McBurney’s point”
○ Weight loss (80% of clients) ○ Blumberg sign = (+) rebound tenderness
○ Beware for signs of peritonitis, bowel obstruction, nutritional ○ Psoas sign = lateral position with right hip flexion
& fluid imbalances ○ Rovsing’s sign = right quadrant pain when left is palpated
● Nursing mgt: ○ Obturator’s sign = pain on external rotation of the right thigh
○ Bedrest without toilet privileges ○ Jarring sign
○ TPN ● NO WARM COMPRESS/ HEATING PADS
● NO LAXATIVE/ ENEMA/LACTULOSE
ULCERATIVE COLITIS ● Assessment findings:
● Ulcerative and inflammatory condition of affecting the mucosal lining ○ Nausea and vomiting
of the colon or rectum ○ Anorexia
● +rectal bleeding ○ Decreased bowel sounds
○ Prone to anemia, shock ○ Fever, low grade
■ During shock: Modified Trendelenburg Position ○ High grade fever = RUPTURED!
⬆️
● Assessment findings: ● Diagnostic test:
○ Anorexia ○ WBC (above 10, 000 cu.mm.)
○ Weight loss ○ Elevated acetone in urine
○ Fever ○ Ultrasound and abdominal x-ray (detection of fecalith)
○ Severe Diarrhea: 20-30 times per day with rectal bleeding ● Nursing intervention:
○ Anemia ○ Administer antibiotics/antipyretics as ordered
○ Dehydration ○ Prevent perforation of the appendix; don't give enemas or
○ Abdominal pain and cramping cathartics or use heating pads
● Surgical mgt: ○ In addition to routine pre-op care for appendectomy:
○ Colectomy ■ Give support to parents if seeking treatment was
delayed
Transcribed by: Emelyn T. Anicoy
⬆️ lipid levels
⬇️serum calcium
■ Explain necessity of obtaining lab work prior to surgery ○
○
PANCREATITIS ○ CT scan: enlargement of the pancreas
● An inflammatory process with varying degrees of pancreatic edema,
fat necrosis, or hemorrhage
● Proteolytic and lipolytic pancreatic enzymes are activated in the
pancreas rather than in the duodenum, resulting to tissue damage
and autodigestion of the pancreas
● Occurs most often in the middle aged
● Assessment findings:
○ Pain LUQ
○ N&V, decrease/absent bowel sounds
○ +cullen’s sign (ecchymoses of periumbilical area)
○ + Grey Turner's spots (ecchymoses on flanks)
○ High amylase, lipase and hyperglycemic
○ Tachycardia
○ Abdominal tenderness w/ muscle-guarding
● Medical/ nursing intervention:
○ NGT - for decompression ; assess for drainage
○ NPO
○ CBG every hour
○ Administer analgesics, antacids, anticholinergics as ordered,
monitor effects
○ Morphine sulfate - pain medication
■ Monitor RR, BP, sensorium, and pupillary reaction
■ Antidote: Narcan 0.4 mg q 3 mins up to 10 mg
○ Assist client to positions of comfort (knee chest, fetal position)
○ Teach relaxation techniques and provide a quiet environment
⬆️
● Diagnostic test:
⬆️
○ serum amylase (>300 somogyi units) & lipase
⬆️
○ urinary amylase
○ blood sugar
Transcribed by: Emelyn T. Anicoy
You might also like
- DIABETES MELLITUS-doneDocument10 pagesDIABETES MELLITUS-donecory kurdapya100% (1)
- DSM 5 Clinical Cases NotesDocument1 pageDSM 5 Clinical Cases Notestim clayNo ratings yet
- NCM 118 LEC - FINALS - Docx Google DocsDocument33 pagesNCM 118 LEC - FINALS - Docx Google DocsFrancesca Aurea MagumunNo ratings yet
- Perioperative NursingDocument9 pagesPerioperative NursingHannah PatriciaNo ratings yet
- Peptic Ulcer DiseaseDocument1 pagePeptic Ulcer DiseaseHANNAH MICOLE GAERLANNo ratings yet
- CA - Emergency and Disaster Nursing PDFDocument5 pagesCA - Emergency and Disaster Nursing PDFMarvin Heramis RyanNo ratings yet
- Gastroenterology Case Discussion: JANUARY 07, 2021 Dr. Stephen Wong Indigo and VioletDocument19 pagesGastroenterology Case Discussion: JANUARY 07, 2021 Dr. Stephen Wong Indigo and VioletJolaine ValloNo ratings yet
- Step 3 Surgery Uworld NotesDocument11 pagesStep 3 Surgery Uworld Notesaleks patralskaNo ratings yet
- HW1 Ibanez Bio PDFDocument2 pagesHW1 Ibanez Bio PDFBanjo IbañezNo ratings yet
- Course Notes FinalDocument97 pagesCourse Notes FinalChantel BlackNo ratings yet
- Bailey LoveDocument4 pagesBailey Lovemonirul islam shohanNo ratings yet
- EctopicDocument9 pagesEctopicJo CanensNo ratings yet
- Functions of The Peritoneum in Health: Causes of Peritoneal InflammationDocument6 pagesFunctions of The Peritoneum in Health: Causes of Peritoneal Inflammationmonirul islam shohanNo ratings yet
- Surgery ReviewerDocument21 pagesSurgery ReviewerHarissa Katrina De LaraNo ratings yet
- TreatmentDocument284 pagesTreatmenthobbycontestsNo ratings yet
- Diverticulitis ConferenceDocument9 pagesDiverticulitis ConferencemimicamasoNo ratings yet
- Tourocom Oms2: Omm (Section Done)Document56 pagesTourocom Oms2: Omm (Section Done)Ritesh PatelNo ratings yet
- NR 602 Week 8 Final Exam Completed Study GuideDocument20 pagesNR 602 Week 8 Final Exam Completed Study GuideTyler HemsworthNo ratings yet
- Peds Exam 2Document38 pagesPeds Exam 2Stephanie SuruNo ratings yet
- (ANES) Mon 01 Epidural For Labor Analgesia (A2021)Document3 pages(ANES) Mon 01 Epidural For Labor Analgesia (A2021)Miguel SantosNo ratings yet
- 04 - Maternal Adaptation To PregnancyDocument4 pages04 - Maternal Adaptation To PregnancyKyrriel CNo ratings yet
- Advanced Clinical Problem Solving Transition Into Nursing PracticeDocument55 pagesAdvanced Clinical Problem Solving Transition Into Nursing PracticeZarida ArabainNo ratings yet
- Disturbances in DigestionDocument2 pagesDisturbances in DigestionAnabelle RicoNo ratings yet
- LEC 08-Hernia-Collective NotesDocument36 pagesLEC 08-Hernia-Collective NotesAmira NabilNo ratings yet
- 2y2s (Surgery) - The Abdomen PrintablesDocument9 pages2y2s (Surgery) - The Abdomen PrintablesCarmela MarianoNo ratings yet
- SHYA Episode 16 ShownotesDocument7 pagesSHYA Episode 16 ShownotesKarthikNo ratings yet
- OnG Viva Sample Ans Nea 2021 b1Document82 pagesOnG Viva Sample Ans Nea 2021 b1MumtaNo ratings yet
- CCE1 AirwayDocument8 pagesCCE1 AirwayHoward ChangNo ratings yet
- Unit 4 PDFDocument24 pagesUnit 4 PDFkryllagtagmaNo ratings yet
- Drug Study - Omeprazole and ParacetamolDocument11 pagesDrug Study - Omeprazole and ParacetamolMarceline VueenNo ratings yet
- HEALTH ASSESSMENT - Breasts & Regional LymphaticsDocument5 pagesHEALTH ASSESSMENT - Breasts & Regional LymphaticsMich Hiel OforraNo ratings yet
- Chapter 38 - Cystic FibrosisDocument3 pagesChapter 38 - Cystic FibrosisNisreen SalameNo ratings yet
- M4 - Didactic - NCM 118Document4 pagesM4 - Didactic - NCM 118KARL FESARITNo ratings yet
- Non-Inflammatory Bowel DisordersDocument33 pagesNon-Inflammatory Bowel Disorderssho bartNo ratings yet
- OB COMPLETE Bleeding 4 Ps Postpartum GyneDocument32 pagesOB COMPLETE Bleeding 4 Ps Postpartum GynelouvvhartNo ratings yet
- Rehabilitation Post StrokeDocument27 pagesRehabilitation Post StrokeNorNashiraMohdIbrahimNo ratings yet
- NCM109 Maternal - Child Nursing (A-C) - Module 5Document6 pagesNCM109 Maternal - Child Nursing (A-C) - Module 5iratsyukieNo ratings yet
- Week 9Document3 pagesWeek 9api-530814583No ratings yet
- Transes Tra - Peri-OpDocument11 pagesTranses Tra - Peri-OpJoshua DelantarNo ratings yet
- GYNECOLOGY Chief ComplaintsDocument3 pagesGYNECOLOGY Chief ComplaintsJennifer HerediaNo ratings yet
- Paraoesophageal HerniaDocument1 pageParaoesophageal HerniamuhammadridhwanNo ratings yet
- MS-SL Prelims FirstsemDocument17 pagesMS-SL Prelims Firstsemmcdonald 1234No ratings yet
- Upper GIT 1Document18 pagesUpper GIT 1Zuhra JabeenNo ratings yet
- MS Lec Gi and Icp Reviewer - Limon, Adine Jeminah DDocument8 pagesMS Lec Gi and Icp Reviewer - Limon, Adine Jeminah DShawn TejanoNo ratings yet
- Med-Surg Final Exam Study GuideDocument40 pagesMed-Surg Final Exam Study GuideCaitlyn BilbaoNo ratings yet
- Basic Care and ComfortDocument49 pagesBasic Care and Comfortdelrosariodenisejoy05No ratings yet
- CMCA FinalsDocument11 pagesCMCA FinalsBagsit Angelique Khryztelle G.No ratings yet
- TransesDocument5 pagesTransesTintin HonraNo ratings yet
- Spinal Cord Injury Lecture Notes Chapter 60Document7 pagesSpinal Cord Injury Lecture Notes Chapter 60Raina Ginella DsouzaNo ratings yet
- Acute Pancreatitis: Aguirre, Lucas Galligani, Guido Gorostiaga, Marcos Kreutzer, GustavoDocument20 pagesAcute Pancreatitis: Aguirre, Lucas Galligani, Guido Gorostiaga, Marcos Kreutzer, GustavoGüids GalliganiNo ratings yet
- Acute Pancreatitis: Aguirre, Lucas Galligani, Guido Gorostiaga, Marcos Kreutzer, GustavoDocument20 pagesAcute Pancreatitis: Aguirre, Lucas Galligani, Guido Gorostiaga, Marcos Kreutzer, GustavoGüids GalliganiNo ratings yet
- EINCDocument8 pagesEINCneehoshiNo ratings yet
- Digestive System Healthcare Center by SlidesgoDocument16 pagesDigestive System Healthcare Center by SlidesgoGhadeer AlobaidNo ratings yet
- 05.3 Problems of The Power and Psyche PDFDocument12 pages05.3 Problems of The Power and Psyche PDFJAN CAMILLE LENONNo ratings yet
- 6 - 19 NotesDocument4 pages6 - 19 NotesFefe JejeNo ratings yet
- Finals - GeriaDocument3 pagesFinals - GeriaKaren May HontiverosNo ratings yet
- OB Notes For Part 2Document14 pagesOB Notes For Part 2aaaalliah2No ratings yet
- SLH TopicsDocument10 pagesSLH TopicskulangkatunNo ratings yet
- Nursing Care of Clients With Vascular DisordersDocument5 pagesNursing Care of Clients With Vascular DisordersVinzii DrtNo ratings yet
- Pediatric ConceptDocument19 pagesPediatric ConceptAntonio Intia IVNo ratings yet
- Diabetes in Hospital: A Practical Approach for Healthcare ProfessionalsFrom EverandDiabetes in Hospital: A Practical Approach for Healthcare ProfessionalsNo ratings yet
- The Complete Dysphagia Diet Cookbook:The Ultimate Nutrition Guide For People With Swallowing And Chewing Difficulties With Foodlist, Meal Plan And Nourishing RecipesFrom EverandThe Complete Dysphagia Diet Cookbook:The Ultimate Nutrition Guide For People With Swallowing And Chewing Difficulties With Foodlist, Meal Plan And Nourishing RecipesNo ratings yet
- DR Lila - Patient Preparation For Emergencies Surgeries - New 11012017Document37 pagesDR Lila - Patient Preparation For Emergencies Surgeries - New 11012017bloadyroar100% (1)
- Commonly Used Medical AbbreviationsDocument7 pagesCommonly Used Medical Abbreviationsabdollah alkhiamyNo ratings yet
- Rheumatoid Arthritis OrenciaDocument8 pagesRheumatoid Arthritis OrenciavishwanathNo ratings yet
- 2nd MAPEH 3Document2 pages2nd MAPEH 3Edmar MejiaNo ratings yet
- Colorectal Cancer - Epidemiology, Risk Factors, and Protective Factors - UpToDateDocument38 pagesColorectal Cancer - Epidemiology, Risk Factors, and Protective Factors - UpToDateYdeli DetanNo ratings yet
- Mental RetardationDocument14 pagesMental RetardationSumam NeveenNo ratings yet
- Diet A Coherent e PDFDocument25 pagesDiet A Coherent e PDFMarcos PallaresNo ratings yet
- Kok OlogyDocument3 pagesKok OlogyAnnie Ofo-obNo ratings yet
- ICMR Diabetes Guidelines.2018Document70 pagesICMR Diabetes Guidelines.2018A. RaufNo ratings yet
- 100 Free NCLEX RN Question and Answers With RationalesDocument32 pages100 Free NCLEX RN Question and Answers With Rationalesaprnworld100% (1)
- Sno Specific Objectives Duratio N Content Teacher /learning Av Aids B/B Activity EvaluationDocument9 pagesSno Specific Objectives Duratio N Content Teacher /learning Av Aids B/B Activity Evaluationjasmine100% (2)
- Msap Safety IDocument5 pagesMsap Safety IJoseph AldrinNo ratings yet
- CLRT Final ProjectDocument28 pagesCLRT Final Projectapi-358148089No ratings yet
- Otologic Hazards Related To Scuba Diving: Primary CareDocument5 pagesOtologic Hazards Related To Scuba Diving: Primary CareaisyahNo ratings yet
- Great Atlas of Dermatology IndexedDocument73 pagesGreat Atlas of Dermatology Indexedjohn pauloNo ratings yet
- Journal Reading Yolla ElfiraDocument24 pagesJournal Reading Yolla Elfiraika irmalaNo ratings yet
- TB (Tuberkulosis)Document30 pagesTB (Tuberkulosis)Fanny BudimanNo ratings yet
- DR Milan Ignjatovic - Ignjatovici 40 Godina U PsihijatrijiDocument152 pagesDR Milan Ignjatovic - Ignjatovici 40 Godina U PsihijatrijiAleksandar Pasku100% (4)
- Clinical Sciences Study PlanDocument30 pagesClinical Sciences Study PlanRomulo Vincent PerezNo ratings yet
- Krabbe, K.S., Nielsen, A.R., Krogh-Madsen, R. Et Al. Diabetologia (2007) 50: 431Document3 pagesKrabbe, K.S., Nielsen, A.R., Krogh-Madsen, R. Et Al. Diabetologia (2007) 50: 431preethiNo ratings yet
- Drug StudyDocument6 pagesDrug StudyMajo Coronel100% (1)
- AURELIO-Issues, Trends and Challenges On The Care of Older Persons in The Different SettingsDocument15 pagesAURELIO-Issues, Trends and Challenges On The Care of Older Persons in The Different Settings3D - AURELIO, Lyca Mae M.No ratings yet
- Pelagio-Drug StudyDocument45 pagesPelagio-Drug StudyShiena Mae PelagioNo ratings yet
- What Is A Liver Disease DietDocument2 pagesWhat Is A Liver Disease DietPrashanth RajuNo ratings yet
- Alcoholic Liver Disease: Mark E. Mailliard, Michael F. SorrellDocument13 pagesAlcoholic Liver Disease: Mark E. Mailliard, Michael F. SorrellJolaine ValloNo ratings yet
- AbscessDocument16 pagesAbscessPlày GameNo ratings yet
- Food Fats and Oils Institute of Shortening and Edible Oil 8ava CampbellDocument46 pagesFood Fats and Oils Institute of Shortening and Edible Oil 8ava Campbellrcrochar100% (1)
- Glenda ResumeDocument6 pagesGlenda Resumeglenda carnajeNo ratings yet