Professional Documents
Culture Documents
Medical 66
Medical 66
Uploaded by
eyobCopyright:
Available Formats
You might also like
- (Oxford Chemistry Primers, 02) David T. Davies - Aromatic Heterocyclic Chemistry (1992, Oxford University Press)Document92 pages(Oxford Chemistry Primers, 02) David T. Davies - Aromatic Heterocyclic Chemistry (1992, Oxford University Press)Awad SaidNo ratings yet
- Brand Positioning The Battle of The Mind: Mccormick vs. FuchsDocument12 pagesBrand Positioning The Battle of The Mind: Mccormick vs. FuchsLaura Mng100% (1)
- More Than 2000 Solved MCQs On Research MethodsDocument127 pagesMore Than 2000 Solved MCQs On Research MethodsBhushan Chaudhari100% (2)
- The Current Relationship Between Surgeon ReimburseDocument4 pagesThe Current Relationship Between Surgeon ReimburseRenan Scalon MachadoNo ratings yet
- Cost Analysis of An Intensive Care UnitDocument7 pagesCost Analysis of An Intensive Care UnitSabrina JonesNo ratings yet
- Circinterventions 120 010228Document3 pagesCircinterventions 120 010228Klinik Bhina Mitra SetyaNo ratings yet
- Estimating The Costs of Hospital Acquired InfectionDocument19 pagesEstimating The Costs of Hospital Acquired InfectionMatthew KuenzelNo ratings yet
- Jamasurgery Childers 2018 Oi 170128Document7 pagesJamasurgery Childers 2018 Oi 170128loloNo ratings yet
- The Costs of Nosocomial InfectionsDocument4 pagesThe Costs of Nosocomial InfectionsCandra BumiNo ratings yet
- An Analysis of Hospital Costs by Cost Center, 1971 Through 1978Document17 pagesAn Analysis of Hospital Costs by Cost Center, 1971 Through 1978YantoNo ratings yet
- Conditions With The Largest Number of Adult Hospital Readmissions by Payer, 2011Document10 pagesConditions With The Largest Number of Adult Hospital Readmissions by Payer, 2011David HarlowNo ratings yet
- Custo Efetividade Monitorizacao - 1Document8 pagesCusto Efetividade Monitorizacao - 1André Almeida e SilvaNo ratings yet
- 8 BaruDocument4 pages8 BaruAnditha Namira RSNo ratings yet
- The Costs of Intensive 2006 Continuing Education in Anaesthesia Critical CADocument4 pagesThe Costs of Intensive 2006 Continuing Education in Anaesthesia Critical CAronaldquezada038No ratings yet
- Proposal Defence Presentation PDFDocument25 pagesProposal Defence Presentation PDFbayu priyatnaNo ratings yet
- 1 s2.0 S1083879120305735 MainDocument3 pages1 s2.0 S1083879120305735 MainCommon JaiswalNo ratings yet
- 18 - Blood Cross-Match Ordering PracticesDocument3 pages18 - Blood Cross-Match Ordering PracticesKamran FarooquiNo ratings yet
- 01 - Cost of AKIDocument7 pages01 - Cost of AKIFloridalma FajardoNo ratings yet
- Direct Medical Costs of Hospitalized Patients With.16Document3 pagesDirect Medical Costs of Hospitalized Patients With.16jai.kumar.maingiNo ratings yet
- Prognosis Pneumonia PDFDocument18 pagesPrognosis Pneumonia PDFamania jeumpa nur alamNo ratings yet
- BEST Kidney StudyDocument10 pagesBEST Kidney StudyJoseph Zenas JungNo ratings yet
- Factors Affecting ED Length-of-Stay in Surgical Critical Care PatientsDocument6 pagesFactors Affecting ED Length-of-Stay in Surgical Critical Care PatientsMuhammad HidayantoNo ratings yet
- New Estimates of Elasticity of Demand For Healthcare in Rural China 2011 0Document11 pagesNew Estimates of Elasticity of Demand For Healthcare in Rural China 2011 0wangxinfeng1998No ratings yet
- Emergency Medicine Resident Efficiency and Emergency Department CrowdingDocument9 pagesEmergency Medicine Resident Efficiency and Emergency Department CrowdingRenzo Iván Marín DávalosNo ratings yet
- Journal Pone 0247042Document9 pagesJournal Pone 0247042irenzdcruzzNo ratings yet
- The Overall Percentage of The Elderly Living in Nursing Homes Is 5%Document21 pagesThe Overall Percentage of The Elderly Living in Nursing Homes Is 5%Kelly FitzgeraldNo ratings yet
- The Direct Medical Costs Of: Healthcare-Associated Infections in U.S. Hospitals and The Benefits of PreventionDocument16 pagesThe Direct Medical Costs Of: Healthcare-Associated Infections in U.S. Hospitals and The Benefits of PreventionjnplnceNo ratings yet
- The Impact of Hospital Safety-Net Burden On Mortality and Readmission After CABG SurgeryDocument10 pagesThe Impact of Hospital Safety-Net Burden On Mortality and Readmission After CABG SurgerymartarguezNo ratings yet
- A High-Volume Specialist Palliative Care Unit and Team May Reduce In-Hospital End-of-Life Care CostsDocument8 pagesA High-Volume Specialist Palliative Care Unit and Team May Reduce In-Hospital End-of-Life Care CostsNurbaiti Indah LestariNo ratings yet
- Emergency Referrals PDFDocument8 pagesEmergency Referrals PDFEngidaNo ratings yet
- Administration of Emergency MedicineDocument9 pagesAdministration of Emergency MedicineNurul AidaNo ratings yet
- J Jacc 2012 07 017Document6 pagesJ Jacc 2012 07 017Andi Tiara S. AdamNo ratings yet
- J Jacc 2012 07 017Document6 pagesJ Jacc 2012 07 017Andi Tiara S. AdamNo ratings yet
- J Jacc 2012 07 017Document6 pagesJ Jacc 2012 07 017Andi Tiara S. AdamNo ratings yet
- Nurse Staffing and Inpatient Hospital Mortality: Special ArticleDocument9 pagesNurse Staffing and Inpatient Hospital Mortality: Special ArticlemourienNo ratings yet
- Burden of Illness For Osteoporotic Fractures Compared With Other Serious Diseases Among Postmenopausal Women in The United StatesDocument10 pagesBurden of Illness For Osteoporotic Fractures Compared With Other Serious Diseases Among Postmenopausal Women in The United StatesSharan SahotaNo ratings yet
- RLE Journal ArticleDocument9 pagesRLE Journal ArticleMia MabaylanNo ratings yet
- 155778-Article Text-406683-1-10-20170509Document6 pages155778-Article Text-406683-1-10-20170509Tricia Jane OpinaldoNo ratings yet
- AbstractDocument36 pagesAbstractJackson MwaiNo ratings yet
- Costs of Hospital MalnutritionDocument6 pagesCosts of Hospital MalnutritionAmalia SarsolNo ratings yet
- quinn2015Document8 pagesquinn2015Familia En AcNo ratings yet
- Mission Hospital Case 11Document12 pagesMission Hospital Case 11Business Monkeys0% (1)
- Archive of SIDDocument5 pagesArchive of SIDSurya WijayaNo ratings yet
- The Effect of Burn Center Volume On Mortality in A Pediatric Population: An Analysis of The National Burn RepositoryDocument6 pagesThe Effect of Burn Center Volume On Mortality in A Pediatric Population: An Analysis of The National Burn Repositoryasmaa elnabawy1No ratings yet
- 1 s2.0 S2212109917300286 MainDocument8 pages1 s2.0 S2212109917300286 MainEya BaldostamonNo ratings yet
- Soi 130026Document7 pagesSoi 130026jose pablo reyes ortizNo ratings yet
- Soi 130026Document7 pagesSoi 130026jose pablo reyes ortizNo ratings yet
- Jurnal LainDocument22 pagesJurnal LainBudi ArsanaNo ratings yet
- Ambulatory Care Groups: A Categorization of Diagnoses For Research and ManagementDocument22 pagesAmbulatory Care Groups: A Categorization of Diagnoses For Research and ManagementbrskopjeNo ratings yet
- Diagnostic Related Groupings Saakat AddDocument46 pagesDiagnostic Related Groupings Saakat AddTheocryte SergeotNo ratings yet
- J Aem 2007 06 035Document8 pagesJ Aem 2007 06 035kingkinresmytaNo ratings yet
- Burden of Surgical Site Infections in The NetherlandsDocument10 pagesBurden of Surgical Site Infections in The NetherlandsKanokwan BorwornphiphattanachaiNo ratings yet
- 10 1001@jamaoncol 2019 0086Document8 pages10 1001@jamaoncol 2019 0086Akshay BadoreNo ratings yet
- Sacks - Variation in Hospital UseDocument9 pagesSacks - Variation in Hospital UseUm ShooqNo ratings yet
- The Preoperative Cost of Carpal Tunnel Syndrome: PurposeDocument11 pagesThe Preoperative Cost of Carpal Tunnel Syndrome: PurposeRonal Zumaeta PortocarreroNo ratings yet
- Migrain in The WorldDocument5 pagesMigrain in The WorldveNo ratings yet
- Hospital Overhead Costs: The Neglected Driver of Health Care Spending?Document15 pagesHospital Overhead Costs: The Neglected Driver of Health Care Spending?hasan najiNo ratings yet
- FRBSF: Conomic EtterDocument5 pagesFRBSF: Conomic EttermamuyaNo ratings yet
- Risk Factors For Falls in Hospital In-Patients: A Prospective Nested Case Control StudyDocument7 pagesRisk Factors For Falls in Hospital In-Patients: A Prospective Nested Case Control StudyNurhasanah HaryaniNo ratings yet
- CMA AntibioticsDocument11 pagesCMA AntibioticsNovita Oktavianti DehiNo ratings yet
- Burden AF With Ischemic StrokeDocument8 pagesBurden AF With Ischemic StrokeWirawan PrabowoNo ratings yet
- The Potential For Cost Savings Through Bundled Episode PaymentsDocument3 pagesThe Potential For Cost Savings Through Bundled Episode PaymentsGeorge L. YerkesNo ratings yet
- Model by Brandon Build by LuisDocument16 pagesModel by Brandon Build by LuisixosotocNo ratings yet
- Project ProposalDocument4 pagesProject ProposalQueenie Diane MontañoNo ratings yet
- GL Period CloseDocument12 pagesGL Period CloseMd MuzaffarNo ratings yet
- .. Thesis Title .Document31 pages.. Thesis Title .Tanut VongsoontornNo ratings yet
- KEM Epoxy Grout ELV - 1Document2 pagesKEM Epoxy Grout ELV - 1BinodNo ratings yet
- KADIMP Book Email 2Document116 pagesKADIMP Book Email 2ZINART MUSANo ratings yet
- WS Emergency Echo SYMCARD 2022Document33 pagesWS Emergency Echo SYMCARD 2022IndRa KaBhuomNo ratings yet
- The Present Perfect and The Present Perfect Continuous: Finished and Unfinished ActionsDocument26 pagesThe Present Perfect and The Present Perfect Continuous: Finished and Unfinished ActionsyahiaouimalekNo ratings yet
- Types of CurriculumDocument3 pagesTypes of CurriculumBabylyn Frias100% (1)
- DBA CockpitDocument337 pagesDBA Cockpithimanshu.singh0011282No ratings yet
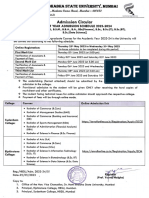
- Circular - HBSU UG Admission, 2023-24Document2 pagesCircular - HBSU UG Admission, 2023-24Shyam GaikwadNo ratings yet
- SCF 020 - Ship Shore Safety ChecklistDocument8 pagesSCF 020 - Ship Shore Safety ChecklistSutarmoNo ratings yet
- Play Format ExampleDocument3 pagesPlay Format ExamplemegbenignoNo ratings yet
- C32 - PFRS 5 Noncurrent Asset Held For SaleDocument4 pagesC32 - PFRS 5 Noncurrent Asset Held For SaleAllaine ElfaNo ratings yet
- Compaction Trends Shale CleanSands Gulf of MexicoDocument8 pagesCompaction Trends Shale CleanSands Gulf of MexicoAfonso ElvaNo ratings yet
- Ee Monthly Price Plans: Your Plan Terms & Price Guide Available From 10 May 2017Document10 pagesEe Monthly Price Plans: Your Plan Terms & Price Guide Available From 10 May 2017Ana ModyNo ratings yet
- Wget - Curl Large File From Google Drive - Stack OverflowDocument29 pagesWget - Curl Large File From Google Drive - Stack OverflowManoj KamisettiNo ratings yet
- SB19 Water-KomprimiertDocument101 pagesSB19 Water-KomprimiertNatasa KakesNo ratings yet
- ZTE LTE FDD Clock Synchronization Feature GuideDocument103 pagesZTE LTE FDD Clock Synchronization Feature Guidem2adeelNo ratings yet
- Inaccuracies in Manometric Central Venous Pressure MeasurementDocument10 pagesInaccuracies in Manometric Central Venous Pressure MeasurementmfhfhfNo ratings yet
- Sf4 ConceptDocument10 pagesSf4 ConceptAndrás FarkasNo ratings yet
- Sip Design and Verification Using AdsDocument34 pagesSip Design and Verification Using AdsMaria Lavinia IordacheNo ratings yet
- MYY&MZZ Manual Transmission (Ver4)Document32 pagesMYY&MZZ Manual Transmission (Ver4)Vahid Reza MohammadiNo ratings yet
- Art NouveauDocument73 pagesArt NouveauRuqayya AhmedNo ratings yet
- WA-LD-45 PPP For New Direction PAC (March 2017)Document2 pagesWA-LD-45 PPP For New Direction PAC (March 2017)Daily Kos ElectionsNo ratings yet
- SNGPL - Web BillDocument1 pageSNGPL - Web BillNazeer Ahmed100% (1)
- Mathematics 3Document2 pagesMathematics 3Tony StarkNo ratings yet
Medical 66
Medical 66
Uploaded by
eyobOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Medical 66
Medical 66
Uploaded by
eyobCopyright:
Available Formats
Source of Admission and Cost: Public Hospitals Face Financial Risk
ERIc Muroz, MD, MBA, RICHARD SOLDANO, BA, MPH, ANN LAUGHLIN, BS,
IRVING B. MARGOLIS, MD, AND LESLIE WISE, MD
Financial Information
Abstract: We studied all admissions to the 11 acute care The Health and Hospitals Corporation (HHC) costing
hospitals of the New York City Health and Hospitals Corporation methodology is a stepdown allocative process by cost cen-
(April 1983-September 1984) matching emergency room (ER) admit- ter. Four costs are reported on each record: ancillary indi-
ted diagnostic related group (DRG) subgroups in each hospital with rect, ancillary direct, routine indirect, routine direct. Direct
at least five non-ER admitted patients (N = 222,961). Mean cost per costs are taken from the hospital's inpatient billing master
ER patient ($8,385) was greater than non-ER mean cost per patient files and merged with clinical files to produce databases.
($4,386) for Medicare and non-Medicare. Our data suggest that Indirect costs are based on 1983 Institutional Cost Reports.
public hospitals with a high proportion of ER admissions may be at For each cost center, there is a ratio of direct to indirect cost
a financial disadvantage under DRG reimbursement. (Am J Public which is added to the record. Routine costs are based on
Health 1986; 76:696-697.) census reports and tallied according to the hospital's specific
inpatient daily rates in effect. Ancillary costs are based on
total volume of ancillary tests performed to arrive at a unit
Introduction cost per ancillary at each hospital. Teaching costs are
The new Medicare Prospective Payment System (PPS) allocated as both direct and indirect components to routine
based on Diagnostic Related Groups (DRGs) will encourage and ancillary costs. Most hospitals in the system show no
providers of medical care to assess the financial risk gener- major case-mix variation.
ated by various populations. We have demonstrated in four
earlier studies that emergency room (ER) admission predicts Results
higher cost per DRG in a large voluntary hospital in New
York City in an affluent New York suburb." The current Aggregate costs for the 18-month period for the entire
project was initiated to study the applicability of these study population were $1,735,062,632 (mean per patient,
findings to a large public multihospital system serving a $7,782). For matched DRGs per hospital, 70.9 per cent of the
different population. study population (158,159 admissions) was in DRGs that had
higher cost ER admissions for that DRG (Table 1). On the
Methods other hand, for 64,802 admissions (29.1 per cent) of the study
population, non-ER admissions were at greater cost than ER
Cost data on all admissions to the 11 acute care hospi- admissions. For Medicare admissions (19,132), 73.0 per cent
tals of the New York City Health and Hospitals Corporation of admissions (13,958) were in matched DRG subgroups
(NYCHHC) were analyzed during the 18-month period, where ER admissions were more costly than non-ER admis-
April 1983-September 1984 (N = 379,682). This system is sions; ER costs in this group were $10,552 vs non-ER costs
the largest non-federal public acute care hospital system in of $5,424. For non-Medicare admissions (203,829), the cor-
the United States. DRG, route of admission-emergency responding figures were $6,218 for ER admissions vs non-ER
room vs non-emergency room (outpatient clinic)-and payor costs of $3,312.
(Medicare vs non-Medicare) are routinely recorded on data Table 2 indicates the mean cost per patient for ER and
tapes. At each hospital, for each DRG, only matched DRG matched non-ER admissions in those DRGs where ER
subgroups containing five patients or more per variable admissions were the more expensive for the 11 hospitals in
(emergency admission and non-emergency admission) were the New York City system. Highest costs per ER admission
analyzed. The study population included 222,961 patients. were at Hospital G (750-850 beds), Hospital A (350450
A cost per patient comparison was then conducted on beds), and Hospital D (550-650 beds). Greatest differences in
ER vs non-ER admission for each matched DRG subgroup cost between ER and matched non-ER admission were at
at each hospital. The only patients admitted via the emer- Hospital F (with 550-650 beds) (267 per cent), Hospital K
gency room are those judged by the attending physicians to (with over 1,000 beds) (240 per cent), and Hospital H (with
have an emergency presentation of their disease. Analysis 750-850 beds) (235 per cent).
by payor type was also conducted for ER and non-ER Emergency admissions were 58.5 per cent of the total
admissions. admissions of'the entire study population for the study
We divided the study population into two periods, first period. Mean DRG consistency from one period to the next
nine months and second nine months. DRGs that had been for the whole population was only 53.5 per cent (Table 3).
shown to be more expensive for ER admissions were com- Number of higher cost DRGs fitting the study design that
piled for each hospital for both periods and compared for remained constant between periods ranged from a high of 97
consistency. DRGs that did not fit the study design, i.e., at DRGs to a low of 20. Three hospitals had high consistency
least five ER and five non-ER admissions in both periods between periods.
were dropped from the analysis.
From the Department of Surgery, Queens Hospital Center and Long Discussion
Island Jewish Medical Center, and the State University of New York, Stony
Brook. Address reprint requests to Eric Muhioz, MD, MBA, Head, Research This study suggests that route of admission in this public
Division, Department of Surgery, Long Island Jewish Medical Center, New hospital system may be a relatively powerful predictor of
Hyde Park, NY 11042. This paper, submitted to the Journal August 7, 1985,
was revised and accepted for publication December 17, 1985. costs within each DRG. This difference seems to be only
moderately DRG-specific, however, for reasons that are
© 1986 American Journal of Public Health 0090-0036/86$1.50 unclear.
696 AJPH June 1986, Vol. 76, No. 6
PUBLIC HEALTH BRIEFS
TABLE 1-Costs by Source of Admission for Matched DRG Subgroups
Matched
ER Cases Non-ER Cases Matched
Category (sample size) ER Mean Cost* (sample size) Non-ER Mean Cost*
ER admissions greater cost than non-ER 79,540 $8,385 78,619 $ 4,386
Non-ER admissions greater cost than ER 50,814 $7,021 13,988 $11,538
'mean per patient cost.
TABLE 2-Costs of ER and Non-ER Admissions Per Matched DRG, Aggregated by Hospital
Mean Cost*
Hospital Type/Size Mean Cost* ER Admission Matched Non-ER Admission
350-450 beds
Hospital A $13,174 ( 4,857)** $9,959 ( 4,268)**
Hospital B 6,693 ( 5,698) 3,327 ( 5,291)
Hospital C 6,357 ( 7,800) 3,563 ( 9,696)
550-650 beds
Hospital D 10,889 ( 6,356) 5,211 ( 4,876)
Hospital E 7,653 ( 5,725) 4,746 ( 6,664)
Hospital F 5,802 ( 4,637) 2,169 ( 7,170)
750-850 beds
Hospital G 13,222 ( 5,228) 5,774 ( 8,292)
Hospital H 7,220 ( 6,789) 3,065 ( 6,051)
Hospital 5,621 ( 3,590) 3,435 ( 2,443)
Over 1000 beds
Hospital J 8,567 (15,141) 3,866 ( 9,212)
Hospital K 7,045 (13,719) 2,935 (14,656)
Mean for All Hospitals $ 8,385 (79,540) $4,386 (78,619)
'mean cost per patient in category: ER admission cost greater than non-ER admission cost.
**sample size.
TABLE 3-Proportion of Matched Admissions Where Cost per ER Ad- By injecting economic risk into the health care market-
mission Exceeds That of Non-ER Admission and Percentage place, the public policy forces that promoted the DRG
of DRG Consistency According to Hospital system may have fostered research that can be used to
Per Cent of Admissions in Per Cent of DRG
improve efficiency.6 Research can also lead to more equita-
Category ER Cost Consistency Period ble reimbursement. The implications of this study need to be
Hospital Greater Non-ER Cost 1-Period 2** further defined by clinical specialty; and the factors that may
produce these higher cost ER admissions need to be more
A 79.8 (+0.75)* 85.2 (23) precisely defined. Thus incentives may be provided for
B 70.4 (-0.04) 62.9 (44) hospitals to negotiate subsidies for the higher costs of ER
C 86.6 (+1.33) 48.8 (40) admissions.
D 62.0 (-0.75) 53.6 (37)
E 64.2 (-0.57) 45.5 (35)
F 58.9 (-1.01) 50.0 (30)
G 87.7 (+1.42) 57.7 (30) ACKNOWLEDGMENTS
H 52.7 (-1.54) 27.8 (20) The authors wish to acknowledge the support of this project by the New
63.4 (-0.64) 57.7 (30) York City Health and Hospitals Corporation, Division of Management
J 82.6 (+1.02) 64.7 (97) Information Systems, Finance, Case-Mix Management, and Reimbursement
K 71.9 (+0.08) 51.5 (53) Planning.
Mean for All Hospitals 70.9% (0) 53.5%
REFERENCES
*difference from the mean of the population (expressed as + standard deviations). I. Mufhoz E, Tinker MA, Margolis I, Wise L: Surgonomics: the cost of
-number of DRGs consistent from period 1-period 2. cholecystectomy. Surgery 1984; 96:642-646.
2. Mudioz E, Regan D, Margolis IB, Wise L: Surgonomics: the identifier
concept: hospital charges in general surgery and surgical specialties under
PPS. Ann Surg 1985; 302:119-125.
The findings raise the question of whether the DRG 3. Mufloz E, Laughlin A, Regan D, Teicher I, Margolis IB, Wise L: The
system adequately compensates hospitals for emergency financial effects of emergency room generated admissions under PPS.
JAMA 1985; 254:1763-1771.
room generated admissions. The effect of higher cost ER 4. Mufioz E, Laughlin A, Regan D, Margolis IB, Wise L: Surgonomics: the
admissions will be to make this population "financially" financial effect of emergency room generated general surgical admissions
unattractive to hospitals; the 6,000 non-federal acute care and factors affecting cost variance under PPS. Am J Surg.
hospitals may be motivated to redirect ("dump") these 5. Omenn GS, Conrad DA: Sounding Board: Implications of DRGs for
Clinicians. N Engi J Med 1984; 311:1314-1317.
patients. Public hospitals may be more vulnerable to "dump- 6. Inglehart JD: Medicare begins prospective payment of hospitals. N Engl J
ing" than voluntary or for-profit institutions.5 Med 1983; 308:1428-1432.
AJPH June 1986, Vol. 76, No. 6 697
You might also like
- (Oxford Chemistry Primers, 02) David T. Davies - Aromatic Heterocyclic Chemistry (1992, Oxford University Press)Document92 pages(Oxford Chemistry Primers, 02) David T. Davies - Aromatic Heterocyclic Chemistry (1992, Oxford University Press)Awad SaidNo ratings yet
- Brand Positioning The Battle of The Mind: Mccormick vs. FuchsDocument12 pagesBrand Positioning The Battle of The Mind: Mccormick vs. FuchsLaura Mng100% (1)
- More Than 2000 Solved MCQs On Research MethodsDocument127 pagesMore Than 2000 Solved MCQs On Research MethodsBhushan Chaudhari100% (2)
- The Current Relationship Between Surgeon ReimburseDocument4 pagesThe Current Relationship Between Surgeon ReimburseRenan Scalon MachadoNo ratings yet
- Cost Analysis of An Intensive Care UnitDocument7 pagesCost Analysis of An Intensive Care UnitSabrina JonesNo ratings yet
- Circinterventions 120 010228Document3 pagesCircinterventions 120 010228Klinik Bhina Mitra SetyaNo ratings yet
- Estimating The Costs of Hospital Acquired InfectionDocument19 pagesEstimating The Costs of Hospital Acquired InfectionMatthew KuenzelNo ratings yet
- Jamasurgery Childers 2018 Oi 170128Document7 pagesJamasurgery Childers 2018 Oi 170128loloNo ratings yet
- The Costs of Nosocomial InfectionsDocument4 pagesThe Costs of Nosocomial InfectionsCandra BumiNo ratings yet
- An Analysis of Hospital Costs by Cost Center, 1971 Through 1978Document17 pagesAn Analysis of Hospital Costs by Cost Center, 1971 Through 1978YantoNo ratings yet
- Conditions With The Largest Number of Adult Hospital Readmissions by Payer, 2011Document10 pagesConditions With The Largest Number of Adult Hospital Readmissions by Payer, 2011David HarlowNo ratings yet
- Custo Efetividade Monitorizacao - 1Document8 pagesCusto Efetividade Monitorizacao - 1André Almeida e SilvaNo ratings yet
- 8 BaruDocument4 pages8 BaruAnditha Namira RSNo ratings yet
- The Costs of Intensive 2006 Continuing Education in Anaesthesia Critical CADocument4 pagesThe Costs of Intensive 2006 Continuing Education in Anaesthesia Critical CAronaldquezada038No ratings yet
- Proposal Defence Presentation PDFDocument25 pagesProposal Defence Presentation PDFbayu priyatnaNo ratings yet
- 1 s2.0 S1083879120305735 MainDocument3 pages1 s2.0 S1083879120305735 MainCommon JaiswalNo ratings yet
- 18 - Blood Cross-Match Ordering PracticesDocument3 pages18 - Blood Cross-Match Ordering PracticesKamran FarooquiNo ratings yet
- 01 - Cost of AKIDocument7 pages01 - Cost of AKIFloridalma FajardoNo ratings yet
- Direct Medical Costs of Hospitalized Patients With.16Document3 pagesDirect Medical Costs of Hospitalized Patients With.16jai.kumar.maingiNo ratings yet
- Prognosis Pneumonia PDFDocument18 pagesPrognosis Pneumonia PDFamania jeumpa nur alamNo ratings yet
- BEST Kidney StudyDocument10 pagesBEST Kidney StudyJoseph Zenas JungNo ratings yet
- Factors Affecting ED Length-of-Stay in Surgical Critical Care PatientsDocument6 pagesFactors Affecting ED Length-of-Stay in Surgical Critical Care PatientsMuhammad HidayantoNo ratings yet
- New Estimates of Elasticity of Demand For Healthcare in Rural China 2011 0Document11 pagesNew Estimates of Elasticity of Demand For Healthcare in Rural China 2011 0wangxinfeng1998No ratings yet
- Emergency Medicine Resident Efficiency and Emergency Department CrowdingDocument9 pagesEmergency Medicine Resident Efficiency and Emergency Department CrowdingRenzo Iván Marín DávalosNo ratings yet
- Journal Pone 0247042Document9 pagesJournal Pone 0247042irenzdcruzzNo ratings yet
- The Overall Percentage of The Elderly Living in Nursing Homes Is 5%Document21 pagesThe Overall Percentage of The Elderly Living in Nursing Homes Is 5%Kelly FitzgeraldNo ratings yet
- The Direct Medical Costs Of: Healthcare-Associated Infections in U.S. Hospitals and The Benefits of PreventionDocument16 pagesThe Direct Medical Costs Of: Healthcare-Associated Infections in U.S. Hospitals and The Benefits of PreventionjnplnceNo ratings yet
- The Impact of Hospital Safety-Net Burden On Mortality and Readmission After CABG SurgeryDocument10 pagesThe Impact of Hospital Safety-Net Burden On Mortality and Readmission After CABG SurgerymartarguezNo ratings yet
- A High-Volume Specialist Palliative Care Unit and Team May Reduce In-Hospital End-of-Life Care CostsDocument8 pagesA High-Volume Specialist Palliative Care Unit and Team May Reduce In-Hospital End-of-Life Care CostsNurbaiti Indah LestariNo ratings yet
- Emergency Referrals PDFDocument8 pagesEmergency Referrals PDFEngidaNo ratings yet
- Administration of Emergency MedicineDocument9 pagesAdministration of Emergency MedicineNurul AidaNo ratings yet
- J Jacc 2012 07 017Document6 pagesJ Jacc 2012 07 017Andi Tiara S. AdamNo ratings yet
- J Jacc 2012 07 017Document6 pagesJ Jacc 2012 07 017Andi Tiara S. AdamNo ratings yet
- J Jacc 2012 07 017Document6 pagesJ Jacc 2012 07 017Andi Tiara S. AdamNo ratings yet
- Nurse Staffing and Inpatient Hospital Mortality: Special ArticleDocument9 pagesNurse Staffing and Inpatient Hospital Mortality: Special ArticlemourienNo ratings yet
- Burden of Illness For Osteoporotic Fractures Compared With Other Serious Diseases Among Postmenopausal Women in The United StatesDocument10 pagesBurden of Illness For Osteoporotic Fractures Compared With Other Serious Diseases Among Postmenopausal Women in The United StatesSharan SahotaNo ratings yet
- RLE Journal ArticleDocument9 pagesRLE Journal ArticleMia MabaylanNo ratings yet
- 155778-Article Text-406683-1-10-20170509Document6 pages155778-Article Text-406683-1-10-20170509Tricia Jane OpinaldoNo ratings yet
- AbstractDocument36 pagesAbstractJackson MwaiNo ratings yet
- Costs of Hospital MalnutritionDocument6 pagesCosts of Hospital MalnutritionAmalia SarsolNo ratings yet
- quinn2015Document8 pagesquinn2015Familia En AcNo ratings yet
- Mission Hospital Case 11Document12 pagesMission Hospital Case 11Business Monkeys0% (1)
- Archive of SIDDocument5 pagesArchive of SIDSurya WijayaNo ratings yet
- The Effect of Burn Center Volume On Mortality in A Pediatric Population: An Analysis of The National Burn RepositoryDocument6 pagesThe Effect of Burn Center Volume On Mortality in A Pediatric Population: An Analysis of The National Burn Repositoryasmaa elnabawy1No ratings yet
- 1 s2.0 S2212109917300286 MainDocument8 pages1 s2.0 S2212109917300286 MainEya BaldostamonNo ratings yet
- Soi 130026Document7 pagesSoi 130026jose pablo reyes ortizNo ratings yet
- Soi 130026Document7 pagesSoi 130026jose pablo reyes ortizNo ratings yet
- Jurnal LainDocument22 pagesJurnal LainBudi ArsanaNo ratings yet
- Ambulatory Care Groups: A Categorization of Diagnoses For Research and ManagementDocument22 pagesAmbulatory Care Groups: A Categorization of Diagnoses For Research and ManagementbrskopjeNo ratings yet
- Diagnostic Related Groupings Saakat AddDocument46 pagesDiagnostic Related Groupings Saakat AddTheocryte SergeotNo ratings yet
- J Aem 2007 06 035Document8 pagesJ Aem 2007 06 035kingkinresmytaNo ratings yet
- Burden of Surgical Site Infections in The NetherlandsDocument10 pagesBurden of Surgical Site Infections in The NetherlandsKanokwan BorwornphiphattanachaiNo ratings yet
- 10 1001@jamaoncol 2019 0086Document8 pages10 1001@jamaoncol 2019 0086Akshay BadoreNo ratings yet
- Sacks - Variation in Hospital UseDocument9 pagesSacks - Variation in Hospital UseUm ShooqNo ratings yet
- The Preoperative Cost of Carpal Tunnel Syndrome: PurposeDocument11 pagesThe Preoperative Cost of Carpal Tunnel Syndrome: PurposeRonal Zumaeta PortocarreroNo ratings yet
- Migrain in The WorldDocument5 pagesMigrain in The WorldveNo ratings yet
- Hospital Overhead Costs: The Neglected Driver of Health Care Spending?Document15 pagesHospital Overhead Costs: The Neglected Driver of Health Care Spending?hasan najiNo ratings yet
- FRBSF: Conomic EtterDocument5 pagesFRBSF: Conomic EttermamuyaNo ratings yet
- Risk Factors For Falls in Hospital In-Patients: A Prospective Nested Case Control StudyDocument7 pagesRisk Factors For Falls in Hospital In-Patients: A Prospective Nested Case Control StudyNurhasanah HaryaniNo ratings yet
- CMA AntibioticsDocument11 pagesCMA AntibioticsNovita Oktavianti DehiNo ratings yet
- Burden AF With Ischemic StrokeDocument8 pagesBurden AF With Ischemic StrokeWirawan PrabowoNo ratings yet
- The Potential For Cost Savings Through Bundled Episode PaymentsDocument3 pagesThe Potential For Cost Savings Through Bundled Episode PaymentsGeorge L. YerkesNo ratings yet
- Model by Brandon Build by LuisDocument16 pagesModel by Brandon Build by LuisixosotocNo ratings yet
- Project ProposalDocument4 pagesProject ProposalQueenie Diane MontañoNo ratings yet
- GL Period CloseDocument12 pagesGL Period CloseMd MuzaffarNo ratings yet
- .. Thesis Title .Document31 pages.. Thesis Title .Tanut VongsoontornNo ratings yet
- KEM Epoxy Grout ELV - 1Document2 pagesKEM Epoxy Grout ELV - 1BinodNo ratings yet
- KADIMP Book Email 2Document116 pagesKADIMP Book Email 2ZINART MUSANo ratings yet
- WS Emergency Echo SYMCARD 2022Document33 pagesWS Emergency Echo SYMCARD 2022IndRa KaBhuomNo ratings yet
- The Present Perfect and The Present Perfect Continuous: Finished and Unfinished ActionsDocument26 pagesThe Present Perfect and The Present Perfect Continuous: Finished and Unfinished ActionsyahiaouimalekNo ratings yet
- Types of CurriculumDocument3 pagesTypes of CurriculumBabylyn Frias100% (1)
- DBA CockpitDocument337 pagesDBA Cockpithimanshu.singh0011282No ratings yet
- Circular - HBSU UG Admission, 2023-24Document2 pagesCircular - HBSU UG Admission, 2023-24Shyam GaikwadNo ratings yet
- SCF 020 - Ship Shore Safety ChecklistDocument8 pagesSCF 020 - Ship Shore Safety ChecklistSutarmoNo ratings yet
- Play Format ExampleDocument3 pagesPlay Format ExamplemegbenignoNo ratings yet
- C32 - PFRS 5 Noncurrent Asset Held For SaleDocument4 pagesC32 - PFRS 5 Noncurrent Asset Held For SaleAllaine ElfaNo ratings yet
- Compaction Trends Shale CleanSands Gulf of MexicoDocument8 pagesCompaction Trends Shale CleanSands Gulf of MexicoAfonso ElvaNo ratings yet
- Ee Monthly Price Plans: Your Plan Terms & Price Guide Available From 10 May 2017Document10 pagesEe Monthly Price Plans: Your Plan Terms & Price Guide Available From 10 May 2017Ana ModyNo ratings yet
- Wget - Curl Large File From Google Drive - Stack OverflowDocument29 pagesWget - Curl Large File From Google Drive - Stack OverflowManoj KamisettiNo ratings yet
- SB19 Water-KomprimiertDocument101 pagesSB19 Water-KomprimiertNatasa KakesNo ratings yet
- ZTE LTE FDD Clock Synchronization Feature GuideDocument103 pagesZTE LTE FDD Clock Synchronization Feature Guidem2adeelNo ratings yet
- Inaccuracies in Manometric Central Venous Pressure MeasurementDocument10 pagesInaccuracies in Manometric Central Venous Pressure MeasurementmfhfhfNo ratings yet
- Sf4 ConceptDocument10 pagesSf4 ConceptAndrás FarkasNo ratings yet
- Sip Design and Verification Using AdsDocument34 pagesSip Design and Verification Using AdsMaria Lavinia IordacheNo ratings yet
- MYY&MZZ Manual Transmission (Ver4)Document32 pagesMYY&MZZ Manual Transmission (Ver4)Vahid Reza MohammadiNo ratings yet
- Art NouveauDocument73 pagesArt NouveauRuqayya AhmedNo ratings yet
- WA-LD-45 PPP For New Direction PAC (March 2017)Document2 pagesWA-LD-45 PPP For New Direction PAC (March 2017)Daily Kos ElectionsNo ratings yet
- SNGPL - Web BillDocument1 pageSNGPL - Web BillNazeer Ahmed100% (1)
- Mathematics 3Document2 pagesMathematics 3Tony StarkNo ratings yet