Professional Documents
Culture Documents
Obesity Is A Disease Infographic
Obesity Is A Disease Infographic
Uploaded by
Franco PacelloOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Obesity Is A Disease Infographic
Obesity Is A Disease Infographic
Uploaded by
Franco PacelloCopyright:
Available Formats
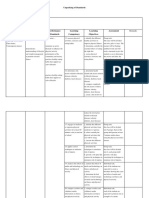
OBESITY IS A DISEASE
Dysregulated Energy Balance Factors Contributing to The
A BMI of ≥30 kg/m2 is consistent is Central to Obesity3,4 Development of Obesity4
Obesity has been defined as “a with a diagnosis of obesity
chronic, progressive, relapsing, and Food Intake: Food intake may be affected by
treatable multi-factorial, Obesity is categorized into 3 sociocultural determinants of health (e.g., social
and community factors, economic and educational
neurobehavioral disease, wherein classes1: factors, the food environment or access to healthy
food), mental health, hunger and satiety signaling,
an increase in body fat promotes Class I Obesity: 30.0-34.9 kg/m2 sleep, and medical conditions or medications that
impact food intake4
adipose tissue dysfunction and Class II Obesity: 35.0-39.9 kg/m2
abnormal fat mass physical forces, Class III Obesity: ≥40.0 kg/m2 Energy Expenditure: Affected by age, sex,
genetic/epigenetic factors, neuroendocrine factors,
resulting in adverse metabolic, The complex biological systems
body composition, medications affecting metabolic
rate, the thermic effect of food, and amount and
biomechanical, and psychosocial that regulate energy balance are
activity of brown adipose tissue (BAT)4
health consequences”1 believed to be disrupted in
Physical activity: May be influenced by social
determinants of health, physical limitations, chronic
people with obesity2 medical conditions, medications, or emotional
barriers4
Multiple Environmental Factors Contribute to Altered Energy Balance5 Pathogenesis of Obesity6
Adipocyte
Energy Expenditure Hypertrophy
MACROENVIRONMENT MICROENVIRONMENT INTERNAL ENVIRONMENT
Weight-promoting FFA release
Food environment medications Energy balance Proinflammatory cytokines
Altered secretion of adipokines
regulation
Eating Energy Storage
Built environment
Genetic CNS
Activity predisposition Energy Energy Ectopic fat deposition
Intake Expenditure
Air pollution and developmental
Sleep and epigenetic
influences
Regulated by the Central Nervous System
Endocrine disruptors Circadian
rhythm
Social cues/norms Depression Obesity Adipocyte
Hyperplasia
Energy Intake
Complications of Obesity
MASLD
Obstructive Heart Type 2 Reduced Gallbladder
Stroke7 Dyslipidemia9 Hypertension10 Gout14 Osteoarthritis15 (formerly known Cancer19 Asthma20
Sleep Apnea8 Disease11 Diabetes12 Fertility13 Disease16 as NAFLD)17,18
Complex Pathophysiology of Obesity Leads to a Variety of Diseases21 Physiological Changes Occurring Due to Obesity6,22,23
Dysregulation of CNS-
SNS Activity Insulin
endocrine signals
Obesogenic Changes of
Factors gut microbiota
MULTISYSTEM
DISEASES Androstenedione
Altered secretion of Total/free
adipokines Leptin
testosterone in men
Endocrine Chemerin
SHBG
Neurological
Adipocytes undergo Adiponectin
Proinflammatory Ectopic fat Local and systemic inflammation
apoptosis, necrosis,
cytokines deposition and insulin resistance Respiratory Omentin Total/Free testosterone
and fibrosis in women
Gastrointestinal
Kisspeptin
Cardiovascular
Increase of triglyceride
and FFA levels Autoimmune
Positive Infectious
Energy SNS activation Reproductive Growth Proinflammatory
Balance Hormone Cytokines
Malignancy
Size increases in organs
and tissues Weight reduction triggers: Increased ghrelin Decreased leptin and insulin Decreased GLP-1, PYY3-36, CCK, and amylin
Barriers in the Management of Obesity
100
87.5
Weight Regained (%) 2
75
62.5
50
37.5
25
12.5
0
1 2 3 4 5
Time After Weight Loss (years)
Gaps in Obesity Lack of Access
Lack of Time Ability to Metabolic Changes With
Education and Weight Bias and to Specialized Ability to Access Access to
Biological barriers 24
During Office Participate in Weight Loss Which Favor
Training for Stigma26 Obesity Clinical Care29 Healthy Foods30
Visits27 Healthcare28 Physical Activity31 Weight Regain32
Clinicians25
Abbreviations and References
BAT=Brown Adipose Tissue; BMI=Body Mass Index; CCK=Cholecystokinin; CNS=Central Nervous System; FFA=Free Fatty Acid; GI=Gastrointestinal; GLP-1=Glucagon-Like Peptide-1; LH=Luteinizing Hormone; MASLD=Metabolic
Dysfunction-Associated Steatotic Liver Disease; NAFLD=Non-Alcoholic Fatty Liver Disease; PYY3-36=Peptide YY3-36; SHBG=Sex Hormone-Binding Globulin; SNS=Sympathetic Nervous System; TSH=Thyroid Stimulating Hormone.
1. https://obesitymedicine.org/definition-of-obesity/ (Accessed September 05, 2023). 2. Spiegelman BM, Flier JS. Cell. 2001;104(4):531-543. 3. Morton GJ, et al. Nat Rev Neurosci. 2014;15(6):367–378. 4. Sharma AM, Padwal R. Obes Rev. 2010;11(5):362-70.
5. https://apps.who.int/iris/bitstream/handle/10665/353747/9789289057738-eng.pdf (Accessed September 05, 2023). 6. Jin X, et al. Acta Pharm Sin B. 2023;13(6):2403-2424. 7. Suk SH, et al. Stroke. 2003;34(7):1586-1592. 8. Senaratna CV, et al. Sleep Med Rev.
2017;34:70-81. 9. Howard BV, et al. Endocrinol Metab Clin North Am. 2003;32(4):855-867. 10. Mokdad AH, et al. JAMA. 2003;289(1):76-79. 11. Kenchaiah S, et al. N Engl J Med. 2002;347(5):305-313. 12. Schnurr TM, et al. Diabetologia. 2020;63(7):1324-1332. 13.
Silvestris E, et al. Reprod Biol Endocrinol. 2018;16(1):22. 14. Bai L, et al. Arthritis Res Ther. 2021;23(1):69. 15. King LK, et al. Indian J Med Res. 2013;138(2):185-193. 16. Stender S, et al. Hepatology. 2013;58(6):2133-2141. 17. Divella R, et al. Int J Biol Sci.
2019;15(3):610-616. 18. De A, et al. J Hepatol. 2023:S0168-8278(23)05044-4. 19. Calle EE, et al. N Engl J Med. 2003;348(17):1625-1638. 20. Peters U, et al. J Allergy Clin Immunol. 2018;141(4):1169-1179. 21. Gutiérrez-Cuevas J, et al. Int J Mol Sci. 2021.
27;22(21):11629. 22.Heymsfield SB, Wadden TA. N Engl J Med. 2017;376:254-66. 23. Ylli D, et al. South Dartmouth (MA): MDText.com, Inc.; 2000-. 2022. 24. Dent R, et al. Metabolism. 2020;113:154388. 25. Alexander SC, et al. Am J Health Promot. 2007;21(6):498-500.
26. Sabin JA, et al. PLoS One. 2012;7(11):e48448. 27. Butryn ML, et al. Psychiatr Clin North Am. 2011;34(4):841-859. 28. Washington TB, et al. Gastroenterol Clin North Am. 2023;52(2):429-441. 29. Kim TN. J Obes Metab Syndr. 2020;29(4):244-247. 30. Munt AE, et al.
Obes Rev. 2017;18(1):1-17. 31. Lee A, et al. South Dartmouth (MA): MDText.com, Inc.; 2000-. 2019. 32. Hall KD, Kahan S. Med Clin North Am. 2018;102(1):183-197.
VV-MED-146827 10/2023 © 2023 Lilly USA, LLC. All rights reserved.
You might also like
- Soma Devi InvoiceDocument1 pageSoma Devi InvoiceManeesh Verma100% (1)
- 17A. Immune ToleranceDocument8 pages17A. Immune ToleranceEssington BeloNo ratings yet
- Maxicare Application FormDocument3 pagesMaxicare Application Formbzkid82No ratings yet
- Craniomandibular Function and Dysfunction: Leaf GaugeDocument7 pagesCraniomandibular Function and Dysfunction: Leaf GaugeAkanksha MahajanNo ratings yet
- LP 1 - Nutritional AssessmentDocument11 pagesLP 1 - Nutritional AssessmentDacuma Rey JohnNo ratings yet
- Cues Nursing Diagnosis Analysis Goals and Objectives Intervention Rationale EvaluationDocument2 pagesCues Nursing Diagnosis Analysis Goals and Objectives Intervention Rationale EvaluationAllana RayosNo ratings yet
- 10.1038@s41575 020 0341 5Document18 pages10.1038@s41575 020 0341 5Noe CorreaNo ratings yet
- Unidad Educativa Luciano Andrade MarínDocument1 pageUnidad Educativa Luciano Andrade MarínMauricio NacionalNo ratings yet
- Principles of Nutritional AssesmentDocument6 pagesPrinciples of Nutritional AssesmentHendro Dan MithochanNo ratings yet
- UkdiDocument25 pagesUkdiAnna GozaliNo ratings yet
- ObesityDocument1 pageObesityJUAN CARLOS OJEDA-GARCESNo ratings yet
- Obesity in Adults, A Clinical Practice GuidelineDocument17 pagesObesity in Adults, A Clinical Practice GuidelineMari PaoNo ratings yet
- Obesity Final Draft-3Document5 pagesObesity Final Draft-3api-643535648No ratings yet
- Os Efeitos Modulatorios Do Treinamento Com Exercicios Sobre As Disfuncoes Imunometabolicas Induzidas Pela ObesidadeDocument26 pagesOs Efeitos Modulatorios Do Treinamento Com Exercicios Sobre As Disfuncoes Imunometabolicas Induzidas Pela ObesidadeAna Souza LimaNo ratings yet
- FCM3-3.07 National Nutrition ProgramDocument24 pagesFCM3-3.07 National Nutrition ProgramJoher MendezNo ratings yet
- Factors Affecting Nutritional Status of The ElderlyDocument2 pagesFactors Affecting Nutritional Status of The ElderlyYohannes DelesaNo ratings yet
- Pathogenesis of Obesity: Josanne VassalloDocument4 pagesPathogenesis of Obesity: Josanne VassalloAdkhiatul MuslihatinNo ratings yet
- Emotional and Intuitive Eating An Emerging Approach To Eating Behaviours Related To ObesityDocument7 pagesEmotional and Intuitive Eating An Emerging Approach To Eating Behaviours Related To ObesityferidecelebiNo ratings yet
- Effectiveness of Community Based Obesity.2Document7 pagesEffectiveness of Community Based Obesity.2mohamed allawyNo ratings yet
- Nutrients Micro and Macro Nutrients: Importance of Good NutritionDocument9 pagesNutrients Micro and Macro Nutrients: Importance of Good NutritionFRANCIS FRANCISCO. CLIMACONo ratings yet
- Is There A Place For Obesity in DSM-V?: Eating Disorder Not Otherwise SpecifiedDocument6 pagesIs There A Place For Obesity in DSM-V?: Eating Disorder Not Otherwise SpecifiedDiego Vargas SotoNo ratings yet
- Nutrição Moderna de Shils Na Saúde E Na Doença 11 Ed PDFDocument16 pagesNutrição Moderna de Shils Na Saúde E Na Doença 11 Ed PDFnnbfgwnrhbNo ratings yet
- CPHMLS Lec 02Document6 pagesCPHMLS Lec 02Jerlyn Francheska RodrinNo ratings yet
- Geriatrics Gerontology Int - 2023 - KuzuyaDocument13 pagesGeriatrics Gerontology Int - 2023 - Kuzuyamadiha ayubNo ratings yet
- Roles of The Gut Microbiome in Weight Management (Carmody y Bisanz, 2023)Document16 pagesRoles of The Gut Microbiome in Weight Management (Carmody y Bisanz, 2023)csrpirataNo ratings yet
- Fall 2022 CultivateDocument15 pagesFall 2022 CultivateFlorida Horticulture for Health NetworkNo ratings yet
- Nutrition and Diet Therapy ReviewerDocument10 pagesNutrition and Diet Therapy ReviewerNicole CastillaNo ratings yet
- Neuropharmacology of Compulsive Eating: ReviewDocument9 pagesNeuropharmacology of Compulsive Eating: ReviewIusti MariNo ratings yet
- NCPDocument5 pagesNCPJalishia Mae DumdumaNo ratings yet
- 1 PL Lect NCM105NDT IntroductionDocument2 pages1 PL Lect NCM105NDT IntroductionMa Ellen LumauagNo ratings yet
- Immune Health SeminarDocument27 pagesImmune Health SeminarNuuraine NasirNo ratings yet
- Eng 360 Obesity RevisedDocument5 pagesEng 360 Obesity Revisedapi-643535648No ratings yet
- Medical Nutrition TherapyDocument27 pagesMedical Nutrition TherapyClarke GriffinNo ratings yet
- Template For Care Plan AssignmentDocument8 pagesTemplate For Care Plan AssignmentAnn OgoloNo ratings yet
- A Comparative Study of Fucus Vesiculosus and Phytolacca Berry Mother Tincture in The Management of ObesityDocument6 pagesA Comparative Study of Fucus Vesiculosus and Phytolacca Berry Mother Tincture in The Management of Obesityayushsinghno1No ratings yet
- Nutrition and Diet Treatment PDFDocument12 pagesNutrition and Diet Treatment PDFMelvin B. TarkporNo ratings yet
- The Role of Energy Homeostasis in Human Health and DiseaseDocument1 pageThe Role of Energy Homeostasis in Human Health and Diseasesalma hanNo ratings yet
- Review 2018Document15 pagesReview 2018giulia.santinNo ratings yet
- Imbalance NutritionDocument4 pagesImbalance NutritionLeah Mae TomasNo ratings yet
- Lesson 0280Document12 pagesLesson 0280Abdikani MohamedNo ratings yet
- Recompensa e ObesidadeDocument9 pagesRecompensa e ObesidadefelipetheNo ratings yet
- European Journal of Theoretical and Applied SciencesDocument9 pagesEuropean Journal of Theoretical and Applied SciencesEJTAS journalNo ratings yet
- The Impact of Eating Behavior On Obesity in Northwestern Morocco Kenitra RegionDocument8 pagesThe Impact of Eating Behavior On Obesity in Northwestern Morocco Kenitra Regionelghouddany.safouaneNo ratings yet
- Health Education - Part 1Document27 pagesHealth Education - Part 1Ta dsNo ratings yet
- Unit 3Document12 pagesUnit 3devidayal9891050No ratings yet
- Dietary Regulation in Health and Disease: Signal Transduction and Targeted TherapyDocument29 pagesDietary Regulation in Health and Disease: Signal Transduction and Targeted Therapyserama15692uacNo ratings yet
- 1 s2.0 S147101531630201X Main PDFDocument7 pages1 s2.0 S147101531630201X Main PDFCristina MariaNo ratings yet
- IBS - Low-FODMAP Diet For Irritable Bowel Syndrome What We Know and What We Have Yet To LearnDocument14 pagesIBS - Low-FODMAP Diet For Irritable Bowel Syndrome What We Know and What We Have Yet To Learnqayyum consultantfpscNo ratings yet
- Tugas Kelompok 1Document17 pagesTugas Kelompok 1FrederickSuryaNo ratings yet
- Characterizing Eating Behavioral Phenotypes in Mood Disorders A Narrative ReviewDocument14 pagesCharacterizing Eating Behavioral Phenotypes in Mood Disorders A Narrative ReviewbssNo ratings yet
- Food Reward SystemDocument12 pagesFood Reward SystemCamilla MendesNo ratings yet
- Nutri LecDocument4 pagesNutri LecAltea PasiaNo ratings yet
- Binge-Eating Disorder-CircadianDocument6 pagesBinge-Eating Disorder-CircadianMafe CordobaNo ratings yet
- Assessing The Nutritional Status of The Elderly THDocument8 pagesAssessing The Nutritional Status of The Elderly THJohn Alfrey PuebloNo ratings yet
- Obesity A Review of Pathophysiology and Classific - 2023 - Mayo Clinic ProceediDocument16 pagesObesity A Review of Pathophysiology and Classific - 2023 - Mayo Clinic Proceedialerta.bfcmNo ratings yet
- Weight Stigma and Health Behaviors: Evidence From The Eating in America StudyDocument11 pagesWeight Stigma and Health Behaviors: Evidence From The Eating in America StudypedroNo ratings yet
- NCP Ovarian CancerDocument6 pagesNCP Ovarian Cancerwendy gaetosNo ratings yet
- Voruganti 2022 Precision Nutrition Recent Advances in ObesityDocument9 pagesVoruganti 2022 Precision Nutrition Recent Advances in Obesityletycia469No ratings yet
- 1 - IntroductionDocument5 pages1 - IntroductionLynnelljhyen MALUBAYNo ratings yet
- Unpacking Standards 2Document3 pagesUnpacking Standards 2api-399672613No ratings yet
- By: Siti Pariani, DR, MS, MSC, PH.D Depart Public Health and Preventive Medicine School of Medicine, Airlangga UniversityDocument17 pagesBy: Siti Pariani, DR, MS, MSC, PH.D Depart Public Health and Preventive Medicine School of Medicine, Airlangga UniversityIanMarvinGNo ratings yet
- Healthy Status and Energy Balance in Pediatrics: Acta Bio-Medica: Atenei Parmensis February 2006Document8 pagesHealthy Status and Energy Balance in Pediatrics: Acta Bio-Medica: Atenei Parmensis February 2006zahfira edwardNo ratings yet
- 6.2 Public HealthDocument4 pages6.2 Public HealthDahlia SuelloNo ratings yet
- Matrix of Nutrition: Macrobiotics and Nutritional ScienceFrom EverandMatrix of Nutrition: Macrobiotics and Nutritional ScienceNo ratings yet
- Nuclear CaseDocument106 pagesNuclear CaseAkramNo ratings yet
- Ossie Guide To Clinical Handover Improvement PDFDocument56 pagesOssie Guide To Clinical Handover Improvement PDFHendra SetiawanNo ratings yet
- M.Sc. MEDICAL LABORATORY TECHNOLOGYDocument23 pagesM.Sc. MEDICAL LABORATORY TECHNOLOGYTanisha ShaikhNo ratings yet
- 2017 OL Biomolecule REVIEWDocument5 pages2017 OL Biomolecule REVIEWIan ZeigerNo ratings yet
- Hyperosmolar Hyperglycemic StateDocument8 pagesHyperosmolar Hyperglycemic StateEsra AljafferNo ratings yet
- World Health DayDocument2 pagesWorld Health DaySahilNo ratings yet
- Tooth Vs Tooth Tissue Supported RPDDocument47 pagesTooth Vs Tooth Tissue Supported RPDDr Pooja KiranNo ratings yet
- Đề Chính Thức Môn: Tiếng AnhDocument8 pagesĐề Chính Thức Môn: Tiếng AnhHuỳnh Thái Uyên Phương100% (1)
- Alcon 2012 Infiniti Cataract and Refractive Surgery Brochure 83 Pages PDFDocument83 pagesAlcon 2012 Infiniti Cataract and Refractive Surgery Brochure 83 Pages PDFcwsalespro100% (1)
- World Mental Health Day by Gaurav RawatDocument3 pagesWorld Mental Health Day by Gaurav RawatGaurav RawatNo ratings yet
- Paranoid Disorders QuizDocument5 pagesParanoid Disorders QuizmalindaNo ratings yet
- Croc Bloc Sunscreen SPF30+50Document5 pagesCroc Bloc Sunscreen SPF30+50PubcrawlNo ratings yet
- Sterilization and DisinfectionDocument9 pagesSterilization and DisinfectionFrances Lau Yee ChinNo ratings yet
- Apixaban 5 PDFDocument2 pagesApixaban 5 PDFWanie Al-basriNo ratings yet
- Views: From The ArchivesDocument1 pageViews: From The ArchivesĐỗ Viết Hà TXA2HNNo ratings yet
- Jiaci Supl - Conjuntivitis-AlergicaDocument24 pagesJiaci Supl - Conjuntivitis-AlergicaNADIANo ratings yet
- ROSABIA, Micaela Pauline J. .-BSN-2A-ISDH-GS-NURSERY-NCPDocument6 pagesROSABIA, Micaela Pauline J. .-BSN-2A-ISDH-GS-NURSERY-NCPkimberly quitonNo ratings yet
- English Remidial/Enrichment: Nama: Aisi Kurniasari Kelas: 12 Tata Busana 3 No. Absen: 01Document8 pagesEnglish Remidial/Enrichment: Nama: Aisi Kurniasari Kelas: 12 Tata Busana 3 No. Absen: 01Tlebeng AstreaNo ratings yet
- Potter: Fundamentals of Nursing, 9th Edition: Chapter 40: Hygiene Answer Key - Review Questions and RationalesDocument3 pagesPotter: Fundamentals of Nursing, 9th Edition: Chapter 40: Hygiene Answer Key - Review Questions and RationalesStaceyNo ratings yet
- Ducoux-Respiration and DigestionDocument9 pagesDucoux-Respiration and DigestionTito AlhoNo ratings yet
- 4th Periodical Mapeh Grade 7 Science PRINTDocument7 pages4th Periodical Mapeh Grade 7 Science PRINTjinky viernesNo ratings yet
- Report On Obsessive-Compulsive-Disorders-and-Trauma-related-DisordersDocument42 pagesReport On Obsessive-Compulsive-Disorders-and-Trauma-related-DisordersMatteo BayotNo ratings yet
- Docsbookstoreacsapac2022b1 Sample PDFDocument30 pagesDocsbookstoreacsapac2022b1 Sample PDFFaheem Mahmood ButtNo ratings yet
- 1 PBDocument7 pages1 PBHigherNo ratings yet
- (Imp) Ras, Basmas Constipation, Draksharishta, Sukhavirechanavati, Swarnakravyadarasa, TriphalachurnaDocument10 pages(Imp) Ras, Basmas Constipation, Draksharishta, Sukhavirechanavati, Swarnakravyadarasa, TriphalachurnaPraveen KumarNo ratings yet
- 1-7 Theorists (THEORY MATRIX)Document16 pages1-7 Theorists (THEORY MATRIX)Princess OlarteNo ratings yet