Professional Documents
Culture Documents
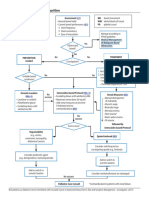
Constipation Treatment Algorithm For Primary Care Management of Chronic Constipation in Adults
Constipation Treatment Algorithm For Primary Care Management of Chronic Constipation in Adults
Uploaded by
Ruth ROriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Constipation Treatment Algorithm For Primary Care Management of Chronic Constipation in Adults
Constipation Treatment Algorithm For Primary Care Management of Chronic Constipation in Adults
Uploaded by
Ruth RCopyright:
Available Formats
Treatment Algorithm for Primary Care Management of Chronic Constipation in Adults
Patient reports or is reported with constipation – patients should have 2 or more of the following features for at least 12 weeks:- <3 bowel movements a week, straining, hard lumpy stool,
sensation of incomplete evacuation, sensation of ano-rectal blockage or digital evacuation more than 25% of bowel movements
1. Identify contributory factors to constipation by carrying out relevant medical history, general examination, If due to opioid therapy (review in line with opioid use): First
abdominal examination, digital rectal examination, review medication, neurological and cognitive assessment line treatment: Senna 2-4 tablets twice daily plus sodium
2. As appropriate assess and treat any suspected clinical problems such as faecal impaction, drug related, docusate 100mg twice daily
haemorrhoids, fissures
3. If acute constipation for less than 3 months with no change in lifestyle, consider red flag signs such as fresh blood If in-effective, for palliative care patients only; co-
mixed in stool, unintentional weight loss, lethargy, anaemia and family history of bowel cancer refer on to danthramer capsules 1-4 twice daily or co-danthramer liquid
colorectal consultant for suspected colon cancer 10-20mls twice daily. Co-danthramer Forte 1-4 capsules (or
4. Provide lifestyle advice based on findings from baseline assessment e.g. bowel education syrup) twice daily (only to be used with persistent
5. Patient education: constipation)
a. Correct toilet positioning,
b. Modify bowel habit – regular toileting about 30 minutes after a meal, Inadequate response in 4 days:
c. Modify diet by possibly increasing or decreasing fibre, 5 fruit and vegetables a day and fluid intake 1 ½ Second Line treatment: Naloxegol (Moventig®) NICE TA345
litres mixed fluid 25mg once daily (or 12.5mg for people with renal
d. Exercise insufficiency)
If drug therapy necessary
First Choice: Bulking Agents – Ispaghula husk, methylcellulose (Onset of effect 12-72 hours)
Dose: Ispaghula Husk 3.5g sachet (Fybogel®) 1 sachet twice daily
Methylcellulose ‘450’500mg (Celevac®) 3-6 tablets twice daily
Adverse effects: Gas, bloating, oesophageal obstruction, colonic obstruction, calcium and iron malabsorption
Prescribing Considerations:
Must be mixed with water and taken as a drink as soon as prepared.
Additional fluid should be drunk throughout the day. (May not be suitable for frail elderly people). Methylcellulose avoid liquid intake for 30 mins before and after dose
Not to be taken before going to bed in order to reduce the risk of obstruction. May reduce appetite
Author: Philippa Blatchford, Prescribing Advisor, Croydon CCG
Approved by: Croydon Prescribing Committee Date: 13.11.15
Review date: January 2018
Second Choice: Osmotic laxative – Macrogol, lactulose (Onset of effect 24-48 Alternative Options:
hours) Stool softener – docusate sodium (Onset of effect 1-3 days)
Dose: Macrogol Oral Powder, Compound: 1-3 sachets daily Dose: Up to 500mg daily in divided doses
Lactulose: 15ml twice daily, adjusted to response Adverse Effects: Stomach, intestinal cramping,
Adverse Effects: nausea, vomiting, flatulence, cramps and abdominal discomfort
Stimulant laxative (Onset of effect 6-12 hours)
Prescribing Considerations: Senna: 2-4 tablets, usually at night (gradually increased)
Administer lactulose with either water or fruit juice, requires regular dosing. Bisacodyl: 5-10mg at night (increased to max 20mg)
Can lead to dehydration if inadequate fluid intake. Adverse Effects: Electrolyte imbalances (e.g. hypokalemia), abdominal discomfort
and cramp, potential for overuse/abuse
If at least two laxatives from different classes, at the highest tolerated recommended doses for at least 6 months, has failed to provide adequate relief and invasive treatment for
constipation is considered
Prucalopride (Resolor®) in women TA211 Lubiprostone (Amitiza®) NICE TA318
Dose: 2 mg once daily (up to 65 years old) and 1 mg once daily (over 65 years) Dose: 24microgrames twice daily
increased to 2 mg once daily if needed. SPC states that a course of treatment is 2 weeks
Review at 4 weeks: If not effective re-examine patient and reconsider the benefit Review at 2 weeks: If not effective re-examine patient and reconsider the benefit of
of continuing treatment continuing treatment
If normal bowel movements are established, review treatment at regular intervals If normal bowel movements are established, review treatment at regular intervals
every 3 months to assess clinical need. No repeat prescriptions >3months every 3 months to assess clinical need. No repeat prescriptions >3months
Adverse Effects: headache, abdominal pain, nausea or diarrhoea. Most frequently Adverse Effects: nausea, palpitations, diarrhoea, abdominal distension, flatulence,
reported at the start of treatment abdominal discomfort/pain, indigestion, oedema, chest discomfort, headache,
dizziness, dyspnoea, hyperhidrosis and hot flushes.
If no improvement consider referral
Author: Philippa Blatchford, Prescribing Advisor, Croydon CCG
Approved by: Croydon Prescribing Committee Date: 13.11.15
Review date: January 2018
You might also like
- Research Paper G-10 ST - John (New)Document66 pagesResearch Paper G-10 ST - John (New)Neil Patrick Lajera CruzNo ratings yet
- Colace (Docusate Sodium)Document1 pageColace (Docusate Sodium)E100% (1)
- The Self Aware Universe How Consciousness Creates The Material World PDFDocument27 pagesThe Self Aware Universe How Consciousness Creates The Material World PDFtstnme3100% (2)
- 580 Hc107r O&mmanengDocument193 pages580 Hc107r O&mmanengMario Garcia67% (6)
- Archives of Practical Pediatrics 12Document5 pagesArchives of Practical Pediatrics 12Ashok jainNo ratings yet
- Drug Study (BISACODYL)Document1 pageDrug Study (BISACODYL)Angela Mae Cabajar83% (6)
- Naplex Complete Study Outline A Topic-Wise Approach DiabetesFrom EverandNaplex Complete Study Outline A Topic-Wise Approach DiabetesRating: 4 out of 5 stars4/5 (3)
- Tesla Coil ReportDocument15 pagesTesla Coil ReportPiyush Raj50% (2)
- Basics of ASP - NET-2Document3 pagesBasics of ASP - NET-2serachguruNo ratings yet
- Enalapril (Vasotec ®) :: Dosing (Adults)Document9 pagesEnalapril (Vasotec ®) :: Dosing (Adults)Ica Joy ArandiaNo ratings yet
- Nursing MedsDocument10 pagesNursing MedsBSN 2014No ratings yet
- Colchicine DosageDocument6 pagesColchicine DosageHam SotheaNo ratings yet
- Lec 7Document21 pagesLec 7Ahmed IsmaillNo ratings yet
- FiberCon (Polycarbophil)Document1 pageFiberCon (Polycarbophil)ENo ratings yet
- Race Cadot RilDocument4 pagesRace Cadot RilDaniela Claire FranciscoNo ratings yet
- Race Cadot RilDocument4 pagesRace Cadot RilAngie MandeoyaNo ratings yet
- Alprazolam (Systemic)Document14 pagesAlprazolam (Systemic)RIRINo ratings yet
- Guia de ConstipacionDocument5 pagesGuia de ConstipacionWalter Barriga ManriqueNo ratings yet
- Drug StudyDocument41 pagesDrug StudyCatherine PradoNo ratings yet
- Effect DoseDocument30 pagesEffect DoseXyprus Darina VeloriaNo ratings yet
- Brand Name Generic Indication Reaction/Precaution/Ed Ucation Dulcolax Bisacodyl ReactionDocument5 pagesBrand Name Generic Indication Reaction/Precaution/Ed Ucation Dulcolax Bisacodyl ReactionLouie George NeriNo ratings yet
- Constipation Formulary (Otago) : DiagnosisDocument4 pagesConstipation Formulary (Otago) : DiagnosisMiguel SanJuanNo ratings yet
- Tugas MedicineDocument2 pagesTugas MedicineRiza Ikhsan MuliaNo ratings yet
- Printed Material Module 7 Gastrointestinal System Drugs - PDFDocument45 pagesPrinted Material Module 7 Gastrointestinal System Drugs - PDFShang MacarayonNo ratings yet
- Gastrointestinal DrugsDocument45 pagesGastrointestinal DrugsCindy MaslagNo ratings yet
- Laxative Treatment Guideline For AdultsDocument7 pagesLaxative Treatment Guideline For AdultsPurim KTshipNo ratings yet
- Attapulgite PDFDocument1 pageAttapulgite PDFWindy Tonapa100% (1)
- GIT DrugsDocument180 pagesGIT DrugsMaria Linevel Balderamos Dalida100% (1)
- Drug Study RivastigmineDocument6 pagesDrug Study RivastigmineRaijenne VersolaNo ratings yet
- Primary Care Constipation Guidelines: Version 1.1 - December 2016Document5 pagesPrimary Care Constipation Guidelines: Version 1.1 - December 2016Budi WicaksonoNo ratings yet
- Drugs Used To Treat Digestive Problems: Classification: AntidiarrhealsDocument68 pagesDrugs Used To Treat Digestive Problems: Classification: AntidiarrhealsTom-tom LunaNo ratings yet
- Discharge Planning 2Document6 pagesDischarge Planning 2Jason MacatuggalNo ratings yet
- Omeprazole Drug StudyDocument4 pagesOmeprazole Drug StudyFeliza Therese A. DeloriaNo ratings yet
- Drug StudyDocument2 pagesDrug StudyXandra ArticuloNo ratings yet
- FamotidineDocument3 pagesFamotidineapi-3797941No ratings yet
- Pharmacologic Class: Proton Pump Therapeutic Class: Antiulcer Drug Pregnancy Risk Category CDocument8 pagesPharmacologic Class: Proton Pump Therapeutic Class: Antiulcer Drug Pregnancy Risk Category CjigokushinigamiaiNo ratings yet
- Metoclopramide: GIT Regulators, Antiflatulents & Anti-Inflammatories Antiemetics See Available Brands of MetoclopramideDocument9 pagesMetoclopramide: GIT Regulators, Antiflatulents & Anti-Inflammatories Antiemetics See Available Brands of MetoclopramideDominique RamosNo ratings yet
- Metoclopramide: GIT Regulators, Antiflatulents & Anti-Inflammatories Antiemetics See Available Brands of MetoclopramideDocument9 pagesMetoclopramide: GIT Regulators, Antiflatulents & Anti-Inflammatories Antiemetics See Available Brands of MetoclopramideDominique RamosNo ratings yet
- Drug LipitorDocument1 pageDrug LipitorSrkocherNo ratings yet
- Section Constipation - AutosavedDocument46 pagesSection Constipation - Autosavedahmedmls206No ratings yet
- Hormonal Therapy in DubDocument20 pagesHormonal Therapy in DubpreethiNo ratings yet
- OtcDocument9 pagesOtcChrissie100% (1)
- Rabeprazole SodiumDocument3 pagesRabeprazole Sodiumapi-37979410% (1)
- Drug Study ColestipolDocument3 pagesDrug Study ColestipolAbby AngNo ratings yet
- EzetimibeDocument3 pagesEzetimibeapi-3797941No ratings yet
- Ranitidine - 1aDocument5 pagesRanitidine - 1aRichard OonNo ratings yet
- Dulcolax Stool Softener Supp (Docusate Sodium)Document2 pagesDulcolax Stool Softener Supp (Docusate Sodium)ENo ratings yet
- Drug StudyDocument3 pagesDrug StudyJames Michael BalicocoNo ratings yet
- DulcolaxDocument1 pageDulcolaxKatie McPeekNo ratings yet
- Ditropan Drug CardDocument2 pagesDitropan Drug CardBenNo ratings yet
- Handout Therapy Increased Intestinal Permeability ClinicianDocument2 pagesHandout Therapy Increased Intestinal Permeability ClinicianThe Machi WellnessNo ratings yet
- Drug StudyDocument13 pagesDrug StudyClarkEstacioNo ratings yet
- Fluoxetine Hydro ChlorideDocument3 pagesFluoxetine Hydro Chlorideapi-3797941No ratings yet
- Bowel Care - Constipation (Algorithm)Document2 pagesBowel Care - Constipation (Algorithm)Fayruz Zahrotin NiswahNo ratings yet
- 01 2015 GI Agents - Lubiprostone (Amitiza)Document6 pages01 2015 GI Agents - Lubiprostone (Amitiza)modayearNo ratings yet
- Nausea and Vomiting (Algorithm) PDFDocument2 pagesNausea and Vomiting (Algorithm) PDFAnggie Anggriyana0% (1)
- Bikash Kumar Sah 2 Semester PucmasDocument22 pagesBikash Kumar Sah 2 Semester PucmasBikash SahNo ratings yet
- Magnesium SulfateDocument6 pagesMagnesium SulfatePrincess Alane MorenoNo ratings yet
- Diclofenac Sodium & Omeprazole Drug StudyDocument3 pagesDiclofenac Sodium & Omeprazole Drug StudyMelah MunchlaxNo ratings yet
- Medications: Medication Name Generic/Trade Classification Pregnancy CategoryDocument8 pagesMedications: Medication Name Generic/Trade Classification Pregnancy CategoryapalestiNo ratings yet
- Operation UeueueueDocument210 pagesOperation UeueueueBSRT1A BERBANO, IAN JEWEL M.No ratings yet
- Dulcolax Stool SoftenerDocument1 pageDulcolax Stool SoftenerSheri490No ratings yet
- Peptic Ulcer Disease DrugsDocument6 pagesPeptic Ulcer Disease DrugsApple MaeNo ratings yet
- Drug Study: History: Hypersensitivity To Any Xanthine or ToDocument2 pagesDrug Study: History: Hypersensitivity To Any Xanthine or ToJean De Vera MelendezNo ratings yet
- AminophyllineDocument6 pagesAminophyllineapi-3797941100% (1)
- Valproic Acid. 2023. RahmanDocument13 pagesValproic Acid. 2023. RahmanRuth RNo ratings yet
- SANAD II ValproateDocument12 pagesSANAD II ValproateveerrajuNo ratings yet
- Antiseizure Medication Withdrawal in Seizure-Free Patients Practice Advisory UpdateDocument73 pagesAntiseizure Medication Withdrawal in Seizure-Free Patients Practice Advisory UpdateRuth RNo ratings yet
- Summarizing The 2023 Chronic Idiopathic Constipation GuidelineDocument13 pagesSummarizing The 2023 Chronic Idiopathic Constipation GuidelineRuth RNo ratings yet
- CJGH2017 8612189Document11 pagesCJGH2017 8612189Ruth RNo ratings yet
- Palliative2 Constipation AlgorithmDocument1 pagePalliative2 Constipation AlgorithmRuth RNo ratings yet
- How To Restore Market Confidence in The NCM 150412Document7 pagesHow To Restore Market Confidence in The NCM 150412ProshareNo ratings yet
- A Comprehensive Review On Fresh State Rheological Properties of Extrusion Mortars Designed For 3D Printing ApplicationsDocument20 pagesA Comprehensive Review On Fresh State Rheological Properties of Extrusion Mortars Designed For 3D Printing ApplicationsAlfonzo SamudioNo ratings yet
- Collibra Prescriptive Path v2Document4 pagesCollibra Prescriptive Path v2AhamedSharifNo ratings yet
- What Is An IP AddressDocument4 pagesWhat Is An IP Addresschandvinay_singhNo ratings yet
- SAP Cloud For Sales Solution Brief - Sap LayoutDocument9 pagesSAP Cloud For Sales Solution Brief - Sap Layoutphogat projectNo ratings yet
- 6 SigmnaDocument15 pages6 SigmnaArjun SinghNo ratings yet
- SED 312 ISO Course Syllabus in Geology and AstronomyDocument6 pagesSED 312 ISO Course Syllabus in Geology and AstronomyRomel Christian Zamoranos MianoNo ratings yet
- Giao An Mon Tieng Anh 7 Hoc Ki 2Document95 pagesGiao An Mon Tieng Anh 7 Hoc Ki 2Vũ Nguyễn ĐứcNo ratings yet
- IT Sector Risk Assessment Report FinalDocument114 pagesIT Sector Risk Assessment Report FinalAdryana Enache100% (1)
- Source: Family Background:: Flight Mechanic World War II Oklahoma Dust BowlDocument4 pagesSource: Family Background:: Flight Mechanic World War II Oklahoma Dust BowlClay Cyril Jastiva LambitNo ratings yet
- J. AOAC Int. 2018, 101 (5), Pages 1566-1577Document12 pagesJ. AOAC Int. 2018, 101 (5), Pages 1566-1577Thanh Tâm TrầnNo ratings yet
- RECON-BRX-2017-Reverse Engineering Satellite Based IP Content DistributionDocument32 pagesRECON-BRX-2017-Reverse Engineering Satellite Based IP Content DistributionpaulNo ratings yet
- Calculo de TNT en Arco ElectricoDocument6 pagesCalculo de TNT en Arco ElectricoAdolfo EcheverriaNo ratings yet
- Lesson Plan Thanksgiving and HalloweenDocument2 pagesLesson Plan Thanksgiving and Halloweenapi-298974620No ratings yet
- Scale Up of KG Final Version of NarrativeDocument50 pagesScale Up of KG Final Version of NarrativeBenjamin AgyareNo ratings yet
- Banty DocumentsDocument82 pagesBanty DocumentsPandu TiruveedhulaNo ratings yet
- Unit 1 - Importance of Safe Drinking Water On health-SC PDFDocument35 pagesUnit 1 - Importance of Safe Drinking Water On health-SC PDFKhryzzia Maye Felicilda100% (1)
- Hubungan Indeks Massa Tubuh Dengan Siklus Menstruasi Pada Siswi SMP Wahid Hasyim Kota MalangDocument13 pagesHubungan Indeks Massa Tubuh Dengan Siklus Menstruasi Pada Siswi SMP Wahid Hasyim Kota MalangRoslince Umbu patiNo ratings yet
- Myanmar Community Security Cartoon Booklet EnglishDocument15 pagesMyanmar Community Security Cartoon Booklet EnglishSaw HsarNo ratings yet
- Addisonia Color Illustr and Popular Descriptions of Plants v05 1920Document109 pagesAddisonia Color Illustr and Popular Descriptions of Plants v05 1920Sitio KayapoNo ratings yet
- Sag-Cookery NC Ii PDFDocument6 pagesSag-Cookery NC Ii PDFArayaskillsdevt InstitutecorpNo ratings yet
- 4 Porifera Spicules & Canal SystemDocument34 pages4 Porifera Spicules & Canal Systemapi-3732735100% (2)
- Print Supple Admit Card - I-EMS - EUBDocument1 pagePrint Supple Admit Card - I-EMS - EUBMustak JuliatNo ratings yet
- From WID To GAD: Conceptual Shifts in The Women and Development DiscourseDocument57 pagesFrom WID To GAD: Conceptual Shifts in The Women and Development DiscourseUnited Nations Research Institute for Social DevelopmentNo ratings yet
- Guidelines and Formats For Capstone ProjectsDocument12 pagesGuidelines and Formats For Capstone ProjectsNikhil AggarwalNo ratings yet