Professional Documents
Culture Documents
Salter - Harris 2 Displaced Fractuers Best Treatment
Salter - Harris 2 Displaced Fractuers Best Treatment
Uploaded by
Deborah SalinasCopyright:
Available Formats
You might also like
- UdaipurDocument52 pagesUdaipurArun Kumar100% (2)
- Salter Harris II Fractures of The Distal Tibia Does Surgical Management Reduce The Risk of Premature Physeal ClosureDocument6 pagesSalter Harris II Fractures of The Distal Tibia Does Surgical Management Reduce The Risk of Premature Physeal ClosureDeborah SalinasNo ratings yet
- Treatment and Outcome of Diatl Tibia Saletr Harris II FracturesDocument6 pagesTreatment and Outcome of Diatl Tibia Saletr Harris II FracturesDeborah SalinasNo ratings yet
- Open Reduction and Internal Fixation For Displaced Salter Harris 2Document7 pagesOpen Reduction and Internal Fixation For Displaced Salter Harris 2Deborah SalinasNo ratings yet
- Surgical Treatment of Metastatic Tumors of The FemurDocument6 pagesSurgical Treatment of Metastatic Tumors of The FemurHitham El ShahatNo ratings yet
- HP 26 99Document8 pagesHP 26 99Juan PagesNo ratings yet
- Premature Physeal Closure Following Distal Tibia Physeal FracturesDocument7 pagesPremature Physeal Closure Following Distal Tibia Physeal FracturesDeborah SalinasNo ratings yet
- Clinical Analysis of The Frosch Approach in The Treatment of Posterolateral Tibial Plateau Fractures Combined With Lateral Tibial Plateau FracturesDocument11 pagesClinical Analysis of The Frosch Approach in The Treatment of Posterolateral Tibial Plateau Fractures Combined With Lateral Tibial Plateau FracturesraynaldidjohariofcNo ratings yet
- Conservative Versus Surgical Management of Intra-Articular Fractures of Distal End of Radius: A Comparative Clinical StudyDocument10 pagesConservative Versus Surgical Management of Intra-Articular Fractures of Distal End of Radius: A Comparative Clinical StudyAnonymous OJELaiw2No ratings yet
- Paper 1 Vinothkumar-1Document5 pagesPaper 1 Vinothkumar-1SK BONE & JOINT CARE DPINo ratings yet
- Brief Resume of Intended WorkDocument7 pagesBrief Resume of Intended WorkNavin ChandarNo ratings yet
- PFN PaperDocument7 pagesPFN PaperNisar Ahmed DarNo ratings yet
- 2019 Article 2632analisis TomograficoDocument6 pages2019 Article 2632analisis TomograficoLenin EstrellaNo ratings yet
- Fratura de UmeroDocument7 pagesFratura de UmerodanfisiofoxNo ratings yet
- Syndesmotic Screw Removed Verusus Retained: A Comparative Functional AnalysisDocument4 pagesSyndesmotic Screw Removed Verusus Retained: A Comparative Functional AnalysisSarath KumarNo ratings yet
- 97-506-1 Segundo CynDocument6 pages97-506-1 Segundo CynGalletita De JengibreNo ratings yet
- Jurnal PfnaDocument10 pagesJurnal PfnaDhea Amalia WibowoNo ratings yet
- Abstracts de Publicaciones Sobre Pilón TibialDocument15 pagesAbstracts de Publicaciones Sobre Pilón TibialAyler AguilarNo ratings yet
- A Study On Management of Bothbones Forearm Fractures With Dynamic Compression PlateDocument5 pagesA Study On Management of Bothbones Forearm Fractures With Dynamic Compression PlateIOSRjournalNo ratings yet
- Stabilization of Distal Humerus Fractures by Precontoured Bi-Condylar Plating in A 90-90 PatternDocument5 pagesStabilization of Distal Humerus Fractures by Precontoured Bi-Condylar Plating in A 90-90 PatternmayNo ratings yet
- Treatment of AO/OTA 31-A3 Intertrochanteric Femoral Fractures With A Percutaneous Compression PlateDocument7 pagesTreatment of AO/OTA 31-A3 Intertrochanteric Femoral Fractures With A Percutaneous Compression PlateNurul AiniNo ratings yet
- Surgical Treatment of Chronic Elbow Dislocation Allowing For Early Range of Motion: Operative Technique and Clinical ResultsDocument8 pagesSurgical Treatment of Chronic Elbow Dislocation Allowing For Early Range of Motion: Operative Technique and Clinical ResultsLuis Carlos HernandezNo ratings yet
- 1 s2.0 S1877056821003029 MainDocument21 pages1 s2.0 S1877056821003029 MainAndrea OsborneNo ratings yet
- Jurnal Fraktur Humerus DistalDocument5 pagesJurnal Fraktur Humerus DistalthisisangieNo ratings yet
- Prabhakar 2020Document9 pagesPrabhakar 2020Lucas LozaNo ratings yet
- Augmentation Plating Leaving The Nail in Situ Is An Excellent Option For Treating Femoral Shaft Nonunion After IM Nailing: A Multicentre StudyDocument7 pagesAugmentation Plating Leaving The Nail in Situ Is An Excellent Option For Treating Femoral Shaft Nonunion After IM Nailing: A Multicentre StudytomimacagnoNo ratings yet
- Tecnica de ChampyDocument7 pagesTecnica de Champyboye022694No ratings yet
- Sicotj160057 PDFDocument6 pagesSicotj160057 PDFDr'Dinesh MishraNo ratings yet
- Association of Pars Defect Type With Clinical Outcome After Smiley Face Rod Methods For Terminal-Stage SpondylolysisDocument8 pagesAssociation of Pars Defect Type With Clinical Outcome After Smiley Face Rod Methods For Terminal-Stage SpondylolysisUzm.Dr.Burhan ORAL GÜDÜNo ratings yet
- Tan2012 PDFDocument10 pagesTan2012 PDFdebyanditaNo ratings yet
- Arthroscopic Partial Trapeziectomy and Tendon Interposition For Thumb Carpometacarpal ArthritisDocument7 pagesArthroscopic Partial Trapeziectomy and Tendon Interposition For Thumb Carpometacarpal ArthritisJayNo ratings yet
- Chang 2017. Skeletal RadiologyDocument7 pagesChang 2017. Skeletal RadiologyteresaNo ratings yet
- Treatment Considerations For Comminuted Mandibular FracturesDocument10 pagesTreatment Considerations For Comminuted Mandibular FracturesAnonymous ENwjWryNo ratings yet
- Research ArticleDocument9 pagesResearch ArticleAni LabibahNo ratings yet
- Medi 97 E0523Document9 pagesMedi 97 E0523Andrea OsborneNo ratings yet
- 1 s2.0 S0901502716300728 MainDocument4 pages1 s2.0 S0901502716300728 MainCaio GonçalvesNo ratings yet
- Functional Outcome of Operative Management of Humeral Shaft FracturesDocument5 pagesFunctional Outcome of Operative Management of Humeral Shaft FracturesDr JunaidNo ratings yet
- Intertan Nail Vs PFN ADocument7 pagesIntertan Nail Vs PFN AzubayetarkoNo ratings yet
- Early and 1 Year Postsurgical Stability and Its Factors in Patients With Complicated Skeletal Class III Mal OcclusionDocument13 pagesEarly and 1 Year Postsurgical Stability and Its Factors in Patients With Complicated Skeletal Class III Mal Occlusionrana.hafezNo ratings yet
- Paper 38Document6 pagesPaper 38Dr Vineet KumarNo ratings yet
- Reisoğlu 2017Document5 pagesReisoğlu 2017Tuğçe KabakcıNo ratings yet
- Canulavos Vs Alambre K Fractura Patela 2020 ChinoDocument7 pagesCanulavos Vs Alambre K Fractura Patela 2020 ChinoGeraldine Alvarez ANo ratings yet
- Treatment of Periprosthetic Knee Fractures With Plate and Screws and With Retrograde Intramedullary Nail Indications Limits and Medium Term Follow UpDocument22 pagesTreatment of Periprosthetic Knee Fractures With Plate and Screws and With Retrograde Intramedullary Nail Indications Limits and Medium Term Follow UpAthenaeum Scientific PublishersNo ratings yet
- Percutaneous Screw Fixation of Crescent Fracture Dislocation of The Sacroiliac JointDocument7 pagesPercutaneous Screw Fixation of Crescent Fracture Dislocation of The Sacroiliac Jointgevowo3277No ratings yet
- Moderator:Dr Vijay Kumar Co-Moderator:Dr Venketish All India Institute of Medical Sciences New DelhiDocument58 pagesModerator:Dr Vijay Kumar Co-Moderator:Dr Venketish All India Institute of Medical Sciences New DelhiWasim R. IssaNo ratings yet
- Fraktur FrakDocument11 pagesFraktur FrakRirin SeptianiNo ratings yet
- Case Series of All-Arthroscopic Treatment For Terrible Triad of The Elbow: Indications and Clinical OutcomesDocument10 pagesCase Series of All-Arthroscopic Treatment For Terrible Triad of The Elbow: Indications and Clinical OutcomesdorfynatorNo ratings yet
- Percutaneous Pinning of Distal Radius Fractures Using Hematoma Block: Outcomes in Our CenterDocument3 pagesPercutaneous Pinning of Distal Radius Fractures Using Hematoma Block: Outcomes in Our CenterPeertechz Publications Inc.No ratings yet
- 2023 JOT Radiological and Long Term Functional Outcomes of Displaced Distal Clavicle FracturesDocument7 pages2023 JOT Radiological and Long Term Functional Outcomes of Displaced Distal Clavicle FracturesjcmarecauxlNo ratings yet
- Goyal 2012Document9 pagesGoyal 2012rahulNo ratings yet
- Claus 2019Document8 pagesClaus 2019abhishekjha0082No ratings yet
- Jurding Inggris RadiologiDocument7 pagesJurding Inggris RadiologiIrawaty Christin Marthyna SimanjuntakNo ratings yet
- Treatment of Tibial Plateau Fractures Dual Plating Dual IncisionDocument6 pagesTreatment of Tibial Plateau Fractures Dual Plating Dual IncisionAnnie JoNo ratings yet
- Fraktur KlavikulaDocument10 pagesFraktur KlavikulaEricsen T.P.No ratings yet
- Medip, IJORO-2331 ODocument7 pagesMedip, IJORO-2331 Oprashant makadiaNo ratings yet
- Type A1 Intertroch PFN VS DHS RetrospectiveDocument11 pagesType A1 Intertroch PFN VS DHS RetrospectiveMuhammad Tabish SaleemNo ratings yet
- Posterolateral Approach For Posterior Malleolus FiDocument12 pagesPosterolateral Approach For Posterior Malleolus FiorlanquisNo ratings yet
- Treatment Distal Radius Fracture With Volar Buttre PDFDocument5 pagesTreatment Distal Radius Fracture With Volar Buttre PDFZia Ur RehmanNo ratings yet
- Ekhtiari 2017Document9 pagesEkhtiari 2017QuiroprácticaParaTodosNo ratings yet
- Acetabular Fractures in Older Patients: Assessment and ManagementFrom EverandAcetabular Fractures in Older Patients: Assessment and ManagementTheodore T. MansonNo ratings yet
- Surgery of the Cranio-Vertebral JunctionFrom EverandSurgery of the Cranio-Vertebral JunctionEnrico TessitoreNo ratings yet
- Pi Is 0363502317301211Document8 pagesPi Is 0363502317301211Deborah SalinasNo ratings yet
- Outcome of Distal Tibial Physeal InjuriesDocument7 pagesOutcome of Distal Tibial Physeal InjuriesDeborah SalinasNo ratings yet
- Open Reduction and Internal Fixation For Displaced Salter Harris 2Document7 pagesOpen Reduction and Internal Fixation For Displaced Salter Harris 2Deborah SalinasNo ratings yet
- 10 1016@j Jhsa 2020 08 001Document8 pages10 1016@j Jhsa 2020 08 001Deborah SalinasNo ratings yet
- Salter Harris II Fractures of The Distal Tibia Does Surgical Management Reduce The Risk of Premature Physeal ClosureDocument6 pagesSalter Harris II Fractures of The Distal Tibia Does Surgical Management Reduce The Risk of Premature Physeal ClosureDeborah SalinasNo ratings yet
- Outcome of Distal Tibia Physeal FracturesDocument5 pagesOutcome of Distal Tibia Physeal FracturesDeborah SalinasNo ratings yet
- 10 1016@j Jhsa 2019 03 014Document6 pages10 1016@j Jhsa 2019 03 014Deborah SalinasNo ratings yet
- Pone 0257038Document9 pagesPone 0257038Deborah SalinasNo ratings yet
- Helical 6-Strand Cruciate Tenorrhaphy: Description of A New Technique and Biomechanical Comparative Analysis With 2 Standard TechniquesDocument8 pagesHelical 6-Strand Cruciate Tenorrhaphy: Description of A New Technique and Biomechanical Comparative Analysis With 2 Standard TechniquesDeborah SalinasNo ratings yet
- Smith 2011Document6 pagesSmith 2011Deborah SalinasNo ratings yet
- Wound Healing Complications in Diabetic Patients UDocument7 pagesWound Healing Complications in Diabetic Patients UDeborah SalinasNo ratings yet
- S0749806321003303Document20 pagesS0749806321003303Deborah SalinasNo ratings yet
- The Biomechanical Effects of Simulated RadioscaphoDocument8 pagesThe Biomechanical Effects of Simulated RadioscaphoDeborah SalinasNo ratings yet
- Rehabilitation AmbulationDocument14 pagesRehabilitation AmbulationDeborah SalinasNo ratings yet
- Fsurg 08 662720Document6 pagesFsurg 08 662720Deborah SalinasNo ratings yet
- Ambulation Spin Cord InjuryDocument16 pagesAmbulation Spin Cord InjuryDeborah SalinasNo ratings yet
- Ambulation and Parkinson DiseaseDocument22 pagesAmbulation and Parkinson DiseaseDeborah SalinasNo ratings yet
- Adaptacion Emocional de La Perdida de Una ExtremidadDocument22 pagesAdaptacion Emocional de La Perdida de Una ExtremidadDeborah SalinasNo ratings yet
- 10 1016@j Cps 2019 02 006Document9 pages10 1016@j Cps 2019 02 006Deborah SalinasNo ratings yet
- 10 1016@j Jhsa 2018 11 012Document5 pages10 1016@j Jhsa 2018 11 012Deborah SalinasNo ratings yet
- HandbookNeurorehabilitation UnknownDocument195 pagesHandbookNeurorehabilitation UnknownDeborah SalinasNo ratings yet
- Chappell 2020Document9 pagesChappell 2020Deborah SalinasNo ratings yet
- 10 1016@j Cps 2019 03 008Document10 pages10 1016@j Cps 2019 03 008Deborah SalinasNo ratings yet
- 10.1007@s40520 015 0497 yDocument8 pages10.1007@s40520 015 0497 yDeborah SalinasNo ratings yet
- Imporving Orientation in Head Injued Adults by Repeat Parctice Multisensory Input and Peer ParticipátionDocument10 pagesImporving Orientation in Head Injued Adults by Repeat Parctice Multisensory Input and Peer ParticipátionDeborah SalinasNo ratings yet
- Assistive Devices For AmbulationDocument13 pagesAssistive Devices For AmbulationDeborah Salinas100% (1)
- AMBULATIONDocument12 pagesAMBULATIONDeborah SalinasNo ratings yet
- Gaitan 1 PDFDocument12 pagesGaitan 1 PDFDeborah SalinasNo ratings yet
- Falls, Aging and DisabilityDocument17 pagesFalls, Aging and DisabilityDeborah SalinasNo ratings yet
- Agingwithmuscular Dystrophy: Pathophysiologyand ClinicalmanagementDocument22 pagesAgingwithmuscular Dystrophy: Pathophysiologyand ClinicalmanagementDeborah SalinasNo ratings yet
- University of Santo Tomas Senior High School Documentation of Ust'S Artworks Through A Walking Tour Brochure and Audio GuideDocument30 pagesUniversity of Santo Tomas Senior High School Documentation of Ust'S Artworks Through A Walking Tour Brochure and Audio GuideNathan SalongaNo ratings yet
- 1 STCW OverviewDocument19 pages1 STCW OverviewJosh SebastianNo ratings yet
- Brand ManagementDocument4 pagesBrand ManagementahmadmujtabamalikNo ratings yet
- Compania de Naveira Nedelka Sa V Tradex Internacional SaDocument3 pagesCompania de Naveira Nedelka Sa V Tradex Internacional SaAbhishek RaiNo ratings yet
- International Council For Management Studies (ICMS), Chennai (Tamilnadu) Chennai, Fees, Courses, Admission Date UpdatesDocument2 pagesInternational Council For Management Studies (ICMS), Chennai (Tamilnadu) Chennai, Fees, Courses, Admission Date UpdatesAnonymous kRIjqBLkNo ratings yet
- Chapter 7 Double Entry System: Very Short QuestionsDocument3 pagesChapter 7 Double Entry System: Very Short QuestionsVipulNo ratings yet
- 28 ESL Discussion TopicsDocument21 pages28 ESL Discussion TopicsMaruthi Maddipatla50% (2)
- New GAP Algorithm Draft 4-7-19Document1 pageNew GAP Algorithm Draft 4-7-19Umber AgarwalNo ratings yet
- Sepak TakrawDocument39 pagesSepak TakrawRandy Gasalao100% (2)
- Rose Doe v. The City of New York, Et. Al.Document57 pagesRose Doe v. The City of New York, Et. Al.Daily Caller News FoundationNo ratings yet
- Lesson 7Document20 pagesLesson 7rj libayNo ratings yet
- Environmental Mercury and Its Toxic Effects: ReviewDocument10 pagesEnvironmental Mercury and Its Toxic Effects: ReviewZusely Garcia SanchezNo ratings yet
- Fall 2012 - BIOL 115 - Essential BiologyDocument3 pagesFall 2012 - BIOL 115 - Essential BiologycreativelyinspiredNo ratings yet
- Peckiana Peckiana Peckiana Peckiana PeckianaDocument29 pagesPeckiana Peckiana Peckiana Peckiana PeckianaWais Al-QorniNo ratings yet
- Architectural Theory: Charles Jencks: Modern Movements in ArchitectureDocument32 pagesArchitectural Theory: Charles Jencks: Modern Movements in ArchitectureBafreen BnavyNo ratings yet
- Dakshina - Kannada - Brochure 2012Document28 pagesDakshina - Kannada - Brochure 2012maheshanischithaNo ratings yet
- The Period of Suppressed NationalismDocument9 pagesThe Period of Suppressed Nationalismkbj_batch0980% (5)
- May 6, 2016 Strathmore TimesDocument28 pagesMay 6, 2016 Strathmore TimesStrathmore TimesNo ratings yet
- Portable Lamps & Converters: W 276 LEDDocument2 pagesPortable Lamps & Converters: W 276 LEDRaghu paryNo ratings yet
- Folding Standards: GeneralDocument9 pagesFolding Standards: GeneralNaadiyah JauharaNo ratings yet
- Leonard Peltier Open Letter - Feb. 6, 2024Document3 pagesLeonard Peltier Open Letter - Feb. 6, 2024jen_benderyNo ratings yet
- Chinese Class Survey (Completed)Document4 pagesChinese Class Survey (Completed)Yibing ZhangNo ratings yet
- C. Ra 6969 - Engr. Czes BongcoDocument87 pagesC. Ra 6969 - Engr. Czes Bongcorandell vasquezNo ratings yet
- Cost Accounting Name: - ActivitiesDocument2 pagesCost Accounting Name: - ActivitiesJosh AlvarezNo ratings yet
- Choreography Proposal: Dance Ensemble 2023: Choreographer'S InformationDocument6 pagesChoreography Proposal: Dance Ensemble 2023: Choreographer'S InformationTrey ErnyNo ratings yet
- Evaluating WebsitesDocument2 pagesEvaluating Websitesapi-322361374No ratings yet
- 5 Brilliant Depictions of Lucifer in Art From The Past 250 YearsDocument1 page5 Brilliant Depictions of Lucifer in Art From The Past 250 Yearsrserrano188364No ratings yet
- Contoh Formal LetterDocument2 pagesContoh Formal LetterFairos Azmi MarzahNo ratings yet
- CP16 Risk AssessmentDocument1 pageCP16 Risk AssessmentJulia KaouriNo ratings yet
Salter - Harris 2 Displaced Fractuers Best Treatment
Salter - Harris 2 Displaced Fractuers Best Treatment
Uploaded by
Deborah SalinasOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Salter - Harris 2 Displaced Fractuers Best Treatment
Salter - Harris 2 Displaced Fractuers Best Treatment
Uploaded by
Deborah SalinasCopyright:
Available Formats
108 Acta Orthopaedica 2018; 89 (1): 108–112
What is the best treatment for displaced Salter–Harris II
physeal fractures of the distal tibia?
Hoon PARK 1, Dong Hoon LEE 2, Seung Hwan HAN 1, Sungmin KIM 2, Nam Kyu EOM 1, and Hyun Woo KIM 2
1 Department of Orthopaedic Surgery, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea; 2 Division of Orthopaedic
Surgery, Severance Children’s Hospital, Yonsei University College of Medicine, Seoul, Korea
Correspondence: pedhkim@yuhs.ac
Submitted 2016-12-30. Accepted 2017-08-14.
Background and purpose — The optimal treatment of displaced et al. 1978, Kay and Matthys 2001). SH II fractures are con-
Salter–Harris (SH) II fractures of the distal tibia is controversial. sidered low-risk fractures because the incidence of premature
We compared the outcomes of operative and nonoperative treat- physeal closure (PPC) was reported as 2–5% in a previous
ment of SH II distal tibial fractures with residual gap of > 3 mm. study (Dugan et al. 1987). However, some studies indicate that
Factors that may be associated with the incidence of premature PPC may be more common than previously realized in specifi-
physeal closure (PPC) were analyzed. cally SH II distal tibial fractures (Spiegel et al. 1978, Kling et
Patients and methods — We retrospectively reviewed 95 patients al. 1984). Several recent studies reported that the incidence
who were treated for SH II distal tibial fractures with residual of PPC was 25–40% in SH II distal tibial fractures (Barmada
gap of > 3 mm after closed reduction. Patients were assigned to et al. 2003, Rohmiller et al. 2006, Leary et al. 2009). Bar-
1 of 2 groups: Group 1 included 25 patients with nonoperative mada et al. (2003) suggested that open reduction and removal
treatment, irrespective of size of residual gap (patients treated of the entrapped periosteum in displaced SH II fractures with
primarily at other hospitals). Group 2 included 70 patients with residual physeal gap of > 3 mm may be beneficial for reducing
operative treatment. All patients were followed for ≥ 12 months the incidence of PPC, and it seems to be a current trend that a
after surgery, with a mean follow-up time of 21 months. Logistic surgical approach is the treatment of choice in displaced SH II
regression analyses were performed to identify risk factors for the fractures of the distal tibia. However, some authors insist that
occurrence of PPC. surgical management of these fractures does not reduce the
Results — The incidence of PPC in patients who received non- incidence of PPC, and might increase the need for subsequent
operative treatment was 13/52, whereas PPC incidence in patients surgeries (Russo et al. 2013).
who received operative treatment was 24/70 (p = 0.1). Multivari- Most previous studies included patients with all types of
able logistic regression analysis determined that significant risk physeal fractures and even transitional fractures (Barmada et
factors for the occurrence of PPC were age at injury, and injury al. 2003, Rohmiller et al. 2006, Leary et al. 2009, Schurz et al.
mechanism. The method of treatment, sex, presence of fibu- 2010). Although some authors recently reported the results of
lar fracture, residual displacement after closed reduction, and surgical treatment only for displaced SH II distal tibial frac-
implant type were not predictive factors for the occurrence of tures, they included patients with residual gap of < 3 mm and
PPC. performed surgical treatment in all patients with residual gap
Interpretation — Operative treatment for displaced SH II of > 4 mm after closed reduction (Russo et al. 2013). To our
distal tibial fractures did not seem to reduce the incidence of PPC knowledge, there is no clinical study that directly compared
compared with nonoperative treatment. We cannot exclude that operative treatment with nonoperative treatment for displaced
surgery may be of value in younger children with pronation– SH II distal tibial fractures with a residual gap of > 3 mm
abduction or pronation–external rotation injuries. to prove the superiority of surgical treatment as suggested by
■ Barmada et al. (2003). Therefore, we compared the incidence
of PPC after operative treatment with that after nonopera-
tive treatment in displaced SH II distal tibial fractures with
Physeal injuries of the distal tibia account for one-tenth of all residual gap of > 3 mm, and aimed to analyze the factors that
physeal fractures (Peterson et al. 1994). Among these, Salter– may be associated with PPC incidence. We hypothesized that
Harris type II (SH II) fractures are the most common, account- anatomical reduction would reduce the incidence of PPC inci-
ing for 40% of all distal tibial fractures in children (Spiegel dence compared with that of nonoperative management.
© 2017 The Author(s). Published by Taylor & Francis on behalf of the Nordic Orthopedic Federation. This is an Open Access article distributed under the terms
of the Creative Commons Attribution-Non-Commercial License (https://creativecommons.org/licenses/by-nc/3.0)
DOI 10.1080/17453674.2017.1373496
11192 Kim D.indd 108 1/3/2018 12:07:47 PM
Acta Orthopaedica 2018; 89 (1): 108–112 109
Patients and methods
Our institution has treated patients with displaced SH II distal
tibial fractures according to the protocol of Barmada et al.
(2003). Initially, all acute displaced fractures were treated with
closed reduction. Then, if the displacement was not reduced or
believed to be > 3 mm, computed tomography (CT) scanning
was performed to measure the residual gap. Patients received
subsequent treatment based on the amount of residual fracture
displacement. Those with residual gap > 3 mm were treated
with open reduction and internal fixation.
We identified 150 patients with SH II distal tibial fractures
between March 2006 and March 2015. The inclusion crite-
ria were: (1) age younger than 15 years, (2) open distal tibial
physis, (3) residual displacement after closed reduction > 3 mm a b
on coronal or sagittal CT images, and (4) minimum follow-up Figure 1. A SH II distal tibia fracture with (a) supination–external rota-
time of 1 year. 46 patients with nondisplaced SH II distal tibial tion (SER) injury, and (b) pronation–external rotation (PER) injury. The
amount of initial displacement (white double-sided arrow) was mea-
fractures were excluded from the study. A further 9 patients sured as the largest displacement between the epiphysis and metaph-
were excluded because they did not have post-reduction CT ysis on initial anteroposterior or lateral view.
scans or follow-up radiographs available for review.
Thus, 95 ankles in 95 patients were included in this study.
Demographic data are presented in Table 1. The mean follow- Data included patient age at the time of injury, sex, mecha-
up period was 21 (12–100) months. nism of injury, presence of concurrent fibular fracture, amount
The patients were assigned to 1 of 2 groups based on the of initial displacement before reduction, amount of residual
method of treatment. Group 1 included 25 patients who displacement after reduction, the type of implant used, and
received nonoperative treatment. All patients in Group 1 occurrence of PPC. Initial displacement before reduction
were treated at other hospitals with cast immobilization after was measured from radiographs as the greatest amount of
closed reduction and then referred to our tertiary care pedi- displacement (in millimeters) between the epiphysis and the
atric hospital. All patients brought their medical records and metaphysis (Figure 1). Residual displacement after reduction
radiographs including CT scans to us. These patients could was measured on coronal or sagittal CT images using the same
not be included in our treatment protocol as described above, method. Initial displacement was measured in 65/70 patients
because the mean interval from injury to the first visit at our in Group 2. However, in Group 1, initial displacement was
hospital was 2.5 (2–4.5) weeks. Instead, they were treated measured in only 6/25 patients. Some patients in Group 1 did
with non-weight-bearing short-leg cast until 6 weeks after not bring their initial radiographs before closed reduction,
injury. Group 2 included 70 patients who received surgical others brought only CT images, the remainder had inappropri-
treatment. All patients in Group 2 were initially diagnosed ate radiographs to measure the gaps. The mechanism of injury
at our hospital and were treated according to our treatment was classified as SER, ABD, or PER based on the Lauge-
protocol as described above. Two surgeons performed all Hansen classification system (Lauge-Hansen 1950) (Figure
surgeries in Group 2. Open reduction was performed under 2). The physis was evaluated from bilateral anteroposterior or
fluoroscopic control. In all cases, periosteum if interposed lateral radiographs during all follow-up appointments. If PPC
was removed. Fixation was either by K-wires, which crossed was questionable, a CT scan was obtained to investigate the
the physis, or with screws placed in the metaphysis according presence of a physeal bar. All radiological measurements were
to the surgeon’s preference. A non-weight-bearing short-leg performed by 2 orthopedic surgeons (SK and NKE) who were
cast was applied for 6 weeks after surgery for all patients. blinded to the study.
K-wires were removed 4 weeks after surgery. Screws were
not routinely removed; if otherwise, this was done 6 months Statistics
after surgery. Comparisons were performed to determine whether the inci-
The mean residual displacement was 4.0 (3.4–5.5) mm in dence of PPC differed statistically significantly between
Group 1, and 5.5 (3.5–20) mm in Group 2. We thought that Groups 1 and 2. We also compared Group 1 with Group 2A
this discrepancy was due to potential bias arising from the sur- with regard to the incidence of PPC. Several demographic
geon’s preference for fixation procedure. Therefore, we cre- and surgical variables were considered as possible factors
ated Group 2A to match the range of residual displacement that could be related to the occurrence of PPC. These factors
in Group 1. Group 2A consisted of 43 patients with residual included (1) age, (2) sex, (3) mechanism of injury, (4) pres-
displacement of 3.5–5.5 mm. ence of fibular fracture, (5) amount of residual displacement,
11192 Kim D.indd 109 1/3/2018 12:07:47 PM
110 Acta Orthopaedica 2018; 89 (1): 108–112
Ethics, funding, and potential con-
flicts of interest
Our Institutional Review Board approved
this retrospective study (date of approval
September 6, 2016; IRB number 4-2016-
0650). Each author certifies that his institu-
tion approved the human protocol for this
investigation, and that all investigations
were conducted in conformity with ethical
principles of research. No financial support
has been received relating to this research.
All authors have no conflicts of interests or
financial disclosures to declare.
a b c
Figure 2. Types of injury: (a) supination-external rotation (SER) injury, (b) pronation-abduc-
tion (ABD) injury, and (c) pronation-external rotation (PER) injury. Results
There were no statistically significant dif-
ferences between Group 1 and Group 2
with respect to age, sex, mechanism of
injury, or the presence of fibular fracture
(6) method of treatment, and (7) type of implant. These pre- (see Table 1). The residual displacement was significantly dif-
dictors were chosen a priori based on our own hypotheses and ferent (p < 0.001) between the 2 groups. The incidence of PPC
previous literature (Rohmiller et al. 2006, Leary et al. 2009, (13/25) in Group 1 was higher than that (24/70) in Group 2,
Russo et al. 2013). However, as mentioned earlier, we could but the difference was not statistically significant (p = 0.1).
not measure the amount of initial displacement in all patients, We created Group 2A to match the range of the residual
because most patients in Group 1 did not bring their initial displacement of Group 1 and compared these 2 groups with
radiograph at the time of injury. Therefore, the amount of ini- regard to same variables and still found no statistically signifi-
tial displacement was excluded in all analyses. Correlation cant difference in PPC incidence between Group 1 (13/25) and
analyses were performed to determine whether the occurrence Group 2A (14/43) (p = 0.1).
of PPC was significantly correlated with these demographic The incidence of PPC was evaluated with multivariable
factors and surgical variables. logistic regression analysis of all included patients. The occur-
Statistical analyses were performed using SPSS® version rence of PPC was associated with older age at injury (OR =
19.0 (SPSS, Chicago, IL, USA). Data were assessed for nor- 1.5), ABD-type injury (OR = 4.0), and PER-type injury (OR =
mality on plots and using the Shapiro–Wilk test. Student’s 6.6). The method of treatment had no effect on the incidence
independent t-test for continuous variables and chi-square of PPC (Table 2). Multivariable logistic regression analysis of
test for categorical variables were used to compare Group 1 Group 2 revealed two significant risk factors for the incidence
and Group 2 with regard to demographic characteristics, pre- of PPC, which were older age at injury (OR = 1.4) and injury
operative variables, and PPC rates. The same analytic tests mechanism: PER injury (OR = 7.2) (Table 3). ABD injury and
were used to compare Group 1 and Group 2A. To identify the type of implant were not predictive factors for the occurrence
independent predictors of PPC, we used univariable and mul- of PPC.
tivariable logistic regression with stepwise selection of candi- There was no nonunion and no implant failures. Superfi-
date variables (see Table 1). Covariate selection was checked cial skin infection developed after surgery in 2 patients, who
by visual inspection of directed acyclic graphs (Shrier and were treated with intravenous antibiotics. The mean time
Platt 2008). Age and mechanism of injury were retained in after surgery for PPC diagnosis was 8 (4–12) months. The
all models. Additionally, the effect of method of treatment on mean age of patients who developed PPC was 12.3 (8.2–15)
incidence of PPC was analyzed in all patients and the effect years. 37 patients had PPC, 13 in Group 1 and 24 in Group
of the type of implant on incidence of PPC was analyzed in 2 (Table 4). Shortening and angular deformity were similar
patients who received surgical treatment (Group 2). All tests between groups. 2 patients underwent correctional osteotomy
were 2-tailed, and p < 0.05 was considered statistically signifi- for angular deformity and one patient underwent permanent
cant and 0.05 ≤ p < 0.1 was considered a trend toward signifi- epiphysiodesis of the proximal tibia on the contralateral side
cance to increase the sensitivity to detect potential selection for leg-length discrepancy in Group 1. In Group 2, we per-
bias (Altman and Bland 1996). formed correctional osteotomy in 1 patient and temporary epi-
physiodesis with tension band plate in 1 patient. Although we
11192 Kim D.indd 110 1/3/2018 12:07:47 PM
Acta Orthopaedica 2018; 89 (1): 108–112 111
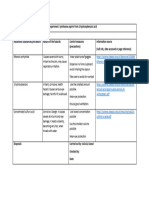
Table 1. Comparisons between groups by treatment method
Group 1 Group 2 Group 2A
Cast Surgery p-value Matched subgroup p-value
Variables (n = 25) (n = 70) (1 versus 2) (n = 43) a (1 versus 2A)
Age, mean (range), years 12.0 (8.2–14.8) 11.6 (5.1–15.0) 0.4 11.3 (5.1–14.5) 0.2
Sex, n 0.9 0.9
Male 17 49 29
Female 8 21 14
Mechanism of injury, n 0.7
Supination–external rotation 16 45 31
Pronation–abduction 7 16 9
Pronation–external rotation 2 9 3
Fibular fracture, n 15 46 0.6 22 0.5
Residual displacement, mean (SD) (mm) 4.0 (0.7) 5.5 (2.7) < 0.001 4.1 (0.7) 0.6
Total number of premature physeal closure 13 24 0.1 14 0.1
aA matched subgroup (Group 2A) consisted of patients with residual displacement of 3.5–5.5 mm to match the range of residual
displacement of Group 1.
Table 2. Univariable and multivariable logistic regression analysis of Table 4. Comparisons of complications between groups by treat-
premature physeal closure ment method. Values are number of patients
Univariable Multivariable Group 1 Group 2
Factor Odds ratio a p-value Odds ratio a p-value Cast Surgery
Variables (n = 25) (n = 70) p-value
Age at time of injury 1.3 (1.0–1.7) 0.02 1.5 (1.1–2.0) 0.01
Female versus male 0.6 (0.2–1.5) 0.3 Total number of PPC a 13 24 0.2
Mechanism of injury b Shortening < 10mm 8 15 0.3
ABD type 2.2 (0.8–5.9) 0.1 4.0 (1.2–13) 0.02 Shortening > 10mm 1 2 0.8
PER type 6.4 (1.5–27) 0.01 6.6 (1.5–29) 0.01 Angulation < 10 degrees 2 5 0.9
Fibular fracture 1.6 (0.6–3.7) 0.3 Angulation > 10 degrees 2 2 0.3
Residual displacement 1.0 (0.9–1.2) 0.8 Required correctional surgery 3 4 0.3
Surgery versus cast 0.5 (0.2–1.2) 0.1 0.5 (0.2–1.3) 0.1
a PPC: premature physeal closure.
a Values are odds ratio (95% confidence interval).
b SER type is the reference group. SER: supination–externalrotation;
ABD: pronation–abduction; PER: pronation–external rotation.
Discussion
Table 3. Univariable and multivariable logistic regression analysis of We found that anatomical reduction using surgical treatment was
premature physeal closure in patients treated with surgery (Group 2) not more effective for reducing the incidence of PPC than non-
operative management for displaced SH II fractures. Although
Univariable Multivariable the PPC incidence in Group 1 patients was higher than that in
Factor Odds ratio a p-value Odds ratio a p-value Group 2 patients, there was no statistically significant difference
Age at time of injury 1.3 (0.9–1.8) 0.06 1.4 (1.0–2.0) 0.06
between groups. Our results showed that the surgical treatment
Female versus male 0.9 (0.3–2.8) 0.9 for displaced SH II fractures with residual physeal gap of > 3
Mechanism of injury b mm was not superior to nonoperative treatment.
ABD type 1.2 (0.4–4.3) 0.7 1.4 (0.3–6.2) 0.6
PER type 9.6 (1.8–53) 0.01 7.2 (1.2–42) 0.03
Although SH II fractures in general have been reported
Fibular fracture 1.1 (0.4–3.0) 0.9 to have a low incidence of growth disturbance, our results
Residual displacement 1.0 (0.9–1.3) 0.7 indicate that the overall incidence of PPC was 0.4 (37/95) in
Screw versus K-wire 1.9 (0.6–5.8) 0.2 2.4 (0.6–8.9) 0.2
displaced SH II distal tibial fractures, similar to previously
a and b See Table 2 reported incidences (Barmada et al. 2003, Rohmiller et al.
2006, Leary et al. 2009). Thus, the presence of a residual gap
(> 3 mm) in these injuries may predict a higher incidence of
recommended permanent epiphysiodesis of the contralateral PPC. Although Dugan et al. (1987) considered SH II distal
proximal tibia for 2 patients showing shortening > 10 mm in tibial fractures to be low-risk fractures based on the rate of
Group 2, they refused subsequent surgery. The remaining 30 complications (2–5%), we believe that displaced SH II distal
patients who had mild angular deformity or shortening did not tibial fractures should be considered high-risk fractures based
undergo correctional surgery as of the last follow-up. on the incidence of PPC.
11192 Kim D.indd 111 1/3/2018 12:07:49 PM
112 Acta Orthopaedica 2018; 89 (1): 108–112
Previous studies report that initial and residual displace- the number of fracture reductions and the degrees of initial
ments are risk factors for PPC (Barmada et al. 2003, Rohm- displacement. Moreover, the amount of initial displacement
iller et al. 2006). We could not prove the effect of the amount could not be analyzed as a risk factor on the incidence of PPC.
of initial and residual displacement on the incidence of PPC Fourth, we focused on radiological results without clinical or
using multivariable logistic regression, because these factors subjective outcome.
were not suitable for multivariable logistic regression using In summary, we suggest that the treatment of displaced SH
visual inspection of directed acyclic graphs (Shrier and Platt II distal tibial physeal fractures with a residual gap of > 3 mm
2008). However, residual displacement was not a significant should be individualized, with consideration of the patient’s
predictor of PPC using univariable logistic regression and the age and injury mechanism.
rate of PPC of Group 2 was similar to that of Group 2A.
ABD and PER injuries were associated with the occur-
rence of PPC, and these associations are consistent with those HP: Data analysis and interpretation, statistical analysis, writing of the man-
reported by recent studies (Rohmiller et al. 2006, Russo et al. uscript. DHL: treatment concepts, revision of the manuscript. SHH: Study
design. SK: data collection. NKE: data collection. HWK: treatment concepts,
2013). Some authors presume that trauma involved in these critical revision of the manuscript.
types of injuries might be greater than that of SER injury, or
that the direction of force during these injuries might damage
Kump’s bump, which could occur during initial physiologi- Acta thanks Vera Baasland Halvorsen and Tanja Kraus for help with peer
cal closure of the distal tibial physis (Kump 1966, Chung and review of this study.
Jaramillo 1995, Rohmiller et al. 2006). We agree: the medial
side of the physis was more commonly injured in ABD or PER
injuries than in SER injury. Altman D G, Bland J M. Absence of evidence is not evidence of absence. Aust
PPC occurred in 37 of our patients. Of these, 7 patients Vet J 1996; 74 (4): 311.
developed deformity which motivated correctional surgery Barmada A, Gaynor T, Mubarak S J. Premature physeal closure follow-
ing distal tibia physeal fractures: A new radiographic predictor. J Pediatr
(performed in 5 of these). The remaining 30 patients did not Orthop 2003; 23 (6): 733-9.
undergo a second surgery, and these rates were similar to those Chung T, Jaramillo D. Normal maturing distal tibia and fibula: Changes with
of previous reports (Leary et al. 2009, Russo et al. 2013). age at MR imaging. Radiology 1995; 194 (1): 227-32.
Although these patients had clinical sequelae such as leg- Dugan G, Herndon W A, McGuire R. Distal tibial physeal injuries in children:
length discrepancy of < 10 mm or angular deformity of < 10 a different treatment concept. J Orthop Trauma 1987; 1 (1): 63-7.
degrees, they did not complain of any discomfort in their daily Kay R M, Matthys G A. Pediatric ankle fractures: Evaluation and treatment. J
Am Acad Orthop Surg 2001; 9 (4): 268-78.
lives. Thus, not all patients with PPC have clinical sequelae
Kling T F, Jr, Bright R W, Hensinger R N. Distal tibial physeal fractures in
that required surgical correction. children that may require open reduction. J Bone Joint Surg (Am) 1984;
Adolescent patients close to skeletal maturity are unlikely 66 (5): 647-57.
to have significant deformity due to PPC; however, younger Kump W L. Vertical fractures of the distal tibial epiphysis. Am J Roentgenol
patients need to be followed up closely for development of Radium Ther Nucl Med 1966; 97 (3): 676-81.
significant deformities of the distal tibia. Lauge-Hansen N. Fractures of the ankle, II: Combined experimental-surgical
and experimental-roentgenologic investigations. Arch Surg 1950; 60 (5):
Although surgical treatment for displaced SH II distal tibial 957-85.
physeal fractures with a residual gap of > 3 mm did not sta- Leary J T, Handling M, Talerico M, Yong L, Bowe J A. Physeal fractures of
tistically significantly reduce the rate of PPC, surgery may be the distal tibia: Predictive factors of premature physeal closure and growth
necessary in some selected patients. We think that surgical arrest. J Pediatr Orthop 2009; 29 (4): 356-61.
treatment may be considered in younger patients with a high Peterson H A, Madhok R, Benson J T, Ilstrup D M, Melton L J, 3rd. Physeal
fractures, Part 1: Epidemiology in Olmsted County, Minnesota, 1979-1988.
possibility of PPC such as ABD or PER type injury. Addi- J Pediatr Orthop 1994; 14 (4): 423-30.
tionally, older patients with a large residual displacement may Rohmiller M T, Gaynor T P, Pawelek J, Mubarak S J. Salter-Harris I and II
require anatomical reduction to improve joint alignment due fractures of the distal tibia: Does mechanism of injury relate to premature
to lower remodeling potential. Therefore, the choice of treat- physeal closure? J Pediatr Orthop 2006; 26 (3): 322-8.
ment for displaced SH II distal tibial physeal fractures should Russo F, Moor M A, Mubarak S J, Pennock A T. Salter-Harris II fractures
of the distal tibia: Soes surgical management reduce the risk of premature
be individualized. physeal closure? J Pediatr Orthop 2013; 33 (5): 524-9.
This study had several limitations. First, it was a retrospec- Schurz M, Binder H, Platzer P, Schulz M, Hajdu S, Vecsei V. Physeal injuries
tive study without randomization and the relatively small of the distal tibia: Long-term results in 376 patients. Int Orthop 2010; 34
number of patients with PER injury reduces the power of the (4): 547-52.
statistical analysis. Second, 2 surgeons were involved, and Shrier I, Platt R W. Reducing bias through directed acyclic graphs. BMC Med
Res Methodol 2008; 8: 70.
the operative techniques and number of reduction attempts Spiegel P G, Cooperman D R, Laros G S. Epiphyseal fractures of the distal
were not standardized. Third, because the patients in Group ends of the tibia and fibula: A retrospective study of two hundred and thirty-
1 did not come from our own institution, we did not know seven cases in children. J Bone Joint Surg (Am) 1978; 60 (8): 1046-50.
11192 Kim D.indd 112 1/3/2018 12:07:49 PM
You might also like
- UdaipurDocument52 pagesUdaipurArun Kumar100% (2)
- Salter Harris II Fractures of The Distal Tibia Does Surgical Management Reduce The Risk of Premature Physeal ClosureDocument6 pagesSalter Harris II Fractures of The Distal Tibia Does Surgical Management Reduce The Risk of Premature Physeal ClosureDeborah SalinasNo ratings yet
- Treatment and Outcome of Diatl Tibia Saletr Harris II FracturesDocument6 pagesTreatment and Outcome of Diatl Tibia Saletr Harris II FracturesDeborah SalinasNo ratings yet
- Open Reduction and Internal Fixation For Displaced Salter Harris 2Document7 pagesOpen Reduction and Internal Fixation For Displaced Salter Harris 2Deborah SalinasNo ratings yet
- Surgical Treatment of Metastatic Tumors of The FemurDocument6 pagesSurgical Treatment of Metastatic Tumors of The FemurHitham El ShahatNo ratings yet
- HP 26 99Document8 pagesHP 26 99Juan PagesNo ratings yet
- Premature Physeal Closure Following Distal Tibia Physeal FracturesDocument7 pagesPremature Physeal Closure Following Distal Tibia Physeal FracturesDeborah SalinasNo ratings yet
- Clinical Analysis of The Frosch Approach in The Treatment of Posterolateral Tibial Plateau Fractures Combined With Lateral Tibial Plateau FracturesDocument11 pagesClinical Analysis of The Frosch Approach in The Treatment of Posterolateral Tibial Plateau Fractures Combined With Lateral Tibial Plateau FracturesraynaldidjohariofcNo ratings yet
- Conservative Versus Surgical Management of Intra-Articular Fractures of Distal End of Radius: A Comparative Clinical StudyDocument10 pagesConservative Versus Surgical Management of Intra-Articular Fractures of Distal End of Radius: A Comparative Clinical StudyAnonymous OJELaiw2No ratings yet
- Paper 1 Vinothkumar-1Document5 pagesPaper 1 Vinothkumar-1SK BONE & JOINT CARE DPINo ratings yet
- Brief Resume of Intended WorkDocument7 pagesBrief Resume of Intended WorkNavin ChandarNo ratings yet
- PFN PaperDocument7 pagesPFN PaperNisar Ahmed DarNo ratings yet
- 2019 Article 2632analisis TomograficoDocument6 pages2019 Article 2632analisis TomograficoLenin EstrellaNo ratings yet
- Fratura de UmeroDocument7 pagesFratura de UmerodanfisiofoxNo ratings yet
- Syndesmotic Screw Removed Verusus Retained: A Comparative Functional AnalysisDocument4 pagesSyndesmotic Screw Removed Verusus Retained: A Comparative Functional AnalysisSarath KumarNo ratings yet
- 97-506-1 Segundo CynDocument6 pages97-506-1 Segundo CynGalletita De JengibreNo ratings yet
- Jurnal PfnaDocument10 pagesJurnal PfnaDhea Amalia WibowoNo ratings yet
- Abstracts de Publicaciones Sobre Pilón TibialDocument15 pagesAbstracts de Publicaciones Sobre Pilón TibialAyler AguilarNo ratings yet
- A Study On Management of Bothbones Forearm Fractures With Dynamic Compression PlateDocument5 pagesA Study On Management of Bothbones Forearm Fractures With Dynamic Compression PlateIOSRjournalNo ratings yet
- Stabilization of Distal Humerus Fractures by Precontoured Bi-Condylar Plating in A 90-90 PatternDocument5 pagesStabilization of Distal Humerus Fractures by Precontoured Bi-Condylar Plating in A 90-90 PatternmayNo ratings yet
- Treatment of AO/OTA 31-A3 Intertrochanteric Femoral Fractures With A Percutaneous Compression PlateDocument7 pagesTreatment of AO/OTA 31-A3 Intertrochanteric Femoral Fractures With A Percutaneous Compression PlateNurul AiniNo ratings yet
- Surgical Treatment of Chronic Elbow Dislocation Allowing For Early Range of Motion: Operative Technique and Clinical ResultsDocument8 pagesSurgical Treatment of Chronic Elbow Dislocation Allowing For Early Range of Motion: Operative Technique and Clinical ResultsLuis Carlos HernandezNo ratings yet
- 1 s2.0 S1877056821003029 MainDocument21 pages1 s2.0 S1877056821003029 MainAndrea OsborneNo ratings yet
- Jurnal Fraktur Humerus DistalDocument5 pagesJurnal Fraktur Humerus DistalthisisangieNo ratings yet
- Prabhakar 2020Document9 pagesPrabhakar 2020Lucas LozaNo ratings yet
- Augmentation Plating Leaving The Nail in Situ Is An Excellent Option For Treating Femoral Shaft Nonunion After IM Nailing: A Multicentre StudyDocument7 pagesAugmentation Plating Leaving The Nail in Situ Is An Excellent Option For Treating Femoral Shaft Nonunion After IM Nailing: A Multicentre StudytomimacagnoNo ratings yet
- Tecnica de ChampyDocument7 pagesTecnica de Champyboye022694No ratings yet
- Sicotj160057 PDFDocument6 pagesSicotj160057 PDFDr'Dinesh MishraNo ratings yet
- Association of Pars Defect Type With Clinical Outcome After Smiley Face Rod Methods For Terminal-Stage SpondylolysisDocument8 pagesAssociation of Pars Defect Type With Clinical Outcome After Smiley Face Rod Methods For Terminal-Stage SpondylolysisUzm.Dr.Burhan ORAL GÜDÜNo ratings yet
- Tan2012 PDFDocument10 pagesTan2012 PDFdebyanditaNo ratings yet
- Arthroscopic Partial Trapeziectomy and Tendon Interposition For Thumb Carpometacarpal ArthritisDocument7 pagesArthroscopic Partial Trapeziectomy and Tendon Interposition For Thumb Carpometacarpal ArthritisJayNo ratings yet
- Chang 2017. Skeletal RadiologyDocument7 pagesChang 2017. Skeletal RadiologyteresaNo ratings yet
- Treatment Considerations For Comminuted Mandibular FracturesDocument10 pagesTreatment Considerations For Comminuted Mandibular FracturesAnonymous ENwjWryNo ratings yet
- Research ArticleDocument9 pagesResearch ArticleAni LabibahNo ratings yet
- Medi 97 E0523Document9 pagesMedi 97 E0523Andrea OsborneNo ratings yet
- 1 s2.0 S0901502716300728 MainDocument4 pages1 s2.0 S0901502716300728 MainCaio GonçalvesNo ratings yet
- Functional Outcome of Operative Management of Humeral Shaft FracturesDocument5 pagesFunctional Outcome of Operative Management of Humeral Shaft FracturesDr JunaidNo ratings yet
- Intertan Nail Vs PFN ADocument7 pagesIntertan Nail Vs PFN AzubayetarkoNo ratings yet
- Early and 1 Year Postsurgical Stability and Its Factors in Patients With Complicated Skeletal Class III Mal OcclusionDocument13 pagesEarly and 1 Year Postsurgical Stability and Its Factors in Patients With Complicated Skeletal Class III Mal Occlusionrana.hafezNo ratings yet
- Paper 38Document6 pagesPaper 38Dr Vineet KumarNo ratings yet
- Reisoğlu 2017Document5 pagesReisoğlu 2017Tuğçe KabakcıNo ratings yet
- Canulavos Vs Alambre K Fractura Patela 2020 ChinoDocument7 pagesCanulavos Vs Alambre K Fractura Patela 2020 ChinoGeraldine Alvarez ANo ratings yet
- Treatment of Periprosthetic Knee Fractures With Plate and Screws and With Retrograde Intramedullary Nail Indications Limits and Medium Term Follow UpDocument22 pagesTreatment of Periprosthetic Knee Fractures With Plate and Screws and With Retrograde Intramedullary Nail Indications Limits and Medium Term Follow UpAthenaeum Scientific PublishersNo ratings yet
- Percutaneous Screw Fixation of Crescent Fracture Dislocation of The Sacroiliac JointDocument7 pagesPercutaneous Screw Fixation of Crescent Fracture Dislocation of The Sacroiliac Jointgevowo3277No ratings yet
- Moderator:Dr Vijay Kumar Co-Moderator:Dr Venketish All India Institute of Medical Sciences New DelhiDocument58 pagesModerator:Dr Vijay Kumar Co-Moderator:Dr Venketish All India Institute of Medical Sciences New DelhiWasim R. IssaNo ratings yet
- Fraktur FrakDocument11 pagesFraktur FrakRirin SeptianiNo ratings yet
- Case Series of All-Arthroscopic Treatment For Terrible Triad of The Elbow: Indications and Clinical OutcomesDocument10 pagesCase Series of All-Arthroscopic Treatment For Terrible Triad of The Elbow: Indications and Clinical OutcomesdorfynatorNo ratings yet
- Percutaneous Pinning of Distal Radius Fractures Using Hematoma Block: Outcomes in Our CenterDocument3 pagesPercutaneous Pinning of Distal Radius Fractures Using Hematoma Block: Outcomes in Our CenterPeertechz Publications Inc.No ratings yet
- 2023 JOT Radiological and Long Term Functional Outcomes of Displaced Distal Clavicle FracturesDocument7 pages2023 JOT Radiological and Long Term Functional Outcomes of Displaced Distal Clavicle FracturesjcmarecauxlNo ratings yet
- Goyal 2012Document9 pagesGoyal 2012rahulNo ratings yet
- Claus 2019Document8 pagesClaus 2019abhishekjha0082No ratings yet
- Jurding Inggris RadiologiDocument7 pagesJurding Inggris RadiologiIrawaty Christin Marthyna SimanjuntakNo ratings yet
- Treatment of Tibial Plateau Fractures Dual Plating Dual IncisionDocument6 pagesTreatment of Tibial Plateau Fractures Dual Plating Dual IncisionAnnie JoNo ratings yet
- Fraktur KlavikulaDocument10 pagesFraktur KlavikulaEricsen T.P.No ratings yet
- Medip, IJORO-2331 ODocument7 pagesMedip, IJORO-2331 Oprashant makadiaNo ratings yet
- Type A1 Intertroch PFN VS DHS RetrospectiveDocument11 pagesType A1 Intertroch PFN VS DHS RetrospectiveMuhammad Tabish SaleemNo ratings yet
- Posterolateral Approach For Posterior Malleolus FiDocument12 pagesPosterolateral Approach For Posterior Malleolus FiorlanquisNo ratings yet
- Treatment Distal Radius Fracture With Volar Buttre PDFDocument5 pagesTreatment Distal Radius Fracture With Volar Buttre PDFZia Ur RehmanNo ratings yet
- Ekhtiari 2017Document9 pagesEkhtiari 2017QuiroprácticaParaTodosNo ratings yet
- Acetabular Fractures in Older Patients: Assessment and ManagementFrom EverandAcetabular Fractures in Older Patients: Assessment and ManagementTheodore T. MansonNo ratings yet
- Surgery of the Cranio-Vertebral JunctionFrom EverandSurgery of the Cranio-Vertebral JunctionEnrico TessitoreNo ratings yet
- Pi Is 0363502317301211Document8 pagesPi Is 0363502317301211Deborah SalinasNo ratings yet
- Outcome of Distal Tibial Physeal InjuriesDocument7 pagesOutcome of Distal Tibial Physeal InjuriesDeborah SalinasNo ratings yet
- Open Reduction and Internal Fixation For Displaced Salter Harris 2Document7 pagesOpen Reduction and Internal Fixation For Displaced Salter Harris 2Deborah SalinasNo ratings yet
- 10 1016@j Jhsa 2020 08 001Document8 pages10 1016@j Jhsa 2020 08 001Deborah SalinasNo ratings yet
- Salter Harris II Fractures of The Distal Tibia Does Surgical Management Reduce The Risk of Premature Physeal ClosureDocument6 pagesSalter Harris II Fractures of The Distal Tibia Does Surgical Management Reduce The Risk of Premature Physeal ClosureDeborah SalinasNo ratings yet
- Outcome of Distal Tibia Physeal FracturesDocument5 pagesOutcome of Distal Tibia Physeal FracturesDeborah SalinasNo ratings yet
- 10 1016@j Jhsa 2019 03 014Document6 pages10 1016@j Jhsa 2019 03 014Deborah SalinasNo ratings yet
- Pone 0257038Document9 pagesPone 0257038Deborah SalinasNo ratings yet
- Helical 6-Strand Cruciate Tenorrhaphy: Description of A New Technique and Biomechanical Comparative Analysis With 2 Standard TechniquesDocument8 pagesHelical 6-Strand Cruciate Tenorrhaphy: Description of A New Technique and Biomechanical Comparative Analysis With 2 Standard TechniquesDeborah SalinasNo ratings yet
- Smith 2011Document6 pagesSmith 2011Deborah SalinasNo ratings yet
- Wound Healing Complications in Diabetic Patients UDocument7 pagesWound Healing Complications in Diabetic Patients UDeborah SalinasNo ratings yet
- S0749806321003303Document20 pagesS0749806321003303Deborah SalinasNo ratings yet
- The Biomechanical Effects of Simulated RadioscaphoDocument8 pagesThe Biomechanical Effects of Simulated RadioscaphoDeborah SalinasNo ratings yet
- Rehabilitation AmbulationDocument14 pagesRehabilitation AmbulationDeborah SalinasNo ratings yet
- Fsurg 08 662720Document6 pagesFsurg 08 662720Deborah SalinasNo ratings yet
- Ambulation Spin Cord InjuryDocument16 pagesAmbulation Spin Cord InjuryDeborah SalinasNo ratings yet
- Ambulation and Parkinson DiseaseDocument22 pagesAmbulation and Parkinson DiseaseDeborah SalinasNo ratings yet
- Adaptacion Emocional de La Perdida de Una ExtremidadDocument22 pagesAdaptacion Emocional de La Perdida de Una ExtremidadDeborah SalinasNo ratings yet
- 10 1016@j Cps 2019 02 006Document9 pages10 1016@j Cps 2019 02 006Deborah SalinasNo ratings yet
- 10 1016@j Jhsa 2018 11 012Document5 pages10 1016@j Jhsa 2018 11 012Deborah SalinasNo ratings yet
- HandbookNeurorehabilitation UnknownDocument195 pagesHandbookNeurorehabilitation UnknownDeborah SalinasNo ratings yet
- Chappell 2020Document9 pagesChappell 2020Deborah SalinasNo ratings yet
- 10 1016@j Cps 2019 03 008Document10 pages10 1016@j Cps 2019 03 008Deborah SalinasNo ratings yet
- 10.1007@s40520 015 0497 yDocument8 pages10.1007@s40520 015 0497 yDeborah SalinasNo ratings yet
- Imporving Orientation in Head Injued Adults by Repeat Parctice Multisensory Input and Peer ParticipátionDocument10 pagesImporving Orientation in Head Injued Adults by Repeat Parctice Multisensory Input and Peer ParticipátionDeborah SalinasNo ratings yet
- Assistive Devices For AmbulationDocument13 pagesAssistive Devices For AmbulationDeborah Salinas100% (1)
- AMBULATIONDocument12 pagesAMBULATIONDeborah SalinasNo ratings yet
- Gaitan 1 PDFDocument12 pagesGaitan 1 PDFDeborah SalinasNo ratings yet
- Falls, Aging and DisabilityDocument17 pagesFalls, Aging and DisabilityDeborah SalinasNo ratings yet
- Agingwithmuscular Dystrophy: Pathophysiologyand ClinicalmanagementDocument22 pagesAgingwithmuscular Dystrophy: Pathophysiologyand ClinicalmanagementDeborah SalinasNo ratings yet
- University of Santo Tomas Senior High School Documentation of Ust'S Artworks Through A Walking Tour Brochure and Audio GuideDocument30 pagesUniversity of Santo Tomas Senior High School Documentation of Ust'S Artworks Through A Walking Tour Brochure and Audio GuideNathan SalongaNo ratings yet
- 1 STCW OverviewDocument19 pages1 STCW OverviewJosh SebastianNo ratings yet
- Brand ManagementDocument4 pagesBrand ManagementahmadmujtabamalikNo ratings yet
- Compania de Naveira Nedelka Sa V Tradex Internacional SaDocument3 pagesCompania de Naveira Nedelka Sa V Tradex Internacional SaAbhishek RaiNo ratings yet
- International Council For Management Studies (ICMS), Chennai (Tamilnadu) Chennai, Fees, Courses, Admission Date UpdatesDocument2 pagesInternational Council For Management Studies (ICMS), Chennai (Tamilnadu) Chennai, Fees, Courses, Admission Date UpdatesAnonymous kRIjqBLkNo ratings yet
- Chapter 7 Double Entry System: Very Short QuestionsDocument3 pagesChapter 7 Double Entry System: Very Short QuestionsVipulNo ratings yet
- 28 ESL Discussion TopicsDocument21 pages28 ESL Discussion TopicsMaruthi Maddipatla50% (2)
- New GAP Algorithm Draft 4-7-19Document1 pageNew GAP Algorithm Draft 4-7-19Umber AgarwalNo ratings yet
- Sepak TakrawDocument39 pagesSepak TakrawRandy Gasalao100% (2)
- Rose Doe v. The City of New York, Et. Al.Document57 pagesRose Doe v. The City of New York, Et. Al.Daily Caller News FoundationNo ratings yet
- Lesson 7Document20 pagesLesson 7rj libayNo ratings yet
- Environmental Mercury and Its Toxic Effects: ReviewDocument10 pagesEnvironmental Mercury and Its Toxic Effects: ReviewZusely Garcia SanchezNo ratings yet
- Fall 2012 - BIOL 115 - Essential BiologyDocument3 pagesFall 2012 - BIOL 115 - Essential BiologycreativelyinspiredNo ratings yet
- Peckiana Peckiana Peckiana Peckiana PeckianaDocument29 pagesPeckiana Peckiana Peckiana Peckiana PeckianaWais Al-QorniNo ratings yet
- Architectural Theory: Charles Jencks: Modern Movements in ArchitectureDocument32 pagesArchitectural Theory: Charles Jencks: Modern Movements in ArchitectureBafreen BnavyNo ratings yet
- Dakshina - Kannada - Brochure 2012Document28 pagesDakshina - Kannada - Brochure 2012maheshanischithaNo ratings yet
- The Period of Suppressed NationalismDocument9 pagesThe Period of Suppressed Nationalismkbj_batch0980% (5)
- May 6, 2016 Strathmore TimesDocument28 pagesMay 6, 2016 Strathmore TimesStrathmore TimesNo ratings yet
- Portable Lamps & Converters: W 276 LEDDocument2 pagesPortable Lamps & Converters: W 276 LEDRaghu paryNo ratings yet
- Folding Standards: GeneralDocument9 pagesFolding Standards: GeneralNaadiyah JauharaNo ratings yet
- Leonard Peltier Open Letter - Feb. 6, 2024Document3 pagesLeonard Peltier Open Letter - Feb. 6, 2024jen_benderyNo ratings yet
- Chinese Class Survey (Completed)Document4 pagesChinese Class Survey (Completed)Yibing ZhangNo ratings yet
- C. Ra 6969 - Engr. Czes BongcoDocument87 pagesC. Ra 6969 - Engr. Czes Bongcorandell vasquezNo ratings yet
- Cost Accounting Name: - ActivitiesDocument2 pagesCost Accounting Name: - ActivitiesJosh AlvarezNo ratings yet
- Choreography Proposal: Dance Ensemble 2023: Choreographer'S InformationDocument6 pagesChoreography Proposal: Dance Ensemble 2023: Choreographer'S InformationTrey ErnyNo ratings yet
- Evaluating WebsitesDocument2 pagesEvaluating Websitesapi-322361374No ratings yet
- 5 Brilliant Depictions of Lucifer in Art From The Past 250 YearsDocument1 page5 Brilliant Depictions of Lucifer in Art From The Past 250 Yearsrserrano188364No ratings yet
- Contoh Formal LetterDocument2 pagesContoh Formal LetterFairos Azmi MarzahNo ratings yet
- CP16 Risk AssessmentDocument1 pageCP16 Risk AssessmentJulia KaouriNo ratings yet