Professional Documents
Culture Documents
2007 - SSRI in Pregnancy in Netherlands
2007 - SSRI in Pregnancy in Netherlands
Uploaded by
otnayibor1Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2007 - SSRI in Pregnancy in Netherlands
2007 - SSRI in Pregnancy in Netherlands
Uploaded by
otnayibor1Copyright:
Available Formats
British Journal of Clinical DOI:10.1111/j.1365-2125.2007.03048.
Pharmacology
Correspondence
Increase in use of selective Professor Lolkje T. W. de Jong van den
Berg, PharmD, PhD, Social Pharmacy,
Pharmacoepidemiology and
serotonin reuptake inhibitors Pharmacotherapy, Groningen University
Institute for Drug Exploration (GUIDE),
University of Groningen, Ant. Deusinglaan
in pregnancy during the last 1, 9713 AV Groningen, the Netherlands.
Tel: + 3150 363 7576
Fax: + 3150 363 2772
decade, a population-based E-mail: l.t.w.de.jong-van.den.berg@rug.nl
----------------------------------------------------------------------
Keywords
cohort study from the drug utilization, exposure rate, pregnancy,
selective serotonin reuptake inhibitors
Netherlands ----------------------------------------------------------------------
Received
27 April 2007
1 1
Marian K. Bakker, Pieternel Kölling, Paul B. van den Berg, Accepted
4 April 2007
Hermien E. K. de Walle & Lolkje T. W. de Jong van den Berg1
Published OnlineEarly
EUROCAT registration of congenital anomalies, Department of Genetics, University Medical Centre 22 October 2007
Groningen, University of Groningen, and 1Social Pharmacy, Pharmacoepidemiology and
Pharmacotherapy, Groningen University Institute for Drug Exploration (GUIDE), University of
Groningen, Groningen, the Netherlands
WHAT IS ALREADY KNOWN ABOUT
THIS SUBJECT
• Recently, the use of selective serotonin AIMS
reuptake inhibitors (SSRIs), particularly Recent case–control studies suggest a relationship between the use of
selective serotonin reuptake inhibitors (SSRIs) and the occurrence of
paroxetine, in pregnancy has been
birth defects and other adverse pregnancy outcomes. The aim was to
associated with an increased risk on specific determine the extent of the use of SSRIs before and during pregnancy
birth defects or other adverse pregnancy and its trend over the years 1995–2004 in the Netherlands.
outcomes.
• However, the extent of SSRI use in METHODS
pregnancy is largely unknown. The study was performed with data from a population-based
prescription database. Within this database, women giving birth to a
child between 1995 and 2004 were identified. The exposure rate and
95% confidence interval (CI) were calculated as the number of
WHAT THIS STUDY ADDS pregnancies per 1000 that were exposed to an SSRI in a defined period
• In the last decade the use of SSRIs in the year (per trimester or in the year preceding delivery). Exposure rates were
calculated for 2-year periods: 1995/1996, 1997/1998, 1999/2000,
preceding delivery has increased twofold.
2001/2002 and 2003/2004. Trends in exposure rates were analysed
• This increase runs parallel with the increase using the c2 test for trend.
in use of SSRIs among women of fertile age.
• Paroxetine is one of the most commonly RESULTS
used SSRIs. Included were 14 902 pregnancies for which complete pharmacy
• Only recently have sufficient data become records were available from 3 months before pregnancy until delivery.
available on the use of paroxetine to detect A total of 310 pregnancies were exposed to an SSRI in the year
preceding delivery. The exposure rate increased from 12.2 (95% CI 7.0,
moderate increased risks for specific
19.8) in 1995/1996 to 28.5 (95% CI 23.0, 34.9) in 2003/2004.
malformations.
• The safety of SSRIs which are less frequently CONCLUSION
used is not yet established. There has been a significant increase in the use of SSRIs among
• Case–control birth defect-monitoring pregnant women in the Netherlands over the last 10 years, parallel with
systems may be helpful in providing safety the increase in exposure in women of fertile age. In light of the recent
warnings about the use of SSRIs in pregnancy, healthcare professionals
and risk estimates that become more
should be careful in prescribing SSRIs to women planning a pregnancy.
precise as data accumulate for these drugs.
600 / Br J Clin Pharmacol / 65:4 / 600–606 © 2007 The Authors
Journal compilation © 2007 Blackwell Publishing Ltd
Use of SSRIs in pregnancy
Introduction 1 January 1994 were selected. For each child within the
IADB.nl, the female person, 15–50 years older than the
Occurrence of significant depressive symptoms and major child and with the same address code, is considered to be
depressive disorders is not uncommon in pregnant the mother, provided there are no other female persons in
women. Prevalence rates vary between 7% [1] and 20% [2]. that age range with the same address code. Validation of
Since the introduction of selective serotonin reuptake this method has been described in detail by Schirm et al.
inhibitors (SSRIs) in the 1980s, the prevalent and incident [20]. Using this method, for 35% of the children the mother
use of SSRIs has increased over the use of tricyclic antide- can not be identified, because the mother has a separate
pressants [3]. Several, mostly prospective, cohort studies address code or is registered with another pharmacy. Since
on the use of SSRIs in pregnancy have found no increased the major reason for not identifying the mother is not the
risk of general major congenital malformations [4–6]. lack of pharmacy registration, selection bias towards drug-
Other cohort studies have found adverse pregnancy out- using families seems to be limited.
comes, such as a higher rate of spontaneous abortions [7], Because the actual length of the pregnancy is
lower birth weight and shorter gestation [8] or an unknown, the theoretical conception date was determined
increased proportion of children with minor anomalies [9]. as the date of birth minus 273 days.The length of the preg-
The use of SSRIs in pregnancy has also been associated nancy is therefore standardized at 39 weeks, which can be
with neonatal withdrawal syndrome [10] and with an divided into three trimesters of 13 weeks.
increased risk of persistent pulmonary hypertension [11]. From this pregnancy database all mothers between 15
The results of recent case–control studies suggest that and 49 years of age were selected, who gave birth to a
SSRIs are not major teratogens, but specific SSRIs appear to child between 1995 and 2004 and for whom complete
increase modestly the risk of various specific (cardiac) mal- data were available on the year preceding delivery
formations [12–17]. (13 weeks before the theoretical conception date until
Since clear data on the prevalence of SSRI use in preg- delivery). The 13 weeks before conception will be referred
nancy over the last decade are limited, we set out to deter- to as trimester 0 and the trimesters in pregnancy as trimes-
mine the extent of SSRI use in the trimester before ters 1, 2 and 3.
pregnancy and during the different trimesters in preg- Prescriptions for SSRIs were identified by ATC codes
nancy and to analyse the trend of its use over the years starting with N06AB. The theoretical period of use was cal-
1995–2004 based on data available for the Netherlands. culated for each prescription for SSRIs, based on the date of
dispensing, the quantity dispensed and the dose regimen.
The exposure rate was then calculated as the number of
Methods pregnancies per 1000 pregnancies that were in theory
exposed to an SSRI in a defined period: women who
For this study data from the Interaction Database (IADB.nl) received a prescription in one trimester which was
were used. The IADB.nl is a population-based prescription extended into the next trimester were counted in both
database which contains data from prescriptions dis- trimesters in which they had had access to the drug. Expo-
pensed from community pharmacies. It covers a popula- sure rates were calculated for 2-year periods: 1995/1996,
tion in the northern and eastern parts of the Netherlands. 1997/1998, 1999/2000, 2001/2002 and 2003/2004.
The database comprised data on approximately 220 000 To compare the exposure rates in the pregnant popu-
people in 1994, and has gradually expanded to data on lation with those in the general population of women of
approximately 500 000 people in 1999. Registration occurs fertile age (15–49 years), the age-standardized 1-year
irrespective of health insurance and is considered repre- exposure rates in women of fertile age were also calculated
sentative of the general population. Each prescription using the 5-year age distribution among the pregnant
record contains information on the name of the drug, the women. The age-standardized 1-year exposure rates were
date of dispensing, the quantity dispensed, the dose averaged over the 2-year periods. The rate ratio was calcu-
regimen and the prescribing physician. The indication for lated as the age-standardized 1-year exposure rate to the
prescribing is not known. All the drugs are coded accord- pregnancy exposure rate.
ing to the Anatomical Therapeutic Chemical (ATC) classifi- The calculation of exposure rates per trimester does
cation system [18]. Each patient has a unique identification not give insight into the patterns of use for individual
number, and date of birth, sex and address code are women. If drugs are prescribed for short-time use, then it is
known. Since most patients restrict their visits to a single in theory possible that for each trimester the exposed
pharmacy, their medication records are virtually complete. pregnancies occur with new users. To study possible
The database does not include information on over-the- changes in the patterns of use in pregnancy we distin-
counter medication and medications dispensed during guished between the following groups: (i) women who
hospitalization [19]. used SSRIs before pregnancy only, (ii) women who used
Within the IADB.nl a pregnancy database has been SSRIs before and continued use in pregnancy, and (iii)
generated. To identify mothers, all children born after women who started use of SSRIs in pregnancy. Patterns of
Br J Clin Pharmacol / 65:4 / 601
M. K. Bakker et al.
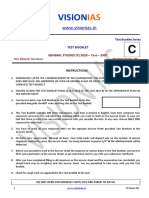
SSRI use were analysed with respect to two time frames: 35.0
Per 1000 pregnancies
birth years 1995–1999 and 2000–2004. 30.0
The defined daily dose (DDD) is the assumed average 25.0
maintenance dose per day for a drug used for its main
20.0
indication in adults. Between the birth years 1995–1999
15.0
and 2000–2004, we compared the total DDDs prescribed in
the year preceding delivery, the total number of days of the 10.0
prescription(s) and the average DDD calculated as the total 5.0
DDDs prescribed, divided by the total number of days of 0.0
the prescription(s) and categorized as ⱕ1 DDD and 95/96 97/98 99/00 01/02 03/04
>1 DDD. Year of birth
Trends in exposure rates over 2-year periods were
analysed in SPSS 12.0 for Windows (Chicago, IL, USA) using Figure 1
the c2 test for trend. Continuous data were analysed using Exposure rate (and 95% confidence interval) for selective serotonin
the T-test for two groups and one-way ANOVA for more reuptake inhibitors per trimester per 1000 pregnancies per 2-year periods
than two groups. The total DDDs prescribed and the total in a cohort of 14 902 pregnancies in the Netherlands (trim 0, (䊐); trim 1,
number of days of the prescriptions were analysed using ( ); trim 2, ( ); trim 3, ( ))
the Mann–Whitney U-test. Proportions were compared
using the c2 test. The 95% confidence interval (CI) for the more than one type of SSRI was used in trimesters 0–3
exposure rates was calculated using the Score method (subsequently). The two most prevalent combinations
with continuity correction for small proportions [21]. were paroxetine and fluoxetine (five pregnancies) and par-
oxetine and fluvoxamine (four pregnancies).
In Figure 1 exposure rates for SSRIs per trimester are
Results shown per 2-year periods. The pattern of use within
periods 0–3 was similar for all 2-year periods. The use of
Within our population, 14 902 pregnancies occurring to SSRIs was highest in the trimester before conception,
10 897 women could be identified between 1995 and decreased in the first trimester and further in the second
2004. For 7432 women (68%), one pregnancy was identi- trimester. The use of SSRIs in the third trimester was com-
fied in the period 1995–2004 and for 3465 women (32%) parable to the use in the second trimester. The decrease in
two or more pregnancies. The maximum number of preg- use over periods 0–3 was statistically significant for all
nancies of one woman was six. The mean maternal age at 2-year periods (1995/1996, c2 for trend = 11.323, P = 0.001;
birth was 29.9 years (SD 4.5). The mean maternal age at 1997/1998, c2 for trend = 25.337, P = 0.000; 1999/2000,
birth differed significantly between the birth years (P = c2 for trend = 33.368, P = 0.000; 2001/2002, c2 for
0.000), from 29.2 years (SD 4.3) in 1995/1996 to 30.1 years trend = 29.503, P = 0.000; 1995/1996, c2 for trend = 21.989,
(SD 4.6) in 2001/2002. P = 0.000). The use of SSRIs showed a significantly increas-
In the year preceding delivery, 455 out of 14 902 preg- ing trend over time for each of the trimesters (trimester 0,
nancies (3.1%) were exposed to an antidepressant (ATC c2 for trend = 21.936, P = 0.000; trimester 1, c2 for
code N06A).The mean age at birth of the women who used trend = 26.038, P = 0.000; trimester 2, c2 for trend = 30.776,
an antidepressant in this period was 30.4 (SD 5.0) and P = 0.000; trimester 3, c2 for trend = 26.186, P = 0.000).
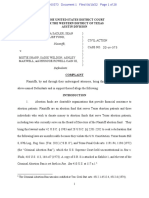
29.9 years (SD 4.5) for women who did not use an antide- In Figure 2 the exposure rate for any use of an SSRI in
pressant before or during pregnancy, respectively (P = the year preceding delivery per 2-year period is presented.
0.043). The exposure rate increased from 12.2 (95% CI 7.0, 19.8)
Exposure to an SSRI (N06AB) in trimester 0–3 occurred per 1000 pregnancies in 1995/1996 to 28.5 (95% CI 23.0,
in 310 pregnancies (2.1%) with 292 women: 274 women 34.9) per 1000 pregnancies in 2003/2004. This increase
with one exposed pregnancy and 18 women with two runs parallel with the increase in use in the general popu-
exposed pregnancies. In the 10-year period, paroxetine lation of women aged 15–49 years. The age-standardized
was the most commonly used SSRI (n = 180, 58.1%), fol- 1-year exposure rate (averaged over 2-year periods) in this
lowed by fluoxetine (n = 67, 21.6%) and fluvoxamine population increased from 36.8 per 1000 in 1995/1996 to
(n = 39, 12.6%). Citalopram and sertraline were the least 75.7 per 1000 in 2003/2004. The rate ratio was 3.0, 4.0, 3.6,
used SSRIs, with 8.4% (n = 26) and 3.5% (n = 11).Among the 3.2 and 2.7 for the respective 2-year periods. Between 1995
exposed pregnancies, the use of paroxetine increased from and 2004, the pregnancy rate in women aged 15–49 years
37.5% (6/16 pregnancies) in 1995/1996 to 60.4% in 2003/ was 13.1 per 1000 person years.
2004 (55/91 pregnancies), whereas the use of fluoxetine Among the women who used SSRIs in the year preced-
and fluvoxamine decreased from 37.5% (6/16) and 31.3% ing delivery (n = 310), 90.0% of the pregnancies were
(5/16), respectively, in 1995/1996 to 19.8% (18/91) and exposed to SSRIs only (including combinations of SSRIs). In
5.5% (5/91), respectively, in 2003/2004. In 13 pregnancies 10.0%, both SSRIs and other types of antidepressants were
602 / 65:4 / Br J Clin Pharmacol
Use of SSRIs in pregnancy
average daily dose prescribed did not change. The most
Exposure rate per 1000
90.0
80.0 commonly prescribed SSRI over the whole study period
70.0 was paroxetine.
60.0 To our knowledge, this study is the first to examine
50.0
40.0 trends in use of SSRIs before and during pregnancy over a
30.0 10-years period.The validity of the exposure rates for use of
20.0 SSRIs in the year preceding delivery is equivalent to the
10.0 age-standardized 1-year exposure rates in women of fertile
0.0
1995/1996 1997/1998 1999/2000 2001/2002 2003/2004 age, since both data derive from the same source popula-
Year tion. We did not adjust for multiple pregnancies per
woman, because we wanted to conduct an observational
study in which each pregnancy was considered as an inde-
Figure 2 pendent event.
Average exposure rate per 2-year period for any use of selective serotonin The use of a population-based prescription database is
reuptake inhibitors in the year preceding delivery (including 95% confi-
dence interval) compared with the average age-standardized 1-year
an important tool in monitoring the use of drugs among
exposure rate per 2-year periods for women of fertile age (15–49 years) pregnant women.The data are recorded prospectively and
(pregnancy, (䊉); women fertile age, age-standardised, ( )) cover prescriptions from different prescribers. The IADB.nl
was gradually expanded between 1994 and 1999 by
including pharmacies from geographical areas not previ-
used. In Table 1 the pattern of SSRI use for pregnancies ously covered. The pharmacies that were added to the
exposed to SSRIs in the year preceding delivery is pre- IADB.nl were representative of the north-eastern region.
sented. Only in 11.6% of the exposed pregnancies did the When the average exposure rates were calculated per
use of SSRIs start in pregnancy. This percentage did not 2-year period for any use of SSRIs in the year preceding
differ between 1995 and 1999 or between 2000 and 2004. delivery restricted to those pharmacies that participated in
However, when we look at the pregnancies in which an the IADB.nl in the first 2 years (1994 and 1995), the results
SSRI had already been used before pregnancy, it can be were comparable to the exposure rates found in Figure 2. It
seen that in the more recent time period continuation of is therefore unlikely that the results of this study have been
SSRI use in pregnancy was more prevalent, with 65.8% vs. influenced by the expansion of the database.
51.9% in the earlier period (P = 0.03). When these analyses There are several limitations in using an administrative
were restricted to those pregnancies in which SSRIs had prescription database, such as the unknown actual use and
already been used before pregnancy and no other types of the standardized length of pregnancy. Since the actual use
antidepressants were used (n = 253), the results were com- is unknown, the exposure rates found in this study are an
parable (65.9% vs. 51.9%). estimate. The use of SSRIs in pregnancy may be an overes-
In 2000–2004 the length of use of SSRIs and the total timation if women stop taking their medication when they
DDDs prescribed were significant higher than in 1995– plan to become pregnant or when they discover they are
1999 (median number of days 99.5 vs. 64, P = 0.008; median pregnant. Also, because the length of the pregnancy was
total DDDs 111.5 vs. 67.5; P = 0.009). The average DDD standardized at 39 weeks, misclassification of exposure is
(average daily dose) in the year preceding delivery varied possible. The use of SSRIs in the first trimester could be an
between 0.3 and 4.0, and 191 women (61.6%) received an overestimation if use in pregnancy is associated with
average DDD of 1.The proportion of women who received preterm birth. From the literature it is not clear if there is a
an average DDD ⱕ1 did not differ between 1995 and 1999 relation between the use of SSRIs and preterm birth. Some
or between 2000 and 2004 with 76.7% and 72.7%, respec- studies have found such an association [9, 22], whereas
tively (Table 1, P = 0.474). others have not [8, 23]. However, definitions of exposure
and preterm birth differ between these studies.
Also, the methodology used to identify mothers and
Discussion pregnancies has its limitations. We were able to identify
approximately 65% of the mothers for children included in
The results of this observational study show that there has the IADB.nl. Since the validated method has a sensitivity of
been a significant increase in the use of SSRIs during preg- 99% [20], it is not to be expected that nonpregnant women
nancy in the Netherlands over the last 10 years. The were misclassified as being pregnant. Failure to identify a
increase in use is present in all trimesters before and pregnancy when the child is known can mostly be attrib-
during pregnancy and runs parallel with the increase in uted to administrative reasons, and selection towards
use of SSRIs in women of fertile age. In addition, in recent drug-using families seems therefore limited. The detection
years continued use of SSRIs from before pregnancy until rate may be improved using less strict criteria. On the other
the first trimester is more frequent along with an increase hand, this would probably lead to an undesirable loss of
in the length of use and the total DDDs prescribed. The sensitivity. Furthermore, pregnancies are not identified if
Br J Clin Pharmacol / 65:4 / 603
M. K. Bakker et al.
Table 1
Pattern of use of SSRIs and average DDD in 1995–1999 and 2000–2004 for pregnancies exposed to an SSRI in period from 3 months before conception until
delivery
Total 1995–1999 2000–2004
n = 310 (100%) n = 90 (100%) n = 220 (100%) P
Use before pregnancy 274 88.4 81 90.0 193 87.7
Use discontinued before theoretical conception date 105 38.3 39 48.1 66 34.2 0.03
Use continued in pregnancy 169 61.7 42 51.9 127 65.8
Start use in pregnancy 36 11.6 9 10.0 27 12.3
Average DDD prescribed
ⱕ1 DDD 229 73.9 69 76.7 160 72.7 0.474
>1 DDD 81 26.1 21 23.3 60 27.3
SSRI, Selective serotonin reuptake inhibitor; DDD, defined daily dose. SSRIs include paroxetine (ATC N06AB05; DDD 20 mg), fluoxetine (ATC N06AB03; DDD 20 mg), fluvoxamine
(ATC N06AB08; DDD 100 mg), citalopram (ATC N06AB04; DDD 20 mg) and sertraline (ATC N06AB06; DDD 50 mg).
they resulted in a spontaneous or induced abortion, a still studies have more statistical power to detect moderately
birth or an early neonatal death or if the child is not (yet) increased risks for specific birth defects than cohort
registered with a pharmacy. A Dutch study on drug use studies.They are more efficient in terms of sample size and
in children, using pharmacy dispensing data from the time. Case–control studies are also sensitive to selection
IADB.nl, has shown that approximately 80% of the children and recall bias, which can be minimized by the choice of an
had used at least one prescription drug (and therefore appropriate control group and the use of prospectively
were registered with a pharmacy) within the first 2 years of collected (pharmacy) data on prenatal medication use.
life [24]. Since it may take some time for a new-born child Since paroxetine is one the most commonly used SSRIs
to be registered with a pharmacy, the number of uniden- among pregnant women, sufficient data are now becom-
tified pregnancies may be larger in more recent than in ing available to detect these moderately increased risks
previous years.This is likely to result in an underestimation for specific congenital malformations [11–13]. The safety
of maternal drug use in more recent years. of SSRIs that are less frequently used has not yet been
The prevalence rates per trimester for use of SSRIs fol- established. It is very important that more data become
lowed the same pattern as for antidepressants in general, available on the safety of the newer antidepressants. Case–
found in a Dutch cohort of 29 005 women giving birth control birth defect-monitoring systems that include
between January 2000 and July 2003 [25]. In this study, the information on prenatal medication use might be helpful
use of antidepressants decreased from 2.9% before preg- in providing these safety and risk estimates. As data accu-
nancy to 2.1% in the first trimester and 1.8% in the second mulate, the risk estimates for these drugs will become
and third trimesters. Paroxetine was the most commonly more precise [28].
used antidepressant (approximately 47% of all antidepres- The decision whether to use antidepressants in preg-
sants used). Reefhuis et al. [26] have found a prevalence of nancy should be taken after careful consideration of the
SSRI use of 2.8% among a cohort of 4094 mothers who benefits and risks for both mother and child. In some cases
gave birth to a healthy child between October 1997 and the benefits of treatment may well outweigh the teratoge-
December 2002. The data were obtained from a nic risks. Untreated depression in pregnancy appears to
population-based case–control study of congenital carry substantial perinatal risks, such as preterm birth,
anomalies, conducted in eight states in the USA. Self restricted fetal growth, preeclampsia, spontaneous abor-
reported measures were used. That prevalence of use is tions and delayed cognitive and emotional development.
comparable to that (2.9%) in a matched control group con- These adverse effects may be caused by psychopathologi-
sisting of mothers of a healthy child found in a study by cal events which have physiological effects on the fetus.
Chambers et al. [11], and estimates from both studies were Depression may also lead to unhealthy behaviour that can
somewhat higher than in our study (i.e. 2.1%). The higher indirectly affect the outcome of the pregnancy [29]. Also, a
use can be explained by the fact that, in general, use of recent cohort study has found that women who discon-
antidepressants is higher in the USA. tinue antidepressant medication close to conception
In the late 1990s a number of prospective cohort experience more frequent relapses of major depression
studies were published which did not find an increased during pregnancy than those who maintain their medica-
overall risk of major congenital malformations after the use tion [30].
of SSRIs in pregnancy [4, 6, 9, 27]. However, most of these The American College of Obstetricians and Gynaecolo-
cohort studies lacked sufficient power to detect increased gists has recently recommended that treatment with all
risk of specific congenital malformations. Case–control SSRIs during pregnancy should be individualized, and par-
604 / 65:4 / Br J Clin Pharmacol
Use of SSRIs in pregnancy
oxetine use among pregnant women or women planning 9 Chambers CD, Johnson KA, Dick LM, Felix RJ, Jones KL. Birth
a pregnancy should be avoided, if possible. Women of outcomes in pregnant women taking fluoxetine. N Engl J
fertile age who take SSRIs should be advised to consult a Med 1996; 335: 1010–5.
specialist before they become pregnant to develop a treat- 10 Sanz EJ, las-Cuevas C, Kiuru A, Bate A, Edwards R. Selective
ment plan regarding their condition and the use of SSRIs, in serotonin reuptake inhibitors in pregnant women and
which risks and benefits for mother and child are well con- neonatal withdrawal syndrome: a database analysis. Lancet
sidered [31]. In the Netherlands, where 80% of pregnancies 2005; 365: 482–7.
are planned, it should then be possible to avoid the unnec- 11 Chambers CD, Hernandez-Diaz S, Van Marter LJ, Werler MM,
essary use of SSRIs in pregnancy as much as possible. Louik C, Jones KL, Mitchel AA. Selective serotonin-reuptake
inhibitors and risk of persistent pulmonary hypertension of
the newborn. N Engl J Med 2006; 354: 579–87.
12 GlaxoSmithKline Clinical Trial Register. Epidemiology Study:
Competing interests Preliminary Report on Bupropion in Pregnancy and the
Occurrence of Cardiovascular and Major Congenital
P.K. has been reimbursed by Eli Lilly, the manufacturer of Malformation. Available at http://ctrgskcouk/Summary/
fluoxetine, and Jansen Cilag/Organon, the manufacturer of paroxetine/epip083.pdf Last accessed 15 November
mirtazepine, for attending several conferences, and has 2005.
been paid by GlaxoSmithKline, manufacturer of paroxet- 13 Kallen B, Otterblad Olausson P. Antidepressant drugs during
ine, and by Pfizer, the manufacturer of sertraline, for pregnancy and infant congenital heart defect. Reprod
running educational programmes. All other authors Toxicol 2006; 21: 221–2.
declare they have no conflict of interests to declare. 14 Wogelius P, Norgaard M, Gislum M, Pedersen L, Munk E,
Mortensen PB, Lipworth L, Toft Sorensen H. Maternal use of
selective serotonin reuptake inhibitors and risk of
congenital malformations. Epidemiology 2006; 17: 701–4.
15 Berard A, Ramos E, Rey E, Blais L, St-Andre M, Oraichi D. First
REFERENCES trimester exposure to paroxetine and risk of cardiac
1 Bennett HA, Einarson A, Taddio A, Koren G, Einarson TR. malformations in infants: the importance of dosage. Birth
Prevalence of depression during pregnancy: systematic Defects Res B Dev Reprod Toxicol 2007; 80: 18–27.
review. Obstet Gynecol 2004; 103: 698–709. 16 Alwan S, Reefhuis J, Rasmussen SA, Olney RS, Friedman JM.
Use of selective serotonin-reuptake inhibitors in pregnancy
2 Marcus SM, Flynn HA, Blow FC, Barry KL. Depressive
and the risk of birth defects. N Engl J Med 2007; 356:
symptoms among pregnant women screened in obstetrics
2684–92.
settings. J Womens Health (Larchmt) 2003; 12: 373–80.
17 Louik C, Lin AE, Werler MM, Hernandez-Diaz S, Mitchell AA.
3 Meijer WE, Heerdink ER, Leufkens HG, Herings RM, First-trimester use of selective serotonin-reuptake inhibitors
Egberts AC, Nolen WA. Incidence and determinants of and the risk of birth defects. N Engl J Med 2007; 356:
long-term use of antidepressants. Eur J Clin Pharmacol 2004; 2675–83.
60: 57–61.
18 WHO Collaborating Centre for Drugs Statistics Methodology.
4 Goldstein DJ, Corbin LA, Sundell KL. Effects of first-trimester Available at http://www.whoccno/atcddd/ Last accessed 2
fluoxetine exposure on the newborn. Obstet Gynecol 1997; December 2004.
89 (5 Part 1): 713–8.
19 Tobi H, van den Berg PB, De Jong-van den Berg LTW. The
5 Hendrick V, Smith LM, Suri R, Hwang S, Haynes D, Altshuler L. Interaction Database: synergy of science and practice in
Birth outcomes after prenatal exposure to antidepressant pharmacy. In Medical Data Analysis, eds. Brause RW,
medication. Am J Obstet Gynecol 2003; 188: 812–5. Hanisch E. Berlin: Springerverlag, 2000; 206–11.
6 Kulin NA, Pastuszak A, Sage SR, Schick-Boschetto B, Spivey G, 20 Schirm E, Tobi H, de Jong-van den Berg LT. Identifying
Feldkamp M, Ormond K, Matsui D, Stein-Schechman AK, parents in pharmacy data: a tool for the continuous
Cook L, Brochu J, Rieder M, Koren G. Pregnancy outcome monitoring of drug exposure to unborn children. J Clin
following maternal use of the new selective serotonin Epidemiol 2004; 57: 737–41.
reuptake inhibitors: a prospective controlled multicenter 21 Tobi H, van den Berg PB, de Jong-van den Berg LT. Small
study. JAMA 1998; 279: 609–10. proportions: what to report for confidence intervals?
7 Chun-Fai-Chan B, Koren G, Fayez I, Kalra S, Voyer-Lavigne S, Pharmacoepidemiol Drug Saf 2005; 14: 239–47.
Boshier A, Shakir S, Einarson A. Pregnancy outcome of 22 Wen SW, Yang Q, Garner P, Fraser W, Olatunbosun O,
women exposed to bupropion during pregnancy: a Nimrod C, Walker M. Selective serotonin reuptake inhibitors
prospective comparative study. Am J Obstet Gynecol 2005; and adverse pregnancy outcomes. Am J Obstet Gynecol
192: 932–6. 2006; 194: 961–6.
8 Simon GE, Cunningham ML, Davis RL. Outcomes of prenatal 23 Malm H, Klaukka T, Neuvonen PJ. Risks associated with
antidepressant exposure. Am J Psychiatry 2002; 159: selective serotonin reuptake inhibitors in pregnancy. Obstet
2055–61. Gynecol 2005; 106: 1289–96.
Br J Clin Pharmacol / 65:4 / 605
M. K. Bakker et al.
24 Schirm EBP, Gebben H, Sauer P, de Jong-van den Berg L. 28 Mitchell AA. Systematic identification of drugs that cause
Drug use of children in the community assessed through birth defects – a new opportunity. N Engl J Med 2003; 349:
pharmacy dispensing data. Br J Clin Pharmacol 2000; 50: 2556–9.
473–8.
29 Bonari L, Pinto N, Ahn E, Einarson A, Steiner M, Koren G.
25 Ververs T, Kaasenbrood H, Visser G, Schobben F, Perinatal risks of untreated depression during pregnancy.
de Jong-van den Berg Egberts T. Prevalence and patterns of Can J Psychiatry 2004; 49: 726–35.
antidepressant drug use during pregnancy. Eur J Clin
Pharmacol 2006; 62: 863–70. 30 Cohen LS, Altshuler LL, Harlow BL, Nonacs R, Newport DJ,
26 Reefhuis J, Rasmussen SA, Friedman JM. Selective Viguera AC, Suri R, Burt VK, Hendrik V, Reminick AM,
serotonin-reuptake inhibitors and persistent pulmonary Loughead A, Vitonis AF, Stowe ZN. Relapse of major
hypertension of the newborn. N Engl J Med 2006; 354: depression during pregnancy in women who maintain or
2188–90. discontinue antidepressant treatment. JAMA 2006; 295:
499–507.
27 Pastuszak A, Schick-Boschetto B, Zuber C, Feldkamp M,
Pinelli M, Sihn S, Donnenfeld A, McCormack M, 31 ACOG Committee on Obstetric Practice. ACOG Committee
Leen-Mitchell M, Woodland C, Gardner A, Hom M, Koren G. Opinion No. 354: treatment with selective serotonin
Pregnancy outcome following first-trimester exposure to reuptake inhibitors during pregnancy. Obstet Gynecol 2006;
fluoxetine (Prozac). JAMA 1993; 269: 2246–8. 108: 1601–3.
606 / 65:4 / Br J Clin Pharmacol
You might also like
- Hesi Review For Health AssessmentDocument18 pagesHesi Review For Health AssessmentJennifer Portillo100% (19)
- Nas Poster FinalDocument1 pageNas Poster Finalapi-545031607No ratings yet
- Causes and Effects of Teenage Pregnancy Among The Female Students and Its Effect On Academic PerformanceDocument12 pagesCauses and Effects of Teenage Pregnancy Among The Female Students and Its Effect On Academic Performancegrossarchive75% (8)
- 2007 - Use of Antidepressants in Pregnancy in The USDocument5 pages2007 - Use of Antidepressants in Pregnancy in The USotnayibor1No ratings yet
- Journal Pone 0165122Document26 pagesJournal Pone 0165122afriska chandraNo ratings yet
- Drug Prescription Patterns Before, During and After Pregnancy For Chronic, Occasional and Pregnancy-Related Drugs in The NetherlandsDocument10 pagesDrug Prescription Patterns Before, During and After Pregnancy For Chronic, Occasional and Pregnancy-Related Drugs in The NetherlandsDrAnisha PatelNo ratings yet
- F. Etwel Et Al 2014Document8 pagesF. Etwel Et Al 2014reclinpharmaNo ratings yet
- Isoxuprine VS Terbutaline in Pre-Term Labor TocolysisDocument29 pagesIsoxuprine VS Terbutaline in Pre-Term Labor TocolysisGarry Kin CamarilloNo ratings yet
- Pregnancy Rate After Emergency Contraception With Single-Dose Oral Levonorgestrel in Japanese WomenDocument7 pagesPregnancy Rate After Emergency Contraception With Single-Dose Oral Levonorgestrel in Japanese WomenAnugerahIndahMarethaNo ratings yet
- Handal Et al-2016-BJOG: An International Journal of Obstetrics & GynaecologyDocument10 pagesHandal Et al-2016-BJOG: An International Journal of Obstetrics & GynaecologyPrima Hari PratamaNo ratings yet
- Continuation Rates of Oral Hormonal Contraceptives in A Cohort of First-Time Users: A Population-Based Registry Study, Sweden 2005 - 2010Document8 pagesContinuation Rates of Oral Hormonal Contraceptives in A Cohort of First-Time Users: A Population-Based Registry Study, Sweden 2005 - 2010Yhoess Mei HadianaNo ratings yet
- Therapeutic Changes of Systemic Lupus Erythematosus (SLE) Patients in Pregnancy and Feto-Maternal Outcomes: A Retrospective Cohort StudyDocument14 pagesTherapeutic Changes of Systemic Lupus Erythematosus (SLE) Patients in Pregnancy and Feto-Maternal Outcomes: A Retrospective Cohort StudyayuNo ratings yet
- Brit J Clinical Pharma - 2015 - Daniel - NSAIDs and Spontaneous Abortions True Effect or An Indication BiasDocument5 pagesBrit J Clinical Pharma - 2015 - Daniel - NSAIDs and Spontaneous Abortions True Effect or An Indication BiasLuis Alberto de la Fuente García PeñaNo ratings yet
- Erythromycin As A Prokinetic Agent in Preterm Neonates: A Systematic ReviewDocument6 pagesErythromycin As A Prokinetic Agent in Preterm Neonates: A Systematic ReviewajescoolNo ratings yet
- Morphine Overdose in A 6 1 - 2 Week-Old Infant - A Case ReportDocument5 pagesMorphine Overdose in A 6 1 - 2 Week-Old Infant - A Case ReportvistaNo ratings yet
- Dosing Interval Between Mifepristone and Misoprostol in Second and Third Trimester TerminationDocument5 pagesDosing Interval Between Mifepristone and Misoprostol in Second and Third Trimester TerminationWILMER HUANGANo ratings yet
- Long Term Effects Neonatal AbstinenceDocument10 pagesLong Term Effects Neonatal AbstinenceChile Crece Contigo HlfNo ratings yet
- Medication Errors & Risk ReductionDocument46 pagesMedication Errors & Risk Reductionadni_wgNo ratings yet
- Mother NejmDocument12 pagesMother NejmIzara Maité Mondragón MorenoNo ratings yet
- Weight Gain and Menstrual Abnormalities Between Users of Depo-Provera and NoristeratDocument6 pagesWeight Gain and Menstrual Abnormalities Between Users of Depo-Provera and NoristeratMauricio Lopez MejiaNo ratings yet
- Pregnancy Rate After Emergency Contraception With Single-Dose Oral Levonorgestrel in Japanese WomenDocument7 pagesPregnancy Rate After Emergency Contraception With Single-Dose Oral Levonorgestrel in Japanese WomenAnugerahIndahMarethaNo ratings yet
- 1238-Article Text-5203-1-10-20220916Document3 pages1238-Article Text-5203-1-10-20220916Sriram NagarajanNo ratings yet
- 1238-Article Text-5203-1-10-20220916Document3 pages1238-Article Text-5203-1-10-20220916srirampharmNo ratings yet
- Levonorgestrel vs. Copper Intrauterine en AnticoncepciónDocument10 pagesLevonorgestrel vs. Copper Intrauterine en AnticoncepciónJose Alejandro Bedoya SanchezNo ratings yet
- Effect of Progestin Compared With Combined Oral.3Document9 pagesEffect of Progestin Compared With Combined Oral.3Dedi SaputraNo ratings yet
- Pi Is 0002937813005139Document5 pagesPi Is 0002937813005139fenskaNo ratings yet
- Article Elsevier Contraception ThymorégulateursDocument5 pagesArticle Elsevier Contraception Thymorégulateursouazzani youssefNo ratings yet
- Gynecology & ObstetricsDocument5 pagesGynecology & ObstetricsAlfadea Irbah APNo ratings yet
- A Systematic Review and Meta Analysis of The Adverse Effects of Levonorgestrel Emergency Oral ContraceptiveDocument26 pagesA Systematic Review and Meta Analysis of The Adverse Effects of Levonorgestrel Emergency Oral ContraceptiveperezhuertalexieNo ratings yet
- Safety of Medicines in Pregnancy: General PrinciplesDocument12 pagesSafety of Medicines in Pregnancy: General PrinciplesAmry Irsyada YusufNo ratings yet
- Calderon Margalit2009Document8 pagesCalderon Margalit2009Aulya ArchuletaNo ratings yet
- Pediatrics 2012 Aja NieDocument7 pagesPediatrics 2012 Aja NiePutu BudiastawaNo ratings yet
- Basic Obstetric PharmacologyDocument24 pagesBasic Obstetric PharmacologyjokosudibyoNo ratings yet
- Isotretinoin Still The Cause of Anxiety For TeratogenicityDocument5 pagesIsotretinoin Still The Cause of Anxiety For TeratogenicityDaniel CastanNo ratings yet
- Singh. NMP Better Result VS DYDDocument2 pagesSingh. NMP Better Result VS DYDRuth RachmawatyNo ratings yet
- Content ServerDocument6 pagesContent ServerJelena VidićNo ratings yet
- Neonatal and Obstetric Risk Assessment (NORA) Pregnancy Cohort Study in SingaporeDocument7 pagesNeonatal and Obstetric Risk Assessment (NORA) Pregnancy Cohort Study in SingaporePremier PublishersNo ratings yet
- 34784898_ The effects of betamethasone on clinical outcome of the late preterm neonates born between 34 and 36 weeks of gestatioDocument5 pages34784898_ The effects of betamethasone on clinical outcome of the late preterm neonates born between 34 and 36 weeks of gestatioaurimeryNo ratings yet
- 14 35 2 PBDocument6 pages14 35 2 PBAnonymous OvAtmoNo ratings yet
- Outcomes of Antiemetic Prophylaxis in Children UndDocument7 pagesOutcomes of Antiemetic Prophylaxis in Children UndquanwuNo ratings yet
- The State of Hormonal Contraception Today: Benefits and Risks of Hormonal Contraceptives: Combined Estrogen and Progestin ContraceptivesDocument5 pagesThe State of Hormonal Contraception Today: Benefits and Risks of Hormonal Contraceptives: Combined Estrogen and Progestin ContraceptivesDeviNo ratings yet
- s10549 005 5701 XDocument11 pagess10549 005 5701 XJIAQI MagicNo ratings yet
- The Effects of Betamethasone On Clinical Outcome of The Late Preterm Neonates Born Between 34 and 36 Weeks of GestationDocument17 pagesThe Effects of Betamethasone On Clinical Outcome of The Late Preterm Neonates Born Between 34 and 36 Weeks of GestationjeffyNo ratings yet
- Comportamiento 2Document9 pagesComportamiento 2JUAN GARCIANo ratings yet
- 1 s2.0 S1744165X07000029 MainDocument8 pages1 s2.0 S1744165X07000029 MainMike MwangiNo ratings yet
- Neonatal PharmacologyDocument61 pagesNeonatal PharmacologyAnaNo ratings yet
- 1 s2.0 S0920996420301584 MainDocument10 pages1 s2.0 S0920996420301584 MainAndreaNo ratings yet
- Evidencebased PracticeDocument10 pagesEvidencebased Practicerevathidadam55555No ratings yet
- A Study To Assess The Knowledge Regarding Teratogens Among The Husbands of Antenatal Mother Visiting Obstetrics and Gynecology OPD of Sharda Hospital, Greater Noida, UpDocument5 pagesA Study To Assess The Knowledge Regarding Teratogens Among The Husbands of Antenatal Mother Visiting Obstetrics and Gynecology OPD of Sharda Hospital, Greater Noida, UpInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Society of Family Planning Clinical Recommendation - 6Document16 pagesSociety of Family Planning Clinical Recommendation - 6Desiska PriciliaNo ratings yet
- Postpartum Mood DisordersDocument33 pagesPostpartum Mood Disorderstanmai nooluNo ratings yet
- Prescribing in PregnancyDocument2 pagesPrescribing in Pregnancymedical studentNo ratings yet
- Medication Related Problem ArticleDocument11 pagesMedication Related Problem ArticleSTERNNo ratings yet
- Focus Paper PregDocument12 pagesFocus Paper PregMaria Magdalena DumitruNo ratings yet
- The Use of Chinese Herbal Medicines Throughout TheDocument12 pagesThe Use of Chinese Herbal Medicines Throughout TheWindy MuldianiNo ratings yet
- Obstetric Outcomes and Effects On Babies Born To Women Treated For Epilepsy During Pregnancy in A Resource Limited Setting: A Comparative Cohort StudyDocument11 pagesObstetric Outcomes and Effects On Babies Born To Women Treated For Epilepsy During Pregnancy in A Resource Limited Setting: A Comparative Cohort StudyMia AishaNo ratings yet
- Paediatrica Indonesiana: Made Sukmawati, Rinawati Rohsiswatmo, Rulina Suradi, Pramita GayatriDocument12 pagesPaediatrica Indonesiana: Made Sukmawati, Rinawati Rohsiswatmo, Rulina Suradi, Pramita GayatriKevinNo ratings yet
- A Review of Sleep-Promoting Medications Used in PregnancyDocument14 pagesA Review of Sleep-Promoting Medications Used in PregnancyDanitza YhovannaNo ratings yet
- The Safety of Metoclopramide Use in The First Trimester of PregnancyDocument8 pagesThe Safety of Metoclopramide Use in The First Trimester of PregnancyINDAH DWI MENTARINo ratings yet
- 2021, Zipursky USO de OPIOIDES Na GRAVIDEZ - EMERGÊNCIA de Uma CRISE de SAÚDE - GESTANTEDocument9 pages2021, Zipursky USO de OPIOIDES Na GRAVIDEZ - EMERGÊNCIA de Uma CRISE de SAÚDE - GESTANTELetícia Faria LealNo ratings yet
- Optimal Timing of Antenatal Corticosteroid Administration and Preterm Neonatal and Early Childhood OutcomesDocument7 pagesOptimal Timing of Antenatal Corticosteroid Administration and Preterm Neonatal and Early Childhood OutcomesMamet Celine W LindaNo ratings yet
- Taking Medicines in Pregnancy: What’s Safe and What’s Not - What The Experts SayFrom EverandTaking Medicines in Pregnancy: What’s Safe and What’s Not - What The Experts SayNo ratings yet
- Provisional Combined Merit List of Candidates Applied For MDS Courses Under NEET PG 2021Document11 pagesProvisional Combined Merit List of Candidates Applied For MDS Courses Under NEET PG 2021pkv2302No ratings yet
- Franchesca and Ria Final Thesis Revision (May 3 2022) UPDATEDDocument165 pagesFranchesca and Ria Final Thesis Revision (May 3 2022) UPDATEDBianca CamangianNo ratings yet
- Blockchain and COVID-19 Pandemic: Applications and ChallengesDocument20 pagesBlockchain and COVID-19 Pandemic: Applications and ChallengesSameerNo ratings yet
- De Cuong On ThiDocument74 pagesDe Cuong On ThiMoney MathNo ratings yet
- Rights of LGBT Persons EthiopiaDocument5 pagesRights of LGBT Persons Ethiopiajemberu gelchuNo ratings yet
- Opium: Retail and Wholesale Prices and Purity Levels: Breakdown by Drug, Region and Country or TerritoryDocument19 pagesOpium: Retail and Wholesale Prices and Purity Levels: Breakdown by Drug, Region and Country or TerritoryboombaNo ratings yet
- Review of Literature Patient SatisfactionDocument5 pagesReview of Literature Patient Satisfactioneldcahvkg100% (1)
- COVID-19 The Great Reset - A Review Review of KlauDocument4 pagesCOVID-19 The Great Reset - A Review Review of KlauILHAM MARTA DINATANo ratings yet
- Vision: WWW - Visionias.inDocument18 pagesVision: WWW - Visionias.inamitNo ratings yet
- GOLD 2023 Teaching Slide Set v1.0 1nov2022Document59 pagesGOLD 2023 Teaching Slide Set v1.0 1nov2022Nattapatt LimloustrakulNo ratings yet
- Doctors WGHDocument6 pagesDoctors WGHsubham.sharmaNo ratings yet
- PB Mental Health Snapshot 4Document5 pagesPB Mental Health Snapshot 4amanda wuNo ratings yet
- Topic 1.4 - User-Requirement and Perception of SpaceDocument8 pagesTopic 1.4 - User-Requirement and Perception of SpaceCarlo PascuaNo ratings yet
- Abdominal Acupuncture For DepressionDocument35 pagesAbdominal Acupuncture For DepressionAGNESE YOLOTZIN OLIVERA TORO REYESNo ratings yet
- ZEBRA Pen SDS R 301Document6 pagesZEBRA Pen SDS R 301chusqueteNo ratings yet
- Group Name 2 English ClubDocument10 pagesGroup Name 2 English ClubWill HensNo ratings yet
- Zone 2 WorkshopDocument58 pagesZone 2 Workshoprehaangulati2009No ratings yet
- ANCC NCPD ManualDocument58 pagesANCC NCPD Manualshadi alshadafanNo ratings yet
- Uncertainity Illness Theory (Merle H.mishel)Document50 pagesUncertainity Illness Theory (Merle H.mishel)Taate Mohammed100% (1)
- ReseachDocument20 pagesReseachLila GrayNo ratings yet
- Question Bankindian Ethos in Management Sem Vi 2019-2020 Mock TestDocument2 pagesQuestion Bankindian Ethos in Management Sem Vi 2019-2020 Mock TestShubhada AmaneNo ratings yet
- Chapter 8 Hospital Pharmacy Notes Complete Notes by Noteskarts Acc To ER20Document20 pagesChapter 8 Hospital Pharmacy Notes Complete Notes by Noteskarts Acc To ER20Shamant TNo ratings yet
- TBT-14 Personal Protective Equipments Week-12Document3 pagesTBT-14 Personal Protective Equipments Week-12saad aliNo ratings yet
- Medial Epicondylitis (Golfer's Elbow) - Shoulder & Elbow - OrthobulletsDocument8 pagesMedial Epicondylitis (Golfer's Elbow) - Shoulder & Elbow - OrthobulletsSylvia GraceNo ratings yet
- Msds Acetyl ChlorideDocument6 pagesMsds Acetyl ChlorideghungrudswapnilNo ratings yet
- Davis v. Sharp ComplaintDocument30 pagesDavis v. Sharp ComplaintWashington Free BeaconNo ratings yet
- Criteria For SQF AuditorsDocument10 pagesCriteria For SQF AuditorsognavaNo ratings yet
- IX CBSE Holiday WorksheetDocument47 pagesIX CBSE Holiday WorksheetRohan KumarNo ratings yet