Professional Documents
Culture Documents
Ent H&P
Ent H&P
Uploaded by
araagh090 ratings0% found this document useful (0 votes)
4 views2 pagesThis document provides guidance on completing an ENT history and physical exam. It lists the key components to include in the history such as age, gender, comorbidities, surgical history, chief complaint, symptoms of involved ENT systems, smoking history, medications. It then describes common symptoms of the ear, nose, throat and larynx that should be assessed. The examination section outlines performing otoscopy, rhinoscopy/endoscopy, and laryngoscopy. It concludes with sections for investigations, diagnosis, and treatment that complete the H&P.
Original Description:
Original Title
ENT H&P
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document provides guidance on completing an ENT history and physical exam. It lists the key components to include in the history such as age, gender, comorbidities, surgical history, chief complaint, symptoms of involved ENT systems, smoking history, medications. It then describes common symptoms of the ear, nose, throat and larynx that should be assessed. The examination section outlines performing otoscopy, rhinoscopy/endoscopy, and laryngoscopy. It concludes with sections for investigations, diagnosis, and treatment that complete the H&P.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
0 ratings0% found this document useful (0 votes)
4 views2 pagesEnt H&P
Ent H&P
Uploaded by
araagh09This document provides guidance on completing an ENT history and physical exam. It lists the key components to include in the history such as age, gender, comorbidities, surgical history, chief complaint, symptoms of involved ENT systems, smoking history, medications. It then describes common symptoms of the ear, nose, throat and larynx that should be assessed. The examination section outlines performing otoscopy, rhinoscopy/endoscopy, and laryngoscopy. It concludes with sections for investigations, diagnosis, and treatment that complete the H&P.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
You are on page 1of 2
ENT H&P
You need to mention the following items in the history part :
1. Age
2. Gender
3. Comorbidities
4. Surgical history ( Example : 23 yo male , k/c of bronchial asthma ,
post FESS surgery / or post tympanoplasty / or no H/O previous
surgery)
5. Main complaint : then analyze the complaint ((onset, course ,
duration , uni or bilateral …..etc ))
6. Ask about the symptoms of involved system and analyze it if
present
7. Ask about symptoms of other ENT systems
8. h/o smoking , recent infection , recent trauma
9. medication
EAR: hearing loss , otorrhea ( ear discharge ) , pain , vertigo ,
tinnitus
Nose : nasal obstruction , Mouth breathing , Snoring ,
Anosmia/hyposmia/ , taste disturbances, Nasal discharge , post
nasal drip , Allergic symptoms ( Sneezing , Itchy and watery
eyes , Clear rhinorrhea ), Facial pain , Headaches
Throat : Mouth breathing , Snoring , recurrent tonsillitis ( how
many times /year)
Larynx : dysphonia ( hoarsness ) , stridor , Choking ,
Aspiration , Dysphagia, Odynophagia , Cough, foreign body
sensation in throat , Frequent throat clearing , Postnasal drip ,
Heartburn , Neck mass, Weight loss
Examination :
Ear : otoscopy , facial nerve , tuning fork
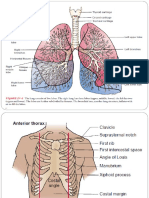
Nose : rhinoscopy or nasal endoscopy
Throat : inspection by togue depressor
Larynx : fibrobtic endoscopy
Investigation
Diagnosis
Treatment
You might also like
- Case Taking Proforma - Respiratory SystemDocument7 pagesCase Taking Proforma - Respiratory SystemK Haynes Raja100% (12)
- (K24) Acute & Chronic LaryngitisDocument47 pages(K24) Acute & Chronic LaryngitisSyarifah Fauziah100% (3)
- Anesthesiology MnemonicsDocument1 pageAnesthesiology MnemonicsMartin Susanto, MD100% (3)
- ENT EXAMINATIONGOOD-instrumentspdfDocument38 pagesENT EXAMINATIONGOOD-instrumentspdfNitin SharmaNo ratings yet
- Ent Eye Osce Totes - YJDocument31 pagesEnt Eye Osce Totes - YJanon_373532435No ratings yet
- Approach To Examination of ENT DisordersDocument39 pagesApproach To Examination of ENT DisordersMohammad SaifullahNo ratings yet
- Ear, Nose and Throat History and ExaminationDocument7 pagesEar, Nose and Throat History and ExaminationStetho Love100% (1)
- Respiratory Osce: AMSA Edinburgh X IMU Y4Document34 pagesRespiratory Osce: AMSA Edinburgh X IMU Y4Abby LiewNo ratings yet
- Ent Case Sheet ProformaDocument8 pagesEnt Case Sheet ProformaDebzz Pradhan100% (4)
- ENT Emergency PresentationDocument135 pagesENT Emergency PresentationshahiruddinNo ratings yet
- ENT - Clinical NotesDocument114 pagesENT - Clinical NotesTANINo ratings yet
- Diagnosis of Acute Rhinitis NewDocument3 pagesDiagnosis of Acute Rhinitis NewNi Wayan Julita KpNo ratings yet
- History Taking and Examination of EarDocument75 pagesHistory Taking and Examination of EarShisam PoudelNo ratings yet
- Ear ExaminationDocument47 pagesEar ExaminationHarshit Bhardwaj100% (4)
- Journal Serak Fix 2Document49 pagesJournal Serak Fix 2Anonymous SeK7brdMc4No ratings yet
- ENT Head and Neck ExamDocument21 pagesENT Head and Neck ExamvickyNo ratings yet
- EntDocument32 pagesEntaini natasha100% (3)
- RespiratoryDocument4 pagesRespiratoryHaliana IzatiNo ratings yet
- Examination of The Ears, Nose, Throat, and Neck: Febryanti P. Sari SP.T.H.T.K.LDocument85 pagesExamination of The Ears, Nose, Throat, and Neck: Febryanti P. Sari SP.T.H.T.K.LRizky PebryanNo ratings yet
- Nose and PNSDocument58 pagesNose and PNSChekole AdaneNo ratings yet
- Review For ENT (2008 Batch)Document9 pagesReview For ENT (2008 Batch)HaslinNo ratings yet
- What Is OtolaryngologyDocument5 pagesWhat Is OtolaryngologyVANSHIKA SINGHNo ratings yet
- Adult 1 Study Guide Exam 2Document7 pagesAdult 1 Study Guide Exam 2Christopher JamesNo ratings yet
- Nasal Obstruction: Meng JuanDocument36 pagesNasal Obstruction: Meng JuanReshma VasuNo ratings yet
- Clerkship - Lecture ENT SEM 7Document117 pagesClerkship - Lecture ENT SEM 7Goh Kah ManNo ratings yet
- EntDocument105 pagesEntNikhil KumarNo ratings yet
- Ent For General PracticeDocument46 pagesEnt For General PracticefenixaNo ratings yet
- Otolaryngology For Medical StudentsDocument112 pagesOtolaryngology For Medical StudentsDrsreeram ValluriNo ratings yet
- 1.md SchoolDocument30 pages1.md Schoolmesay zelekeNo ratings yet
- The Respiratory System: Physical ExaminationDocument24 pagesThe Respiratory System: Physical ExaminationJunina JaferNo ratings yet
- Otology: Ear DischargeDocument5 pagesOtology: Ear DischargeSravan TotakuraNo ratings yet
- Acute Otitis Externa Left Orl HNS RotationDocument34 pagesAcute Otitis Externa Left Orl HNS RotationRash PaltepNo ratings yet
- Common ENT ComplaintsDocument9 pagesCommon ENT ComplaintsHo Yong WaiNo ratings yet
- Assessment of Patients With Repiratory ProblemsDocument33 pagesAssessment of Patients With Repiratory Problemshunter zoneNo ratings yet
- Parts: Nose Throat Pharynx LarynxDocument47 pagesParts: Nose Throat Pharynx LarynxRANJIT GOGOINo ratings yet
- Examination of EarDocument2 pagesExamination of EarMelania ErbghaMoghzietNo ratings yet
- The ENT History and ExaminationDocument11 pagesThe ENT History and ExaminationSuresh MettaNo ratings yet
- Ent History Taking and Examination-1Document16 pagesEnt History Taking and Examination-1Jyotirmayee100% (6)
- Medicine: CardiorespiratoryDocument56 pagesMedicine: CardiorespiratoryWalaa abo foolNo ratings yet
- 5 - Respiratory AssessmentDocument61 pages5 - Respiratory AssessmentAbboud Ali100% (1)
- CSOM Retroauricular FistulaDocument154 pagesCSOM Retroauricular FistulaM.rizki DestiantoroNo ratings yet
- Oh! Sana: Failed Intubation: CausesDocument3 pagesOh! Sana: Failed Intubation: CausesAbdur RahamanNo ratings yet
- Lung ExaminationDocument14 pagesLung Examinationსალომე მუმლაძე “Slay” TMANo ratings yet
- WheezingDocument17 pagesWheezingCk LamaNo ratings yet
- Physiology of Nose & P.N.S.: Dr. Vishal SharmaDocument54 pagesPhysiology of Nose & P.N.S.: Dr. Vishal SharmaE=MC2No ratings yet
- Common Ent Emergencies: University College of Dublin / ST - Vincent's University HospitalDocument41 pagesCommon Ent Emergencies: University College of Dublin / ST - Vincent's University HospitalHakimi JohariNo ratings yet
- Nursing Care Management: The Respiratory SystemDocument80 pagesNursing Care Management: The Respiratory Systemcute_gurljhoanNo ratings yet
- ENT VIVA CompiledDocument4 pagesENT VIVA CompiledhermionewolfgangNo ratings yet
- Final 641 NodayDocument9 pagesFinal 641 Nodaynatalie nodayNo ratings yet
- ENT Case Proforma-EarDocument8 pagesENT Case Proforma-EarGaneshNo ratings yet
- Oxfordmedicaleducation.com-Shortness of Breath HistoryDocument4 pagesOxfordmedicaleducation.com-Shortness of Breath HistorySakshi SinghNo ratings yet
- DR Manpreet Singh Nanda Associate Professor ENT MMMC&H SolanDocument33 pagesDR Manpreet Singh Nanda Associate Professor ENT MMMC&H SolanAmit SinghNo ratings yet
- Med Surg CH 49Document19 pagesMed Surg CH 49amberNo ratings yet
- Sinusite 3Document16 pagesSinusite 3Victor EnachiNo ratings yet
- Casea Omsk W Fas N PalDocument28 pagesCasea Omsk W Fas N PalMegan ShanzuNo ratings yet
- Foreign Body in AirwayDocument32 pagesForeign Body in Airwayana10gab5942No ratings yet
- Assessment of Respiratory SystemDocument18 pagesAssessment of Respiratory SystemIbi Yulia Setyani100% (1)
- Case SInusitis KronikDocument9 pagesCase SInusitis KronikAnnisa TrihandayaniNo ratings yet
- OHNS--Otolaryngology; Head and Neck surgery: pocket field guideFrom EverandOHNS--Otolaryngology; Head and Neck surgery: pocket field guideNo ratings yet