Professional Documents
Culture Documents
Pulmonary Sclerosing Pneumocytoma - A Comprehensive Exploration of Clinical, Radiological, and Surgical Dimensions
Pulmonary Sclerosing Pneumocytoma - A Comprehensive Exploration of Clinical, Radiological, and Surgical Dimensions
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pulmonary Sclerosing Pneumocytoma - A Comprehensive Exploration of Clinical, Radiological, and Surgical Dimensions
Pulmonary Sclerosing Pneumocytoma - A Comprehensive Exploration of Clinical, Radiological, and Surgical Dimensions
Copyright:
Available Formats
Volume 9, Issue 3, March – 2024 International Journal of Innovative Science and Research Technology
ISSN No:-2456-2165 https://doi.org/10.38124/ijisrt/IJISRT24MAR705
Pulmonary Sclerosing
Pneumocytoma - A Comprehensive
Exploration of Clinical, Radiological, and
Surgical Dimensions
Dipendra Pathak1 Xiwen Sun2
MBBS, MD Final year Resident, MD, PhD, Professor and HOD,
Department of Radiology, Shanghai Pulmonary Hospital’ Department of Radiology, Shanghai Pulmonary Hospital’
Tongji University School of Medicine, Shanghai, PR China Tongji University School of Medicine, Shanghai, PR China
Abstract:- I. INTRODUCTION
Objectives: Pulmonary Sclerosing Pneumocytoma (PSP), is a rare
The study findings have important Clinical Benign tumor with malignant potential (1).IT was described
implications, especially in the preoperative evaluation of by Liebow and hubbell in the years 1956(2). Earlier it was
Lung Nodules and aid in the radiological diagnosis based believed to be arised from vascular endothelia cell, latter
on CT features. was proved to be arised from respiratory epithelium,
especially type -2 pneumocytes(3). Although it is regarded
Pulmonary Sclerosing pneumocytoma is a Benign, as the benign tumor, it represents diagnostic challenge due
rare tumor of the lung that represents a diagnostic to unknown etiology and tumor behavior, as well as the
challenge due to the Non-specific CT findings. The Aim variety of the pathohistological findings. This tumor was
of this study was to present a 10-year experience with frequently seen in middle aged female, especially in the fifth
sclerosing pneumocytoma of a large center of CHINA decade(3), It could have been brought about by progesterone
for the diagnosis and treatment of pulmonary diseases, receptors (1). The World Health Organization (WHO)
and to emphasize differential diagnostic dilemmas as a suggested in 2004 that PSH is classified histologically
potential source of errors. differently from other benign tumors, making it an
intermediate tumor with the potential to become
Material and Methods: malignant(4). Primary PSH was formally renamed as PSP
This represents a retrospective study of 31 patients and categorized as a pulmonary adenoma by the WHO in
diagnosed and treated with sclerosing pneumocytoma in 2021(5). Treatment for this type of benign tumor is still up
the 10-year period. The study analyzed various for debate. The primary treatment for pulmonary sclerosing
Variables, including Gender, Age, Smoking history, pneumocytoma was surgery. Sublobectomy, including
Reason for CT, Nodule location, Nodule shape, Clinical mainly segmentectomy and wedge resection, tended to be
symptoms, Calcifications, and Surgical Resections. preferred for peripheral small-sized tumor(6), while
lobectomy could stop the possibility of metastasis and
Results: recurrence, which would worsen the prognosis in the long
Sclerosing pneumocytoma was more frequently run(7).
diagnosed in females (93.5%). The patients ranged in age
from 28 to 68. Most of the patients (77.4%) were The objective of this study was to provide a
asymptomatic. 30 patients had no history of smoking comprehensive analysis of a 10-year period involving
(96.8%). Mean Nodule size was 14.4mm. Most nodules sclerosing pneumocytoma at a prominent medical facility
have Round, oval and smooth margin, with majority of specializing in the diagnosis and treatment of pulmonary
Nodules have location in the lower lobes of both lungs. disorders. Herein, we retrospectively reviewed pulmonary
Most nodules were peripherally situated (54.83%). sclerosing pneumocytoma patients admitted to our center
VATS with lobectomy performed in 25 (80.64%) from 2013 to 2023, aiming to investigate demographic
patients while VATS with wedge resection performed in characteristics, clinical characteristics, CT characteristics
6(19.64%) patients, without post-surgical complications and treatment for patients with pulmonary sclerosing
and Normal follow up. pneumocytoma.
IJISRT24MAR705 www.ijisrt.com 766
Volume 9, Issue 3, March – 2024 International Journal of Innovative Science and Research Technology
ISSN No:-2456-2165 https://doi.org/10.38124/ijisrt/IJISRT24MAR705
II. MATERIALS AND METHODS The picture archiving and communication system applied
axial image adjustments to all photographs. The mediastinal
PSP, treated at the Shanghai Pulmonary Hospital, picture was 450 HU wide, and the lung window image was
Tongji University School of Medicine, are the key subjects 1500 HU wide and -700 HU. PACS displayed all CT
of this study. Retrospective Data between 2013 September imaging data. When patients were laying supine throughout
to December 2023 gathered for this study includes all data the operation, all CT pictures were captured from the apex
from history to medical records. The total number of to the base of the lungs while holding their breath while
patients who participated in this study was 31.A diagnosis of breathing.
PSP was confirmed in all patients via surgical resection.
Statistical Analysis
Demographic Characteristic, Clinical Characteristics All of the collected data was tabulated in Microsoft
and CT characteristics, including Gender, Age, Smoking Excel 2007.The study data sample characteristics were
history, Reason for CT, Nodule location, Nodule shape, assessed by using descriptive statistics parameters which
Clinical symptoms, Calcifications, Surgical Resections and include mean, Median, standard deviations, and percentages.
Immuno-histochemistry was gathered from the patient’s
medical records. III. RESULTS
Inclusion Criteria: The study on patients with pulmonary solitary
pulmonary nodules (PSP) revealed that the mean age was
Presence of a Solid Pulmonary Nodule. 53.5±9.5 years with a standard deviation (SD) of 9.5. PSP
Histological Confirmation: Requires the acquisition of a was commonly observed in individuals aged 29 to 68 years,
verified histological diagnosis through biopsy or surgical with the lowest and highest age in the group being 29 and 68
resection. years, respectively. The age range was categorized into five
The presence of high-quality CT imaging is required . groups, and the majority of patients (90.30%) fell into the
Patient Demographics and Clinical Information: 40-49 (19.35%), 50-59 (35.48%), and 60-69 (35.48%) age
Inclusion criteria encompass instances that possess ranges. The study reported a higher prevalence of PSP in
accessible Demographic Data (Age, Gender) and females, with 29 (93.5%) female patients compared to only
pertinent clinical information, such as Symptoms and 2 (6.5%) male patients, resulting in a female-to-male ratio of
Smoking history. 14.5:1.
Exclusion Criteria: Among the PSP patients, only 1 (3.2%) had a history
of smoking, while 30 (96.8%) had no history of smoking. In
Non-Solid or Sub solid Nodules. terms of presentation, 22 (71.0%) cases were identified
Exclusion of Cases without Histopathological during physical examinations for other reasons; 6 (19.4%)
Confirmation. patients underwent a CT scan after experiencing clinical
symptoms; 2 (6.5%) patients had a CT scan for pre-
Exclusion of Cases with Inadequate CT Imaging Quality.
operative evaluation; and 1 (3.2%) case underwent a CT
CT Protocols scan due to an accident. Symptoms among PSP patients
included cough (3.2%), cough with sputum (9.7%), and 77.4%
Somatom definition AS (Siemens Medical Solutions,
of patients reported no symptoms.
Forchheim, Germany) and Brilliance-64 (Phillips Medical
Systems, the Netherlands) were used for chest CT scans.
Regarding the location of nodules in PSP cases, 17
The scanners came with a 512 X 512 matrix, a 120KVp tube
(54.83%) nodules were peripheral, and 14 (45.16%) were
voltage, a 100-200mAs tube current, a 0.875-1.5mm pith, a
0.625-1.0mm collimation, and a 0.5s rotating speed. A central. The mean PSP nodule diameter was 14.4±4.6 mm
(range, 7–27 mm), with nodules distributed between 1–9
medium sharp reconstruction approach with a thickness of
mm (12.9%), 10–19 mm (74.19%), and 20–29 mm (12.9%).
0.625 to 1.0 millimeters was used to rebuild the images. The
The majority of nodules were observed in the lower lobes of
reconstruction intervals were 5 millimeters thick, with the
the lungs (58.1%).
B50 technique using a 5-millimeter interval without a gap
and the B60 approach using a 1-millimeter reconstruction
Morphological CT characteristics of the nodules
with a 5-millimeter gap. The General Electric CT scanner
showed that 38.7% had oval shapes with smooth and clear
used all of these parameters: Using dose modulation, 120
margins, 32.3% had round shapes with clear margins, 22.6%
kV peak and 100–300 mA are accomplished.
had lobulated shapes, and 6.5% had irregular shapes. Only 3
out of 31 cases exhibited calcification, particularly punctate
The reconstruction intervals were 5 millimeters thick,
with a lung algorithm 5-millimeter interval without a gap calcification. The observed CT values (Hounsfield units)
ranged from 6.34 to 87.96.
and a bone technique 1.25-millimeter reconstruction with a
5-millimeter gap. CT images were generated fifty seconds
In terms of treatment, out of the 31 patients, 25
after intravenous infusion of 100 mL contrast and 50 mL
(80.64%) underwent Video-Assisted Thoracoscopic Surgery
normal saline at 2.5 mL/s using a power injector. The
(VATS) with lobectomy, and 6 (19.36%) had VATS with
supraclavicular to adrenal gland scan range was covered.
wedge resection.
IJISRT24MAR705 www.ijisrt.com 767
Volume 9, Issue 3, March – 2024 International Journal of Innovative Science and Research Technology
ISSN No:-2456-2165 https://doi.org/10.38124/ijisrt/IJISRT24MAR705
Fig 1 Axial and Mediastinal CT View in a 58 years old Female old Female with PSP, Showing the oval, Smooth Margin PSP,27
mm in Longest Diameter Showing the Calcification in the Mediastinal View
Fig 2 Axial and Mediastinal CT of 51 years old Female with PSP Showing Lobulated,
Solid Nodule in the Lower lobe of Left Lungs
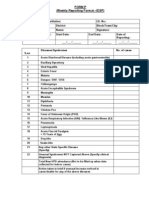
Table 1 Clinical Characteristics of the Patients
Characteristics PSP, (%)
Gender
Male 2(6.5%)
Female 29 (93.5%)
Mean Age 53. 5(29-68)
Age Range (years)
20-29 1(3.22%)
30-39 2(6.45%)
40-49 6(19.35%)
50-59 11(35.48%),
60-69 11(35.48%)
Smoking History
Yes 1(3.2%)
No 30(96.8%)
IJISRT24MAR705 www.ijisrt.com 768
Volume 9, Issue 3, March – 2024 International Journal of Innovative Science and Research Technology
ISSN No:-2456-2165 https://doi.org/10.38124/ijisrt/IJISRT24MAR705
Table 2 Clinical Manifestation
Clinical Manifestation PSP, (%)
Cough 3(9.7%)
Cough, chest pain 0
Cough, fever 1(3.2%)
Cough, sputum 3(9.7%)
Fever, sputum 0
No symptoms 24(77.4%)
Table 3 Manifestation of Lung Lesion at on Set
Location of Lobe
RUL 1 (3.2%)
RML 1 (3.2%)
RLL 1 (3.2%)
LUL 1 (3.2%)
LLL 1 (3.2%)
Mean nodule size (mm) 14.4 (7-27)
Size (mm)
1-9 4 (12.9%)
10-19 23 (74.19%)
20-29 4 (12.9%)
Table 4 CT Findings of Patients with PSP
CT Findings PSP, (%)
Nodule Laterality
Central 14(45.16%)
peripheral 17(54.83%)
Mean Nodule size(mm) 14.4 (7-27)
Shape and Margin
Oval, clear 12(38.7%)
Round, clear 10(32.3%)
Lobulated 7(22.6%)
Irregular 2(6.5%)
calcification 3(9.67%)
CT Value(Hounsfield Unit) 6.34 to 87.96 H.U
Table 5 Surgical Procedure used in PSP
Surgical Procedure N=31, (%)
VATS with lobectomy 25, (80.64%)
VATS with wedge resection 16, (19.34%)
IV. DISCUSSION asymptomatic, and routine chest radiographs often identify
the tumor as a soft-tissue mass incidentally (3). In our study,
Pulmonary sclerosing pneumocytoma is a rare benign two-thirds of patients had no symptoms at all; coughing with
neoplasm originating from type 2 pneumocytes. sputum production was the most common symptom when
the condition was clinically apparent. Besides cough and
Recent studies have reported the female population is sputum, fever was the only presenting symptom. The
affected, mostly occurring in the middle-aged population, presence of unspecific symptoms can be explained by the
with peak incidence in the age group 40–70 years (8, 9). fact that the most frequent location of the nodule is in the
This is similar to our study. The female population is more lung parenchyma. Symptoms are typically caused by the
affected by PSP, with a female-to-male ratio of 14.5:1. The compression of surrounding lung tissue as the mass grows at
mean age of our study was 53.5 ± 9.5 SD. The Asian female a variable rate (8). Usually, the pulmonary parenchyma is
population is the most affected as compared to the western involved in PSP, but there have been a few documented
population (8). Thirty of the thirty patients in our research instances of endobronchial presentation. Typically, the
were nonsmokers. The incidence of smokers and tumor in its endobronchial growth appears as a polypoid
nonsmokers with confirmed PSP varied in other papers that mass with surrounding mucosa that is edematous or
are currently accessible; however, none of this research ulcerative, and there may be necrotic and hemorrhagic
identified smoking as a risk factor or its impact on the regions. Severe respiratory arrest may occur if the tumor
neoplasm's development (9). Most patients are obstructs the lumen due to its development. A bronchoscopy
IJISRT24MAR705 www.ijisrt.com 769
Volume 9, Issue 3, March – 2024 International Journal of Innovative Science and Research Technology
ISSN No:-2456-2165 https://doi.org/10.38124/ijisrt/IJISRT24MAR705
is necessary to reveal this unusual placement. Post- V. CONCLUSION
obstructive pneumonia may result from this tumor if it is not
appropriately detected [11]. In our study, 22 (71.0%) cases A rare, benign lung tumor, pulmonary sclerosing
were found during a physical examination. This proved that pneumocytoma (PSP) mostly affects middle-aged females.
most patients were asymptomatic, and CT was performed Usually asymptomatic, found on routine chest radiographs.
only after a physical examination for other conditions. If symptoms occur, lung tissue compression is involved.
Different nodule sizes contradict size-based symptom
In our study, patients’ greatest diameters ranged from 7 presentation assumptions. Imaging properties (round/oval
to 27 mm; other research indicates that lesions have a forms, smooth edges) suggest benignity but lack specificity.
maximum diameter of 0.3 to 7 cm (3, 8, 12). Some writers Favoring peripheral, lower lung lobe. Calcification
have postulated that because of expansion and the pressure it infrequent, CT density variable. VATS with Lobectomy is
puts on the nearby lung parenchyma, clinical symptoms may preferable due to low complications and no recurrences in
become apparent. Other writers, however, have taken issue our study. Our findings illuminate PSP and emphasize the
with this assumption. However, one of the studies reported need for careful assessment and customized surgery for best
no relationship between the nodule size and the appearance results.
of the clinical symptoms. Among the patients in our group,
the smallest, 7mm, had no symptoms, and the largest, 27 REFERENCES
mm, also had no symptoms. Although lobulated shape
nodule were also noted. The majority of PSP in our study [1]. Devouassoux-Shisheboran M, Hayashi T, Linnoila
appeared in a round or oval form with a smooth edge on an RI, et al. A clinicopathologic study of 100 cases of
unenhanced CT scan. In general, these imaging features pulmonary sclerosing hemangioma with
point to a benign procedure rather than being specific immunohistochemical studies: TTF-1 is expressed in
enough to distinguish PSH from other solitary nodules in the both round and surface cells, suggesting an origin
lung. More than half of the nodules were peripherally from primitive respiratory epithelium. Am J Surg
located in PSP. In terms of the distribution of nodules in Pathol. 2000;24:906–16.
different lobes of the lungs, 16 nodules were located in the [2]. Liebow AA, Hubbell DS. Sclerosing hemangioma
right lung [upper lobe = three, the middle lobe = seven, and (histiocytoma, xanthoma) of the lung. Cancer.
the right lower lobe = eight], and fifteen nodules were 1956;9:53–75.
located in the left lung [upper lobe = five and lower lobe = [3]. Baysak A, Oz AT, Moğulkoç N, et al. A rare tumor
ten]. In this study, we observed the maximum number of of the lung: pulmonary sclerosing hemangioma
lung nodules in the lower lobes of the lung. The lack of (pneumocytoma). Respir Med. 2013;107:448–50
preference for any specific lung lobe was found in a study [4]. Travis WD, Brambilla E, Müller-Hermelink HK, et
that included 28 individuals with a conclusive diagnosis of al. Pathology and Genetics: Tumours of the Lung,
sclerosing pneumocytoma. Of the nodules, the lung's right Pleura, Thymus and Heart. Lyon: IARC; 2004.
upper lobe contained five, the right middle lobe had four, [5]. WHO Classification of Tumours Editorial Board.
the right lower lobe contained six, the left lower lobe WHO classification of tumours. 5th. In: Thoracic
contained nine, and the left upper lobe contained three. (13). Tumours. Lyon: IARC Press; 2021
Our results are consistent with the other report. In our study, [6]. Park JS, Kim K, Shin S, et al. Surgery for Pulmonary
only 3 of the cases had calcification. The fewer incidences Sclerosing Hemangioma: Lobectomy versus Limited
might be due to the nature of solid nodules, which are solid Resection. Korean J Thorac Cardiovasc Surg.
and dense in nature. CT results for the PSP in our study 2011;44:39–43
range from 6.34 to 87.96 H. U, demonstrating nodule [7]. Maeda R, Isowa N, Miura H, et al. Bilateral multiple
density fluctuation. This difference may be due to the sclerosing hemangiomas of the lung. Gen Thorac
nodules' varied tissue compositions, including fibrous tissue, Cardiovasc Surg. 2009;57:667–70.
cellular components, and maybe calcifications. Such [8]. He, C.; Fang, H.; Liu, Y.; Huang, X.; Zhen, W.; Ren,
components can produce variable CT values. Overall, PSP's L. Pulmonary sclerosing hemangioma: Report of two
median CT value of 28.9 shows the dataset's central cases. World J. Surg. Oncol. 2012, 10, 182.
tendency and nodule density. Considering composition [CrossRef] [PubMed]
heterogeneity, it represents the average radiodensity of PSP [9]. Soumil, V.J.; Navin, B.; Sangeeta, D.; Na, J.; Sharma,
lesions. Radiologists and clinicians can use CT values to S.; Deshpande, R. Multiple sclerosing hemangiomas
describe pulmonary lesions and diagnose PSP.In our study of the lung. Asian Cardiovasc. Thorac. Ann. 2004, 12,
26 patients had performed VATS with Lobectomy and only 357–359. [CrossRef] [PubMed]
5 had VATS with wedge resection, Table :5. From our study [10]. Chen, B.; Gao, J.; Chen, H.; Cao, Y.; He, X.; Zhang,
we can conclude VATS with Lobectomy is the widely used W.; Luo, M.; Zhang, S.; Li, W. Pulmonary sclerosing
procedure for the treatment of PSP in our center, reducing hemangioma: A unique epithelial neoplasm of the
the post-operative complications and There is no recurrences lung (report of 26 cases). World J. Surg. Oncol. 2013,
and post follow up complication observed in our study. 11, 85. [CrossRef] [PubMed]
IJISRT24MAR705 www.ijisrt.com 770
Volume 9, Issue 3, March – 2024 International Journal of Innovative Science and Research Technology
ISSN No:-2456-2165 https://doi.org/10.38124/ijisrt/IJISRT24MAR705
[11]. Latif, M.J.; Rahman, G.F.; Connery, C.P. Respiratory
arrest caused by endobronchial sclerosing
hemangioma of the left main bronchus. J. Bronchol.
Interv. Pulmonol. 2009, 16, 188–190. [CrossRef]
[PubMed
[12]. Ekinci, G.H.; Hacıömero ˘glu, O.; Ersev, A.; Alpay,
L.; ¸Sen, A.; Güney, P.A.; Yılmaz, A. Pulmonary
Sclerosing Hemangioma (Pneumocytoma): An
Analysis of 8 Cases. Eurasian J. Pulmonol. 2015, 17,
159–162. [CrossRef]
[13]. Yang, L.; Duan, Y.; Ruan, J.-Z.; Yang, Z.; Wang, Z.-
T. Treatment of 28 patients with sclerosing
hemangioma (SH) of the lung. J. Cardiothorac. Surg.
2012, 7, 9–12. [CrossRef]
IJISRT24MAR705 www.ijisrt.com 771
You might also like
- IDSP P&L FormsDocument2 pagesIDSP P&L FormsKunal YadavNo ratings yet
- Active Cycle Breathing TechniqueDocument20 pagesActive Cycle Breathing TechniqueRAM100% (2)
- What Is HomeoprophylaxisDocument6 pagesWhat Is HomeoprophylaxiswrestlerloverNo ratings yet
- Pul InfectionsDocument5 pagesPul InfectionsSameer VermaNo ratings yet
- The Value of HRCT Chest in Diagnosis of COVID 19 and Its Correlation With RT-PCRDocument5 pagesThe Value of HRCT Chest in Diagnosis of COVID 19 and Its Correlation With RT-PCREditor IJETBSNo ratings yet
- The Accuracy of Ultrasound-Guided Lung Biopsy Pathology andDocument8 pagesThe Accuracy of Ultrasound-Guided Lung Biopsy Pathology andHeru SigitNo ratings yet
- Predicting Lung Nodules MalignancyDocument7 pagesPredicting Lung Nodules MalignancyhajajNo ratings yet
- 06 Pathological Characteristics of FiberopticDocument7 pages06 Pathological Characteristics of FiberopticSaifulhadi BarohNo ratings yet
- Bacciu 2013Document10 pagesBacciu 2013AshokNo ratings yet
- Imaging-Guided Chest Biopsies: Techniques and Clinical ResultsDocument10 pagesImaging-Guided Chest Biopsies: Techniques and Clinical Resultsweni kartika nugrohoNo ratings yet
- Ijcmr 2324 v1 1Document6 pagesIjcmr 2324 v1 1ahsaanillahi9No ratings yet
- Diagnosis and Staging of Lung Carcinoma With CT Scan and Its Histopathological CorrelationDocument7 pagesDiagnosis and Staging of Lung Carcinoma With CT Scan and Its Histopathological CorrelationinesNo ratings yet
- 360 713 1 SMDocument8 pages360 713 1 SMadityachupezNo ratings yet
- 11.2 AP Radiological Evaluation of Various Types of PrimarDocument6 pages11.2 AP Radiological Evaluation of Various Types of PrimardrdivyeshgoswamiNo ratings yet
- The Place of The Department of Pathological Anatomy of The CHU Ibn Rochd Casablanca in The Diagnosis and Classification of Bronchopulmonary CancerDocument6 pagesThe Place of The Department of Pathological Anatomy of The CHU Ibn Rochd Casablanca in The Diagnosis and Classification of Bronchopulmonary CancerInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Cancers 15 03981 v2Document33 pagesCancers 15 03981 v2abhi16243No ratings yet
- JTD 09 07 2178Document8 pagesJTD 09 07 2178Hafiz Hari NugrahaNo ratings yet
- HRCT Profile in Diagnosing Active Pulmonary TuberculosisDocument4 pagesHRCT Profile in Diagnosing Active Pulmonary TuberculosisDiana Dewi PribadiNo ratings yet
- 02 Ultrasound TipsDocument7 pages02 Ultrasound TipsSaifulhadi BarohNo ratings yet
- Machine Learning Automatically Detects Covid-19 Using Chest Cts in A Large Multicenter CohortDocument27 pagesMachine Learning Automatically Detects Covid-19 Using Chest Cts in A Large Multicenter CohortballechaseNo ratings yet
- Hemoptisis 9Document9 pagesHemoptisis 9habiba rositaNo ratings yet
- Islam612023AORJ108845 DR - Tariqul IslamDocument6 pagesIslam612023AORJ108845 DR - Tariqul Islamsazzad suvroNo ratings yet
- (2009) Radiographic Improvement and Its Predictors in Patients With Pulmonary TuberculosisDocument6 pages(2009) Radiographic Improvement and Its Predictors in Patients With Pulmonary TuberculosisMohd RahimiNo ratings yet
- The Value of Chest Ultrasonography Applications in The Respiratory ICUDocument6 pagesThe Value of Chest Ultrasonography Applications in The Respiratory ICUHeru SigitNo ratings yet
- Reynolds 2010Document6 pagesReynolds 2010Putra PratamaNo ratings yet
- Organizing Pneumonia: Chest HRCT Findings : Pneumonia em Organização: Achados Da TCAR de TóraxDocument7 pagesOrganizing Pneumonia: Chest HRCT Findings : Pneumonia em Organização: Achados Da TCAR de TóraxPutra PratamaNo ratings yet
- Children’ S Interstitial Lung Disease MultiDocument7 pagesChildren’ S Interstitial Lung Disease MultideaNo ratings yet
- Chest Radiographic Manifestations of Scrub Typhus - PMCDocument9 pagesChest Radiographic Manifestations of Scrub Typhus - PMCSurachai PraimaiNo ratings yet
- As Trocito MaDocument10 pagesAs Trocito Majeimy_carolina4163No ratings yet
- Final Presentation PPT - Group 2Document13 pagesFinal Presentation PPT - Group 2Cess Abad AgcongNo ratings yet
- RolqxcaplmonDocument8 pagesRolqxcaplmonjesus armando mandujano barcenasNo ratings yet
- Different clinicopathological features between young and older patients with pulmonary adenocarcinoma and ground-glass opacityDocument7 pagesDifferent clinicopathological features between young and older patients with pulmonary adenocarcinoma and ground-glass opacityreshma eldhoNo ratings yet
- CMMM2022 8192832Document8 pagesCMMM2022 8192832Desiree MejicaNo ratings yet
- Bronchiectasis in nonCF in ChildrenDocument9 pagesBronchiectasis in nonCF in ChildrenathaNo ratings yet
- Cancer GuidelinesDocument17 pagesCancer GuidelinesJoni WitziNo ratings yet
- Les Aspects Epidemiologiques Et Evolutifs de La Sarcoidose Mediastinopulmonaire Au Sein Du Service de Pneumologie Chu Hassan Ii FesDocument6 pagesLes Aspects Epidemiologiques Et Evolutifs de La Sarcoidose Mediastinopulmonaire Au Sein Du Service de Pneumologie Chu Hassan Ii FesIJAR JOURNALNo ratings yet
- The Effect of Season of Operation On The Survival of Patients With Resected Non-Small Cell Lung CancerDocument5 pagesThe Effect of Season of Operation On The Survival of Patients With Resected Non-Small Cell Lung CancerDaniel AriasNo ratings yet
- Bronchoscopic Procedures During COVID-19 PandemicDocument8 pagesBronchoscopic Procedures During COVID-19 PandemicwantoNo ratings yet
- ArticleDocument11 pagesArticlemilaNo ratings yet
- Boonsarngsuk - Factors Affecting The Diagnostic Yield of Flexible Bronchoscopy Without Guidance in Pulmonary Nodules or MassesDocument6 pagesBoonsarngsuk - Factors Affecting The Diagnostic Yield of Flexible Bronchoscopy Without Guidance in Pulmonary Nodules or MassesXaralyn XaviereNo ratings yet
- Iaa CovisDocument8 pagesIaa Covissanya eusebia lupaca lupacaNo ratings yet
- Diagnostic Delay MoroccoDocument5 pagesDiagnostic Delay MoroccoOmaima ElyounsiNo ratings yet
- Profil Hasil Pemeriksaan CT-Scan Pada Pasien Tumor Paru Di Bagian Radiologi RSUD Dr. Zainoel Abidin Periode Juli 2018-Oktober 2018Document6 pagesProfil Hasil Pemeriksaan CT-Scan Pada Pasien Tumor Paru Di Bagian Radiologi RSUD Dr. Zainoel Abidin Periode Juli 2018-Oktober 2018Dheana IsmaniarNo ratings yet
- Features of Diagnosis and Optimization of Treatment of Nodular GoiterDocument4 pagesFeatures of Diagnosis and Optimization of Treatment of Nodular GoiterSilvio PardiiniiNo ratings yet
- Richeldi Et Al 2021 Utility of A Molecular Classifier As A Complement To High Resolution Computed Tomography ToDocument10 pagesRicheldi Et Al 2021 Utility of A Molecular Classifier As A Complement To High Resolution Computed Tomography Toحسام الوجيهNo ratings yet
- Clinical Approach For The Pneumomediastinum After Blunt Chest TraumaDocument7 pagesClinical Approach For The Pneumomediastinum After Blunt Chest TraumaIdham Adyasa Manggala PutraNo ratings yet
- 2022 48 3 3675 EnglishDocument10 pages2022 48 3 3675 EnglishRaul Matute MartinNo ratings yet
- Radiologic Manifestations of Pulmonary Tuberculosis in Patients of Intensive Care UnitsDocument6 pagesRadiologic Manifestations of Pulmonary Tuberculosis in Patients of Intensive Care UnitsAnonymous qwH3D0KrpNo ratings yet
- 2015 BJMMR 18180rev1Document14 pages2015 BJMMR 18180rev1Hülya SungurtekinNo ratings yet
- Chest X Ray in CAPDocument7 pagesChest X Ray in CAPsahatmanurungNo ratings yet
- Computed Tomography-Guided Preoperative Semi-Rigid Hook-Wire Localization of Small Pulmonary Nodules: 74 Cases ReportDocument8 pagesComputed Tomography-Guided Preoperative Semi-Rigid Hook-Wire Localization of Small Pulmonary Nodules: 74 Cases ReportsofiaNo ratings yet
- MicronodulosDocument9 pagesMicronodulosWildcane SalmeronNo ratings yet
- An Ensemble Deep Learning Model For Risk Stratificat Source NPJ Digit Med 2023Document12 pagesAn Ensemble Deep Learning Model For Risk Stratificat Source NPJ Digit Med 2023lliuyueeNo ratings yet
- Covid CT Chest Scan Score & SeverityDocument7 pagesCovid CT Chest Scan Score & SeverityMohan DesaiNo ratings yet
- Clinical Microbiology and Infection: Research NoteDocument4 pagesClinical Microbiology and Infection: Research NoteNoorNo ratings yet
- Full TextDocument34 pagesFull TextkanNo ratings yet
- Journal ReadingDocument7 pagesJournal ReadingTheresa JulietNo ratings yet
- Clinical Presentation and Treatment Outcomes of Thyroglossal Duct Cysts: A Systematic ReviewDocument8 pagesClinical Presentation and Treatment Outcomes of Thyroglossal Duct Cysts: A Systematic ReviewR KNo ratings yet
- The Place of HRCT Imaging in The Investigation of ILDDocument17 pagesThe Place of HRCT Imaging in The Investigation of ILDrbatjun576No ratings yet
- NotesDocument4 pagesNotesRaza HodaNo ratings yet
- Montouri 2019 Lung Us in PTBDocument6 pagesMontouri 2019 Lung Us in PTBmarvic gabitanNo ratings yet
- Diagnostics 11 02008 v2Document12 pagesDiagnostics 11 02008 v2Fatoş TekelioğluNo ratings yet
- The Papanicolaou Society of Cytopathology System for Reporting Respiratory Cytology: Definitions, Criteria, Explanatory Notes, and Recommendations for Ancillary TestingFrom EverandThe Papanicolaou Society of Cytopathology System for Reporting Respiratory Cytology: Definitions, Criteria, Explanatory Notes, and Recommendations for Ancillary TestingNo ratings yet
- A Study to Effect of Reminiscence Therapy on Psychological Well-Being among Elderly Residing in Selected Old Age HomeDocument5 pagesA Study to Effect of Reminiscence Therapy on Psychological Well-Being among Elderly Residing in Selected Old Age HomeInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Application of Project Management using CPM (Critical Path Method) and Pert (Project Evaluation and Review Technique) in the Nava House Bekasi Cluster Housing Development ProjectDocument12 pagesApplication of Project Management using CPM (Critical Path Method) and Pert (Project Evaluation and Review Technique) in the Nava House Bekasi Cluster Housing Development ProjectInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Analysis of Opaque, Peel-Off and Flex Rejects in the Electro Plating Process Using the Six Sigma Dmaic MethodDocument18 pagesAnalysis of Opaque, Peel-Off and Flex Rejects in the Electro Plating Process Using the Six Sigma Dmaic MethodInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- A Rare Complication: Cardiac Arrest and Pulmonary Embolism in Polyarteritis NodosaDocument5 pagesA Rare Complication: Cardiac Arrest and Pulmonary Embolism in Polyarteritis NodosaInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Application of the Economic Order Quantity (EOQ) Method on the Supply of Chemical Materials in the Laboratory of PT. Fajar Surya Wisesa TbkDocument15 pagesApplication of the Economic Order Quantity (EOQ) Method on the Supply of Chemical Materials in the Laboratory of PT. Fajar Surya Wisesa TbkInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Quality Control to Reduce Appearance Defects at PT. Musical InstrumentDocument11 pagesQuality Control to Reduce Appearance Defects at PT. Musical InstrumentInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Forecasting PM10 Concentrations Using Artificial Neural Network in Imphal CityDocument10 pagesForecasting PM10 Concentrations Using Artificial Neural Network in Imphal CityInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- A Comprehensive Review on the Therapeutic Potential of PectinDocument6 pagesA Comprehensive Review on the Therapeutic Potential of PectinInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- The Impact of Integrated Border Security System on Human Trafficking in Bangladesh: The Mediating Effect of the Use of Advanced TechnologyDocument12 pagesThe Impact of Integrated Border Security System on Human Trafficking in Bangladesh: The Mediating Effect of the Use of Advanced TechnologyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Quizlet's Usefulness for Vocabulary Learning: Perceptions of High-Level and Low-Level Chinese College EFL LearnersDocument5 pagesQuizlet's Usefulness for Vocabulary Learning: Perceptions of High-Level and Low-Level Chinese College EFL LearnersInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Analysis of Carton Packaging Quality Control Using Statistical Quality Control Methods at PT XYZDocument10 pagesAnalysis of Carton Packaging Quality Control Using Statistical Quality Control Methods at PT XYZInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Health Care - An Android Application Implementation and Analyzing user Experience Using PythonDocument7 pagesHealth Care - An Android Application Implementation and Analyzing user Experience Using PythonInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Entrepreneurial Adult Education as a Catalyst for Youth Employability in Disadvantaged AreasDocument9 pagesEntrepreneurial Adult Education as a Catalyst for Youth Employability in Disadvantaged AreasInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Visitor Perception Related to the Quality of Service in Todo Tourism VillageDocument10 pagesVisitor Perception Related to the Quality of Service in Todo Tourism VillageInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Enhancing Estimating the Charge Level in Electric Vehicles: Leveraging Force Fluctuation and Regenerative Braking DataDocument6 pagesEnhancing Estimating the Charge Level in Electric Vehicles: Leveraging Force Fluctuation and Regenerative Braking DataInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- A New Model of Rating to Evaluate Start-ups in Emerging Indian MarketDocument7 pagesA New Model of Rating to Evaluate Start-ups in Emerging Indian MarketInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- A Proof of Concept Using BLE to Optimize Patients Turnaround Time (PTAT) in Health CareDocument14 pagesA Proof of Concept Using BLE to Optimize Patients Turnaround Time (PTAT) in Health CareInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Gravity Investigations Applied to the Geological Framework Study of the Mambasa Territory in Democratic Republic of CongoDocument9 pagesGravity Investigations Applied to the Geological Framework Study of the Mambasa Territory in Democratic Republic of CongoInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Developing Digital Fluency in Early Education: Narratives of Elementary School TeachersDocument11 pagesDeveloping Digital Fluency in Early Education: Narratives of Elementary School TeachersInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Intrusion Detection System with Ensemble Machine Learning Approaches using VotingClassifierDocument4 pagesIntrusion Detection System with Ensemble Machine Learning Approaches using VotingClassifierInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Crop Monitoring System with Water Moisture Levels Using ControllerDocument8 pagesCrop Monitoring System with Water Moisture Levels Using ControllerInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Naturopathic Approaches to Relieving Constipation: Effective Natural Treatments and TherapiesDocument9 pagesNaturopathic Approaches to Relieving Constipation: Effective Natural Treatments and TherapiesInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Inclusive Leadership in the South African Police Service (SAPS)Document26 pagesInclusive Leadership in the South African Police Service (SAPS)International Journal of Innovative Science and Research TechnologyNo ratings yet
- Optimizing Bio-Implant Materials for Femur Bone Replacement:A Multi-Criteria Analysis and Finite Element StudyDocument5 pagesOptimizing Bio-Implant Materials for Femur Bone Replacement:A Multi-Criteria Analysis and Finite Element StudyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Year Wise Analysis and Prediction of Gold RatesDocument8 pagesYear Wise Analysis and Prediction of Gold RatesInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Synthetic and Natural Vitamin C Modulation of Leaded Paint-Induced Nephrotoxicity of Automobile Painters in Ile-Ife, Nigeria.Document21 pagesSynthetic and Natural Vitamin C Modulation of Leaded Paint-Induced Nephrotoxicity of Automobile Painters in Ile-Ife, Nigeria.International Journal of Innovative Science and Research TechnologyNo ratings yet
- Design and Implementation of Software-Defined ReceiverDocument8 pagesDesign and Implementation of Software-Defined ReceiverInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Financial Prudence as Determinant of Employees’ Interest in Graduate StudyDocument13 pagesFinancial Prudence as Determinant of Employees’ Interest in Graduate StudyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- The Role of Leadership Training in Developing Effective Police SupervisorsDocument17 pagesThe Role of Leadership Training in Developing Effective Police SupervisorsInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Fahfi/Mochaina Illegal Gambling Activities and its Average Turnover within Limpopo ProvinceDocument8 pagesFahfi/Mochaina Illegal Gambling Activities and its Average Turnover within Limpopo ProvinceInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- HomicideDocument22 pagesHomicideniraj_sdNo ratings yet
- Chicken Pox Research PaperDocument5 pagesChicken Pox Research Paperc9rvz6mm100% (1)
- Male InfertilityDocument1 pageMale Infertilitya jNo ratings yet
- NeonatologyDocument47 pagesNeonatologySoumya K SNo ratings yet
- Pediatric Research ArticleDocument2 pagesPediatric Research Articleapi-653708698No ratings yet
- Nystagmus: Dr. Enny Lestari, M. Biomed, SP.SDocument39 pagesNystagmus: Dr. Enny Lestari, M. Biomed, SP.SPuji Yunisyah100% (1)
- Discus Prolaps (HNP)Document22 pagesDiscus Prolaps (HNP)Fitriyani Rahma IINo ratings yet
- Hypoxia: Lori HolmesDocument5 pagesHypoxia: Lori HolmesDanson Githinji ENo ratings yet
- Study Hours: Days Until ExamDocument32 pagesStudy Hours: Days Until ExamYASSER100% (1)
- Zika VirusDocument2 pagesZika VirusYousef Hassan BazarNo ratings yet
- Soppi 2018Document5 pagesSoppi 2018dr_joe23No ratings yet
- 1-Panadol Advance 6-Panadol Sinus 2-Panadol Extra 7-Panadol Night 3-Panadol Actifast 4-Panadol Joint 5-Panadol Cold and Flu and Their TypesDocument12 pages1-Panadol Advance 6-Panadol Sinus 2-Panadol Extra 7-Panadol Night 3-Panadol Actifast 4-Panadol Joint 5-Panadol Cold and Flu and Their TypesSulaiman AlqatfNo ratings yet
- Acute Raptured Appendicitis - VMCDocument6 pagesAcute Raptured Appendicitis - VMCMicahMananguitNo ratings yet
- Herbal PlantsDocument11 pagesHerbal PlantsDechy Lyn PalmaNo ratings yet
- Acute Vs Chronic Renal FailureDocument7 pagesAcute Vs Chronic Renal FailurePellan Rhey CapuyanNo ratings yet
- Question Paper 2023 AIAPGETDocument20 pagesQuestion Paper 2023 AIAPGETrohinibrajole123No ratings yet
- Special Education ClassificationsDocument3 pagesSpecial Education ClassificationsEdmar AgarpaoNo ratings yet
- Interview Guide For Nursing Health HistoryDocument3 pagesInterview Guide For Nursing Health HistoryDersly LaneNo ratings yet
- Manual Handling Training Use ThisDocument17 pagesManual Handling Training Use ThisPrimelift Safety Resources Limited100% (3)
- 100 Case Studies in Pathophysiology-532hlm (Warna Hanya Cover)Document11 pages100 Case Studies in Pathophysiology-532hlm (Warna Hanya Cover)Haymanot AnimutNo ratings yet
- Islands in Palmistry Extremely Bad Sign On Your HandsDocument1 pageIslands in Palmistry Extremely Bad Sign On Your Handssantosh TiwariNo ratings yet
- Asthma: Topic OutlineDocument2 pagesAsthma: Topic OutlineKdamnzNo ratings yet
- ShinglesDocument8 pagesShinglesapi-3366481170% (1)
- davidson - mcq - 20th Edition مدونة كل العرب الطبيةDocument244 pagesdavidson - mcq - 20th Edition مدونة كل العرب الطبيةAlokh Saha RajNo ratings yet
- Chromosome Abnormalities Flash CardsDocument3 pagesChromosome Abnormalities Flash CardsAmirreza ReyNo ratings yet
- Post Test NUR 219 17Document3 pagesPost Test NUR 219 17Naomi VirtudazoNo ratings yet
- (Week 10) Epidemiology and Disease TransmissionDocument1 page(Week 10) Epidemiology and Disease TransmissionDiana Leen Dela CruzNo ratings yet