Professional Documents
Culture Documents
TDM Monitoring Sampling Guideline Form 2022 Iso Code
TDM Monitoring Sampling Guideline Form 2022 Iso Code
Uploaded by
nur nadirahCopyright:
Available Formats
You might also like
- Step 3 CCS Mnemonics... NEW..Document1 pageStep 3 CCS Mnemonics... NEW..madiha85% (13)
- Lesson Plan ContentDocument6 pagesLesson Plan ContentSrijana Gurung100% (2)
- Laboratory Request FormDocument1 pageLaboratory Request FormEric Nagum100% (2)
- Diagnostic Lab Request Form PDFDocument1 pageDiagnostic Lab Request Form PDFAlthea PelipasNo ratings yet
- CASESHEETPHARMDDocument6 pagesCASESHEETPHARMDSai SharathNo ratings yet
- Hospital Document Tariff Statement (Mini SOC)Document1 pageHospital Document Tariff Statement (Mini SOC)Deepak KaushikNo ratings yet
- Formulir Pemeriksaan LabDocument2 pagesFormulir Pemeriksaan Labandi ansoriNo ratings yet
- Beginners Guide To DigitalRXDocument14 pagesBeginners Guide To DigitalRXStarrx714No ratings yet
- Preclinical Testing FlowchartDocument30 pagesPreclinical Testing FlowchartAnonymous Ao0hFRNo ratings yet
- Laboratory Request Form: Specimen Collected Patient Details Insurance Info ICD-9 CodeDocument2 pagesLaboratory Request Form: Specimen Collected Patient Details Insurance Info ICD-9 CodeJoy BautistaNo ratings yet
- TDM Request FormDocument3 pagesTDM Request FormWildan Setyo RayandiNo ratings yet
- TDM Request FormDocument3 pagesTDM Request FormMuhammad IqbalNo ratings yet
- Lab ReportDocument36 pagesLab ReportY.v. SandeepNo ratings yet
- Contoh Formulir Rekam Medis Rawat InapDocument11 pagesContoh Formulir Rekam Medis Rawat InapResti ayuNo ratings yet
- PCPDocument6 pagesPCPBob BobNo ratings yet
- MMMH-M-PAL-QP-003 Form1 Rev.1-Clinical Laboratory Request: City of Batac, Ilocos Norte, PhilippinesDocument1 pageMMMH-M-PAL-QP-003 Form1 Rev.1-Clinical Laboratory Request: City of Batac, Ilocos Norte, PhilippinesWyn AgustinNo ratings yet
- To The Requesting Lab / Person, Please Stamp HereDocument4 pagesTo The Requesting Lab / Person, Please Stamp HereRicardanteNo ratings yet
- Info On Different CasesDocument5 pagesInfo On Different CasesAlka SangwanNo ratings yet
- Med-Surg - Skills ChecklistDocument4 pagesMed-Surg - Skills Checklisthealth careNo ratings yet
- Autar DVT Risk Assessment ScaleDocument2 pagesAutar DVT Risk Assessment ScalerenuNo ratings yet
- ReportDocument1 pageReportabbasalizaidi07No ratings yet
- Normal Medical FormDocument1 pageNormal Medical FormAHESANALI GULAMHAIDER MOMINNo ratings yet
- Laboratory Report Final: Sherly Dr. Sruti Mary JosephDocument2 pagesLaboratory Report Final: Sherly Dr. Sruti Mary JosephVande GuruParamparaNo ratings yet
- Ancillary Order Form PDFDocument2 pagesAncillary Order Form PDFHASANAHRR_347724114No ratings yet
- Suez Canal University/ Faculty of Nursing (Medical Surgical Nursing/ Clinical Assessment Sheet 2 Year 2020/2021)Document18 pagesSuez Canal University/ Faculty of Nursing (Medical Surgical Nursing/ Clinical Assessment Sheet 2 Year 2020/2021)طالب جامعة100% (1)
- Jayla Wright Chart Materials Sim 1Document8 pagesJayla Wright Chart Materials Sim 1tNo ratings yet
- New Clinical Log Form 202302FINAL - 240307 - 015229 4Document2 pagesNew Clinical Log Form 202302FINAL - 240307 - 015229 4aabbccss1.z71No ratings yet
- Clinical Worksheet-Summer 08 REVISEDDocument17 pagesClinical Worksheet-Summer 08 REVISEDDaniJeanNo ratings yet
- Coagulopathy and Antiphospholipid Antibodies in Patients With Covid-19Document5 pagesCoagulopathy and Antiphospholipid Antibodies in Patients With Covid-19Zelgi PutraNo ratings yet
- Borang Diabetes Clinical AuditDocument2 pagesBorang Diabetes Clinical AuditHafizzah Mohd FirdausNo ratings yet
- Kardex - End Stage Renal FailureDocument5 pagesKardex - End Stage Renal FailureKiara Denise TamayoNo ratings yet
- Wa0110Document3 pagesWa0110venkat yeluriNo ratings yet
- City of Batac, Ilocos Norte, Philippines Contact Details: Direct Line: (077) 6000105 Trunk Line: (077) 7923133 Loc. 102Document1 pageCity of Batac, Ilocos Norte, Philippines Contact Details: Direct Line: (077) 6000105 Trunk Line: (077) 7923133 Loc. 102LexiePascuaSantosNo ratings yet
- All Items Are Required:nothing Should Be Left BlankDocument6 pagesAll Items Are Required:nothing Should Be Left BlankNancy shwayatNo ratings yet
- 01023405LB 2022 09 25Document2 pages01023405LB 2022 09 25santabarsinghthapaNo ratings yet
- Borang CP2 (Hospital Manual)Document2 pagesBorang CP2 (Hospital Manual)William TanNo ratings yet
- PROTOCOL For Management of COVID-19 Cases WB 2nd Edition.Document49 pagesPROTOCOL For Management of COVID-19 Cases WB 2nd Edition.Shahin KhanNo ratings yet
- Management Protocol For Covid-19: Department of Health and Family WelfareDocument34 pagesManagement Protocol For Covid-19: Department of Health and Family Welfarechandra sekharNo ratings yet
- Star Health and Allied Insurance Company Limited Tariff Statement - Mini SOC (FINALISED)Document1 pageStar Health and Allied Insurance Company Limited Tariff Statement - Mini SOC (FINALISED)Sanket Sahare100% (1)
- Progress Note IcuDocument2 pagesProgress Note Icumena gergesNo ratings yet
- TRRF FormDocument2 pagesTRRF Formsachinyadav22200No ratings yet
- Edith Jacobson Kardex To DIscharge PlanDocument16 pagesEdith Jacobson Kardex To DIscharge PlanFranz Patrick Legria, CPAC - SNNo ratings yet
- A22M0163DR - ArponDocument7 pagesA22M0163DR - ArponAnton CornelNo ratings yet
- Medibuddy 12385526Document5 pagesMedibuddy 12385526gowthami sirana baluNo ratings yet
- Complete Blood Count (CBC With E.S.R) .: Investigation Units Result Biological Reference IntervalDocument4 pagesComplete Blood Count (CBC With E.S.R) .: Investigation Units Result Biological Reference Intervalmaryam.ksohrabNo ratings yet
- 02.borang Diabetes Clinical Audit MELAYUDocument3 pages02.borang Diabetes Clinical Audit MELAYUnorhaslizaNo ratings yet
- (Template Only) DSDocument2 pages(Template Only) DSMAE ANN MU�OZNo ratings yet
- Care Plan TemplateDocument12 pagesCare Plan TemplateemipNo ratings yet
- Care Plan For GastrectomyDocument16 pagesCare Plan For GastrectomyPriyal ParikhNo ratings yet
- HematologyDocument5 pagesHematologyDeepak KumarNo ratings yet
- Discharge SheetDocument5 pagesDischarge Sheetprahadishwar.backupNo ratings yet
- Physical Examination Report: Philippine National Police Health ServiceDocument2 pagesPhysical Examination Report: Philippine National Police Health Servicelara michelleNo ratings yet
- Test Report: 1124001950 35 Years/Male MR.M A Mukhtadir 10-May-2024 /08:50 10-May-2024 /10:43Document4 pagesTest Report: 1124001950 35 Years/Male MR.M A Mukhtadir 10-May-2024 /08:50 10-May-2024 /10:43Anirudh CVNo ratings yet
- Rajesh R D - 2312316Document2 pagesRajesh R D - 2312316dr.menganeNo ratings yet
- Report (3)Document21 pagesReport (3)aryancradlesNo ratings yet
- History FormDocument5 pagesHistory FormYazeed AsrawiNo ratings yet
- ICU General Admission Orders: OthersDocument2 pagesICU General Admission Orders: OthersHANIMNo ratings yet
- Administering Metoprolol IV Push 1Document22 pagesAdministering Metoprolol IV Push 1api-357388170No ratings yet
- Dr. Sudarto Sppd's FileDocument22 pagesDr. Sudarto Sppd's FileVindy CesarianaNo ratings yet
- Patient Name Age / Gender Uhid/Mr No. OP Visit No Sample Collected On: 03-07-2018 18:33 Reported On LRN# Specimen Ref DoctorDocument2 pagesPatient Name Age / Gender Uhid/Mr No. OP Visit No Sample Collected On: 03-07-2018 18:33 Reported On LRN# Specimen Ref DoctormukhleshNo ratings yet
- Department of Hematology Covid-19 Health Checkup (Post Recovery)Document8 pagesDepartment of Hematology Covid-19 Health Checkup (Post Recovery)Geetika GuptaNo ratings yet
- Blood Form 3Document1 pageBlood Form 3jennifer.borleyNo ratings yet
- Asthma: Kaps PrepDocument21 pagesAsthma: Kaps PrepImee TingzonNo ratings yet
- FDA 483 and Warning LetterDocument38 pagesFDA 483 and Warning LetterOmar FaruqNo ratings yet
- Dilution Protocol BPF JKNSDocument272 pagesDilution Protocol BPF JKNSArmin Tordecilla MercadoNo ratings yet
- Creative AdjustmentDocument56 pagesCreative AdjustmentNancy Azanasía Karantzia100% (2)
- Yashaswini Pader - Resume - Abroad AssistDocument3 pagesYashaswini Pader - Resume - Abroad AssistMuneer Basha SkNo ratings yet
- Doxorubicin and Ifosfamide Sarcoma Protocol V1.0Document8 pagesDoxorubicin and Ifosfamide Sarcoma Protocol V1.0Joseph TrevinoNo ratings yet
- UntitledDocument13 pagesUntitledFengyue LvNo ratings yet
- NO Produk Isi/Box HNA Kode Produk: Penawaran Harga Rs Harapan Keluarga Pt. Hexpharm Jaya 2021Document6 pagesNO Produk Isi/Box HNA Kode Produk: Penawaran Harga Rs Harapan Keluarga Pt. Hexpharm Jaya 2021YENNYNo ratings yet
- Neuraxial ProceduresDocument2 pagesNeuraxial ProceduresRessy HastoprajaNo ratings yet
- BLS PretestDocument6 pagesBLS PretestElnoor Sapah100% (2)
- Preventing and Managing Medication ErrorsDocument31 pagesPreventing and Managing Medication ErrorsLiza Marie de GuzmanNo ratings yet
- Ge 110 Drug EducationDocument20 pagesGe 110 Drug EducationRojelu BurdeosNo ratings yet
- Nursing Cheat SheetDocument1 pageNursing Cheat Sheetramesh kumarNo ratings yet
- Procaine: BupivicaineDocument7 pagesProcaine: BupivicaineBirara ChakilieNo ratings yet
- Forces of Commonly Used Chiropractic Techniques For Children: A Review of The LiteratureDocument10 pagesForces of Commonly Used Chiropractic Techniques For Children: A Review of The LiteratureAlejandro LópezNo ratings yet
- AntidepressantsDocument31 pagesAntidepressantsIzhaan AkmalNo ratings yet
- Giulia Endo Eng Rev05Document6 pagesGiulia Endo Eng Rev05Steven BrownNo ratings yet
- Pharmacodynamics:: What The Drug Does To The BodyDocument38 pagesPharmacodynamics:: What The Drug Does To The BodyWong Sin Ting HebeNo ratings yet
- Daftar Harga PT Pradipta Adipacific: Produk: PT Ifars Pharmaceutical LaboratoriesDocument5 pagesDaftar Harga PT Pradipta Adipacific: Produk: PT Ifars Pharmaceutical Laboratoriesapotek aslitmgNo ratings yet
- Unit 5 - The Placebo EffectDocument2 pagesUnit 5 - The Placebo EffectDat HoangNo ratings yet
- DR Tommy - Cancer PainDocument60 pagesDR Tommy - Cancer Painrisalbalu100% (1)
- 2 - CNS QDocument4 pages2 - CNS QTan Hing LeeNo ratings yet
- TabletsDocument14 pagesTabletsMuhammad WaleedNo ratings yet
- Aerosol TherapyDocument12 pagesAerosol TherapyDejan ŽujovićNo ratings yet
- Kaimax BrochureDocument8 pagesKaimax Brochurekbeauty.pharmaNo ratings yet
- Analisis Waktu Tunggu Pelayanan Resep Di Puskesmas Pasir Panjang Kota Kupang Bulan April Tahun 2018Document8 pagesAnalisis Waktu Tunggu Pelayanan Resep Di Puskesmas Pasir Panjang Kota Kupang Bulan April Tahun 2018Ridhatul AzizahNo ratings yet
- Past-Years' Exam Questions Cns Anticonvulsant 3. Local AnaestheticDocument2 pagesPast-Years' Exam Questions Cns Anticonvulsant 3. Local Anaestheticnmyza89No ratings yet
TDM Monitoring Sampling Guideline Form 2022 Iso Code
TDM Monitoring Sampling Guideline Form 2022 Iso Code
Uploaded by
nur nadirahOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
TDM Monitoring Sampling Guideline Form 2022 Iso Code
TDM Monitoring Sampling Guideline Form 2022 Iso Code
Uploaded by
nur nadirahCopyright:
Available Formats
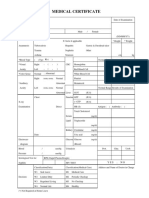
HSAJB/FAR-66/VER2.
0/2022
HOSPITAL SULTANAH AMINAH JOHOR BAHRU (HSAJB) Pharmacy Ref No:
CLINICAL PHARMACOKINETICS SERVICE
Therapeutic Drug Monitoring (TDM) Request Form PhIS Report No:
3 – 5 ml of blood sample is needed for analysis of 1 – 3 drugs. Date Received :
Note : Use plain tubes for all the drugs except for Cyclosporin/Tacrolimus/Sirolimus/Everolimus (EDTA tube).
Correct information is crucial as interpretation of results is dependent on the information provided. Time Received :
PATIENT PROFILE
Name : Ward/Unit : RN :
Age : Gender : M/F Race: M /C/ I/O IC :
Weight (kg) : Height (cm) : DOA :
CLINICAL SUMMARY AND DIAGNOSIS
PATIENT CONDITION INDICATION FOR REQUEST
Oedema Liver Disease Dehydration Therapeutic Monitoring Non-compliance
Others
Dialysis Burn Fit Frequency: ….……… Suspected Toxicity
……………………….
LATEST LAB RESULTS CONCURRENT MEDICATIONS
Parameters Date Results (unit) Parameters Date Results(unit)
Blood Urea Temperature
Na+ / K+ WBC
Creatinine ALT / AST / ALP
Albumin HR
Culture & Sensitivity
Drug Analysis Dose Pre-dose / Post- dose
Present Dose Dose Given Random
( Tick where Started Post 2 / C0 / Post 6 / C2
Regimen
appropriate )
Date Time Date Time Date Time Date Time Date Time
Acetaminophen
Amikacin
Carbamazepine
Cyclosporin
Digoxin
Everolimus
Gentamicin
Lithium
Methotrexate
Phenobarbitone
Phenytoin
Salicylate
Sirolimus
Tacrolimus
Theophylline
Valproic acid
Vancomycin
Others (please specify):
REFER TO TDM SERUM SAMPLING GUIDELINES(refer back page)
For injectable drug being analysed : REQUESTED BY:
Infusion rate : ……………………………………………….
Duration of Infusion : …………………………………….. Doctor’s Signature : _______________ Name & Stamp : _______________ Date : ___________
Drug analysis Result Therapeutic Range Calculated Pharmacokinetic Parameters Time
Finished:
Ke : hr-1 t1/2 : hr Vd: L/kg
FOR PHARMACY USE ONLY
Cmin : µg/ml Cmax : µg/ml
Test done
AUC24: µg.hr/ml by:
Css : Cadjusted : CrCl:
Pharmacist’s Assessment & Recommendation :
Pharmacist’s signature & stamp
Informed : DR / SN / PF ……………………on ……………… at …………………am/pm
HSAJB/FAR-66/VER2.0/2022
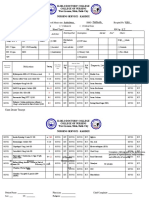
TDM SERUM SAMPLING GUIDE
DRUG STEADY STATE SAMPLING TIME THERAPEUTIC RANGE
(Time to monitor plasma concentrations) (*The target reference ranges may SAMPLE
SINGLE DAILY MULTIPLE SINGLE DAILY MULTIPLE varybasedon institutional reference& STABILITY
DOSING DOSING DOSING DOSING indication)
Trough:
SDD: <2 mcg/ml
AMIKACIN Neonates: < 5mcg/ml
1st sample MDD & Dialysis : <10mcg/ml
Pre 8 hours
Post 2 hours
0 – 30 min
AMINOGLYCOSIDE
#Peak:
before dose Neonates, MDD: 20-40 mcg/ml
2nd sample
SDD : *60 mcg/ml
2nd dose 3rdor4thdose Post 6 hours
Post
Trough:
30 min after 30 SDD, Neonates & synergistic: <1mcg/ml
(or any two post min infusion MDD & Dialysis: <2mcg/ml
sampling at completed
least 2 t1/2 apart) #Peak:
Neonates: 5-12 mcg/ml
GENTAMICIN 4 hours
MDD: 5-10 mcg/ml
SDD: *10-30 mcg/ml
Synergy: 3-4 mcg/ml (conventional dosing against
Impaired Renal Function: Gram positive organism)
After24 hours (after 1st stat dose) or Pre-HD
#
adjustable according to indication
Normal Renal Function : Trough:
4thdose Non-complicated infection :10 – 15 mcg/ml
Impaired Renal Function : Complicated infection :15 – 20 mcg/ml
Trough level: 30mins before dose
After 24hours (after 1st stat dose) Peak: 25 – 40 mcg/ml
VANCOMYCIN Peak level: 1 hour after the infusion 4 hours
completed
Continuous Infusion: Continuous Infusion: 15 ‒ 25mcg/mL
Take a sample after 12 – 24 hours of
starting the continuous infusion AUC24/MIC : 400-600mg.h/L
Initiation : 2-3 weeks (Induction Phase)
CARBAMAZEPINE MD : 2-5 days after initiation and dose Pre: 0 – 30 min before dose 4 – 12 mcg/ml 8 hours
changes
Epilepsy : 10 – 40 mcg/ml
Without LD : 2- 3 weeks
PHENOBARBITAL Pre: 0 – 30 min before dose Refractory status epileptics : > 70mcg/ml 8 hours
After LD : 2 – 3 hrs after administration
(up to 100mcg/ml)
With LD :Oral: 24 hours
IV : 2 hours (if rapid therapeutic 10-20 mcg/ml
PHENYTOIN Pre: 0 – 30 min before dose 8 hours
concentration is needed) Neonates: 8 – 15 mcg/mL
Without LD :7 – 10 days
Epilepsy : 50 – 100 mcg/ml
VALPROIC ACID 2- 4 days Pre: 0 – 30 min before dose 2 days
Psychiatric Disorder: 50 – 125 mcg/ml
Adults : 2days
Children : 1 – 2 days
Apnoea/Bradycardia in neonates : 5 – 10 mcg/ml
THEOPHYLLINE Infants : 1 – 5 days Pre: 0 – 30 min before dose 8 hours
Asthma/COAD : 10 – 20 mcg/ml
Newborn : 120 hrs (5 days)
Premature neonates : 150 hrs (6 days)
Pre :
Without LD : 7 – 14 days 0-30 min before dose
CHF : 0.5 – 0.9 ng/mL
DIGOXIN With LD : 12 – 24 hours Post : 8 hours
AF : 0.8 – 2 ng/mL
ESRD : 15-20 days Oral : At least 6 hours after dose
IV : At least 4 hours after dose
According to drug indication
CYCLOSPORINE Co: Immediately before next dose
3-5 days General Therapeutic Range: 7 days
(EDTA tube) C2: 2 hours after dose
C0∼100-500mcg/L
C2∼600 - 1700mcg/L
TACROLIMUS
3 – 5 days Pre : 0 – 30 min before dose 5 – 20 mg / ml 7 days
(EDTA tube)
SIROLIMUS Adults : 5 – 7days
Pre : 0 – 30 min before dose 4 – 24 mg/ml 8 days
(EDTA tube) Children : 3 – 5 days
METHOTREXATE 24 - 48 hours 24hr or 48hr post infusion Variable – Refer to specific protocols 2 days
(Room Temp)
Toxic :>200 mg/L
Therapeutic : 5 – 7 days Therapeutic : 1 – 3 hours after dose
SALICYLATE Anti-inflammatory : 150 ‒ 300 mg/L 8 hours
Toxicity :Random Toxicity :Random
Rheumatic Fever: 250 ‒ 400 mg/L
Toxicity : 4 hours after single acute
ingestion
PARACETAMOL Toxicity : 4 hours after ingestion Refer Rummack Matthew Nomogram 8 hours
Unknown Ingestion Time: 2 samples
at 2 hours interval
Pre: 12 hours after dose
(twice daily dosing)
LITHIUM 4 – 5 days 0.5 – 1.5 mmol/L 24 hours
Pre: 24 hours after dose
(once daily dosing)
References:
i) Martindale 33th Ed. 2002ii) Basic Clinical Pharmacokinetic (Winter) 2010 iii) Drug Information Handbook 10 th Ed. 2003 iv) British National Formulary, Vol. 70 Sept 2015 v) Micromedex(R) Healthcare
Series 2018vi)Infectious Disease Society of America vii)Drug Doses, Frank Shank, 17 th Edition 2017vii)https://journals.lww.com/drug-monitoring/Abstract/200/08000/
Stability_of_Sirolimus_Rapamycin_in_Whole_Blood.10.aspx., viii)https://journals.lww.com/drug-monitoring/Abstract/2003/02000/In_Vitro_Stability_Study_of_Methotrexate_in_Blood.12.aspx. Ix) Gidwani
Lithium Stability Study 2018. x) Clinical Therapeutic/Vol.22, SUPPL.B,2000 Measurement of Sirolimus in Whole Blood using High Performance Liquid Chromatography with Ultraviolet Detection, D.W.Holt
et.al., xi) Stability of Tacrolimus (FK506) and Cyclosporin G in Whole Blood, T.M. Annesley. et. al., TDM 17:361-365 1995 Lippincott-Raven Publishers, Philadelphia
You might also like
- Step 3 CCS Mnemonics... NEW..Document1 pageStep 3 CCS Mnemonics... NEW..madiha85% (13)
- Lesson Plan ContentDocument6 pagesLesson Plan ContentSrijana Gurung100% (2)
- Laboratory Request FormDocument1 pageLaboratory Request FormEric Nagum100% (2)
- Diagnostic Lab Request Form PDFDocument1 pageDiagnostic Lab Request Form PDFAlthea PelipasNo ratings yet
- CASESHEETPHARMDDocument6 pagesCASESHEETPHARMDSai SharathNo ratings yet
- Hospital Document Tariff Statement (Mini SOC)Document1 pageHospital Document Tariff Statement (Mini SOC)Deepak KaushikNo ratings yet
- Formulir Pemeriksaan LabDocument2 pagesFormulir Pemeriksaan Labandi ansoriNo ratings yet
- Beginners Guide To DigitalRXDocument14 pagesBeginners Guide To DigitalRXStarrx714No ratings yet
- Preclinical Testing FlowchartDocument30 pagesPreclinical Testing FlowchartAnonymous Ao0hFRNo ratings yet
- Laboratory Request Form: Specimen Collected Patient Details Insurance Info ICD-9 CodeDocument2 pagesLaboratory Request Form: Specimen Collected Patient Details Insurance Info ICD-9 CodeJoy BautistaNo ratings yet
- TDM Request FormDocument3 pagesTDM Request FormWildan Setyo RayandiNo ratings yet
- TDM Request FormDocument3 pagesTDM Request FormMuhammad IqbalNo ratings yet
- Lab ReportDocument36 pagesLab ReportY.v. SandeepNo ratings yet
- Contoh Formulir Rekam Medis Rawat InapDocument11 pagesContoh Formulir Rekam Medis Rawat InapResti ayuNo ratings yet
- PCPDocument6 pagesPCPBob BobNo ratings yet
- MMMH-M-PAL-QP-003 Form1 Rev.1-Clinical Laboratory Request: City of Batac, Ilocos Norte, PhilippinesDocument1 pageMMMH-M-PAL-QP-003 Form1 Rev.1-Clinical Laboratory Request: City of Batac, Ilocos Norte, PhilippinesWyn AgustinNo ratings yet
- To The Requesting Lab / Person, Please Stamp HereDocument4 pagesTo The Requesting Lab / Person, Please Stamp HereRicardanteNo ratings yet
- Info On Different CasesDocument5 pagesInfo On Different CasesAlka SangwanNo ratings yet
- Med-Surg - Skills ChecklistDocument4 pagesMed-Surg - Skills Checklisthealth careNo ratings yet
- Autar DVT Risk Assessment ScaleDocument2 pagesAutar DVT Risk Assessment ScalerenuNo ratings yet
- ReportDocument1 pageReportabbasalizaidi07No ratings yet
- Normal Medical FormDocument1 pageNormal Medical FormAHESANALI GULAMHAIDER MOMINNo ratings yet
- Laboratory Report Final: Sherly Dr. Sruti Mary JosephDocument2 pagesLaboratory Report Final: Sherly Dr. Sruti Mary JosephVande GuruParamparaNo ratings yet
- Ancillary Order Form PDFDocument2 pagesAncillary Order Form PDFHASANAHRR_347724114No ratings yet
- Suez Canal University/ Faculty of Nursing (Medical Surgical Nursing/ Clinical Assessment Sheet 2 Year 2020/2021)Document18 pagesSuez Canal University/ Faculty of Nursing (Medical Surgical Nursing/ Clinical Assessment Sheet 2 Year 2020/2021)طالب جامعة100% (1)
- Jayla Wright Chart Materials Sim 1Document8 pagesJayla Wright Chart Materials Sim 1tNo ratings yet
- New Clinical Log Form 202302FINAL - 240307 - 015229 4Document2 pagesNew Clinical Log Form 202302FINAL - 240307 - 015229 4aabbccss1.z71No ratings yet
- Clinical Worksheet-Summer 08 REVISEDDocument17 pagesClinical Worksheet-Summer 08 REVISEDDaniJeanNo ratings yet
- Coagulopathy and Antiphospholipid Antibodies in Patients With Covid-19Document5 pagesCoagulopathy and Antiphospholipid Antibodies in Patients With Covid-19Zelgi PutraNo ratings yet
- Borang Diabetes Clinical AuditDocument2 pagesBorang Diabetes Clinical AuditHafizzah Mohd FirdausNo ratings yet
- Kardex - End Stage Renal FailureDocument5 pagesKardex - End Stage Renal FailureKiara Denise TamayoNo ratings yet
- Wa0110Document3 pagesWa0110venkat yeluriNo ratings yet
- City of Batac, Ilocos Norte, Philippines Contact Details: Direct Line: (077) 6000105 Trunk Line: (077) 7923133 Loc. 102Document1 pageCity of Batac, Ilocos Norte, Philippines Contact Details: Direct Line: (077) 6000105 Trunk Line: (077) 7923133 Loc. 102LexiePascuaSantosNo ratings yet
- All Items Are Required:nothing Should Be Left BlankDocument6 pagesAll Items Are Required:nothing Should Be Left BlankNancy shwayatNo ratings yet
- 01023405LB 2022 09 25Document2 pages01023405LB 2022 09 25santabarsinghthapaNo ratings yet
- Borang CP2 (Hospital Manual)Document2 pagesBorang CP2 (Hospital Manual)William TanNo ratings yet
- PROTOCOL For Management of COVID-19 Cases WB 2nd Edition.Document49 pagesPROTOCOL For Management of COVID-19 Cases WB 2nd Edition.Shahin KhanNo ratings yet
- Management Protocol For Covid-19: Department of Health and Family WelfareDocument34 pagesManagement Protocol For Covid-19: Department of Health and Family Welfarechandra sekharNo ratings yet
- Star Health and Allied Insurance Company Limited Tariff Statement - Mini SOC (FINALISED)Document1 pageStar Health and Allied Insurance Company Limited Tariff Statement - Mini SOC (FINALISED)Sanket Sahare100% (1)
- Progress Note IcuDocument2 pagesProgress Note Icumena gergesNo ratings yet
- TRRF FormDocument2 pagesTRRF Formsachinyadav22200No ratings yet
- Edith Jacobson Kardex To DIscharge PlanDocument16 pagesEdith Jacobson Kardex To DIscharge PlanFranz Patrick Legria, CPAC - SNNo ratings yet
- A22M0163DR - ArponDocument7 pagesA22M0163DR - ArponAnton CornelNo ratings yet
- Medibuddy 12385526Document5 pagesMedibuddy 12385526gowthami sirana baluNo ratings yet
- Complete Blood Count (CBC With E.S.R) .: Investigation Units Result Biological Reference IntervalDocument4 pagesComplete Blood Count (CBC With E.S.R) .: Investigation Units Result Biological Reference Intervalmaryam.ksohrabNo ratings yet
- 02.borang Diabetes Clinical Audit MELAYUDocument3 pages02.borang Diabetes Clinical Audit MELAYUnorhaslizaNo ratings yet
- (Template Only) DSDocument2 pages(Template Only) DSMAE ANN MU�OZNo ratings yet
- Care Plan TemplateDocument12 pagesCare Plan TemplateemipNo ratings yet
- Care Plan For GastrectomyDocument16 pagesCare Plan For GastrectomyPriyal ParikhNo ratings yet
- HematologyDocument5 pagesHematologyDeepak KumarNo ratings yet
- Discharge SheetDocument5 pagesDischarge Sheetprahadishwar.backupNo ratings yet
- Physical Examination Report: Philippine National Police Health ServiceDocument2 pagesPhysical Examination Report: Philippine National Police Health Servicelara michelleNo ratings yet
- Test Report: 1124001950 35 Years/Male MR.M A Mukhtadir 10-May-2024 /08:50 10-May-2024 /10:43Document4 pagesTest Report: 1124001950 35 Years/Male MR.M A Mukhtadir 10-May-2024 /08:50 10-May-2024 /10:43Anirudh CVNo ratings yet
- Rajesh R D - 2312316Document2 pagesRajesh R D - 2312316dr.menganeNo ratings yet
- Report (3)Document21 pagesReport (3)aryancradlesNo ratings yet
- History FormDocument5 pagesHistory FormYazeed AsrawiNo ratings yet
- ICU General Admission Orders: OthersDocument2 pagesICU General Admission Orders: OthersHANIMNo ratings yet
- Administering Metoprolol IV Push 1Document22 pagesAdministering Metoprolol IV Push 1api-357388170No ratings yet
- Dr. Sudarto Sppd's FileDocument22 pagesDr. Sudarto Sppd's FileVindy CesarianaNo ratings yet
- Patient Name Age / Gender Uhid/Mr No. OP Visit No Sample Collected On: 03-07-2018 18:33 Reported On LRN# Specimen Ref DoctorDocument2 pagesPatient Name Age / Gender Uhid/Mr No. OP Visit No Sample Collected On: 03-07-2018 18:33 Reported On LRN# Specimen Ref DoctormukhleshNo ratings yet
- Department of Hematology Covid-19 Health Checkup (Post Recovery)Document8 pagesDepartment of Hematology Covid-19 Health Checkup (Post Recovery)Geetika GuptaNo ratings yet
- Blood Form 3Document1 pageBlood Form 3jennifer.borleyNo ratings yet
- Asthma: Kaps PrepDocument21 pagesAsthma: Kaps PrepImee TingzonNo ratings yet
- FDA 483 and Warning LetterDocument38 pagesFDA 483 and Warning LetterOmar FaruqNo ratings yet
- Dilution Protocol BPF JKNSDocument272 pagesDilution Protocol BPF JKNSArmin Tordecilla MercadoNo ratings yet
- Creative AdjustmentDocument56 pagesCreative AdjustmentNancy Azanasía Karantzia100% (2)
- Yashaswini Pader - Resume - Abroad AssistDocument3 pagesYashaswini Pader - Resume - Abroad AssistMuneer Basha SkNo ratings yet
- Doxorubicin and Ifosfamide Sarcoma Protocol V1.0Document8 pagesDoxorubicin and Ifosfamide Sarcoma Protocol V1.0Joseph TrevinoNo ratings yet
- UntitledDocument13 pagesUntitledFengyue LvNo ratings yet
- NO Produk Isi/Box HNA Kode Produk: Penawaran Harga Rs Harapan Keluarga Pt. Hexpharm Jaya 2021Document6 pagesNO Produk Isi/Box HNA Kode Produk: Penawaran Harga Rs Harapan Keluarga Pt. Hexpharm Jaya 2021YENNYNo ratings yet
- Neuraxial ProceduresDocument2 pagesNeuraxial ProceduresRessy HastoprajaNo ratings yet
- BLS PretestDocument6 pagesBLS PretestElnoor Sapah100% (2)
- Preventing and Managing Medication ErrorsDocument31 pagesPreventing and Managing Medication ErrorsLiza Marie de GuzmanNo ratings yet
- Ge 110 Drug EducationDocument20 pagesGe 110 Drug EducationRojelu BurdeosNo ratings yet
- Nursing Cheat SheetDocument1 pageNursing Cheat Sheetramesh kumarNo ratings yet
- Procaine: BupivicaineDocument7 pagesProcaine: BupivicaineBirara ChakilieNo ratings yet
- Forces of Commonly Used Chiropractic Techniques For Children: A Review of The LiteratureDocument10 pagesForces of Commonly Used Chiropractic Techniques For Children: A Review of The LiteratureAlejandro LópezNo ratings yet
- AntidepressantsDocument31 pagesAntidepressantsIzhaan AkmalNo ratings yet
- Giulia Endo Eng Rev05Document6 pagesGiulia Endo Eng Rev05Steven BrownNo ratings yet
- Pharmacodynamics:: What The Drug Does To The BodyDocument38 pagesPharmacodynamics:: What The Drug Does To The BodyWong Sin Ting HebeNo ratings yet
- Daftar Harga PT Pradipta Adipacific: Produk: PT Ifars Pharmaceutical LaboratoriesDocument5 pagesDaftar Harga PT Pradipta Adipacific: Produk: PT Ifars Pharmaceutical Laboratoriesapotek aslitmgNo ratings yet
- Unit 5 - The Placebo EffectDocument2 pagesUnit 5 - The Placebo EffectDat HoangNo ratings yet
- DR Tommy - Cancer PainDocument60 pagesDR Tommy - Cancer Painrisalbalu100% (1)
- 2 - CNS QDocument4 pages2 - CNS QTan Hing LeeNo ratings yet
- TabletsDocument14 pagesTabletsMuhammad WaleedNo ratings yet
- Aerosol TherapyDocument12 pagesAerosol TherapyDejan ŽujovićNo ratings yet
- Kaimax BrochureDocument8 pagesKaimax Brochurekbeauty.pharmaNo ratings yet
- Analisis Waktu Tunggu Pelayanan Resep Di Puskesmas Pasir Panjang Kota Kupang Bulan April Tahun 2018Document8 pagesAnalisis Waktu Tunggu Pelayanan Resep Di Puskesmas Pasir Panjang Kota Kupang Bulan April Tahun 2018Ridhatul AzizahNo ratings yet
- Past-Years' Exam Questions Cns Anticonvulsant 3. Local AnaestheticDocument2 pagesPast-Years' Exam Questions Cns Anticonvulsant 3. Local Anaestheticnmyza89No ratings yet