Professional Documents
Culture Documents
Japan Journal Nursing Sci - 2015 - Albayrak Cosar - Scale Development Study The Fluid Control in Hemodialysis Patients
Japan Journal Nursing Sci - 2015 - Albayrak Cosar - Scale Development Study The Fluid Control in Hemodialysis Patients
Uploaded by
Alviyatus SalimahOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Japan Journal Nursing Sci - 2015 - Albayrak Cosar - Scale Development Study The Fluid Control in Hemodialysis Patients
Japan Journal Nursing Sci - 2015 - Albayrak Cosar - Scale Development Study The Fluid Control in Hemodialysis Patients
Uploaded by
Alviyatus SalimahCopyright:
Available Formats
bs_bs_banner
Japan Journal of Nursing Science (2016) 13, 174–182 doi:10.1111/jjns.12083
METHODOLOGICAL ARTICLE
Scale development study: The Fluid Control in
Hemodialysis Patients
Arife ALBAYRAK COSAR1 and Sezgi CINAR PAKYUZ2
1
Alanya Private Vocational and Technical High School, Antalya and 2Department of Internal Medicine, Celal Bayar University
School of Sciences Nursing, Manisa, Turkey
Abstract
Aim: The aim of this study was to develop a valid and reliable measurement instrument to identify
knowledge, behaviors, and attitudes of hemodialysis (HD) patients about fluid control as these patients are
inadequate in ensuring and sustaining fluid control.
Methods: The sample of this methodological study consisted of 276 HD patients who are being treated in
two public and two private hemodialysis centers. The validity of the scale was assessed through content
validity, construct validity, and similar scale validity, and its reliability through item analysis, internal
consistency coefficient and test–retest. For the content validity of the scale, expert views were assessed, and
opinions of a Turkish language specialist were obtained.
Results: According to the exploratory factor analysis, the scale had 24 items and three subdimensions,
namely, knowledge, behavior, and attitude. The total variance explained was found to be 51.15%.
Cronbach’s alpha reliability coefficient of the Fluid Control in Hemodialysis Patients Scale (FCHPS) turned
out to be 0.88 and Cronbach’s alpha for its subdimensions were 0.92, 0.80, and 0.67, respectively. The
correlation value between test and retest was 0.94 (P < 0.001). A moderate significant correlation (r = 0.58,
P < 0.001) was found between the scale scores and the scores of the Dialysis Diet and Fluid Restrictions
Non-adherence Questionnaire.
Conclusion: The FCHPS that was developed has good validity and reliability. This scale can be used to
measure knowledge, behavior, and attitude of hemodialysis patients about fluid restriction.
Key words: fluid control, hemodialysis, scale development.
INTRODUCTION the UF speed increases, complications such as hypoten-
sion, nausea/vomiting, dizziness, muscle cramps, and
Despite all the developments in hemodialysis therapy, malaise emerge in patients (Daugirdas, Blake, & Ing,
excess fluid intake between two dialysis sessions contin- 2003; Hoenich & Levin, 2003). Additionally, excess
ues to be a serious problem. If the weight gain (fluid fluid intake may result in hypervolemia, edema in lower
intake) between two dialysis sessions is more than 5.7% extremes, ascites, left ventricular hypertrophy, conges-
of the dry weight, this is defined as inappropriate tive heart failure, pulmonary vascular congestion, or
interdialytic weight gain (Hecking et al., 2004). acute pulmonary edema (Lindberg, 2010; Movilli et al.,
The fluid intake between two dialysis sessions during 2007).
a 4 h hemodialysis is drawn by ultrafiltration (UF). As Fluid control is a major problem in hemodialysis
Correspondence: Arife Albayrak Cosar, Oba Beldesi, patients (Denhaerynck et al., 2007; Lindberg, 2010) and
Çarşamba Mahallesi, 2 Soğancilar Çikmazi, Alanya/Antalya it is the most crucial restriction in patient diet (Pace,
07400, Turkey. Email: albayrakcosar@hotmail.com 2007). Research results show that 10–60% of hemodi-
Received 17 October 2014; accepted 23 March 2015. alysis patients are non-compliant with fluid control
© 2015 The Authors
Japan Journal of Nursing Science © 2015 Japan Academy of Nursing Science
17427924, 2016, 1, Downloaded from https://onlinelibrary.wiley.com/doi/10.1111/jjns.12083 by Nat Prov Indonesia, Wiley Online Library on [14/03/2024]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Japan Journal of Nursing Science (2016) 13, 174–182 Fluid control in hemodialysis
(Bame, Petersen, & Wray, 1993; Denhaerynck et al., MATERIALS AND METHODS
2007). Physical debility and depression are also seen in
patients not complying with fluid restriction (Welch & This study was of methodological design.
Davis, 2000). Therefore, excess fluid intake significantly
Study population and sample
increases morbidity in hemodialysis patients (Pace,
2007). The study population consisted of 430 chronic hemodi-
Eating and drinking are basic needs for humans and alysis patients who were being treated in two public and
are associated with sociocultural structure and tradi- two private dialysis centers in Istanbul in 2011. The
tions. For this reason, it is difficult for patients to change sample consisted of 276 chronic hemodialysis patients
their usual eating and drinking habits (Sagawa, Oka, who agreed to take part in the study and who met the
Chaboyer, Satoh, & Yamaguchi, 2001). Individuals inclusion criteria. The sample size was determined con-
receiving hemodialysis have different dietary habits, sidering the fact that the sample size suggested for meth-
knowledge, living conditions, and personal reactions to odological studies has to be 5–10 times more than the
prescribed limitations. They are prescribed a complex number of items in the scale (Özdamar, 2002).
diet that requires many cognitive and behavioral skills The inclusion criteria were: being between 18 and 65
for successful self-management. The methods that are years of age; undergoing a hemodialysis therapy three
agreed to be effective for ensuring compliance with fluid times a week for a period longer than 3 months; being
restriction include “Measuring the amount of fluid literate; having no communication disability such as
taken in during the whole day, apportioning the fluid to blindness, deafness, and aphasia; not having received a
be taken in during the whole day and avoiding salty psychiatric diagnosis; not having residual urine of more
food in their diets” (Welch & Davis, 2000; p. 394). The than 1 L; and having an interdialytic weight between 1
Dietary Intake Monitoring Application (DIMA) is and 5 kg.
extremely helpful for individuals as they self-monitor The cognitive abilities of hemodialysis patients were
their intake. If desired, DIMA could also be used for evaluated by a physician and the patients who were
dietary counseling (Welch et al., 2009). The DIMA is a found to have problems related to cognitive abilities
feasible and acceptable intervention that had a marginal were excluded.
effect on some aspects of dietary and fluid intake. (Welch The patients receiving hemodialysis in the morning
et al., 2013). The DIMA has potential to facilitate session were enrolled for the test–retest because it is easy
dietary and fluid self-monitoring but requires additional to reach these patients.
refinement and further testing (Welch et al., 2013).
Data collecting instrument
It is important for the hemodialysis nurses, who play
a key role in the treatment, care, and training of hemo- The study data were collected using a Patient Descrip-
dialysis patients, to know about the knowledge, behav- tion Form, the Fluid Control in Hemodialysis Patients
iors, and attitudes of patients about fluid control, so that Scale (FCHPS), and the Dialysis Diet and Fluid Restric-
they can train patients in issues they are not adequate tions Non-adherence Questionnaire (QDDF).
and develop custom-made fluid control methods. The
Patient description form
present authors have not encountered any measurement
instrument in the published work to be used for identi- This form includes sociodemographic characteristics
fying knowledge, behaviors, and attitudes of hemodialy- and data on the disease and treatment.
sis patients. Because the difficulty in fluid control is
FCHPS
among the serious problems still prevailing in hemodi-
alysis patients, there is a need to develop a valid and Preparation of an item pool for the scale
reliable measurement instrument for fluid control. At the first stage of the FCHPS, which is developed to
Because hemodialysis patients are inadequate in measure the knowledge, behaviors, and attitudes of
ensuring and sustaining fluid control, this study was chronic hemodialysis patients about fluid restriction, a
carried out for the purpose of developing a valid and question pool was formed in line with the information in
reliable measurement instrument to identify knowledge, the published work review (Pace, 2007; Sagawa et al.,
behaviors, and attitudes of patients about fluid control, 2001; Welch & Davis, 2000; Welch et al., 2009), inter-
so that their quality of life can be improved and their views, and the knowledge and experiences of the
safety secured by increasing their compliance with fluid researchers. Views of 20 hemodialysis patients on the
restriction. prepared questions were obtained. The patients were
© 2015 The Authors 175
Japan Journal of Nursing Science © 2015 Japan Academy of Nursing Science
17427924, 2016, 1, Downloaded from https://onlinelibrary.wiley.com/doi/10.1111/jjns.12083 by Nat Prov Indonesia, Wiley Online Library on [14/03/2024]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
A. Albayrak Cosar and S. C. Pakyuz Japan Journal of Nursing Science (2016) 13, 174–182
asked about comprehensibility of the questions and their consists of four items that assess patients’ behaviors of
positive or negative opinions and suggestions about the non-compliance to diet (items 1 and 2) and fluid (items
questions. The questions were prepared in line with the 3 and 4) based on their frequency and extent. The scale
patients’ opinions and suggestions and then presented to has a Likert-type structure (“no non-compliance”, 0;
a Turkish-language specialist for opinion. The necessary “slight”, 1; “moderate”, 2; “serious”, 3; “very serious”,
corrections were made in line with the recommendations 4). As the score obtained from the QDDF increases,
and a draft scale was formed containing 41 items that patient compliance to diet and fluid restriction
were agreed to appear in the scale. decreases. Kara (2009) found the Cronbach’s alpha
coefficient of the scale to be 0.70. The Cronbach’s alpha
Content validity of the FCHPS reliability coefficient was reassessed for this study and
For content validity, the draft scale of 41 items was sent found to be 0.84.
to 11 specialists including nephrologists, nurse instruc-
tors, and scale development specialists. The scale items
were assessed by these specialists as “appropriate”, Data collection and evaluation
“partly appropriate”, and “not appropriate”. A “your The study data were collected by the researchers
suggestions” section was opened next to each item to through face-to-face interviews with the patients. The
enable them to write their comments on the items. In data related to the disease and treatment, and biochemi-
evaluating the responses from the specialists, a content cal parameters were obtained from patient files. The
validity ratio (CVR) index was calculated for each item data were entered and evaluated on the SPSS program
and five items with CVR less than 0.59 were excluded version 17.0 (SPSS, Chicago, IL, USA). The patients’
from the scale (Murray et al., 2006; Odagiri et al., 2011; descriptive characteristics were assessed as percentage
Piliskin, Yurk, TammyHo, & Umans, 1996; Tamura and mean ± standard deviation (SD).
et al., 2010). The content validity defines the degree The scale was tested for reliability using the content
to which the items of the measurement instrument validity, construct validity, and similar scale validity
adequately reflect the construct to be measured methods. In content validity, the scale items were pre-
(Scholtes, Terwee, Rudolf, & Poolman, 2011). Addi- sented to specialists for their opinions. In determining
tionally, eight items in the scale were brought down to construct validity, the exploratory factor analysis (prin-
four items due to similarity as suggested by the special- cipal components analysis) was applied and the varimax
ists and three new items were added to obtain the final rotation method was used. For similar scale validity, the
version of the scale containing 35 items. The items that relationship between the QDDF and FCHPS was
were stated to be problematic by the specialists were assessed using Pearson correlation analysis.
corrected in line with the suggestions. Before adminis- In reliability assessment, the internal consistency was
tering the 35 item scale to all patients, it was adminis- determined using Cronbach’s alpha, Guttman’s and
tered to a pilot group of 20 hemodialysis patients by the Spearman–Brown reliability coefficient, item analysis
investigator to determine its comprehensibility and the (item–total, item–remainder, and item–discrimination
scale’s content validity was completed. Because cogni- indices), and test–retest techniques. For the test–retest
tive decline related to uremia were common among reliability, the relationship between the two applications
hemodialysis patients, the scale was prepared in the was assessed using Pearson correlation analysis.
form of a 3 point Likert-type scale (Murray et al., 2006;
Odagiri et al., 2011; Piliskin et al., 1996; Tamura et al.,
2010). The participants were asked to respond to each Ethical considerations
item as “agree”, “indecisive”, or “don’t agree”. This study was approved by the ethical review boards at
When assessing positive items, “agree” was scored 3, the authors’ institutions. Written permissions were
“indecisive” 2, and “don’t agree” 1. The negative items obtained from the private hemodialysis centers and
(6, 7, and 18–24) are reversely scored. Istanbul Provincial Health Directorate.
Care was taken to base the participation in the study
QDDF on volunteering principle, the patients were explained
The QDDF was developed by Vlaminc and associates about the study objective both verbally and through the
(2001) to assess non-compliance to diet and fluid restric- information form before the study and their written
tions in hemodialysis patients. It was tested for validity permissions were obtained through the Subject Informa-
and reliability in Turkey by Kara (2009). The QDDF tion and Consent Form.
176 © 2015 The Authors
Japan Journal of Nursing Science © 2015 Japan Academy of Nursing Science
17427924, 2016, 1, Downloaded from https://onlinelibrary.wiley.com/doi/10.1111/jjns.12083 by Nat Prov Indonesia, Wiley Online Library on [14/03/2024]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Japan Journal of Nursing Science (2016) 13, 174–182 Fluid control in hemodialysis
The participants were ensured that their identities and that were not suitable for the factor structure. At the end
information they provided would not be disclosed to of the rotation procedure, a structure was obtained
others. which consisted of three dimensions and 24 items with
homogeneous characteristics and 51.15% of whose
RESULTS variance was explained (Table 1). The three factors that
were obtained as a result of the factor analysis were
Results related to sociodemographic named as knowledge, behavior, and attitude in view of
characteristics of patients the item expressions they contained (Table 2).
The sample consisted of 276 chronic hemodialysis
patients and the majority of the patients were male Similar scale validity
(58.3%), in the 50–65 year age group (53.6%), and For similar scale validity, the FCHPS together with the
married (69.6%). Of the patients, 32.6% were retired, QDDF was administered to the group of 276 people and
47.8% unemployed, and most graduates of primary the correlation between them was assessed using
school (62.3%). Pearson correlation analysis. The FCHPS and QDDF
were found to be harmonious at a moderate level
Validity of the FCHPS in hemodialysis patients (r = −0.58, P < 0.001). This result meant that as the
Construct validity FCHPS scores increased, the QDDF scores decreased.
The principal components analysis was used to test the
scale’s construct validity and identify the factors. As a Reliability of the FCHPS
result of the exploratory factor analysis that was carried Internal consistency
out to explore the factor structure of FCHPS, the The scale’s general Cronbach’s alpha internal consis-
Kaiser–Meyer–Olkin (KMO) coefficient was found to be tency coefficient was 0.88. Its Spearman–Brown and
0.89 and the result of the Bartlett test to be P < 0.001. Guttman’s internal consistency coefficients, which were
The varimax rotation method was used to name and calculated by dividing the test into two equal halves,
easily interpret the factors. No limitation was applied to were 0.87 and 0.86. The internal consistency coefficients
the number of factors in the factor analysis and values of the scale’s subdimensions are given in Table 3.
with an eigenvalue greater than 1.00 were included in The scale’s item total correlations ranged 0.18–0.83
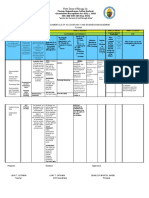
the scale. The scree plot of factor (subdimension) eigen- and item remaining correlations ranged 0.26–0.85
values is shown in Figure 1. When the plot is reviewed, (Table 4). The Student’s t-test values that show the item
there is a breaking point at the third factor and there is discrimination coefficients ranged 3.99–16.13. The
a rapid decline in the graph after this point. Therefore, entire items in the whole scale was found to be highly
the number of factors was limited to three in the scale. (P < 0.001) significant statistically.
After examining the initial results of the factor analy-
sis, the analysis was repeated after excluding 11 items Test–retest reliability
For the test–retest reliability to reveal invariability in
time, the scale was administered to a group of 35 people
10
twice with an interval of 15 days and the correlation
between the two administrations was assessed with
8
Pearson correlation analysis. A highly significant posi-
tive correlation was found between the scores of the first
6
and second administrations (r = 0.94, P < 0.001).
4
Eigenvalue
2 Table 1 Total variance explained and internal consistency
coefficients
0
1 3 5 7 9 11 13 15 17 19 21 23 Factors Eigenvalues % of variance Cumulative %
Component Number 1 8.58 35.78 26.39
2 1.92 8.00 40.52
Figure 1 Scree plot of the subdimensions of the fluid control
3 1.76 7.35 51.15
scale.
© 2015 The Authors 177
Japan Journal of Nursing Science © 2015 Japan Academy of Nursing Science
17427924, 2016, 1, Downloaded from https://onlinelibrary.wiley.com/doi/10.1111/jjns.12083 by Nat Prov Indonesia, Wiley Online Library on [14/03/2024]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
A. Albayrak Cosar and S. C. Pakyuz Japan Journal of Nursing Science (2016) 13, 174–182
Table 2 Result of factor analysis for the Fluid Control in Hemodialysis Patients (n = 276)
No. of Item no. Factor
Factor items included Items load
Factor 1 (knowledge) 7 1 Eating salty and spicy food increases fluid intake 0.89
3 Excess intake of fluid by dialysis patients causes swelling in the body 0.89
(face, legs, and feet)
5 Some other foods also increase weight (fluid) 0.69
8 Taking in more than 2–3 L of fluid between two dialysis sessions is 0.88
harmful
16 Excess water drinking causes shortness of breath in dialysis patients 0.79
30 The higher the fluid intake is between two dialysis sessions, the more 0.79
comfortable that dialysis session is
35 Excess intake of fluid by dialysis patients lowers blood pressure 0.84
Factor 2 (behavior) 6 I use a measuring cup when taking fluid food 0.32
13 I consume food in brine such as cheese and olives after I keep them in 0.38
water for a while (1 h)
15 I keep away from activities that cause me to drink much fluid 0.60
18 Fluid restriction prevents me from eating outside 0.58
11 19 I drink my beverages sip by sip over a long time 0.31
23 I keep a record of how much fluid I take in daily 0.50
26 I rinse my mouth when I feel thirsty 0.64
27 I chew gum to overcome my thirst 0.57
29 I take care not to put salt on my food 0.56
33 I avoid salty food such as pickles, chips, sunflower seeds, and crisps 0.30
34 I cannot restrict fluids when meeting with friends 0.62
Factor 3 (attitude) 10 I find it very difficult to comply with fluid restriction 0.61
11 There are times when I do not comply with fluid restriction 0.67
6 17 There are times when I exceed 2 L of fluid between two dialysis 0.40
sessions
20 I have no idea how I can reduce my need for water 0.65
25 I feel more thirsty when I leave the dialysis session 0.66
31 Using a lot of drugs increases my intake of fluid 0.39
Table 3 Internal consistency coefficients ity, and construct validity are used (Büyüköztürk, 2008;
Factors Cronbach’s alpha Spearman–Brown* Guttman* Tavşancıl, 2006; Şencan, 2005).
For the content validity of the scale, the scale was
1 0.92 0.91 0.92
presented to specialists for their views and specialist
2 0.80 0.75 0.81
views were assessed. Then, the opinions of a Turkish-
3 0.67 0.62 0.66
language specialist were obtained and the scale was
*P < 0.001.
presented to the hemodialysis patients for their views
and in this way the content validity was secured.
The exploratory factor analysis was used to assess
DISCUSSION construct validity and to identify factors. Whether or
not a factor analysis will be applied to a scale used and
For a study to be strong scientifically, the measurement suitability of data are assessed through the KMO and
instrument used (data collection instrument) should be a Bartlett tests. The KMO test assesses whether the distri-
valid and reliable instrument (Şencan, 2005). bution is sufficient for a factor analysis and 0.80–0.90
interval is evaluated as very good (Şencan, 2005). The
Validity of the FCHPS KMO value is 0.899 in this study and the sample size
In assessing validity of a data collection instrument, the can be considered to be very good to be able to carry
methods of face validity, content validity, criterion valid- out a factor analysis. Whether the data come from a
178 © 2015 The Authors
Japan Journal of Nursing Science © 2015 Japan Academy of Nursing Science
17427924, 2016, 1, Downloaded from https://onlinelibrary.wiley.com/doi/10.1111/jjns.12083 by Nat Prov Indonesia, Wiley Online Library on [14/03/2024]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Japan Journal of Nursing Science (2016) 13, 174–182 Fluid control in hemodialysis
Table 4 Results of item analyses and internal consistency coefficients of the Fluid Control in Hemodialysis Patients (n = 276)
Item Item Item Cronbach’s alpha
Item no. total* remaining* discrimination* if item removed
M.01 0.83 0.85 6.36 0.87
M.03 0.82 0.84 6.18 0.87
M.05 0.51 0.55 4.55 0.88
M.06 0.19 0.27 3.99 0.89
M.08 0.83 0.85 6.41 0.87
M.10 0.34 0.42 8.71 0.88
M.11 0.45 0.52 12.22 0.88
M.13 0.67 0.70 7.25 0.87
M.15 0.47 0.53 7.99 0.88
M.16 0.50 0.56 6.94 0.88
M.17 0.36 0.43 7.76 0.88
M.18 0.26 0.35 4.85 0.88
M.19 0.51 0.57 7.81 0.88
M.20 0.18 0.26 5.63 0.89
M.23 0.40 0.47 9.06 0.88
M.25 0.38 0.45 11.44 0.88
M.26 0.46 0.52 16.08 0.88
M.27 0.53 0.58 8.38 0.88
M.29 0.49 0.56 16.13 0.88
M.30 0.56 0.60 4.50 0.88
M.31 0.35 0.44 7.56 0.88
M.33 0.66 0.69 6.59 0.87
M.34 0.51 0.57 11.05 0.88
M.35 0.81 0.82 5.79 0.87
*P < 0.001.
multivariate and normal distribution is assessed with the present authors used the principal components analysis
Bartlett test. The Bartlett test is said to give χ2-statistic and the varimax rotation method. No limitation was
value, and if the significance value is less than 0.05, the applied to the number of factors in the study and factors
factors can be identified (Şencan, 2005). The result of with an eigenvalue greater than 1.00 were included in
the Bartlett test in this study turned out to be P < 0.001. the scale. Higher variance rates obtained from a factor
This result indicated that data were suitable to carry out analysis indicate a strong factor structure in the scale
a factor analysis. and variance rates ranging 40–60% are considered ideal
Although there are various methods for an explor- (Şencan, 2005). The total variance amount obtained in
atory factor analysis that is to be performed according the present authors’ study (51.15%) can be said to be
to the results of Bartlett and KMO tests, the principal ideal.
components analysis is used in general. The rotation A factor loading value is a coefficient explaining the
technique is used to name the factors and easily interpret relationship of items with subdimensions. It is stated in
them. The rotation technique is an orthogonal rotation the published work that factor loads ranging 0.30–0.40
and it can be varimax, equamax, or quartimax (Baydur can be taken as the lower cut-off point when designing
& Eser, 2006). The eigenvalue is used to decide on the the factor pattern (Büyüköztürk, 2008; Gözüm &
number of factors. The eigenvalue is employed in both Aksayan, 2003; Şencan, 2005; Tavşancıl, 2006). The
calculating the variance explained by the factors and lower cut-off point was set at 0.30 in this study. When
deciding on the number of significant factors. In factor the first outcomes of the factor analysis were reviewed,
analysis, factors with an eigenvalue of 1 or more are seven items were seen to have a factor load value less
considered as significant factors. As the eigenvalue than 0.30. At the end of the factor analysis, the FCHPS
increases, the explained variance rates also increase consisting of three subdimensions and 24 items was
(Baydur & Eser, 2006; Şencan, 2005). In this study, the formed. After rotation of factors, the first subdimension
© 2015 The Authors 179
Japan Journal of Nursing Science © 2015 Japan Academy of Nursing Science
17427924, 2016, 1, Downloaded from https://onlinelibrary.wiley.com/doi/10.1111/jjns.12083 by Nat Prov Indonesia, Wiley Online Library on [14/03/2024]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
A. Albayrak Cosar and S. C. Pakyuz Japan Journal of Nursing Science (2016) 13, 174–182
of the scale (knowledge) included seven items, the two items in the FCHPS remained below 0.20, but the
second subdimension (behavior) 11 items, and the third present authors decided to keep these items in the scale,
subdimension (attitude) six items. because exclusion of these would lower the Cronbach’s
Another method to assess validity in a scale develop- alpha coefficient, the item total correlations were high
ment effort is to look at the correlation between the in the subdimensions where these items were and the
scores obtained from the scale being developed and the items were statistically significant. Item discrimination
scores of another measurement instrument that had is a comparison of the mean scores given to each item
been developed previously which measures a similar by the terminal groups (upper group, lower group)
characteristic and is known to have a high validity. In when the groups are sequenced from the highest score
comparisons with similar scales, correlation coefficients to the lowest score according to the total scores
between 0.50 and 0.70 that show a moderate relation- obtained from the scale. The difference between the
ship are considered to be the proof of validity (Şencan, item averages of the lower group (the part in the lower
2005). The FCHPS the present authors were developing 27%) and the upper group (the part in the upper 27%)
and the QDDF were found to be in harmony at a mod- that are formed according to the test’s total scores are
erate level (r = 0.58, P < 0.001). According to this result, compared using Student’s t-test for independent groups
as the fluid control scale scores go up, the QDDF scores (Şencan, 2005). The present authors decided to keep all
go down. Given these results, the FCHPS and QDDF the items in the scale when they observed that the item
show similarity. total, item remaining, and item discrimination features
at there FCHPS overall and subdimensions were statis-
Reliability of the FCHPS tically significant. These results prove that the items are
Reliability is about to what extent a test or a measure- discriminative with respect to the characteristic they
ment instrument measures that which it measures cor- measure, and the reliabilities of the items in the scale
rectly. A measurement instrument should measure the are high and they are meant to measure the same
aspect it measures consistently and should produce the objective.
same results when it is administered once more under Cronbach’s alpha coefficient, which is used for
the same conditions (Ercan & Kan, 2004; Şencan, measuring the reliability of Likert-type scales, is calcu-
2005). Although there are various methods to assess the lated for the adapted scale and its subdimensions and
reliability of a scale being developed, the present authors this coefficient provides information on consistency/
used item analyses, Cronbach’s alpha, Spearman–Brown homogeneity of the items (Büyüköztürk, 2008; Şencan,
and Guttman’s internal consistency coefficients, and 2005). Cronbach’s alpha coefficient for the total FCHPS
test–retest reliability. was found to be good and for the subdimension of
The item analysis is meant to calculate item statistics, knowledge to be highly, behavior to be good, and atti-
to choose the items that can be directly included in the tude to be moderate. Moderate Cronbach’s alpha coef-
test, to identify items that can be added to the test after ficients (>0.60) are assumed to indicate that the scale is
being corrected, and to discard the items that are not composed of more consistent items (Öksüz & Malhan,
possible to include in the test. Although there is no 2005; Özdamar, 2002). According to Özdamar (2002),
distinct standard as to below what measure the item if Cronbach’s alpha internal consistency coefficient of a
total correlation falls to consider its reliability insuffi- scale is within the interval of 0.80–0.99, then the scale is
cient, 0.20 is used as the lower limit in practice (Gözüm highly reliable. These results indicate that all the items in
& Aksayan, 2003). The item remaining correlation is the scale measure the same feature; in other words, the
the relationship of the item in question with the total feature measured by the FCHPS is homogenous and the
score obtained from the other items excluding the item FCHPS is a reliable measurement instrument.
in question. Both in item total and item remaining, the The test–retest reliability, which is performed to reveal
results are expected to be at a minimum of P < 0.05 the stability of an instrument over time, involves admin-
level statistically (Şencan, 2005). In the present authors’ istration of a scale developed to the same group under
study, the item total score correlations ranged 0.18– the same conditions in a certain interval and looking at
0.83 and the item remaining correlation coefficients the relationship in between using the Pearson correla-
0.26–0.85. In the item analyses made for all the tion. The correlation coefficient is expected to show a
subdimensions of the FCHPS, the item total and item positive and high-level relationship. The test–retest cor-
remaining correlations of the entire subdimensions relation of the present authors’ scale was high, indicat-
were observed to be high. The item total coefficients of ing a good stability over time. This means that the
180 © 2015 The Authors
Japan Journal of Nursing Science © 2015 Japan Academy of Nursing Science
17427924, 2016, 1, Downloaded from https://onlinelibrary.wiley.com/doi/10.1111/jjns.12083 by Nat Prov Indonesia, Wiley Online Library on [14/03/2024]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Japan Journal of Nursing Science (2016) 13, 174–182 Fluid control in hemodialysis
FCHPS can ensure similar measurement outcomes in supervised the whole study process. All authors read and
repeated measurements and is consistent over time. approved the final manuscript.
In this study, the total mean score obtained from
the FCHPS was 56.55 ± 6.37, the mean knowledge
REFERENCES
subdimension score was 19.80 ± 1.59, the mean behav-
ior subdimension score was 25.5 ± 4.54, and the mean Bame, S. I., Petersen, N. & Wray, N. P. (1993). Variation in
attitude subdimension score was 11.21 ± 3.35. An hemodialysis patient compliance according to demo-
increase in the total score indicates that the knowledge, graphic characteristics. Social Science & Medicine, 37,
behaviors, and attitudes of hemodialysis patients about 1035–1043.
fluid control are positive and a decrease that they are Baydur, H. & Eser, E. (2006). Yaşam Kalitesi Ölçeklerinin
negative. Psikometrik Çözümlemesi. Sağlikta Birikim Dergisi, 1,
99–123 (in Turkish).
Büyüköztürk, Ş. (2008). Sosyal Bilimler için Veri Analizi El
Limitations of this study Kitabi (9nd edn). Ankara: Pegem Akademi.
A limitation of the study is that it cannot be generalized Daugirdas, J. T., Blake, P. G. & Ing, T. S. (2003). Handbook of
for the entire HD patients, because the study population dialysis (3nd edn). Bozfakioğlu, S: Güneş Kitabevi.
includes only the HD centers that could be reached by Denhaerynck, K., Manhaeve, D., Dobbels, F., Garzoni, D.,
the researchers in Istanbul. Nolte, C. & De Geest, S. (2007). Prevalence and conse-
quences of nonadherence to hemodialysis regimens.
American Journal of Critical Care, 16, 222–235.
CONCLUSION Ercan, İ. & Kan, İ. (2004). Reliability and validity in the scales.
Uludağ Universitesi Tip Fakultesi Dergisi, 30, 211–216
The FCHPS is a good validity and reliability measure- (in Turkish).
ment instrument measuring the knowledge, behaviors, Gözüm, S. & Aksayan, S. (2003). A guide for transcultural
and attitudes of hemodialysis patients about fluid adaptation of the scale II: Psychometric characteristics
restriction. The scale can be used by doctors, nurses, and and cross-cultural comparison. Hemşirelikte Araştirma
Geliştirme Dergisi, 5, 3–14 (in Turkish).
other health professionals in developing personal fluid
Hecking, E., Bragg-Gresham, J. L., Rayner, H. C., Pisoni, R.
restriction methods before and after training on fluid
N., Andreucci, V. E., Combe, C. et al. (2004).
restriction to be given to hemodialysis patients. The Haemodialysis prescription, adherence and nutritional
present authors recommend that the scale be tested for indicators in five European countries: Results from the
validity and reliability for various cultures to verify that Dialysis Outcomes and Practice Patterns Study (DOPPS).
its factor structure is preserved. Nephrology, Dialysis Transplantation, 19, 100–107.
Hoenich, N. A. & Levin, N. W. (2003). Can technology-
solvetheclinical problem of “dryweight”? Nephrology,
ACKNOWLEDGMENTS Dialysis, Transplantation, 18, 647–650.
Kara, B. (2009). A validity and reliability study of the nonad-
The authors thank all patients who participated in this herence questionnaire with dialysis diet and fluid restric-
study. tions. Atatürk Üniversitesi Hemşirelik Yüksekokulu
Dergisi, 12, 20–27 (in Turkish).
Lindberg, M. (2010). Excessive fluid overload among
CONFLICT OF INTEREST haemodialysis patients. Prevalence, individual characteris-
tics and self-regulation of fluid intake. Acta Universitatis
The authors declare that there is no conflict of interest in Upsaliensis. Digital Comprehensive summaries of uppsala
publishing this research article. There are no sources of dissertations from the faculty of medicine. Uppsala.
funding and the role of funders in the conduct of the Movilli, E., Gaggia, P., Zubani, R., Camerini, C., Vizzardi, V.,
research. Parrinello, G. et al. (2007). Association between high
ultrafiltration rates and mortality in uraemic patients on
regular haemodialysis. A 5-year prospective observational
AUTHOR CONTRIBUTIONS multicentre study. Nephrology, Dialysis, Transplantation,
22, 3547–3552.
A. A. C. contributed to acquisition of data, drafted data Murray, A. M., Tupper, D. E., Knopman, D. S., Gilbertson, D.
of this study, and drafted the manuscript. S. C. contrib- T., Pederson, S. L., Li, S. et al. (2006). Cognitive impair-
uted to the conception and design, interpreted the sta- ment in hemodialysis patient is common. Neurology, 67,
tistical analysis, critically reviewed the manuscript, and 216–223.
© 2015 The Authors 181
Japan Journal of Nursing Science © 2015 Japan Academy of Nursing Science
17427924, 2016, 1, Downloaded from https://onlinelibrary.wiley.com/doi/10.1111/jjns.12083 by Nat Prov Indonesia, Wiley Online Library on [14/03/2024]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
A. Albayrak Cosar and S. C. Pakyuz Japan Journal of Nursing Science (2016) 13, 174–182
Odagiri, G., Sugawara, N., Kikuchi, A., Takahashi, I., Umeda, Tamura, M. K., Larive, B., Unruh, M. L., Stokes, J. B.,
T., Saitoh, H. et al. (2011). Cognitivefunctionamong- Nissenson, A., Mehta, R. L. et al. (2010). Prevalence
hemodialysispatients in Japan. Annals of General Psychia- and correlates of cognitive impairment in hemodialysis
try, 10, 1–5. patients: The frequent hemodialysis network trials. Clini-
Öksüz, E. & Malhan, S. (2005). Sağliğa bağli yaşam kalitesi cal Journal of the American Society of Nephrology, 5,
kalitemetri. Ankara: Başkent Üniversitesi. 1429–1438.
Özdamar, K. (2002). Güvenirlik ve Soru Analizi. In: Özdamar Tavşancıl, E. (2006). Tutumlarin ölçülmesi ve SPSS ile veri
K (Ed.), Paket Programlar ile İstatistiksel Veri Analizi analizi (2nd edn). İstanbul: Nobel Yayin Dağitim.
(4nd edn, pp. 511–525). Eskişehir: Etam AŞ. Welch, J. L., Astroth, K. S., Perkins, S. M., Johnson, C.,
Pace, R. C. (2007). Fluidmanagement in patients on hemodi- Connelly, K., Siek, K. et al. (2013). Using a mobile appli-
alysis. Nephrology Nursing Journal, 34, 557–559. cation to self-monitor diet and fluid intake among adults
Piliskin, N. H., Yurk, H. M., TammyHo, L. & Umans, J. G. receiving hemodialysis. Research in Nursing & Health,
(1996). Neurocognitivefunction in chronic hemodialysis 36, 284–298.
patients. Kidney International, 49, 1435–1440. Welch, J. L. & Davis, J. (2000). Self-care strategies to reduce
Sagawa, M., Oka, M., Chaboyer, W., Satoh, W. & Yamaguchi, fluid intake and control thirst in hemodialysis patients.
M. (2001). Cognitive behavioral therapy for fluid control Nephrology Nursing Journal, 27, 393–395.
in hemodialysis patients. Nephrology Nursing Journal, Welch, J. L., Siek, K. A., Connelly, K. H., Astroth, K. S.,
28, 37–39. McManus, M. S., Scott, L. et al. (2009). Merging health
Scholtes, V. A., Terwee, C. B., Rudolf, W. & Poolman, R. W. literacy with computer technology: Self-managing diet and
(2011). What makes a measurement instrument valid and fluid intake among adult hemodialysis patients. Patient
reliable? Injury, 42, 236–240. Education and Counseling, 79, 192–198.
Şencan, H. (2005). Sosyal ve Davranişsal Ölçümlerde
Güvenilirlik ve Geçerlilik (2nd edn). Ankara: Seçkin
Yayincilik.
182 © 2015 The Authors
Japan Journal of Nursing Science © 2015 Japan Academy of Nursing Science
You might also like
- Chem 28 SyllabusDocument11 pagesChem 28 SyllabusDianne TorrecampoNo ratings yet
- 2019 Article 1596Document9 pages2019 Article 1596Arina FitrianiNo ratings yet
- Clinical Epidemiology and Global Health: Original ArticleDocument4 pagesClinical Epidemiology and Global Health: Original Articleinnani wildaniaNo ratings yet
- Effects of A Free Water Protocol On Inpatients inDocument7 pagesEffects of A Free Water Protocol On Inpatients inCamila Jaque RamosNo ratings yet
- Graziella Allana Serra Alves de Oliveira Olle 2018Document12 pagesGraziella Allana Serra Alves de Oliveira Olle 2018Anindya Laksmi LarasatiNo ratings yet
- Rajiv Gandhi University of Health Sciences, Karnataka BangaloreDocument13 pagesRajiv Gandhi University of Health Sciences, Karnataka BangaloreFebri SuryoNo ratings yet
- GROUP 4 EBP On Renal NursingDocument7 pagesGROUP 4 EBP On Renal Nursingczeremar chanNo ratings yet
- Marie Antonette D.O. TanDocument159 pagesMarie Antonette D.O. TanJeffreydanceljr100% (5)
- Preference Dry WeightDocument8 pagesPreference Dry WeightdharmaNo ratings yet
- Contributing Factors To Hemodialysis Adherence in Aceh, Indonesia - ScienceDirectDocument6 pagesContributing Factors To Hemodialysis Adherence in Aceh, Indonesia - ScienceDirectlaamaghfirohNo ratings yet
- Association Between Hemodialysis Adequacy, Family Support, and Quality of Life in Chronic Renal Failure PatientsDocument10 pagesAssociation Between Hemodialysis Adequacy, Family Support, and Quality of Life in Chronic Renal Failure PatientsJelisaaNo ratings yet
- Jurnal 5Document8 pagesJurnal 5innani wildaniaNo ratings yet
- Albumin in aSAH NeuroCrit2023Document11 pagesAlbumin in aSAH NeuroCrit2023Ahida VelazquezNo ratings yet
- The Compliance Chronic Renal Failure Patient On Restrictions Liquids in Hemodialysis TherapyDocument7 pagesThe Compliance Chronic Renal Failure Patient On Restrictions Liquids in Hemodialysis TherapyJurnal Ners UNAIRNo ratings yet
- Fluid and Dietary Restriction's Effi Cacy On Chronic Kidney Disease Patients in HemodialysisDocument9 pagesFluid and Dietary Restriction's Effi Cacy On Chronic Kidney Disease Patients in HemodialysisfitriNo ratings yet
- The Association Between High Volume Intraoperative Fluid Administration and Outcomes Among Pediatric Patients Undergoing Large Bowel ResectionDocument7 pagesThe Association Between High Volume Intraoperative Fluid Administration and Outcomes Among Pediatric Patients Undergoing Large Bowel ResectionPablo Segales BautistaNo ratings yet
- Improving Adherence and Biomedical Markers in Hemodialysis Patients: The Effects of Relaxation TherapyDocument9 pagesImproving Adherence and Biomedical Markers in Hemodialysis Patients: The Effects of Relaxation TherapyheriNo ratings yet
- Resume Jurnal ADocument11 pagesResume Jurnal AannisaNo ratings yet
- MousaDocument12 pagesMousaGiriNo ratings yet
- The Relationship Between Social Support With Dietary and Fluids Restrictions Adherence Among Hemodialysis Patients in IndonesiaDocument5 pagesThe Relationship Between Social Support With Dietary and Fluids Restrictions Adherence Among Hemodialysis Patients in IndonesiaIndah Ayu KustianingsihNo ratings yet
- Acta Anaesthesiol Scand - 2022 - JessenDocument10 pagesActa Anaesthesiol Scand - 2022 - Jessenนิ่ม มมNo ratings yet
- Protein Energy Malnutrition in CKD PatientsDocument4 pagesProtein Energy Malnutrition in CKD PatientsEditor IJTSRDNo ratings yet
- Japan Journal Nursing Sci - 2014 - Efe - Adherence To Diet and Fluid Restriction of Individuals On Hemodialysis TreatmentDocument11 pagesJapan Journal Nursing Sci - 2014 - Efe - Adherence To Diet and Fluid Restriction of Individuals On Hemodialysis TreatmentCacaNo ratings yet
- Early TIPS Versus Endoscopic Therapy For Secondary Prophylaxis After Management of Acute Esophageal Variceal Bleeding in Cirrhotic Patients: A Meta-Analysis of Randomized Controlled TrialsDocument26 pagesEarly TIPS Versus Endoscopic Therapy For Secondary Prophylaxis After Management of Acute Esophageal Variceal Bleeding in Cirrhotic Patients: A Meta-Analysis of Randomized Controlled Trialsray liNo ratings yet
- Original Article: Saudi Journal of Kidney Diseases and TransplantationDocument5 pagesOriginal Article: Saudi Journal of Kidney Diseases and TransplantationNiponis ChunchunNo ratings yet
- Four Phases of Intravenous Fluid Therapy: A Conceptual ModelDocument8 pagesFour Phases of Intravenous Fluid Therapy: A Conceptual ModelriahtakarinaNo ratings yet
- Effect of Comprehensive Nursing Strategies On Thirst Distress Management Among The Patients With Chronic Kidney Disease (CKD)Document6 pagesEffect of Comprehensive Nursing Strategies On Thirst Distress Management Among The Patients With Chronic Kidney Disease (CKD)yanuar esthoNo ratings yet
- Manajemen Cairan Pada Pasien Hemodialisis Untuk Meningkatkan Kualitas Hidup Di RSUD Dr. Harjono PonorogoDocument11 pagesManajemen Cairan Pada Pasien Hemodialisis Untuk Meningkatkan Kualitas Hidup Di RSUD Dr. Harjono PonorogonikaNo ratings yet
- Prob 2Document12 pagesProb 2jinsi georgeNo ratings yet
- Tips For Dialysis Patients With Fluid Restrictions: Melanie Wong, BS, Parianna Ghebleh, BS, and Stacey Phillips, MS, RDDocument4 pagesTips For Dialysis Patients With Fluid Restrictions: Melanie Wong, BS, Parianna Ghebleh, BS, and Stacey Phillips, MS, RDanarosli251No ratings yet
- PIIS2213398416300380Document6 pagesPIIS2213398416300380LiliNurmawatiNo ratings yet
- Noninvasive Monitoring 2016Document6 pagesNoninvasive Monitoring 2016Maria LaiaNo ratings yet
- Acta Anaesthesiol Scand - 2022 - Jessen - Fluid Management of Emergency Department Patients With Sepsis A Survey of FluidDocument10 pagesActa Anaesthesiol Scand - 2022 - Jessen - Fluid Management of Emergency Department Patients With Sepsis A Survey of FluidEros CastellaniNo ratings yet
- Environmental Research and Public Health: International Journal ofDocument12 pagesEnvironmental Research and Public Health: International Journal ofdarnila watiNo ratings yet
- Family Concern: Facilitating Self-Management of Patients Undergoing HemodialysisDocument4 pagesFamily Concern: Facilitating Self-Management of Patients Undergoing HemodialysisGalica GalicaNo ratings yet
- Ghimire 2016Document7 pagesGhimire 2016john markNo ratings yet
- Comparison The Effect of High Flux and Low Flux Dialyzer On Quality of Life in Hemodialysis Patients A Clinical TrialDocument8 pagesComparison The Effect of High Flux and Low Flux Dialyzer On Quality of Life in Hemodialysis Patients A Clinical TrialMrQmonkNo ratings yet
- The Effects of Nursing of Roy Adaptation Model On The Elderly Hypertensive: A Randomised Control StudyDocument10 pagesThe Effects of Nursing of Roy Adaptation Model On The Elderly Hypertensive: A Randomised Control Studyjinsi georgeNo ratings yet
- Questionnaire Survey On Nutritional Supplement TheDocument10 pagesQuestionnaire Survey On Nutritional Supplement Theanselma.villafrancaNo ratings yet
- Effects of Oral Intake of WateDocument11 pagesEffects of Oral Intake of WateChenNo ratings yet
- Identification of The Needs of Haemodialysis Patients Using The Concept of Maslow's Hierarchy of NeedsDocument8 pagesIdentification of The Needs of Haemodialysis Patients Using The Concept of Maslow's Hierarchy of NeedsAlyssa LeonesNo ratings yet
- Nutritional Status and Malnutrition Prevalence Among Maintenance Hemodialysis PatientsDocument8 pagesNutritional Status and Malnutrition Prevalence Among Maintenance Hemodialysis PatientsIOSRjournalNo ratings yet
- Ojsadmin, 12Document5 pagesOjsadmin, 12Yohana SimanjuntakNo ratings yet
- Dwi Arya Jurnal UjianDocument8 pagesDwi Arya Jurnal Ujianwulan nadiaNo ratings yet
- Salina Vs GlucosadaDocument10 pagesSalina Vs GlucosadaEmmanuel Guar HuaNo ratings yet
- The Most Frequent Diagnosis On Patients Undergoing HemodialysisDocument5 pagesThe Most Frequent Diagnosis On Patients Undergoing HemodialysisChristine Rose EmNo ratings yet
- Fluid Balance and Optimal Hydration Guideline For Adult InpatientsDocument6 pagesFluid Balance and Optimal Hydration Guideline For Adult InpatientsOvidiu MCNo ratings yet
- JNursMidwiferySci7294-9611226 024011Document5 pagesJNursMidwiferySci7294-9611226 024011Nurul SaufikaNo ratings yet
- s00134 022 06882 ZDocument18 pagess00134 022 06882 ZEmmanuel Hernandez SantiagoNo ratings yet
- Prevention of Dehydration in Hospital PatientsDocument6 pagesPrevention of Dehydration in Hospital PatientseatthescrollNo ratings yet
- DiabetesDocument15 pagesDiabetesJunior GonzalesNo ratings yet
- Safety ChecklistDocument8 pagesSafety ChecklistdharmaNo ratings yet
- The Effect of Intradialytic Aerobic Exercise On Dialysis Efficacy in Hemodialysis Patients: A Randomized Controlled TrialDocument5 pagesThe Effect of Intradialytic Aerobic Exercise On Dialysis Efficacy in Hemodialysis Patients: A Randomized Controlled TrialFitriatun NisaNo ratings yet
- Yuanita PanmaDocument6 pagesYuanita PanmaHagane TetsuNo ratings yet
- Advances in The Management of Pediatric Septic Shock: Old Questions, New AnswersDocument7 pagesAdvances in The Management of Pediatric Septic Shock: Old Questions, New AnswersSandip KumarNo ratings yet
- ST RD ST NDDocument25 pagesST RD ST NDdevanganduNo ratings yet
- Jurnal 16 inDocument11 pagesJurnal 16 inAn anonymousNo ratings yet
- Common Sense Approach To Managing SepsisDocument12 pagesCommon Sense Approach To Managing SepsiszepedrocorreiaNo ratings yet
- RMHP 14 1823Document9 pagesRMHP 14 1823Deny SyachputraNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 8: UrologyFrom EverandComplementary and Alternative Medical Lab Testing Part 8: UrologyRating: 3 out of 5 stars3/5 (1)
- Evaluation and Management of Dysphagia: An Evidence-Based ApproachFrom EverandEvaluation and Management of Dysphagia: An Evidence-Based ApproachDhyanesh A. PatelNo ratings yet
- Irctcs E-Ticketing Service Electronic Reservation Slip (Personal User)Document1 pageIrctcs E-Ticketing Service Electronic Reservation Slip (Personal User)Jay ParkheNo ratings yet
- Methods-Time Measurement: MODAPTS Technique. This Technique Was Introduced in 1966 byDocument2 pagesMethods-Time Measurement: MODAPTS Technique. This Technique Was Introduced in 1966 byChisom IkengwuNo ratings yet
- Activity - 2 - (Discretel) (A1)Document1 pageActivity - 2 - (Discretel) (A1)AnkitChutaniNo ratings yet
- Notre Dame of Masiag, Inc.: What Formativ e Question S Shall Lead To The Completi On of Efaa? ToDocument2 pagesNotre Dame of Masiag, Inc.: What Formativ e Question S Shall Lead To The Completi On of Efaa? ToLANY T. CATAMINNo ratings yet
- 03 Splash Park Design PDFDocument13 pages03 Splash Park Design PDFKikie Felis SilvestrisNo ratings yet
- Recruiting StrategiesDocument10 pagesRecruiting StrategiesAbhijeet PatraNo ratings yet
- Tổng Hợp Đề Thi Và Bài Mẫu IELTS Writing Năm 2021Document38 pagesTổng Hợp Đề Thi Và Bài Mẫu IELTS Writing Năm 2021Đoan Trang Trần NữNo ratings yet
- Forget No MoreDocument14 pagesForget No MoreSheeqin Mn100% (2)
- Talent Acquisition 2008 - Survey and Analysis of The Changing Recruiting Landscape PDFDocument20 pagesTalent Acquisition 2008 - Survey and Analysis of The Changing Recruiting Landscape PDFVaishnavi SivaNo ratings yet
- Expt. 8 Salivary DigestionDocument25 pagesExpt. 8 Salivary DigestionLESLIE JANE BALUYOS JALANo ratings yet
- Institutions and Regional Integration in AfricaDocument24 pagesInstitutions and Regional Integration in AfricaOrnela FabaniNo ratings yet
- Boiler WaterDocument70 pagesBoiler WaterDarius DsouzaNo ratings yet
- Full Download Elementary Statistics A Step by Step Approach Bluman 9Th Edition Solutions Manual PDFDocument49 pagesFull Download Elementary Statistics A Step by Step Approach Bluman 9Th Edition Solutions Manual PDFsteven.engelke246100% (21)
- Principles of Electricity PDFDocument371 pagesPrinciples of Electricity PDFJohn C. Stephens100% (5)
- Lewis Dot Structures #1Document3 pagesLewis Dot Structures #1Dustin MoenchNo ratings yet
- Free Bhel Transformer Book PDFDocument4 pagesFree Bhel Transformer Book PDFMilan ShahNo ratings yet
- Marketing Plan: GoldilocksDocument18 pagesMarketing Plan: GoldilocksAkhia Visitacion100% (1)
- Chapter 9 LectureDocument29 pagesChapter 9 Lectureinam vf100% (6)
- ABLRFD v1403 Summary RevisionsDocument2 pagesABLRFD v1403 Summary RevisionsMiguel AngelNo ratings yet
- Safety Grating CatalogDocument22 pagesSafety Grating CatalogzhukeeNo ratings yet
- Block 3Document17 pagesBlock 3Dianne ChristineNo ratings yet
- John Hagstrom: Philip BiggsDocument4 pagesJohn Hagstrom: Philip BiggsDarci HallNo ratings yet
- 3 2 A UnitconversionDocument6 pages3 2 A Unitconversionapi-312626334No ratings yet
- PetretecDocument8 pagesPetretecVenkatesan KrishnachariNo ratings yet
- Crane Design Guide 2Document8 pagesCrane Design Guide 2Mesfin Derbew0% (1)
- Chapter 10 - Eco LiteracyDocument15 pagesChapter 10 - Eco LiteracyMichelle Bandoquillo100% (1)
- Yealink Phone UserGuide PDFDocument2 pagesYealink Phone UserGuide PDFEric SmithNo ratings yet
- Chapter#3 - Assignmnet ProblemDocument36 pagesChapter#3 - Assignmnet ProblemHarishNo ratings yet
- Important Questions For MID I CNDocument14 pagesImportant Questions For MID I CN20H51A0540-NAKKA SREEKAR B.Tech CSE (2020-24)No ratings yet