Professional Documents
Culture Documents
Jama Jabornisky 2024 Ed 230116 1705616418.4945
Jama Jabornisky 2024 Ed 230116 1705616418.4945
Uploaded by
Prima Hari NastitiOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Jama Jabornisky 2024 Ed 230116 1705616418.4945
Jama Jabornisky 2024 Ed 230116 1705616418.4945
Uploaded by
Prima Hari NastitiCopyright:
Available Formats
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/377573083
Transitioning From SIRS to Phoenix With the Updated Pediatric Sepsis
Criteria:The Difficult Task of Simplifying the Complex
Article in Journal of the American Medical Association · January 2024
DOI: 10.1001/jama.2023.27988
CITATIONS READS
0 589
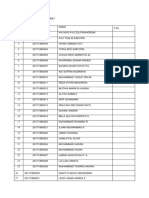
3 authors:
Roberto Jabornisky Nathan Kuppermann
National University of the Northeast University of California, Davis
35 PUBLICATIONS 392 CITATIONS 437 PUBLICATIONS 16,919 CITATIONS
SEE PROFILE SEE PROFILE
Sebastián González-Dambrauskas
Universidad de la República de Uruguay
140 PUBLICATIONS 738 CITATIONS
SEE PROFILE
All content following this page was uploaded by Sebastián González-Dambrauskas on 21 January 2024.
The user has requested enhancement of the downloaded file.
Opinion
EDITORIAL
Transitioning From SIRS to Phoenix With the Updated
Pediatric Sepsis Criteria
The Difficult Task of Simplifying the Complex
Roberto Jabornisky, MD, PhD; Nathan Kuppermann, MD, MPH; Sebastián González-Dambrauskas, MD
Everyone must acknowledge the difficulty of distinguishing Unlike the creation of previous criteria, these investiga-
diseases…whoever denies this may as well deny that there is such tors developed a 3-pronged data-driven approach, which
a thing as medical art. included a global survey,7 a meta-analysis,8 and the devel-
William Cullen1 opment of a new organ dysfunction scoring system. Consis-
tent with adult Sepsis-3,5 the task force considered that the
Diagnosis as a Social Construct in Medicine existing sepsis definitions did not meet clinicians’ needs
The art of making a diagnosis is essential to high-quality and suggested that definitions focusing on organ dysfunc-
medical practice and is arguably the most valuable skill of a tion would be more pertinent.3 The subsequent research
health care practitioner. Diagnosis serves as the articulation phase led to the creation of the Phoenix Sepsis Score.9 This
of the language of medical score was developed using robust multivariable regression
science, guiding medical techniques to derive and validate a composite model using
Editorial practice at every clinical en- organ dysfunction measures from electronic health data in
counter and through health 10 health systems across 5 countries, including high- and
Related articles
policy.1 Developing medical low-resource settings.9 This involved complex data harmo-
knowledge entails a social nization across many different large electronic databases
construct rooted in the prevailing medical framework, ethi- encompassing more than 3.6 million pediatric encounters.
cal perspectives, and the socialization of these ideas among The primary objective was to identify and validate factors
physicians. For medical knowledge to evolve, there must be associated with in-hospital mortality in children with sep-
an interaction between a condition’s definition and its scien- sis, with the positive predictive value and sensitivity serv-
tific identification. This framework is shaped by how these ing as the primary performance measures. The task force
elements interact and how the definition of a condition is then established novel pediatric sepsis definitions following
configured.2 a modified Delphi process.
Medical science has been driven to establish boundaries
defining the start of illnesses, although this frequently sim- The Phoenix Pediatric Sepsis Criteria
plifies complex biological phenomena. The trade-off The updated pediatric sepsis definition is now operational-
between sensitivity and specificity unfolds in the face of this ized by 2 or more points in the Phoenix Sepsis Score (indicat-
complexity and is particularly acute for syndromes such as ing life-threatening organ dysfunction of the respiratory,
sepsis. In the face of these challenges, we discuss the new cardiovascular, coagulation, and/or neurologic systems) in a
diagnostic paradigm for pediatric sepsis published in this child with suspected or confirmed infection.3 Septic shock is
issue of JAMA.3 operationalized by the presence of sepsis in addition to 1 or
more points in the cardiovascular component of the Phoenix
The Transition From SIRS to the Phoenix Criteria Sepsis Score (ie, severe hypotension, blood lactate >5 mmol/L,
Pediatricians commonly rely on sepsis definitions estab- or vasoactive medication infusion). 3 These criteria per-
lished in 2005. 4 These definitions were based on expert formed better than previous criteria across differently re-
opinions from physicians in high-resource settings and sourced settings. A substantial change in the newly proposed
depend on the identification of an infection-induced sys- criteria is the removal of SIRS as a diagnostic factor. This adds
temic inflammatory response syndrome (SIRS).4 Introduction clarity and minimizes confusion, particularly in the emer-
of adult Sepsis-3 definitions in 2016 marked a shift in the gency department setting, where many febrile children who
conceptual framework from infection-associated SIRS to do not have sepsis meet SIRS criteria (eg, febrile infants with
infection-associated organ dysfunction. 5 In response to bronchiolitis who have tachycardia and tachypnea). Addition-
emerging data indicating that SIRS criteria in children lacked ally, the distinction of severe sepsis as a separate condition has
specificity for identifying those at higher risk of mortality,6 been eliminated, as the term is redundant with sepsis. Con-
the pediatric sepsis research community took action. In 2019, sidering the worldwide implications of this change, it is im-
a task force of 35 pediatric sepsis experts from 12 countries portant to acknowledge the challenges that will be encoun-
on 6 continents to develop updated operational definitions tered in adoption by the global pediatric community, especially
was convened.3 in low-resource settings.
jama.com (Reprinted) JAMA Published online January 21, 2024 E1
© 2024 American Medical Association. All rights reserved.
Downloaded from jamanetwork.com by Roberto Jabornisky on 01/21/2024
Opinion Editorial
The task force deserves commendation for incorporating shock are intended to operationalize the concept of life-
the input of professionals from low-resource settings and for threatening organ dysfunction due to an infection in chil-
validating the Phoenix Sepsis Score by creating an extensive dren, not for screening or early identification of patients with
database that included hospitals in these settings, where the suspected sepsis.”3 Awareness of this more limited focus is criti-
greatest burden of sepsis occurs. 10 The disproportionate cal for those who practice outside of the PICU setting.
impact was confirmed in the validation cohort, in which chil- Finally, the investigators did not eliminate the most sub-
dren with sepsis had a 7.1% mortality rate in high-resource jective part of the diagnostic pathway in sepsis which is the
settings and a 28.5% rate in low-resource settings.9 Those “suspected infection” criteria. Clinicians seeking to imple-
with septic shock in the first 24 hours had a 10.8% mortality ment these criteria must take this important aspect into con-
rate at the former sites and a 33.5% mortality rate at the latter sideration when managing children with suspected sepsis.
sites.9 The new criteria demonstrated a higher positive pre-
dictive value and comparable or higher sensitivity to the Global Challenges of the Phoenix Sepsis Criteria
previous criteria for sepsis, severe sepsis, and septic shock. for Research and Clinical Practice
However, only 3.1% of the cohort used to validate the score A clinically satisfactory definition of sepsis has been elusive
came from low-resource settings, limiting its precision. 9 since the term was first coined by the ancient Greeks. 11
Notably, the Phoenix Sepsis Score demonstrated lower sensi- Reconceptualizing sepsis based on the enhanced compre-
tivity compared with previous criteria (23% vs 77%) at 1 hension of its nature and complexity and identifying it as
lower-resource site,9 further underscoring the need for addi- the pivotal juncture when an infection escalates into a life-
tional study before implementing the Phoenix Sepsis Score threatening condition was a bold, complex, and imperative
broadly in lower-resource settings. undertaking for which the authors should be praised. Iden-
Furthermore, the global survey that served as the start- tifying the moment when the immune system begins to
ing point7 for developing this score reflected the perceptions deregulate is a critical issue, along with whether clinicians
of physicians primarily working in hospital settings, particu- should wait for a patient to present with organ dysfunction
larly in pediatric intensive care units (PICUs) (57%), with only to diagnose sepsis. Given the higher mortality in lower-
15% based in emergency departments. Moreover, all the low- resource settings, are other clinical criteria needed in these
resource validation sites were institutions with electronic settings for earlier detection?
health records and most had PICUs, which does not ad- This important work introduces novel challenges for imple-
equately reflect conditions in most low-resource settings. These mentation, requiring substantial further investigation to as-
factors introduce a distinct bias favoring a “PICU-based certain whether these revised definitions result in improved
consensus,” potentially limiting the generalizability and patient care. These criteria must be further validated in a pro-
adoption of the new criteria by health care practitioners in spective manner, in differently resourced and varied set-
non-PICU and nonhospital settings responsible for recogniz- tings, particularly those with the highest disease burden.
ing and managing children with sepsis. The authors also ac- Until then, it is essential to refrain from considering these
knowledge an additional barrier, the requirement for serum criteria as an inflexible directive governing medical interven-
lactate measurement and coagulation parameters in the score. tions for pediatric sepsis. No definition can fully substitute for
These laboratory tests are not readily available in many low- the clinical judgment of an experienced, vigilant clinician car-
resource settings,7 although it is noteworthy that the Phoenix ing for an unwell child. We commend the Pediatric Sepsis
score performed well even in centers where lactate informa- Definition Task Force for their outstanding work, marking a
tion was not available. substantial advance in the approach to pediatric sepsis. Nev-
It is important to recognize that the Phoenix Sepsis Score ertheless, recognizing that sepsis is a complex process, the jour-
was not designed as a screening tool for sepsis and should not ney ahead remains expansive. Dismissing the notion of
be misconstrued as an early warning tool or a sepsis test. The “simple” sepsis, we anticipate ongoing dialogues among cli-
purpose of the Phoenix Sepsis Score is to assist clinicians in nicians and researchers worldwide to further refine this up-
identifying children with both infection and life-threatening dated conceptual framework. The departure from the widely
organ dysfunction. The score was not designed to predict which adopted SIRS paradigm over the past 2 decades poses an im-
children are at risk of developing sepsis. As the authors have portant change yet a formidable challenge, as cultural shifts
stated, “The new pediatric sepsis criteria for sepsis and septic in medicine are inherently arduous.
ARTICLE INFORMATION Unidad de Cuidados Intensivos de Niños del Centro REFERENCES
Author Affiliations: Department of Women, Hospitalario Pereira Rossell, Facultad de Medicina, 1. Rosenberg CE. The tyranny of diagnosis.
Children, and Adolescents, Faculty of Medicine, Universidad de la República, Montevideo, Uruguay Milbank Q. 2002;80(2):237-260. doi:10.1111/1468-
National University of the Northeast, Corrientes, (González-Dambrauskas). 0009.t01-1-00003
Argentina (Jabornisky); Red Colaborativa Pediátrica Corresponding Author: Roberto Jabornisky, MD, 2. Brown P. Naming and framing. J Health Soc Behav.
de Latinoamérica (LARed Network), Montevideo, PhD, Universidad Nacional del Nordeste Facultad 1995;(special issue):34-52. doi:10.2307/2626956
Uruguay (Jabornisky, González-Dambrauskas); de Medicina, 1240 Moreno, Corrientes 3400,
Departments of Emergency Medicine and Argentina (rjabornisky@gmail.com). 3. Schlapbach LJ, Watson RS, Sorce LR, et al;
Pediatrics, UC Davis School of Medicine and UC Society of Critical Care Medicine Pediatric Sepsis
Published Online: January 21, 2024. Definition Task Force. International consensus
Davis Health, Sacramento, California doi:10.1001/jama.2023.27988
(Kuppermann); Departamento de Pediatría y criteria for pediatric sepsis and septic shock. JAMA.
Conflict of Interest Disclosures: None reported.
E2 JAMA Published online January 21, 2024 (Reprinted) jama.com
© 2024 American Medical Association. All rights reserved.
Downloaded from jamanetwork.com by Roberto Jabornisky on 01/21/2024
Editorial Opinion
Published online January 21, 2024. doi:10.1001/jama. PELOD-2, and qSOFA for in-hospital mortality 9. Sanchez-Pinto LN, Bennett TD, DeWitt PE, et al;
2024.0179 among children with suspected infection admitted Society of Critical Care Medicine Pediatric Sepsis
4. Goldstein B, Giroir B, Randolph A. International to the intensive care unit. Intensive Care Med. 2018; Definition Task Force. Development and validation
pediatric sepsis consensus conference. Pediatr Crit 44(2):179-188. doi:10.1007/s00134-017-5021-8 of the Phoenix criteria for pediatric sepsis and
Care Med. 2005;6(1):2-8. doi:10.1097/01.PCC. 7. Morin L, Hall M, de Souza D, et al. The current septic shock. JAMA. Published online January 21,
0000149131.72248.E6 and future state of pediatric sepsis definitions. 2024. doi:10.1001/jama.2024.0196
5. Singer M, Deutschman CS, Seymour CW, et al. Pediatrics. 2022;149(6):e2021052565. doi:10.1542/ 10. Tan B, Wong JJ, Sultana R, et al. Global
The Third International Consensus Definitions for peds.2021-052565 case-fatality rates in pediatric severe sepsis and
Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315 8. Menon K, Schlapbach LJ, Akech S, et al. Criteria septic shock. JAMA Pediatr. 2019;173(4):352-362.
(8):801-810. doi:10.1001/jama.2016.0287 for pediatric sepsis—a systematic review and doi:10.1001/jamapediatrics.2018.4839
6. Schlapbach LJ, Straney L, Bellomo R, et al. meta-analysis by the Pediatric Sepsis Definition 11. Funk DJ, Parrillo JE, Kumar A. Sepsis and septic
Prognostic accuracy of age-adapted SOFA, SIRS, Taskforce. Crit Care Med. 2022;50(1):21-36. doi:10. shock: a history. Crit Care Clin. 2009;25(1):83-101.
1097/CCM.0000000000005294 doi:10.1016/j.ccc.2008.12.003
jama.com (Reprinted) JAMA Published online January 21, 2024 E3
© 2024 American Medical Association. All rights reserved.
Downloaded from jamanetwork.com by Roberto Jabornisky on 01/21/2024
View publication stats
You might also like
- Magic MouthwashDocument5 pagesMagic MouthwashAdiAri Rosiu100% (3)
- The Art and Science of CIRS MedicineFrom EverandThe Art and Science of CIRS MedicineRating: 5 out of 5 stars5/5 (5)
- DSSC Intake QuestionnaireDocument7 pagesDSSC Intake QuestionnairePrima Hari NastitiNo ratings yet
- (Jason Corburn) Street Science Community KnowledgeDocument46 pages(Jason Corburn) Street Science Community KnowledgeLuciana NegrettoNo ratings yet
- 2024 Context and Implications of The New Pediatric Sepsis CriteriaDocument4 pages2024 Context and Implications of The New Pediatric Sepsis CriteriaRaquel Alves da SilvaNo ratings yet
- Defining Pediatric SepsisDocument2 pagesDefining Pediatric SepsisArisa DeguchiNo ratings yet
- 2024 International Consensus Criteria of Pediatric Sepsis and SepticDocument10 pages2024 International Consensus Criteria of Pediatric Sepsis and SepticRaquel Alves da SilvaNo ratings yet
- Jama Schlapbach 2024 Oi 240002 1705616415.31602Document10 pagesJama Schlapbach 2024 Oi 240002 1705616415.31602Laura Alejandra Torres CanchalaNo ratings yet
- Sepsis CurrentDocument8 pagesSepsis CurrentfelipeNo ratings yet
- Consenso SepsisDocument20 pagesConsenso SepsisNayeli Sanchez RamosNo ratings yet
- Critrios Phoenix para Sepsis NiñosDocument12 pagesCritrios Phoenix para Sepsis NiñosJorge MéndezNo ratings yet
- 1 s2.0 S0196655320310385 MainDocument6 pages1 s2.0 S0196655320310385 MainSalome MwangiNo ratings yet
- Defining Pediatric Sepsis by Different Criteria: Discrepancies in Populations and Implications For Clinical PracticeDocument8 pagesDefining Pediatric Sepsis by Different Criteria: Discrepancies in Populations and Implications For Clinical PracticeMuhamad RockystankiNo ratings yet
- Pope - Moseley@cpr - Ku.dk: To The EditorDocument2 pagesPope - Moseley@cpr - Ku.dk: To The EditorLili MorgadoNo ratings yet
- Machine Learning For Early Detection of Sepsis - An Internal and Temporal Validation StudyDocument9 pagesMachine Learning For Early Detection of Sepsis - An Internal and Temporal Validation StudyMariana NannettiNo ratings yet
- Advances in Pediatric Sepsis and Shock: E. Scott HalsteadDocument2 pagesAdvances in Pediatric Sepsis and Shock: E. Scott HalsteadnadiaNo ratings yet
- 2005 International Ped Sepsis Consensus ConfDocument7 pages2005 International Ped Sepsis Consensus ConfMartin LafuenteNo ratings yet
- Sepsis 3Document82 pagesSepsis 3Solange Vargas LiclaNo ratings yet
- Paediatric Early Warning SysteDocument14 pagesPaediatric Early Warning SysteTengku rasyidNo ratings yet
- Guia Practica Sepsis AAP 2023Document3 pagesGuia Practica Sepsis AAP 2023NoraNo ratings yet
- Pediatric Sepsis Definition-A Systematic Review Protocol by The Pediatric Sepsis Definition TaskforceDocument7 pagesPediatric Sepsis Definition-A Systematic Review Protocol by The Pediatric Sepsis Definition TaskforceGunduz AgaNo ratings yet
- Designación de Alto Riesgo de Parálisis Cerebral Una Declaración de Consenso ClínicoDocument10 pagesDesignación de Alto Riesgo de Parálisis Cerebral Una Declaración de Consenso ClíniconulintavaNo ratings yet
- Phoenix Sepsis ScoreDocument3 pagesPhoenix Sepsis ScoreNur Amaliah idrusNo ratings yet
- Marcotte Et Al Frontiers2021Document16 pagesMarcotte Et Al Frontiers2021Taissa NunesNo ratings yet
- Eclinicalmedicine: Research PaperDocument8 pagesEclinicalmedicine: Research PaperChacanNo ratings yet
- 2023 - Development and Validation of A New Tool The Sarcopenia Knowledge QuestionnaireDocument6 pages2023 - Development and Validation of A New Tool The Sarcopenia Knowledge QuestionnaireAlex LimaNo ratings yet
- HHS Public Access: Initial Resuscitation and Management of Pediatric Septic ShockDocument26 pagesHHS Public Access: Initial Resuscitation and Management of Pediatric Septic ShockRizky Nur EvindaNo ratings yet
- EditorialDocument2 pagesEditorialmanfel_26No ratings yet
- Sankar 2019Document8 pagesSankar 2019Janny Torres AvilaNo ratings yet
- NEC SimposioDocument8 pagesNEC Simposionacho InfanteNo ratings yet
- Procalcitonin, C-Reactive Protein, Albumin, and Blood Cultures As Early Markers of Sepsis Diagnosis or Predictors of Outcome: A Prospective AnalysisDocument7 pagesProcalcitonin, C-Reactive Protein, Albumin, and Blood Cultures As Early Markers of Sepsis Diagnosis or Predictors of Outcome: A Prospective Analysistaufik.abdiNo ratings yet
- Diabetes Metabolism Res - 2023 - Naemi - Predicting Diabetic Foot Ulceration Using Routinely Collected Data in A FootDocument9 pagesDiabetes Metabolism Res - 2023 - Naemi - Predicting Diabetic Foot Ulceration Using Routinely Collected Data in A FootelhierofanteNo ratings yet
- 2022 02 28 22271643v1 FullDocument49 pages2022 02 28 22271643v1 FullA GouveiaNo ratings yet
- Paediatric and Neonatal Sepsis and Inflammation PDFDocument3 pagesPaediatric and Neonatal Sepsis and Inflammation PDFSultan Rahmat SeptianNo ratings yet
- Bliss 2015Document5 pagesBliss 2015Dii ScottouNo ratings yet
- Nejmp 1215594Document4 pagesNejmp 1215594Cj AlmazanNo ratings yet
- Transdisciplinary Approaches Enhance The Production of Translational KnowledgeDocument12 pagesTransdisciplinary Approaches Enhance The Production of Translational KnowledgereneNo ratings yet
- La Respuesta Del Huesped A La SepsisDocument18 pagesLa Respuesta Del Huesped A La SepsisAngelicia Varela MuñozNo ratings yet
- Fped 10 890767Document18 pagesFped 10 890767Feby JuwitaNo ratings yet
- Peritonitis Guidelines PDI 2012Document56 pagesPeritonitis Guidelines PDI 2012Muhammad Yusuf Arief AkbarNo ratings yet
- Managing The Risks and BenefitDocument8 pagesManaging The Risks and BenefitcacaNo ratings yet
- Sepsis 33Document10 pagesSepsis 33alpha7memesNo ratings yet
- 2023 SPCCMP Sepsis ConsensusDocument82 pages2023 SPCCMP Sepsis ConsensusFar CanakanNo ratings yet
- Surviving Sepsis Campaign Guidelines 2021 Highlights For The Practicing ClinicianDocument8 pagesSurviving Sepsis Campaign Guidelines 2021 Highlights For The Practicing ClinicianMariah BrownNo ratings yet
- MC Intosh 2017Document9 pagesMC Intosh 2017Nadia SetianingsihNo ratings yet
- Critical Pathways For The Management of PreeclampsiaDocument16 pagesCritical Pathways For The Management of PreeclampsiabouattourNo ratings yet
- 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions ConferenceDocument7 pages2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions ConferenceFanny Ari SandyNo ratings yet
- Nikma Alfi RosidaDocument14 pagesNikma Alfi RosidaSejuta AdaNo ratings yet
- Hospitalizations For Ambulatory Care-Sensitive Conditions Among Children With Chronic and Complex DiseasesDocument7 pagesHospitalizations For Ambulatory Care-Sensitive Conditions Among Children With Chronic and Complex DiseasesHasriana BudimanNo ratings yet
- ADE and Dengue Vaccination: Vaccine June 2017Document4 pagesADE and Dengue Vaccination: Vaccine June 2017anon_301318896No ratings yet
- PediatricDocument2 pagesPediatricIndah IndrianiNo ratings yet
- Septic Shock Carcillo PDFDocument14 pagesSeptic Shock Carcillo PDFjesus_berber_2No ratings yet
- HydrocephalusDocument9 pagesHydrocephalusDeby AnditaNo ratings yet
- SR and Guidelines For Periop MGMT of Peds Patients Undergoing Major Plastic SurgeryDocument10 pagesSR and Guidelines For Periop MGMT of Peds Patients Undergoing Major Plastic SurgeryPaul MarjiNo ratings yet
- Learning The Art and Science of Diagnosis - JAMADocument2 pagesLearning The Art and Science of Diagnosis - JAMAJose Antonio Tous OlagortaNo ratings yet
- Blood Culture With CAPDocument10 pagesBlood Culture With CAPKaye Antonette AntioquiaNo ratings yet
- The Third International Consensus Definitions For Sepsis and Septic Shock (Sepsis-3)Document10 pagesThe Third International Consensus Definitions For Sepsis and Septic Shock (Sepsis-3)Majito ParraNo ratings yet
- Onken2021. Critical Values in CytologyDocument8 pagesOnken2021. Critical Values in CytologyMD LarasatiNo ratings yet
- Piis0025619614006636 PDFDocument7 pagesPiis0025619614006636 PDFDeary DearyNo ratings yet
- Sepsis 2Document14 pagesSepsis 2ROCIO Vasquez OVALLENo ratings yet
- Newsepsisandseptic Shockdefinitions: Clinical Implications and ControversiesDocument17 pagesNewsepsisandseptic Shockdefinitions: Clinical Implications and ControversiesJulio CesarNo ratings yet
- Review Sepsi LancetDocument13 pagesReview Sepsi LancetMr. LNo ratings yet
- ThompsonMacias 2015 RecognitionandMana PDFDocument9 pagesThompsonMacias 2015 RecognitionandMana PDFelsaNo ratings yet
- Neo Int 9 November 2021Document35 pagesNeo Int 9 November 2021Prima Hari NastitiNo ratings yet
- Neo Int 18 July 2021Document39 pagesNeo Int 18 July 2021Prima Hari NastitiNo ratings yet
- Case Congenital AV BlockDocument27 pagesCase Congenital AV BlockPrima Hari NastitiNo ratings yet
- Revisi Sp2 Tumbuh Kembang (Pertama) FinalDocument9 pagesRevisi Sp2 Tumbuh Kembang (Pertama) FinalPrima Hari NastitiNo ratings yet
- Manuscript 24092017 UcldDocument46 pagesManuscript 24092017 UcldPrima Hari NastitiNo ratings yet
- Daftar Hadir Angkatan 2017Document2 pagesDaftar Hadir Angkatan 2017Prima Hari NastitiNo ratings yet
- Ecff PDFDocument8 pagesEcff PDFPrima Hari NastitiNo ratings yet
- Internet-Addiction Understanding - Counseling - CopingDocument34 pagesInternet-Addiction Understanding - Counseling - CopingPrima Hari NastitiNo ratings yet
- Buat KakkaDocument9 pagesBuat KakkaPrima Hari NastitiNo ratings yet
- Micropara LabDocument8 pagesMicropara LabFatima KateNo ratings yet
- Acta 88 134Document9 pagesActa 88 134Andre ErlisNo ratings yet
- (Literasi Bahasa Inggris) Soal Try Out SKOLLA SNBT Episode 2Document8 pages(Literasi Bahasa Inggris) Soal Try Out SKOLLA SNBT Episode 2Fauzan Al GhazaliNo ratings yet
- Hubungan Usia Dan Jenis Kelamin Dengan Jenis Kelainan Refraksi Pada Anak Di Pusat Mata Nasional Rumah Sakit Mata Cicendo - Dianita Veulina GintingDocument7 pagesHubungan Usia Dan Jenis Kelamin Dengan Jenis Kelainan Refraksi Pada Anak Di Pusat Mata Nasional Rumah Sakit Mata Cicendo - Dianita Veulina Gintingmirza kumalaNo ratings yet
- Lung Cancer Detection Using Machine LearningDocument24 pagesLung Cancer Detection Using Machine Learningsj647387No ratings yet
- Hereditary Hemochromatosis and Iron MetabolismDocument8 pagesHereditary Hemochromatosis and Iron MetabolismVienne Yuen Wing YanNo ratings yet
- Nelson MCQ Fluid TherapyDocument10 pagesNelson MCQ Fluid TherapyBelinderjit Kaur100% (2)
- Pe 1 Final ModuleDocument10 pagesPe 1 Final Modulealexa dawatNo ratings yet
- Social and Preventive Pharmacy Solution For 2 Marks Most Important QuestionsDocument14 pagesSocial and Preventive Pharmacy Solution For 2 Marks Most Important QuestionsInnovation That ExcitesNo ratings yet
- MOH Needs For COVID 19Document32 pagesMOH Needs For COVID 19instrumed_globalNo ratings yet
- Potdar 2020Document8 pagesPotdar 2020Christian Leonardo Molina HinojosaNo ratings yet
- Community-Acquired Pneumonia in Children: Clinical Features and Diagnosis - UpToDateDocument62 pagesCommunity-Acquired Pneumonia in Children: Clinical Features and Diagnosis - UpToDateYeidhy Karin Cayo CoñezNo ratings yet
- Textbook Ebook Diagnostic Ultrasound For Sonographers Aya Kamaya All Chapter PDFDocument43 pagesTextbook Ebook Diagnostic Ultrasound For Sonographers Aya Kamaya All Chapter PDFolivia.anderson705100% (9)
- Effectiveness of Foot Reflexology On Pain Among Hemodialysis PatientsDocument5 pagesEffectiveness of Foot Reflexology On Pain Among Hemodialysis PatientsIJAR JOURNALNo ratings yet
- Nail Anatomy: David de Berker, MDDocument7 pagesNail Anatomy: David de Berker, MDVita BūdvytėNo ratings yet
- Frequently Missed Fractures in Pediatric TraumaDocument13 pagesFrequently Missed Fractures in Pediatric Traumaalejasuarez248No ratings yet
- Final: Client Code: Client'S Name and AddressDocument9 pagesFinal: Client Code: Client'S Name and AddressBagadi AvinashNo ratings yet
- The Seqirus Portfolio of Influenza Vaccines-2021-2022 SeasonDocument2 pagesThe Seqirus Portfolio of Influenza Vaccines-2021-2022 SeasonKari BallardNo ratings yet
- Integrating Health and Mental Health Services - A Past and Future HistoryDocument6 pagesIntegrating Health and Mental Health Services - A Past and Future HistoryPedro ReyesNo ratings yet
- Second Grading Exam in MAPEH-10Document4 pagesSecond Grading Exam in MAPEH-10Reymundo PenialaNo ratings yet
- Sensory and Its DisordersDocument8 pagesSensory and Its Disordersjalan_zNo ratings yet
- BEKAMDocument26 pagesBEKAMeko rustamajiNo ratings yet
- Efsa 1Document125 pagesEfsa 1palomaluna00No ratings yet
- Pediatric Advanced Life Support (PALS) - UpToDateDocument57 pagesPediatric Advanced Life Support (PALS) - UpToDateSofíaNo ratings yet
- L1 - SyncopeDocument5 pagesL1 - SyncopeMuthukumaranNo ratings yet
- DrugsDocument7 pagesDrugsCaine ReganNo ratings yet
- (MICRO2) Gram Negative CocciDocument41 pages(MICRO2) Gram Negative CocciMadhu MithaNo ratings yet
- Eng - Raed DubaiMunicipality Working at HeightsDocument41 pagesEng - Raed DubaiMunicipality Working at HeightsBhuvaneshwaran BNNo ratings yet