Professional Documents
Culture Documents
Electro Cardiograph y
Electro Cardiograph y
Uploaded by
kajonasfoodproducts0 ratings0% found this document useful (0 votes)
6 views94 pagesThe document provides information on how to use an electrocardiogram (ECG/EKG) including how to prepare the patient, place the electrodes, and connect the device. It discusses nursing responsibilities before, during, and after the procedure. Key aspects of interpreting the ECG are summarized such as normal electrical conduction, identifying waves and intervals, and determining heart rate. Common cardiac rhythms like normal sinus rhythm, bradycardia, tachycardia, and premature atrial complexes are outlined.
Original Description:
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThe document provides information on how to use an electrocardiogram (ECG/EKG) including how to prepare the patient, place the electrodes, and connect the device. It discusses nursing responsibilities before, during, and after the procedure. Key aspects of interpreting the ECG are summarized such as normal electrical conduction, identifying waves and intervals, and determining heart rate. Common cardiac rhythms like normal sinus rhythm, bradycardia, tachycardia, and premature atrial complexes are outlined.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
6 views94 pagesElectro Cardiograph y
Electro Cardiograph y
Uploaded by
kajonasfoodproductsThe document provides information on how to use an electrocardiogram (ECG/EKG) including how to prepare the patient, place the electrodes, and connect the device. It discusses nursing responsibilities before, during, and after the procedure. Key aspects of interpreting the ECG are summarized such as normal electrical conduction, identifying waves and intervals, and determining heart rate. Common cardiac rhythms like normal sinus rhythm, bradycardia, tachycardia, and premature atrial complexes are outlined.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 94
HOW TO USE THE ECG
• Detects the heart's electrical activity during myocardial
contraction and relaxation, usually recorded by electrodes on
the skin.
• ECG/EKG signals are recorded to examine heart rate, heart
rate variability, analysis of the waveform morphology,
arrhythmia, and other similar functions.
NURSING RESPONSIBILITIES
BEFORE THE PROCEDURE
• Remove any metallic objects such as jewelry
• Clip chest hair
• Avoid drinking cold water right before test
• No exercising, or increasing your heart rate, before the test
• Keep the room at a moderate temperature to avoid shivering
NURSING RESPONSIBILITIES
DURING THE PROCEDURE
• During the test, ask patient to lie still on the table and
breathe normally.
• Instruct patient to not talk during the test.
HOW TO USE THE ECG
1. Prepare the skin.
Prepare the subject's skin by wiping the chest area thoroughly
with skin cleansing (alcohol) swabs. This removes any oil that
may be on the patient's skin and which can cause drift in your
ECG/EKG signals.
HOW TO USE THE ECG
2. Find and mark the correct lead placements for the 12 lead ECG
HOW TO USE THE ECG
3. Identify V1 and V2.
• Identify the top of your subject's sternum. Approximately 4
centimeters below this, there is a ridge. This identifies the
second intercostal space. Feeling down, you will come across
the third and fourth intercostal spaces. Use a skin-safe
marker to mark the fourth intercostal space as V2.
• Mark V1 in the mirror position on the opposite side of the
chest.
HOW TO USE THE ECG
4. Find and mark V3 - V6.
• V4 can be found one intercostal space lower than V2, in line
with the middle of the clavicle.
• Next, track along the torso to the subject's left to find V6 at
mid auxiliary on the same horizontal level as V4. Mark V6.
• V5 can be marked at midway between V4 and V6.
• Mark V3 midway between V2 and V4.
HOW TO USE THE ECG
5. Apply electrodes to the chest at V1 - V6
• Apply your electrodes to your 6 marks.
6. Connect wires from V1 to V6 to the recording device
HOW TO USE THE ECG
7. Apply limb leads.
HOW TO USE THE ECG
8. Connect cable wires to one of the following:
• An ECG machine placed at the patient’s side for an immediate
recording (standard 12-lead ECG)
• A cardiac monitor at the patient’s bedside for continuous reading; this
kind of monitoring, usually called hardwire monitoring, is used in
intensive care units
• A small box that the patient carries that continuously transmits the
ECG information by radiowaves to a central monitor located
elsewhere (called telemetry)
• A small, lightweight tape recorder–like machine (called ambulatory
ECG monitoring or a Holter mon_x0002_itor) that the patient wears
and that continuously records the ECG on a tape, which is later
viewed and analyzed with a scanner
HOW TO USE THE ECG
HOW TO USE THE ECG
HOW TO USE THE ECG
HOW TO USE THE ECG
HOW TO USE THE ECG
• https://www.adinstruments.com/blog/correctly-place-electrodes-12-
lead-ecg
HOW TO USE THE ECG
NORMAL ELECTRICAL CONDUCTION
• Electrical impulse originates from SA node (near the superior vena
cava in the right atrium)
• Electrical impulse from SA node to AV node (CONDUCTION) →
causes the atria to contract → ventricles filled with blood
• Electrical impulse travels through Bundle of His and the Purkinje
fibers (located in ventricular muscle)
• Electrical stimulation causes mechanical contraction of
ventricles (systole)
• Cells repolarize and the ventricles relax (diastole)
NORMAL ELECTRICAL CONDUCTION
• DEPOLARIZATION
• electrical stimulation
• REPOLARIZATION
• electrical relaxation
• SYSTOLE
• mechanical contraction
• DIASTOLE
• mechanical relaxation
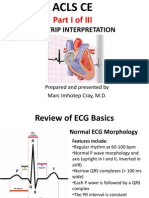
INTERPRETING THE ELECTROCARDIOGRAM
WAVES, COMPLEXES, AND INTERVALS
• P wave
• represents atrial depolarization
• N: 2.5 mm or less in height
• N: 0.11 seconds or less in duration
• QRS complex
• ventricular depolarization
• N: less than 0.12 seconds in duration
• where atrial repolarization also occurs
INTERPRETING THE ELECTROCARDIOGRAM
WAVES, COMPLEXES, AND INTERVALS
• QRS complex
• Q wave
• first negative deflection after the P wave
• N: less than 0.04 seconds in duration
• R wave
• first positive deflection after the P wave
• S wave
• first negative deflection after the R wave
INTERPRETING THE ELECTROCARDIOGRAM
WAVES, COMPLEXES, AND INTERVALS
• T wave
• represents ventricular repolarization
• usually the same direction as QRS complex
• U wave
• represents repolarization of Purkinje fibers
• usually smaller than P wave
• sometimes seen in patients with hypokalemia, HPN, or
heart disease
INTERPRETING THE ELECTROCARDIOGRAM
WAVES, COMPLEXES, AND INTERVALS
• PR interval
• measured from beginning of P wave to beginning of QRS complex
• N: 0.12 to 0.20 seconds in duration
• ST segment
• measured from end of QRS complex to the beginning of T wave
• QT interval
• represents total time for ventricular depolarization and repolarization
• measured from beginning of QRS complex to end of T wave
• N: 0.32 to 0.40 seconds in duration
INTERPRETING THE ELECTROCARDIOGRAM
WAVES, COMPLEXES, AND INTERVALS
• TP interval
• measured from end of T wave to the beginning of next P
wave
• no electrical activity, graph remains flat -> isoelectric line
• PP interval
• atrial rhythm and atrial rate
• RR interval
• ventricular rhythm and ventricular rate
INTERPRETING THE ELECTROCARDIOGRAM
DETERMINING HEART RATE FROM ECG
• 1 minute-strip = 60 seconds
• 300 large boxes (0.2 seconds each)
• 1500 small boxes (0.04 seconds each)
• Count the number of small boxes within an RR interval and
divide that 1500 by that number
• E.g. There are 25 small boxes within the RR interval,
HR= 1500/25 = 60 BPM
INTERPRETING THE ELECTROCARDIOGRAM
DETERMINING HEART RATE FROM ECG
• Count number of RR intervals in 6 seconds then
multiply that number by 10
• 3 second-intevals = 15 large boxes
NORMAL SINUS RHYTHM
• Ventricular and atrial rate: 60 - 100 bpm
• Ventricular and atrial rhythm: Regular
• QRS shape and duration: Usually normal, but may be
regularly abnormal
• P wave: Normal and consistent shape
• PR interval: Interval between 0.12 - 0.20 seconds
• P:QRS ratio: 1:1
NORMAL SINUS RHYTHM
NORMAL SINUS RHYTHM
SINUS NODE DYSRHYTHMIAS
SINUS BRADYCARDIA
• Ventricular and atrial rate: Less than 60
• Ventricular and atrial rhythm: Regular
• QRS shape and duration: Usually normal, but may be
regularly abnormal
• P wave: Normal and consistent shape
• PR interval: Interval between 0.12 - 0.20 seconds
• P:QRS ratio: 1:1
SINUS NODE DYSRHYTHMIAS
SINUS BRADYCARDIA
• Causes:
• Vagal stimulation (vomiting, suctioning, severe pain)
• Medications (calcium channel blockers, beta blockers)
• ICP (hyper-brady-brady)
• Myocardial infarction
• Management:
• Atropine to block vagal stimulation
SINUS NODE DYSRHYTHMIAS
SINUS BRADYCARDIA
SINUS NODE DYSRHYTHMIAS
SINUS BRADYCARDIA
SINUS NODE DYSRHYTHMIAS
SINUS TACHYCARDIA
• Ventricular and atrial rate: greater than 100 bpm but
usually less than 120 bpm
• Ventricular and atrial rhythm: Regular
• QRS shape and duration: Usually normal, but may be
regularly abnormal
• P wave: Normal and consistent shape, may be buried in
preceding T wave
• PR interval: Interval between 0.12 - 0.20 seconds
• P:QRS ratio: 1:1
SINUS NODE DYSRHYTHMIAS
SINUS TACHYCARDIA
• Causes:
• Physiologic/Psychological stress ( acute blood loss, anemia,
exercise, anxiety)
• Meds that stimulate sympathetic response
(catecholamines)
• Stimulants (caffeine, nicotine)
• Illicit drugs (cocaine, ecstasy)
• Postural orthostatic tachycardia syndrome (POTS)
• Management:
• Beta blockers or calcium channel blockers
SINUS NODE DYSRHYTHMIAS
SINUS TACHYCARDIA
SINUS NODE DYSRHYTHMIAS
SINUS TACHYCARDIA
SINUS NODE DYSRHYTHMIAS
SINUS ARRHYTHMIA
• Ventricular and atrial rate: 60-100bpm
• Ventricular and atrial rhythm: Irregular
• QRS shape and duration: Usually normal, but may be
regularly abnormal
• P wave: Normal and consistent shape
• PR interval: Interval between 0.12 - 0.20 seconds
• P:QRS ratio: 1:1
SINUS NODE DYSRHYTHMIAS
SINUS ARRHYTHMIA
• Causes:
• Increases with inspiration and decreases with expiration
• Heart disease or valvular disease
Management:
• Usually not treated
SINUS NODE DYSRHYTHMIAS
SINUS ARRHYTHMIA
SINUS NODE DYSRHYTHMIAS
SINUS ARRHYTHMIA
ATRIAL DYSRHYTHMIAS
PREMATURE ATRIAL COMPLEX
• “Heart skipped a beat.”
• Ventricular and atrial rate: Depends on the underlying rhythm
• Ventricular and atrial rhythm: Irregular due to early P waves, shorter
PP interval, followed by a longer than usual PP interval
• QRS shape and duration: QRS that follows the early P wave may be
normal or absent (blocked PAC)
• P wave: There may be an early or different P wave seen
• PR interval: Interval between 0.12 - 0.20 seconds
• P:QRS ratio: 1:1
ATRIAL DYSRHYTHMIAS
PREMATURE ATRIAL COMPLEX
• Causes:
• Caffeine, alcohol, nicotine
• Hypokalemia
• Atrial ischemia
• Often seen with sinus tachycardia
Management:
• If unfrequent, no treatment is necessary
ATRIAL DYSRHYTHMIAS
PREMATURE ATRIAL COMPLEX
ATRIAL DYSRHYTHMIAS
PREMATURE ATRIAL COMPLEX
ATRIAL DYSRHYTHMIAS
ATRIAL FLUTTER
• Ventricular and atrial rate: Atrial rate: 250-400 bpm;
Ventricular rate: 75-150 bpm
• Ventricular and atrial rhythm:Atrial and ventricular rhythms
are regular but ventricular rhythm may be irregular
• QRS shape and duration: Usually normal, but may be
abnormal or absent
• P wave: Saw-toothed shape (F waves)
• PR interval: Difficult to determine
• P:QRS ratio: 2:1, 3:1, 4:1
ATRIAL DYSRHYTHMIAS
ATRIAL FLUTTER
• Causes:
• COPD
• Thyrotoxicosis
• S/P Open heart surgery
Management:
• Administration of adenosine
• Electrical cardioversion to convert rhythm to sinus rhythm
ATRIAL DYSRHYTHMIAS
ATRIAL FLUTTER
ATRIAL DYSRHYTHMIAS
ATRIAL FLUTTER
ATRIAL DYSRHYTHMIAS
ATRIAL FIBRILLATION
• Ventricular and atrial rate: Atrial rate: 300-600 bpm;
Ventricular rate: 120-200 bpm
• Ventricular and atrial rhythm: Highly irregular
• QRS shape and duration: Usually normal, but may be
abnormal
• P wave: No discernible P waves; irregular undulating
waves that vary in amplitude and shape are seen
• PR interval: Cannot be measured
• P:QRS ratio: Many:1
ATRIAL DYSRHYTHMIAS
ATRIAL FIBRILLATION
• Causes:
• Structural heart disease in people of advanced age
• Pericarditis, Myocarditis
• CAD
• Heart failure
• Sepsis
• RHD
• Mitral stenosis
ATRIAL DYSRHYTHMIAS
ATRIAL FIBRILLATION
• Management:
• If patient is unstable with ventricular rate > 150 bpm,
prepare for immediate cardioversion
• If stable, calcium channel blockers, digoxin, procainamide
may be administered
• Anticoagulation therapy to prevent emboli
ATRIAL DYSRHYTHMIAS
ATRIAL FIBRILLATION
ATRIAL DYSRHYTHMIAS
ATRIAL FIBRILLATION
JUNCTIONAL DYSRHYTHMIAS
PREMATURE JUNCTIONAL COMPLEX
• Ventricular and atrial rate: Depends on the underlying rhythm
• Ventricular and atrial rhythm: Irregular due to early P waves, shorter
PP interval, followed by a longer than usual PP interval
• QRS shape and duration: QRS that follows the early P wave may be
normal or absent (blocked PAC)
• P wave: May be absent, may follow QRS, or may occur before QRS but
with
• PR interval: Less than 0.12 seconds
• P:QRS ratio: 1:1
JUNCTIONAL DYSRHYTHMIAS
PREMATURE JUNCTIONAL COMPLEX
• Causes:
• Digitalis Toxivity
• Heart failure
• CAD
Management:
• If unfrequent, no treatment is necessary
JUNCTIONAL DYSRHYTHMIAS
PREMATURE JUNCTIONAL COMPLEX
JUNCTIONAL DYSRHYTHMIAS
PREMATURE JUNCTIONAL COMPLEX
JUNCTIONAL DYSRHYTHMIAS
JUNCTIONAL RHYTHM
• The AV node becomes the pacemaker of the heart
• Ventricular and atrial rate: 40-60 bpm
• Ventricular and atrial rhythm: Regular
• QRS shape and duration: Usually normal, but may be
abnormal
• P wave: May be absent, may follow QRS, or may occur
before QRS, may be inverted
• PR interval: Less than 0.12 seconds
• P:QRS ratio: 1:1, 0:1
JUNCTIONAL DYSRHYTHMIAS
JUNCTIONAL RHYTHM
• Causes:
• Increased vagal tone
• Complete heart block
Management:
• Same as for sinus bradycardia
JUNCTIONAL DYSRHYTHMIAS
JUNCTIONAL RHYTHM
VENTRICULAR DYSRHYTHMIAS
PREMATURE VENTRICULAR COMPLEX
• “Heart skipped a beat.”
• Ventricular and atrial rate: Depends on underlying rhythm
• Ventricular and atrial rhythm: Irregular due to early QRS,
creating one RR interval that is shorter than the others
• QRS shape and duration: Duration is 0.12 seconds or longer;
shape is bizarre and abnormal
• P wave: May be absent, or in front of QRS. If P wave follows
the QRS, P wave shape may be different
• PR interval: Less than 0.12 seconds
• P:QRS ratio: 1:1, 0:1
VENTRICULAR DYSRHYTHMIAS
PREMATURE VENTRICULAR COMPLEX
• Causes:
• Increased workload of the heart
• Digitalis toxicity
• Hypoxia
• Electrolyte imbalances
Management:
• Lidocaine or amiodarone
VENTRICULAR DYSRHYTHMIAS
PREMATURE VENTRICULAR COMPLEX
VENTRICULAR DYSRHYTHMIAS
PREMATURE VENTRICULAR COMPLEX
VENTRICULAR DYSRHYTHMIAS
VENTRICULAR TACHYCARDIA
• Three or more PVCs in a row, occurring at >100 bpm
• Ventricular and atrial rate: Ventricular rate is 100-200 bpm
• Ventricular and atrial rhythm: Usually regular
• QRS shape and duration: Duration is 0.12 seconds or longer;
shape is bizarre and abnormal
• P wave: Very difficult to detect so atrial rate and rhythm may
be indeterminable
• PR interval: Very irregular, P waves are seen
• P:QRS ratio: Difficult to determine but if P waves are apparent,
less P waves: more QRS
VENTRICULAR DYSRHYTHMIAS
VENTRICULAR TACHYCARDIA
• VT is an emergency because the patient is usually (although
not always) unresponsive and pulseless.
• Causes:
• Larger MIs
Management:
• If pulseless, initiate CPR.
• If with pulse, administer amiodarone. If ineffective,
initiate synchronized cardioversion.
VENTRICULAR DYSRHYTHMIAS
VENTRICULAR TACHYCARDIA
VENTRICULAR DYSRHYTHMIAS
VENTRICULAR TACHYCARDIA
VENTRICULAR DYSRHYTHMIAS
VENTRICULAR FIBRILLATION
• Most common dysrhythmia in patients with cardiac arrest
• Ventricular rate: Greater than 300 per minute
• Ventricular rhythm: Extremely irregular, without specific pattern
• QRS shape and duration: Irregular, undulating waves without
recognizable QRS complexes
• P wave: Very difficult to detect so atrial rate and rhythm may be
indeterminable
• Characterized by absence of audible heartbeat, palpable pulse, and
respirations.
• Cardiac arrest and death are imminent if not corrected.
VENTRICULAR DYSRHYTHMIAS
VENTRICULAR FIBRILLATION
• Causes:
• MI
• Digoxin, epinephrine toxicity
• Electric shock
Management:
• If pulseless, initiate CPR. Follow protocols for defibrillation,
intubation, and administration of epinephrine or
vasopressin, lidocaine, or amiodarone.
VENTRICULAR DYSRHYTHMIAS
VENTRICULAR FIBRILLATION
VENTRICULAR DYSRHYTHMIAS
VENTRICULAR FIBRILLATION
VENTRICULAR DYSRHYTHMIAS
VENTRICULAR ASYSTOLE
• Commonly called flatline
• QRS shape and duration: Absent
• P wave: May be apparent for a short duration
• Characterized by absence of audible heartbeat, palpable pulse,
and respirations.
• Fatal
VENTRICULAR DYSRHYTHMIAS
VENTRICULAR ASYSTOLE
• Causes:
• MI
• Cocaine Overdose
Management:
• Initiate CPR.
VENTRICULAR DYSRHYTHMIAS
VENTRICULAR ASYSTOLE
CONDUCTION ABNORMALITIES
FIRST-DEGREE ATRIOVENTRICULAR BLOCK
• Ventricular and atrial rate: Depends on underlying rhythm
• Ventricular and atrial rhythm: Depends on underlying rhythm
• QRS shape and duration: Usually normal but may be abnormal
• P wave: In front of the QRS complex; shows sinus rhythm,
regular shape
• PR interval: Greater than 0.20 seconds; PR interval
measurement is constant
• P:QRS ratio: 1:1
CONDUCTION ABNORMALITIES
FIRST-DEGREE ATRIOVENTRICULAR BLOCK
CONDUCTION ABNORMALITIES
FIRST-DEGREE ATRIOVENTRICULAR BLOCK
CONDUCTION ABNORMALITIES
SECOND-DEGREE AV BLOCK, TYPE I (WENCKE-BACH)
• Ventricular and atrial rate: Depends on underlying rhythm
• Ventricular and atrial rhythm: Starting from the RR that is the
longest, the RR interval gradually shortens until there is
another long RR interval.
• QRS shape and duration: Usually normal but may be abnormal
• P wave: In front of the QRS complex; shape depends on
underlying rhythm
• PR interval: PR becomes longer with each succeeding ECG
complex until there is a P wave not followed by a QRS
• P:QRS ratio: 3:2, 4:3, 5:4, and so forth
CONDUCTION ABNORMALITIES
SECOND-DEGREE AV BLOCK, TYPE I (WENCKE-BACH)
CONDUCTION ABNORMALITIES
SECOND-DEGREE AV BLOCK, TYPE I (WENCKE-BACH)
CONDUCTION ABNORMALITIES
SECOND-DEGREE AV BLOCK, TYPE II
• Ventricular and atrial rate: Depends on underlying rhythm
• Ventricular and atrial rhythm: RR interval may be irregular
depending on the P:QRS ratio
• QRS shape and duration: Usually anormal but may be normal
• P wave: In front of the QRS complex; shape depends on
underlying rhythm
• PR interval: PR interval is constant for those P waves just
before QRS complexes
• P:QRS ratio: 2:1, :1, 4:1, 5:1, and so forth
CONDUCTION ABNORMALITIES
SECOND-DEGREE AV BLOCK, TYPE II
CONDUCTION ABNORMALITIES
THIRD-DEGREE AV BLOCK
• Ventricular and atrial rate: Depends on the escape and
underlying rhythm
• Ventricular and atrial rhythm: PP interval is regular and RR
interval is regular, but PP interval is not equal to RR interval
• QRS shape and duration: Depends on escape rhythm
• P wave: Depends on underlying rhythm
• PR interval: Very irregular
• P:QRS ratio: More P waves than QRS complexes
CONDUCTION ABNORMALITIES
THIRD-DEGREE AV BLOCK
CONDUCTION ABNORMALITIES
THIRD-DEGREE AV BLOCK
You might also like
- Strongholds of HeritageDocument9 pagesStrongholds of Heritageusman zafarNo ratings yet
- Official History of 86th DivisionDocument344 pagesOfficial History of 86th DivisionFilipNo ratings yet
- ECG-EKG Presentation - Gunda GDocument21 pagesECG-EKG Presentation - Gunda GGadzikaNo ratings yet
- Electro Cardiogram & DysrythmiasDocument40 pagesElectro Cardiogram & DysrythmiasshobharamkrishnaNo ratings yet
- Electrocardiography (ECG) Recording and InterpretationDocument59 pagesElectrocardiography (ECG) Recording and Interpretationkhushsandhu0% (1)
- Diagnostic Investigations of Cardiovascular System: A Presentation by Tejaswini MDocument70 pagesDiagnostic Investigations of Cardiovascular System: A Presentation by Tejaswini MDea Amelia YolandaNo ratings yet
- Cardiac Arrest: April B. Perez, RN, Man, PHD, FpchaDocument50 pagesCardiac Arrest: April B. Perez, RN, Man, PHD, Fpchayuuki konnoNo ratings yet
- N12 Cardiac DysrhythmiasDocument68 pagesN12 Cardiac Dysrhythmiaskathbondoc03No ratings yet
- Ekg PsikDocument69 pagesEkg PsikZEISVA APRILIANINGRUMNo ratings yet
- Tomasz WikarekDocument95 pagesTomasz Wikareknamar13766No ratings yet
- Kuliah EKG Blok Kegawatdaruratan September 2018Document122 pagesKuliah EKG Blok Kegawatdaruratan September 2018khanzaisdiharanaNo ratings yet
- Electrocardiogram: By: Keverne Jhay P. Colas, RN, MANDocument72 pagesElectrocardiogram: By: Keverne Jhay P. Colas, RN, MANGaras AnnaBerniceNo ratings yet
- Electrocardiogram: Electrocardiogram EKG Heart Heart's Electrical Activity DiagnosisDocument38 pagesElectrocardiogram: Electrocardiogram EKG Heart Heart's Electrical Activity DiagnosislorhenzsoNo ratings yet
- Basic of ECG: Prepared By: Zahid HussainDocument38 pagesBasic of ECG: Prepared By: Zahid HussainZahid Hussain100% (1)
- ECG InterpretationDocument95 pagesECG InterpretationShiela Mae Lopez100% (11)
- ECG ArrythemiaDocument79 pagesECG ArrythemiaMahadevNo ratings yet
- ECGs The Basics (Part 1) LectureDocument32 pagesECGs The Basics (Part 1) Lectureliudmyla zakordonetsNo ratings yet
- ECGs The Basics (Part 1) LectureDocument33 pagesECGs The Basics (Part 1) Lectureliudmyla zakordonetsNo ratings yet
- Ecg Treadmill and Holter TestDocument77 pagesEcg Treadmill and Holter TestRiteka Singh100% (1)
- Atrial FlutterDocument16 pagesAtrial Flutterapi-527603714100% (1)
- Chapter - 036 Arrhythmias ClassDocument129 pagesChapter - 036 Arrhythmias ClassWisdomIsMiseryNo ratings yet
- ACLS CE-Part I of III - ECG Strip Interpretation W Case Scenarios SupplementalDocument80 pagesACLS CE-Part I of III - ECG Strip Interpretation W Case Scenarios SupplementalMarc Imhotep Cray, M.D.100% (2)
- NUR207 Lecture3 CVS 07012021Document197 pagesNUR207 Lecture3 CVS 07012021Ashley TsoiNo ratings yet
- Arrhythmia Clinical PracticeDocument12 pagesArrhythmia Clinical PracticeSaba ElmahadiNo ratings yet
- EKG 12 Leads: Internal Medicine 2010Document59 pagesEKG 12 Leads: Internal Medicine 2010M Lukman HakimNo ratings yet
- Ecg in ExDocument70 pagesEcg in ExLakshmi PrasannaNo ratings yet
- ECG UpdatedDocument115 pagesECG Updatedmominarasool7No ratings yet
- Electrocardiography (Ecg) : Presented By: Fahad I. HussienDocument102 pagesElectrocardiography (Ecg) : Presented By: Fahad I. HussienMustafa A. DawoodNo ratings yet
- Electrical Impulse Viewed: Interpretation of The ElectrocardiogramDocument41 pagesElectrical Impulse Viewed: Interpretation of The ElectrocardiogramNesru Ahmed AkkichuNo ratings yet
- Ecg Interpretation New TemplateDocument88 pagesEcg Interpretation New TemplateJonathan NgNo ratings yet
- Basic Arrythmias: Prof. Maximin A. Pomperada, RN, MNDocument70 pagesBasic Arrythmias: Prof. Maximin A. Pomperada, RN, MNRellie CastroNo ratings yet
- ECG ECG Basics Presentation 201309101527422446 PDFDocument45 pagesECG ECG Basics Presentation 201309101527422446 PDFRamesh RajNo ratings yet
- Aritmia LetalDocument49 pagesAritmia LetalfebriyakNo ratings yet
- EcgDocument248 pagesEcgRohini SelvarajahNo ratings yet
- MUCLecture 2021 1292271Document34 pagesMUCLecture 2021 1292271Kouka MahfoudiNo ratings yet
- ElectrocardiogramDocument29 pagesElectrocardiogrammahnoorNo ratings yet
- Acute Coronary SyndromeDocument79 pagesAcute Coronary SyndromeMuhammad Yufimar Rizza FadilahNo ratings yet
- Workshop Pit IV THN 2017Document57 pagesWorkshop Pit IV THN 2017anettepardedeNo ratings yet
- Lec7 Sem2 CVSWK3 20140920 PDFDocument12 pagesLec7 Sem2 CVSWK3 20140920 PDFAprina RosyadahNo ratings yet
- Basics ECGDocument102 pagesBasics ECGAnnie KhanNo ratings yet
- Module 1.ECG BasicDocument11 pagesModule 1.ECG BasicFerry SofyanriNo ratings yet
- Cardiac Arrhythmia & Basics ECGDocument79 pagesCardiac Arrhythmia & Basics ECGMazhar UllahNo ratings yet
- Cardiovascular DisordersDocument9 pagesCardiovascular Disordersdlneisha6175% (4)
- Basic EKG InterpretationDocument48 pagesBasic EKG InterpretationAimee Ann Pauco MacaraegNo ratings yet
- Basic Ecg: A Report By: Clinical Clerk Mary Hazel TeDocument74 pagesBasic Ecg: A Report By: Clinical Clerk Mary Hazel TeHazel Arcosa100% (1)
- Prof. Maila Claire A. Lichauco, RN, MANDocument86 pagesProf. Maila Claire A. Lichauco, RN, MANCedie GomezNo ratings yet
- Normal Sinus RhythmDocument48 pagesNormal Sinus RhythmStella mNo ratings yet
- No VideoDocument47 pagesNo VideoTimothy John BautistaNo ratings yet
- ACLS SubhankarDocument87 pagesACLS SubhankarMarc Andreo MalalaNo ratings yet
- ECG Rhythm InterpretationDocument200 pagesECG Rhythm InterpretationabramNo ratings yet
- ECG3Document58 pagesECG3Plzstudylav SyedNo ratings yet
- 3881 - Prosedur Pendaftaran Internship Per November 2016Document57 pages3881 - Prosedur Pendaftaran Internship Per November 2016Munawir_Syam91No ratings yet
- APEC 611 Scientific and Industrial Instrumentation: Electrocardiogram (ECG)Document22 pagesAPEC 611 Scientific and Industrial Instrumentation: Electrocardiogram (ECG)Faisal Bin KashemNo ratings yet
- Ecg Reading PresntDocument101 pagesEcg Reading PresntbasilielnasirNo ratings yet
- Diagnostic Investigations of Cardiovascular System: A Presentation by Tejaswini MDocument70 pagesDiagnostic Investigations of Cardiovascular System: A Presentation by Tejaswini MKusum RoyNo ratings yet
- ECG MonitoringDocument96 pagesECG MonitoringJey BautistaNo ratings yet
- Ecg Interpretation: Presented by:-ROHINI RAI M SC Nursing Part I, C.O.N, N.B.M.C.HDocument69 pagesEcg Interpretation: Presented by:-ROHINI RAI M SC Nursing Part I, C.O.N, N.B.M.C.HRohini RaiNo ratings yet
- ECG (Unit3)Document34 pagesECG (Unit3)Komal DagarNo ratings yet
- ECG Complete LectureDocument33 pagesECG Complete LectureDr. SUVA NATHNo ratings yet
- Cardio AssessmentDocument104 pagesCardio Assessmentlowell.cerezo.ihsNo ratings yet
- D_4_heart__2_Document22 pagesD_4_heart__2_Jyoti singhNo ratings yet
- EKG and ECG Interpretation: Learn EKG Interpretation, Rhythms, and Arrhythmia Fast!From EverandEKG and ECG Interpretation: Learn EKG Interpretation, Rhythms, and Arrhythmia Fast!No ratings yet
- MIl-C-70508 Municion Cal. 9 MMDocument17 pagesMIl-C-70508 Municion Cal. 9 MMDavid BasanteNo ratings yet
- Appendix 1: I. Exercise ToleranceDocument5 pagesAppendix 1: I. Exercise Tolerancejfcule1No ratings yet
- Chapter 1 Introduction To International BusinessDocument19 pagesChapter 1 Introduction To International BusinessKushagra RathiNo ratings yet
- 01-System Devices Configuration - Rev GDocument36 pages01-System Devices Configuration - Rev GPABITRA PATRANo ratings yet
- PDF Oxford Textbook of Neuropsychiatry Niruj Agrawal Ebook Full ChapterDocument53 pagesPDF Oxford Textbook of Neuropsychiatry Niruj Agrawal Ebook Full Chapterjames.fahey314100% (1)
- Inventions and InventorsDocument26 pagesInventions and Inventorstaniaul94No ratings yet
- MATLAB-Simulink Based Analysis ofDocument4 pagesMATLAB-Simulink Based Analysis ofAmare KassawNo ratings yet
- Proposal Rev 02Document30 pagesProposal Rev 02suronocaturatmojo100% (1)
- MAC Layer Protocols For Sensor Networks: Leonardo Leiria FernandesDocument29 pagesMAC Layer Protocols For Sensor Networks: Leonardo Leiria FernandesSrinivas GopisettiNo ratings yet
- AnswersDocument8 pagesAnswersDaniyal AsifNo ratings yet
- Insight NDT Equipment LTD - ..Document2 pagesInsight NDT Equipment LTD - ..aoxoxzNo ratings yet
- EP-501, Evolution of Indian Economy Midterm: Submitted By: Prashun Pranav (CISLS)Document8 pagesEP-501, Evolution of Indian Economy Midterm: Submitted By: Prashun Pranav (CISLS)rumiNo ratings yet
- MaglevDocument10 pagesMaglevCaramihai DenisNo ratings yet
- DIYode Issue 1 July 2017Document100 pagesDIYode Issue 1 July 2017Victor Hugo Garay Saez100% (2)
- WSP India Compendium of Good Practices Rural Water Supply SchemesDocument104 pagesWSP India Compendium of Good Practices Rural Water Supply SchemesNguyen Van KienNo ratings yet
- Creative Writing Q1W1Document39 pagesCreative Writing Q1W1Jhun Ar-Ar Roa RamosNo ratings yet
- Uh - B-Eye-D Uh - Bil-Ih-Tee: Senior NESC-GE 2018 Regional Round Word List Grades 9, 10, 11, 12Document12 pagesUh - B-Eye-D Uh - Bil-Ih-Tee: Senior NESC-GE 2018 Regional Round Word List Grades 9, 10, 11, 12Tiko MakharadzeNo ratings yet
- Fire Phenomena of Rigid Polyurethane FoamsDocument22 pagesFire Phenomena of Rigid Polyurethane FoamsNicola MelaNo ratings yet
- Behavioral Neuroscience of Motivation: Eleanor H. Simpson Peter D. Balsam EditorsDocument584 pagesBehavioral Neuroscience of Motivation: Eleanor H. Simpson Peter D. Balsam EditorsKyle penzes100% (1)
- Resistors Module 01Document10 pagesResistors Module 01VinodKumarTummalurNo ratings yet
- Isotonix OPC-3 Sep 2016Document4 pagesIsotonix OPC-3 Sep 2016Pching Yong100% (1)
- Evaluation of SHMP and Advanced Scale Inhibitors For Control of and Scales in RO DesalinationDocument10 pagesEvaluation of SHMP and Advanced Scale Inhibitors For Control of and Scales in RO DesalinationKool LokeshNo ratings yet
- 1MRK002136-D: Package of Contact Sockets 20A, 100 PCSDocument1 page1MRK002136-D: Package of Contact Sockets 20A, 100 PCSWilfridoMatusSanchesNo ratings yet
- Mini Project Report On: Visvesvaraya Technological UniversityDocument8 pagesMini Project Report On: Visvesvaraya Technological UniversityTejáś ĢøwđâNo ratings yet
- Ricketts - Insurance Is PlaintiffDocument24 pagesRicketts - Insurance Is PlaintiffAnn DwyerNo ratings yet
- Leak Detector and Auto Cut OffDocument8 pagesLeak Detector and Auto Cut OffARUN CHRISTEL ANo ratings yet
- Ratio, Variation and Proportion: MATH10 AlgebraDocument19 pagesRatio, Variation and Proportion: MATH10 AlgebraEd VillNo ratings yet