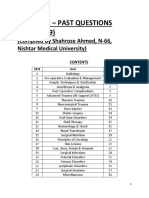
Professional Documents
Culture Documents
BIRADS
BIRADS
Uploaded by
anjeliemendozaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
BIRADS
BIRADS
Uploaded by
anjeliemendozaCopyright:
Available Formats
Current Status and Future of BI-RADS in Multimodality
Imaging, From the AJR Special Series on Radiology
Reporting and Data Systems
Mohammad Eghtedari, MD, PhD1, Alice Chong, MD, MHCI, Rebecca Rakow-Penner, MD, PhD, Haydee Ojeda-Fournier, MD
Downloaded from ajronline.org by 202.90.128.252 on 03/27/24 from IP address 202.90.128.252. Copyright ARRS. For personal use only; all rights reserved
Breast Imaging · Review
Keywords
BI-RADS is a communication and data tracking system that has evolved since its
BI-RADS, breast cancer, breast ultrasound,
dynamic contrast-enhanced breast MRI, inception as a brief mammography lexicon and reporting guide into a robust struc-
mammography tured reporting platform and comprehensive quality assurance tool for mammog-
raphy, ultrasound, and MRI. Consistent and appropriate use of the BI-RADS lexicon
Submitted: Sep 28, 2020 terminology and assessment categories effectively communicates findings, esti-
Revision requested: Oct 16, 2020 mates the risk of malignancy, and provides management recommendations to pa-
Revision received: Nov 12, 2020 tients and referring clinicians. The impact of BI-RADS currently extends internation-
Accepted: Dec 1, 2020
ally through six language translations. A condensed version has been proposed to
First published online: Dec 9, 2020
facilitate a phased implementation of BI-RADS in resource-constrained regions. The
The authors declare that they have no primary advance of the 5th edition of BI-RADS is harmonization of the lexicon terms
disclosures relative to the subject matter of across mammography, ultrasound, and MRI. Harmonization has also been achieved
this article. across these modalities for the reporting structure, assessment categories, manage-
ment recommendations, and data tracking system. Areas for improvement relate to
Based on presentations at the Radiological certain common findings that lack lexicon descriptors and a need for further clarifica-
Society of North America 2014 annual tion of proper use of category 3. BI-RADS is anticipated to continue to evolve for ap-
meeting, Chicago, IL, and the 2019 plication to a range of emerging breast imaging modalities.
European Congress of Radiology annual
meeting, Vienna, Austria.
BI-RADS was developed and updated to the current 5th edition by committees compris-
ing breast imaging radiologists and breast-specific subspecialty clinicians [1–5]. It has evolved
from a simple mammography lexicon to a multimodality lexicon for mammography, ultra-
sound (US), and MRI. As a structured reporting platform and comprehensive quality assur-
ance tool, BI-RADS provides assessment categories and management recommendations.
This review describes the origin, current functions, and potential future applications of
BI-RADS. It summarizes breast imaging lexicons’ harmonization across multiple imaging
modalities, resulting in improved reporting and communication.
Past
The first edition of BI-RADS in 1992 introduced the practice of standardized reporting
in mammography whereby a specific lexicon of imaging features was created to provide
specific and consistent management recommendations [1]. Lexicon descriptors predict-
ed probabilities for both benign and malignant disease on the basis of lesion shape and
margin across multiple modalities including mammography, US, and breast MRI (Figs. 1
and 2). Subsequent editions of BI-RADS were released in 1995, 1998, and 2003 [2–4]. The
3rd edition (1998) was the first to contain an atlas of images to illustrate examples of each
descriptor [3]. The 4th edition (2003) revised terminology; subdivided category 4 findings
into a, b, and c; and introduced US and MRI standardized reporting [4].
Present
The BI-RADS 5th edition, copyrighted in 2013 and released in February 2014, is substan-
Eghtedari et al.
tially expanded [5]. It contains over 700 illustrations and has an accompanying electronic
BI-RADS in Multimodality Imaging version. The digital BI-RADS manual provides hyperlinks to lexicon descriptors, frequently
Breast Imaging
asked questions (FAQ), and references. Reorganization and consolidation of terms include
Review simplification of US and MRI lexicon descriptors in the special cases section. The 5th edi-
Eghtedari M, Chong A, Rakow-Penner R, tion also allows a diagnosis to serve as descriptor; for example, “post-surgical change” may
Ojeda-Fournier H be used to describe an area of postsurgical change rather than describing shape, margins,
and echogenicity of the finding or findings (Fig. 3). New lesion descriptors include devel-
doi.org/10.2214/AJR.20.24894 oping asymmetry for mammography, elasticity assessment for US (Fig. 4), and breast im-
AJR 2021; 216:860–873 plant descriptors for MRI (Fig. 5).
ISSN-L 0361–803X/21/2164–860 1
All authors: Department of Radiology, University of California San Diego Health System, 9400 Campus Point Dr,
© American Roentgen Ray Society La Jolla, CA 92037. Address correspondence to H. Ojeda-Fournier (hojeda@health.ucsd.edu).
860 | www.ajronline.org AJR:216, April 2021
BI-RADS in Multimodality Imaging
Although assessment categories and recommendations re-
main unchanged in the 5th edition, BI-RADS categories and rec- HIGHLIGHTS
ommendations are now decoupled and may stand independent-
ly. For instance, BI-RADS category 2 is assigned to a breast The primary advance of the 5th edition of BI-RADS is
abscess or a simple cyst that is symptomatic because of size to harmonization of lexicon terms across mammography,
indicate benignity. Recommendation for aspiration may be made US, and MRI.
for symptomatic relief rather than a recommendation to return to The assessment categories 0 through 6 estimate prob-
Downloaded from ajronline.org by 202.90.128.252 on 03/27/24 from IP address 202.90.128.252. Copyright ARRS. For personal use only; all rights reserved
annual mammography that was previously coupled to a BI-RADS ability of malignancy and provide management rec-
category 2 assignment. This change allows flexibility in manage- ommendations; further clarification of proper usage of
ment recommendations while maintaining accurate medical au- category 3 is warranted.
dits based on imaging findings.
BI-RADS will likely continue to evolve for application to
Other improvements to the BI-RADS manual include an ex-
emerging breast imaging modalities, including molec-
panded FAQ section and data tables summarizing published
ular breast imaging, contrast-enhanced mammogra-
studies that validate descriptors in the lexicon (e.g., the likelihood
phy, and positron emission mammography.
of malignancy associated with the distribution of calcifications).
The BI-RADS website provides publicly available downloadable
reference cards, FAQ documents, a digital breast tomosynthesis dation. However, BI-RADS category 3 remains confusing and in-
(DBT) supplement, and selected content from the mammogra- correctly used [10]. Three BI-RADS category 3 findings that have
phy, US, and MRI manuals. Open access to website content in- been validated for use at baseline mammography or in exam-
cludes a summary of clinically relevant audits, guidance on data inations with no available prior imaging include grouped round
to be collected, and derived data to evaluate. (punctate) calcifications, circumscribed solitary mass, or a focal
asymmetry with no US correlate after complete diagnostic eval-
Assessment Categories and Recommendations uation [11–13]. Specific US criteria for BI-RADS category 3 include
Table 1 summarizes the seven assessment categories with as- nonpalpable circumscribed oval masses suggesting fibroadeno-
sociated standardized recommendations. The Mammography ma and complicated cysts. Evidence for specific criteria, appro-
Quality Standards Act (MQSA) regulations mandate that each priate length of follow-up, or acceptable cancer detection rates
mammography report include the assessment category [6]. Spe- is lower for MRI BI-RADS category 3, possibly relating to the high-
cifically, the report must include the assessment category word, er cancer yield for lesions in that category compared with mam-
rather than the number. For example, a negative screening mam- mographically detected BI-RADS category 3 lesions [14]. Grimm
mogram needs to state “negative.” Stating solely “category 1” or et al. [15] reported a 4.3% malignancy rate for MRI BI-RADS cate-
“BI-RADS category 1” is insufficient to comply with the federal gory 3 lesions, with nonmass enhancement exhibiting over twice
law. The final category applies to the overall study. However, fa- the malignancy rate of foci and masses. Several studies have re-
cilities may obtain permission to give a final assessment to each ported that the short-term follow-up afforded by BI-RADS cate-
breast. BI-RADS recommendations are concordant with the man- gory 3 allowed early-stage breast cancer identification, with no
dated assessment recommendations. Although not required by adverse outcomes attributed to a short delay in diagnosis [14–17].
MQSA, the same assessment categories and their accompanying BI-RADS category 3 should not be used in patients with a new
recommendation should also be used for US and MRI. breast cancer diagnosis, patients awaiting organ transplant, or
The assessment categories predict benign versus malignant patients who are pregnant or planning pregnancy.
breast disease [7, 8]. Categories 0, 1, and 2 are used at screening BI-RADS category 4, which has a broad range of expected risk
mammography, US, and MRI with the same implication. Catego- of malignancy (2% to < 95%), has been subdivided into catego-
ry 0 indicates an incomplete study, whereas categories 1 and 2 in- ries 4A (low suspicion, > 2% to 10% expected risk), 4B (moder-
dicate a benign finding. Categories 3, 4, and 5 are assigned after ate suspicion, > 10% to 50% expected risk), and 4C (high sus-
a complete diagnostic imaging evaluation. Performing diagnos- picion, > 50% to < 95% expected risk) to convey more specific
tic evaluation of a finding identified at screening mammography, expected risk of malignancy and to help address radiology-pa-
even if the finding has features characteristic of malignancy, allows thology discordance [18]. Category 4A can be used to direct cas-
direct conversation with the patient regarding the imaging finding es that may be safely downgraded, by using possible supple-
as well as discussion of next steps, including image-guided biopsy. mental technologies such as elastography or contrast-enhanced
BI-RADS category 3 is associated with a less than 2% likelihood mammography (CEM) [19–21]. Categories 4C and 5 should not
of malignancy and is not intended to be used when a radiologist be considered for downgrade because the risk of malignancy is
is unsure of a finding. A favorable outcome of appropriate use too high. In a single-institution study by Strigel et al. [22], subdi-
of BI-RADS category 3 is reducing the number of false-positive visions of BI-RADS category 4 on MRI yielded malignancy rates in
biopsies while maintaining an acceptable cancer detection rate. the same range as on mammography and US, supporting the use
A study by Berg et al. [9] of 45,202 women from 471 centers in of BI-RADS category 4 subdivisions for MRI. Otherwise, evidence
the National Mammography Database found a 1.86% cumulative for the MRI subdivision of category 4 is limited.
cancer yield for BI-RADS category 3, validating the appropriate BI-RADS category 5 implies a high likelihood of malignan-
use of this category. In that study, nearly 58% of the malignancies cy (95% or greater) and is applied identically across mammog-
were diagnosed at or before the 6-month interval follow-up, un- raphy, US, and MRI. Historically, a category 5 designation guides
derscoring the efficacy of this short-term follow-up recommen- surgeons toward a one-step surgical plan rather than an incision-
AJR:216, April 2021 861
Eghtedari et al.
TABLE 1: BI-RADS 5th Edition: Assessment Categories and Recommendations
Category Description Recommendation
0 Assessment is incomplete: examination is incomplete until further Additional evaluation with mammographic views, US, or less
evaluation is performed commonly MRI; counted toward the recall rate; after completion of
workup, new final assessment category is provided; should rarely
be used after US and MRI examinations are complete
Downloaded from ajronline.org by 202.90.128.252 on 03/27/24 from IP address 202.90.128.252. Copyright ARRS. For personal use only; all rights reserved
0 Assessment is incomplete: comparison films requested Category 0 for comparison should only be used when such
comparison is required to make a final assessment; not counted
toward the recall rate
1 Negative: completely negative examination Return to screening in 1 year (per ACR and SBI recommendations);
malignancy is not expected
2 Benign findings: radiologist chooses to describe a benign lesion that Return to screening in 1 year (per ACR and SBI recommendations);
carries no malignant potential recommendation is the same as in category 1; because description
of benign findings may lead to patient and referring clinician
anxiety and ordering of unnecessary imaging studies, category 1 is
preferred over category 2 whenever appropriate
3 Probably benign finding: controversial category to be used when a Follow-up examinations at short intervals of < 1 year (typically 6
finding is almost certainly benign but for which a short interval months) for 24–36 months is recommended; stability seen at the
follow-up is desired; unlikely to require biopsy and carries a chance end of follow-up is considered benign, at which point the finding is
of malignancy up to 2% reassigned category 2; category to be used after a complete
diagnostic workup of the lesion and is never to be used at the time
of screening mammograms
4a Suspicious abnormality: finding not classic for malignancy, > 2% to Some form of intervention is necessary, preferably image-guided
< 95% chance of malignancy core biopsy to establish a histopathologic diagnosis; follow-up of
biopsy results with radiology-pathology correlation is assigned to
the radiologist performing the biopsy; in clinical practices using the
subdivision categories, the report needs to first state suspicious,
followed by the subcategory (e.g., “suspicious right breast,
moderate suspicion for malignancy”)
5 Highly suggestive of malignancy: 95–100% chance of malignancy; Percutaneous core biopsy for tissue sampling to assist with oncologic
findings are characteristic of malignancy management or to plan one-stage definitive surgical intervention,
which may include lymph node sampling; benign result is
considered discordant, and additional intervention is typically
recommended and may include repeat image-guided vs surgical
biopsy
6 Known biopsy-proven malignancy: proven cancer that has not Appropriately used in patients who are undergoing neoadjuvant
completed definitive treatment therapy or in those who require further staging; clinical manage-
ment of the malignancy is recommended
Note—ACR = American College of Radiology, SBI = Society of Breast Imaging, US = ultrasound.
a
On mammography and US, category 4 can be subdivided into 4A (low suspicion for malignancy, > 2% to 10%), 4B (moderate suspicion for malignancy, > 10% to 50%),
and 4C (high suspicion for malignancy, > 50% to < 95%). This subdivision does not apply to MRI.
al biopsy that would necessitate a second surgery for oncologic Since the 5th edition of BI-RADS, several breast imaging mo-
therapy. If percutaneous biopsy of a category 5 lesion reveals a dalities have emerged that lack a defined lexicon within the BI-
benign histopathology, careful radiology-pathology correlation RADS standardization, including CEM, molecular breast imaging
is required to determine if repeat image-guided biopsy or surgi- (MBI), and positron emission mammography. Studies have at-
cal biopsy is the optimal next step. Finally, BI-RADS category 6, tempted to adapt existing descriptors for these modalities. For
introduced in the 4th edition, describes patients with a known example, several studies that evaluated the adoption of MRI BI-
malignancy who require no further imaging or who are undergo- RADS descriptors to CEM suggest that mass lesion features, in-
ing oncologic therapy. cluding shape, margin, and internal enhancement, convey the
most consistent results across MRI and CEM [19–21]. Kamal et
Lexicon al. [19] evaluated nonmass enhancement on CEM and reported
A lexicon is a list of standardized terms used to describe imag- that the MRI descriptors for symmetry, distribution, and internal
ing findings concisely and reproducibly. The lexicons for mam- enhancement were predictive of benign versus malignant out-
mography, US, and MRI have been validated in multiple studies comes and could be applied for CEM. Similarly, the BI-RADS lexi-
across the different imaging modalities [20, 21, 23–25]. The BI- con has been adapted for MBI and positron emission mammog-
RADS 5th edition harmonizes the terminology across imaging raphy, incorporating recommendations for lesion location, size,
modalities. Tables 2–4 summarize the relevant changes in the features, and qualitative and quantitative relevant molecular
mammography, US, and MRI lexicons. agent uptake [23–25].
862 AJR:216, April 2021
BI-RADS in Multimodality Imaging
TABLE 2: Masses, Calcifications, and Other Mammographic Findings in BI-RADS 5th Edition
Finding, Classification Descriptors Comments
Mass
Shape Oval, round, irregular Defined as a space-occupying 3D object; reordered “oval” and
“round” from 4th edition; removed “lobular” to avoid confusion
with margin
Downloaded from ajronline.org by 202.90.128.252 on 03/27/24 from IP address 202.90.128.252. Copyright ARRS. For personal use only; all rights reserved
Margin Circumscribed, obscured, microlobulated, indistinct, Describes the periphery of a mass and should not be confused with
spiculated the shape of a mass
Density High density, equal density, low density, fat-containing Density of a mass should not be confused with the mammographic
density and should not be used to describe asymmetries; replaced
“radiolucent” with “fat-containing”
Calcification
Typically benign Skin, vascular, coarse or “popcornlike,” large rodlike, To simplify descriptors, “eggshell” and “lucent-centered” were
round, rim, dystrophic, milk of calcium, suture combined into “skin calcifications”; “punctate” and “round” were
combined into the preferred term “round”
Suspicious morphology Amorphous, coarse, heterogeneous, fine pleomorphic, “Intermediate concern” and “higher probability malignancy”
fine linear or fine-linear branching calcifications were combined into the general category of
“suspicious” calcifications; the term “indistinct” was removed from
the lexicon, and the terms “fine pleomorphic,” “fine linear,” and
“fine-linear branching” were added
Distribution Diffuse, regional, grouped, linear, segmental Used with both benign and suspicious morphology; the terms
“scattered” and “clustered” were removed, with “grouped” added
as the term preferred to the latter
Architectural distortion Term may be a primary descriptor or may be used as an associated
feature
Asymmetry Asymmetry, global asymmetry, focal asymmetry, Added section for asymmetries alone and term “developing
developing asymmetry asymmetry”
Intramammary lymph Separated findings of intramammary lymph node, skin lesion, and
node solitary dilated duct; removed “asymmetric tubular structure”
Skin lesion
Solitary dilated duct
Associated features Skin retraction, nipple retraction, skin thickening, Removed “skin lesion,” which is now a separate finding;
trabecular thickening, axillary adenopathy, “calcifications” may be used as a primary descriptor or as an
architectural distortion, calcifications associated feature
Breast Composition higher breast density was associated with increased probabil-
Mammography ity that a finding may be hidden by normal dense breast tis-
Breast composition is determined by subjective analysis of the sue on mammography, the so-called masking effect [27–30]. In
area of attenuating glandular breast tissue on mammography and February 2019, the U.S. Congress passed a law that amended
is divided into four categories: almost entirely fatty, scattered areas the MQSA, mandating inclusion of lay language about breast
of fibroglandular density, heterogeneously dense, and extremely density in all mammography reports and summaries sent to
dense. Density on mammography was previously coded as densi- patients and their providers [31]. The risk associated with mam-
ty categories 1 through 4, creating confusion with the assessment mographic density remains controversial given the unresolved
categories. In the 5th edition, breast composition is now coded as question of whether dense breast tissue is a risk factor for
density a, b, c, or d for fatty through extremely dense. In addition, breast cancer per se, whether it decreases the sensitivity for
percentiles and quartiles assigned to breast composition on mam- finding cancers that are masked or obscured, or both [32, 33].
mography have been removed, and density is now assessed visu- Incorporation of texture analysis may help better define the
ally. Also, a breast may be assessed as dense on the basis of focal role of breast density in risk assessment, and this type of anal-
areas of dense breast tissue that potentially mask the presence of ysis will likely play a larger role in image interpretation in the
cancer, even if the entire breast is nondense. A single-institution future [34].
study reported increased use of the dense category assessment
based on these changes, even though not all radiologists adopted Ultrasound
the new BI-RADS density assessment [26]. The change in the US lexicon of “background echotexture” to
In 2009, Connecticut passed a law mandating radiologists to “tissue composition” represents an effort to harmonize “breast
inform women of their breast density, relying on evidence that composition” on US with mammographic density and breast fi-
AJR:216, April 2021 863
Eghtedari et al.
TABLE 3: Ultrasound Features in BI-RADS 5th Edition
Finding, Classification Descriptors Comments
Tissue composition Renamed, used only for whole breast screening ultrasound
Background echotexture
Homogeneous Fat, fibroglandular
Downloaded from ajronline.org by 202.90.128.252 on 03/27/24 from IP address 202.90.128.252. Copyright ARRS. For personal use only; all rights reserved
Heterogeneous
Masses
Shape Oval, round, irregular
Orientation Parallel, not parallel
Margin Circumscribed or not circumscribed (indistinct, angular, Removed “lesion boundary” category
microlobulated, spiculated)
Echo pattern Anechoic, hyperechoic, complex cystic and solid, Changed “complex” echo pattern descriptor to “complex cystic
hypoechoic, isoechoic, heterogeneous and solid,” added “heterogeneous” descriptor for echo
pattern
Posterior features No posterior acoustic features, enhancement, shadowing, Removed “surrounding tissue” category (some descriptors
combined pattern from that category added to “associated features” category)
Calcifications Calcifications in a mass, calcifications outside of a mass, Removed “micro” vs “macro” distinction, added “intraductal
intraductal calcifications calcifications”
Associated features Added “associated features” category (includes descriptors
from previous “lesion boundary” and “vascularity” categories)
Architectural distortion
Duct changes
Skin changes Skin thickening, skin retraction
Edema
Vascularity Absent, internal vascularity, vessels in rim
Elasticity assessment Soft, intermediate, hard Added descriptors for elasticity assessment, “elasticity” may be
used for both strain and shear wave in the assessment of
tissue stiffness
Special cases Simple cyst, clustered microcysts, complicated cyst, mass in Section expanded to simplify reporting by providing a unique
or on skin, foreign body including implants, lymph nodes diagnosis rather than trying to insinuate descriptors into a
(intramammary or axillary), vascular abnormalities (AVMs, diagnosis
pseudoaneurysms, or Mondor disease), postsurgical fluid
collection, fat necrosis
Note—The dedicated vascularity section has been removed in the 5th edition, and this section’s lexicon terms have been incorporated into the associated features
section. AVM = arteriovenous malformation.
broglandular tissue on MRI. Figure 6 shows how breast density on pausal women that indicated that the menstrual cycle phase did
mammography correlates with tissue composition on US and the not differentiate outcomes [39].
quantity of fibroglandular tissue on MRI.
Harmonization
MRI Harmonization of terminology across mammography, US,
Background parenchymal enhancement (BPE) is distinct from and MRI allows accurate correlation between imaging modali-
mammographic density or MRI fibroglandular tissue. BPE, in- ties, communication among radiologists, and uniform reporting
dependent of breast density, is more clearly associated with in- to referring clinicians. The lexicon applies identically to screen-
creased breast cancer risk. This association has been shown on ing and diagnostic mammography and is nearly uniform across
MRI and MBI [33, 35]. Agreement for BPE has been shown be- mammography, US, and breast MRI. The descriptors provide esti-
tween CEM and MRI, suggesting that CEM enhancement may mated risk of malignancy, and repeat biopsy may be required to
also be associated with increased breast cancer risk [36]. Screen- establish a histopathologic diagnosis when radiologic-patholog-
ing MRI was previously recommended to be scheduled in the ic correlation is discordant (Fig. 7).
second week of the menstrual cycle to decrease background BPE An example of the updates to allow harmonization in the 5th
[37, 38]. However, timing of the MRI based on menstrual cycle has edition of BI-RADS is the change of the MRI term “smooth mar-
been questioned on the basis of a study of over 1200 premeno- gins” to “circumscribed” to be concordant with mammography
864 AJR:216, April 2021
BI-RADS in Multimodality Imaging
TABLE 4: MRI Findings in BI-RADS 5th Edition
Finding, Classification Descriptors Comments
Amount of fibroglandular tissue Almost entirely fat, scattered fibroglandular tissue, heterogeneous New section harmonized with mammogra-
fibroglandular tissue, extreme fibroglandular tissue phy descriptors
BPE New section unique to contrast-enhanced
breast MRI
Downloaded from ajronline.org by 202.90.128.252 on 03/27/24 from IP address 202.90.128.252. Copyright ARRS. For personal use only; all rights reserved
Level Minimal, mild, moderate, marked
Symmetry Symmetric or asymmetric
Focus Changed definition of “focus”; no longer
based on size criteria
Mass Removed “enhancing internal septations”
and “central enhancement” because those
terms were infrequently used
Shape Oval (includes lobulated), round, irregular
Margin Circumscribed; not circumscribed (irregular, spiculated)
Internal enhancement Homogeneous, heterogeneous, rim enhancement, dark internal
septations
Nonmass enhancement
Distribution Focal, linear, segmental, regional, multiple regions, diffuse Removed “ductal”
Internal enhancement patterns Homogeneous, heterogeneous, clumped, clustered ring Removed “stippled/punctate,” added
“clustered ring”
Intramammary lymph node
Skin lesion
Nonenhancing findings Ductal hyperintensity on unenhanced T1-weighted imaging; cyst;
postoperative collections (hematoma or seroma); posttherapy skin
and trabecular thickening; nonenhancing mass; architectural
distortion; signal void from foreign bodies, clips, and so forth
Associated findings Nipple retraction, nipple invasion, skin retraction, skin thickening, skin Separated “associated findings” into
invasion, direct invasion, inflammatory breast cancer, axillary “nonenhancing findings,” “associated
adenopathy, pectoralis muscle invasion, chest wall invasion, architec- findings,” and “fat-containing lesions”
tural distortion
Fat-containing lesions Lymph nodes (normal or abnormal), fat necrosis, hamartoma,
postoperative seroma or hematoma with fat
Location of lesion and depth
Kinetic curve assessment (signal
intensity–time curve description)
Initial phase Slow, medium, fast The term “rapid” was changed to “fast” in
the initial phase of enhancement
Delayed phase Persistent, plateau, washout
Implant findings Implant material and lumen type, location, contour, intra- and Unenhanced MRI for implant evaluation is
extracapsular findings, water droplets, periimplant findings not assigned a BI-RADS category code
Note—BPE = background parenchymal enhancement.
and US. On the other hand, exceptions to harmonization in- allows kinetic assessment of changes in signal intensity over
volve descriptors specific to an imaging modality, such as mam- time. Accordingly, the MRI lexicon contains unique descriptors
mographic density, US echogenicity, and MRI signal intensity. for the initial and delayed phases of the contrast kinetics that
When lexicon descriptors overlap between benign and malig- do not apply to other imaging techniques (Fig. 9). Lexicon de-
nant features or are discordant between imaging modalities, the scriptors for contrast kinetics may be applied in the future to
most suspicious feature is used to recommend an assessment evolving technologies such as CEM. For example, Perry et al.
category and management (Fig. 8). [40] suggested applying existing descriptors to CEM by lever-
The lexicon descriptors that have evolved for specific imag- aging mammographic lesion descriptors for low-energy images
ing techniques may not be amenable to harmonization. Spe- and MRI descriptors (BPE and enhancement characteristics) for
cifically, the MRI technique of dynamic contrast enhancement recombined images.
AJR:216, April 2021 865
Eghtedari et al.
Multimodality imaging allows mammography, US, and MRI and multiple charts with established benchmarks. This section
to be used in a complementary way to evaluate breast cancer. of the BI-RADS manual is a critical quality assurance resource in
The limitations of mammography include limited evaluation of guiding feedback to individual radiologists as well as to practic-
the upper inner quadrant, lack of assessment of the chest wall, es as a whole.
and decreased sensitivity in dense breasts. US is limited by op- Each imaging modality chapter contains guidance subsections
erator dependence, and posterior shadowing from lesions may that have been expanded in the 5th edition. The guidance subsec-
decrease the ability to accurately assess the chest wall. Although tions provide useful information, advice, clarifications, and FAQ
Downloaded from ajronline.org by 202.90.128.252 on 03/27/24 from IP address 202.90.128.252. Copyright ARRS. For personal use only; all rights reserved
the amount of fibroglandular breast tissue does not limit MRI, answers. Examples from the guidance subsections include differ-
marked BPE may limit assessment of small masses. However, MRI entiation of mass versus asymmetry on mammography, use of ra-
is superior in the evaluation of the chest wall (Fig. 10). diopaque skin markers for clinically palpable lesions, details of the
In addition to harmonization of lesion descriptors, harmoni- US findings appropriate for coding a lesion as BI-RADS category
zation across modalities has also been applied for the reporting 3, and multiple points of clarification in the MRI BI-RADS lexicon.
structure, assessment categories, management recommenda-
tions, and data tracking system. Global Implications
The BI-RADS manual is used in North America and most of Eu-
Reporting rope [46]. The 5th edition has been translated to Spanish, Ger-
The BI-RADS manual provides guidance on the following as- man, Portuguese, Chinese, Japanese, and Greek.
pects of structured reporting: indication for the study, breast tis- In countries that lack the resources to support the full imple-
sue composition, descriptions of essential findings, comparison mentation of BI-RADS, ensuring consistent reporting, tracking pa-
with previous studies, assessment, and management. MQSA re- tient management, and improving performance and patient out-
quires facilities to provide a structured mammography report. comes may be challenging. The Breast Health Global Initiative has
Close to 40 million mammography examinations were per- proposed a phased implementation strategy to implement BI-
formed in the United States last year, most of which were inter- RADS in low-resource areas. The use of a condensed version of BI-
preted using a structured report [41]. Increasing familiarity with RADS, such as one containing limited descriptors from the breast
mammography structured reports will likely lead to increased ef- US lexicon, is recommended before the transition to full BI-RADS
ficiency by referring clinicians [42]. Although not part of MQSA, for each phase of implementation [47]. In Uganda, breast US edu-
the same structured reporting should be used across all breast cation using a condensed BI-RADS resulted in improved interpre-
imaging modalities. Whenever possible, a combined report tative performance and fewer unnecessary biopsies [48].
should be issued. For example, if a patient presents for diagnos-
tic evaluation and both mammography and US are performed, Current Limitations
then a combined report containing a section for mammography Several limitations of varying clinical importance are evident
findings and a separate section for US findings, with a final overall in the use of BI-RADS. For example, the definition of “regional
assessment and recommendation for both modalities, is encour- distribution” of an abnormal finding varies between mammog-
aged and ideal for decreasing confusion. Consider a patient who raphy and MRI. Although a regional distribution of calcifications
presents for a palpable finding. Mammography shows no posi- on mammography means that the calcifications are more exten-
tive findings, but further US evaluation is required (category 0). sive than 2 cm but smaller than a segment, regional distribution
US performed the same day shows a simple cyst (category 2). In of nonmass enhancement on MRI implies that the area of abnor-
this scenario, two separate reports with two different recommen- mality is in at least one quadrant and more than a single duct sys-
dations (i.e., recommendation for additional imaging, followed tem of the breast.
by a recommendation for return to routine screening) could be a A main goal of BI-RADS is to simplify management. Therefore,
source of confusion to the patient and referring clinician. the differential use of BI-RADS categories 1 and 2 is controversial
given that their management is identical. Although some radiol-
Guidance and Audit Parameters ogists comment on benign findings (calcifications, stable masses,
MQSA requires a minimum audit of all mammography facilities or asymmetries, all of which are category 2), other radiologists
and is subject to annual review during the MQSA inspection. As choose not to comment on them. The guidance chapter suggests
noted, each mammography report must be assigned one of the that whenever possible, the same category (either 1 or 2) be ap-
seven assessment categories. For screening mammography, BI- plied from year to year to avoid confusing patients and referring
RADS categories 0 and 3 are considered positive in the medical clinicians. The same issue applies to the management of BI-RADS
audit, whereas BI-RADS categories 1 and 2 are considered nega- 4 and five lesions, and within BI-RADS category 4, to categories
tive. The use of BI-RADS categories 4 and 5 are discouraged in the 4A, 4B, and 4C findings. Both categories 4 and 5 predict malig-
screening setting. During diagnostic imaging workup, BI-RADS nancy and warrant recommendation for biopsy, thus creating op-
category 3 is considered negative for audit purposes. Appropri- portunity for confusion among patients and referring providers.
ate examination coding allows efficient outcome tracking. Common findings that lack lexicon descriptors also present
Important audit parameters include cancer detection rate per a limitation. For example, benign postsurgical scar (without an
1000 women, recall rate, PPV, interval cancer rate, sensitivity, and associated fluid collection), though commonly encountered in
specificity [8, 43–45]. A section of the 5th edition manual is ded- breast imaging practices, is not a descriptor in the mammogra-
icated to follow-up and outcome monitoring and includes a de- phy lexicon. The descriptor “architectural distortion” may be ap-
tailed glossary of statistical terms, guidance for data calculation, plied to this finding, but architectural distortion is presumed to
866 AJR:216, April 2021
BI-RADS in Multimodality Imaging
be a malignancy until proven otherwise. Additional verbiage is gists who may not be breast subspecialists is therefore particu-
needed to clarify that the architectural distortion represents a larly important.
benign scar, undermining the goal of simplifying the report. Also,
the mammography lexicon definitions of “mass” and “asymme- Conclusion
try” do not take into account DBT technique. The mammogra- BI-RADS was developed as a communication, reporting, and data
phy lexicon defines a mass as a finding that is seen on two views. tracking system. Consistent and appropriate use of the BI-RADS lex-
However, using DBT, a “mass” or space-occupying lesion may be icon terminology and assessment categories effectively communi-
Downloaded from ajronline.org by 202.90.128.252 on 03/27/24 from IP address 202.90.128.252. Copyright ARRS. For personal use only; all rights reserved
seen over multiple planes in a single projection. The definition cates findings, articulates the degree of concern, and provides rec-
of “mass” could be refined to harmonize DBT with US and MRI, ommendations to patients and referring clinicians. The most recent
which would be particularly useful for developing computer-aid- BI-RADS edition harmonized the lexicon across the multiple imag-
ed detection and diagnosis software for DBT [49]. In addition, US ing modalities used to evaluate the breast. BI-RADS will continue to
“nonmass” lesions (focal hypoechoic areas with no associated evolve because changes in technology and research provide new
shape or margins) currently have no associated lexicon descrip- data points, including new breast imaging modalities.
tors [50]. These lesions are found in patients with and without
symptoms, and pathology correlation includes both benign and References
malignant histology. 1. American College of Radiology. Breast Imaging Reporting and Data System
The term “interval cancer” is defined as cancer that is found (BI-RADS). American College of Radiology, 1992
during the time between a regular screening mammogram that 2. American College of Radiology. Breast Imaging Reporting and Data System,
appears normal and the next screening mammogram. Interval 2nd ed. American College of Radiology, 1995
cancers are recognized in the BI-RADS manual in Europe, but 3. American College of Radiology. Illustrated Breast Imaging Reporting and
not in the United States. In the United States, BI-RADS instead Data System (BI-RADS), 3rd ed. American College of Radiology, 1998
encourages the calculation of a false-negative rate, which is the 4. D’Orsi C, Bassett L, Berg W, et al. American College of Radiology. Breast Imag-
rate of cancer detection within 1 year after negative mammogra- ing Reporting and Data System (BI-RADS), 4th ed. American College of Ra-
phy. This 1-year time frame was selected because most organiza- diology, 2003
tions recommend that screening mammography be performed 5. D’Orsi C, Sickles E, Mendelson E, et al. ACR BI-RADS Atlas, Breast Imaging
annually. This approach may warrant reevaluation, given that Reporting and Data System, 5th ed. American College of Radiology, 2013
the most recent American Cancer Society breast cancer screen- 6. 21 CFR 900.12(c)(1)(iv)
ing guidelines recommend switching to biennial mammography 7. Orel SG, Kay N, Reynolds C, Sullivan DC. BI-RADS categorization as a pre-
after 55 years old for a patient with average risk [51]. Future BI- dictor of malignancy. Radiology 1999; 211:845–850
RADS versions may benefit from a more precise definition for the 8. Liberman L, Abramson AF, Squires FB, Glassman JR, Morris EA, Dershaw
false-negative mammography rate or for interval cancer. DD. The breast imaging reporting and data system: positive predictive val-
ue of mammographic features and final assessment categories. AJR 1998;
Future 171:35–40
Emerging breast imaging modalities will follow suit in the use 9. Berg WA, Berg JM, Sickles EA, et al. Cancer yield and patterns of follow-up
of imaging descriptors. For example, MBI and CEM will benefit for BI-RADS category 3 after screening mammography recall in the nation-
from uniform BI-RADS terminology as they become more widely al mammography database. Radiology 2020; 296:32–41
adopted. The latest edition of the American Joint Committee on 10. Lee KA, Talati N, Oudsema R, Steinberger S, Margolies LR. BI-RADS 3: cur-
Cancer has already implemented breast cancer’s molecular pro- rent and future use of probably benign. Curr Radiol Rep 2018; 6:5
file as a parameter for breast cancer staging. Future BI-RADS edi- 11. Sickles EA. Management of probably benign breast lesions. Radiol Clin
tions should include terminology describing the molecular pro- North Am 1995; 33:1123–1130
file of cancer or the quantitative measurements of water diffusion 12. Sickles EA. Periodic mammographic follow-up of probably benign lesions:
on DWI [52, 53]. In de-escalation treatment, a malignancy may not results in 3,184 consecutive cases. Radiology 1991; 179:463–468
undergo surgical excision after neoadjuvant systemic therapy 13. Sickles EA. Breast calcifications: mammographic evaluation. Radiology
that leads to complete pathologic response on core biopsy of the 1986; 160:289–293
tumor bed. An assessment category descriptor will need to be 14. Spick C, Bickel H, Polanec SH, Baltzer PA. Breast lesions classified as proba-
developed for such lesions as they present for follow-up. bly benign (BI-RADS 3) on magnetic resonance imaging: a systematic re-
Future BI-RADS editions should also clarify category 3 lesions view and meta-analysis. Eur Radiol 2018; 28:1919–1928
[10, 14, 54]. Specifically, greater consideration should be given for 15. Grimm LJ, Anderson AL, Baker JA, et al. Frequency of malignancy and im-
what represents “sufficient experience” to justify using category aging characteristics of probably benign lesions seen at breast MRI. AJR
3 in MRI or for lesions other than calcifications, circumscribed sol- 2015; 205:442–447
id mass, or asymmetry. The definition of category 3 could also be 16. Chikarmane SA, Birdwell RL, Poole PS, Sippo DA, Giess CS. Characteristics,
expanded to include new or developing lesions such as develop- malignancy rate, and follow-up of BI-RADS category 3 lesions identified at
ing fat necrosis; it is currently limited to baseline studies or exam- breast MR imaging: implications for MR image interpretation and manage-
inations without comparison studies available. ment. Radiology 2016; 280:707–715
Studies have shown that training in BI-RADS increases inter- 17. Lee SE, Lee JH, Han K, et al. BI-RADS category 3, 4, and 5 lesions identified
pretative performance and agreement in feature analysis for at preoperative breast MRI in patients with breast cancer: implications for
both mammography and US [55, 56]. Continued BI-RADS train- management. Eur Radiol 2020; 30:2773–2781
ing and education of residents, fellows, and practicing radiolo- 18. Elezaby M, Li G, Bhargavan-Chatfield M, Burnside ES, DeMartini WB. ACR
AJR:216, April 2021 867
Eghtedari et al.
BI-RADS assessment category 4 subdivisions in diagnostic mammogra- strual cycle and age: influence on parenchymal contrast medium enhance-
phy: utilization and outcomes in the National Mammography Database. ment in MR imaging of the breast. Radiology 1997; 203:145–149
Radiology 2018; 287:416–422 39. Lee CH, Bryce Y, Zheng J, et al. Outcome of screening MRI in premenopaus-
19. Kamal RM, Helal MH, Mansour SM, et al. Can we apply the MRI BI-RADS al women as a function of the week of the menstrual cycle. AJR 2020;
lexicon morphology descriptors on contrast-enhanced spectral mam- 214:1175–1181
mography? Br J Radiol 2016; 89:20160157 40. Perry H, Phillips J, Dialani V, et al. Contrast-enhanced mammography: a sys-
20. Knogler T, Homolka P, Hoernig M, et al. Application of BI-RADS descriptors tematic guide to interpretation and reporting. AJR 2019; 212:222–231
Downloaded from ajronline.org by 202.90.128.252 on 03/27/24 from IP address 202.90.128.252. Copyright ARRS. For personal use only; all rights reserved
in contrast-enhanced dual-energy mammography: comparison with MRI. 41. Margolies LR, Pandey G, Horowitz ER, Mendelson DS. Breast imaging in the
Breast Care (Basel) 2017; 12:212–216 era of big data: structured reporting and data mining. AJR 2016; 206:259–264
21. Travieso-Aja MM, Maldonado-Saluzzi D, Naranjo-Santana P, et al. Evalua- 42. Weiss DL, Langlotz CP. Structured reporting: patient care enhancement or
tion of the applicability of BI-RADS® MRI for the interpretation of con- productivity nightmare? Radiology 2008; 249:739–747
trast-enhanced digital mammography. Radiologia (Madr) 2019; 61:477–488 43. Lehman CD, Arao RF, Sprague BL, et al. National performance benchmarks
22. Strigel RM, Burnside ES, Elezaby M, et al. Utility of BI-RADS assessment cat- for modern screening digital mammography: update from the Breast Can-
egory 4 subdivisions for screening breast MRI. AJR 2017; 208:1392–1399 cer Surveillance Consortium. Radiology 2017; 283:49–58
23. Narayanan D, Madsen KS, Kalinyak JE, Berg WA. Interpretation of positron 44. Sickles EA, Miglioretti DL, Ballard-Barbash R, et al. Performance bench-
emission mammography: feature analysis and rates of malignancy. AJR marks for diagnostic mammography. Radiology 2005; 235:775–790
2011; 196:956–970 45. Miglioretti DL, Ichikawa L, Smith RA, et al. Criteria for identifying radiologists
24. Narayanan D, Madsen KS, Kalinyak JE, Berg WA. Interpretation of positron with acceptable screening mammography interpretive performance on ba-
emission mammography and MRI by experienced breast imaging radiolo- sis of multiple performance measures. AJR 2015; 204:[web]W486–W491
gists: performance and observer reproducibility. AJR 2011; 196:971–981 46. Taylor K, Britton P, O’Keeffe S, Wallis MG. Quantification of the UK 5-point
25. Conners AL, Maxwell RW, Tortorelli CL, et al. Gamma camera breast imag- breast imaging classification and mapping to BI-RADS to facilitate compar-
ing lexicon. AJR 2012; 199:[web]W767–W774 ison with international literature. Br J Radiol 2011; 84:1005–1010
26. Irshad A, Leddy R, Lewis M, et al. Changes in breast density reporting pat- 47. Lam DL, Entezari P, Duggan C, et al. A phased approach to implementing
terns of radiologists after publication of the 5th edition BI-RADS guide- the Breast Imaging Reporting and Data System (BI-RADS) in low-income
lines: a single institution experience. AJR 2017; 209:943–948 and middle-income countries. Cancer 2020; 126(Suppl 10):2424–2430
27. Hooley RJ. Breast density legislation and clinical evidence. Radiol Clin North 48. Scheel JR, Peacock S, Orem J, et al. Improving breast ultrasound interpreta-
Am 2017; 55:513–526 tion in Uganda using a condensed Breast Imaging Reporting and Data Sys-
28. Destounis SV, Santacroce A, Arieno A. Update on breast density, risk esti- tem. Acad Radiol 2016; 23:1271–1277
mation, and supplemental screening. AJR 2020; 214:296–305 49. Chan HP, Wu YT, Sahiner B, et al. Characterization of masses in digital breast
29. Destounis S, Johnston L, Highnam R, Arieno A, Morgan R, Chan A. Using tomosynthesis: comparison of machine learning in projection views and
volumetric breast density to quantify the potential masking risk of mam- reconstructed slices. Med Phys 2010; 37:3576–3586
mographic density. AJR 2017; 208:222–227 50. Park KW, Park S, Shon I, et al. Non-mass lesions detected by breast US: strat-
30. Houssami N, Lee CI. The impact of legislation mandating breast density ification of cancer risk for clinical management. Eur Radiol 2020 Sep 4 [pub-
notification: review of the evidence. Breast 2018; 42:102–112 lished online]
31. Keating NL, Pace LE. New federal requirements to inform patients about 51. Oeffinger KC, Fontham ETH, Etzioni R, et al.; American Cancer Society.
breast density: will they help patients? JAMA 2019; 321:2275–2276 Breast cancer screening for women at average risk: 2015 guideline update
32. McCormack VA, dos Santos Silva I. Breast density and parenchymal pat- from the American Cancer Society. JAMA 2015; 314:1599–1614
terns as markers of breast cancer risk: a meta-analysis. Cancer Epidemiol 52. Baltzer P, Mann RM, Iima M, et al.; EUSOBI International Breast Diffusion-Weight-
Biomarkers Prev 2006; 15:1159–1169 ed Imaging Working Group. Diffusion-weighted imaging of the breast: a con-
33. King V, Brooks JD, Bernstein JL, Reiner AS, Pike MC, Morris EA. Background sensus and mission statement from the EUSOBI International Breast Diffu-
parenchymal enhancement at breast MR imaging and breast cancer risk. sion-Weighted Imaging Working Group. Eur Radiol 2020; 30:1436–1450
Radiology 2011; 260:50–60 53. Partridge SC, Zhang Z, Newitt DC, et al.; ACRIN 6698 Trial Team and I-SPY 2
34. Kontos D, Winham SJ, Oustimov A, et al. Radiomic phenotypes of mam- Trial Investigators. Diffusion-weighted MRI findings predict pathologic re-
mographic parenchymal complexity: toward augmenting breast density sponse in neoadjuvant treatment of breast cancer: the ACRIN 6698 multi-
in breast cancer risk assessment. Radiology 2019; 290:41–49 center trial. Radiology 2018; 289:618–627
35. Hruska CB, Geske JR, Conners AL, et al. Background parenchymal uptake 54. Michaels AY, Birdwell RL, Chung CSW, Frost EP, Giess CS. Assessment and
on molecular breast imaging and breast cancer risk: a cohort study. AJR management of challenging BI-RADS category 3 mammographic lesions.
2020 Jul 29 [published online] RadioGraphics 2016; 36:1261–1272
36. Sogani J, Morris EA, Kaplan JB, et al. Comparison of background parenchy- 55. Berg WA, Blume JD, Cormack JB, Mendelson EB. Training the ACRIN 6666
mal enhancement at contrast-enhanced spectral mammography and Investigators and effects of feedback on breast ultrasound interpretive
breast MR imaging. Radiology 2017; 282:63–73 performance and agreement in BI-RADS ultrasound feature analysis. AJR
37. Kuhl CK, Bieling HB, Gieseke J, et al. Healthy premenopausal breast paren- 2012; 199:224–235
chyma in dynamic contrast-enhanced MR imaging of the breast: normal 56. Berg WA, D’Orsi CJ, Jackson VP, et al. Does training in the Breast Imaging
contrast medium enhancement and cyclical-phase dependency. Radiolo- Reporting and Data System (BI-RADS) improve biopsy recommendations
gy 1997; 203:137–144 or feature analysis agreement with experienced breast imagers at mam-
38. Müller-Schimpfle M, Ohmenhaüser K, Stoll P, Dietz K, Claussen CD. Men- mography? Radiology 2002; 224:871–880
(Figures start on next page)
868 AJR:216, April 2021
BI-RADS in Multimodality Imaging
Downloaded from ajronline.org by 202.90.128.252 on 03/27/24 from IP address 202.90.128.252. Copyright ARRS. For personal use only; all rights reserved
A B C
Fig. 1—42-year-old woman with oval mass with circumscribed margins, consistent with fibroadenoma.
A, Right mediolateral oblique mammogram shows oval equal-density mass with circumscribed margins (arrow) in upper outer right breast.
B, Transverse ultrasound shows oval mass with circumscribed margins and hypoechoic echo pattern (arrow) corresponding to mammographic finding.
C, Dynamic axial contrast-enhanced T1-weighted MRI shows oval mass with circumscribed margins and homogeneous internal enhancement (arrow).
A B C
Fig. 2—70-year-old woman with invasive lobular breast cancer.
A, Right mediolateral oblique synthetic view digital breast tomosynthesis screening mammogram shows architectural distortion (circle).
B, Transverse ultrasound shows irregular hypoechoic mass with angular margins and posterior shadowing (arrow) corresponding to mammographic finding.
C, Axial dynamic contrast-enhanced T1-weighted breast MRI shows irregular mass with irregular margins and heterogeneous internal enhancement. Signal void from
biopsy clip is marked by arrow.
AJR:216, April 2021 869
Eghtedari et al.
Downloaded from ajronline.org by 202.90.128.252 on 03/27/24 from IP address 202.90.128.252. Copyright ARRS. For personal use only; all rights reserved
B C
Fig. 3—52-year-old woman who had undergone lumpectomy and radiation therapy and presented with
palpable finding (arrow) at left breast 3-o’clock position.
A, Left mediolateral oblique 2D mammogram shows focal asymmetry correlating with lumpectomy site.
B, Transverse ultrasound shows postsurgical seroma.
C, Axial T2-weighted MRI shows postoperative seroma with nonenhancing T2 hyperintensity. Simplified
ultrasound “special cases” lexicon allows diagnosis using “post-surgical change” descriptor.
Fig. 4—69-year-old woman with intracapsular rupture of silicone gel–filled implant. Axial fat-suppressed and
water-suppressed silicone-specific MRI shows keyhole sign (arrow) and subcapsular line (arrowhead).
870 AJR:216, April 2021
BI-RADS in Multimodality Imaging
Fig. 5—Adaptation of BI-RADS lexicon to novel
application of elastography. 30-year-old woman
with T2N0M0 invasive ductal carcinoma (estrogen
receptor–positive, progesterone receptor–negative,
HER2 [also known as ERBB2]-negative).
A, Right mediolateral oblique 2D mammogram
shows irregular high density mass with indistinct
margins (arrow).
B, Axial dynamic T1-weighted contrast-enhanced
Downloaded from ajronline.org by 202.90.128.252 on 03/27/24 from IP address 202.90.128.252. Copyright ARRS. For personal use only; all rights reserved
MRI shows irregular mass with irregular margins,
rim enhancement, and heterogeneous internal
enhancement (arrow).
C, Radial gray-scale ultrasound shows irregular mass
with angular margins and complex cystic and solid
echo patterns corresponding to mammographic and
MRI findings.
D, Radial shear wave elastography using acoustic
radiation force shows increased stiffness, suggesting
malignancy.
A B
C D
Fig. 6—Effects of breast tissue composition on
image interpretation in 40-year-old woman.
A, Left craniocaudal mammogram shows extremely
dense breast tissue, which lowers sensitivity of
mammography.
B, Left radial ultrasound shows homogeneous
fibroglandular background echotexture, concordant
with mammographic finding. Tissue composition is
only used in facilities that use screening ultrasound.
A B (Fig. 6 continues on next page)
AJR:216, April 2021 871
Eghtedari et al.
Downloaded from ajronline.org by 202.90.128.252 on 03/27/24 from IP address 202.90.128.252. Copyright ARRS. For personal use only; all rights reserved
C D
Fig. 6 (continued)—Effects of breast tissue composition on image interpretation in 40-year-old woman.
C, Axial T1-weighted non–fat-saturated MRI shows extreme fibroglandular tissue correlating with mammographic density, which does not limit MRI sensitivity.
D, Axial dynamic contrast-enhanced T1-weighted MRI shows minimal background parenchymal enhancement (BPE). When marked, BPE may limit sensitivity of MRI.
A B C
Fig. 7—62-year-old woman with abnormal mammogram.
A, Craniocaudal 2D mammogram shows irregular mass with spiculated margins and fine pleomorphic calcifications.
B, Transverse ultrasound shows irregular mass with angular margins and posterior shadowing (arrow) corresponding to mammogram finding. Ultrasound-guided
biopsy revealed stromal fibrosis without atypia or malignancy, which represented radiologic-pathologic discordance. Wire-guided localization and surgical excision
were recommended.
C, Specimen radiograph of excised lesion shows mass, calcifications, and clip marker. Histopathology revealed extensive sclerosing adenosis with no malignancy.
Fig. 8—55-year-old woman with biopsy-proven
triple-negative invasive ductal carcinoma,
noted as round mass. Imaging characteristics on
mammography, ultrasound (US), and MRI provide
complementary information.
A, Mediolateral oblique 2D right digital
mammogram shows high-density round mass with
circumscribed margins. High density is suspicious
finding on mammography.
B, Radial US shows round mass with circumscribed
margins and complex cystic and solid echo pattern
with posterior enhancement. Term “complex cystic
and solid” is suspicious finding, BI-RADS category
4C.
A B (Fig. 8 continues on next page)
872 AJR:216, April 2021
BI-RADS in Multimodality Imaging
Fig. 8 (continued)—55-year-old woman with
biopsy-proven triple-negative invasive ductal
carcinoma, noted as round mass. Imaging
characteristics on mammography, ultrasound (US),
and MRI provide complementary information.
C, Axial fat-saturated T2-weighted MRI shows
hyperintense fluid within mass.
D, Axial contrast-enhanced fat-saturated T1-
weighted MRI shows round mass with spiculated
Downloaded from ajronline.org by 202.90.128.252 on 03/27/24 from IP address 202.90.128.252. Copyright ARRS. For personal use only; all rights reserved
margins and rim enhancement. Spiculations and rim
enhancement are highly suggestive of malignancy,
BI-RADS category 5.
C D
Fig. 9—55-year-old woman with invasive
ductal carcinoma (estrogen receptor–positive,
progesterone receptor–negative, HER2 [also
known as ERBB2]-positive). MRI provides unique
quantitative kinetic information that is based on
signal intensity–time curve and further characterizes
lesions.
A and B, Axial T1-weighted fat-saturated dynamic
contrast-enhanced MR images without (A) and
with (B) kinetic color overlay superimposed over
segmental nonmass enhancement at site of known
malignancy. In this software package, blue indicates
persistent kinetics, yellow indicates plateau, and
red indicates washout. Most suspicious descriptor is
used to increase sensitivity. L1 = lesion 1.
A B
B C
Fig. 10—43-year-old woman with palpable invasive ductal breast cancer (estrogen receptor–positive,
progesterone receptor–positive, HER2 [also known as ERBB2]-negative). Descriptors may be based on information
provided by imaging technique; MRI shows chest wall invasion that is not seen on mammography or ultrasound.
A, Right 2D mediolateral oblique mammogram shows focal asymmetry (arrow) that is only seen in retrospect.
B, Longitudinal ultrasound shows irregular mass with indistinct margins corresponding to mammographic
finding.
C, Axial dynamic T1-weighted contrast-enhanced MRI shows irregular mass invading through chest wall (arrows).
A
AJR:216, April 2021 873
You might also like
- Surgery I - Topical Past Papers (2007-2019)Document41 pagesSurgery I - Topical Past Papers (2007-2019)AnmahNo ratings yet
- Breast Imaging: - DR Anamika Jha, MDDocument122 pagesBreast Imaging: - DR Anamika Jha, MDDr KhanNo ratings yet
- Mammography MachineDocument17 pagesMammography MachineGaurav Molankar100% (1)
- BI-RADS Terminology For Mam-Mography Reports: What Resi - Dents Need To KnowDocument2 pagesBI-RADS Terminology For Mam-Mography Reports: What Resi - Dents Need To KnowOncología CdsNo ratings yet
- Wbac 032Document14 pagesWbac 032dr.elahe.babantaherNo ratings yet
- Automatic Speech Recognition For Biomedical Data in Bengali LanguagDocument9 pagesAutomatic Speech Recognition For Biomedical Data in Bengali LanguagNicola NatalettiNo ratings yet
- Lenzi 2019Document12 pagesLenzi 2019Mainul HossainNo ratings yet
- New DNNSDocument5 pagesNew DNNSMaryam AhmedNo ratings yet
- Computer Methods and Programs in BiomedicineDocument15 pagesComputer Methods and Programs in BiomedicineDr Mohammed KamalNo ratings yet
- 005 - 2018 - Multimedia-Enhanced Radiology Reports Concept, Components, and ChallengesDocument21 pages005 - 2018 - Multimedia-Enhanced Radiology Reports Concept, Components, and ChallengesAušra KabišienėNo ratings yet
- Prostate Imaging Reporting and Data System Version 2.1: 2019 Update of Prostate Imaging Reporting and Data System Version 2Document12 pagesProstate Imaging Reporting and Data System Version 2.1: 2019 Update of Prostate Imaging Reporting and Data System Version 2crownofwormsNo ratings yet
- Hul TechDocument12 pagesHul TechMOHIT MALVIYA PGP 2020 BatchNo ratings yet
- Breast Cancer Detection by Leveraging Machine Learning - 2020 - ICT ExpressDocument5 pagesBreast Cancer Detection by Leveraging Machine Learning - 2020 - ICT ExpressvkvNo ratings yet
- Breast MRI Structured Report TEMPLATESDocument6 pagesBreast MRI Structured Report TEMPLATESGábor BorbásNo ratings yet
- Application of Computer-Aided Diagnosis in Breast Ultrasound Interpretation - Improvements in Diagnostic Performance According To Reader ExperienceDocument9 pagesApplication of Computer-Aided Diagnosis in Breast Ultrasound Interpretation - Improvements in Diagnostic Performance According To Reader ExperienceChuyên Mai TấtNo ratings yet
- 1 s2.0 S1361841520302838 MainDocument11 pages1 s2.0 S1361841520302838 Mainedfewf3No ratings yet
- Grupo 1Document7 pagesGrupo 1Oscar EstayNo ratings yet
- Identification of The Inferior Alveolar Canal Using Cone-Beam Computed Tomography vs. Panoramic Radiography: A Retrospective Comparative StudyDocument10 pagesIdentification of The Inferior Alveolar Canal Using Cone-Beam Computed Tomography vs. Panoramic Radiography: A Retrospective Comparative StudyKemas IrsanNo ratings yet
- Risk and Reliability Assessment in ChemicalDocument22 pagesRisk and Reliability Assessment in ChemicalragulNo ratings yet
- ACR TI-RADS: Pitfalls, Solutions, and Future DirectionsDocument13 pagesACR TI-RADS: Pitfalls, Solutions, and Future Directionsmapeos tiroides100% (1)
- Face-Iris Multi-Modal Biometric System Using Multi-Resolution Log-Gabor Filter With Spectral Regression Kernel Discriminant AnalysisDocument8 pagesFace-Iris Multi-Modal Biometric System Using Multi-Resolution Log-Gabor Filter With Spectral Regression Kernel Discriminant AnalysisnkNo ratings yet
- Pattern Recognition: Catarina Barata, M. Emre Celebi, Jorge S. MarquesDocument11 pagesPattern Recognition: Catarina Barata, M. Emre Celebi, Jorge S. MarquesMarcos OliveiraNo ratings yet
- Republic of The Philippines Department of Education Region VII, Central VisayasDocument4 pagesRepublic of The Philippines Department of Education Region VII, Central VisayasMarvin AmancioNo ratings yet
- Literature SurveyDocument11 pagesLiterature SurveyYeswanth YeswanthNo ratings yet
- Predicting Autism Spectrum Disorder Using Machine Learning ClassifiersDocument4 pagesPredicting Autism Spectrum Disorder Using Machine Learning Classifiersahfn79No ratings yet
- Certifications Systems As Independent and Rigorous Tools For Assessing Urban SustainabilityDocument15 pagesCertifications Systems As Independent and Rigorous Tools For Assessing Urban SustainabilityGoudaNo ratings yet
- Chexbert: Combining Automatic Labelers and Expert Annotations For Accurate Radiology Report Labeling Using BertDocument20 pagesChexbert: Combining Automatic Labelers and Expert Annotations For Accurate Radiology Report Labeling Using BertGhassane AnibaNo ratings yet
- European Journal of Radiology: SciencedirectDocument5 pagesEuropean Journal of Radiology: SciencedirectRachid RifaiNo ratings yet
- 1-5 Artificial Intelligence (AI) For Screening MammographyDocument13 pages1-5 Artificial Intelligence (AI) For Screening Mammography14mervekaya01No ratings yet
- ADS-Bsec: A Holistic Framework To Secure ADS-B: Thabet Kacem, Duminda Wijesekera and Paulo CostaDocument11 pagesADS-Bsec: A Holistic Framework To Secure ADS-B: Thabet Kacem, Duminda Wijesekera and Paulo CostaDimas Wahyu PrabowoNo ratings yet
- Benchmarking: An International Journal: Article InformationDocument45 pagesBenchmarking: An International Journal: Article InformationSamir KaleNo ratings yet
- Pacific Symposium On Biocomputing 2023Document12 pagesPacific Symposium On Biocomputing 2023RUIQI BAINo ratings yet
- Unit 3 - Assessment of Individuals With ASDDocument17 pagesUnit 3 - Assessment of Individuals With ASDHeeta PanchasaraNo ratings yet
- Archive of SID: Diagnostic Reference Levels at Intraoral and Dental Panoramic ExaminationsDocument4 pagesArchive of SID: Diagnostic Reference Levels at Intraoral and Dental Panoramic ExaminationsNindy PutriNo ratings yet
- Imagej Software in Periodontics An Insight.12Document3 pagesImagej Software in Periodontics An Insight.12NareshNo ratings yet
- A R R L - M R M: Dvancing Adiograph Epresentation Earn Ing With Asked Ecord OdelingDocument16 pagesA R R L - M R M: Dvancing Adiograph Epresentation Earn Ing With Asked Ecord OdelingThanh Võ Thị HoàiNo ratings yet
- Rhapsody Product Update Vision and RoadmapDocument17 pagesRhapsody Product Update Vision and RoadmapJaume MayorNo ratings yet
- Artículo 013 2023-IIDocument13 pagesArtículo 013 2023-IIhugo saire pumaNo ratings yet
- SC SustDocument26 pagesSC SustAziz Ibn MusahNo ratings yet
- Artificial Intelligence Solutions For Analysis of X-Ray ImagesDocument13 pagesArtificial Intelligence Solutions For Analysis of X-Ray ImagesYamah PrincewillNo ratings yet
- Radiology Information SystemDocument5 pagesRadiology Information SystemKARUN RAJ K MBA IB 2018-20No ratings yet
- Reducing Length of Stay Using LeanDocument42 pagesReducing Length of Stay Using LeanAsiimwe D Pius100% (1)
- 1 s2.0 S0959652620304650 MainDocument20 pages1 s2.0 S0959652620304650 Mainwagih elsharkawyNo ratings yet
- Linear Diophantine Fuzzy Rough Setson Paired Universeswith Multi Stage Decision AnalysisDocument19 pagesLinear Diophantine Fuzzy Rough Setson Paired Universeswith Multi Stage Decision AnalysiszanibNo ratings yet
- Session 3 - Gap AnalysisDocument23 pagesSession 3 - Gap AnalysisfreepassNo ratings yet
- 放射学中的持续学习人工智能:实施 原理和早期应用Document16 pages放射学中的持续学习人工智能:实施 原理和早期应用meiwanlanjunNo ratings yet
- Abdulaziz Alzeban 2017Document23 pagesAbdulaziz Alzeban 2017mariNo ratings yet
- 05 Strategic Challenges in Development Planning For Denpasar CityDocument8 pages05 Strategic Challenges in Development Planning For Denpasar CityMohammad Ilham AkbarNo ratings yet
- JDattaMegheInstMedSciUniv164794-2188987 003628Document3 pagesJDattaMegheInstMedSciUniv164794-2188987 003628Evelyn Dayanna Quinche CoronelNo ratings yet
- 10 1002@jmri 26896Document21 pages10 1002@jmri 26896Nina CavokNo ratings yet
- Rodgers - Challenges and PerspectivesDocument18 pagesRodgers - Challenges and PerspectivesAzis Kemal FauzieNo ratings yet
- VocabularyDocument4 pagesVocabularyRomeo De OsioNo ratings yet
- 16 The Chi-Square Test oDocument21 pages16 The Chi-Square Test oRahman RajabNo ratings yet
- Increasing The Efficient Usage of Electric Vehicle Range Effects of Driving Experience and Coping InformationDocument15 pagesIncreasing The Efficient Usage of Electric Vehicle Range Effects of Driving Experience and Coping InformationMichitha BandaraNo ratings yet
- Data-Driven Prognostic Scheme for Bearings Based on a Novel Health Indicator and Gated Recurrent Unit NetworkDocument11 pagesData-Driven Prognostic Scheme for Bearings Based on a Novel Health Indicator and Gated Recurrent Unit Networkex wNo ratings yet
- Reba Scopus 2Document11 pagesReba Scopus 2Silvana MohamadNo ratings yet
- Robotic-Weeding-LitReview-White Paper Pandey Dakshinamurthy Young 2020Document26 pagesRobotic-Weeding-LitReview-White Paper Pandey Dakshinamurthy Young 2020trephenaNo ratings yet
- Automatic Radiology Report Generation Based On Multi-View Image Fusion and Medical Concept EnrichmentDocument9 pagesAutomatic Radiology Report Generation Based On Multi-View Image Fusion and Medical Concept Enrichmentsebampitako duncanNo ratings yet
- Radiometric Indices-Based Spectro-Spatial Approach For Hyperspectral Image ClassificationDocument15 pagesRadiometric Indices-Based Spectro-Spatial Approach For Hyperspectral Image Classificationyaakoub boualleg100% (1)
- A Literature Review of Performance Metrics of Automated Driving Systems For On-Road VehiclesDocument19 pagesA Literature Review of Performance Metrics of Automated Driving Systems For On-Road VehiclesWang JiaweiNo ratings yet
- Computers & Geosciences: Bakhtiar Feizizadeh, Majid Shadman Roodposhti, Piotr Jankowski, Thomas BlaschkeDocument14 pagesComputers & Geosciences: Bakhtiar Feizizadeh, Majid Shadman Roodposhti, Piotr Jankowski, Thomas BlaschkeMuhammad Shaifullah SasmonoNo ratings yet
- 16303264Document36 pages16303264Harley Alejo MNo ratings yet
- PACS-Based Multimedia Imaging Informatics: Basic Principles and ApplicationsFrom EverandPACS-Based Multimedia Imaging Informatics: Basic Principles and ApplicationsNo ratings yet
- صيانة الاجهزة الطبيةDocument9 pagesصيانة الاجهزة الطبيةSayed BadawyNo ratings yet
- CTStudy QuestionsDocument2 pagesCTStudy Questionsjaijai magbanuaNo ratings yet
- Radiography Image Production and EvaluationDocument57 pagesRadiography Image Production and EvaluationDally Rodriguez GammadNo ratings yet
- Selenia Dimensions-3Dimensions v1.8 or Greater Quality Control Manual (MAN-03706) English Rev - 011 11-2021Document242 pagesSelenia Dimensions-3Dimensions v1.8 or Greater Quality Control Manual (MAN-03706) English Rev - 011 11-2021Rafa PopocaNo ratings yet
- Chapter 3 5 Intelligent AgentDocument10 pagesChapter 3 5 Intelligent Agentnick788No ratings yet
- ML 2022 Sheet 01Document2 pagesML 2022 Sheet 01dummyNo ratings yet
- Medical Application of Doppler TechniqueDocument7 pagesMedical Application of Doppler TechniqueCharlotte LambardiNo ratings yet
- MAM VENUS+ USER MANUAL (1)Document28 pagesMAM VENUS+ USER MANUAL (1)redutmedicaNo ratings yet
- Chapter 09Document66 pagesChapter 09moeNo ratings yet
- NCS Rapport "Diagnostische Referentieniveaus in Nederland"Document56 pagesNCS Rapport "Diagnostische Referentieniveaus in Nederland"drn3389100% (1)
- Mammography QA Solutions: Confidential - Subject To Distributor Confidentiality AgreementDocument31 pagesMammography QA Solutions: Confidential - Subject To Distributor Confidentiality AgreementMohamed Abd ElazizNo ratings yet
- Google DeepMind Health - Independent Reviewers Report 2018Document28 pagesGoogle DeepMind Health - Independent Reviewers Report 2018Gina SmithNo ratings yet
- Case Study MastectomyDocument26 pagesCase Study MastectomyIcheAnne Nilay100% (2)
- Literature Review On Awareness of Breast CancerDocument7 pagesLiterature Review On Awareness of Breast Cancerea8dfysf100% (1)
- Mamo GramDocument1 pageMamo GramtaniamarqueslawNo ratings yet
- Digital Mammogram (2020)Document11 pagesDigital Mammogram (2020)anjalineNo ratings yet
- MinorDocument14 pagesMinorWhatsoever BlogsNo ratings yet
- Data Sheet 2Document3 pagesData Sheet 2survery analysisNo ratings yet
- All Products BrochureDocument14 pagesAll Products BrochureholysaatanNo ratings yet
- Hologic Dimensions 3DDocument12 pagesHologic Dimensions 3DfarmaciaNo ratings yet
- Ductal Carcinoma Case StudyDocument72 pagesDuctal Carcinoma Case StudyRayjundie EstradaNo ratings yet
- Try HeartDocument8 pagesTry HeartManiNo ratings yet
- ACOG Revises Breast Cancer Screening Guidance - Ob-Gyns Promote Shared Decision Making - ACOGDocument7 pagesACOG Revises Breast Cancer Screening Guidance - Ob-Gyns Promote Shared Decision Making - ACOGLaura RojasNo ratings yet
- Overview: The Health Communication Process: in This SectionDocument17 pagesOverview: The Health Communication Process: in This SectionMoh AdibNo ratings yet
- Usa Today 2910Document24 pagesUsa Today 2910Balu BalasubramanianNo ratings yet
- Brosur Melody III Anlg - DGTLDocument4 pagesBrosur Melody III Anlg - DGTLAgus AminNo ratings yet
- Breast SurgeryDocument14 pagesBreast SurgeryUday Prabhu100% (1)