Professional Documents
Culture Documents
JCLI BASIL Editorial Revision 2
JCLI BASIL Editorial Revision 2
Uploaded by
Noor Hafizah HassanCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
JCLI BASIL Editorial Revision 2
JCLI BASIL Editorial Revision 2
Uploaded by
Noor Hafizah HassanCopyright:
Available Formats
Editorial
Following BEST-CLI and BASIL-2,
Do We Better Understand How to
“Best” Serve Critical Limb Threatening
Ischemia Patients?
Jos C. van den Berg, MD, PhD1; Barry T. Katzen, MD2; Walter Dorigo, MD3; Andrew Holden, MD4;
Daniella Kadian-Dodov, MD5; Robert Lookstein, MD6; Jihad A. Mustapha, MD7;
John H. Rundback, MD8; Thomas Zeller, MD9
*On behalf of the Critical Limb Ischemia Global Society Board of Directors
J CRIT LIMB ISCHEM 2023 June, Epub Ahead of Issue
Key words: amputation, chronic limb threatening ischemia (CLTI), critical limb ischemia (CLI), endovascular, peripheral arterial
disease (PAD), BASIL-2, BEST CLI
Chronic limb-threatening ischemia (CLTI) is the most severe What are the primary endpoint outcomes?
manifestation of peripheral arterial disease (PAD) including In BASIL-2, after a minimum follow-up of 2 years, the pri-
ischemic pain, ulcerations, and/or gangrene representing a mary outcome (major amputation or death) occurred in 63% of
major medical and socioeconomic burden on health and social the bypass group and 53% of the best endovascular group, with
care services worldwide.1 Recently, 2 randomized controlled an adjusted hazard ratio of 1.35 (95% confidence interval CI
landmark trials (RCT), the BEST-CLI (Best Endovascular versus 1.02-1.80, P=.037), in favor of best endovascular treatment. The
Best Surgical Therapy in Patients with CLTI)2 and BASIL-2 (By- mortality difference continues throughout the trial rather than
pass versus Angioplasty for Severe Ischemia of the Leg)3 studies, only during the peri-operative period, whereas there was no
were published investigating patient and limb-related outcomes difference in amputation rates.
of participants with CLTI who underwent endovascular versus In BEST-CLI, in cohort 1 at a median 2.7 years of follow-up, a
open-surgical treatment. In the BEST-CLI study uniquely, pa- primary outcome event (major adverse limb event or all-cause
tients were divided into 2 cohorts, those with a single segment mortality) occurred in 42.6% in the bypass group and in 57.4%
of adequate greater saphenous vein for bypass (cohort 1), and in the endovascular group, hazard ratio 0.68 (95% CI .59-.79;
those without (cohort 2). Randomization included stratification P<.001). There were significantly more re-interventions in the
by clinical presentation (Rutherford-Becker category 4 vs 5/6) endovascular group, and a significantly reduced rate of major
and the presence vs absence of significant tibial disease. BASIL-2 amputations with bypass surgery. In cohort 2, a primary outcome
compared the clinical effectiveness of a “vein bypass first” or a event occurred in 42.8% in the surgical group and in 47.7% in the
“best endovascular treatment first” strategy for revascularization endovascular group, hazard ratio 0.79 (95% CI .58-1.06; P=.12)
of severe ischemia due to infrapopliteal arterial disease. Correc- after a median follow-up of 1.6 years. Adverse event rates were
tion of additional proximal inflow disease was allowed prior to similar in both cohorts.
infrapopliteal revascularization.
Since there was a striking paucity of high-level comparative What are similarities between BASIL-2 and BEST-CLI?
effectiveness evidence on the optimal treatment of patients with Both are prospective randomized controlled studies com-
CLTI so far, both these landmark trials were awaited with great paring the safety and effectiveness of bypass surgery with use
interest. However, study outcomes are conflicting and therefore of an optimal vein and “best” endovascular therapy in patients
worthy of intensive review and in-depth analysis for all medical suffering from critical limb threatening ischemia (CLTI) using
professions confronted with such patients. a pragmatic approach leaving in particular the decision of best
Vol. 3 · no. 3 June 2023 E1
Treatment Lessons From BEST-CLI and BASIL-2 VAN DEN BERG, et al.
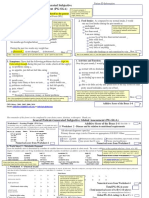
Table 1. Comparison of key study characteristics comparing BEST-CLI and BASIL-2.
BEST-CLI cohort 2 BEST-CLI cohort 2 BASIL-2
Primary endpoints • Composite of major adverse limb events or • Idem • Amputation-free survival (time to above
death from any cause the ankle) amputation of the trial leg or
death from any cause
Main secondary endpoints • Occurrence of a major adverse limb event at • Idem • Time to death from any cause
any time or postoperative death within 30 days (overall survival)
• Minor reinterventions • Time to major amputation of
• Major adverse cardiovascular event (MACE)* the trial leg
• Serious adverse events • Time to first major adverse limb
event (MALE)**
• Time to first major adverse cardiac
event (MACE)***
Main inclusion criteria • CLTI, which was defined as arterial insufficiency • Idem •CLTI due to atherosclerotic disease and
of the lower limb with ischemic foot pain at rest, • Need for an who required an infra-popliteal, with or
a nonhealing ischemic ulcer, or gangrene, as alternative bypass without an additional more proximal
corroborated by hemodynamic criteria conduit infra-inguinal revascularization procedure
• Life expectancy 2 years •Life expectancy > 6 months
• An investigator with expertise in surgical •Judged by two consultants (one of whom
bypass procedures had to agree with another could undertake infra-popliteal vein
investigator with expertise in endovascular re- bypass and one of whom could undertake
vascularization procedures that clinical equipoise infra-popliteal endovascular interventions)
existed in the randomization of each patient to require and be suitable for both
• Availability of autogenous bypass (single seg- infra-popliteal vein bypass and infra-
ment of great saphenous vein) popliteal endovascular intervention
•Adequate aortoiliac inflow to support both
revascularization strategies
Main exclusion criteria •Excessive risk associated with open vascular • Idem • Previous vascular intervention to the
surgery according to the criteria of the American target infra-popliteal artery within the
Heart Association and the American College of previous 12 months
Cardiology or according to the medical judgment • Ischemic pain or tissue loss considered
of the investigator not to be primarily due to atherosclerotic
peripheral artery disease
Number of study sites 150 41
Average number of patients 12.2 8.4
per site entire study
Intended sample size 1620 participants 480 participants 600 participants
Final sample size 1434 participants 396 participants 345 participants
Power calculation 85% 80% 90% reduced to 80%
Enrollment period 08/2014 – 10/2019 Idem 07/2014 – 11/ 2020
* In BEST CLI, MACE was defined as a composite of myocardial infarction, stroke, or death from any cause.
** MALE = major adverse limb events.
***MACE = major adverse coronary events defined as a composite of myocardial infarction, stroke, or death from any cause.
endovascular therapy to the discretion of the operator. The second BEST-CLI defined the composite endpoint as death of any cause and
similarity is that both studies were terminated early due to slow major adverse limb event defined as above ankle amputation of the
enrollment and termination of funding. index limb or a major index-limb re-intervention (new bypass,
interposition graft revision, thrombectomy, or thrombolysis). An
What are the differences between the two studies? endovascular procedure such as balloon angioplasty or stenting
Major differences exist regarding patient and interventional was not considered to be a major re-intervention, a procedure
characteristics as summarized in Table 1, Table 2, and Table 3: that is, in most institutions, standard of care for salvaging, eg,
a stenotic bypass-graft anastomosis (Table 1).
Study endpoints. BASIL-2 used a harder, more investigator
independent endpoint of amputation-free survival defined as time to Patient population. Patient enrollment was stopped in both
major (above the ankle) amputation or death of any cause whereas studies before reaching the per-defined sample size, with BEST-
E2 Journal of Critical Limb Ischemia
Treatment Lessons From BEST-CLI and BASIL-2 VAN DEN BERG, et al.
Table 2. Comparison of key patient characteristics comparing BEST-CLI and BASIL-2.
BEST-CLI cohort 1 BEST-CLI cohort 2 BASIL-2
Patients who did not undergo 4.3% / 1.1% 3.6% / 2.0% 8.7% / 1.2%
any procedure
Cross-over to other revascular- 3.5% / 0.4% 1.0% / 2.0% 7% / 3.5%
ization method
Median age (years) 66.9 / 67.0 68.4 / 68.8 72.4 / 72.5
Male 72% / 71.1% 71.6% / 72.4% 81% / 82%
Diabetes mellitus 72.1% / 71.6% 62.2% / 58.3% 68% / 69%
Mean eGFR (ml/min) NA NA 66.5 / 67.6
Chronic hemodialysis 9.4% / 11.8% 12.8% / 10.1% 6% / 3%
Previous stroke 12.8% / 13.9% 19.4% / 12.1% 15% / 20%
Coronary artery disease 42.3% / 44.4% 49.5% / 53.8% NA
Previous MI NA NA 24% / 13%
Previous PCI & CABG NA NA 26% / 19%
Previous intervention study leg 5.6% / 5.2% 10.3% / 10.1% 31% / 39%
RBC 4 20.3%/20% 29.4%/30.2% 13% / 11%
RBC 5 (and 6) 79.7%/80% 70.6%/69.8% 87% / 89% (RBC 5 only)
ASA class 3 or 4 80.8%/75.9% 83.5%/80.9% NA
No. patients completing the trial 560/1434 (39%) 226/396 (57.1%) 212/345 (61.4%)
Screen failures unknown unknown unknown
CABG = coronary artery bypass graft surgery; eGFR = estimated glomerular filtration rate; MI = myocardial infarction; NA = not availabler;
PCI = percutaneous coronary intervention; RBC = Rutherford-Becker classification.
For all columns, where 2 data elements are listed, the first figure refers to ‘open” and the second to ‘endo’ (open/endo)
CLI being the much bigger study (cohort 1: 1434 of intended 1620 by the authors of the BASIL-2 publication, “clinical experience
patients, cohort 2: 396/480 patients enrolled in 150 study sites) suggests that few patients with chronic limb-threatening ischemia
compared to BASIL-2 (345/600 patients enrolled in 41 study sites). are deemed suitable and have an optimal vein for infrapopliteal
Patients enrolled in BASIL-2 were older (median age 72.5 years vs bypass.” Moreover, a further limitation of generalizability of the
67 and 68.5 years in cohort 1 and 2, respectively), had undergone study results is the low acceptance of patients for randomiza-
more previous interventions of the target limb, and seemed to tion between an open surgical procedure and an endovascular
have more frequent cardiac concomitant diseases. Of note, the intervention. The key question is which data apply more to a
requested life expectancy had to be at least (only) 6 months in daily practice patient population.
BASIL-2 (not further defined) as compared to 2 years in BEST-CLI First, data from BEST-CLI cohort 2 suggest equivalent efficacy
(due to reasons other than PAD only) (Table 2). of clinical outcomes between bypass surgery in patients without
a suitable single great saphenous vein and endovascular therapy.
Study procedure. In BASIL-2, all distal bypass anastomoses More difficult to understand is the different outcome between
were either tibial or pedal, whereas in BEST-CLI, 40% of the grafts cohort 1 in the BEST-CLI trial and the BASIL-2 study population.
were anastomosed onto the popliteal artery. Similarly, in BASIL-2 The better outcome of the endovascular cohort in BASIL-2 is
besides inflow lesion treatment all endovascular procedures did driven by a significant lower mortality rate throughout the
include at least one below-the-knee target vessel, whereas tibial entire follow-up period whereas in BEST-CLI the benefit of vein
artery intervention was performed in BEST-CLI in 53.2% of cases bypass surgery was a reduced major re-intervention and major
only, in the remaining cases the femoral-popliteal artery was the amputation rate. Interestingly, despite these higher major event
single target (Table 3). rates in the endovascular cohort, patient satisfaction was similar
in both study cohorts regarding quality of life measures. It is
What are the consequences of these landmark studies? unclear how much the exclusion of patients with “excessive risk
Both studies included a highly selected patient cohort. As stated associated with open vascular surgery” may have contributed to
Vol. 3 · no. 3 June 2023 E3
Treatment Lessons From BEST-CLI and BASIL-2 VAN DEN BERG, et al.
Table 3. Comparison of key outcome characteristics comparing BEST-CLI and BASIL-2.
BEST-CLI Cohort 1 BEST-CLI Cohort 2 BASIL-2
Bypass location
Femoro-popliteal 40% 47.9% 1%
Femoro-popliteal AK NA NA 0%
Femoro-popliteal BK NA NA 1%
Femoro-BTK 35.7% 37.4% 59%
Popliteal-BTK 15.7% 8.4% 40%
Endovascular techniques
Balloon angioplasty 52.7% 47.2% 60%
Atherectomy 13.6% 15.4% 0%
Drug-coated balloon 27.8% 25.1% 0%
Bare-metal stent 39.3% 43.1% 10%
Drug-eluting stent 24.2% 21.5% 0%
Stent graft 8.6% 12.8% 0%
Technical success 98.3% / 84.7% 100%/80.6% 96% / 80%
All cause death 33% / 37.6% 25.9% / 24.1% 53% / 45%
Major amputation (above ankle) 10.4%/14.9% 15.2%/14.1% 20%/18%
AK amputation NA NA NA
BK amputation NA NA NA
Amputation free survival 43.3%/52.4% 41.1%/38.2% 37%/47%
Cross-over intervention during NA NA 27% / 19%
FU
Reintervention**** 9.2% / 33.1% 14.2%/25.6% 5% / 19%
AK = above knee; BK = below knee; BTK = below the knee; FU = follow-up; NA = not available
**** reintervention: ‘major’ for BEST-CLI, ‘not-specified’ for BASIL 2
the similar mortality rates seen in the open and endovascular (Table 3) that technical success rates were in a similar range.
arms in both cohorts in the BEST-CLI trial. Considering death as Opposite to BEST-CLI, re-intervention rates in BASIL-2 do
the most serious possible event one could argue, BASIL-2 being not differ between both revascularization strategies. A reason
the more relevant study favoring the endovascular first strat- for this may be a higher redo rate for tibial bypass surgery as
egy. However, are both study populations comparable besides compared to a distal popliteal artery anastomosis. Whereas
presenting with CLTI? BASIL-2 enrolled exclusively lesion anatomies requiring tibial
It seems as if the BASIL-2 study population represents a higher bypass anastomoses, only 60% of the venous bypass in BEST-CLI
risk patient population as compared to BEST-CLI as demonstrated had a tibial bypass anastomosis. It would be interesting to see
by the highest all-cause death rate of the 3 cohorts (open vs. endo upcoming sub-cohort analyses of BEST-CLI regarding major
BASIL-2: 53% / 45%, BEST-CLI cohort 1: 33% / 37.6% and cohort 2: re-intervention rates comparing popliteal and tibial distal bypass
25.9% / 24.1%). Reasons for this high mortality rate may be that targets. Another factor that may have influenced the differences
BASIL-2 patients are older, they seem to have a higher prevalence in outcomes is the fact that BEST-CLI included patients with RBC
of clinically relevant coronary heart disease, and, in particular, 4-6 (Rutherford-Becker classification), while RBC 6 patients were
they have a more distally located disease anatomy. not included in BASIL-2.
Although there were differences in specialty performing the What has become clear from both studies is that medical
endovascular techniques (in BEST-CLI, 73% of the endo-proce- therapy is sub-optimal in the majority of patients, and therefore
dures were performed by vascular surgeons, while in BASIL-2 it is necessary to strive for reduction of excess cardiovascular
84% were performed by interventional radiologists) it can be seen mortality by performing a proper cardiovascular diagnostic
E4 Journal of Critical Limb Ischemia
Treatment Lessons From BEST-CLI and BASIL-2 VAN DEN BERG, et al.
work-up and optimization of secondary prevention (by estab- References
lishing optimal medical therapy). 1. Conte MS, Bradbury AW, Kolh P, et al. Global vascular guidelines on the management
It has to be kept in mind that the results of both these studies of chronic limb-threatening ischemia. Eur J Vasc Endovasc Surg 2019;58(1S):S1-S109
are only valid when the technical success rates in an institution e33. Epub 2019 Jun 8. doi: 10.1016/j.ejvs.2019.05.006
are comparable to those achieved in BEST-CLI and BASIL-2. This is 2. Farber A, Menard MT, Conte MS, et al. Surgery or endovascular therapy for chronic
especially true for (distal) bypass surgery, and therefore internal limb-threatening ischemia. N Engl J Med 2022;387(25):2305-2316. Epub 2022 Nov
auditing/credentialing should be considered when applying the 7. doi: 10.1056/NEJMoa2207899
results in a local practice (cf, carotid endarterectomy, and stenting). 3. Bradbury AW, Moakes CA, Popplewell M, et al. A vein bypass first versus a best
endovascular treatment first revascularisation strategy for patients with chronic
Conclusion limb threatening ischaemia who required an infra-popliteal, with or without an
additional more proximal infra-inguinal revascularisation procedure to restore
limb perfusion (BASIL-2): an open-label, randomised, multicentre, phase 3 trial.
The bottom line is, if a patient is suitable for both revascular- Lancet 2023;401(10390):1798-1809. Epub 2023 Apr 25. doi: 10.1016/S0140-
ization strategies, technical revascularization success is higher 6736(23)00462-2
with bypass surgery independent of the bypass material. Besides
this, on mid-term, patients seem to benefit from both treatment
strategies. Open surgery and endovascular intervention should From the 1Ospedale Regionale di Lugano, Lugano, Switzerland; 2Miami Cardiac & Vascular
Institute, Miami, Florida; 3University of Florence, Firenze, Italy; 4Auckland City Hospital,
be considered as complementary treatment options. The treat- Auckland, New Zealand; 5Icahn School of Medicine at Mount Sinai, New York, New York;
ment offered to an individual patient should be tailored to the 6
Mount Sinai Health System, New York, New York; 7ACV Centers, Grand Rapids, Michigan;
8
NJ Endovascular & Amputation Prevention, Teaneck, New Jersey; 9Universitaets Herzz-
patient’s needs and the available operator expertise in a given entrum, Bad Krozingen, Germany.
vascular center.
Disclosure: The authors have completed and returned the ICMJE Form for Disclosure
Both BEST-CLI and BASIL-2 have generated a wealth of data of Potential Conflicts of Interest. The authors report no conflicts of interest regarding
the content herein.
that can already be implemented in choosing the optimal treat-
ment modalities for patients with CLTI. The planned individual Manuscript accepted June 6, 2023.
patient data driven pooled analysis of both studies (both trial Address for correspondence: Thomas Zeller, MD, Universitaets Herzzentrum, Bad Krozingen,
investigators entered into a data sharing agreement), will provide Germany. Email: thomas.zeller@uniklinik-freiburg.de
probably a more granular view that will allow further fine-tuning.
Vol. 3 · no. 3 June 2023 E5
You might also like
- Retained PlacentaDocument56 pagesRetained PlacentaElisha Joshi100% (9)
- FCPS Part 1 Medicine and Allied Paper 1 and 2Document52 pagesFCPS Part 1 Medicine and Allied Paper 1 and 2drhirasalmanNo ratings yet
- Best CliDocument32 pagesBest ClivsurgeonkamranNo ratings yet
- Nej M Abbotts TentDocument11 pagesNej M Abbotts TentWKYC.comNo ratings yet
- Leriche Fontaine Classification PDFDocument8 pagesLeriche Fontaine Classification PDFCute Clothing StoreNo ratings yet
- Chronic Limb Threatening IschemiaDocument35 pagesChronic Limb Threatening Ischemiasifatullah khanNo ratings yet
- Biomedicines 11 00979Document10 pagesBiomedicines 11 00979akinaNo ratings yet
- WoundCare PDFDocument43 pagesWoundCare PDFMahi AekNo ratings yet
- Articol ExempluDocument12 pagesArticol ExempluVlad NeagoeNo ratings yet
- 56 Anaesthesia For Carotid Endarterectomy PDFDocument10 pages56 Anaesthesia For Carotid Endarterectomy PDFHarish BhatNo ratings yet
- Spinal Cord Injury PDFDocument14 pagesSpinal Cord Injury PDFNiaNo ratings yet
- Fusion Rates and SF-36 Outcomes After Multilevel Laminectomy and Noninstrumented Lumbar Fusions in A Predominantly Geriatric PopulationDocument6 pagesFusion Rates and SF-36 Outcomes After Multilevel Laminectomy and Noninstrumented Lumbar Fusions in A Predominantly Geriatric PopulationMaria Daniela Jiménez AguilarNo ratings yet
- Acute MonoarthritisDocument7 pagesAcute MonoarthritiskafosidNo ratings yet
- Early Predictors of Mortality in HemodynamicallyDocument7 pagesEarly Predictors of Mortality in HemodynamicallytesfahuntekletilahunNo ratings yet
- Advances in Acute Stroke Treatment 2020Document6 pagesAdvances in Acute Stroke Treatment 2020ayman shomanNo ratings yet
- Extracorporeal Life Support in Pediatric Cardiac DysfunctionDocument5 pagesExtracorporeal Life Support in Pediatric Cardiac DysfunctionNoor Aida AriyaniNo ratings yet
- The EXCEL and NOBLE Trials - Similarities, Contrasts and Future Perspectives For Left Main RevascularisationDocument8 pagesThe EXCEL and NOBLE Trials - Similarities, Contrasts and Future Perspectives For Left Main RevascularisationRui FonteNo ratings yet
- Left Ventricular Volume Reduction: HistoryDocument6 pagesLeft Ventricular Volume Reduction: HistoryPeter Paul PascualNo ratings yet
- BasilDocument10 pagesBasilDavid FlynnNo ratings yet
- Intra AortaDocument5 pagesIntra AortaPamungkasHandyMulyawanNo ratings yet
- Ahn-Park 1.prevent Acc2024f6Document45 pagesAhn-Park 1.prevent Acc2024f6Lau Waye YoungNo ratings yet
- Multiple TraumaDocument27 pagesMultiple Traumaasya100% (1)
- Preventable Death: Dco: DR Thit Lwin School of Medicine UMSDocument56 pagesPreventable Death: Dco: DR Thit Lwin School of Medicine UMSStar CruiseNo ratings yet
- Glomus EmbolizacionDocument13 pagesGlomus EmbolizacionJuan TijerinaNo ratings yet
- Lower Extremity Arterial Injuries Over A Six-Year Period: Outcomes, Risk Factors, and ManagementDocument9 pagesLower Extremity Arterial Injuries Over A Six-Year Period: Outcomes, Risk Factors, and ManagementrizcoolNo ratings yet
- Approach To Polytrauma and Damage Control OrthopedicsDocument63 pagesApproach To Polytrauma and Damage Control OrthopedicsSubarna PaudelNo ratings yet
- Complications Predicting Perioperative Mortality in Patients Undergoing Elective Craniotomy A Population Based StudyDocument11 pagesComplications Predicting Perioperative Mortality in Patients Undergoing Elective Craniotomy A Population Based Study49hr84j7spNo ratings yet
- 2021 - Damage Control Orthopaedics in Spinal TraumaDocument12 pages2021 - Damage Control Orthopaedics in Spinal TraumaJimena BetancurNo ratings yet
- Manual Aspiration Thrombectomy in Acute Myocardial Infarction: A Clinical ExperienceDocument9 pagesManual Aspiration Thrombectomy in Acute Myocardial Infarction: A Clinical ExperienceArdiana FirdausNo ratings yet
- How To Clear Polytrauma Patients For Fracture FixationDocument26 pagesHow To Clear Polytrauma Patients For Fracture FixationTiago FeitosaNo ratings yet
- Prevalence of Anatomical Variations of Circle of Willis in South Indian Population Succumbing To Isolated Traumatic Brain Injury - A Cadaveric StudyDocument6 pagesPrevalence of Anatomical Variations of Circle of Willis in South Indian Population Succumbing To Isolated Traumatic Brain Injury - A Cadaveric StudyIJAR JOURNALNo ratings yet
- Lower Limb Replantations Indications Anda New Scoring SystemDocument6 pagesLower Limb Replantations Indications Anda New Scoring SystemcubirojasNo ratings yet
- Siriwardena Et Al 2015 Complications of Intra Aortic Balloon Pump Use Does The Final Position of The Iabp Tip MatterDocument8 pagesSiriwardena Et Al 2015 Complications of Intra Aortic Balloon Pump Use Does The Final Position of The Iabp Tip MatterYEZINo ratings yet
- Journal of Cardiac Surgery - 2019 - Hamiko - Timely Extracorporeal Membrane Oxygenation Assist Reduces Mortality AfterDocument13 pagesJournal of Cardiac Surgery - 2019 - Hamiko - Timely Extracorporeal Membrane Oxygenation Assist Reduces Mortality Afterjairo enrique de la peña lopezNo ratings yet
- Jurding BTKV AliDocument31 pagesJurding BTKV AliGani ArlondNo ratings yet
- Journal Reading Decompressive Craniectomy For EDHDocument10 pagesJournal Reading Decompressive Craniectomy For EDHmasyfuqNo ratings yet
- Results of One-Hundred and Seventy Patients After Elective Bentall OperationDocument8 pagesResults of One-Hundred and Seventy Patients After Elective Bentall OperationkodagaNo ratings yet
- Arterial Trauma During Central Venous Catheter Insertion: Case Series, Review and Proposed AlgorithmDocument8 pagesArterial Trauma During Central Venous Catheter Insertion: Case Series, Review and Proposed AlgorithmJuan Jose Velasquez GutierrezNo ratings yet
- Abdominal Trauma From Nursing Perspective: JunaediDocument50 pagesAbdominal Trauma From Nursing Perspective: JunaediDana KhoirulNo ratings yet
- 33 Spinal Cord InjuryDocument17 pages33 Spinal Cord InjuryMiguel SanJuanNo ratings yet
- Post Reteplase Evaluation PDFDocument5 pagesPost Reteplase Evaluation PDFAnonymous ysrxggk21cNo ratings yet
- Prevenção de IraDocument21 pagesPrevenção de IrajoseNo ratings yet
- PainDocument9 pagesPainwijaya ajaaNo ratings yet
- Jcen 22 2 78Document7 pagesJcen 22 2 78Aik NoeraNo ratings yet
- Safety and Ef Ficacy of An Endovascular-First Approach To Acute Limb IschemiaDocument9 pagesSafety and Ef Ficacy of An Endovascular-First Approach To Acute Limb IschemiaSisca Dwi AgustinaNo ratings yet
- E000836 FullDocument7 pagesE000836 Fullalejandro montesNo ratings yet
- Ehv 217Document8 pagesEhv 217Said Qadaru ANo ratings yet
- 1 Bridging Anticoag Primum Non NocereDocument12 pages1 Bridging Anticoag Primum Non NocereSpencerNo ratings yet
- 2015 Manejo Postquirurgico Del Paciente Con Cirugia Cardiaca Parte IIDocument20 pages2015 Manejo Postquirurgico Del Paciente Con Cirugia Cardiaca Parte IIAdiel OjedaNo ratings yet
- s12872 019 1096 1Document9 pagess12872 019 1096 1sarahNo ratings yet
- Principles of Damage Control For Pelvic Ring Injuries: P.V. Giannoudis and Hans-Christoph PapeDocument14 pagesPrinciples of Damage Control For Pelvic Ring Injuries: P.V. Giannoudis and Hans-Christoph PapewhiezardNo ratings yet
- Do Cardiac Risk Stratification Indexes Accurately Estimate Perioperative Risk in Noncardiac Surgery PatientsDocument5 pagesDo Cardiac Risk Stratification Indexes Accurately Estimate Perioperative Risk in Noncardiac Surgery Patientstsiko111No ratings yet
- Evidence-Based Perioperative Medicine (EBPOM) : A Summary of The 8th EBPOM Conference 2009Document6 pagesEvidence-Based Perioperative Medicine (EBPOM) : A Summary of The 8th EBPOM Conference 2009ashut1No ratings yet
- Lower Extremity AmputationDocument41 pagesLower Extremity AmputationvsurgeonkamranNo ratings yet
- Pape2005 PDFDocument12 pagesPape2005 PDFantonio dengNo ratings yet
- Alar Hay em 2018Document5 pagesAlar Hay em 2018Amelia Kristin SimanjuntakNo ratings yet
- Identifying Severe StrokeDocument8 pagesIdentifying Severe StrokekunneiNo ratings yet
- Analysis of Risk Factors Affecting Mortality in Elderly Patients Operated On For Hip FracturesDocument6 pagesAnalysis of Risk Factors Affecting Mortality in Elderly Patients Operated On For Hip FracturesloliNo ratings yet
- Anesthesia and Surgical Microvascular FlapsDocument17 pagesAnesthesia and Surgical Microvascular FlapsLuis KarlNo ratings yet
- Ivs 459Document3 pagesIvs 459melon segerNo ratings yet
- Microcirculation in Cardiovascular DiseasesFrom EverandMicrocirculation in Cardiovascular DiseasesEnrico Agabiti-RoseiNo ratings yet
- Computed-Tomography a Powerful Tool for Diagnosis of Pediatric and Adult Congenital Heart Disease: Methodology and Interpretation GuideFrom EverandComputed-Tomography a Powerful Tool for Diagnosis of Pediatric and Adult Congenital Heart Disease: Methodology and Interpretation GuideNo ratings yet
- Progress in Systemic Lupus 2007 Nova Medical BooksDocument278 pagesProgress in Systemic Lupus 2007 Nova Medical BooksOana CristeaNo ratings yet
- Suzhou Vocaional University Courses NAVTTC OnlineDocument10 pagesSuzhou Vocaional University Courses NAVTTC Onlineshafiq rehmanNo ratings yet
- CaffeineDocument3 pagesCaffeineJamah Al-qosadiNo ratings yet
- When, Why and Where in Oral and Maxillofacial Surgery.Document205 pagesWhen, Why and Where in Oral and Maxillofacial Surgery.LAIBA WAHABNo ratings yet
- Of Antimicrobial Resistance: The Who Aware (Access, Watch, Reserve) Antibiotic Book and PreventionDocument7 pagesOf Antimicrobial Resistance: The Who Aware (Access, Watch, Reserve) Antibiotic Book and PreventionBBD BBDNo ratings yet
- Drug StudyDocument8 pagesDrug StudyTheresa Reyes De JesusNo ratings yet
- Form Pg-Sga PDFDocument2 pagesForm Pg-Sga PDFzain syalsabilaNo ratings yet
- PRC LeahDocument8 pagesPRC LeahInes Hamoy JunioNo ratings yet
- Acute Respiratory Distress Syndrome Nursing Management and Interventions - NurseslabsDocument2 pagesAcute Respiratory Distress Syndrome Nursing Management and Interventions - NurseslabsSachin SinghNo ratings yet
- Order of Blood DrawDocument3 pagesOrder of Blood DrawindahNo ratings yet
- Physical Examination of The PatientDocument9 pagesPhysical Examination of The PatientzbrojkoNo ratings yet
- 1.5 Historical Background of Fehintoluwa Clinic and MaternityDocument6 pages1.5 Historical Background of Fehintoluwa Clinic and Maternitygolden abidemNo ratings yet
- Types of PE StudiesDocument44 pagesTypes of PE StudiesVincentNgKuangCheanNo ratings yet
- Assignmemt 4: What Is Hospital Waste ?Document6 pagesAssignmemt 4: What Is Hospital Waste ?அபினேஷ்குமார்No ratings yet
- Systemic Light Chain Amyloidosis: NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines)Document26 pagesSystemic Light Chain Amyloidosis: NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines)Adina StemateNo ratings yet
- Psychotropic Drugs: By: Rheajane Aguilar-RosalesDocument77 pagesPsychotropic Drugs: By: Rheajane Aguilar-Rosalesjean samson100% (1)
- Renal Calculi IntroductionDocument4 pagesRenal Calculi IntroductionirysatherfinestNo ratings yet
- Updated How To Deal ACS in Limited Resources Facilities - Danie Syahrir, DR., SP - JPDocument32 pagesUpdated How To Deal ACS in Limited Resources Facilities - Danie Syahrir, DR., SP - JPmaria sintaNo ratings yet
- Lifestyle DiseasesDocument16 pagesLifestyle DiseasesDinesh GawandeNo ratings yet
- Radiation Therapy and Esophageal CancerDocument14 pagesRadiation Therapy and Esophageal Cancerkrsna2studyNo ratings yet
- Pharmaceutical Industry in BangladeshDocument3 pagesPharmaceutical Industry in BangladeshWalidur Rahman MridulNo ratings yet
- HemorrhoidsDocument27 pagesHemorrhoidsNicklaus RiveraNo ratings yet
- Amandaresume 1Document2 pagesAmandaresume 1api-510011907No ratings yet
- BronchiolitisDocument45 pagesBronchiolitisYuusuf MubarikNo ratings yet
- Growth in Cerebral Palsy Children Between 3-13 Years in Urban Dharwad, IndiaDocument7 pagesGrowth in Cerebral Palsy Children Between 3-13 Years in Urban Dharwad, IndiaDr. Krishna N. Sharma100% (1)
- NLOA Prelims RationalizationDocument7 pagesNLOA Prelims RationalizationVincent JadolNo ratings yet
- COVID Requirements For North Carolina SchoolsDocument5 pagesCOVID Requirements For North Carolina SchoolsKeung HuiNo ratings yet
- English Practice AssignmentsDocument3 pagesEnglish Practice AssignmentsNatasya VirginiaNo ratings yet