Professional Documents
Culture Documents
Ds 48 087
Ds 48 087
Uploaded by
Jim HopkinsCopyright:
Available Formats
You might also like
- The Selection of Hyaluronic Acid When Treating With The Nasolabial Fold A Meta-Analysis - Peng, 2021Document9 pagesThe Selection of Hyaluronic Acid When Treating With The Nasolabial Fold A Meta-Analysis - Peng, 2021Rafael Autran Cavalcante AraújoNo ratings yet
- Calcium Hydroxylapatite (Radiesse) For Correction of The Mid-And Lower Face: Consensus RecommendationsDocument12 pagesCalcium Hydroxylapatite (Radiesse) For Correction of The Mid-And Lower Face: Consensus RecommendationsMichele Carvalho100% (1)
- Antiaging Efficacy of A Retinaldehyde-Based Cream Compared With Glycolic Acid Peel Sessions: A Randomized Controlled StudyDocument8 pagesAntiaging Efficacy of A Retinaldehyde-Based Cream Compared With Glycolic Acid Peel Sessions: A Randomized Controlled Studypermen_lollypopzNo ratings yet
- Q3 G11 Physical Science Module 7Document19 pagesQ3 G11 Physical Science Module 7Lebz RicaramNo ratings yet
- An Approach To Structural Facial Rejuvenation With Fillers in WomenDocument15 pagesAn Approach To Structural Facial Rejuvenation With Fillers in WomenJhon RodriguezNo ratings yet
- A Randomized Study of The Efficacy and Safety of Injectable Poly-L-lactic Acid Versus Human-Based Collagen Implant in The Treatment of Nasolabial Fold Wrinkles - Narins, 2010Document15 pagesA Randomized Study of The Efficacy and Safety of Injectable Poly-L-lactic Acid Versus Human-Based Collagen Implant in The Treatment of Nasolabial Fold Wrinkles - Narins, 2010Rafael Autran Cavalcante AraújoNo ratings yet
- Evaluation Long-Term Safety Biodegradability Hyaluronic Acid Dermal Fillers (YVOIRE®) Correction Nasolabial Folds Two Multicenter, Prospective, Observational Cohort Studies - Xie, 2022Document11 pagesEvaluation Long-Term Safety Biodegradability Hyaluronic Acid Dermal Fillers (YVOIRE®) Correction Nasolabial Folds Two Multicenter, Prospective, Observational Cohort Studies - Xie, 2022Rafael Autran Cavalcante AraújoNo ratings yet
- Rinomodelacion - HidroxiapatitaDocument6 pagesRinomodelacion - HidroxiapatitaMauricio Ocampo MazoNo ratings yet
- Efektivitas Dan Keamanan Kojic DipalmitatDocument6 pagesEfektivitas Dan Keamanan Kojic DipalmitatmurjonocrbNo ratings yet
- A Randomized, Evaluator-Blinded, Controlled Study of The Effectiveness and Safety of Small Gel Particle Hyaluronic Acid For Lip Augmentation2021Document13 pagesA Randomized, Evaluator-Blinded, Controlled Study of The Effectiveness and Safety of Small Gel Particle Hyaluronic Acid For Lip Augmentation2021Jhon RodriguezNo ratings yet
- A Series of in Vitro and Human Studies of A Novel Lip Cream FormulationDocument16 pagesA Series of in Vitro and Human Studies of A Novel Lip Cream FormulationDummy CipawNo ratings yet
- Thehyaluronicacid Fillers: Current Understanding of The Tissue Device InterfaceDocument10 pagesThehyaluronicacid Fillers: Current Understanding of The Tissue Device InterfaceLuis Fernando WeffortNo ratings yet
- 2018.degradation HialuronidaseDocument6 pages2018.degradation Hialuronidaseingrid castroNo ratings yet
- 65 DDB 7 CF 79183Document11 pages65 DDB 7 CF 79183marisa araujoNo ratings yet
- A Review of The Metabolism of 1,4-Butanediol Diglycidyl Ether-Crosslinked Hyaluronic Acid Dermal FillersDocument9 pagesA Review of The Metabolism of 1,4-Butanediol Diglycidyl Ether-Crosslinked Hyaluronic Acid Dermal FillersJhon RodriguezNo ratings yet
- Hyaluronic Acid Fillers in Facial Rejuvenation: Mary P. Lupo, MDDocument5 pagesHyaluronic Acid Fillers in Facial Rejuvenation: Mary P. Lupo, MDEduarda De Menezes GerlachNo ratings yet
- Current Concepts in The Use of Small-Particle Hyaluronic AcidDocument7 pagesCurrent Concepts in The Use of Small-Particle Hyaluronic AcidThaís SagratzhiNo ratings yet
- Dermatologic Therapy - 2022 - WongprasertDocument9 pagesDermatologic Therapy - 2022 - Wongprasertdocrubes50No ratings yet
- 2016 Lagatta Rheology ALLIAXINDocument8 pages2016 Lagatta Rheology ALLIAXINANDRÉ CAMARGONo ratings yet
- A Novel at Home Procedure Providing Marked Improvements - 2014 - Journal of The PDFDocument1 pageA Novel at Home Procedure Providing Marked Improvements - 2014 - Journal of The PDFNachi MontianarrtNo ratings yet
- Treatment of Acne Scars With RadiesseDocument3 pagesTreatment of Acne Scars With RadiesseMethawin Chatmethinwat100% (1)
- Jcad 12 9 32Document4 pagesJcad 12 9 32Gerardo Valenzuela GonzálezNo ratings yet
- 001 Lip LiftDocument11 pages001 Lip Liftdr.antonio.velasquezNo ratings yet
- 10 1111@jocd 12861Document8 pages10 1111@jocd 12861Erik BrooksNo ratings yet
- Changes in The Strategies For Caries Management in Older Adults A Non-Invasive AlternativeDocument2 pagesChanges in The Strategies For Caries Management in Older Adults A Non-Invasive AlternativeSeba MirandaNo ratings yet
- Global Periorbital Skin Rejuvenation by A Topical Eye Cream (JOCD-18-530)Document9 pagesGlobal Periorbital Skin Rejuvenation by A Topical Eye Cream (JOCD-18-530)FuckyaNo ratings yet
- Clinical and Dermoscopic Evaluation of PeriorbitalDocument6 pagesClinical and Dermoscopic Evaluation of Periorbitalruby.wryNo ratings yet
- Journal of Biomedical Materials Research Part A Volume 87A Issue 1 2008 (Doi 10.1002 - Jbm.a.31675) Samuel J. Falcone Richard A. Berg - Crosslinked Hyaluronic Acid Dermal Fillers - A Comparison of RHDocument8 pagesJournal of Biomedical Materials Research Part A Volume 87A Issue 1 2008 (Doi 10.1002 - Jbm.a.31675) Samuel J. Falcone Richard A. Berg - Crosslinked Hyaluronic Acid Dermal Fillers - A Comparison of RHImanuel CristiantoNo ratings yet
- 10 1097@DSS 0000000000001281Document11 pages10 1097@DSS 0000000000001281plastic guardiansNo ratings yet
- ZO điều trị TSTDocument7 pagesZO điều trị TSTHong Nguyen ThiNo ratings yet
- Evaluation of A Kojic Acid, PDFDocument6 pagesEvaluation of A Kojic Acid, PDFvanitha13No ratings yet
- 10 1097@DSS 0000000000002271Document9 pages10 1097@DSS 0000000000002271Rhelvis1No ratings yet
- Radiesse For Aesthetic Soft Tissue Augmentation PDFDocument7 pagesRadiesse For Aesthetic Soft Tissue Augmentation PDFfishvalNo ratings yet
- عقار 24Document8 pagesعقار 24عمار حسين عبدعلي جاسم biologyNo ratings yet
- Adv Healthcare Materials - 2021 - Herrmann - Hydrogels and Their Role in Biosensing Applications PDFDocument25 pagesAdv Healthcare Materials - 2021 - Herrmann - Hydrogels and Their Role in Biosensing Applications PDFAlejandro Rojas GómezNo ratings yet
- JAMA Facial Plastic Surgery: Novel Use of A Volumizing Hyaluronic Acid Filler For Treatment of Infraorbital HollowsDocument23 pagesJAMA Facial Plastic Surgery: Novel Use of A Volumizing Hyaluronic Acid Filler For Treatment of Infraorbital HollowsDr. Hilder HernandezNo ratings yet
- Choi2015 Sculptra Sulco NasoDocument10 pagesChoi2015 Sculptra Sulco Nasoana clara scopelNo ratings yet
- Analysis of U.S. Food and Drug Administration Data On Filler Complications 2019Document5 pagesAnalysis of U.S. Food and Drug Administration Data On Filler Complications 2019maat1No ratings yet
- Physiochemical Properties and Application of Hyaluronic Acid A SystematicDocument7 pagesPhysiochemical Properties and Application of Hyaluronic Acid A SystematicThaís SagratzhiNo ratings yet
- Clinical Assessment of A Combination Lip TreatmentDocument6 pagesClinical Assessment of A Combination Lip TreatmentDummy CipawNo ratings yet
- Update On The Management of Rosacea From The American Acne & Rosacea SocietyDocument8 pagesUpdate On The Management of Rosacea From The American Acne & Rosacea SocietySong JieunNo ratings yet
- The Efficacy of Colloidal Oatmeal Cream 1 Percent As Addon Therapy in The Management of Chronic Irritant Hand Eczema - A Double-Blind StudyDocument11 pagesThe Efficacy of Colloidal Oatmeal Cream 1 Percent As Addon Therapy in The Management of Chronic Irritant Hand Eczema - A Double-Blind StudyQualityMattersNo ratings yet
- Modif Structure of HADocument6 pagesModif Structure of HAnina asrianaNo ratings yet
- Ghanim Et Al-2019-International Journal of Paediatric DentistryDocument8 pagesGhanim Et Al-2019-International Journal of Paediatric DentistryFamily DentalNo ratings yet
- SCMS Vol31 No2 HyperpigmentationDocument7 pagesSCMS Vol31 No2 HyperpigmentationFachrizal AuliaNo ratings yet
- Beneficial Effects of Hyaluronic Acid: Prasad N. Sudha, Maximas H. RoseDocument40 pagesBeneficial Effects of Hyaluronic Acid: Prasad N. Sudha, Maximas H. RosePaulo Emílio Alves AlvesNo ratings yet
- A 10-Point Plan For Avoiding Hyaluronic Acid Dermal Filler-Related Complications During Facial Aesthetic Procedures and Algorithms For ManagementDocument9 pagesA 10-Point Plan For Avoiding Hyaluronic Acid Dermal Filler-Related Complications During Facial Aesthetic Procedures and Algorithms For Managementleenatalia93100% (1)
- Ccid 13 701Document10 pagesCcid 13 701jess.sooares12No ratings yet
- Soft Tissue Augmentation With Dermal Fillers, Part 1: Lips and Lower FaceDocument6 pagesSoft Tissue Augmentation With Dermal Fillers, Part 1: Lips and Lower FaceMichele CarvalhoNo ratings yet
- J Colsurfb 2018 08 061Document7 pagesJ Colsurfb 2018 08 061Ratih Anindita Rahajeng RipyonoNo ratings yet
- Dermatologic Therapy (2020)Document7 pagesDermatologic Therapy (2020)고은영No ratings yet
- Physical Properties of A Novel SmallDocument8 pagesPhysical Properties of A Novel SmallSheila BerbelzinhaNo ratings yet
- Six Steps To The Perfect LipDocument9 pagesSix Steps To The Perfect LipTatiana Araujo100% (1)
- Ccid 179430 A Series of in Vitro and Human Studies of A Novel Lip Cream 032119Document16 pagesCcid 179430 A Series of in Vitro and Human Studies of A Novel Lip Cream 032119Lina WinartiNo ratings yet
- Hyaluronic Acid: A New Approach For The Treatment of Gingival Recession-A Systematic ReviewDocument11 pagesHyaluronic Acid: A New Approach For The Treatment of Gingival Recession-A Systematic ReviewGali Alfaro ZagalNo ratings yet
- Smith 2007Document10 pagesSmith 2007CARLOS ZUÑIGANo ratings yet
- Comparative Evaluation of Efficacy and Tolerability ofDocument8 pagesComparative Evaluation of Efficacy and Tolerability ofMelanny CindyNo ratings yet
- Fluoride Alternatives My PaperDocument10 pagesFluoride Alternatives My PaperNazim SallamNo ratings yet
- Chemical Peeling With Trichloroacetic Acid and Lactic Acid For Infraorbital Dark CirclesDocument6 pagesChemical Peeling With Trichloroacetic Acid and Lactic Acid For Infraorbital Dark CirclesAna Claudia Kordelos DinizNo ratings yet
- 1 Consenso Carruthers2016Document12 pages1 Consenso Carruthers2016Lorena AcevedoNo ratings yet
- Role of Lipid Excipients in Modifying Oral and Parenteral Drug Delivery: Basic Principles and Biological ExamplesFrom EverandRole of Lipid Excipients in Modifying Oral and Parenteral Drug Delivery: Basic Principles and Biological ExamplesKishor M. WasanNo ratings yet
- Gr11 Mock Exam Schedule 2024Document13 pagesGr11 Mock Exam Schedule 2024potrillo0330No ratings yet
- Cookie Experimental DesignDocument2 pagesCookie Experimental Designapi-293314791No ratings yet
- Marked Fake Deck Tricks3Document7 pagesMarked Fake Deck Tricks3Tito Banerjee100% (1)
- Distribution Channel of AMULDocument13 pagesDistribution Channel of AMULMeet JivaniNo ratings yet
- Detailed Report On Gwadar PortDocument4 pagesDetailed Report On Gwadar PortxeninNo ratings yet
- UN - HIV and Prison - Policy BriefDocument12 pagesUN - HIV and Prison - Policy BriefParomita2013No ratings yet
- Matrices of Violence: A Post-Structural Feminist Rendering of Nawal El Saadawi's Woman at Point Zero and Lola Soneyin's The Secrets of Baba Segi's WivesDocument6 pagesMatrices of Violence: A Post-Structural Feminist Rendering of Nawal El Saadawi's Woman at Point Zero and Lola Soneyin's The Secrets of Baba Segi's WivesIJELS Research JournalNo ratings yet
- Pharmacognosy-Large FontDocument35 pagesPharmacognosy-Large FontArantxa HilarioNo ratings yet
- EDTA CHEMICAL CLEANING (BLR) PDFDocument16 pagesEDTA CHEMICAL CLEANING (BLR) PDFAnudeep Chittluri100% (2)
- Module 6 - Sequential Circuits, Excitation Function, State Table, State DiagramDocument21 pagesModule 6 - Sequential Circuits, Excitation Function, State Table, State DiagramYvanne Esquia CuregNo ratings yet
- XC9572 PDFDocument9 pagesXC9572 PDFAvs ElectronNo ratings yet
- 1000mm BOPP Tape Coating Machine Two Color Printing 40 Speed TangerangDocument6 pages1000mm BOPP Tape Coating Machine Two Color Printing 40 Speed TangerangJaja JamaludinNo ratings yet
- Scala AccesoriesDocument27 pagesScala AccesoriesZiggy BussyNo ratings yet
- BenfordDocument9 pagesBenfordAlex MireniucNo ratings yet
- Santa Cruz Scanner FreqsDocument35 pagesSanta Cruz Scanner FreqsdonsterthemonsterNo ratings yet
- Supervisi Akademik Melalui Pendekatan Kolaboratif Oleh Kepala Sekolah Dalammeningkatkan Kualitas Pembelajarandisd Yari DwikurnaningsihDocument11 pagesSupervisi Akademik Melalui Pendekatan Kolaboratif Oleh Kepala Sekolah Dalammeningkatkan Kualitas Pembelajarandisd Yari DwikurnaningsihKhalid Ibnu SinaNo ratings yet
- Ca-Cw106451-Mat-098 - Manga Termocontraible WoerDocument5 pagesCa-Cw106451-Mat-098 - Manga Termocontraible WoerJhoel Ipanaque AlarconNo ratings yet
- Daily PlatterDocument3 pagesDaily PlatterRajah KanoNo ratings yet
- S9 Safety Labeling For Electrical Equipment and Facilities ManagementDocument74 pagesS9 Safety Labeling For Electrical Equipment and Facilities Managementalfonzo.keilerNo ratings yet
- D197-Lab Exercise 2.2 - Bihay and SumaljagDocument5 pagesD197-Lab Exercise 2.2 - Bihay and Sumaljagjelly bihayNo ratings yet
- Acm 4 - B4-A1Document4 pagesAcm 4 - B4-A1Heru HaryantoNo ratings yet
- Conventional Transfer PumpsDocument15 pagesConventional Transfer PumpsNhocSkyzNo ratings yet
- RAMMINGDocument3 pagesRAMMINGmatheswaran a sNo ratings yet
- End-Of-Course Test (Word)Document4 pagesEnd-Of-Course Test (Word)los ikandasNo ratings yet
- Body MechanismDocument31 pagesBody MechanismAnnapurna DangetiNo ratings yet
- Turbine Gas G.T.G. 1Document17 pagesTurbine Gas G.T.G. 1wilsonNo ratings yet
- Testbank ch01Document14 pagesTestbank ch01HườngNo ratings yet
- Understand Trading in 2 Hours SteveRyanDocument63 pagesUnderstand Trading in 2 Hours SteveRyanAkash Biswal100% (3)
- SSP 666 Audi A8 Type 4N Infotainment and Audi ConnectDocument72 pagesSSP 666 Audi A8 Type 4N Infotainment and Audi Connectylk1No ratings yet
Ds 48 087
Ds 48 087
Uploaded by
Jim HopkinsOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ds 48 087
Ds 48 087
Uploaded by
Jim HopkinsCopyright:
Available Formats
Original Article
Efficacy and Safety of a New Resilient Hyaluronic Acid
Filler in the Correction of Moderate-to-Severe Dynamic
Perioral Rhytides: A 52-Week Prospective, Multicenter,
Controlled, Randomized, Evaluator-Blinded Study
Hema Sundaram, MD, FAAD,* Ava Shamban, MD,† Joel Schlessinger, MD,‡ Joely Kaufman-Janette, MD,§
John H. Joseph, MD,k Mark Lupin, MD, FRCP, FAAD,{ Zoe Draelos, MD,** Wayne Carey, MD, FRCP, FAAD,††
Stacy Smith, MD,‡‡ and Laura Eaton, RN, BSN§§
BACKGROUND The perioral region is highly mobile and subject to multifactorial changes during aging. Resilient Hya-
luronic Acid Redensity (RHAR), an RHA filler, was developed with the aim of optimizing outcomes in dynamic facial areas.
OBJECTIVE This randomized, blinded, multicenter clinical study aimed to demonstrate superiority of RHAR over no-
treatment control for correction of moderate-to-severe dynamic perioral rhytides.
MATERIALS AND METHODS Blinded live evaluator assessments of efficacy included improvement in perioral rhytides
severity using a proprietary scale (Perioral Rhytids Severity Rating Scale [PR-SRS]) and the Global Aesthetic Improvement
Scale. Subjects self-assessed their results with FACE-Q, a validated patient-reported outcome measure, and satisfaction
scales. Safety was monitored throughout the study based on common treatment responses (CTRs) and adverse events
(AEs).
RESULTS The primary efficacy end point was achieved, with the treatment group showing statistically significant su-
periority over the control group at Week 8 (80.7% vs 7.8% responder rate by PR-SRS, p , .0001). Most patients (66%)
were still responders at Week 52 (study completion). Most AEs were CTRs after perioral injection of a dermal filler, and
none was a clinically significant treatment-related AE.
CONCLUSION Resilient Hyaluronic Acid Redensity is effective and safe for the correction of dynamic perioral rhytides in
all Fitzpatrick phototypes, with marked durability.
P erioral aging is highly individualized, comprising
several distinct and simultaneous processes in the
bone, and subcutaneous and cutaneous tissues that
are driven by extrinsic and intrinsic factors.1–4
Manifestations of volume loss in the upper lip include
decreased tissue elasticity, lip ptosis, decreased lip thickness
relative to length, loss of lip volume, contour and vermilion
border eversion, and skin textural changes.2,5,6 Fine vertical
rhytides above the upper lip and under the lower lip are
primarily related to repetitive movements, photoaging with
From the *Dermatology, Cosmetic, and Laser Surgery Center, Rockville, Maryland
thinning of the skin and subcutis,7 and resorption of underlying
and Fairfax, Virginia; † ATS Clinical Research, Santa Monica, California; ‡ Skin
Specialists PC, Omaha, Nebraska; § Skin Research Institute, LLC, Coral Gables, bone and dentition.
Florida; kClinical Testing of Beverly Hills, Beverly Hills, California; {Cosmedica Laser Risk factors for development of perioral rhytides include
Center, Victoria, Canada; **Dermatology Consulting Services, High Point, North
Carolina; †† Siena Medical Research Corporation, Montreal, Canada; ‡ ‡ California
age, history of smoking, cumulative sun exposure, sex, and
Dermatology & Clinical Research Institute, Encinitas, California; §§ UltaMed skin phototype. Greater innate photoprotection contributes to
Corporation, Fort Lauderdale, Florida the decreased propensity of individuals with higher Fitzpatrick
Materials and funding for this study were provided by TEOXANE.
skin phototypes to develop perioral lines.8 Female patients
H. Sundaram, A. Shamban, J. Schlessinger, J. Kaufman-Janette, J. H. Joseph, M.
Lupin, Z. Draelos, and W. Carey were clinical investigators for this study and received tend to develop more and deeper perioral wrinkling, and more
research grants for study participation. L. Eaton is a paid consultant for TEOXANE. S. pronounced general manifestations of lip aging.8,9
Smith was compensated by TEOXANE for his role as the study medical monitor. The perioral region and lips are critical markers of youth,
While the US FDA premarketing approval (PMA) submission process of RHAR is
ongoing, the device is not currently approved by FDA.
attractiveness, and beauty.10 Although injection of hyaluronic
Address correspondence and reprint requests to: Hema Sundaram, MD, FAAD, acid (HA) dermal filler into perioral lines is a common
11119 Rockville Pike, Ste 205, Rockville, MD 20852, or e-mail: hemasundaram@ rejuvenation strategy, the structural and functional anatomy
gmail.com
of this region, as well as its mobility, present significant
This is an open access article distributed under the Creative Commons Attribution
License 4.0 (CCBY), which permits unrestricted use, distribution, and reproduction challenges.
in any medium, provided the original work is properly cited. The investigational device for this study, Resilient
Supplemental digital content is available for this article. Direct URL citations appear Hyaluronic Acid Redensity (RHAR), belongs to a range of
in the printed text and are provided in the full text and PDF versions of this article on
the journal’s Web site (www.dermatologicsurgery.org). RHA fillers that are specifically designed to adapt to facial
http://dx.doi.org/10.1097/DSS.0000000000003238 dynamics. Resilient hyaluronic acid fillers are crosslinked
RHAR Filler for Dynamic Perioral Rhytides • Sundaram et al www.dermatologicsurgery.org 87
with 1,4-butanediol diglycidyl ether (BDDE) using a unique Materials and Methods
manufacturing process, the Preserved Network technology,
that results in a greater preservation of HA chains, thus
Trial Design and Population
This randomized, single-blinded, no-treatment control,
requiring a low degree of modification (MoD) to provide
multicenter, prospective clinical trial was conducted in
clinically relevant product properties.11 Resilient Hyalur-
accordance with the International Conference on Harmo-
onic Acid Redensity has a HA concentration of 15 mg/mL
nization, Good Clinical Practice guidelines, Code of Federal
and a low MoD of 2%, as compared with 5% to 10% in
Regulations, and the Declaration of Helsinki. The study
most HA gels,12 translating into rheological properties
received approval from an institutional review board and
adapted to treat fine lines and superficial wrinkles in mobile
was registered on ClinicalTrials.gov (NCT03092219). All
areas such as the perioral region.13,14
subjects gave informed consent before any study procedures
Biomechanical characterization of RHA fillers has
being performed.
demonstrated their resilient behavior, that is, improved
The target population for inclusion was adults 22 years
capacity to recover their original shape and mechanical
of age and older, with moderate-to-severe perioral rhytides
features after compression, stretching, or bending.11,13
(Grade 2 or 3 on the 4-point scale, PR-SRS15). The study
Other investigators have reported homogeneous tissue
aimed to recruit at least 25% subjects with Fitzpatrick skin
integration of RHA fillers after intradermal injection.14
phototypes IV to VI. Considering the global population size,
This study was conducted to demonstrate the superi-
this was sufficient for detection of any adverse event (AE)
ority of RHAR over no-treatment control for the
with an incidence of 2.5% or more in these skin types.
correction of moderate-to-severe dynamic perioral
Subjects who met all inclusion criteria and no exclusion
rhytides, as assessed by a blinded live evaluator on the
criteria were randomized 3:1 to treatment with RHAR
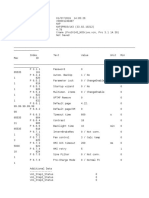
Perioral Rhytids Severity Rating Scale (PR-SRS;
(treatment group) or to no treatment (control group).
Figure 1) 8 weeks after treatment. The study also
Subjects in the control group commenced treatment with
evaluated product safety and durability of the aesthetic
RHAR at Week 8 after primary end point evaluation. They
improvement, up to 52 weeks after initial or touch-up
subsequently followed the same schedule of injection and
injection.
evaluation as subjects in the treatment group (see Supple-
mental Digital Content 1, Figure S1, http://links.lww.com/
DSS/A911, which demonstrates the study schematics).
Treatment
Resilient Hyaluronic Acid Redensity (TEOXANE S.A.,
Geneva, Switzerland) is a dermal filler composed of 15 mg/
mL high-molecular-weight, BDDE-crosslinked HA, and
0.3% lidocaine hydrochloride, in a physiologic phosphate
buffer (pH 7.3). The device was injected using 30-gauge
½-inch needles. The treatment group received injections of
RHAR into the upper and lower perioral rhytides at Day
0 (Visit 1). Subjects were offered optional touch-up
treatment 14 days later to provide optimal aesthetic
correction. Subjects were eligible for repeat treatment at
12, 16, 24, or 36 weeks after their last treatment if their PR-
SRS score had returned to its baseline value. All subjects
were offered retreatment at the end of the study (Week 52).
Supplemental preinjection and postinjection pain control
was at the investigator’s discretion and included regional
anesthesia (nerve block), topical anesthesia (4% lidocaine
cream or EMLA eutectic mixture of lidocaine 2.5% and
prilocaine 2.5%), and ice and cool packs.
Injection Technique
Treating physicians aimed for intradermal injection of the
product by using blanching serial puncture, linear threading
or cross-hatching, raising a wheal with a 30-gauge ½-inch
needle bevel-up at an angle of 5 to 15° to the skin surface.
During linear threading or cross-hatching, investigators
aimed to keep the needle superficial enough to be visible
Figure 1. Perioral Rhytids Severity Rating Scale (PR-SRS). A
through the skin surface. Injections could be anterograde or
proprietary 4-grade rating scale [0–3].
retrograde, and postinjection skin massage was permitted.
88 DERMATOLOGIC SURGERY • January 2022 • Volume 48 • Number 1 www.dermatologicsurgery.org
Study End Points and Variables defined as subjects achieving $1-point improvement on the
PR-SRS.
Safety End Points
Per protocol (PP), intent-to-treat (ITT), and safety
Subjects assessed their injection site pain after each injection (SAFT) populations were defined for statistical analysis.
on a 100-mm visual analog scale (VAS). For 14 days after The PP population consisted of subjects who had completed
each treatment visit, subjects recorded the nature, severity, 8 weeks of treatment follow-up without any major protocol
and duration of any local injection site events in a 14-day deviation. The ITT population included all randomized
common treatment responses (CTRs) diary. Any CTR subjects who had received at least one treatment with RHAR
persisting at the 14-day timepoint was automatically filler in compliance with their treatment protocol allocation
considered an AE. Periodic safety evaluations included (randomized group assignment). The SAFT population
CTR and AE review and lip functionality assessment and comprised all subjects who had received at least one
were conducted on-site at Weeks 2, 4, 8, 12, 16, 24, 36, and treatment, whether or not they complied with their
52, as well as 4 weeks after Week 52 retreatment if treatment protocol allocation.
performed. Analyses of the primary and secondary end points of
efficacy were performed separately for the ITT and PP
Efficacy End Points populations. Safety descriptive analyses used the SAFT
population.
The primary study end point was the severity score for One-sided Fisher exact tests were used to detect
perioral rhytides on the PR-SRS, as assessed by the BLE at significant differences between the treatment and control
Week 8 after the last treatment (initial or touch-up). Of groups for the primary and secondary end points, with a
note, the PR-SRS is a photo-validated scale. Repeatability 0.025 significance level.
and reproducibility of subject grading using the scale was
confirmed by statistical analysis of the validation data
(weighted kappa scores for intrarater and interrater Results
agreement were all .0.7; data not published). Study Population
Secondary end points included the Perioral Rhytids Two hundred two subjects with moderate-to-severe perio-
Domain of the FACE-Q, a validated patient-reported ral rhytides (PR-SRS Grade 2 or 3) were enrolled at 8 study
outcome measure16–18; BLE assessment of improvement sites, 6 in the United States and 2 in Canada. One hundred
on the Global Aesthetic Improvement Scale (GAIS); and fifty subjects were randomized to the treatment group and
subject satisfaction. 52 to the control group. The sizes and dispositions of the PP,
Efficacy evaluations were conducted by the BLE at ITT, and SAFT populations are detailed in Supplemental
Weeks 8, 12, 16, 24, 36, and 52 after the last treatment. Digital Content 2 (see Figure S2, http://links.lww.com/DSS/
Subject self-evaluations were also performed at Weeks 2 A912, consort diagram). The mean ages in the treatment
and 4. Efficacy end points were assessed separately for the group and control group were 61.6 6 7.2 years and 60.7 6
treatment and control groups and compared up to Week 8; 7.6 years, respectively. Ninety-eight percent of the subjects
they were then evaluated within the pooled population up to were women and 27% had Fitzpatrick skin Phototypes IV
Week 52 after last treatment. to VI. There were 35 (17.3%) Hispanic, 4 (2.0%) African
Exploratory end points assessed in the pooled population American, and 2 (1.0%) Asian subjects (see Supplemental
until Week 52 included the following: BLE grading on the Digital Content 3, Table S1, http://links.lww.com/DSS/
PR-SRS and GAIS; Subject Satisfaction; Natural Look & A914, which demonstrates subject demographics and
Feel score; and the Perioral Rhytids Domain of the FACE-Q. injection volume).
Subject satisfaction with the study treatment was evaluated
using a 5-point scale from very satisfied (Grade 1) to very Injection Volume and Technique
dissatisfied (Grade 5). Natural Look & Feel was assessed on The mean initial injection volume of RHAR was 2.0 6 1.2
a study-specific, 11-point scale ranging from 0 (unnatural) mL. At Week 2, 68% of subjects received a touch-up
to 10 (natural); any subject with a score of $7 was deemed a treatment with an average injected volume of 1.2 6 1.1 mL.
responder for this assessment. The total volume—including initial and touch-up
treatments—to achieve optimal correction of perioral
Statistical Analysis rhytides was 2.8 6 2.0 mL.
The primary objective of the study was to demonstrate Nine subjects who had perioral furrows and were on the
statistical superiority of RHAR filler to no-treatment, based extreme end of Grade 3 (severe) of the PR-SRS received
on improvement of perioral rhytides as assessed by the BLE significantly higher volumes of RHAR ($5 mL). When
on the PR-SRS at Week 8. excluding these outliers, the mean initial and touch-up
The primary end point was a co-primary end point that volumes of RHAR were 1.8 6 1.0 mL and 1.1 6 0.9 mL,
required 3 conditions to be met: the responder rate in the respectively, and the total volume required for optimal
RHAR treatment group had to be (1) statistically superior, correction was 2.5 6 1.6 mL.
and (2) $50 percentage points higher compared with no- Early repeat treatments at Week 12, 16, 24, or 36
treatment control; and (3) above 70%. Responders were occurred in a total of 17.6% of subjects—3.3%, 2.2%,
RHAR Filler for Dynamic Perioral Rhytides • Sundaram et al www.dermatologicsurgery.org 89
4.7% and 8.5%, respectively. The mean injected volume for the presence, duration, and severity of predefined CTRs for
those early repeat treatments was approximately 2 mL. 14 days after each treatment. Any CTR that was ongoing on
Taking all injections into account (initial, touch-up, early the last diary day was automatically considered an AE.
repeat treatment, and final retreatment), mean total injected There were no serious treatment-related AEs (TRAEs),
volume ranged from 1.4 to 7.7 mL over the 52-week study unanticipated device-related events or late-onset TRAEs,
period. nodular complications, or vascular compromise events.
Subjects experiencing at least one TRAE accounted for
Primary Effectiveness 31.1% of the SAFT population. All TRAEs were mild to
The primary efficacy end point at Week 8 was achieved. moderate in severity, all resolved, and none was deemed
Resilient Hyaluronic Acid Redensity showed statistically clinically significant.
significant superiority to no-treatment for the correction of Three TRAEs (1.6%) were reported independently of the
dynamic perioral rhytides, as assessed on the PR-SRS CTR diary: skin discoloration, headache, and oral herpes
(80.7% vs 7.8% responder rate, p , .0001) (Figure 2A). simplex.
The 2 co-primary end points were met, as the responder rate The rate of CTRs after initial injection was comparable
of the treatment group was above 70%, and more than 50 with the rate after touch-up. Across all injections performed
percentage points higher than that of the control group. (initial, touch-up, and early repeat treatment), the most
The effect was durable, with 66% subjects of the pooled common TRAEs were lumps and bumps/contour irregular-
population still classified as responders at Week 52 ities (17%), firmness (11.0%), and injection site bruising
(Figure 2A). (10.5%) (see Supplemental Digital Content 5, Table S2,
Representative pretreatment and posttreatment subject http://links.lww.com/DSS/A915, which demonstrates the
images are shown in Figure 3. CTR rates after initial injection).
Twenty-six (14.0%) TRAEs originated from a CTR
Secondary and Exploratory End Points diary section labelled “Other,” where symptoms could be
written in. They included headache, hypoesthesia, injection
FACE-Q site paresthesia, and injection site scabbing.
Assessment of patient-reported outcomes with the FACE-Q Mean score on the 100-mm VAS for pain was 19.9 mm
showed significantly higher scores at Weeks 4 and 8 for the (95% confidence interval [CI] [17.1–22.6]) during initial
treatment group than for the control group. FACE-Q scores injection and 3.1 mm (95% CI [2.0–4.3]) 15 minutes after
were maintained in the pooled population after Week 8, injection. Assessments of lip functionality were unchanged
with a mean of 59 points at Week 52 (Figure 2b). postinjection, except for one subject who reported moderate
inability to pucker while whistling, which resolved within
1 day.
Global Aesthetic Improvement Scale
Thirty-seven percent of subjects with Fitzpatrick skin
As assessed by the BLE using the GAIS, the degree of phototypes I to III experienced at least one TRAE, as
aesthetic improvement at Week 8 was significantly higher compared with 35.2% of subjects with photoypes IV to VI.
for the treatment group than for the control group (92.5%
vs 8.3%, p , .0001) (Figure 2C). After Week 8, the GAIS Discussion
was assessed by the BLE at each subsequent visit until Week This publication reports the first randomized, no-treatment
52 for the pooled population. Improvement was still visible control clinical trial to evaluate efficacy, safety, tolerability, and
in 80.9% of subjects at their last visit. durability of Resilient Hyaluronic Acid Redensity (RHAR), a
novel RHA dermal filler, for improvement of perioral rhytides.
Subject Satisfaction A large study cohort inclusive of all Fitzpatrick skin phototypes
provides evidence to support the indication for RHAR in the
The proportion of subjects satisfied with treatment peaked
diverse North American population.
at 91.8% at Week 4 and was 88.3% at Week 52 (see
Resilient Hyaluronic Acid Redensity was superior to no-
Supplemental Digital Content 4, Figure S3, http://links.lww.
treatment (p , .0001) for correction of moderate-to-severe
com/DSS/A913, which demonstrates subject satisfaction). dynamic perioral rhytides, as rated by BLEs on a pro-
prietary wrinkle severity scale (PR-SRS). Scores on GAIS
Natural Look & Feel Scale and patient satisfaction scales were consistently high.
The percentage of subjects who scored their natural look Treatment outcomes were durable through Week 52, with
and feel as $7/10 was 46% before treatment, 88.8% at a small proportion (17.6%) of subjects requiring early
Week 8 after treatment, and 87.2% in the pooled retreatment.
population at Week 52. Based on AEs monitored throughout the study, treat-
ment with RHAR was safe and well-tolerated. Most TRAEs
were CTR that were documented as AEs due to their
Safety
persistence on or beyond the last day of the subjects’ 14-day
Adverse events were recorded by the treating investigator at postinjection diaries. The reporting of lumps and bumps
study visits. Subjects also completed a daily diary, recording typically reflected the subjects’ ability to feel some product
90 DERMATOLOGIC SURGERY • January 2022 • Volume 48 • Number 1 www.dermatologicsurgery.org
Figure 2. Effectiveness end points at Week 8 in the treatment group versus no-treatment control, and throughout the study in the
pooled population.
RHAR Filler for Dynamic Perioral Rhytides • Sundaram et al www.dermatologicsurgery.org 91
Figure 3. Before (A) and after (B) photo-
graphs of a 69-year-old female subject with
moderate perioral rhytides at baseline (A),
who improved to mild at Week 8 posttreat-
ment (B). Initial volumes injected into the
upper and lower perioral rhytides were, re-
spectively, 0.6 and 0.4 mL, with touch-up
volumes of 0.5 and 0.4 mL. Injection tech-
niques were retrograde linear threading and
serial punctures.
under the skin due to its superficial placement, which Conclusion
resolved spontaneously. No late-onset nodules were noted. In this prospective, multicenter, blinded-evaluator con-
Previous studies have attributed lesser durability in trolled study of 202 subjects of all Fitzpatrick skin photo-
mobile facial areas to frequent muscular activity, resulting types, RHAR was shown to be effective and safe for the
in shearing forces that promote filler degradation.19,20 In correction of dynamic perioral rhytides.
the perioral region, the desire for durability must be Resilient Hyaluronic Acid Redensity demonstrated
weighed against the risk of nodules from filler products marked durability, with 66% of subjects maintaining a
that are too firm or subject to displacement within the tissue clinical response at the Week 52 visit. Importantly, no late-
due to strong muscular forces. In this study, RHAR provided onset AEs were observed. Aesthetic improvement assessed
lasting aesthetic improvement without emergence of late- on the GAIS was maintained throughout the study, and
onset AEs throughout the study evaluation period of 52 patient satisfaction was consistently high.
weeks. Resilient Hyaluronic Acid Redensity is the most super-
The results of this study agree with prior randomized ficially implanted product in a range of RHA fillers
controlled trials that have demonstrated the safety, efficacy, developed to treat wrinkles and folds in different areas
and lasting effects of other RHA fillers for aesthetic while accommodating facial dynamics. This range of RHA
treatments in dynamic facial areas.21,22 fillers that provides durable results with a low degree of
Study limitations included the participation of only 4 crosslinking modification of the HA chains may represent a
male subjects, representing 2% of the study population. novel and useful addition to the aesthetic toolbox.
Additionally, only 3 subjects had Fitzpatrick skin phototype
VI; all were enrolled in the RHAR treatment group. One
challenge to recruitment of subjects with skin phototype VI Acknowledgments
and of male patients was the inclusion criterion of The authors are grateful to Ethica CRO, Canfield Scientific,
moderate-to-severe perioral rhytides. Both higher photo- TEOXANE Laboratories, specifically the Clinical Development
type individuals and male patients have a lower incidence of team, and all involved in the conduct of this study, including the
perioral rhytides.23 This challenge may be addressed in the Blinded Live Evaluators and Study Coordinators at each site. The
future studies through expanded inclusion criteria and/or a authors would also like to thank Vidya Srinivasan for critical review
specific focus on underrepresented patients. Nevertheless, of this manuscript.
no significant difference in safety outcomes was found
between lower (I–III) and higher (IV–VI) phototypes in this References
study; the treatment was well tolerated by all subjects. 1. Ali MJ, Ende K, Maas CS. Perioral rejuvenation and lip augmentation.
Facial Plast Surg Clin North Am 2007;15:491–500, vii.
Injection volumes were variable between subjects, as
2. Iblher N, Kloepper J, Penna V, Bartholomae JP, et al. Changes in the
shown by large standard deviations, and some were higher aging upper lip–a photomorphometric and MRI-based study (on a
than expected for superficial fine lines. This can be quest to find the right rejuvenation approach). J Plast Reconstr Aesthet
explained by the inclusion of subjects with significant Surg 2008;61:1170–6.
perioral furrows, who were at the extreme end of PR-SRS 3. Penna V, Stark GB, Voigt M, Mehlhorn A, et al. Classification of the
Grade 3 (“severe”), thereby needing greater volumes to aging lips: a foundation for an integrated approach to perioral re-
juvenation. Aesthet Plast Surg 2015;39:1–7.
achieve an optimal correction. 4. Scarano A, Mortellaro C, Mavriqi L, Di Cerbo A. Evaluation effec-
It has been saliently noted that clinical studies of fillers tiveness of the voltaic arc dermabrasion in perioral rhytides eradica-
differ in a number of respects from everyday dermatological tion. J Craniofac Surg 2016;27:1205–8.
practice.24 This reflects the limitations of clinical trials 5. Ramaut L, Tonnard P, Verpaele A, Verstraete K, et al. Aging of the
whose efficacy end points must be selected to show effects of upper lip: Part I: a retrospective analysis of metric changes in soft tissue
on magnetic resonance imaging. Plast Reconstr Surg 2019;143:440–6.
a single product. In everyday clinical practice, sustained
6. Shah AR, Kennedy PM. The aging face. Med Clin North Am 2018;
perioral correction may be more volume-efficient because 102:1041–54.
dermal fillers can be combined with botulinum toxin 7. Iblher N, Stark GB, Penna V. The aging perioral region—do we really
treatment. know what is happening?. J Nutr Health Aging 2012;16:581–5.
92 DERMATOLOGIC SURGERY • January 2022 • Volume 48 • Number 1 www.dermatologicsurgery.org
8. Chien AL, Qi J, Cheng N, Do TT, et al. Perioral wrinkles are associated 18. Klassen AF, Cano SJ, Scott A, Snell L, et al. Measuring patient-
with female gender, aging, and smoking: development of a gender- reported outcomes in facial aesthetic patients: development of the
specific photonumeric scale. J Am Acad Dermatol 2016;74:924–30. FACE-Q. Facial Plast Surg 2010;26:303–9.
9. Paes EC, Teepen HJ, Koop WA, Kon M. Perioral wrinkles: histologic 19. Carruthers A, Carruthers J, Monheit GD, Davis PG, et al. Multicenter,
differences between men and women. Aesthet Surg J 2009;29:467–72. randomized, parallel-group study of the safety and effectiveness of
10. Wollina U. Perioral rejuvenation: restoration of attractiveness in onabotulinumtoxinA and hyaluronic acid dermal fillers (24-mg/ml
ageing females by minimally invasive procedures. Clin Interv Ageing smooth, cohesive gel) alone and in combination for lower facial re-
2013;8:1149–55. juvenation. Dermatol Surg 2010;36(Suppl 4):2121–34.
11. Faivre J, Gallet M, Tremblais E, Trévidic P, et al. Advanced concepts in 20. Küçüker İ, Aksakal IA, Polat AV, Engin MS, et al. The effect of che-
rheology for the evaluation of hyaluronic acid–based soft tissue fillers. modenervation by botulinum neurotoxin on the degradation of hya-
Dermatol Surg 2021;47:e159–e167. luronic acid fillers: an experimental study. Plast Reconstr Surg 2016;
12. Edsman K, Nord LI, Ohrlund A, Lärkner H, et al. Gel properties of 137:109–13.
hyaluronic acid dermal fillers. Dermatol Surg 2012;38:1170–9. 21. Kaufman-Janette J, Taylor SC, Cox SE, Weinkle SH, et al. Efficacy and
13. Bourdon F, Meunier S, Inventors. Process for evaluating the mechanical safety of a new resilient hyaluronic acid dermal filler, in the correction
performance of a filler gel. US patent WO 2016/150974 A12016. of moderate-to-severe nasolabial folds: a 64-week, prospective, mul-
14. Micheels P, Sarazin D, Besse S, Eliasd B. Comparison of two Swiss- ticenter, controlled, randomized, double-blind and within-subject
designed hyaluronic acid gels: six-month clinical follow-up. J Drugs study. J Cosmet Dermatol 2019;18:1244–53.
Dermatol 2017;16:154–61. 22. Monheit G, Kaufman-Janette J, Joseph JH, Shamban A, et al. Efficacy
15. Data on file T. Development and Validation of a Severity Rating Scale and safety of two resilient hyaluronic acid fillers in the treatment of
for Perioral Rhytids—Internal Report. Geneva, Switzerland: Teox- moderate-to-severe nasolabial folds: a 64-week, prospective, multi-
ane; 2016. center, controlled, randomized, double-blinded, and within-subject
16. Kappos EA, Temp M, Schaefer DJ, Haug M, et al. Validating facial study. Dermatol Surg 2020;46:1521–29.
aesthetic surgery results with the FACE-Q. Plast Reconstr Surg 2017; 23. Taylor SC, Downie JB, Shamban A, Few J, et al. Lip and perioral
139:839–45. enhancement with hyaluronic acid dermal fillers in individuals with
17. Klassen AF, Cano SJ, Schwitzer JA, Baker SB, et al. Development and skin of color. Dermatol Surg 2019;45:959–67.
psychometric validation of the FACE-Q skin, lips, and facial rhytids 24. Del Campo R, Mandy S. Commentary on safety and effectiveness of
appearance scales and adverse effects checklists for cosmetic proce- VYC-15L, a hyaluronic acid filler for lip and perioral enhancement.
dures. JAMA Dermatol 2016;152:443–51. Dermatol Surg 2017;43:405–6.
RHAR Filler for Dynamic Perioral Rhytides • Sundaram et al www.dermatologicsurgery.org 93
You might also like
- The Selection of Hyaluronic Acid When Treating With The Nasolabial Fold A Meta-Analysis - Peng, 2021Document9 pagesThe Selection of Hyaluronic Acid When Treating With The Nasolabial Fold A Meta-Analysis - Peng, 2021Rafael Autran Cavalcante AraújoNo ratings yet
- Calcium Hydroxylapatite (Radiesse) For Correction of The Mid-And Lower Face: Consensus RecommendationsDocument12 pagesCalcium Hydroxylapatite (Radiesse) For Correction of The Mid-And Lower Face: Consensus RecommendationsMichele Carvalho100% (1)
- Antiaging Efficacy of A Retinaldehyde-Based Cream Compared With Glycolic Acid Peel Sessions: A Randomized Controlled StudyDocument8 pagesAntiaging Efficacy of A Retinaldehyde-Based Cream Compared With Glycolic Acid Peel Sessions: A Randomized Controlled Studypermen_lollypopzNo ratings yet
- Q3 G11 Physical Science Module 7Document19 pagesQ3 G11 Physical Science Module 7Lebz RicaramNo ratings yet
- An Approach To Structural Facial Rejuvenation With Fillers in WomenDocument15 pagesAn Approach To Structural Facial Rejuvenation With Fillers in WomenJhon RodriguezNo ratings yet
- A Randomized Study of The Efficacy and Safety of Injectable Poly-L-lactic Acid Versus Human-Based Collagen Implant in The Treatment of Nasolabial Fold Wrinkles - Narins, 2010Document15 pagesA Randomized Study of The Efficacy and Safety of Injectable Poly-L-lactic Acid Versus Human-Based Collagen Implant in The Treatment of Nasolabial Fold Wrinkles - Narins, 2010Rafael Autran Cavalcante AraújoNo ratings yet
- Evaluation Long-Term Safety Biodegradability Hyaluronic Acid Dermal Fillers (YVOIRE®) Correction Nasolabial Folds Two Multicenter, Prospective, Observational Cohort Studies - Xie, 2022Document11 pagesEvaluation Long-Term Safety Biodegradability Hyaluronic Acid Dermal Fillers (YVOIRE®) Correction Nasolabial Folds Two Multicenter, Prospective, Observational Cohort Studies - Xie, 2022Rafael Autran Cavalcante AraújoNo ratings yet
- Rinomodelacion - HidroxiapatitaDocument6 pagesRinomodelacion - HidroxiapatitaMauricio Ocampo MazoNo ratings yet
- Efektivitas Dan Keamanan Kojic DipalmitatDocument6 pagesEfektivitas Dan Keamanan Kojic DipalmitatmurjonocrbNo ratings yet
- A Randomized, Evaluator-Blinded, Controlled Study of The Effectiveness and Safety of Small Gel Particle Hyaluronic Acid For Lip Augmentation2021Document13 pagesA Randomized, Evaluator-Blinded, Controlled Study of The Effectiveness and Safety of Small Gel Particle Hyaluronic Acid For Lip Augmentation2021Jhon RodriguezNo ratings yet
- A Series of in Vitro and Human Studies of A Novel Lip Cream FormulationDocument16 pagesA Series of in Vitro and Human Studies of A Novel Lip Cream FormulationDummy CipawNo ratings yet
- Thehyaluronicacid Fillers: Current Understanding of The Tissue Device InterfaceDocument10 pagesThehyaluronicacid Fillers: Current Understanding of The Tissue Device InterfaceLuis Fernando WeffortNo ratings yet
- 2018.degradation HialuronidaseDocument6 pages2018.degradation Hialuronidaseingrid castroNo ratings yet
- 65 DDB 7 CF 79183Document11 pages65 DDB 7 CF 79183marisa araujoNo ratings yet
- A Review of The Metabolism of 1,4-Butanediol Diglycidyl Ether-Crosslinked Hyaluronic Acid Dermal FillersDocument9 pagesA Review of The Metabolism of 1,4-Butanediol Diglycidyl Ether-Crosslinked Hyaluronic Acid Dermal FillersJhon RodriguezNo ratings yet
- Hyaluronic Acid Fillers in Facial Rejuvenation: Mary P. Lupo, MDDocument5 pagesHyaluronic Acid Fillers in Facial Rejuvenation: Mary P. Lupo, MDEduarda De Menezes GerlachNo ratings yet
- Current Concepts in The Use of Small-Particle Hyaluronic AcidDocument7 pagesCurrent Concepts in The Use of Small-Particle Hyaluronic AcidThaís SagratzhiNo ratings yet
- Dermatologic Therapy - 2022 - WongprasertDocument9 pagesDermatologic Therapy - 2022 - Wongprasertdocrubes50No ratings yet
- 2016 Lagatta Rheology ALLIAXINDocument8 pages2016 Lagatta Rheology ALLIAXINANDRÉ CAMARGONo ratings yet
- A Novel at Home Procedure Providing Marked Improvements - 2014 - Journal of The PDFDocument1 pageA Novel at Home Procedure Providing Marked Improvements - 2014 - Journal of The PDFNachi MontianarrtNo ratings yet
- Treatment of Acne Scars With RadiesseDocument3 pagesTreatment of Acne Scars With RadiesseMethawin Chatmethinwat100% (1)
- Jcad 12 9 32Document4 pagesJcad 12 9 32Gerardo Valenzuela GonzálezNo ratings yet
- 001 Lip LiftDocument11 pages001 Lip Liftdr.antonio.velasquezNo ratings yet
- 10 1111@jocd 12861Document8 pages10 1111@jocd 12861Erik BrooksNo ratings yet
- Changes in The Strategies For Caries Management in Older Adults A Non-Invasive AlternativeDocument2 pagesChanges in The Strategies For Caries Management in Older Adults A Non-Invasive AlternativeSeba MirandaNo ratings yet
- Global Periorbital Skin Rejuvenation by A Topical Eye Cream (JOCD-18-530)Document9 pagesGlobal Periorbital Skin Rejuvenation by A Topical Eye Cream (JOCD-18-530)FuckyaNo ratings yet
- Clinical and Dermoscopic Evaluation of PeriorbitalDocument6 pagesClinical and Dermoscopic Evaluation of Periorbitalruby.wryNo ratings yet
- Journal of Biomedical Materials Research Part A Volume 87A Issue 1 2008 (Doi 10.1002 - Jbm.a.31675) Samuel J. Falcone Richard A. Berg - Crosslinked Hyaluronic Acid Dermal Fillers - A Comparison of RHDocument8 pagesJournal of Biomedical Materials Research Part A Volume 87A Issue 1 2008 (Doi 10.1002 - Jbm.a.31675) Samuel J. Falcone Richard A. Berg - Crosslinked Hyaluronic Acid Dermal Fillers - A Comparison of RHImanuel CristiantoNo ratings yet
- 10 1097@DSS 0000000000001281Document11 pages10 1097@DSS 0000000000001281plastic guardiansNo ratings yet
- ZO điều trị TSTDocument7 pagesZO điều trị TSTHong Nguyen ThiNo ratings yet
- Evaluation of A Kojic Acid, PDFDocument6 pagesEvaluation of A Kojic Acid, PDFvanitha13No ratings yet
- 10 1097@DSS 0000000000002271Document9 pages10 1097@DSS 0000000000002271Rhelvis1No ratings yet
- Radiesse For Aesthetic Soft Tissue Augmentation PDFDocument7 pagesRadiesse For Aesthetic Soft Tissue Augmentation PDFfishvalNo ratings yet
- عقار 24Document8 pagesعقار 24عمار حسين عبدعلي جاسم biologyNo ratings yet
- Adv Healthcare Materials - 2021 - Herrmann - Hydrogels and Their Role in Biosensing Applications PDFDocument25 pagesAdv Healthcare Materials - 2021 - Herrmann - Hydrogels and Their Role in Biosensing Applications PDFAlejandro Rojas GómezNo ratings yet
- JAMA Facial Plastic Surgery: Novel Use of A Volumizing Hyaluronic Acid Filler For Treatment of Infraorbital HollowsDocument23 pagesJAMA Facial Plastic Surgery: Novel Use of A Volumizing Hyaluronic Acid Filler For Treatment of Infraorbital HollowsDr. Hilder HernandezNo ratings yet
- Choi2015 Sculptra Sulco NasoDocument10 pagesChoi2015 Sculptra Sulco Nasoana clara scopelNo ratings yet
- Analysis of U.S. Food and Drug Administration Data On Filler Complications 2019Document5 pagesAnalysis of U.S. Food and Drug Administration Data On Filler Complications 2019maat1No ratings yet
- Physiochemical Properties and Application of Hyaluronic Acid A SystematicDocument7 pagesPhysiochemical Properties and Application of Hyaluronic Acid A SystematicThaís SagratzhiNo ratings yet
- Clinical Assessment of A Combination Lip TreatmentDocument6 pagesClinical Assessment of A Combination Lip TreatmentDummy CipawNo ratings yet
- Update On The Management of Rosacea From The American Acne & Rosacea SocietyDocument8 pagesUpdate On The Management of Rosacea From The American Acne & Rosacea SocietySong JieunNo ratings yet
- The Efficacy of Colloidal Oatmeal Cream 1 Percent As Addon Therapy in The Management of Chronic Irritant Hand Eczema - A Double-Blind StudyDocument11 pagesThe Efficacy of Colloidal Oatmeal Cream 1 Percent As Addon Therapy in The Management of Chronic Irritant Hand Eczema - A Double-Blind StudyQualityMattersNo ratings yet
- Modif Structure of HADocument6 pagesModif Structure of HAnina asrianaNo ratings yet
- Ghanim Et Al-2019-International Journal of Paediatric DentistryDocument8 pagesGhanim Et Al-2019-International Journal of Paediatric DentistryFamily DentalNo ratings yet
- SCMS Vol31 No2 HyperpigmentationDocument7 pagesSCMS Vol31 No2 HyperpigmentationFachrizal AuliaNo ratings yet
- Beneficial Effects of Hyaluronic Acid: Prasad N. Sudha, Maximas H. RoseDocument40 pagesBeneficial Effects of Hyaluronic Acid: Prasad N. Sudha, Maximas H. RosePaulo Emílio Alves AlvesNo ratings yet
- A 10-Point Plan For Avoiding Hyaluronic Acid Dermal Filler-Related Complications During Facial Aesthetic Procedures and Algorithms For ManagementDocument9 pagesA 10-Point Plan For Avoiding Hyaluronic Acid Dermal Filler-Related Complications During Facial Aesthetic Procedures and Algorithms For Managementleenatalia93100% (1)
- Ccid 13 701Document10 pagesCcid 13 701jess.sooares12No ratings yet
- Soft Tissue Augmentation With Dermal Fillers, Part 1: Lips and Lower FaceDocument6 pagesSoft Tissue Augmentation With Dermal Fillers, Part 1: Lips and Lower FaceMichele CarvalhoNo ratings yet
- J Colsurfb 2018 08 061Document7 pagesJ Colsurfb 2018 08 061Ratih Anindita Rahajeng RipyonoNo ratings yet
- Dermatologic Therapy (2020)Document7 pagesDermatologic Therapy (2020)고은영No ratings yet
- Physical Properties of A Novel SmallDocument8 pagesPhysical Properties of A Novel SmallSheila BerbelzinhaNo ratings yet
- Six Steps To The Perfect LipDocument9 pagesSix Steps To The Perfect LipTatiana Araujo100% (1)
- Ccid 179430 A Series of in Vitro and Human Studies of A Novel Lip Cream 032119Document16 pagesCcid 179430 A Series of in Vitro and Human Studies of A Novel Lip Cream 032119Lina WinartiNo ratings yet
- Hyaluronic Acid: A New Approach For The Treatment of Gingival Recession-A Systematic ReviewDocument11 pagesHyaluronic Acid: A New Approach For The Treatment of Gingival Recession-A Systematic ReviewGali Alfaro ZagalNo ratings yet
- Smith 2007Document10 pagesSmith 2007CARLOS ZUÑIGANo ratings yet
- Comparative Evaluation of Efficacy and Tolerability ofDocument8 pagesComparative Evaluation of Efficacy and Tolerability ofMelanny CindyNo ratings yet
- Fluoride Alternatives My PaperDocument10 pagesFluoride Alternatives My PaperNazim SallamNo ratings yet
- Chemical Peeling With Trichloroacetic Acid and Lactic Acid For Infraorbital Dark CirclesDocument6 pagesChemical Peeling With Trichloroacetic Acid and Lactic Acid For Infraorbital Dark CirclesAna Claudia Kordelos DinizNo ratings yet
- 1 Consenso Carruthers2016Document12 pages1 Consenso Carruthers2016Lorena AcevedoNo ratings yet
- Role of Lipid Excipients in Modifying Oral and Parenteral Drug Delivery: Basic Principles and Biological ExamplesFrom EverandRole of Lipid Excipients in Modifying Oral and Parenteral Drug Delivery: Basic Principles and Biological ExamplesKishor M. WasanNo ratings yet
- Gr11 Mock Exam Schedule 2024Document13 pagesGr11 Mock Exam Schedule 2024potrillo0330No ratings yet
- Cookie Experimental DesignDocument2 pagesCookie Experimental Designapi-293314791No ratings yet
- Marked Fake Deck Tricks3Document7 pagesMarked Fake Deck Tricks3Tito Banerjee100% (1)
- Distribution Channel of AMULDocument13 pagesDistribution Channel of AMULMeet JivaniNo ratings yet
- Detailed Report On Gwadar PortDocument4 pagesDetailed Report On Gwadar PortxeninNo ratings yet
- UN - HIV and Prison - Policy BriefDocument12 pagesUN - HIV and Prison - Policy BriefParomita2013No ratings yet
- Matrices of Violence: A Post-Structural Feminist Rendering of Nawal El Saadawi's Woman at Point Zero and Lola Soneyin's The Secrets of Baba Segi's WivesDocument6 pagesMatrices of Violence: A Post-Structural Feminist Rendering of Nawal El Saadawi's Woman at Point Zero and Lola Soneyin's The Secrets of Baba Segi's WivesIJELS Research JournalNo ratings yet
- Pharmacognosy-Large FontDocument35 pagesPharmacognosy-Large FontArantxa HilarioNo ratings yet
- EDTA CHEMICAL CLEANING (BLR) PDFDocument16 pagesEDTA CHEMICAL CLEANING (BLR) PDFAnudeep Chittluri100% (2)
- Module 6 - Sequential Circuits, Excitation Function, State Table, State DiagramDocument21 pagesModule 6 - Sequential Circuits, Excitation Function, State Table, State DiagramYvanne Esquia CuregNo ratings yet
- XC9572 PDFDocument9 pagesXC9572 PDFAvs ElectronNo ratings yet
- 1000mm BOPP Tape Coating Machine Two Color Printing 40 Speed TangerangDocument6 pages1000mm BOPP Tape Coating Machine Two Color Printing 40 Speed TangerangJaja JamaludinNo ratings yet
- Scala AccesoriesDocument27 pagesScala AccesoriesZiggy BussyNo ratings yet
- BenfordDocument9 pagesBenfordAlex MireniucNo ratings yet
- Santa Cruz Scanner FreqsDocument35 pagesSanta Cruz Scanner FreqsdonsterthemonsterNo ratings yet
- Supervisi Akademik Melalui Pendekatan Kolaboratif Oleh Kepala Sekolah Dalammeningkatkan Kualitas Pembelajarandisd Yari DwikurnaningsihDocument11 pagesSupervisi Akademik Melalui Pendekatan Kolaboratif Oleh Kepala Sekolah Dalammeningkatkan Kualitas Pembelajarandisd Yari DwikurnaningsihKhalid Ibnu SinaNo ratings yet
- Ca-Cw106451-Mat-098 - Manga Termocontraible WoerDocument5 pagesCa-Cw106451-Mat-098 - Manga Termocontraible WoerJhoel Ipanaque AlarconNo ratings yet
- Daily PlatterDocument3 pagesDaily PlatterRajah KanoNo ratings yet
- S9 Safety Labeling For Electrical Equipment and Facilities ManagementDocument74 pagesS9 Safety Labeling For Electrical Equipment and Facilities Managementalfonzo.keilerNo ratings yet
- D197-Lab Exercise 2.2 - Bihay and SumaljagDocument5 pagesD197-Lab Exercise 2.2 - Bihay and Sumaljagjelly bihayNo ratings yet
- Acm 4 - B4-A1Document4 pagesAcm 4 - B4-A1Heru HaryantoNo ratings yet
- Conventional Transfer PumpsDocument15 pagesConventional Transfer PumpsNhocSkyzNo ratings yet
- RAMMINGDocument3 pagesRAMMINGmatheswaran a sNo ratings yet
- End-Of-Course Test (Word)Document4 pagesEnd-Of-Course Test (Word)los ikandasNo ratings yet
- Body MechanismDocument31 pagesBody MechanismAnnapurna DangetiNo ratings yet
- Turbine Gas G.T.G. 1Document17 pagesTurbine Gas G.T.G. 1wilsonNo ratings yet
- Testbank ch01Document14 pagesTestbank ch01HườngNo ratings yet
- Understand Trading in 2 Hours SteveRyanDocument63 pagesUnderstand Trading in 2 Hours SteveRyanAkash Biswal100% (3)
- SSP 666 Audi A8 Type 4N Infotainment and Audi ConnectDocument72 pagesSSP 666 Audi A8 Type 4N Infotainment and Audi Connectylk1No ratings yet