Professional Documents
Culture Documents
ISAYAMA 2017 - Revisiting The Definition of Bronchopulmonary Dysplasia
ISAYAMA 2017 - Revisiting The Definition of Bronchopulmonary Dysplasia
Uploaded by
Rafael JustinoCopyright:
Available Formats
You might also like
- Rapid Maxillary Expansion in Pediatric Patients With Obstructive Sleep Apnea - An Umbrella ReviewDocument9 pagesRapid Maxillary Expansion in Pediatric Patients With Obstructive Sleep Apnea - An Umbrella ReviewAly OsmanNo ratings yet
- WRIGHT 2016 - Continuous Positive Airway Pressure To Prevent Neonatal Lung InjuryDocument10 pagesWRIGHT 2016 - Continuous Positive Airway Pressure To Prevent Neonatal Lung InjuryRafael JustinoNo ratings yet
- Machine Learning To Predict Late Respiratory Support in Preterm Infants: A Retrospective Cohort StudyDocument9 pagesMachine Learning To Predict Late Respiratory Support in Preterm Infants: A Retrospective Cohort StudyNodi MNo ratings yet
- Displasia BroncopulmonarDocument12 pagesDisplasia BroncopulmonarRaul VillacresNo ratings yet
- Bronchopulmonary Dysplasia An Update On Experimental TherapeuticsDocument14 pagesBronchopulmonary Dysplasia An Update On Experimental TherapeuticsIván Gustavo Magaña CeballosNo ratings yet
- Lodha 2014Document12 pagesLodha 2014madhuNo ratings yet
- Mortality in Pediatric Acute Respiratory Distress Syndrome: A Systematic Review and Meta-AnalysisDocument9 pagesMortality in Pediatric Acute Respiratory Distress Syndrome: A Systematic Review and Meta-Analysisesya putrri oktareginaNo ratings yet
- FKT en Neonatos ChestDocument17 pagesFKT en Neonatos ChestSofia MandolaNo ratings yet
- Retrospective Analysis of Inpatient Polysomnogram Characteristics in Infants With Broncopulmonary DisplasiaDocument30 pagesRetrospective Analysis of Inpatient Polysomnogram Characteristics in Infants With Broncopulmonary DisplasiaJHONATAN MATA ARANDANo ratings yet
- Clouse 2016 RSLDocument18 pagesClouse 2016 RSLwisdom loverNo ratings yet
- Jurnal PediDocument13 pagesJurnal PediHansNo ratings yet
- Nejmoa 1708831Document10 pagesNejmoa 1708831Lissaberti AmaliahNo ratings yet
- Bassler 2018 Ensayo CohorteDocument10 pagesBassler 2018 Ensayo Cohortewisdom loverNo ratings yet
- Assessment of Postnatal Corticosteroids For The Prevention of BronchopulmonaryDocument19 pagesAssessment of Postnatal Corticosteroids For The Prevention of BronchopulmonaryFernando Guzmán VegaNo ratings yet
- BMJ n1974 FullDocument18 pagesBMJ n1974 FullErick HernandezNo ratings yet
- Bronchopulmonary Dysplasia Executive Summary of A 2018Document18 pagesBronchopulmonary Dysplasia Executive Summary of A 2018Raul VillacresNo ratings yet
- Modified Lung Ultrasound in Evaluating BPD at 36 WeeksDocument11 pagesModified Lung Ultrasound in Evaluating BPD at 36 WeeksArjun VermaNo ratings yet
- Prediction of Pneumonia in A Pediatric Emergency Department: PediatricsDocument10 pagesPrediction of Pneumonia in A Pediatric Emergency Department: PediatricsLeslie Lindsay AlvarezNo ratings yet
- JOBE 2016 - Surfactant Treatment For RDS Improves OxygenationDocument4 pagesJOBE 2016 - Surfactant Treatment For RDS Improves OxygenationRafael JustinoNo ratings yet
- Displasia BronkopulmonerDocument54 pagesDisplasia BronkopulmonerVivi DeviyanaNo ratings yet
- Study of Respiratory Distress in Newborn: International Journal of Contemporary Pediatrics March 2017Document6 pagesStudy of Respiratory Distress in Newborn: International Journal of Contemporary Pediatrics March 2017Elison J PanggaloNo ratings yet
- JurnalDocument6 pagesJurnalIzzyNo ratings yet
- 2174 8646 1 PBDocument5 pages2174 8646 1 PBKiran PantheeNo ratings yet
- Hemorragia PulmonarDocument11 pagesHemorragia PulmonarFer45No ratings yet
- BBLR 2Document8 pagesBBLR 2Radhiatul AdillahNo ratings yet
- Pi Is 1875957219305510Document10 pagesPi Is 1875957219305510madimadi11No ratings yet
- Venkataraman 2017 - Metaanálisis y RSLDocument8 pagesVenkataraman 2017 - Metaanálisis y RSLwisdom loverNo ratings yet
- Respiratory Pearls CombinedDocument7 pagesRespiratory Pearls CombinedVishal ParmarNo ratings yet
- 10 1002@ppul 24581Document6 pages10 1002@ppul 24581Roberto Guerrero MonsivaisNo ratings yet
- Dyke 2023 Ped Radiol PREFUL Lung MRI Ventilation NICUDocument9 pagesDyke 2023 Ped Radiol PREFUL Lung MRI Ventilation NICUJonathan DykeNo ratings yet
- Buonsenso Et Al-2018-Pediatric PulmonologyDocument9 pagesBuonsenso Et Al-2018-Pediatric Pulmonologywawa chenNo ratings yet
- Neonatal Outcomes of Extremely Preterm Infants From The NICHD Neonatal Research NetworkDocument14 pagesNeonatal Outcomes of Extremely Preterm Infants From The NICHD Neonatal Research NetworkKattia FloresNo ratings yet
- Nicu 1Document7 pagesNicu 1PPDS ANAK FK USUNo ratings yet
- Wright Et Al 2022 PDFDocument9 pagesWright Et Al 2022 PDFRadu CiprianNo ratings yet
- 2023 - Suplementación de Ácido Araquidónico y Docosaexanoico y Resultados Respiratorios en Infantes @wendelDocument7 pages2023 - Suplementación de Ácido Araquidónico y Docosaexanoico y Resultados Respiratorios en Infantes @wendelJorge Toshio Yazawa ChaconNo ratings yet
- Pxaa 116Document7 pagesPxaa 116Geísa VasconcelosNo ratings yet
- 2021 Predictors of Lung Function Trajectories in Population-Based Studies A Systematic ReviewDocument22 pages2021 Predictors of Lung Function Trajectories in Population-Based Studies A Systematic Reviewjose.maletNo ratings yet
- 3Document16 pages3marianaNo ratings yet
- S177 Full PDFDocument4 pagesS177 Full PDFCalvin AffendyNo ratings yet
- Advanced Proteomics and Cluster Analysis For Identifying Novel Obstructive Sleep Apnea Subtypes Before and After CPAP TherapyDocument34 pagesAdvanced Proteomics and Cluster Analysis For Identifying Novel Obstructive Sleep Apnea Subtypes Before and After CPAP Therapy马三强No ratings yet
- The Impact of A Dedicated Physiotherapist Clinic For Children With Dysfunctional BreathingDocument6 pagesThe Impact of A Dedicated Physiotherapist Clinic For Children With Dysfunctional BreathingKuro ShibaNo ratings yet
- Guidelines For Surfactant Replacement Therapy in NeonatesDocument7 pagesGuidelines For Surfactant Replacement Therapy in NeonatesFer45No ratings yet
- Canadian Guidelines 2021Document7 pagesCanadian Guidelines 2021Radu CiprianNo ratings yet
- 2024 - Appnoeic Oxygenation During Paediatric Tracheal Intubation A Systematic Review and Meta AnalysisDocument15 pages2024 - Appnoeic Oxygenation During Paediatric Tracheal Intubation A Systematic Review and Meta AnalysisPamela Mamani FloresNo ratings yet
- SPPRGG DescargarPDFDocument8 pagesSPPRGG DescargarPDFS ONo ratings yet
- Basic Principlies of Respiratory Function Monitoring in Ventilated NewornDocument8 pagesBasic Principlies of Respiratory Function Monitoring in Ventilated NewornNoe Perez GonzalezNo ratings yet
- Study of Different Treatment Modalities and Outcome in Preterm Babies With Respiratory Distress Syndrome 2017Document4 pagesStudy of Different Treatment Modalities and Outcome in Preterm Babies With Respiratory Distress Syndrome 2017Vita DesriantiNo ratings yet
- Resolving Our Uncertainty About Oxygen TherapyDocument7 pagesResolving Our Uncertainty About Oxygen TherapyAwadhNo ratings yet
- Epinephrine and Dexamethasone in Children With BronchiolitisDocument11 pagesEpinephrine and Dexamethasone in Children With BronchiolitisAdelina Wahyuni LubisNo ratings yet
- Adjunctive Therapies in Bronchopulmonary Dysplasia, NeoReview 2017Document9 pagesAdjunctive Therapies in Bronchopulmonary Dysplasia, NeoReview 2017Edrei Lopez CNo ratings yet
- Viral Respiratory Infections in Preterm Infants During andDocument9 pagesViral Respiratory Infections in Preterm Infants During andMariusNo ratings yet
- Clinical Controversies in Aerosol Therapy For Infants and ChildrenDocument23 pagesClinical Controversies in Aerosol Therapy For Infants and Childrencelma44No ratings yet
- Upper Airway Visualization in Pediatric Obstructive Sleep ApneaDocument20 pagesUpper Airway Visualization in Pediatric Obstructive Sleep ApneaDra. María José CastilloNo ratings yet
- Causes and Outcomes of Respiratory Distress in NeonatesDocument8 pagesCauses and Outcomes of Respiratory Distress in NeonatesMohammad AlmuhaiminNo ratings yet
- Risk Factors For Premenstrual Asthma. A Systematic Review and Meta-AnalysisDocument43 pagesRisk Factors For Premenstrual Asthma. A Systematic Review and Meta-Analysisrifka riskaNo ratings yet
- Displasia BroncopulmonarDocument4 pagesDisplasia BroncopulmonarRaul VillacresNo ratings yet
- Accepted Manuscript: Paediatric Respiratory ReviewsDocument16 pagesAccepted Manuscript: Paediatric Respiratory ReviewsAlvaro Guillen CerpaNo ratings yet
- Severity Scoring Systems: Are They Internally Valid, Reliable and Predictive of Oxygen Use in Children With Acute Bronchiolitis?Document7 pagesSeverity Scoring Systems: Are They Internally Valid, Reliable and Predictive of Oxygen Use in Children With Acute Bronchiolitis?Ivan VeriswanNo ratings yet
- SA PerformanceDocument8 pagesSA Performancefernin96No ratings yet
- Precision in Pulmonary, Critical Care, and Sleep Medicine: A Clinical and Research GuideFrom EverandPrecision in Pulmonary, Critical Care, and Sleep Medicine: A Clinical and Research GuideJose L. GomezNo ratings yet
- POLIN 2009 - Bubble CPAP - A Clash of Science Culture and ReligionDocument2 pagesPOLIN 2009 - Bubble CPAP - A Clash of Science Culture and ReligionRafael JustinoNo ratings yet
- MIEDEMA 2013 - Effect of Nasal Continuous and Biphasic Positive Airway Pressure On Lung Volume in Preterm InfantsDocument7 pagesMIEDEMA 2013 - Effect of Nasal Continuous and Biphasic Positive Airway Pressure On Lung Volume in Preterm InfantsRafael JustinoNo ratings yet
- GUPTA 2009 - A RCT of Post Extubation BCPAP Versus Infant Flow Driver CPAP in Preterm Infants With RDSDocument8 pagesGUPTA 2009 - A RCT of Post Extubation BCPAP Versus Infant Flow Driver CPAP in Preterm Infants With RDSRafael JustinoNo ratings yet
- ABIGAIL 2010 - Diffuse Alveolar HemorrhageDocument10 pagesABIGAIL 2010 - Diffuse Alveolar HemorrhageRafael JustinoNo ratings yet
- BURG 2014 - Cross-Sectional Changes in Lung Volume Measured by Electrical Impedance Tomography Are Representative For The Whole Lung in Ventilated Preterm InfantsDocument8 pagesBURG 2014 - Cross-Sectional Changes in Lung Volume Measured by Electrical Impedance Tomography Are Representative For The Whole Lung in Ventilated Preterm InfantsRafael JustinoNo ratings yet
- ORENSTEIN 2002 - Cystic Fibrosis - A 2002 UpdateDocument9 pagesORENSTEIN 2002 - Cystic Fibrosis - A 2002 UpdateRafael JustinoNo ratings yet
- NARASIMHAN - Pulmonary Haemorrhage in NeonatesDocument3 pagesNARASIMHAN - Pulmonary Haemorrhage in NeonatesRafael JustinoNo ratings yet
- HOUGH 2014 - Lung Recruitment and Endotracheal Suction in Ventilated Preterm Infants Measured With Electrical Impedance TomographyDocument7 pagesHOUGH 2014 - Lung Recruitment and Endotracheal Suction in Ventilated Preterm Infants Measured With Electrical Impedance TomographyRafael JustinoNo ratings yet
- NEWHOUSE 1999 - Asthma Therapy With AerosolsDocument4 pagesNEWHOUSE 1999 - Asthma Therapy With AerosolsRafael JustinoNo ratings yet
- BURG 2016 - Effect of Minimally Invasive Surfactant Therapy On Lung Volume and Ventilation in Preterm InfantsDocument6 pagesBURG 2016 - Effect of Minimally Invasive Surfactant Therapy On Lung Volume and Ventilation in Preterm InfantsRafael JustinoNo ratings yet
- BIBAN 2012 - Exogenous Surfactant Replacement - How To Deliver ItDocument6 pagesBIBAN 2012 - Exogenous Surfactant Replacement - How To Deliver ItRafael JustinoNo ratings yet
- ALVIRA 2017 - Can We Understand The Pathobiology of Bronchopulmonary DysplasiaDocument11 pagesALVIRA 2017 - Can We Understand The Pathobiology of Bronchopulmonary DysplasiaRafael JustinoNo ratings yet
- MIEDEMA 2011 - Changes in Lung Volume and Ventilation During Surfactant Treatment in Ventilated Preterm InfantsDocument6 pagesMIEDEMA 2011 - Changes in Lung Volume and Ventilation During Surfactant Treatment in Ventilated Preterm InfantsRafael JustinoNo ratings yet
- Ultrasound in Obstet Gyne - 2002 - Laudy - The Fetal Lung 1 Developmental AspectsDocument7 pagesUltrasound in Obstet Gyne - 2002 - Laudy - The Fetal Lung 1 Developmental AspectsRafael JustinoNo ratings yet
- LISTA 2012 - Surfactant and Mechanical VentilationDocument3 pagesLISTA 2012 - Surfactant and Mechanical VentilationRafael JustinoNo ratings yet
- Neuroprotective MgSO4Document6 pagesNeuroprotective MgSO4Rafael JustinoNo ratings yet
- SOLALIGUE 2017 - 1 Recent Advances in Our Understanding of The Mechanisms of Late Lunf Development and BPDDocument190 pagesSOLALIGUE 2017 - 1 Recent Advances in Our Understanding of The Mechanisms of Late Lunf Development and BPDRafael JustinoNo ratings yet
- Ca 27 29Document2 pagesCa 27 29डा. सत्यदेव त्यागी आर्यNo ratings yet
- Snake Bite National Protocol PediatricsDocument45 pagesSnake Bite National Protocol Pediatricsarjun_paulNo ratings yet
- ADA Guideline - Chronic Kidney Disease Evidence-Based Nutrition Practice GuidelineDocument19 pagesADA Guideline - Chronic Kidney Disease Evidence-Based Nutrition Practice GuidelineJorge SánchezNo ratings yet
- Centric and Eccentric OcclusionsDocument8 pagesCentric and Eccentric OcclusionsYan Lau100% (1)
- Feline Pyometra and Its Surgical Management: A Case: Received: 30.03.2021 Accepted: 13.04.2021Document5 pagesFeline Pyometra and Its Surgical Management: A Case: Received: 30.03.2021 Accepted: 13.04.2021dewaNo ratings yet
- EMNoteDocument1 pageEMNoteKC Dela RosaNo ratings yet
- Dentists CADocument44 pagesDentists CABruce AmigoNo ratings yet
- Medical Skills Physical ExamDocument150 pagesMedical Skills Physical Examsholay100% (1)
- ENEMADocument3 pagesENEMAdenNo ratings yet
- Website Advt EnglishDocument7 pagesWebsite Advt EnglishsapnaNo ratings yet
- Forensic MedicineDocument7 pagesForensic MedicineAlta Sofia CriminologyNo ratings yet
- Promoting Personal Hygiene & Promoting Rest & SleepDocument26 pagesPromoting Personal Hygiene & Promoting Rest & SleepYousef JafarNo ratings yet
- Difficulty in Hearing: Prepared By: Francis Quarre Lyka Jane Roguel John Lester Romero Alana Marees DolosoDocument31 pagesDifficulty in Hearing: Prepared By: Francis Quarre Lyka Jane Roguel John Lester Romero Alana Marees DolosoJessa Mae SusonNo ratings yet
- Penicillin G Benza Drug StudyDocument2 pagesPenicillin G Benza Drug StudyRussel Kate SulangNo ratings yet
- List of Nursing Abbreviations and Acronyms 1Document5 pagesList of Nursing Abbreviations and Acronyms 1Jay Debby RuizoNo ratings yet
- Product InformationDocument80 pagesProduct InformationElla LiuNo ratings yet
- Hyperuricemia XXXX XXXXX XxjeuneDocument32 pagesHyperuricemia XXXX XXXXX XxjeuneOziq Juga ReMa-eNo ratings yet
- Programa Aua San Francisco 2018Document76 pagesPrograma Aua San Francisco 2018Rosemary FranquizNo ratings yet
- Extraordinary Vessel PointsDocument3 pagesExtraordinary Vessel PointsIhes HesNo ratings yet
- PODCAST #67 DR.B The Vet Show - Drh. Syavira EkdhiasmaraDocument26 pagesPODCAST #67 DR.B The Vet Show - Drh. Syavira EkdhiasmaraLailatun NafisahNo ratings yet
- Report On Term Paper Presentation-Ii Artificial Vision-A Bionic EyeDocument7 pagesReport On Term Paper Presentation-Ii Artificial Vision-A Bionic Eye3nadhsNo ratings yet
- Virus ClassificationDocument2 pagesVirus ClassificationJoshua PrinceNo ratings yet
- So You Want To Be A Urologist?: The First StepDocument2 pagesSo You Want To Be A Urologist?: The First StepDrThamma ShahiNo ratings yet
- Price ALL Z-VentDocument9 pagesPrice ALL Z-VentPanco NanaNo ratings yet
- HydrocephalusDocument39 pagesHydrocephalusspiritNo ratings yet
- TRM03.01 Cervical Spine Guideline V5.0 - 12.17Document6 pagesTRM03.01 Cervical Spine Guideline V5.0 - 12.17Alexandria Firdaus Al-farisyNo ratings yet
- Genital Tract InfectionsDocument4 pagesGenital Tract Infectionsmed.progressNo ratings yet
- Important Questions For Esic Staff Nurse Recruitment ExamDocument4 pagesImportant Questions For Esic Staff Nurse Recruitment ExamSuchitaNo ratings yet
- Endodontics ObturationDocument8 pagesEndodontics ObturationShameer Parambil100% (2)
- 2011 Risk Score To Hospitalized Patients For Clinical Pharmacy RationalizationDocument6 pages2011 Risk Score To Hospitalized Patients For Clinical Pharmacy RationalizationIgnacio NamuncuraNo ratings yet
ISAYAMA 2017 - Revisiting The Definition of Bronchopulmonary Dysplasia
ISAYAMA 2017 - Revisiting The Definition of Bronchopulmonary Dysplasia
Uploaded by
Rafael JustinoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
ISAYAMA 2017 - Revisiting The Definition of Bronchopulmonary Dysplasia
ISAYAMA 2017 - Revisiting The Definition of Bronchopulmonary Dysplasia
Uploaded by
Rafael JustinoCopyright:
Available Formats
Research
JAMA Pediatrics | Original Investigation
Revisiting the Definition of Bronchopulmonary Dysplasia
Effect of Changing Panoply of Respiratory Support
for Preterm Neonates
Tetsuya Isayama, MD; Shoo K. Lee, MBBS, PhD; Junmin Yang, MSc; David Lee, MD; Sibasis Daspal, MD;
Michael Dunn, MD; Prakesh S. Shah, MD, MSc; for the Canadian Neonatal Network and Canadian Neonatal
Follow-Up Network Investigators
Supplemental content
IMPORTANCE Several definitions of bronchopulmonary dysplasia are clinically used; however,
their validity remains uncertain considering ongoing changes in the panoply of respiratory
support treatment strategies used within neonatal units.
OBJECTIVE To identify the optimal definition of bronchopulmonary dysplasia that best
predicts respiratory and neurodevelopmental outcomes in preterm infants.
DESIGN, SETTING, AND PARTICIPANTS Retrospective cohort study at tertiary neonatal
intensive care units. Preterm infants born at less than 29 weeks’ gestation between 2010 and
2011 who were admitted to neonatal intensive care units participating in the Canadian
Neonatal Network and completed follow-up assessments in a Canadian Neonatal Follow-Up
Network clinic at 18 to 21 months.
EXPOSURES Various traditional bronchopulmonary dysplasia criteria based on respiratory
status at different postmenstrual ages.
MAIN OUTCOMES AND MEASURES Serious respiratory morbidity, neurosensory impairment at
18 to 21 months of age, and a composite outcome of respiratory or neurosensory morbidity or
death after discharge. Adjusted odds ratios (AORs) and 95% CIs were calculated.
RESULTS Of 1914 eligible survivors, 1503 were assessed (mean gestational age was 26.3
weeks; 68% were white, 9% were black, and 23% were other race/ethnicity), 88 had serious
respiratory morbidity, 257 infants had neurosensory impairment, and 12 infants died after
discharge. Definitions using oxygen requirement alone as the criterion at various
postmenstrual ages were less predictive compared with those using the criterion of
oxygen/respiratory support (RS) (receiving supplemental oxygen and/or positive-pressure
RS); among those, oxygen/RS at 36 weeks had the highest AOR and area under the curve
(AUC) for all outcomes. Further analyses of oxygen/RS at each week between 34 and 44
weeks’ postmenstrual age indicated that the predictive ability for serious respiratory
morbidity increased from 34 weeks (AOR, 1.8; 95% CI, 0.9-3.4, AUC, 0.721) to 40 weeks
(AOR, 6.1; 95% CI, 3.4-11.0; AUC, 0.799). For serious neurosensory impairment, the AOR and
AUC at 40 weeks’ PMA (AOR, 1.5, 95% CI, 1.0-2.1; AUC, 0.740) were only marginally below
their peak values at 37 weeks’ PMA (AOR, 1.8; 95% CI, 1.3-2.6; AUC, 0.743). Author Affiliations: Author
affiliations are listed at the end of this
article.
CONCLUSIONS AND RELEVANCE Defining bronchopulmonary dysplasia by the use of oxygen
Group Information: Investigators of
alone is inadequate because oxygen/RS is a better indicator of chronic respiratory the Canadian Neonatal Network and
insufficiency. In particular, oxygen/RS at 40 weeks’ PMA was identified as the best predictor Canadian Neonatal Follow-Up
for serious respiratory morbidity, while it also displayed a good ability to predict neurosensory Network are listed at the end of the
article.
morbidity at 18 to 21 months.
Corresponding Author: Prakesh S.
Shah, MD, MSc, Department of
Pediatrics, 19-231F, 600 University
Ave, Toronto, ON M5G 1X5, Canada,
JAMA Pediatr. doi:10.1001/jamapediatrics.2016.4141 (prakeshkumar.shah
Published online January 23, 2017. @sinaihealthsystem.ca).
(Reprinted) E1
Copyright 2017 American Medical Association. All rights reserved.
Downloaded From: http://archpedi.jamanetwork.com/pdfaccess.ashx?url=/data/journals/peds/0/ on 01/24/2017
Research Original Investigation Bronchopulmonary Dysplasia Definitions and Outcomes
B
ronchopulmonary dysplasia (BPD) is an important
morbidity in preterm infants that has short- and Key Points
long-term serious adverse consequences for infants,
Question What is the optimal definition of bronchopulmonary
their families, and the health care system.1-3 Approximately dysplasia that best predicts respiratory and neurodevelopmental
45% of preterm infants born at less than 29 weeks’ gestation outcomes in preterm infants and the postmentstrual age
are diagnosed as having BPD.4 While accurate and timely associated with the best predictive characteristics for serious
diagnosis of the condition is important to identify high-risk adverse respiratory or neurosensory outcomes?
infants in need of surveillance or special support, preva- Findings In this cohort study, receipt of supplemental oxygen
lence of BPD has also been proven to be a valuable short- and/or positive-pressure respiratory support at 40 weeks’
term indicator for benchmarking the quality of neonatal postmentstrual age was identified as the best predictor for serious
care provided by institutions, networks, and countries.4 respiratory morbidity and displayed a good ability to predict
The term bronchopulmonary dysplasia was coined by neurosensory morbidity at 18 to 21 months.
Northway et al5 in 1967 to describe a chronic pulmonary Meaning Defining BPD by the use of oxygen alone is inadequate
condition observed in infants with respiratory distress syn- because oxygen and/or positive-pressure respiratory support is a
drome and treated with high oxygen concentration and better indicator of chronic respiratory insufficiency.
mechanical ventilation, but it has since undergone numer-
ous revisions to accommodate different criteria.5 In 1978, a
clinical definition based on the dependency on oxygen at 30 Methods
days or 1 month of age with any radiographic abnormality
was proposed 6 and widely used. In 1988, Shennan et al 7 Study Population and Data Collection
reported that oxygen use at 36 weeks’ postmenstrual age This retrospective cohort study included preterm infants born
(PMA) had a higher accuracy for predicting long-term respi- at less than 29 weeks’ gestation from January 2010 to Septem-
ratory problems than that at 28 days of age or other PMAs, ber 2011 who were admitted to tertiary NICUs participating in
which has become the most commonly used measure to the Canadian Neonatal Network. Those surviving until dis-
define BPD.8 In 2001, a workshop held by the National Insti- charge or transferred to step-down units and followed up in
tutes of Health proposed to define BPD as oxygen use for 28 affiliated clinics participating in the Canadian Neonatal Fol-
days and categorized BPD into 3 severity levels (mild, mod- low-Up Network were included. We excluded infants who had
erate, and severe) based on oxygen use and/or respiratory major congenital anomalies or were discharged or trans-
support at 36 weeks’ PMA (or 56 days of age for infants at ferred to step-down units before 34 weeks’ PMA. Maternal and
≥32 weeks’ gestational age).9 An oxygen reduction test was infant data were collected by trained data abstractors based
also recommended to confirm physiologic al oxygen on the Canadian Neonatal Network abstractor’s manual.14 All
requirement.10,11 26 Canadian Neonatal Follow-Up Network clinics provided fol-
The validity of these BPD definitions based on respira- low-up data for this study, making up approximately 80% of
tory status at 36 weeks’ PMA is uncertain because there neonates younger than 29 weeks’ gestation in 28 of 30 ter-
have been substantial changes in the perinatal and neonatal tiary NICUs in Canada. Experienced and trained health care
management of preterm infants since the single-center professionals obtained medical histories by interviews and con-
study by Shennan et al,7 particularly in respiratory support ducted physical and neurological examinations of children at
modalities available for preterm neonates.12 This concern is 18 to 21 months of corrected age at Canadian Neonatal Fol-
particularly relevant because many previous studies used low-Up Network clinics as previously described.15
the Shennan et al definition8 and therefore did not capture This study was approved by the research ethics board of
infants who might be on noninvasive respiratory support Mount Sinai Hospital, Toronto. Neonatal data were collected
but in room air, a situation that is not infrequent in modern- retrospectively after approval from ethics or quality improve-
day neonatal intensive care units (NICUs). Although the ment committee at each unit without direct consent to en-
National Institutes of Health definition 13 incorporated sure data collection of all neonates. For follow-up data, indi-
respiratory support in room air to define severe BPD vidual written consent was obtained from parents when they
while also requiring oxygen use for 28 days after birth presented for assessment in clinics.
for BPD diagnosis, the validity of doing so has yet to be
determined. Definitions Compared
Here, we compared various traditional BPD criteria used Respiratory support (RS) was defined as the use of any me-
in the literature to identify the best definition predictive of chanical ventilation or noninvasive respiratory support that
serious long-term adverse respiratory or neurosensory out- provides positive end-expiratory pressure including continu-
comes in preterm infants less than 29 weeks’ gestation in a ous positive airway pressure, biphasic continuous positive air-
large, population-based cohort. Using this definition, we way pressure, high flow of air or oxygen (>1.5 L/min), nonin-
conducted sensitivity analyses for the entire range of vasive intermittent positive pressure ventilation, and
infants between 34 and 44 weeks of PMA, with the aim to noninvasive high-frequency oscillation. Six different criteria
identify the PMA associated with the best predictive charac- for classifying neonates with BPD were identified: (1) oxygen
teristics for serious adverse respiratory or neurosensory at 28 days of age, (2) receiving supplemental oxygen and/or re-
outcomes. spiratory positive-pressure support (oxygen/RS) at 28 days of
E2 JAMA Pediatrics Published online January 23, 2017 (Reprinted) jamapediatrics.com
Copyright 2017 American Medical Association. All rights reserved.
Downloaded From: http://archpedi.jamanetwork.com/pdfaccess.ashx?url=/data/journals/peds/0/ on 01/24/2017
Bronchopulmonary Dysplasia Definitions and Outcomes Original Investigation Research
age, (3) oxygen at 36 weeks’ PMA, (4) oxygen/RS at 36 weeks’ with long-term outcomes adjusting for potential confound-
PMA, (5) oxygen at 28 days and oxygen/RS at 36 weeks’ ers. The areas under the receiver operating characteristic
PMA, and (6) oxygen/RS at 28 days of age and at 36 weeks’ curves (AUCs) of the regression models were calculated for
PMA. Once the best measure among these 6 definitions was each BPD definition.22 Area under the curve indicates the
identified, sensitivity analyses were conducted to identify predictive ability for discrimination, a quality that expresses
the PMA at which the particular measure would perform how well prediction models discriminate between patients
best for the prediction of serious adverse respiratory and with and without the outcomes of interest. 22 The AUC
neurosensory outcomes. was used to select the best regression model to predict
outcomes.23 Furthermore, modified versions of the best tra-
Outcomes ditional BPD definition (defined at different PMAs between
Three long-term adverse outcomes were assessed including se- 34-44 weeks) were evaluated by logistic regression analyses
rious respiratory morbidity, serious neurosensory impair- to decide the best timing of the assessment of respiratory
ment, and a composite outcome of serious respiratory mor- status based on the associations with outcomes and the
bidity and/or neurosensory impairment at 18 to 21 months AUC. Sensitivity, specificity, and positive or negative predic-
corrected age or death after NICU discharge and prior to 21 tive values of BPD definitions for predicting long-term out-
months corrected age. Serious respiratory morbidity was de- comes were also calculated.
fined as either (1) 3 or more rehospitalizations after NICU dis- Infants who were discharged or transferred to step-
charge owing to respiratory problems (infectious or noninfec- down units without oxygen and without respiratory support
tious); (2) having a tracheostomy; (3) using respiratory between 34 and 44 weeks’ PMA were assumed to not
monitoring or support devices at home such as an apnea moni- require oxygen or respiratory support post-discharge or
tor or pulse oximeter; and (4) being on home oxygen or con- post-transfer. Infants who were discharged home using
tinuous positive airway pressure at the time of assessment either oxygen or respiratory support were considered to use
between 18 and 21 months corrected age.16 At least 3 rehos- oxygen/RS the week following discharge. If infants were
pitalizations was chosen because the 95th percentile of the transferred to step-down units using either oxygen or respi-
number of readmissions owing to respiratory problems in ratory support, their oxygen use and RS were considered
this cohort was 2 (which could be considered within normal unknown after the week of transfer. To assess the effect of
limits). Neurosensory impairment was defined as having these inclusion/exclusion criteria of infants discharged or
any of the following: (1) moderate to severe cerebral palsy transferred between 34 and 40 weeks’ PMA, 2 sensitivity
(Gross Motor Function Classification System ≥3)17; (2) severe analyses were conducted assuming that (1) infants dis-
developmental delay (Bayley Scales of Infant and Toddler charged home on oxygen/RS were excluded from the analy-
Development Third Edition [Bayley III] composite score <70 ses after the week of discharge or (2) infants who trans-
in either cognitive, language, or motor domains)18; (3) hear- ferred to step-down units on oxygen/RS were considered
ing aid or cochlear implant use; and (4) bilateral severe using oxygen/RS after the week of transfer. We limited our
visual impairment.16 assessment up until 44 weeks’ PMA because neonates older
than 44 weeks are a very selective group of neonates with
Covariates additional complications necessitating their prolonged hos-
Covariates known to affect outcomes included maternal pital stay. All statistical analyses were conducted using SAS,
age, hypertension, antenatal steroids, delivery mode, mul- version 9.3 (SAS Institute Inc).
tiple births, sex, gestational age at birth, birth weight, small
for gestational age (birth weight <10th percentile), 5-minute
Apgar score less than 4, Score for Neonatal Acute Physiol-
ogy II score 19 greater than 20, severe cerebral injuries
Results
defined as having severe intraventricular hemorrhage Among 2760 infants at younger than 29 weeks’ gestational
(grade 3 or 4, based on the Papile et al grading),20 and/or age admitted to Canadian Neonatal Network NICUs during
periventricular leukomalacia, necrotizing enterocolitis the study period, 1914 infants were eligible for this study
(stage 2 or higher based on Bell criteria21), patent ductus (Figure 1). After excluding 411 infants (21%) without
arteriosus requiring surgical or medical treatment, late- follow-up data, 1503 infants were included. The proportion
onset sepsis (isolation of a pathogenic organism in blood or of infants using oxygen/RS decreased from 63% to 9% from
cerebrospinal fluid in a symptomatic neonate after 2 days of 34 to 44 weeks’ PMA (eFigure 1 in the Supplement). A total
age), maternal race/ethnicity (white, black, and others), and of 321 infants (21%) had a composite outcome of respiratory
maternal education (completing college or higher). morbidity and/or neurosensory impairment or death after
discharge at 18 to 21 months’ corrected age, among which 12
Statistical Analyses infants (1%) died after initial discharge, 88 infants (6%) had
Covariates were compared between infants with and with- serious respiratory morbidity, and 257 infants (17%) had
out serious respiratory morbidity or neurosensory impair- serious neurosensory impairment (Table 1). Table 2 shows
ment using the χ2 test or t test as appropriate. Initially, mul- maternal and infant characteristics of neonates with or
tiple logistic regression models were developed to assess without serious respiratory morbidity or neurosensory
the association between the 6 traditional BPD definitions impairment. Infants of lower birth weight and gestational
jamapediatrics.com (Reprinted) JAMA Pediatrics Published online January 23, 2017 E3
Copyright 2017 American Medical Association. All rights reserved.
Downloaded From: http://archpedi.jamanetwork.com/pdfaccess.ashx?url=/data/journals/peds/0/ on 01/24/2017
Research Original Investigation Bronchopulmonary Dysplasia Definitions and Outcomes
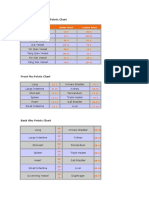
Figure 1. Study Population Table 1. Adverse Long-Term Outcomes Among the Study Population at 18
to 21 Months of Corrected Age
2760 Neonates <29 wk admitted to Outcome No. (%)
participating sites in the CNN
during study period Serious respiratory morbidity 88 (6)
47 Moribund infants ≥3 Rehospitalizations owing to respiratory problems 58 (4)
119 Major congenital anomalies
Use of respiratory monitoring or support devices 44 (3)
409 Discharge/death
Serious neurosensory impairment 257 (17)
2185 Infants survived
Moderate to severe cerebral palsy, GMFCS ≥3 91 (6)
271 Tranferred before 34 wk with
oxygen/RS Bayley-III<70 in cognitive, language, or motor 208 (14)
Bayley-III composite score
1914 Eligible infants
<70 in cognitive 47 (3)
411 No follow-up data <70 in language 157 (11)
<70 in motor 87 (6)
1503 Follow-up data available from follow-up network sites Hearing aid or cochlear implant 35 (2)
Bilateral severe visual impairment 20 (1)
CNN indicates Canadian Neonatal Network and Oxygen/RS indicates receiving Death after initial discharge 12 (1)
supplemental oxygen and/or respiratory positive-pressure support.
Composite outcomea 321 (21)
Abbreviation: GMFCS, Gross Motor Function Classification System.
a
Composite outcome was defined as serious respiratory morbidity and/or
age were more likely to display serious respiratory morbid- neurosensory impairment at 18 to 21 months corrected age, or death after
ity (mean birth weight, 777 g vs 933 g; mean gestational age, neonatal intensive care unit discharge before 21 months corrected age.
25.3 weeks vs 26.3 weeks; P < .001) and neurosensory
impairment (mean birth weight, 861 g vs 944 g; mean gesta-
tional age, 25.8 weeks vs 26.4 weeks; P < .001). Discussion
Infants with oxygen/RS at 28 days or 34 to 44 weeks’
PMA had a higher likelihood of all long-term adverse out- In this large retrospective study with comprehensive evalua-
comes (Figures 2 and 3). Four of 6 traditional BPD defini- tion of respiratory and neurosensory impairment, we deter-
tions were significantly associated with all the 3 long-term mined that oxygen/RS at 36 weeks’ PMA was the best among
adverse outcomes after adjusting for potential confounders all contemporary definitions of BPD to predict serious severe
(Figure 2). Among them, the definition of oxygen/RS at 36 respiratory morbidity at 18 to 21 months corrected age with the
weeks’ PMA displayed the highest predictive values for seri- highest AUC. Moreover, oxygen/RS at 40 weeks’ PMA was most
ous respiratory morbidity and neurosensory impairment, strongly associated with serious respiratory outcome among
suggesting oxygen requirement alone was not adequate cri- those at each of 34 to 44 weeks’ PMA. For serious neurosen-
teria. Based on this finding, subsequent analyses focused on sory impairment and composite outcome, variations in pre-
oxygen/RS at various PMAs between 34 and 44 weeks. diction ability and strength of association with oxygen/RS at
As the PMA for the assessment of oxygen/RS increased, the 34 to 44 weeks’ PMA were marginal, with oxygen/RS at 37 to
specificity and positive predictive values increased while the 40 weeks’ PMA resulting in similar estimates.
sensitivity decreased. Changes in negative predictive values Several studies have evaluated accuracy or predictive abil-
were minimal (eFigure 2 in the Supplement). In most cases, ity of various diagnostic criteria of BPD for long-term adverse
oxygen/RS at 34 to 44 weeks’ PMA was significantly associ- respiratory outcomes. The original Shennan et al study7 evalu-
ated with adverse outcomes (Figure 3). For serious respira- ated the diagnostic accuracy of oxygen use at 31 to 38 weeks’
tory morbidity, the adjusted odds ratio (AOR) estimates in- PMA for predicting adverse respiratory outcomes in the first
creased from 34 to 40 weeks’ PMA and decreased after 40 2 years of life. Oxygen use at 36 weeks’ PMA had the highest
weeks’ PMA (Figure 3). The AUC also increased from 34 to 40 accuracy of 85%, with a sensitivity of 63% and specificity of
weeks’ PMA, from 0.721 to 0.799, and peaked at 40 weeks’ PMA 91%. The validity of this finding was limited by the fact that
(Figure 3). For neurosensory impairment, the AORs and AUCs (1) it was a single-center study that may not have been an ac-
between 34 and 44 weeks’ PMA were less different and those curate representation of the general preterm infant popula-
at 40 weeks’ PMA (AOR, 1.5; 95% CI, 1.0-2.1; AUC, 0.740) were tion, (2) the respiratory management strategies have been
only marginally below their peak values at 37 weeks’ PMA (AOR, changed since then, and (3) it only evaluated long-term ad-
1.8; 95% CI, 1.3-2.6; AUC, 0.743). Marginal variations were also verse respiratory outcomes and not neurodevelopmental im-
observed for the composite outcome (AOR estimates, 1.6-2.3 pairment. Davis et al24 reported that the diagnostic accuracy
and AUC, 0.724-0.746). Two sensitivity analyses uncovered of oxygen use at 36 weeks’ PMA for predicting poor respira-
similar results: the AOR and AUC peaked at 40 weeks’ PMA for tory outcome before 18 months of corrected age (63%) was simi-
serious respiratory morbidity and displayed minimal in- lar to those at other PMAs between 32 and 40 weeks in a co-
creases for serious neurosensory impairment or the compos- hort from a multicenter trial. In contrast, our study revealed
ite outcome between 34 and 44 weeks’ PMA (eTables 1 and 2 that the AUC of oxygen/RS at 34 to 44 weeks’ PMA for predict-
in the Supplement). ing long-term serious respiratory morbidity was highest at 40
E4 JAMA Pediatrics Published online January 23, 2017 (Reprinted) jamapediatrics.com
Copyright 2017 American Medical Association. All rights reserved.
Downloaded From: http://archpedi.jamanetwork.com/pdfaccess.ashx?url=/data/journals/peds/0/ on 01/24/2017
Bronchopulmonary Dysplasia Definitions and Outcomes Original Investigation Research
Table 2. Maternal and Infant Characteristics
No. (%)
No Serious No Serious
Respiratory Serious Respiratory Neurosensory Serious Neurosensory
All Infants Morbidity Morbidity Impairment Impairment
Characteristics (n = 1503) (n = 1459) (n = 44) P Value (n = 1230) (n = 257) P Value
Maternal age, 30.7 (6) 30.7 (5.9) 30.8 (5.0) .88 30.8 (5.9) 30.2 (5.8) .12
mean (SD), y
Hypertensive disorders of 267 (18) 262 (18.2) 5 (11.4) .24 216 (17.8) 48 (19.0) .67
pregnancy
Antenatal steroids 1349 (92) 1310 (91.6) 39 (90.7) .83 1112 (92.2) 222 (88.5) .05
Rupture of membrane 325 (22) 314 (22.0) 11 (25.6) .58 173 (22.7) 50 (19.9) .34
>24 h
Chorioamnionitis 320 (27) 303 (26.2) 17 (48.6) <.001 261 (26.7) 55 (27.4) .84
Multiple birth 415 (28) 404 (27.7) 11 (25.0) .69 342 (27.8) 65 (25.3) .41
Cesarean section 876 (58) 850 (58.4) 26 (59.1) .93 721 (58.8) 145 (56.4) .48
Race/ethnicity
White 853 (68) 829 (67.9) 24 (60.0) 730 (69.7) 123 (57.8)
Black 112 (9) 108 (8.9) 4 (10.0) .56 83 (7.9) 29 (13.6) <.001
Other 296 (23) 284 (23.3) 12 (30.0) 235 (22.4) 61 (28.6)
Maternal education, 729 (53) 707 (53.2) 22 (55.0) .82 624 (54.6) 104 (46.0) .02
≥complete college
Male 775 (52) 750 (51.4) 25 (58.1) .39 606 (49.3) 162 (63.3) <.001
Gestational age, mean 26.3 (1) 26.3 (1.4) 25.3 (1.4) <.001 26.4 (1.4) 25.8 (1.5) <.001
(SD), wk
Birth weight, mean (SD), g 929 (226) 933 (225) 777 (169) <.001 944 (225) 861 (213) <.001
Small for gestational age 116 (8) 111 (7.6) 5 (11.6) .33 92 (7.5) 22 (8.6) .55
SNAP II score >20 410 (27) 387 (26.6) 23 (54.8) <.001 293 (23.9) 109 (42.9) <.001
Severe cerebral injuries 160 (11) 153 (10.6) 7 (16.7) .21 90 (7.4) 68 (26.7) <.001
Necrotizing enterocolitis 120 (8) 112 (7.7) 8 (19.1) .01 84 (6.8) 34 (13.3) <.001
Patent ductus arteriosus 903 (60) 868 (59.6) 35 (83.3) <.001 712 (58.0) 179 (69.9) <.001
Late onset sepsis 429 (29) 410 (28.1) 19 (43.2) .03 313 (25.5) 109 (42.4) <.001
Abbreviation: SNAP, Score for Neonatal Acute Physiology.
weeks. These differences may be owing to variations in cri- for neurosensory impairment. Davis et al24 reported that the
teria for adverse respiratory outcomes, as well as differ- accuracy of oxygen use at 32 to 40 weeks’ PMA for predicting
ences in indices used (accuracy vs AUC). Unlike our study, neurosensory impairment at 18 months of corrected age in-
these previous studies included oxygen use at 40 weeks’ creased as the PMA for assessment increased (accuracy from
PMA or at discharge as a component of long-term adverse 54% for the assessment at 32 weeks’ PMA to 68% for that at
respiratory outcomes that did not necessarily reflect func- 40 weeks’ PMA). However, unlike our study, they did not ad-
tionally important problems at follow-up. Furthermore, just for important confounders.24 Given that other major mor-
they also included 1 or more, or more than 1, admissions as bidities, such as severe cerebral injuries, necrotizing entero-
long-term adverse respiratory outcomes, in contrast to our colitis, and sepsis, are associated with both BPD and
study in which at least 3 admissions were required to be neurosensory impairment,13,25 adjustment for these poten-
classified as serious respiratory morbidity. A validation tial confounders is critical for evaluating the independent as-
study of the National Institutes of Health BPD definition sociation and predictive ability of BPD for neurosensory im-
revealed a greater association between BPD and long-term pairment.
respiratory adverse outcomes as the severity of BPD This study is marked by several strengths. First, the study
increased.13 The study also reported significant associations cohort had a large sample size and contained a nearly popu-
between other various BPD definitions and long-term lation-based sample from Canada. Second, this study as-
adverse respiratory outcomes. However, unlike our study, it sessed not only the commonly used traditional BPD defini-
did not assess the predictive ability of these BPD definitions tions but also other promising alternatives including oxygen/RS
and did not evaluate the timing of the assessment of respi- at each PMA between 34 and 44 weeks. Third, the adjust-
ratory status other than at 28 days of age and 36 weeks’ ment for potential confounders, including major neonatal mor-
PMA.13 bidities, enabled us to evaluate independent predictive abili-
Our study confirmed the significant association between ties of oxygen/RS at various PMAs using AUCs of logistic
BPD and neurosensory impairment that was previously regression models. Finally, the sensitivity analyses con-
reported.1-3,25 Thus far, few groups have assessed the associa- firmed the robustness of the findings, especially for serious re-
tion or predictive ability of oxygen use or RS at various PMAs spiratory morbidity.
jamapediatrics.com (Reprinted) JAMA Pediatrics Published online January 23, 2017 E5
Copyright 2017 American Medical Association. All rights reserved.
Downloaded From: http://archpedi.jamanetwork.com/pdfaccess.ashx?url=/data/journals/peds/0/ on 01/24/2017
Research Original Investigation Bronchopulmonary Dysplasia Definitions and Outcomes
Figure 2. Associations of 6 Traditional Bronchopulmonary Dysplasia (BPD) Definitions With Adverse Outcomes at 18 to 21 Months of Age
A Serious respiratory morbidity
Adverse Outcome Adverse Outcome
Traditional BPD Definitions in BPD (+) Infants in BPD (−) Infants AOR (95% CI)a
Oxygen, 28 d 71/893 (8.0) 17/513 (3.3) 1.3 (0.7-2.4) 0.72
Oxygen/RS, 28 d 81/1123 (7.2) 7/283 (2.5) 1.9 (0.7-5.0) 0.721
Oxygen, 28 d and Oxygen/RS 36 wk PMA 62/579 (10.7) 26/827 (3.1) 2.4 (1.4-4.2) 0.735
Oxygen/RS, 28 d and 36 wk PMA 66/620 (10.7) 22/786 (2.8) 2.9 (1.6-5.2) 0.743
Oxygen, 36 wk PMA 61/548 (11.1) 27/858 (3.2) 2.6 (1.5-4.4) 0.742
Oxygen/RS 36 wk PMA 69/652 (10.6) 19/754 (2.5) 3.4 (1.8-6.3) 0.75
0.5 1 2 5 10 0.71 0.73 0.75 0.77
AOR (95% CI) AUC
B Serious neurosensory impairment
Adverse Outcome Adverse Outcome
Traditional BPD Definitions in BPD (+) Infants in BPD (−) Infants AOR (95% CI)a
Oxygen, 28 d 192/892 (21.5) 55/511 (10.8) 1.3 (0.9-1.9) 0.729
Oxygen/RS, 28 d 217/1120 (19.4) 30/283 (10.6) 1.1 (0.7-1.8) 0.729
Oxygen, 28 d and Oxygen/RS 36 wk PMA 145/578 (25.1) 102/825 (12.4) 1.6 (1.1-2.2) 0.733
Oxygen/RS, 28 d and 36 wk PMA 153/619 (24.7) 94/784 (12.0) 1.7 (1.2-2.4) 0.737
Oxygen, 36 wk PMA 134/547 (24.5) 113/856 (13.2) 1.7 (1.2-2.3) 0.736
Oxygen/RS 36 wk PMA 158/651 (24.3) 89/752 (11.8) 1.7 (1.2-2.4) 0.738
0.5 1 2 5 10 0.71 0.73 0.75 0.77
AOR (95% CI) AUC
C Composite outcomeb
Adverse Outcome Adverse Outcome
Traditional BPD Definitions in BPD (+) Infants in BPD (−) Infants AOR (95% CI)a
Oxygen, 28 d 241/902 (26.7) 70/516 (13.6) 1.3 (0.9-1.8) 0.724
Oxygen/RS, 28 d 277/1134 (24.2) 34/284 (12.0) 1.4 (0.9-2.2) 0.725
Oxygen, 28 d and Oxygen/RS 36 wk PMA 185/586 (31.6) 126/832 (15.1) 1.7 (1.2-2.3) 0.731
Oxygen/RS, 28 d and 36 wk PMA 198/628 (31.5) 113/790 (14.3) 1.9 (1.4-2.7) 0.737
Oxygen, 36 wk PMA 174/556 (31.3) 137/862 (15.9) 1.8 (1.3-2.5) 0.733
Oxygen/RS 36 wk PMA 205/661 (31.0) 106/757 (14.0) 1.9 (1.4-2.7) 0.736
0.5 1 2 5 10 0.71 0.73 0.75 0.77
AOR (95% CI) AUC
The second and third columns show the number of infants with adverse Acute Physiology II score >20, maternal education, severe intraventricular
outcomes/the number of infants assessed at 18 to 21 months, with percentages hemorrhage and/or periventricular leukomalacia, necrotizing enterocolitis,
in brackets for infants with or without BPD defined in the first column. The and late-onset sepsis.
forest plots show the adjusted odds ratios (AORs; filled squares) and 95% CIs b
Composite outcome was defined as serious respiratory morbidity and/or
(lines). AUC indicates area under the receiver operating characteristic curve; neurosensory impairment at 18 to 21 months’ corrected age or death after
Oxygen/RS, receiving supplemental oxygen and/or any respiratory neonatal intensive care unit discharge before 21 months’ corrected age.
positive-pressure support; PMA, postmenstrual age.
a
Adjusted for gestational age, sex, small for gestational age, Score for Neonatal
Limitations was considered small. Fourth, 21% of infants did not have fol-
There were several limitations in our study. First, the poten- low-up outcomes; however, our previous comparisons have
tial for recall bias may exist in long-term adverse respiratory revealed that those who were lost to follow-up were likely to
morbidity findings because information was collected from be less ill15 and thus, our estimates of association may be mod-
parents by interviewers in follow-up visits at 18 to 21 months est. Finally, residual bias and confounding factors cannot be
of age; however, recall items only included the number of hos- ruled out based on the retrospective nature of our study.
pitalizations, which is very unlikely to be falsely reported. Sec-
ond, infants who were discharged home or were transferred
to step-down units before 44 weeks’ PMA using oxygen/RS did
not have data available on oxygen/RS after discharge/
Conclusions
transfer. The sensitivity analysis assessed the effect of this limi- From a predictive ability and strength of association perspec-
tation. Third, the oxygen challenge test was not mandatory to tive, oxygen/RS at 40 weeks’ PMA appears to be the optimal
assess oxygen requirement in this study and was unlikely to criterion to define or diagnose BPD associated with serious re-
have been conducted for the assessment at PMA other than 36 spiratory morbidity. This is particularly relevant for modern
weeks. Although we may have overestimated oxygen use at neonatal care practice, whereby wide panoply of respiratory
each PMA, its effect on the association or predictive abilities support modalities are offered to preterm neonates. Given the
E6 JAMA Pediatrics Published online January 23, 2017 (Reprinted) jamapediatrics.com
Copyright 2017 American Medical Association. All rights reserved.
Downloaded From: http://archpedi.jamanetwork.com/pdfaccess.ashx?url=/data/journals/peds/0/ on 01/24/2017
Bronchopulmonary Dysplasia Definitions and Outcomes Original Investigation Research
Figure 3. Association of Oxygen Use or Respiratory Support at 34 to 40 Weeks’ Postmenstrual Age With Adverse Outcomes at 18 to 21 Months of Age
A Serious respiratory morbidity
Traditional BPD Adverse Outcome Adverse Outcome
Definitions in BPD (+) Infants in BPD (−) Infants AOR (95% CI)a
34 wk PMA 72/939 (7.7) 16/552 (2.9) 1.8 (0.9-3.4) 0.721
35 wk PMA 70/780 (9.0) 18/673 (2.7) 2.6 (1.4-4.9) 0.732
36 wk PMA 69/652 (10.6) 19/754 (2.5) 3.4 (1.8-6.3) 0.75
37 wk PMA 67/555 (12.1) 19/821 (2.3) 4.2 (2.3-7.8) 0.766
38 wk PMA 65/467 (13.9) 20/879 (2.3) 5.2 (2.8-9.5) 0.785
39 wk PMA 60/392 (15.3) 22/928 (2.4) 5.6 (3.1-10.1) 0.792
40 wk PMA 59/362 (16.3) 23/942 (2.4) 6.1 (3.4-11.0) 0.799
41 wk PMA 45/315 (14.3) 30/966 (3.1) 4.0 (2.3-7.1) 0.778
42 wk PMA 43/294 (14.6) 32/974 (3.3) 3.9 (2.2-6.9) 0.779
43 wk PMA 40/272 (14.7) 29/981 (3.0) 4.6 (2.5-8.2) 0.782
44 wk PMA 41/269 (15.2) 28/980 (2.9) 5.1 (2.8-9.2) 0.789
0.5 1 2 5 10 20 0.7 0.75 0.8
AOR (95% CI) AUC
B Serious neurosensory impairment
Traditional BPD Adverse Outcome Adverse Outcome
Definitions in BPD (+) Infants in BPD (−) Infants AOR (95% CI)a
34 wk PMA 199/937 (21.2) 58/550 (10.6) 1.6 (1.1-2.3) 0.729
35 wk PMA 171/778 (27.0) 82/671 (12.2) 1.4 (1.0-2.1) 0.731
36 wk PMA 158/651 (24.3) 89/752 (11.8) 1.7 (1.2-2.4) 0.738
37 wk PMA 146/554 (26.4) 92/819 (11.2) 1.8 (1.3-2.6) 0.743
38 wk PMA 124/466 (26.6) 110/877 (12.5) 1.6 (1.2-2.3) 0.739
39 wk PMA 107/391 (27.4) 119/926 (12.9) 1.7 (1.2-2.4) 0.737
40 wk PMA 99/361 (27.4) 124/940 (13.2) 1.5 (1.0-2.1) 0.74
41 wk PMA 84/315 (26.7) 128/963 (13.3) 1.5 (1.0-2.1) 0.737
42 wk PMA 80/294 (27.2) 128/971 (13.2) 1.5 (1.0-2.2) 0.732
43 wk PMA 80/272 (29.4) 126/978 (12.9) 1.7 (1.1-2.5) 0.735
44 wk PMA 74/269 (27.5) 131/977 (13.4) 1.4 (0.9-2.1) 0.731
0.5 1 2 5 10 20 0.7 0.75 0.8
AOR (95% CI) AUC
C Composite outcomeb
Traditional BPD Adverse Outcome Adverse Outcome
Definitions in BPD (+) Infants in BPD (−) Infants AOR (95% CI)a
34 wk PMA 248/949 (26.1) 73/554 (13.2) 1.6 (1.1-2.2) 0.724
35 wk PMA 219/790 (27.7) 98/675 (14.5) 1.6 (1.1-2.2) 0.729
36 wk PMA 205/661 (31.0) 106/757 (14.0) 1.9 (1.4-2.7) 0.736
37 wk PMA 191/564 (33.9) 109/824 (13.2) 2.2 (1.6-3.1) 0.746
38 wk PMA 171/478 (35.8) 125/880 (14.2) 2.2 (1.6-3.0) 0.744
39 wk PMA 150/401 (37.4) 137/931 (14.7) 2.3 (1.6-3.2) 0.743
40 wk PMA 138/370 (37.3) 144/944 (15.3) 2.0 (1.4-2.8) 0.745
41 wk PMA 114/322 (35.4) 155/969 (16.0) 1.8 (1.3-2.6) 0.74
42 wk PMA 111/302 (36.8) 154/976 (15.8) 1.9 (1.4-2.8) 0.737
43 wk PMA 104/278 (37.4) 154/985 (15.6) 2.0 (1.4-2.8) 0.735
44 wk PMA 100/276 (36.2) 157/983 (16.0) 1.7 (1.2-2.5) 0.732
0.5 1 2 5 10 20 0.7 0.75 0.8
AOR (95% CI) AUC
The second and third columns show the number of infants with adverse Acute Physiology II score >20, maternal education, severe intraventricular
outcomes/the number of infants assessed at 18-21 months with percentages in hemorrhage and/or periventricular leukomalacia, necrotizing enterocolitis,
brackets for infants with or without bronchopulmonary dysplasia (BPD) defined in and late-onset sepsis.
the first column. The forest plots show the adjusted odds ratios (AORs; filled b
Composite outcome was defined as serious respiratory morbidity and/or
squares) and 95% CIs (lines). AUC indicates area under the receiver operating neurosensory impairment at 18 to 21 months’ corrected age, or death after
characteristic curve; Oxygen/RS, receiving supplemental oxygen and/or any neonatal intensive care unit discharge before 21 months’ corrected age.
respiratory positive-pressure support; PMA, postmenstrual age.
a
Adjusted for gestational age, sex, small for gestational age, Score for Neonatal
jamapediatrics.com (Reprinted) JAMA Pediatrics Published online January 23, 2017 E7
Copyright 2017 American Medical Association. All rights reserved.
Downloaded From: http://archpedi.jamanetwork.com/pdfaccess.ashx?url=/data/journals/peds/0/ on 01/24/2017
Research Original Investigation Bronchopulmonary Dysplasia Definitions and Outcomes
persistent inconsistency of BPD definitions in the literature, respiratory and neurodevelopmental outcomes are con-
this unique information should be useful to develop a cerned in future exercises. Future large prospective cohort
future consensus on a BPD definition based on outcome studies are also needed to confirm our study findings such
data. We strongly encourage incorporation of parental per- as the Prematurity and Respiratory Outcomes Program cur-
spectives in defining what matters to them most as far as rently under way.26
ARTICLE INFORMATION Ontario; Michael Dunn, MD, Sunnybrook Health Saint John, New Brunswick; Hala Makary, MD, Dr
Accepted for Publication: October 23, 2016. Sciences Centre, Toronto, Ontario; Brigitte Lemyre, Everett Chalmers Hospital, Fredericton, New
MD, Children’s Hospital of Eastern Ontario and Brunswick; Michael Vincer, MD, IWK Health Centre,
Published Online: January 23, 2017. Ottawa General Hospital, Ottawa, Ontario; Kimberly Halifax, Nova Scotia; Phil Murphy, Charles Janeway
doi:10.1001/jamapediatrics.2016.4141 Dow, MD, Kingston General Hospital, Kingston, Children’s Health and Rehabilitation Centre, St.
Author Affiliations: Department of Pediatrics, Ontario; Ermelinda Pelausa, MD, Jewish General John’s, Newfoundland.
University of Toronto, Toronto, Ontario, Canada Hospital, Montréal, Québec; Keith Barrington, Conflicts of Interest Disclosures: None reported.
(Isayama, S. K. Lee, Dunn, Shah); Department of MBChB, Hôpital Sainte-Justine, Montréal, Québec;
Clinical Epidemiology and Biostatistics, McMaster Christine Drolet, MD, and Bruno Piedboeuf, MD, Funding/Support: Organizational support was
University, Hamilton, Ontario, Canada (Isayama); Centre Hospitalier Universitaire de Québec, Sainte provided by the Maternal-Infant Care Research
Maternal-Infant Care Research Centre, Department Foy Québec; Martine Claveau, and Daniel Faucher, Centre at Mount Sinai Hospital in Toronto, Ontario,
of Paediatrics, Mount Sinai Hospital, Toronto, MD, McGill University Health Centre, Montréal, Canada. Neonatal follow-up data were supported
Ontario, Canada (S. K. Lee, Yang, Shah); Québec; Valerie Bertelle, MD, and Edith Masse, MD, by team grant FRN87518 from the Canadian
Department of Paediatrics, University of Western Centre Hospitalier Universitaire de Sherbrooke, Institutes of Health Research awarded to Dr Lee,
Ontario, London, Ontario, Canada (D. Lee); Sherbrooke, Québec; Roderick Canning, MD, and in-kind support from Mount Sinai Hospital. Dr
Department of Paediatrics, University of Moncton Hospital, Moncton, New Brunswick; Hala Isayama is supported by the Ontario Graduate
Saskatchewan, Saskatoon, Canada (Daspal). Makary, MD, Dr Everett Chalmers Hospital, Scholarships program. Dr Shah holds an Applied
Fredericton, New Brunswick; Cecil Ojah, MBBS, and Research Chair in Reproductive and Child Health
Author Contributions: Dr Shah had full access to all Services and Policy Research awarded by the
the data in the study and takes responsibility for the Luis Monterrosa, MD, Saint John Regional Hospital,
Saint John, New Brunswick; Akhil Deshpandey, Canadian Institutes of Health Research (APR-
integrity of the data and the accuracy of the data 126340).
analysis. MBBS, MRCPI, Janeway Children’s Health and
Concept and design: Isayama, S. K. Lee, D. Lee, Rehabilitation Centre, St. John’s, Newfoundland; Role of the Funder/Sponsor: The funders had no
Daspal, Dunn, Shah. Jehier Afifi, MB BCh, MSc, IWK Health Centre, role in the design and conduct of the study;
Acquisition, analysis, or interpretation of data: Halifax, Nova Scotia; Andrzej Kajetanowicz, MD, collection, management, analysis, and
Isayama, S. K. Lee, Yang, Shah. Cape Breton Regional Hospital, Sydney, Nova interpretation of the data; preparation, review, or
Drafting of the manuscript: Isayama, Daspal. Scotia; Shoo K Lee, MBBS, PhD (Chairman, approval of the manuscript; and decision to submit
Critical revision of the manuscript for important Canadian Neonatal Network), Mount Sinai Hospital, the manuscript for publication.
intellectual content: Isayama, S. K. Lee, Yang, D. Lee, Toronto, Ontario. Canadian Neonatal Follow-Up Additional Contributions: We gratefully
Dunn, Shah. Network investigators: Thevanisha Pillay, MD, acknowledge all investigators and data abstractors
Statistical analysis: Isayama, Yang, Shah. Victoria General Hospital, Victoria, British of the Canadian Neonatal and Follow-Up Networks.
Obtained funding: S. K. Lee. Columbia; Anne Synnes, MDCM, MHSC (Director We also thank Natasha Musrap, PhD, from the
Administrative, technical, or material support: Lee, CNFUN), British Columbia Women’s Hospital, Maternal-Infant Care Research Centre, for editorial
Shah. Vancouver, British Columbia; Reg Sauvé, MD, MPh, assistance in the preparation of the manuscript. She
Supervision: S. K. Lee, D. Lee, Shah. Leonora Hendson MBBCH, MSc, Alberta’s Children’s received salaried compensation for her work from
Hospital, Foothills Medical Centre, Calgary, Alberta; funding support (grant FRN87518).
Group Information: Investigators of the Canadian Amber Reichert, MD, Glenrose Rehabilitation
Neonatal Network and Canadian Neonatal Follow- Hospital, Edmonton, Alberta; Jaya Bodani, MD,
Up Network are listed here. Canadian Neonatal REFERENCES
Regina General Hospital, Regina, Saskatchewan;
Network investigators: Prakesh S Shah, MD, MSc Koravangattu Sankaran, MD, Royal University 1. Doyle LW, Anderson PJ. Long-term outcomes of
(Director, Canadian Neonatal Network and site Hospital, Saskatoon, Saskatchewan; Diane bronchopulmonary dysplasia. Semin Fetal Neonatal
investigator), Mount Sinai Hospital, Toronto, Moddemann, MD, Winnipeg Health Sciences Med. 2009;14(6):391-395.
Ontario; Adele Harrison, MD, MBChB, Victoria Centre, St. Boniface General Hospital, Winnipeg, 2. Schmidt B, Asztalos EV, Roberts RS, Robertson
General Hospital, Victoria, British Columbia; Anne Manitoba; Chuks Nwaesei, MD, Windsor Regional CM, Sauve RS, Whitfield MF; Trial of Indomethacin
Synnes, MDCM, MHSC, and Joseph Ting, MD, Hospital, Windsor, Ontario; Thierry Daboval, MD, Prophylaxis in Preterms (TIPP) Investigators.
British Columbia Women’s Hospital, Vancouver, Children’s Hospital of Eastern Ontario, Ottawa, Impact of bronchopulmonary dysplasia, brain
British Columbia; Zenon Cieslak, MD, Royal Ontario; Kimberly Dow, Kingston General Hospital, injury, and severe retinopathy on the outcome of
Columbian Hospital, New Westminster, British Kingston, Ontario; David Lee, MD, Children’s extremely low-birth-weight infants at 18 months:
Columbia; Rebecca Sherlock, MD, Surrey Memorial Hospital London Health Sciences Centre, London, results from the trial of indomethacin prophylaxis in
Hospital, Surrey, British Columbia; Wendy Yee, MD, Ontario; Linh Ly, MD, Hospital for Sick Children, preterms. JAMA. 2003;289(9):1124-1129.
Foothills Medical Centre, Calgary, Alberta; Khalid Toronto, Ontario; Edmond Kelly, MD, Mount Sinai
Aziz, MBBS, MA, MEd, and Jennifer Toye, MD, Royal 3. Vohr BR, Wright LL, Poole WK, McDonald SA.
Hospital, Toronto, Ontario; Salhab el Helou, MD, Neurodevelopmental outcomes of extremely low
Alexandra Hospital, Edmonton, Alberta; Carlos Hamilton Health Sciences Centre, Hamilton,
Fajardo, MD, Alberta Children’s Hospital, Calgary, birth weight infants <32 weeks’ gestation between
Ontario; Paige Church, MD, Sunnybrook Health 1993 and 1998. Pediatrics. 2005;116(3):635-643.
Alberta; Zarin Kalapesi, MD, Regina General Sciences Centre, Toronto, Ontario; Ermelinda
Hospital, Regina, Saskatchewan; Koravangattu Pelausa, MD, Jewish General Hospital, Montréal, 4. Stoll BJ, Hansen NI, Bell EF, et al; Eunice
Sankaran, MD, MBBS, and Sibasis Daspal, MD, Royal Québec; Patricia Riley, MD, Montréal Children’s Kennedy Shriver National Institute of Child Health
University Hospital, Saskatoon, Saskatchewan; Hospital, Royal Victoria Hospital, Montréal, Québec; and Human Development Neonatal Research
Mary Seshia, MBChB, Winnipeg Health Sciences Francine Levebrve, Centre Hospitalier Universitaire Network. Trends in care practices, morbidity, and
Centre, Winnipeg, Manitoba; Ruben Alvaro, MD, St. Sainte-Justine, Montréal, Québec; Charlotte mortality of extremely preterm neonates,
Boniface General Hospital, Winnipeg, Manitoba; Demers, Centre Hospitalier Universitaire de 1993-2012. JAMA. 2015;314(10):1039-1051.
Sandesh Shivananda, MBBS, MD, DM, Hamilton Sherbrooke, Sherbrooke, Québec; Sylvie Bélanger, 5. Northway WH Jr, Rosan RC, Porter DY.
Health Sciences Centre, Hamilton, Ontario; Orlando MD, Centre Hospitalier Universitaire de Québec, Pulmonary disease following respirator therapy of
Da Silva, MD, MSc, London Health Sciences Centre, Québec City, Québec; Roderick Canning, MD, hyaline-membrane disease. Bronchopulmonary
London, Ontario; Chuks Nwaesei, MD, Windsor Moncton Hospital, Moncton, New Brunswick; Luis dysplasia. N Engl J Med. 1967;276(7):357-368.
Regional Hospital, Windsor, Ontario; Kyong-Soon Monterrosa, MD, Saint John Regional Hospital,
Lee, MD, MSc, Hospital for Sick Children, Toronto,
E8 JAMA Pediatrics Published online January 23, 2017 (Reprinted) jamapediatrics.com
Copyright 2017 American Medical Association. All rights reserved.
Downloaded From: http://archpedi.jamanetwork.com/pdfaccess.ashx?url=/data/journals/peds/0/ on 01/24/2017
Bronchopulmonary Dysplasia Definitions and Outcomes Original Investigation Research
6. Tooley WH. Epidemiology of bronchopulmonary Development Neonatal Research Network. intraventricular hemorrhage: a study of infants with
dysplasia. J Pediatr. 1979;95(5 Pt 2):851-858. Validation of the National Institutes of Health birth weights less than 1,500 gm. J Pediatr. 1978;92
7. Shennan AT, Dunn MS, Ohlsson A, Lennox K, consensus definition of bronchopulmonary (4):529-534.
Hoskins EM. Abnormal pulmonary outcomes in dysplasia. Pediatrics. 2005;116(6):1353-1360. 21. Bell MJ, Ternberg JL, Feigin RD, et al. Neonatal
premature infants: prediction from oxygen 14. Canadian Neonatal Network. The Canadian necrotizing enterocolitis. Therapeutic decisions
requirement in the neonatal period. Pediatrics. Neonatal Network Abstractor's Manual, version based upon clinical staging. Ann Surg. 1978;187(1):1-
1988;82(4):527-532. 1.3.4. http://www.canadianneonatalnetwork.org 7.
8. Beam KS, Aliaga S, Ahlfeld SK, Cohen-Wolkowiez /Portal/LinkClick.aspx?fileticket=U4anCYsSN20 22. Steyerberg EW. Evaluation of performance. In:
M, Smith PB, Laughon MM. A systematic review of %3D&tabid=69. Accessed December 15, 2016. Steyerberg EW, ed. Clinical Prediction Models:
randomized controlled trials for the prevention of 15. Synnes A, Luu TM, Moddemann D, et al; a Practical Approach to Development, Validation,
bronchopulmonary dysplasia in infants. J Perinatol. Canadian Neonatal Network and the Canadian and Updating. New York: Springer; 2009.
2014;34(9):705-710. Neonatal Follow-Up Network. Determinants of 23. Zou KH, O’Malley AJ, Mauri L.
9. Jobe AH, Bancalari E. Bronchopulmonary developmental outcomes in a very preterm Receiver-operating characteristic analysis for
dysplasia. Am J Respir Crit Care Med. 2001;163(7): Canadian cohort. Arch Dis Child Fetal Neonatal Ed. evaluating diagnostic tests and predictive models.
1723-1729. 2016;fetalneonatal-2016-311228. Circulation. 2007;115(5):654-657.
10. Walsh MC, Wilson-Costello D, Zadell A, 16. Canadian Neonatal Follow-Up Network. 24. Davis PG, Thorpe K, Roberts R, Schmidt B,
Newman N, Fanaroff A. Safety, reliability, and 18-Month Corrected Age Assessment Manual, Doyle LW, Kirpalani H; Trial Indomethacin
validity of a physiologic definition of Version 5. http://www.cnfun.ca/LinkClick.aspx Prophylaxis in Preterms Investigators. Evaluating
bronchopulmonary dysplasia. J Perinatol. 2003;23 ?fileticket=d4p7mZoXWDU%3D&tabid=68. “old” definitions for the “new” bronchopulmonary
(6):451-456. Accessed December 15, 2016. dysplasia. J Pediatr. 2002;140(5):555-560.
11. Walsh MC, Yao Q, Gettner P, et al; National 17. Morris C, Bartlett D. Gross motor function 25. Mercier CE, Dunn MS, Ferrelli KR, Howard DB,
Institute of Child Health and Human Development classification system: impact and utility. Dev Med Soll RF; Vermont Oxford Network ELBW Infant
Neonatal Research Network. Impact of a Child Neurol. 2004;46(1):60-65. Follow-Up Study Group. Neurodevelopmental
physiologic definition on bronchopulmonary 18. Bayley N. The Bayley Scales of Infant and outcome of extremely low birth weight infants from
dysplasia rates. Pediatrics. 2004;114(5):1305-1311. Toddler Development. 3rd ed. San Antonio, TX: The the Vermont Oxford network: 1998-2003.
12. Poindexter BB, Feng R, Schmidt B, et al; Psychological Corporation; 2006. Neonatology. 2010;97(4):329-338.
Prematurity and Respiratory Outcomes Program. 19. Richardson DK, Corcoran JD, Escobar GJ, Lee 26. Maitre NL, Ballard RA, Ellenberg JH, et al;
Comparisons and limitations of current definitions SK. SNAP-II and SNAPPE-II: simplified newborn Prematurity and Respiratory Outcomes Program.
of bronchopulmonary dysplasia for the prematurity illness severity and mortality risk scores. J Pediatr. Respiratory consequences of prematurity:
and respiratory outcomes program. Ann Am Thorac 2001;138(1):92-100. evolution of a diagnosis and development of a
Soc. 2015;12(12):1822-1830. 20. Papile LA, Burstein J, Burstein R, Koffler H. comprehensive approach. J Perinatol. 2015;35(5):
13. Ehrenkranz RA, Walsh MC, Vohr BR, et al; Incidence and evolution of subependymal and 313-321.
National Institutes of Child Health and Human
jamapediatrics.com (Reprinted) JAMA Pediatrics Published online January 23, 2017 E9
Copyright 2017 American Medical Association. All rights reserved.
Downloaded From: http://archpedi.jamanetwork.com/pdfaccess.ashx?url=/data/journals/peds/0/ on 01/24/2017
You might also like
- Rapid Maxillary Expansion in Pediatric Patients With Obstructive Sleep Apnea - An Umbrella ReviewDocument9 pagesRapid Maxillary Expansion in Pediatric Patients With Obstructive Sleep Apnea - An Umbrella ReviewAly OsmanNo ratings yet
- WRIGHT 2016 - Continuous Positive Airway Pressure To Prevent Neonatal Lung InjuryDocument10 pagesWRIGHT 2016 - Continuous Positive Airway Pressure To Prevent Neonatal Lung InjuryRafael JustinoNo ratings yet
- Machine Learning To Predict Late Respiratory Support in Preterm Infants: A Retrospective Cohort StudyDocument9 pagesMachine Learning To Predict Late Respiratory Support in Preterm Infants: A Retrospective Cohort StudyNodi MNo ratings yet
- Displasia BroncopulmonarDocument12 pagesDisplasia BroncopulmonarRaul VillacresNo ratings yet
- Bronchopulmonary Dysplasia An Update On Experimental TherapeuticsDocument14 pagesBronchopulmonary Dysplasia An Update On Experimental TherapeuticsIván Gustavo Magaña CeballosNo ratings yet
- Lodha 2014Document12 pagesLodha 2014madhuNo ratings yet
- Mortality in Pediatric Acute Respiratory Distress Syndrome: A Systematic Review and Meta-AnalysisDocument9 pagesMortality in Pediatric Acute Respiratory Distress Syndrome: A Systematic Review and Meta-Analysisesya putrri oktareginaNo ratings yet
- FKT en Neonatos ChestDocument17 pagesFKT en Neonatos ChestSofia MandolaNo ratings yet
- Retrospective Analysis of Inpatient Polysomnogram Characteristics in Infants With Broncopulmonary DisplasiaDocument30 pagesRetrospective Analysis of Inpatient Polysomnogram Characteristics in Infants With Broncopulmonary DisplasiaJHONATAN MATA ARANDANo ratings yet
- Clouse 2016 RSLDocument18 pagesClouse 2016 RSLwisdom loverNo ratings yet
- Jurnal PediDocument13 pagesJurnal PediHansNo ratings yet
- Nejmoa 1708831Document10 pagesNejmoa 1708831Lissaberti AmaliahNo ratings yet
- Bassler 2018 Ensayo CohorteDocument10 pagesBassler 2018 Ensayo Cohortewisdom loverNo ratings yet
- Assessment of Postnatal Corticosteroids For The Prevention of BronchopulmonaryDocument19 pagesAssessment of Postnatal Corticosteroids For The Prevention of BronchopulmonaryFernando Guzmán VegaNo ratings yet
- BMJ n1974 FullDocument18 pagesBMJ n1974 FullErick HernandezNo ratings yet
- Bronchopulmonary Dysplasia Executive Summary of A 2018Document18 pagesBronchopulmonary Dysplasia Executive Summary of A 2018Raul VillacresNo ratings yet
- Modified Lung Ultrasound in Evaluating BPD at 36 WeeksDocument11 pagesModified Lung Ultrasound in Evaluating BPD at 36 WeeksArjun VermaNo ratings yet
- Prediction of Pneumonia in A Pediatric Emergency Department: PediatricsDocument10 pagesPrediction of Pneumonia in A Pediatric Emergency Department: PediatricsLeslie Lindsay AlvarezNo ratings yet
- JOBE 2016 - Surfactant Treatment For RDS Improves OxygenationDocument4 pagesJOBE 2016 - Surfactant Treatment For RDS Improves OxygenationRafael JustinoNo ratings yet
- Displasia BronkopulmonerDocument54 pagesDisplasia BronkopulmonerVivi DeviyanaNo ratings yet
- Study of Respiratory Distress in Newborn: International Journal of Contemporary Pediatrics March 2017Document6 pagesStudy of Respiratory Distress in Newborn: International Journal of Contemporary Pediatrics March 2017Elison J PanggaloNo ratings yet
- JurnalDocument6 pagesJurnalIzzyNo ratings yet
- 2174 8646 1 PBDocument5 pages2174 8646 1 PBKiran PantheeNo ratings yet
- Hemorragia PulmonarDocument11 pagesHemorragia PulmonarFer45No ratings yet
- BBLR 2Document8 pagesBBLR 2Radhiatul AdillahNo ratings yet
- Pi Is 1875957219305510Document10 pagesPi Is 1875957219305510madimadi11No ratings yet
- Venkataraman 2017 - Metaanálisis y RSLDocument8 pagesVenkataraman 2017 - Metaanálisis y RSLwisdom loverNo ratings yet
- Respiratory Pearls CombinedDocument7 pagesRespiratory Pearls CombinedVishal ParmarNo ratings yet
- 10 1002@ppul 24581Document6 pages10 1002@ppul 24581Roberto Guerrero MonsivaisNo ratings yet
- Dyke 2023 Ped Radiol PREFUL Lung MRI Ventilation NICUDocument9 pagesDyke 2023 Ped Radiol PREFUL Lung MRI Ventilation NICUJonathan DykeNo ratings yet
- Buonsenso Et Al-2018-Pediatric PulmonologyDocument9 pagesBuonsenso Et Al-2018-Pediatric Pulmonologywawa chenNo ratings yet
- Neonatal Outcomes of Extremely Preterm Infants From The NICHD Neonatal Research NetworkDocument14 pagesNeonatal Outcomes of Extremely Preterm Infants From The NICHD Neonatal Research NetworkKattia FloresNo ratings yet
- Nicu 1Document7 pagesNicu 1PPDS ANAK FK USUNo ratings yet
- Wright Et Al 2022 PDFDocument9 pagesWright Et Al 2022 PDFRadu CiprianNo ratings yet
- 2023 - Suplementación de Ácido Araquidónico y Docosaexanoico y Resultados Respiratorios en Infantes @wendelDocument7 pages2023 - Suplementación de Ácido Araquidónico y Docosaexanoico y Resultados Respiratorios en Infantes @wendelJorge Toshio Yazawa ChaconNo ratings yet
- Pxaa 116Document7 pagesPxaa 116Geísa VasconcelosNo ratings yet
- 2021 Predictors of Lung Function Trajectories in Population-Based Studies A Systematic ReviewDocument22 pages2021 Predictors of Lung Function Trajectories in Population-Based Studies A Systematic Reviewjose.maletNo ratings yet
- 3Document16 pages3marianaNo ratings yet
- S177 Full PDFDocument4 pagesS177 Full PDFCalvin AffendyNo ratings yet
- Advanced Proteomics and Cluster Analysis For Identifying Novel Obstructive Sleep Apnea Subtypes Before and After CPAP TherapyDocument34 pagesAdvanced Proteomics and Cluster Analysis For Identifying Novel Obstructive Sleep Apnea Subtypes Before and After CPAP Therapy马三强No ratings yet
- The Impact of A Dedicated Physiotherapist Clinic For Children With Dysfunctional BreathingDocument6 pagesThe Impact of A Dedicated Physiotherapist Clinic For Children With Dysfunctional BreathingKuro ShibaNo ratings yet
- Guidelines For Surfactant Replacement Therapy in NeonatesDocument7 pagesGuidelines For Surfactant Replacement Therapy in NeonatesFer45No ratings yet
- Canadian Guidelines 2021Document7 pagesCanadian Guidelines 2021Radu CiprianNo ratings yet
- 2024 - Appnoeic Oxygenation During Paediatric Tracheal Intubation A Systematic Review and Meta AnalysisDocument15 pages2024 - Appnoeic Oxygenation During Paediatric Tracheal Intubation A Systematic Review and Meta AnalysisPamela Mamani FloresNo ratings yet
- SPPRGG DescargarPDFDocument8 pagesSPPRGG DescargarPDFS ONo ratings yet
- Basic Principlies of Respiratory Function Monitoring in Ventilated NewornDocument8 pagesBasic Principlies of Respiratory Function Monitoring in Ventilated NewornNoe Perez GonzalezNo ratings yet
- Study of Different Treatment Modalities and Outcome in Preterm Babies With Respiratory Distress Syndrome 2017Document4 pagesStudy of Different Treatment Modalities and Outcome in Preterm Babies With Respiratory Distress Syndrome 2017Vita DesriantiNo ratings yet
- Resolving Our Uncertainty About Oxygen TherapyDocument7 pagesResolving Our Uncertainty About Oxygen TherapyAwadhNo ratings yet
- Epinephrine and Dexamethasone in Children With BronchiolitisDocument11 pagesEpinephrine and Dexamethasone in Children With BronchiolitisAdelina Wahyuni LubisNo ratings yet
- Adjunctive Therapies in Bronchopulmonary Dysplasia, NeoReview 2017Document9 pagesAdjunctive Therapies in Bronchopulmonary Dysplasia, NeoReview 2017Edrei Lopez CNo ratings yet
- Viral Respiratory Infections in Preterm Infants During andDocument9 pagesViral Respiratory Infections in Preterm Infants During andMariusNo ratings yet
- Clinical Controversies in Aerosol Therapy For Infants and ChildrenDocument23 pagesClinical Controversies in Aerosol Therapy For Infants and Childrencelma44No ratings yet
- Upper Airway Visualization in Pediatric Obstructive Sleep ApneaDocument20 pagesUpper Airway Visualization in Pediatric Obstructive Sleep ApneaDra. María José CastilloNo ratings yet
- Causes and Outcomes of Respiratory Distress in NeonatesDocument8 pagesCauses and Outcomes of Respiratory Distress in NeonatesMohammad AlmuhaiminNo ratings yet
- Risk Factors For Premenstrual Asthma. A Systematic Review and Meta-AnalysisDocument43 pagesRisk Factors For Premenstrual Asthma. A Systematic Review and Meta-Analysisrifka riskaNo ratings yet
- Displasia BroncopulmonarDocument4 pagesDisplasia BroncopulmonarRaul VillacresNo ratings yet
- Accepted Manuscript: Paediatric Respiratory ReviewsDocument16 pagesAccepted Manuscript: Paediatric Respiratory ReviewsAlvaro Guillen CerpaNo ratings yet
- Severity Scoring Systems: Are They Internally Valid, Reliable and Predictive of Oxygen Use in Children With Acute Bronchiolitis?Document7 pagesSeverity Scoring Systems: Are They Internally Valid, Reliable and Predictive of Oxygen Use in Children With Acute Bronchiolitis?Ivan VeriswanNo ratings yet
- SA PerformanceDocument8 pagesSA Performancefernin96No ratings yet
- Precision in Pulmonary, Critical Care, and Sleep Medicine: A Clinical and Research GuideFrom EverandPrecision in Pulmonary, Critical Care, and Sleep Medicine: A Clinical and Research GuideJose L. GomezNo ratings yet
- POLIN 2009 - Bubble CPAP - A Clash of Science Culture and ReligionDocument2 pagesPOLIN 2009 - Bubble CPAP - A Clash of Science Culture and ReligionRafael JustinoNo ratings yet
- MIEDEMA 2013 - Effect of Nasal Continuous and Biphasic Positive Airway Pressure On Lung Volume in Preterm InfantsDocument7 pagesMIEDEMA 2013 - Effect of Nasal Continuous and Biphasic Positive Airway Pressure On Lung Volume in Preterm InfantsRafael JustinoNo ratings yet
- GUPTA 2009 - A RCT of Post Extubation BCPAP Versus Infant Flow Driver CPAP in Preterm Infants With RDSDocument8 pagesGUPTA 2009 - A RCT of Post Extubation BCPAP Versus Infant Flow Driver CPAP in Preterm Infants With RDSRafael JustinoNo ratings yet
- ABIGAIL 2010 - Diffuse Alveolar HemorrhageDocument10 pagesABIGAIL 2010 - Diffuse Alveolar HemorrhageRafael JustinoNo ratings yet
- BURG 2014 - Cross-Sectional Changes in Lung Volume Measured by Electrical Impedance Tomography Are Representative For The Whole Lung in Ventilated Preterm InfantsDocument8 pagesBURG 2014 - Cross-Sectional Changes in Lung Volume Measured by Electrical Impedance Tomography Are Representative For The Whole Lung in Ventilated Preterm InfantsRafael JustinoNo ratings yet
- ORENSTEIN 2002 - Cystic Fibrosis - A 2002 UpdateDocument9 pagesORENSTEIN 2002 - Cystic Fibrosis - A 2002 UpdateRafael JustinoNo ratings yet
- NARASIMHAN - Pulmonary Haemorrhage in NeonatesDocument3 pagesNARASIMHAN - Pulmonary Haemorrhage in NeonatesRafael JustinoNo ratings yet
- HOUGH 2014 - Lung Recruitment and Endotracheal Suction in Ventilated Preterm Infants Measured With Electrical Impedance TomographyDocument7 pagesHOUGH 2014 - Lung Recruitment and Endotracheal Suction in Ventilated Preterm Infants Measured With Electrical Impedance TomographyRafael JustinoNo ratings yet
- NEWHOUSE 1999 - Asthma Therapy With AerosolsDocument4 pagesNEWHOUSE 1999 - Asthma Therapy With AerosolsRafael JustinoNo ratings yet
- BURG 2016 - Effect of Minimally Invasive Surfactant Therapy On Lung Volume and Ventilation in Preterm InfantsDocument6 pagesBURG 2016 - Effect of Minimally Invasive Surfactant Therapy On Lung Volume and Ventilation in Preterm InfantsRafael JustinoNo ratings yet
- BIBAN 2012 - Exogenous Surfactant Replacement - How To Deliver ItDocument6 pagesBIBAN 2012 - Exogenous Surfactant Replacement - How To Deliver ItRafael JustinoNo ratings yet
- ALVIRA 2017 - Can We Understand The Pathobiology of Bronchopulmonary DysplasiaDocument11 pagesALVIRA 2017 - Can We Understand The Pathobiology of Bronchopulmonary DysplasiaRafael JustinoNo ratings yet
- MIEDEMA 2011 - Changes in Lung Volume and Ventilation During Surfactant Treatment in Ventilated Preterm InfantsDocument6 pagesMIEDEMA 2011 - Changes in Lung Volume and Ventilation During Surfactant Treatment in Ventilated Preterm InfantsRafael JustinoNo ratings yet
- Ultrasound in Obstet Gyne - 2002 - Laudy - The Fetal Lung 1 Developmental AspectsDocument7 pagesUltrasound in Obstet Gyne - 2002 - Laudy - The Fetal Lung 1 Developmental AspectsRafael JustinoNo ratings yet
- LISTA 2012 - Surfactant and Mechanical VentilationDocument3 pagesLISTA 2012 - Surfactant and Mechanical VentilationRafael JustinoNo ratings yet
- Neuroprotective MgSO4Document6 pagesNeuroprotective MgSO4Rafael JustinoNo ratings yet
- SOLALIGUE 2017 - 1 Recent Advances in Our Understanding of The Mechanisms of Late Lunf Development and BPDDocument190 pagesSOLALIGUE 2017 - 1 Recent Advances in Our Understanding of The Mechanisms of Late Lunf Development and BPDRafael JustinoNo ratings yet
- Ca 27 29Document2 pagesCa 27 29डा. सत्यदेव त्यागी आर्यNo ratings yet
- Snake Bite National Protocol PediatricsDocument45 pagesSnake Bite National Protocol Pediatricsarjun_paulNo ratings yet
- ADA Guideline - Chronic Kidney Disease Evidence-Based Nutrition Practice GuidelineDocument19 pagesADA Guideline - Chronic Kidney Disease Evidence-Based Nutrition Practice GuidelineJorge SánchezNo ratings yet
- Centric and Eccentric OcclusionsDocument8 pagesCentric and Eccentric OcclusionsYan Lau100% (1)
- Feline Pyometra and Its Surgical Management: A Case: Received: 30.03.2021 Accepted: 13.04.2021Document5 pagesFeline Pyometra and Its Surgical Management: A Case: Received: 30.03.2021 Accepted: 13.04.2021dewaNo ratings yet
- EMNoteDocument1 pageEMNoteKC Dela RosaNo ratings yet
- Dentists CADocument44 pagesDentists CABruce AmigoNo ratings yet
- Medical Skills Physical ExamDocument150 pagesMedical Skills Physical Examsholay100% (1)
- ENEMADocument3 pagesENEMAdenNo ratings yet
- Website Advt EnglishDocument7 pagesWebsite Advt EnglishsapnaNo ratings yet
- Forensic MedicineDocument7 pagesForensic MedicineAlta Sofia CriminologyNo ratings yet
- Promoting Personal Hygiene & Promoting Rest & SleepDocument26 pagesPromoting Personal Hygiene & Promoting Rest & SleepYousef JafarNo ratings yet
- Difficulty in Hearing: Prepared By: Francis Quarre Lyka Jane Roguel John Lester Romero Alana Marees DolosoDocument31 pagesDifficulty in Hearing: Prepared By: Francis Quarre Lyka Jane Roguel John Lester Romero Alana Marees DolosoJessa Mae SusonNo ratings yet
- Penicillin G Benza Drug StudyDocument2 pagesPenicillin G Benza Drug StudyRussel Kate SulangNo ratings yet
- List of Nursing Abbreviations and Acronyms 1Document5 pagesList of Nursing Abbreviations and Acronyms 1Jay Debby RuizoNo ratings yet
- Product InformationDocument80 pagesProduct InformationElla LiuNo ratings yet
- Hyperuricemia XXXX XXXXX XxjeuneDocument32 pagesHyperuricemia XXXX XXXXX XxjeuneOziq Juga ReMa-eNo ratings yet
- Programa Aua San Francisco 2018Document76 pagesPrograma Aua San Francisco 2018Rosemary FranquizNo ratings yet
- Extraordinary Vessel PointsDocument3 pagesExtraordinary Vessel PointsIhes HesNo ratings yet
- PODCAST #67 DR.B The Vet Show - Drh. Syavira EkdhiasmaraDocument26 pagesPODCAST #67 DR.B The Vet Show - Drh. Syavira EkdhiasmaraLailatun NafisahNo ratings yet
- Report On Term Paper Presentation-Ii Artificial Vision-A Bionic EyeDocument7 pagesReport On Term Paper Presentation-Ii Artificial Vision-A Bionic Eye3nadhsNo ratings yet
- Virus ClassificationDocument2 pagesVirus ClassificationJoshua PrinceNo ratings yet
- So You Want To Be A Urologist?: The First StepDocument2 pagesSo You Want To Be A Urologist?: The First StepDrThamma ShahiNo ratings yet
- Price ALL Z-VentDocument9 pagesPrice ALL Z-VentPanco NanaNo ratings yet
- HydrocephalusDocument39 pagesHydrocephalusspiritNo ratings yet
- TRM03.01 Cervical Spine Guideline V5.0 - 12.17Document6 pagesTRM03.01 Cervical Spine Guideline V5.0 - 12.17Alexandria Firdaus Al-farisyNo ratings yet
- Genital Tract InfectionsDocument4 pagesGenital Tract Infectionsmed.progressNo ratings yet
- Important Questions For Esic Staff Nurse Recruitment ExamDocument4 pagesImportant Questions For Esic Staff Nurse Recruitment ExamSuchitaNo ratings yet
- Endodontics ObturationDocument8 pagesEndodontics ObturationShameer Parambil100% (2)
- 2011 Risk Score To Hospitalized Patients For Clinical Pharmacy RationalizationDocument6 pages2011 Risk Score To Hospitalized Patients For Clinical Pharmacy RationalizationIgnacio NamuncuraNo ratings yet