Professional Documents
Culture Documents
F - BCBCR Five Year Follow Up of Patients With Early Stage Breast Cancer After2.pdf - 4610
F - BCBCR Five Year Follow Up of Patients With Early Stage Breast Cancer After2.pdf - 4610
Uploaded by
Windy HardiyantyCopyright:
Available Formats
You might also like
- Coursebook-1 - Pass ProgramDocument529 pagesCoursebook-1 - Pass Programbobbyparera69% (16)
- A Series of Catastrophes and MiraclesDocument9 pagesA Series of Catastrophes and Miracleswamu8850% (1)
- Medical - Surgical Nursing 3 & 4: Final ExaminationsDocument6 pagesMedical - Surgical Nursing 3 & 4: Final ExaminationsBRYAN JOSEPH TIONGSON100% (1)
- CREOG OutlineDocument68 pagesCREOG OutlineadfsnkdfNo ratings yet
- Does The Sequence of Anthracycline and Taxane Matter? The Neosamba TrialDocument7 pagesDoes The Sequence of Anthracycline and Taxane Matter? The Neosamba Trialyujliyur naveenNo ratings yet
- GynaecologicalCancerChemoProtocols PDFDocument7 pagesGynaecologicalCancerChemoProtocols PDFRyan IlhamNo ratings yet
- Aoki 2002Document10 pagesAoki 2002Drsaumyta MishraNo ratings yet
- 5 Fracciones RT CA MAMA - FAST-Forward To IMPLEMENTACION 2021Document10 pages5 Fracciones RT CA MAMA - FAST-Forward To IMPLEMENTACION 2021hugo francisco romero anduagaNo ratings yet
- Annonc mdw587.026Document1 pageAnnonc mdw587.026Aaron Paul BernasNo ratings yet
- EBRT in DTCDocument7 pagesEBRT in DTCElena FlorentinaNo ratings yet
- 166440996249740030Document10 pages166440996249740030111No ratings yet
- Lsteele, CBN 2017 3 36-40Document5 pagesLsteele, CBN 2017 3 36-40Mohammad AlrefaiNo ratings yet
- TraztuzumabDocument8 pagesTraztuzumabArlina Wiyata GamaNo ratings yet
- Curran 2011Document9 pagesCurran 2011Nguyễn Hoàng PhúcNo ratings yet
- 1 s2.0 S1028455922001346 MainDocument2 pages1 s2.0 S1028455922001346 MainMutia Paramadita AnugrahNo ratings yet
- Glynne Jones2015Document3 pagesGlynne Jones2015Robert ChristevenNo ratings yet
- Cad 26 1054Document7 pagesCad 26 1054Nico PantoroNo ratings yet
- Neoadjuvant Chemotherapy in Advanced-Stage Ovarian Cancer - State of The Art. 2022Document4 pagesNeoadjuvant Chemotherapy in Advanced-Stage Ovarian Cancer - State of The Art. 2022Prodromos KoutoukoglouNo ratings yet
- Clinical Treatment of Ovarian Cancer First Line Chemotherapy or Targeted Therapy For Recurrent CasesDocument4 pagesClinical Treatment of Ovarian Cancer First Line Chemotherapy or Targeted Therapy For Recurrent CasesEditor IJTSRDNo ratings yet
- Acs 06 02 167Document8 pagesAcs 06 02 167MixalisKaplanisNo ratings yet
- MeduloblastomaDocument7 pagesMeduloblastomasilvia erfanNo ratings yet
- First-Line Gemcitabine and Carboplatin in Advanced Ovarian Carcinoma: A Phase II StudyDocument5 pagesFirst-Line Gemcitabine and Carboplatin in Advanced Ovarian Carcinoma: A Phase II Studyatikha apriliaNo ratings yet
- Journal ClubDocument56 pagesJournal ClubDr. Ankita singhNo ratings yet
- Surgery of Primary in de Novo Metastatic CaDocument28 pagesSurgery of Primary in de Novo Metastatic CaMariajanNo ratings yet
- 013 - Surgeon-Led-Clinical-Trials-in-Pancrea - 2023 - Surgical-Oncology-Clinics-of-NorDocument9 pages013 - Surgeon-Led-Clinical-Trials-in-Pancrea - 2023 - Surgical-Oncology-Clinics-of-NorDr-Mohammad Ali-Fayiz Al TamimiNo ratings yet
- NPCDocument8 pagesNPCArsy Mira PertiwiNo ratings yet
- 961 FullDocument5 pages961 FullWilliyoNo ratings yet
- RT en Pancreas Horowitz 2021Document2 pagesRT en Pancreas Horowitz 2021Carlos N. Rojas PuyolNo ratings yet
- Adjuvant ChemotheraphyDocument10 pagesAdjuvant ChemotheraphyFatona AgungNo ratings yet
- Bradley J Monk First Line Pembrolizumab ChemotherapyDocument9 pagesBradley J Monk First Line Pembrolizumab ChemotherapyRaúl DíazNo ratings yet
- 10 1016@j LPM 2019 02 025Document15 pages10 1016@j LPM 2019 02 025Paulina Sobarzo VegaNo ratings yet
- Adjuvant RadiotherapyDocument7 pagesAdjuvant Radiotherapyciko momonNo ratings yet
- 1 s2.0 S0302283823030208 MainDocument10 pages1 s2.0 S0302283823030208 MainJoy IsmailNo ratings yet
- Heitz Et Al 2011 Surgery For Recurrent Ovarian CancerDocument7 pagesHeitz Et Al 2011 Surgery For Recurrent Ovarian Cancerhop truongvanNo ratings yet
- 31576697Document8 pages31576697Ahana MukherjeeNo ratings yet
- Cancer of The EsophagusDocument6 pagesCancer of The EsophagusDileep SrinivasanNo ratings yet
- Journal Report: Running Head: (Shortened Title Up To 50 Characters) 1Document4 pagesJournal Report: Running Head: (Shortened Title Up To 50 Characters) 1Ahmed NawazNo ratings yet
- Sfakianos 2015Document7 pagesSfakianos 2015nimaelhajjiNo ratings yet
- Survival With Cemiplimab in Recurrent Cervical CancerDocument12 pagesSurvival With Cemiplimab in Recurrent Cervical CancerKassem HijazyNo ratings yet
- Icmcrj 1 1013Document12 pagesIcmcrj 1 1013Shivaramakrishna SriramojuNo ratings yet
- 2018 - Breast and Ovarian Cancer - BMC Cancer - BauersfeldDocument10 pages2018 - Breast and Ovarian Cancer - BMC Cancer - BauersfeldHouda BouachaNo ratings yet
- Topical Chemotherapy For Penile Carcinoma in Situ Contemporary Outcomes and Reported ToxicityDocument5 pagesTopical Chemotherapy For Penile Carcinoma in Situ Contemporary Outcomes and Reported ToxicityEdgar GarciaNo ratings yet
- QUAD. 0 7 21 RegimenDocument6 pagesQUAD. 0 7 21 RegimenEskadmas BelayNo ratings yet
- 9 Randomized Phase III Evaluation of Cisplatin PlusDocument6 pages9 Randomized Phase III Evaluation of Cisplatin Plustrifamonika23No ratings yet
- 1 s2.0 S0965229906000926 MainDocument10 pages1 s2.0 S0965229906000926 MainUtami DewiNo ratings yet
- Eligibility Criteria: Previous Sectionnext SectionDocument6 pagesEligibility Criteria: Previous Sectionnext Sectionbettzy21No ratings yet
- Goserelinversuscyclophosphamide, Methotrexate, and Fluorouracilasadjuvanttherapyinpremenopausalpatients Withnode-Positivebreastcancer:Thezoladexearlybreast CancerresearchassociationstudyDocument11 pagesGoserelinversuscyclophosphamide, Methotrexate, and Fluorouracilasadjuvanttherapyinpremenopausalpatients Withnode-Positivebreastcancer:Thezoladexearlybreast CancerresearchassociationstudyRaksha MoghariyaNo ratings yet
- EVIDoa 2200015Document11 pagesEVIDoa 2200015Gustavo BraccoNo ratings yet
- Estudo HERA Herceptin 2005Document14 pagesEstudo HERA Herceptin 2005Thayná AraújoNo ratings yet
- Zhang COR 2022Document12 pagesZhang COR 2022icemoonNo ratings yet
- Nejmoa 2104162Document11 pagesNejmoa 2104162GwasuNo ratings yet
- De Novo Stage 4 Metastatic Breast Cancer: A Surgical Disease?Document3 pagesDe Novo Stage 4 Metastatic Breast Cancer: A Surgical Disease?jenmercadoNo ratings yet
- Maintenance Therapy With AromataseDocument13 pagesMaintenance Therapy With Aromatasen2763288No ratings yet
- 3 254 1 PBDocument5 pages3 254 1 PBbeepboop20No ratings yet
- Intergroup 0123Document8 pagesIntergroup 0123radonc17No ratings yet
- Background: Nivolumab For Recurrent Squamous-Cell Carcinoma of The Head and NeckDocument10 pagesBackground: Nivolumab For Recurrent Squamous-Cell Carcinoma of The Head and NeckjoitNo ratings yet
- Oral Intake of Ginger For Chemotherapy-Induced Nausea and Vomiting Among Women With Breast CancerDocument11 pagesOral Intake of Ginger For Chemotherapy-Induced Nausea and Vomiting Among Women With Breast Cancerermylia pravestyNo ratings yet
- Cisplatin-Based Adjuvant Chemotherapy in Patients With Completely Resected Non-Small-Cell Lung CancerDocument10 pagesCisplatin-Based Adjuvant Chemotherapy in Patients With Completely Resected Non-Small-Cell Lung CancerSouvik SahaNo ratings yet
- CA ServiksDocument10 pagesCA ServiksAndi Farid ANo ratings yet
- DJN 498Document9 pagesDJN 498dz fiddinNo ratings yet
- Capecitabine Monotherapy For Recurrent and Metastatic Nasopharyngeal CancerDocument6 pagesCapecitabine Monotherapy For Recurrent and Metastatic Nasopharyngeal Cancertrifamonika23No ratings yet
- Nejmoa 2032125Document13 pagesNejmoa 2032125CARLOS DURANNo ratings yet
- Klafke 2015Document22 pagesKlafke 2015Irna SulistiyaniNo ratings yet
- Nej Me 068121Document2 pagesNej Me 068121anissakikinNo ratings yet
- How To Calculate The Dose of Chemotherapy: Short CommunicationDocument6 pagesHow To Calculate The Dose of Chemotherapy: Short CommunicationShivam DuttaNo ratings yet
- Acute LeukemiaDocument4 pagesAcute LeukemiaRonald Cszar Fabian VillanoNo ratings yet
- Quiz Hematology Oncology Part 2 of 2Document60 pagesQuiz Hematology Oncology Part 2 of 2MedShare100% (5)
- Theodore Hong, Prajnan Das (Eds.) - Radiation Therapy For Gastrointestinal Cancers (2017, Springer InternatiDocument244 pagesTheodore Hong, Prajnan Das (Eds.) - Radiation Therapy For Gastrointestinal Cancers (2017, Springer InternatiTolga ŞanlıNo ratings yet
- Cancer CaDocument6 pagesCancer CaRocco WalksNo ratings yet
- Antibiotic (Bacteriostatic) DrugsDocument15 pagesAntibiotic (Bacteriostatic) DrugsVictor LeeNo ratings yet
- Pediatric Concept MapDocument6 pagesPediatric Concept Mapapi-507427888No ratings yet
- Ozone - A Wide Spectrum Healer by Gary Null PHDDocument20 pagesOzone - A Wide Spectrum Healer by Gary Null PHDangelakimba100% (4)
- Medicinal Plants From Farm To Pharmacy 2019 PDFDocument445 pagesMedicinal Plants From Farm To Pharmacy 2019 PDFJesús Gabriel Múnera Baloco100% (3)
- 2014 Book InflammationAndCancer PDFDocument489 pages2014 Book InflammationAndCancer PDFGustavo Alejandro Malvaez OlguinNo ratings yet
- On05 6 2 01Document8 pagesOn05 6 2 01aoife123No ratings yet
- Carg in Asian ElderlyDocument13 pagesCarg in Asian ElderlySarly Puspita AriesaNo ratings yet
- Antimicrobial AgentsDocument34 pagesAntimicrobial Agentssuchi_mohan08No ratings yet
- Biology Stem CellsDocument1 pageBiology Stem CellsmimiNo ratings yet
- Thesis - S.UDHAYAKUMAR FinalDocument41 pagesThesis - S.UDHAYAKUMAR FinalMuthuraman ArNo ratings yet
- Cancers of The Blood: Leukemia and LymphomaDocument46 pagesCancers of The Blood: Leukemia and LymphomaMaica LectanaNo ratings yet
- Anticancer Activity of Bioactive Compounds From Kaempferia Rotunda Rhizome Against Human Breast CancerDocument8 pagesAnticancer Activity of Bioactive Compounds From Kaempferia Rotunda Rhizome Against Human Breast CancerLivia TanjungNo ratings yet
- Mushroom Growers Handbook 2 Shiitake Cultivation - 2005 - Mushworld - 17391377 - 256pgDocument256 pagesMushroom Growers Handbook 2 Shiitake Cultivation - 2005 - Mushworld - 17391377 - 256pgAdrian Alberto Romero BernalNo ratings yet
- Kalanchoe Review 11101 - 2017 - Article - 9525 PDFDocument17 pagesKalanchoe Review 11101 - 2017 - Article - 9525 PDFAnonymous iOYpj92No ratings yet
- NCM 106 Course OutlineDocument5 pagesNCM 106 Course Outlinedennisreveni100% (1)
- Cancer Is A Survival MechanismDocument25 pagesCancer Is A Survival Mechanismisabelle1371No ratings yet
- Mon Anemia and CancerDocument10 pagesMon Anemia and CancertyasNo ratings yet
- Acta Poloniae Pharmaceutica Ñ Drug Research, Vol. 68 No. 3 Pp. 357ñ373, 2011Document17 pagesActa Poloniae Pharmaceutica Ñ Drug Research, Vol. 68 No. 3 Pp. 357ñ373, 2011Willy CoioteNo ratings yet
- Fournel 2020Document9 pagesFournel 2020tim yuNo ratings yet
- Current Clinical Strategies of Pancreatic CancerDocument28 pagesCurrent Clinical Strategies of Pancreatic CancerfikriafisNo ratings yet
F - BCBCR Five Year Follow Up of Patients With Early Stage Breast Cancer After2.pdf - 4610
F - BCBCR Five Year Follow Up of Patients With Early Stage Breast Cancer After2.pdf - 4610
Uploaded by
Windy HardiyantyOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
F - BCBCR Five Year Follow Up of Patients With Early Stage Breast Cancer After2.pdf - 4610
F - BCBCR Five Year Follow Up of Patients With Early Stage Breast Cancer After2.pdf - 4610
Uploaded by
Windy HardiyantyCopyright:
Available Formats
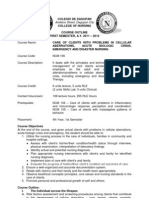
Breast Cancer: Basic and Clinical Research
Open Access
Full open access to this and
thousands of other papers at
O igin Re e h
http://www.la-press.com.
Five-Year Follow-Up of atients with arly tage Breast ancer
After a Randomized tudy omparing Additional Treatment
with Viscum Album (L.) xtract to hemotherapy Alone
Wilfried Tröger1, Zdravko Ždrale2, Nikola Stanković3 and Miodrag Matijašević2
1
Clinical Research Dr. Tröger, Freiburg, ermany. 2 nstitute of Oncology and Radiology of Serbia, Belgrade, Serbia.
3
Clinicobss, iš, Serbia. Corresponding author email: troeger@crdt.de
Abstract: Additional therapy with extracts of Viscum album [L.] (VaL) increases the quality of life of patients suffering from early stage
breast cancer during chemotherapy. In the current study patients received chemotherapy, consisting of six cycles of cyclophosphamide,
anthracycline, and 5-Fluoro-Uracil (CAF). Two groups also received one of two VaL extracts differing in their preparation as subcutaneous
injection three times per week. A control group received CAF with no additional therapy. Six of 28 patients in one of the VaL groups
and eight of 29 patients in the control group developed relapse or metastasis within 5 years. Subgroup analysis for hormone- and radio-
therapy also showed no difference between groups. Additional VaL therapy during chemotherapy of early stage breast cancer patients
appears not to influence the frequency of relapse or metastasis within 5 years.
Keywords: mistletoe therapy, chemotherapy, breast cancer, randomized clinical trial, disease-free survival rate, 5-year follow-up
Breast Cancer: Basic and Clinical Research 2012:6 173–180
doi: 10.4137/BCBCR.S10558
This article is available from http://www.la-press.com.
© the author(s), publisher and licensee Libertas Academica Ltd.
This is an open access article. Unrestricted non-commercial use is permitted provided the original work is properly cited.
Breast Cancer: Basic and Clinical Research 2012:6 173
Tröger et al
Introduction tion to the chemotherapy. Here we report the results
Background of one of the VaL groups compared to the control
Viscum album[L.] (VaL) extracts are widely used in group. Results of the other VaL group compared to
cancer therapy in central Europe. In general, VaL is the control group will be published elsewhere. The
administered during and after conventional therapies patients did not continue VaL therapy after the end of
like surgery, chemo-, hormone-, or radiotherapy and chemotherapy. The aim of the study was to show the
lasts for several years. Clinical evidence suggests that impact of VaL therapy in addition to chemotherapy on
VaL influences the immune system1 and increases quality of life, as assessed by the European Organiza-
quality of life.2 Recently, a randomized trial examin- tion for Research and Treatment of Cancer Quality
ing VaL showed a significant and relevant prolonga- of Life Questionnaire (EORTC-QLQ-C30), as well as
tion of overall survival in late-stage pancreatic cancer its impact on the frequency of neutropenia. In one of
patients compared to untreated controls.3 Therefore, the groups treated with VaL extract, all 15 scores of
VaL is claimed to be used in both adjuvant and pallia- the EORTC-QLQ-C30 showed better quality of life
tive situations of cancer therapy. in the VaL group as compared to the control group. In
Patients with early stage breast cancer regularly 12 scores the differences were significant (P , 0.02),
undergo chemotherapy after surgery in order to pre- with nine scores showing a clinically relevant and sig-
vent relapse and metastasis. Often, the combination of nificant difference of at least 5 points.17 Neutropenia
cyclophosphamide, anthracycline, and 5-fluorouracil occurred in 3/30 VaL patients and in 8/31 control
(CAF) is used. The side effects of these chemothera- patients (P = 0.182). None of the patients received
pies include nausea, emesis, pain, and fatigue. Fatigue VaL therapy after the end of chemotherapy, but some
is regarded as one of the major concerns for patients patients in both groups began hormone therapy or
with cancer4 and is related to reduced activity, depres- underwent radiotherapy. In this non-interventional
sion, anxiety, and mood disorders.5,6 Subcutaneous 5-year follow-up, the frequency of relapses and
injection of VaL additionally applied to chemother- metastases of all patients was documented.
apy is regularly used to decrease chemotherapy side
effects (e.g. neutropenia) and to increase the quality Methods
of life, and has been examined in twelve random- Objectives
ized clinical trials.7–18 Theoretically, higher quality of The objective of this 5-year follow-up study is to ana-
life and less neutropenia of patients receiving addi- lyze whether VaL therapy in addition to chemotherapy
tional VaL therapy to chemotherapy may lead to the has an influence on the median disease-free survival
assumption that VaL reduces the toxicity (and with time as well as the total frequency of relapses and
this, the efficacy) of chemotherapeutics. Although metastases in patients with early stage breast cancer.
VaL increases the cytotoxicity of chemotherapy on
malignant cells,19 additional VaL therapy is still under Design
discussion. A clinical evaluation is overdue. This is a prospective non-interventional follow-up
VaL therapy is traditionally continued after chemo- study of two patient groups after participation in a ran-
therapy for several years in order to prevent relapses domized clinical trial. None of the patients received
and metastases. Therefore, no documentation of VaL extract after the end of the chemotherapy. Ethi-
relapse and metastasis exists that reports long-term cal approval was obtained from Institute for Oncology
results of the use of VaL limited to the duration of and Radiology of Serbia. All patients provided written
chemotherapy. informed consent before commencing participation.
In a prospective randomized clinical trial,
95 patients suffering from early stage breast cancer Participants
were randomized into three groups.17 All three groups Breast cancer patients in stages T1–3N0–2M0 treated at
received chemotherapy consisting of six cycles of the Institute of Oncology and Radiology, National
CAF. Two of the three groups received one of two VaL Cancer Research Centre of Serbia in Belgrade
extracts from two different manufacturers in addi- who received six consecutive cycles of CAF after
174 Breast Cancer: Basic and Clinical Research 2012:6
Mistletoe therapy during chemotherapy: a 5-year follow-up
surgery were included. For participation in the long included 28 of 30 patients of the VaL group and 29
term follow-up, the following inclusion criteria of 30 patients of the control group in this analysis
were obligatory: patients should have had 6 cycles (see Fig. 1). The follow-up began in June 2006 and
of chemotherapy, should definitively not have had ended in May 2012.
metastases before the chemotherapy began, and
should not have refused to participate in the study. nterventions
Two patients in the VaL group had an unknown meta- All patients have had CAF therapy administered in six
static status (M = x) before the chemotherapy began, cycles with a three-week interval between each cycle.
and one patient in the control group did not give her The applied dose intensities (DI) of cyclophosph-
consent for continued participation. Therefore, we amide, Adriamycin, and 5-FU (DI in mean mg/m² per
Assessed for eligibility n = 123
Other VaL therapy
Randomized (1:1:1) n = 95
n = 34
Inclusion of 61 patients
Control group
VaL group
- Six cycles CAF (500 mg/50 mg/500 mg)
- Six cycles CAF (500 mg/50 mg/500 mg) within 18 weeks, every 3rd week
within 18 weeks, every 3rd week
Allocation
- VaL 54 s.c. injections within 18 weeks - No additional therapy
3x weekly (0.01 mg–5 mg)
- Received VaL n = 30 - Received VaL n=0
- Did not receive VaL n=0 - Did not receive VaL n = 31
Drop-out Drop-out
None n=0 Heart disease n=1
Analysis of quality of life and neutropenia(17)
Analysis
Analysed n = 30 Analysed n = 30
Patients excluded Patients excluded
from 5-year follow-up: from 5-year follow-up:
Selection
Reasons: Reasons:
- M = X at inclusion n=2 - M = X at inclusion n=0
- Refused to participate n=0 - Refused to participate n=1
Analysis of 5-year disease-free survival
Analysis
Analysed n = 28 Analysed n = 29
Figure 1. Flow chart according to CO SORT.
Abbreviation: CAF, cyclophosphamide/adriamycin/5-fluorouracil.
Breast Cancer: Basic and Clinical Research 2012:6 175
Tröger et al
week, ±standard deviation) were 160.5 ± 5.6, 16.1 ± 0.6, Wallis test, and t-test were used to check the balance
and 160.5 ± 5.6, respectively, in the VaL group of demographic and clinical baseline characteristics
and 159.4 ± 7.3, 15.9 ± 0.7, and 159.4 ± 7.3, respectively, as well as for the therapies after chemotherapy. The
in the control group. The results correspond to 98% of disease-free survival curves were calculated by the
planned DI in the VaL group and 97% of planned DI Kaplan-Meier method and compared between study
in the control group. No other antineoplastic or immu- groups using a log-rank test (Cox-Mantel).
nomodulating therapies were applied during chemo-
therapy. All patients received antiemetic therapy with Results
a single dose of ondansetron chloride 8 mg, dexam- Baseline and treatment data
ethasone 8 mg, and ranitidine 50 mg, respectively, The baseline data of the two groups are well balanced
administered prior to each CAF cycle. (Table 1).
Patients randomly allocated to additional therapy After chemotherapy and VaL therapy ended,
with VaL received Iscador®M special, a fermented patients underwent other therapies, which may have
aqueous extract of VaL from apple tree (ratio of influenced the disease-free survival rate. There-
plant to extract = 1:5), manufactured by Weleda AG, fore, other therapies were documented in both
Schwäbisch Gmünd, Germany. VaL comes in 1 mL groups. The most frequent therapies were adjuvant
ampoules for injection and each ampoule contains radiotherapy (n = 37) and anti-hormonal therapy
the fermented extract of 0.01, 0.1, 1, 2, or 5 mg of (tamoxifen; n = 32; Table 2). Both therapies were
fresh extract of VaL, respectively, in isotonic saline well balanced between the study groups and have
solution. VaL was administered by subcutaneous been analyzed as separate subgroups (Figs. 3 and
injections of 1 mL into the upper abdominal region 4). Other therapies were trastuzumab (n = 4), goser-
three times per week (e.g. Monday, Wednesday, elin (n = 2), docetaxel (n = 1), and letrozole (n = 1;
Friday). The patients in the VaL group were instructed Table 2). The latter therapies in total were also well
to inject themselves subcutaneously. The dosage of balanced between the groups, but their frequency of
VaL was increased stepwise: 2 × 0.01 mg, 2 × 0.1 mg, application was too small to represent subgroups for
11 × 1 mg, 8 × 2 mg, remaining doses 5 mg. An an analysis.
average of 53.8 ± 2.6 injections with altogether
174.0 ± 26.6 mg of VaL per patient were administered Disease-free survival
in the VaL group. The median disease-free survival time could not be
The control group did not receive additional VaL calculated, because the highest probability for relapse
therapy to chemotherapy. or metastasis in 5 years was 28%. The disease-free
5-year survival rates were 6/28 and 8/29 patients in
Outcomes the VaL and the control groups, respectively (Fig. 2).
Occurrence of relapse and/or metastasis was docu- The difference was not statistically significant
mented annually up to 5 years during the prescribed (P = 0.551; Cox-Mantel log-rank test).
routine follow-up visits of the study centre. The results The subgroup analysis of patients undergoing
were documented in case report forms designed for radiotherapy yielded 4/19 and 3/18 patients in the
this study. A deviation of ±2 months was tolerated VaL and the control group, respectively (Fig. 3); the
for the annual visits. The follow-up for an individual subgroup analyses of patients with anti-hormonal
patient ended with the occurrence of a relapse or a therapy yielded 4/18 and 4/14 patients in the VaL and
metastasis. control group, respectively (Fig. 4). None of the dif-
ferences were statistically significant (Fisher’s exact
Statistical methods test P = 0.792 and P = 0.659, respectively).
Statistical analysis (StatExact V9.0, WinStat
V2012.1) included all participating patients. All Discussion
results are of exploratory nature and may serve for No studies have examined the impact of medica-
hypothesis building or sample size calculation. The ments like analgesics, antiemetics, antibiotics or VaL
Mann-Whitney test, Fisher’s exact test, Kruskal- routinely used in parallel to chemotherapy, taking
176 Breast Cancer: Basic and Clinical Research 2012:6
Mistletoe therapy during chemotherapy: a 5-year follow-up
Table 1. Baseline status.
Group P values
VaL n = 28 ontrol n = 29
Age at inclusion
patients 28 (100%) 29 (100%)
Median 47.5 52.9 P(MWT) = 0.175
Range 35 to 61.6 32.5 to 66.8
Mean ± SD 49.0 ± 7.8 51.8 ± 7.8 P(TT) = 0.169
BM
patients 28 (100%) 29 (100%)
Median 26.0 25.6 P(MWT) = 0.444
Range 18.9 to 52.1 18.7 to 33.4
Mean ± SD 27.0 ± 6.3 25.5 ± 4.7 P(TT) = 0.316
Karnofsky P(F T) = 1.000
100 28 (100%) 29 (100%)
Stage (U CC) P(KWT) = 0.990
2 (7%) 4 (14%)
25 (89%) 22 (76%)
1 (4%) 3 (10%)
Tumour classification T P(KWT) = 0.594
1 6 (21%) 9 (31%)
2 20 (71%) 17 (59%)
3 1 (4%) 2 (7%)
X 1 (4%) 1 (3%)
Positive lymph nodes P(KWT) = 0.200
0 10 (36%) 16 (55%)
1 18 (64%) 12 (41%)
2 0 (0%) 1 (3%)
Metastasis M P(F T) = 1.000
0 28 (100%) 29 (100%)
Tumour grade P(KWT) = 1.000
1 0 (0%) 0 (0%)
2 24 (86%) 24 (83%)
3 4 (14%) 5 (17%)
L taken out P(MWT) = 0.762
Median 15 15
Range 5 to 22 8 to 32
patients 28 (100%) 29 (100%)
L affected P(MWT) = 0.641
Median 1 1
Range 0 to 8 0 to 8
patients 28 (100%) 29 (100%)
Menopausal status P(F T) = 0.407
Pre 15 (54%) 11 (38%)
Peri 2 (7%) 1 (3%)
Post 11 (39%) 17 (59%)
Receptor status oestrogen P(F T) = 0.545
+ 19 (68%) 16 (55%)
- 7 (25%) 11 (38%)
n.d. 2 (7%) 2 (7%)
Receptor status progesterone P(F T) = 1.000
+ 17 (61%) 18 (62%)
- 9 (32%) 9 (31%)
n.d. 2 (7%) 2 (7%)
Abbreviations: MWT, Mann-Whitney-test; TT, t-test; F T, Fisher’s exact test, KWT, Kruskal-Wallis-test.
Breast Cancer: Basic and Clinical Research 2012:6 177
Tröger et al
Table 2. Therapies after chemotherapy (CAF). 100%
Group P values
VaL ontrol
VaL additionaly to CAF (18 weeks)
n = 28 n = 29 75%
Radiotherapy P(F T) = 0.783
Probability
Radiotherapy 19 (68%) 18 (62%)
(50 ray) 50%
one 9 (31%) 11 (39%)
Tamoxifen P(F T) = 0.289 Disease-free survival
Tamoxifen 18 (64%) 14 (48%) Control: 3/18
(20 mg/d) 25%
VaL: 4/19
P = 0.792
one 10 (36%) 15 (52%) Log-rank-test
Other therapies P(F T) = 0.730 (Cox-mantel)
Other 5 (18%) 4 (14%)
therapies 0%
one 23 (82%) 25 (86%) 0 1 2 3 4 5
Disease free survival (in years)
Abbreviation: F T, Fisher’s exact test. Number of disease free patients:
Control: 18 18 18 17 16 15
VaL: 19 18 18 17 17 15
relapse and metastasis into consideration. In the case Figure 3. Disease-free interval of patients receiving radiotherapy.
of VaL, patients reported an increase in quality of life,
and a reduction of neutropenia was detected during
the additional use of VaL during chemotherapy. disease-free survival rate compared to a control group
Therefore, it may be assumed that the reduction of receiving chemotherapy alone, and also yielded no
the clinical toxicity of the chemotherapy also leads indication that subsequently started therapies were
to a reduction of its efficacy. In this study the addi- influenced in any way. Moreover, the clinical ben-
tional VaL therapy during chemotherapy of patients efit of additional VaL therapy during chemotherapy
with early stage breast cancer did not affect the 5-year may prevent patients from dropping out or delaying
100% 100%
IVaL additionaly to CAF (18 weeks)
VaL additionaly to CAF (18 weeks)
75% 75%
Probability
Probability
50% 50%
Disease-free survival Disease-free survival
Control: 8/29 Control: 4/14
VaL: 6/28 VaL: 4/18
25% 25%
P = 0.551 P = 0.659
Log-rank-test Log-rank-test
(Cox-mantel) (Cox-mantel)
0% 0%
0 1 2 3 4 5 0 1 2 3 4 5
Disease free survival (in years) Disease free survival (in years)
Number of disease free patients: Number of disease free patients:
Control: 29 28 26 24 22 21 Control: 14 14 12 11 10 10
VaL: 28 27 25 24 24 22 VaL: 18 18 16 15 15 14
Figure 2. Disease-free interval of all patients. Figure 4. Disease-free interval of patients receiving tamoxifen.
178 Breast Cancer: Basic and Clinical Research 2012:6
Mistletoe therapy during chemotherapy: a 5-year follow-up
Table 3. Outcomes of patients with different relevant prog- Further research on drug combinations should be
nosis factors. conducted.
rognostic factor umber of patients
with events onclusion
Group VaL therapy in addition to chemotherapy increases the
VaL ontrol quality of life of patients with early stage breast can-
cer and may prevent neutropenia. In the current study
U CC = 3 – –
T (T M ) = 3 – – no negative influence of additional Val therapy on the
(T M ) . 0 4 4 effectiveness of chemotherapy of patients with early
(T M ) = 3 – – stage breast cancer was detected, referring to the fre-
Receptor status 1 1 quency of relapse or metastasis within 5 years.
oestrogen = negative
Acknowledgements
chemotherapy cycles. Speculations about a possible We like to thank the participating patients and the
negative impact of additional VaL therapy on the study nurse Z. Ranđeljović.
efficacy of the chemotherapy are not founded. On the
contrary: VaL increases the cytotoxicity of chemo- Funding
therapeutics if added in cell culture assays; VaL and The study was financially supported by the Society
chemotherapeutics have been used with good results for Cancer Research, Arlesheim, Switzerland.
since decades and this prospective study shows no
disadvantages of the additional use of VaL to chemo- Author ontributions
therapy during a 5-year follow-up regarding relapses MM and ZZ were investigators. NS carried out the
and metastases. monitoring and quality assurance, WT was the prin-
A strength of this study is that VaL treatment only cipal author of the paper, wrote the study protocol,
occurs for the duration of chemotherapy. Because of coordinated the study, had full access to all data, and
this strength, results cannot be biased by a continu- is guarantor. All authors read and approved the final
ation of VaL therapy, which may have had a further manuscript.
impact on the disease free survival rate.
The low sample size used in this study limits its ompeting Interests
generalizability, and calls for confirmation using Author(s) disclose no potential conflicts of interest.
larger clinical trials. A statistical confirmation of non-
inferiority for combined VaL/chemotherapy com- thics
pared to chemotherapy alone would require about The sponsor had no influence on study design, plan-
1,000 patients per group.20 ning, conduct or analysis. Besides the approval of the
The results suggest that there is a small advan- Ethics Committee of the National Cancer Research
tage from VaL therapy in the number of disease-free Center of Serbia without modifications (No. 16-05
patients after five years. This advantage may be due dated: 3rd October 2005) no further decision was
to a slight prognostic advantage for the patients in necessary for this non-interventional observation
the VaL group regarding age, frequency of UICC study.
(III, T = 3, N . 0, G = 3), and receptor status (oestro-
gen = negative). As no differences in the frequency References
1. Büssing A. Immune modulation using mistletoe (Viscum album L.) extracts
of relapse and metastasis occurred in both groups Iscador. Arzneimittelforschung. 2006;56(6A):508–15.
regarding these factors, therefore, only the differ- 2. Kienle GS, Kiene H. Influence of Viscum Album L. (European Mistletoe)
extracts on quality of life in cancer patients: a systematic review of controlled
ence in age (2.8 years) may have influenced results clinical studies. Integr Cancer Ther. 2010;9(2):142–57.
(Table 3). 3. Galun D, Tröger W, Reif M, Schumann A, Stankovic N, Milicevic M.
The study results support the use of VaL Mistletoe extract therapy versus no antineoplastic therapy in patients with
locally advanced or metastatic pancreatic cancer: a randomized clinical
therapy in addition to chemotherapy, in con- phase III trial on overall survival. Annals of Oncology. 2012;23(Suppl 9):
trast to objections against this type of treatment. ix237.
Breast Cancer: Basic and Clinical Research 2012:6 179
Tröger et al
4. Butt Z, Rosenbloom SK, Abernethy AP, et al. Fatigue is the most important 13. Piao BK, Wang YX, Xie GR, et al. Impact of complementary mistletoe
symptom for advanced cancer patients who have had chemotherapy. J Natl extract treatment on quality of life in breast, ovarian and non-small cell
Compr Canc Netw. 2008;6(5):448–55. lung cancer patients. A prospective randomized controlled clinical trial.
5. de Jong N, Candel MJ, Schouten HC, Abu-Saad HH, Courtens AM. Course Anticancer Res. 2004;24(1):303–9.
of mental fatigue and motivation in breast cancer patients receiving adju- 14. Salzer G, Denck H. Randomisierte Studie über medikamentöse
vant chemotherapy. Ann Oncol. 2005;16(3):372–82. Rezidivprophylaxe mit 5-Fluorouracil und Iscador beim resezierten Magen-
6. Goldstein D, Bennett B, Friedlander M, Davenport T, Hickie I, Lloyd A. karzinom—Ergebnisse einer Zwischenauswertung. Krebsgeschehen. 1979;
Fatigue states after cancer treatment occur both in association with, and 11(5):130–1.
independent of, mood disorder: a longitudinal study. BMC Cancer. Oct 9, 15. Salzer G, Havelec L. Adjuvante Iscador-Behandlung nach operiertem
2006;6(1):240. Magenkarzinom. Ergebnisse einer randomisierten Studie. Krebsgeschehen.
7. Auerbach L, Dostal V, Václavik-Fleck I, et al. Signifikant höherer Anteil 1983;15(4):106–10.
aktivierter NK-Zellen durch additive Misteltherapie bei chemotherapierten 16. Salzer G, Danmayr E, Wutzlhofer F, Frey S. Adjuvante Iscador-Behandlung
Mamma-Ca-Patientinnen in einer prospektiven randomisierten doppelblin- operierter nicht kleinzelliger Bronchuskarzinome. Dtsch Zschr Onkol.
den Studie. In: Scheer R, Bauer R, Becker H, Fintelmann V, Kemper FH, 1991;23(4):93–8.
Schilcher H, editors. Fortschritte in der Misteltherapie. Aktueller Stand der 17. Tröger W, Jezdic S, Zdrale Z, Tisma N, Hamre HJ, Mattijasevic M. Quality
Forschung und klinischen Anwendung. 2005; Essen: KCV Verlag. of life and neutropenia in patients with early stage breast cancer: a random-
8. Douwes FR, Wolfrum DI, Migeod F. Ergebnisse einer prospektiv ran- ized pilot study comparing additional treatment with mistletoe extract to
domisierten Studie: Chemotherapie versus Chemotherapie plus “Biological chemotherapy alone. Breast Cancer: (Auckl). 2009;3:35–45.
Response Modifier” bei metastasierendem kolorektalen Karzinom. 18. von Hagens A, Loewe-Mesch A, Kuehn JJ, Abel U, Gerhard I. Prospektive
Krebsgeschehen. 1986;18(6):155–63. kontrollierte nicht randomisierte Machbarkeits-Studie zu einer post-
9. Douwes FR, Kalden M, Frank G, Holzhauer P. Behandlung des fortgeschrit- operativen simultanen Mistel-/Chemotherapie bei Patientinnen mit
tenen kolorektalen Karzinoms. Dtsch Zschr Onkol. 1988;20(3):63–7. Mammakarzinom—Ergebnisse zu Rekrutier- und Randomisierbarkeit,
10. Eisenbraun J, Huber R, Kröz M, Schad F, Scheer R. Lebensqualität von Immunparametern, Lebensqualität und Verträglichkeit. In: Scheer R,
Brustkrebs-Patientinnen während der Chemotherapie und einer begleiten- Bauer R, Becker H, Fintelmann V, Kemper FH, Schilcher H, editors.
den Therapie mit einem Apfelbaum-Mistelextrakt. In: Scheer R, Alban S, Fortschritte in der Misteltherapie. Aktueller Stand der Forschung und
Becker H, Holzgrabe U, Kemper FH, Kreis W, et al, editors. Die Mistel klinischen Anwendung. 2005; Essen: KCV Verlag.
in der Tumortherapie 2. Aktueller Stand der Forschung und klinische 19. Büssing A, Jurin M, Zarkovic N, Azhari T, Schweizer K. DNA-
Anwendung. 2009; Essen: KVC Verlag. stabilisierende Wirkungen von Viscum album L.—Sind Mistelextrakte als
11. Gutsch J, Kühne A. Pharmakologische und klinische Erfahrung mit dem Adjuvans während der konventionellen Chemotherapie indiziert? Forsch
Mistelextrakt Helixor. Die Heilkunst. 1986;99:156–72. Komplementärmed Klass Naturheilkd. 1996;3:244–8.
12. Loewe-Mesch A, Kuehn JH, Borho K, et al. Adjuvante simultane Mistel-/ 20. Schoenfeld DA. The asymptotic properties of nonparametric tests for com-
Chemotherapie bei Mammakarzinom—Einfluss auf Immunparameter, paring survival distributions. Biometrika. 1981;68:316–9.
Lebensqualität und Verträglichkeit. Forschende Komplementärmedizin.
2008;15(1):22–30.
180 Breast Cancer: Basic and Clinical Research 2012:6
You might also like
- Coursebook-1 - Pass ProgramDocument529 pagesCoursebook-1 - Pass Programbobbyparera69% (16)
- A Series of Catastrophes and MiraclesDocument9 pagesA Series of Catastrophes and Miracleswamu8850% (1)
- Medical - Surgical Nursing 3 & 4: Final ExaminationsDocument6 pagesMedical - Surgical Nursing 3 & 4: Final ExaminationsBRYAN JOSEPH TIONGSON100% (1)
- CREOG OutlineDocument68 pagesCREOG OutlineadfsnkdfNo ratings yet
- Does The Sequence of Anthracycline and Taxane Matter? The Neosamba TrialDocument7 pagesDoes The Sequence of Anthracycline and Taxane Matter? The Neosamba Trialyujliyur naveenNo ratings yet
- GynaecologicalCancerChemoProtocols PDFDocument7 pagesGynaecologicalCancerChemoProtocols PDFRyan IlhamNo ratings yet
- Aoki 2002Document10 pagesAoki 2002Drsaumyta MishraNo ratings yet
- 5 Fracciones RT CA MAMA - FAST-Forward To IMPLEMENTACION 2021Document10 pages5 Fracciones RT CA MAMA - FAST-Forward To IMPLEMENTACION 2021hugo francisco romero anduagaNo ratings yet
- Annonc mdw587.026Document1 pageAnnonc mdw587.026Aaron Paul BernasNo ratings yet
- EBRT in DTCDocument7 pagesEBRT in DTCElena FlorentinaNo ratings yet
- 166440996249740030Document10 pages166440996249740030111No ratings yet
- Lsteele, CBN 2017 3 36-40Document5 pagesLsteele, CBN 2017 3 36-40Mohammad AlrefaiNo ratings yet
- TraztuzumabDocument8 pagesTraztuzumabArlina Wiyata GamaNo ratings yet
- Curran 2011Document9 pagesCurran 2011Nguyễn Hoàng PhúcNo ratings yet
- 1 s2.0 S1028455922001346 MainDocument2 pages1 s2.0 S1028455922001346 MainMutia Paramadita AnugrahNo ratings yet
- Glynne Jones2015Document3 pagesGlynne Jones2015Robert ChristevenNo ratings yet
- Cad 26 1054Document7 pagesCad 26 1054Nico PantoroNo ratings yet
- Neoadjuvant Chemotherapy in Advanced-Stage Ovarian Cancer - State of The Art. 2022Document4 pagesNeoadjuvant Chemotherapy in Advanced-Stage Ovarian Cancer - State of The Art. 2022Prodromos KoutoukoglouNo ratings yet
- Clinical Treatment of Ovarian Cancer First Line Chemotherapy or Targeted Therapy For Recurrent CasesDocument4 pagesClinical Treatment of Ovarian Cancer First Line Chemotherapy or Targeted Therapy For Recurrent CasesEditor IJTSRDNo ratings yet
- Acs 06 02 167Document8 pagesAcs 06 02 167MixalisKaplanisNo ratings yet
- MeduloblastomaDocument7 pagesMeduloblastomasilvia erfanNo ratings yet
- First-Line Gemcitabine and Carboplatin in Advanced Ovarian Carcinoma: A Phase II StudyDocument5 pagesFirst-Line Gemcitabine and Carboplatin in Advanced Ovarian Carcinoma: A Phase II Studyatikha apriliaNo ratings yet
- Journal ClubDocument56 pagesJournal ClubDr. Ankita singhNo ratings yet
- Surgery of Primary in de Novo Metastatic CaDocument28 pagesSurgery of Primary in de Novo Metastatic CaMariajanNo ratings yet
- 013 - Surgeon-Led-Clinical-Trials-in-Pancrea - 2023 - Surgical-Oncology-Clinics-of-NorDocument9 pages013 - Surgeon-Led-Clinical-Trials-in-Pancrea - 2023 - Surgical-Oncology-Clinics-of-NorDr-Mohammad Ali-Fayiz Al TamimiNo ratings yet
- NPCDocument8 pagesNPCArsy Mira PertiwiNo ratings yet
- 961 FullDocument5 pages961 FullWilliyoNo ratings yet
- RT en Pancreas Horowitz 2021Document2 pagesRT en Pancreas Horowitz 2021Carlos N. Rojas PuyolNo ratings yet
- Adjuvant ChemotheraphyDocument10 pagesAdjuvant ChemotheraphyFatona AgungNo ratings yet
- Bradley J Monk First Line Pembrolizumab ChemotherapyDocument9 pagesBradley J Monk First Line Pembrolizumab ChemotherapyRaúl DíazNo ratings yet
- 10 1016@j LPM 2019 02 025Document15 pages10 1016@j LPM 2019 02 025Paulina Sobarzo VegaNo ratings yet
- Adjuvant RadiotherapyDocument7 pagesAdjuvant Radiotherapyciko momonNo ratings yet
- 1 s2.0 S0302283823030208 MainDocument10 pages1 s2.0 S0302283823030208 MainJoy IsmailNo ratings yet
- Heitz Et Al 2011 Surgery For Recurrent Ovarian CancerDocument7 pagesHeitz Et Al 2011 Surgery For Recurrent Ovarian Cancerhop truongvanNo ratings yet
- 31576697Document8 pages31576697Ahana MukherjeeNo ratings yet
- Cancer of The EsophagusDocument6 pagesCancer of The EsophagusDileep SrinivasanNo ratings yet
- Journal Report: Running Head: (Shortened Title Up To 50 Characters) 1Document4 pagesJournal Report: Running Head: (Shortened Title Up To 50 Characters) 1Ahmed NawazNo ratings yet
- Sfakianos 2015Document7 pagesSfakianos 2015nimaelhajjiNo ratings yet
- Survival With Cemiplimab in Recurrent Cervical CancerDocument12 pagesSurvival With Cemiplimab in Recurrent Cervical CancerKassem HijazyNo ratings yet
- Icmcrj 1 1013Document12 pagesIcmcrj 1 1013Shivaramakrishna SriramojuNo ratings yet
- 2018 - Breast and Ovarian Cancer - BMC Cancer - BauersfeldDocument10 pages2018 - Breast and Ovarian Cancer - BMC Cancer - BauersfeldHouda BouachaNo ratings yet
- Topical Chemotherapy For Penile Carcinoma in Situ Contemporary Outcomes and Reported ToxicityDocument5 pagesTopical Chemotherapy For Penile Carcinoma in Situ Contemporary Outcomes and Reported ToxicityEdgar GarciaNo ratings yet
- QUAD. 0 7 21 RegimenDocument6 pagesQUAD. 0 7 21 RegimenEskadmas BelayNo ratings yet
- 9 Randomized Phase III Evaluation of Cisplatin PlusDocument6 pages9 Randomized Phase III Evaluation of Cisplatin Plustrifamonika23No ratings yet
- 1 s2.0 S0965229906000926 MainDocument10 pages1 s2.0 S0965229906000926 MainUtami DewiNo ratings yet
- Eligibility Criteria: Previous Sectionnext SectionDocument6 pagesEligibility Criteria: Previous Sectionnext Sectionbettzy21No ratings yet
- Goserelinversuscyclophosphamide, Methotrexate, and Fluorouracilasadjuvanttherapyinpremenopausalpatients Withnode-Positivebreastcancer:Thezoladexearlybreast CancerresearchassociationstudyDocument11 pagesGoserelinversuscyclophosphamide, Methotrexate, and Fluorouracilasadjuvanttherapyinpremenopausalpatients Withnode-Positivebreastcancer:Thezoladexearlybreast CancerresearchassociationstudyRaksha MoghariyaNo ratings yet
- EVIDoa 2200015Document11 pagesEVIDoa 2200015Gustavo BraccoNo ratings yet
- Estudo HERA Herceptin 2005Document14 pagesEstudo HERA Herceptin 2005Thayná AraújoNo ratings yet
- Zhang COR 2022Document12 pagesZhang COR 2022icemoonNo ratings yet
- Nejmoa 2104162Document11 pagesNejmoa 2104162GwasuNo ratings yet
- De Novo Stage 4 Metastatic Breast Cancer: A Surgical Disease?Document3 pagesDe Novo Stage 4 Metastatic Breast Cancer: A Surgical Disease?jenmercadoNo ratings yet
- Maintenance Therapy With AromataseDocument13 pagesMaintenance Therapy With Aromatasen2763288No ratings yet
- 3 254 1 PBDocument5 pages3 254 1 PBbeepboop20No ratings yet
- Intergroup 0123Document8 pagesIntergroup 0123radonc17No ratings yet
- Background: Nivolumab For Recurrent Squamous-Cell Carcinoma of The Head and NeckDocument10 pagesBackground: Nivolumab For Recurrent Squamous-Cell Carcinoma of The Head and NeckjoitNo ratings yet
- Oral Intake of Ginger For Chemotherapy-Induced Nausea and Vomiting Among Women With Breast CancerDocument11 pagesOral Intake of Ginger For Chemotherapy-Induced Nausea and Vomiting Among Women With Breast Cancerermylia pravestyNo ratings yet
- Cisplatin-Based Adjuvant Chemotherapy in Patients With Completely Resected Non-Small-Cell Lung CancerDocument10 pagesCisplatin-Based Adjuvant Chemotherapy in Patients With Completely Resected Non-Small-Cell Lung CancerSouvik SahaNo ratings yet
- CA ServiksDocument10 pagesCA ServiksAndi Farid ANo ratings yet
- DJN 498Document9 pagesDJN 498dz fiddinNo ratings yet
- Capecitabine Monotherapy For Recurrent and Metastatic Nasopharyngeal CancerDocument6 pagesCapecitabine Monotherapy For Recurrent and Metastatic Nasopharyngeal Cancertrifamonika23No ratings yet
- Nejmoa 2032125Document13 pagesNejmoa 2032125CARLOS DURANNo ratings yet
- Klafke 2015Document22 pagesKlafke 2015Irna SulistiyaniNo ratings yet
- Nej Me 068121Document2 pagesNej Me 068121anissakikinNo ratings yet
- How To Calculate The Dose of Chemotherapy: Short CommunicationDocument6 pagesHow To Calculate The Dose of Chemotherapy: Short CommunicationShivam DuttaNo ratings yet
- Acute LeukemiaDocument4 pagesAcute LeukemiaRonald Cszar Fabian VillanoNo ratings yet
- Quiz Hematology Oncology Part 2 of 2Document60 pagesQuiz Hematology Oncology Part 2 of 2MedShare100% (5)
- Theodore Hong, Prajnan Das (Eds.) - Radiation Therapy For Gastrointestinal Cancers (2017, Springer InternatiDocument244 pagesTheodore Hong, Prajnan Das (Eds.) - Radiation Therapy For Gastrointestinal Cancers (2017, Springer InternatiTolga ŞanlıNo ratings yet
- Cancer CaDocument6 pagesCancer CaRocco WalksNo ratings yet
- Antibiotic (Bacteriostatic) DrugsDocument15 pagesAntibiotic (Bacteriostatic) DrugsVictor LeeNo ratings yet
- Pediatric Concept MapDocument6 pagesPediatric Concept Mapapi-507427888No ratings yet
- Ozone - A Wide Spectrum Healer by Gary Null PHDDocument20 pagesOzone - A Wide Spectrum Healer by Gary Null PHDangelakimba100% (4)
- Medicinal Plants From Farm To Pharmacy 2019 PDFDocument445 pagesMedicinal Plants From Farm To Pharmacy 2019 PDFJesús Gabriel Múnera Baloco100% (3)
- 2014 Book InflammationAndCancer PDFDocument489 pages2014 Book InflammationAndCancer PDFGustavo Alejandro Malvaez OlguinNo ratings yet
- On05 6 2 01Document8 pagesOn05 6 2 01aoife123No ratings yet
- Carg in Asian ElderlyDocument13 pagesCarg in Asian ElderlySarly Puspita AriesaNo ratings yet
- Antimicrobial AgentsDocument34 pagesAntimicrobial Agentssuchi_mohan08No ratings yet
- Biology Stem CellsDocument1 pageBiology Stem CellsmimiNo ratings yet
- Thesis - S.UDHAYAKUMAR FinalDocument41 pagesThesis - S.UDHAYAKUMAR FinalMuthuraman ArNo ratings yet
- Cancers of The Blood: Leukemia and LymphomaDocument46 pagesCancers of The Blood: Leukemia and LymphomaMaica LectanaNo ratings yet
- Anticancer Activity of Bioactive Compounds From Kaempferia Rotunda Rhizome Against Human Breast CancerDocument8 pagesAnticancer Activity of Bioactive Compounds From Kaempferia Rotunda Rhizome Against Human Breast CancerLivia TanjungNo ratings yet
- Mushroom Growers Handbook 2 Shiitake Cultivation - 2005 - Mushworld - 17391377 - 256pgDocument256 pagesMushroom Growers Handbook 2 Shiitake Cultivation - 2005 - Mushworld - 17391377 - 256pgAdrian Alberto Romero BernalNo ratings yet
- Kalanchoe Review 11101 - 2017 - Article - 9525 PDFDocument17 pagesKalanchoe Review 11101 - 2017 - Article - 9525 PDFAnonymous iOYpj92No ratings yet
- NCM 106 Course OutlineDocument5 pagesNCM 106 Course Outlinedennisreveni100% (1)
- Cancer Is A Survival MechanismDocument25 pagesCancer Is A Survival Mechanismisabelle1371No ratings yet
- Mon Anemia and CancerDocument10 pagesMon Anemia and CancertyasNo ratings yet
- Acta Poloniae Pharmaceutica Ñ Drug Research, Vol. 68 No. 3 Pp. 357ñ373, 2011Document17 pagesActa Poloniae Pharmaceutica Ñ Drug Research, Vol. 68 No. 3 Pp. 357ñ373, 2011Willy CoioteNo ratings yet
- Fournel 2020Document9 pagesFournel 2020tim yuNo ratings yet
- Current Clinical Strategies of Pancreatic CancerDocument28 pagesCurrent Clinical Strategies of Pancreatic CancerfikriafisNo ratings yet