Professional Documents
Culture Documents
Acute Tick-Borne Disease Testing Algorithm
Acute Tick-Borne Disease Testing Algorithm
Uploaded by
Simon WHookOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Acute Tick-Borne Disease Testing Algorithm
Acute Tick-Borne Disease Testing Algorithm
Uploaded by
Simon WHookCopyright:
Available Formats
Acute Tick-Borne Disease Testing Algorithm
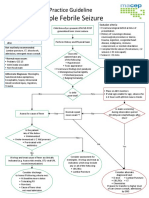
Clinical suspicion of tick-borne disease based on patient characteristics:
■ Illness during tick season: fever, chills, headache, muscle aches, joint pain, neck pain,
skin rash, Bell’s palsy, heart rhythm disturbances, hypotension, jaundice, sepsis
AND
■ Known tick exposure
OR
■ Environmental exposure (outdoor activities, wildlife)
Based on geographic exposure, consider the following
tick-borne pathogens (choose all that are appropriate)
At risk for Rocky Mountain Spotted Fever ■ At risk for Lyme disease, ehrlichiosis, anaplasmosis, babesiosis, and Borrelia
(states with the highest incidence include North miyamotoi disease (BMD)
Carolina, Oklahoma, Arkansas, Tennessee, ■ Endemic areas for Lyme disease, anaplasmosis, babesiosis, and BMD
Missouri, Arizona, and the tribal Southwest) include the Northeastern and Upper Midwestern United States, into Canada
■ Ehrlichiosis is most frequently reported from the Southeastern and South
Central United States
Yes Yes
SFGP / Spotted Fever Group Antibody, IgG and IgM, Serum Classic erythema migrans (target
Consider empiric treatment while awaiting test results lesion or bull’s-eye rash)
NegAtive Positive No Yes
Consider empiric treatment for ehrlichiosis/
anaplasmosis while awaiting test results
■ Report as negative Treat as
■ If short disease duration, appropriate
submit follow-up specimen ■ Perform LYME / Lyme Disease Serology, Serum (Enzyme- ■ No laboratory testing for
for repeat testing in 2-3 Linked Immunosorbent Assay) Lyme disease is needed
weeks if clinically indicated ■ For patients with exposure to ticks in Europe, consider ■ Treat for Lyme disease
ELYME / Lyme Disease European Antibody Screen, Serum ■ Monitor for symptoms of
■ If systemic symptoms are present (eg, fever, chills, sepsis) other tick-borne illness
also perform TKPNL / Tick-Borne Panel, Molecular
Detection, PCR, Blood1,2
■ Consider collecting baseline serology (TICKS / Tick-Borne
Disease Antibodies Panel, Serum) if patient presents with
>7 days of symptoms
TKPNL Results LYME or ELYME Results
NegAtive Positive NegAtive Positive or eQUivoCAL
■ Report as negative Treat as Report as negative ■ LYWB / Lyme Disease Antibody, Immunoblot,
■ If short disease duration, consider follow-up appropriate ■ If short disease duration, submit Serum (performed automatically when LYME
specimen for serologic tests in 2-3 weeks if follow-up specimen for repeat testing result is positive or equivocal)
clinically indicated using: TICKS / Tick-Borne in 2-3 weeks if clinically indicated ■ ELYMI / Lyme Disease European Immunoblot,
Disease Antibodies Panel, Serum (includes Serum (performed automatically when ELYME
Lyme disease serology) result is positive or equivocal
OR
■ Individual serologic tests:
■ BABG / Babesia microti IgG Antibodies, Serum
NegAtive Positive
■ ANAP / Anaplasma phagocytophilum (Human
Granulocytic Ehrlichiosis) Antibody, Serum
■ EHRCP / Ehrlichia Antibody Panel, Serum
■ Report as negative ■ Treat as appropriate
■ If short disease duration, submit follow-up specimen for ■ If neurologic or joint symptoms, consider
repeat testing if clinically indicated PBORR / Lyme Disease, Molecular Detection,
■ In immunocompromised patient, consider PBORR / Lyme PCR (for CSF, synovial fluid, or fresh tissue
Disease, Molecular Detection, PCR (for CSF, synovial fluid, samples)
or fresh tissue samples) OR
AND/OR ■ LNBAB / Lyme CNS Infection IgG with
PBORB / Lyme Disease, Molecular Detection, PCR, Blood3 Antibody Index Reflex
1
The TKPNL includes PCR tests for Babesia species, Anaplasma phagocytophilum, Ehrlichia species, and Borrelia miyamotoi.
2
In place of the PCR panel, PCR tests for the individual organisms and/or smear for Babesia species can be ordered based on the suspected organism(s).
3
PCR testing of blood may be useful for detection of Borrelia mayonii (patients with exposure to ticks in Minnesota or Wisconsin).
See Lyme Neuroborreliosis Diagnostic Algorithm for more information.
© Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Reviewed 09/2018
02/2018
You might also like
- University of Tennessee Religious ExemptionDocument3 pagesUniversity of Tennessee Religious ExemptionDonnaNo ratings yet
- Reading Part A ShinglesDocument6 pagesReading Part A Shinglesfernanda1rondelliNo ratings yet
- SeizuresDocument33 pagesSeizuresLubinda SitaliNo ratings yet
- Pid 1 86Document9 pagesPid 1 86SandraNo ratings yet
- Is Module 14Document33 pagesIs Module 14gladyskheyagamNo ratings yet
- ImmunoSeroLab M4Document3 pagesImmunoSeroLab M4ela kikayNo ratings yet
- Sti Lecture NotesDocument8 pagesSti Lecture NotesSTACEY SALVILLANo ratings yet
- Ilovepdf MergedDocument408 pagesIlovepdf MergedSAKSHI DUBEYNo ratings yet
- NeurosyphilisDocument2 pagesNeurosyphiliserfNo ratings yet
- Communicable Diseases 1 Vector Borne DiseasesDocument13 pagesCommunicable Diseases 1 Vector Borne DiseasesManaswi DebbermaNo ratings yet
- Comparison of The Effects of Clobazam and Diazepam in Prevention of Recurrent Febrile SeizuresDocument2 pagesComparison of The Effects of Clobazam and Diazepam in Prevention of Recurrent Febrile SeizuresCharina Geofhany DeboraNo ratings yet
- Hubers MayoClinProc 2019 SuppDocument1 pageHubers MayoClinProc 2019 SuppDaniel LupuNo ratings yet
- Part 2 Exam FM - 2021Document70 pagesPart 2 Exam FM - 2021rahafas95No ratings yet
- All About Fever 6Document42 pagesAll About Fever 6brajendra singhNo ratings yet
- B. 11 Situation - Care of Client With Problems in Inflammatory & Immunologic ResponseDocument4 pagesB. 11 Situation - Care of Client With Problems in Inflammatory & Immunologic ResponseSOLEIL LOUISE LACSON MARBAS100% (1)
- Antinuclear Antibody ANADocument3 pagesAntinuclear Antibody ANAanaelisabetapNo ratings yet
- Immunohematology Handouts UpdatedDocument15 pagesImmunohematology Handouts UpdateddmclmllNo ratings yet
- Auto Immune Hemolytic Anemia: Dr. Devesh A. Tiwari Pediatric Hematology Oncology LTMMC & GHDocument37 pagesAuto Immune Hemolytic Anemia: Dr. Devesh A. Tiwari Pediatric Hematology Oncology LTMMC & GHdrdeveshNo ratings yet
- Concept MapDocument10 pagesConcept MapStephen YorNo ratings yet
- Diagnostic and Therapeutic Challenges of Primary Autoimmune Haemolytic Anaemia in ChildrenDocument7 pagesDiagnostic and Therapeutic Challenges of Primary Autoimmune Haemolytic Anaemia in ChildrenAdrian KhomanNo ratings yet
- Pediatric Emergency Medicine Resource 33164 - CSDY - FeverDocument7 pagesPediatric Emergency Medicine Resource 33164 - CSDY - FevervannesNo ratings yet
- Concept MapDocument10 pagesConcept MapStephen Yor100% (1)
- Is Lab WeekDocument3 pagesIs Lab Weekkimmynemil80No ratings yet
- ICSI Stroke June2019 v2Document55 pagesICSI Stroke June2019 v2PerwiraNo ratings yet
- H008019 Resolving ABO Discrepancies E 2017 01Document2 pagesH008019 Resolving ABO Discrepancies E 2017 01Wei Leng OngNo ratings yet
- Model Poster MedicinaDocument1 pageModel Poster MedicinaGabriela BichirNo ratings yet
- Daisy LabReportDocument1 pageDaisy LabReportosky35No ratings yet
- Ascpi Recalls 1Document10 pagesAscpi Recalls 1Ben SabladaNo ratings yet
- Marc Leone Ten Tips On Fever 2023Document4 pagesMarc Leone Ten Tips On Fever 2023aleifelNo ratings yet
- Syphilis in ChildrenDocument16 pagesSyphilis in ChildrenFatmi Eka PutriNo ratings yet
- Laboratory-Diagnosis-Yellow - Fever-September-2018Document8 pagesLaboratory-Diagnosis-Yellow - Fever-September-2018FirmanHidayatNo ratings yet
- Seizure New Onset Clinical PathwayDocument17 pagesSeizure New Onset Clinical PathwayKim Shyen BontuyanNo ratings yet
- Ten Tips On FeverDocument4 pagesTen Tips On FeverOscar F RojasNo ratings yet
- Benign Febrile Seizure: PediatricsDocument2 pagesBenign Febrile Seizure: PediatricsKrista P. AguinaldoNo ratings yet
- 22 Neonatal SepsisDocument2 pages22 Neonatal Sepsisokwadha simionNo ratings yet
- Diagnosis and Management of Paediatric Autoimmune Hepatitis AIH. ESPGHAN Advice Guide. 2019. Ver1.Document4 pagesDiagnosis and Management of Paediatric Autoimmune Hepatitis AIH. ESPGHAN Advice Guide. 2019. Ver1.Carmen OpreaNo ratings yet
- Fana TrainingDocument174 pagesFana TrainingHaidee SaavedraNo ratings yet
- Febrile Phase Iii. Recovery PhaseDocument7 pagesFebrile Phase Iii. Recovery PhaseMaman Lubnaa LafeefNo ratings yet
- Spirochetes 2023Document42 pagesSpirochetes 2023Ahmed khanNo ratings yet
- BB Lec - Topic 14 - AIHADocument3 pagesBB Lec - Topic 14 - AIHAcarvajalraizzaeloisseNo ratings yet
- PRN Aids ms3Document197 pagesPRN Aids ms3jeremiahNo ratings yet
- Evaluating A Patient With Seizure Disorders 2Document47 pagesEvaluating A Patient With Seizure Disorders 2Yvonne Sorviel SiiloNo ratings yet
- Hayats ResponsesDocument18 pagesHayats Responsesyacineone01No ratings yet
- Principles of Serodiagnosis: Ms. Piyumali Arachchi Mphil (Usjp) BSC (Uoc)Document26 pagesPrinciples of Serodiagnosis: Ms. Piyumali Arachchi Mphil (Usjp) BSC (Uoc)Nipun ShamikaNo ratings yet
- Syphilis Amen 07 13 2017Document43 pagesSyphilis Amen 07 13 2017ambiliNo ratings yet
- Allergy and Immunology 2023 FINALDocument18 pagesAllergy and Immunology 2023 FINALBelinda ELISHANo ratings yet
- Lecture - HypersensitivityDocument52 pagesLecture - Hypersensitivityrockyrawat01012003No ratings yet
- CERTIFICATE OF HEALTH (To Be Filled Out by A Physician) - Page 1Document2 pagesCERTIFICATE OF HEALTH (To Be Filled Out by A Physician) - Page 1gnzbdbNo ratings yet
- Respiratory Viral IllnessDocument43 pagesRespiratory Viral IllnessSiti TiaraNo ratings yet
- Case Presentation Febrile Neutropenia NizarDocument25 pagesCase Presentation Febrile Neutropenia NizarNizar IJNo ratings yet
- Toronto Internal Medicine Review 2024Document2,189 pagesToronto Internal Medicine Review 2024luz carime CorreaNo ratings yet
- Anti-SM (SLE) & RFDocument46 pagesAnti-SM (SLE) & RFjulesarojineeNo ratings yet
- Mtap - Immunohema Transfusion MedicineDocument9 pagesMtap - Immunohema Transfusion MedicineMoira Pauline LibroraniaNo ratings yet
- Henoch-Scholein Purpura - 240524 - 092956Document15 pagesHenoch-Scholein Purpura - 240524 - 092956dakwah mujahadahNo ratings yet
- HLH Diagnostic AlgorithmDocument2 pagesHLH Diagnostic AlgorithmHammad MuhammadNo ratings yet
- Assessment and Management of Unconscious PatientDocument10 pagesAssessment and Management of Unconscious PatientDebasis SahooNo ratings yet
- Pharmacologic Management of Neuropsychiatric Lupus: Expert Review of Clinical PharmacologyDocument7 pagesPharmacologic Management of Neuropsychiatric Lupus: Expert Review of Clinical PharmacologyNungki TriandariNo ratings yet
- Sindrome de Fiebre PeriodicaDocument10 pagesSindrome de Fiebre PeriodicaHakundusNo ratings yet
- 2-Syphilis Congenital PKEL FinalDocument24 pages2-Syphilis Congenital PKEL FinalGilang KusdinarNo ratings yet
- Anti - Infectives AgentsDocument83 pagesAnti - Infectives AgentsRhien Yrah P. CabalongaNo ratings yet
- Efta Triastuti Study Program of Pharmacy Faculty of Medicine - Brawijaya UniversityDocument33 pagesEfta Triastuti Study Program of Pharmacy Faculty of Medicine - Brawijaya UniversityWidi Alya ZhafiraNo ratings yet
- Vitdpositionstatement FINAL 20121210 - 0Document3 pagesVitdpositionstatement FINAL 20121210 - 0Simon WHookNo ratings yet
- RDP 403 Levey Jennings Chart - ExampleDocument1 pageRDP 403 Levey Jennings Chart - ExampleSimon WHookNo ratings yet
- 003 NURSE Standard Medical V005.1.05122017Document5 pages003 NURSE Standard Medical V005.1.05122017Simon WHookNo ratings yet
- G181 Key Assurance Indicators For Pathology ServicesDocument26 pagesG181 Key Assurance Indicators For Pathology ServicesSimon WHookNo ratings yet
- Transfusion Medicine - 2012 - Guidelines For Pre Transfusion Compatibility Procedures in Blood Transfusion LaboratoriesDocument33 pagesTransfusion Medicine - 2012 - Guidelines For Pre Transfusion Compatibility Procedures in Blood Transfusion LaboratoriesSimon WHookNo ratings yet
- 6th Charles Merieux Conference 2019 Criteria For Blood Smear ReviewDocument5 pages6th Charles Merieux Conference 2019 Criteria For Blood Smear ReviewSimon WHookNo ratings yet
- Edwin Mwangi Zool 143 Assgn 6Document3 pagesEdwin Mwangi Zool 143 Assgn 6nattydreadfathelahNo ratings yet
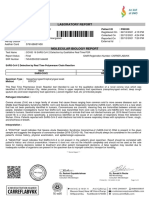
- Laboratory Report: Name: MR .Sandeep Mane Patient ID: P80359Document1 pageLaboratory Report: Name: MR .Sandeep Mane Patient ID: P80359akash srivastavaNo ratings yet
- Alcantara, Charmine Swab PDFDocument1 pageAlcantara, Charmine Swab PDFJohnmar AquinoNo ratings yet
- Department of Education: Republic of The PhilippinesDocument2 pagesDepartment of Education: Republic of The PhilippinesEizen DivinagraciaNo ratings yet
- Multidrug-Resistant Tuberculosis: Agus Suharto BasukiDocument45 pagesMultidrug-Resistant Tuberculosis: Agus Suharto BasukidrhendraagusNo ratings yet
- Hiv and The Nigerian ChildDocument3 pagesHiv and The Nigerian ChildÀàrẹ ÀgòNo ratings yet
- Crosswords Human HealthDocument1 pageCrosswords Human HealthRiana Ab RahmanNo ratings yet
- Daily Time Record Daily Time RecordDocument4 pagesDaily Time Record Daily Time RecordInchic MirandaNo ratings yet
- Zika VirusDocument2 pagesZika VirusYousef Hassan BazarNo ratings yet
- Penatalaksanaan Mouth Preparation Pada Anak Dengan Kelainan Jantung Bawaan Tipe Atrial Septal Defect Di Bawah Anestesi UmumDocument5 pagesPenatalaksanaan Mouth Preparation Pada Anak Dengan Kelainan Jantung Bawaan Tipe Atrial Septal Defect Di Bawah Anestesi Umumnonaviona_nonavionaNo ratings yet
- Abm-11-D Viernesfritzie M4 Fil-AkadDocument3 pagesAbm-11-D Viernesfritzie M4 Fil-AkadIsha Manzano Lacuesta100% (1)
- Egg Inoculation Techniques: Dr. R. KalaimathiDocument53 pagesEgg Inoculation Techniques: Dr. R. Kalaimathiprakyy2kNo ratings yet
- Icd10cm Codes 2018Document1,786 pagesIcd10cm Codes 2018alvin bramantyoNo ratings yet
- Daftar PustakaDocument4 pagesDaftar PustakaAmelia AlresnaNo ratings yet
- ImpetigoDocument3 pagesImpetigoLauraNo ratings yet
- Eb Harp February Aidsreg2019Document7 pagesEb Harp February Aidsreg2019Prince AshannaNo ratings yet
- New Form Pelaporan Tahap 2 Termin 2Document36 pagesNew Form Pelaporan Tahap 2 Termin 2bambangNo ratings yet
- Position Paper - El SalvadorDocument2 pagesPosition Paper - El SalvadorLily KazemiNo ratings yet
- Pathognomonic Signs of Communicable Diseases: JJ8009 Health & NutritionDocument2 pagesPathognomonic Signs of Communicable Diseases: JJ8009 Health & NutritionMauliza Resky NisaNo ratings yet
- Zuku Visual Flashnotes Distemper CondensedDocument1 pageZuku Visual Flashnotes Distemper CondensedRayza LubisNo ratings yet
- Hansen's DiseaseDocument11 pagesHansen's Diseasekellie_byrd_1No ratings yet
- Childcod Estimates 2000 2017Document1,024 pagesChildcod Estimates 2000 2017Rafa NaufalinNo ratings yet
- Icd 10 Excell NewDocument491 pagesIcd 10 Excell Newlilik fitriatulNo ratings yet
- Revised National TB Control ProgramDocument12 pagesRevised National TB Control ProgramsaurabhNo ratings yet
- White Blue Modern Marine Pollution InfographicDocument2 pagesWhite Blue Modern Marine Pollution InfographicJanella Mae C. RiegoNo ratings yet
- Info GraphicsDocument1 pageInfo GraphicsMay Ann RosalesNo ratings yet
- Harsh PatientReportDocument1 pageHarsh PatientReportHarsh GuptaNo ratings yet
- Infections:: Jadwal Acara Pelatihan In-Alarm Hari II: Minggu, 28 Februari 2021 Waktu Menit Acara Pembicara AbsensiDocument1 pageInfections:: Jadwal Acara Pelatihan In-Alarm Hari II: Minggu, 28 Februari 2021 Waktu Menit Acara Pembicara AbsensiClarestaNo ratings yet