Professional Documents
Culture Documents
0 ratings0% found this document useful (0 votes)
12 views(PH156) 14 CSF, Transudates, Exudates, and Other Fluids
(PH156) 14 CSF, Transudates, Exudates, and Other Fluids
Uploaded by
Rosshlein Marian YangsonCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You might also like
- Stuxnet and Its Hidden Lessons On The Ethics of CyberweaponsDocument9 pagesStuxnet and Its Hidden Lessons On The Ethics of CyberweaponsprofcameloNo ratings yet
- Aubf Lec - Serous FluidDocument12 pagesAubf Lec - Serous FluidColene MoresNo ratings yet
- B.F Lecture 8 Serous F.analysisDocument23 pagesB.F Lecture 8 Serous F.analysisSalah AbassNo ratings yet
- 2023.LabDx - Trans05.Serous Effusion & Synovial FluidDocument4 pages2023.LabDx - Trans05.Serous Effusion & Synovial FluidstellaNo ratings yet
- Serous FluidDocument1 pageSerous FluidJl OiraNo ratings yet
- AUBF Serous FluidDocument7 pagesAUBF Serous FluidRichelyn Grace B. VenusNo ratings yet
- 5766 Serous FluidsDocument21 pages5766 Serous FluidsAdeniyi AkisekuNo ratings yet
- Pa Tho Physiology of Cavitary EffusionDocument11 pagesPa Tho Physiology of Cavitary EffusionybaeumliNo ratings yet
- Sysmex Educational Enhancement and Development SEED Body FluidsDocument6 pagesSysmex Educational Enhancement and Development SEED Body FluidsbalkisNo ratings yet
- Unit 3 - Transudates and Exudates IIIDocument17 pagesUnit 3 - Transudates and Exudates IIIRubina KhatunNo ratings yet
- SerousDocument8 pagesSerouspekibelssNo ratings yet
- Nursing Foundation 2 Module 6Document6 pagesNursing Foundation 2 Module 6johnbryanmalonesNo ratings yet
- Clase 8 - Examen de Efusiones Torácicas y Abdominales: MVZ Renato Zúñiga FDocument69 pagesClase 8 - Examen de Efusiones Torácicas y Abdominales: MVZ Renato Zúñiga FLisette Velásquez AnticonaNo ratings yet
- Pmls 2 Prelim To FinalsDocument25 pagesPmls 2 Prelim To FinalsisyandanNo ratings yet
- Clinical Microscopy:: Case Study AnalysisDocument12 pagesClinical Microscopy:: Case Study Analysischocoholic potchiNo ratings yet
- Hematology PreliminariesDocument7 pagesHematology PreliminariesRomie SolacitoNo ratings yet
- Cytology of Body FluidDocument28 pagesCytology of Body FluidMalliga SundareshanNo ratings yet
- Serous Fluid Powerpoint HandoutDocument3 pagesSerous Fluid Powerpoint HandoutAnonymous ceYk4p4No ratings yet
- SEROUS-FLUID NotesDocument5 pagesSEROUS-FLUID NotesSpongebob SquarepantsNo ratings yet
- LESSON 8 Special Collection and Point-Of-Care TestingDocument2 pagesLESSON 8 Special Collection and Point-Of-Care TestingAlthea EspirituNo ratings yet
- AUBF Lec M Microscopic Examination of Urine Sediment Part 1Document11 pagesAUBF Lec M Microscopic Examination of Urine Sediment Part 1Haniah DsNo ratings yet
- Fluid and Electrolyte ReplacementDocument60 pagesFluid and Electrolyte ReplacementAlex WagnerNo ratings yet
- Lesson 10Document6 pagesLesson 10GelaaaNo ratings yet
- MLS305 Hema Lab PrelimsDocument11 pagesMLS305 Hema Lab PrelimsEvanka BaguistanNo ratings yet
- Serous Fluid Hand OutDocument3 pagesSerous Fluid Hand OutAhmed AboamerNo ratings yet
- 7 - Fluid Balance - AntinDocument55 pages7 - Fluid Balance - AntinHelen PratiwiNo ratings yet
- Aubf Lec Week 15Document7 pagesAubf Lec Week 15Joanne RemolloNo ratings yet
- Specimen ConsiderationsDocument17 pagesSpecimen ConsiderationsRace MendezNo ratings yet
- Serous Fluid: Presented By: Pauline BautistaDocument13 pagesSerous Fluid: Presented By: Pauline BautistaPauline BautistaNo ratings yet
- Blood Physiology LectureDocument174 pagesBlood Physiology Lectureemmanuelakinola2006No ratings yet
- Body FluidsDocument24 pagesBody FluidsMohamed MidoNo ratings yet
- PMLS 2 Unit 8Document4 pagesPMLS 2 Unit 8Elyon Jirehel AlvarezNo ratings yet
- Sampling: Assistant Instructor. Jinan Hameed Source By:-Practical Clinical BiochemistryDocument24 pagesSampling: Assistant Instructor. Jinan Hameed Source By:-Practical Clinical BiochemistryaddwrNo ratings yet
- Serous Fluid: FormationDocument4 pagesSerous Fluid: FormationemmanuelNo ratings yet
- Exudative Pleural Effusion: Approach To Management: Medicine UpdateDocument10 pagesExudative Pleural Effusion: Approach To Management: Medicine UpdateMukti MuliantoNo ratings yet
- Intravenous Fluids PDFDocument10 pagesIntravenous Fluids PDFGReadRNo ratings yet
- Review of Laboratory and Diagnostic TestsDocument25 pagesReview of Laboratory and Diagnostic TestsCrystal CireraNo ratings yet
- Body Fluids Analysis LectureDocument17 pagesBody Fluids Analysis LectureAsd Asd100% (1)
- Blood TransfusionDocument4 pagesBlood TransfusionYalc LapidNo ratings yet
- Maternal 2 - Blood TransfusionDocument5 pagesMaternal 2 - Blood TransfusionJuliana Anne RamosNo ratings yet
- Specimen Collection HandoutDocument7 pagesSpecimen Collection HandoutCelne CentinoNo ratings yet
- Body Fluids Tsilioni SlidesDocument31 pagesBody Fluids Tsilioni SlidesShaira Jane AlcantaraNo ratings yet
- Fluids and Electrolytes Study GuideDocument13 pagesFluids and Electrolytes Study GuideElizabeth McKeeNo ratings yet
- CC2 Laboratory (Finals)Document118 pagesCC2 Laboratory (Finals)Faith Ann CortezNo ratings yet
- Peritoneal Fluid Analysis: Basic InformationDocument1 pagePeritoneal Fluid Analysis: Basic InformationNoviano Benny RepiNo ratings yet
- EffusionsDocument26 pagesEffusionsfomishisilasNo ratings yet
- Unit Iv Body Fluid AnalysisDocument8 pagesUnit Iv Body Fluid AnalysispriyagerardNo ratings yet
- Glomerulonephritis and The Acute Nephritic Syndrome: Chapter ObjectivesDocument10 pagesGlomerulonephritis and The Acute Nephritic Syndrome: Chapter ObjectivesMiguel AngelNo ratings yet
- Serous Physiology Pleural FluidDocument3 pagesSerous Physiology Pleural FluidGhina Ü MaderaNo ratings yet
- Lesson On Analysis and Body FluidsDocument24 pagesLesson On Analysis and Body FluidsJustin Lawrence VillasNo ratings yet
- Terms/ Choices/questions Given by Other Students With The Same RecallDocument27 pagesTerms/ Choices/questions Given by Other Students With The Same RecallchippaiqweqweNo ratings yet
- Laboratory: Reference: Labtest PDFDocument6 pagesLaboratory: Reference: Labtest PDFChris Denver BancaleNo ratings yet
- Aubf Lab CSFDocument6 pagesAubf Lab CSFAndrei Tumarong AngoluanNo ratings yet
- Seri 1Document30 pagesSeri 1Taufik RamadhanNo ratings yet
- I.V. Fluid Therapy IDocument4 pagesI.V. Fluid Therapy IPrabath ChinthakaNo ratings yet
- Specimen Considerations CCDocument21 pagesSpecimen Considerations CCZeian Jacob BaylaNo ratings yet
- Online Practice Tests, Live Classes, Tutoring, Study Guides Q&A, Premium Content and MoreDocument25 pagesOnline Practice Tests, Live Classes, Tutoring, Study Guides Q&A, Premium Content and MoreabctutorNo ratings yet
- Online Practice Tests, Live Classes, Tutoring, Study Guides Q&A, Premium Content and MoreDocument25 pagesOnline Practice Tests, Live Classes, Tutoring, Study Guides Q&A, Premium Content and MoreYoAmoNYCNo ratings yet
- Online Practice Tests, Live Classes, Tutoring, Study Guides Q&A, Premium Content and MoreDocument25 pagesOnline Practice Tests, Live Classes, Tutoring, Study Guides Q&A, Premium Content and MoreJSlinkNYNo ratings yet
- Metabolic Disorders and Critically Ill Patients: From Pathophysiology to TreatmentFrom EverandMetabolic Disorders and Critically Ill Patients: From Pathophysiology to TreatmentCarole IchaiNo ratings yet
- JILG Students Learn by Serving Others.: Benton High School JILG ReportDocument4 pagesJILG Students Learn by Serving Others.: Benton High School JILG ReportjilgincNo ratings yet
- Action ResearchDocument6 pagesAction Researchbenita valdezNo ratings yet
- Sfdunj Jkon PH 1F 3DM Mep 000014Document1 pageSfdunj Jkon PH 1F 3DM Mep 000014Syauqy AlfarakaniNo ratings yet
- Immuno DiffusionDocument3 pagesImmuno DiffusionSai SridharNo ratings yet
- CPESC Scope of PracticeDocument3 pagesCPESC Scope of Practicealphapinnacle techNo ratings yet
- DichotomousKeyNYFish PDFDocument13 pagesDichotomousKeyNYFish PDFNermine AbedNo ratings yet
- Verb Pattern in EnglishDocument4 pagesVerb Pattern in EnglishValentina Yanella Caudullo SeoaneNo ratings yet
- Variables, Validity & ReliabilityDocument42 pagesVariables, Validity & ReliabilityNsem Rao100% (1)
- Lamellar TearingDocument6 pagesLamellar TearingAndreaNo ratings yet
- 25 Secrets of Mona Lisa RevealedDocument12 pages25 Secrets of Mona Lisa Revealeddeebee80No ratings yet
- Measuring Strain in RocksDocument2 pagesMeasuring Strain in Rocksdarebusi1No ratings yet
- Modeling & Simulation of Spherical Robot Configuration Using Solidworks & MatlabDocument3 pagesModeling & Simulation of Spherical Robot Configuration Using Solidworks & Matlabkarthi0% (1)
- IB Chemistry - SL Topic 7 Questions 1Document19 pagesIB Chemistry - SL Topic 7 Questions 1vaxor16689No ratings yet
- Laporan Kasus (Stroke NHS)Document4 pagesLaporan Kasus (Stroke NHS)keluargacendanaNo ratings yet
- Aegis - Designer and AnalyzerDocument26 pagesAegis - Designer and Analyzeropenid_S1hHcZODNo ratings yet
- Sensitive PracticeDocument122 pagesSensitive PracticeFederica FarfallaNo ratings yet
- Ethics in Accounting A Decision Making Approach 1St Edition Klein Solutions Manual Full Chapter PDFDocument40 pagesEthics in Accounting A Decision Making Approach 1St Edition Klein Solutions Manual Full Chapter PDFLisaMartinykfz100% (9)
- Model QuestionsDocument27 pagesModel Questionskalyan555No ratings yet
- User's Guide: NAS SeriesDocument290 pagesUser's Guide: NAS SeriesJULIO CESAR BERNAL CASASNo ratings yet
- Species Concepts PDFDocument5 pagesSpecies Concepts PDFMayhaaaNo ratings yet
- CCNA1 Mod 6Document28 pagesCCNA1 Mod 6KlokanNo ratings yet
- (1142) Grade XI Admissions 2016-17Document7 pages(1142) Grade XI Admissions 2016-17Naveen ShankarNo ratings yet
- Analytical ExpositionDocument9 pagesAnalytical Expositionkeira raishaNo ratings yet
- Feasibility Study Project Proposal RequirementsDocument2 pagesFeasibility Study Project Proposal RequirementsErick NgosiaNo ratings yet
- Nakshtra Swami and BhramanDocument12 pagesNakshtra Swami and Bhramansagar_m26100% (1)
- TDS - Masterseal 420 HBDocument2 pagesTDS - Masterseal 420 HBVenkata RaoNo ratings yet
- Aspirations of Peace and Nonviolence-Chandan-Sukumar-SenguptaDocument7 pagesAspirations of Peace and Nonviolence-Chandan-Sukumar-SenguptaSENGUPTA CHANDANNo ratings yet
- PhilosophyDocument4 pagesPhilosophyJudalineNo ratings yet
(PH156) 14 CSF, Transudates, Exudates, and Other Fluids
(PH156) 14 CSF, Transudates, Exudates, and Other Fluids
Uploaded by
Rosshlein Marian Yangson0 ratings0% found this document useful (0 votes)
12 views6 pagesOriginal Title
[PH156] 14 CSF, Transudates, Exudates, and Other Fluids
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
12 views6 pages(PH156) 14 CSF, Transudates, Exudates, and Other Fluids
(PH156) 14 CSF, Transudates, Exudates, and Other Fluids
Uploaded by
Rosshlein Marian YangsonCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 6
PH 156: CLINICAL MICROSCOPY
CSF, TRANSUDATES, EXUDATES, AND OTHER FLUIDS
MAHOREN C. TOBIAS-ALTURA, RMT, DMM, MSc | APRIL 2022
TABLE OF CONTENTS → Effusion is transudate if it is associated with systemic disorders
▪ Result from secondary or remote (i.e, not directly related to
I. Overview of Body Fluids IV. Cerebrospinal Fluid
serous membrane) pathologies
II. Serous Fluids A. Sample Collection,
− May be the result of a mechanical disorder affecting
A. Overview Storage, And
movement of fluid across a membrane (e.g., congestive
B. Pleural Fluid Transportation
heart failure, nephrotic syndrome, and hepatic cirrhosis)
C. Pericardial Fluid B. Gross Examination
− Example: Ascites, an effusion in the peritoneal cavity, can
D. AscItic Fluid C. Cell Count
be caused by liver cirrhosis or congestive heart failure
III. Synovial Fluid D. Biochemistry
▪ Further testing is generally unnecessary
A. Recommended Tests V. References
→ Effusion is exudate if it results from an inflammatory response
B. Interpretation
to conditions that directly affect the serous cavity
I. OVERVIEW OF BODY FLUIDS ▪ Indicates primary involvement of the associated serous
membrane and damage to the membranes
Note: Information for this section was directly taken from Linné & Ringsrud’s
Clinical Laboratory Science (Turgeon, 2016).
▪ Requires immediate attention and further testing to
determine diagnosis and treatment (e.g., Gram stain and
● Body fluids circulating in various body cavities are sterile under culture if infection is suspected; cytologic tests and biopsy for
normal conditions malignancies)
→ Diseases and disorders can cause the quantity of fluids to ▪ Causes:
increase significantly − Localized infection
→ Examples of body fluids: Circulating blood, urine, and body fluids − Malignancy
from various cavities − Trauma or infarction
● Fluids from various sites can be aspirated and tested for various − Immunological disorder (e.g., systemic lupus erythematosus
markers (e.g., total number of RBCs and WBCs, differentiation of [SLE] and rheumatoid disease [RD]
white cell types, chemical composition, and microorganisms) ▪ Chylous exudate
→ Type of examination depends on the source of the specimen − Associated with rupture or blockage of thoracic duct
→ Standard precautions must be practiced
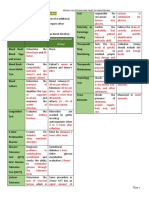
Table 1. Transudates vs. exudates
→ Specimen must be fresh
Findings Transudates Exudates
▪ Cell counts cannot be done on clotted specimen
▪ Thus, anticoagulants are used Appearance Clear, colorless, Cloudy, purulent,
→ Aliquots of various specimens are sent to a particular division of straw-colored hemorrhagic
the clinical laboratory (e.g., hematology, chemistry, microbiology, Specific Gravity <1.015 >1.015
immunology, or cytology) Total Protein <3.0g/dL >3.0g/dL
Fluid Protein: <0.5 >0.5
II. SEROUS FLUIDS Serum Protein Ratio
A. OVERVIEW Pleural fluid lactate < ⅔ upper limit of > ⅔ upper limit of
dehydrogenase (LD) normal serum normal serum LD
Note: Text in blue contains information taken from Linné & Ringsrud’s
Clinical Laboratory Science (Turgeon, 2016).Text in red contains information Pleural fluid/serum <0.6 >0.6
taken from Clinical Chemistry Techniques, Principles, Correlations (Bishop LD ratio
et al., 2010). Pleural fluid <45 mg/dL >45 mg/dL
cholesterol
● Ultrafiltrates of plasma that are continuously formed and reabsorbed
Pleural fluid/serum <0.3 >0.3
● Composition is similar to serum
cholesterol ratio
● Fluids contained within the closed cavities of the body
Note: In other references, (1) fluid/plasma (F/P) ratio for total protein, (2)
→ Include pleural, pericardial, and peritoneal fluids found in the
ratio for LDH, and (3) pleural fluid LDH/upper limit serum LDH ratio
pleural, pericardial, and peritoneal cavities respectively reference interval fall under F/P ratios or Light’s criteria
→ Serous membrane: Lining of body cavities, contiguous
membrane that forms a double layer of mesothelial cell Testing Protocol
● Normal appearance: Pale and yellow-colored ● Aspirated for diagnostic purposes or if they are mechanically
● Exists in small amounts and fills the spaces between two layers inhibiting the function of associated organs
and serve to lubricate the surfaces of these membranes as they → Collected specimen are placed in various containers, depending
move against each other on the test to be performed
→ Normally formed continuously in the body cavities, then ● If the fluid clots, it is useless for many analyses
reabsorbed and leaves only very small volumes Table 2. Appropriate container for serous fluids depending on test
→ Serous fluid formation is also affected by capillary pressure and requirements.
permeability Container Purpose/Test
Effusion, Transudates, and Exudates Ethylenediaminetetraacetic Cell counts and smear evaluation
● Increase in volume of any serous fluid acid (EDTA) tube
● Common causes: Sterile tube Culture
→ Inflammation Oxalate and fluoride tubes Protein, glucose, or other chemistry tests
▪ Fluid also becomes more turbid as the total cell count rises Container with For large volumes of fluid aspirated
→ Decrease in serum protein level [anticoagulant] additive
▪ Normally, serum protein exerts colloidal osmotic pressure and Note: Information in this table is taken from Linné & Ringsrud’s Clinical
helps impair movement of fluid into the serous cavity Laboratory Science (Turgeon, 2016).
▪ If plasma protein level decreases, colloidal osmotic pressure B. PLEURAL FLUID
falls, and effusion results
▪ Movement of transudates into the serous cavity increases Overview
● In determining the cause of the effusion, it is helpful to determine if ● Surrounds the lungs and lines the wall of the thoracic cavity
the effusion is a transudate or exudate → 1-10 mL of pleural fluid moistens pleural surfaces
● Interstitial fluid of the systemic circulation
Trans # 14 Group G: Burigsay, Castillo, Rosuello, Samson 1 of 6
● Fluid exits by drainage into the lymphatics of the visceral pleura and Cytology
the visceral circulation ● Mesothelial cells
● Thoracentesis – removal of pleural fluid from pleural space through → Reactive cells common in pleural fluid which are shed by pleura
the use of needle and syringe after visualization by radiology → Seen in:
Normal Pleural Fluid ▪ Inflammatory,
● Transudate ▪ Rheumatoid, and
● Clear ultrafiltrate of plasma that originates from the parietal pleura ▪ Malignant conditions
Table 3. Normal pleural fluid content
pH 7.60-7.64
Protein <1-2 g/dL
WBC <1000/mm3
Glucose 70-110 mg/dL (similar to plasma)
LDH <50% of plasma level
● Effusion – Build up of serous fluid that may be due to:
→ Increased capillary permeability
→ Increased capillary hydrostatic pressure
→ Decreased plasma oncotic pressure
Figure 1. Mesothelial cells.
→ Decreased lymphatic resorption
● Lupus erythematosus (LE) cells
Recommended Tests
→ May be seen in some cases of effusion from SLE
Table 4. Recommended tests for pleural fluid.
Routine Tests Additional Tests
● Gross examination ● Enzymes
● Chemical examination → Amylase
→ Protein → Lactate dehydrogenase (LDH)
→ Glucose ● Lipids
→ Pleural fluid/serum protein ratio → Chylous effusions
→ Pleural fluid/serum lactate ● Tumor markers
dehydrogenase (LD) ratio → CEA (found in metastatic lung
→ Cholesterol level or breast carcinoma)
● Cell count ● Immunological
→ Total and differential count → Rheumatoid arthritis (RA) factor Figure 2. Lupus erythematosus cells.
● Cytology → Antinuclear antibody
● Culture and gram stain (ANA) factor C. PERICARDIAL FLUID
→ Complement levels ● Normally, 10-50 mL of fluid is present in the pericardial space
around the heart
Interpreting Pleural Fluid ● The process of fluid formation is same as described earlier
Table 5. Interpretation of pleural fluid. ● Abnormal accumulation of pericardial fluid fills up space around the
● Transudate heart and can mechanically inhibit its normal function (cardiac
→ Pale tamponade)
→ Clear straw-colored fluid → Immediate aspiration of excess fluid is indicated
● Exudate
Color → Turbid Recommended Tests
→ Cloudy Table 6. Recommended tests for pericardial fluid.
→ Presence of clot Routine Tests Additional Tests
● Malignancy/trauma/pulmonary infarct ● Gross examination ● Enzymes
→ Bloody color ● Chemical examination → Adenosine Deaminase (ADA)
● Protein measurement is not useful → Protein for tubercular pericarditis
● Decreased glucose levels in rheumatoid pleuritis, → Glucose ● Lipids
malignancy, tuberculosis, and bacterial infections ● Cell count → Chylous effusions
● Increased lactate levels in bacterial infection and → Total and differential → Pseudochylous effusions
Chemical
tubercular pleural infection ● Cytology
Examination
● Increased lactate dehydrogenase levels in pleural ● Culture and gram stain
inflammation
● Low pH and low glucose level in parapneumonic Interpreting Pericardial Fluid
effusion, rheumatoid pleuritis, and malignant effusion Table 7. Interpretation of pericardial fluid
● Total WBC count > 1000/μL ● Large volume (> 350 mL) in malignancy or uremia
→ Suggests exudate ● Turbid fluid suggests infection or malignancy
→ Infective etiology ● Blood-like fluid
● Differential with Neutrophils > 50% Gross
→ Hemorrhagic effusion
→ Bacterial pneumonia Appearance
→ Blood from heart chamber
→ Pulmonary infarction ▪ Check the hematocrit
→ Early tuberculosis ▪ It will be same as that of venous blood with clot
● Differential with Lymphocytes> 50% ● Protein measurement is not useful
→ Tubercular ● Glucose level < 40 mg/dL in bacterial, tubercular,
→ Viral Chemical
rheumatic, and malignant effusions
Cell Count → Malignancy Examination
● Increased adenosine deaminase activity (ADA) in
→ Rheumatoid pleuritis tuberculous pericarditis
→ SLE ● Gram-positive in 50% of bacterial pericarditis
● Differential with Eosinophils> 10% Microbiological ● Culture may be positive in up to 80% of cases
→ Pulmonary infarct Examination ● Acid fast stain may be positive in up to 50% of
→ Trauma tuberculous pericarditis
→ Rheumatological disease ● Total WBC count > 10,000/ μL
● RBC count >100,000/μL Cell Count → Bacterial pericarditis
→ Malignancy → Tuberculous or malignant pericarditis
→ Trauma ● PAP or Giemsa stains
→ Pulmonary infarct Cytology → May show presence of malignant cells, commonly
metastatic cells from breast or lung malignancy
PH 156 CSF, Transudates, Exudates, and Other Fluids 2 of 6
C. ASCITIC FLUID → Decreased glucose levels
▪ [Late] spontaneous bacterial peritonitis
● Ultrafiltrate of plasma across capillary walls − As low as 0 mg/dL
● Normal peritoneal fluid is <50 mL of transudative fluid in the − Secondary to bacterial consumption
mesothelial-lined peritoneal cavity ▪ 30-60% of cases of tubercular peritonitis
● Ascites ● Alkaline phosphatase (ALP) > 10 U/L
→ Excessive accumulation of free fluid in peritoneal cavity → Predicts hollow visceral injury
● Ascitic Fluid → Helps differentiate primary and secondary bacterial
→ Fluid received in the laboratory peritonitis
→ Classification into transudates and exudates is not well defined ● Lactate dehydrogenase (LD)
→ Paracentesis – process of obtaining samples of this fluid by → Increase in LD activity in malignant effusion
needle aspiration → Ascitic fluid/serum LD ratio > 0.6
▪ Fluid is visualized by ultrasound to confirm its presence and ● Adenosine deaminase (ADA)
volume before para- centesis is attempted → To identify patients with tuberculosis in endemic
areas using a cut-off of 30 [international] U/L
Table 8. Common cause for Ascites ● Tumor markers (e.g., CEA, CA-125, CA 19-9)
Transudative Exudative → To differentiate intra-abdominal tumors
● Congestive cardiac failure ● Infections ● Obtained by inoculating blood culture bottles at the
● Cirrhosis ● Malignancies bedside
● Nephrotic syndrome ● Trauma Cultures and → Improves sensitivity to at least 80%, compared to
● [Pancreatitis-associated Gram Stains 50% for conventional culture methods
changes in] ammonia levels ● Gram stains are rarely positive as concentration of
organisms is not high enough
Recommended Tests
● Only partially helpful to diagnose malignant ascites
● Sample: Ideally, 50-100 mL of fluid should be sent for examination → Most intra-abdominal cancers do not frequently
Table 9. Recommended tests for pleural fluid. metastasize to the peritoneum
→ 100% sensitivity found only in the diagnosis of
Routine Tests Additional Tests Cytology
peritoneal carcinomatosis
● Gross examination ● Enzymes ● Liquid based cytology and thin layer preparation are
● Chemical examination → Alkaline phosphatase superior to standard cytological preparation
→ Protein ▪ to check for ● Note: Negative cytology does not rule out cancers
→ Glucose intestinal injuries
→ Serum ascites albumin → Lactate dehydrogenase Serum-Ascites Albumin Gradient (SAAG)
concentration gradient ▪ for patients with suspected ● Superior to total protein concentration to differentiate cirrhosis as a
● Cell count malignant effusion cause
→ Total and differential count ● Creatinine and urea ● Formula: 𝑆𝐴𝐴𝐺 = 𝑆𝑒𝑟𝑢𝑚 𝑎𝑙𝑏𝑢𝑚𝑖𝑛 – 𝐴𝑠𝑐𝑖𝑡𝑖𝑐 𝑓𝑙𝑢𝑖𝑑 𝑎𝑙𝑏𝑢𝑚𝑖𝑛
● Cytology → To differentiate peritoneal fluid
● Culture and gram stain from urine Table 11. Interpretation of SAAG
● Ammonia levels Low SAAG (<1.1 g/dL) High SAAG (≥1.1 g/dL)
→ For suspected cases of ● Ascites not due to ● Ascites due to
perforated peptic ulcer, portal hypertension portal hypertension
ruptured appendix, or → Infection → Liver cirrhosis
intestinal strangulation → Malignancy → Congestive heart failure
Interpreting Pericardial Fluid II. SYNOVIAL FLUID
Table 10. Interpretation of ascitic fluid ● Fluid in joints
● Transudate ● Imperfect ultrafiltrate of plasma, combined with hyaluronic acid
→ Pale yellow produced by synovial cells
→ Clear → The presence of hyaluronate differentiates synovial fluid from
● Exudate other serous fluids and spinal fluid
→ Cloudy or turbid → Hyaluronic acid is responsible for the normal viscosity of
▪ Due to presence of leukocytes or tumor cells synovial fluid which lubricate the joints so that they move freely
Gross
● Green yellow color
Examination ▪ Normal viscosity is responsible for some difficulties in the
→ Due to perforation of GI tract or biliary tract
examination of synovial fluid, especially in performing cell
● Blood-tinged or grossly bloody fluid
→ Traumatic tap
counts
→ Malignancy ● Examined for undiagnosed effusions to differentiate between.
→ Tuberculosis → Inflammatory (e.g., OA, rheumatoid arthritis, or gout), and
→ Intra-abdominal organ rupture → Infectious disorders
● No standardized ascitic fluid cell count ▪ Septic arthritis
● Generally accepted ‘cut off’ limits of normal: < 250 ▪ Crystalline arthropathies (e.g., gout)
[leukocytes] PMNs/mm3 ● Arthrocentesis: Liquid biopsy of the joint
Cell Count → If >500 cells/mm3 with 70% PMNs, highly suggestive ● Ideally, the specimen is divided into three parts depending on the
of spontaneous bacterial peritonitis quantity of effusion fluid and the clinical requirement sample
→ In tuberculous ascites, there is a lymphocytic → EDTA tube (Purple top)
predominance ▪ For total and differential counts
● Serum-Ascites Albumin Gradient (SAAG) → Blood culture bottle
→ superior to total protein concentration to differentiate ▪ For aerobic and anaerobic cultures
cirrhosis as a cause → Heparinized tube (Green top)
● Amylase ▪ For biochemistry and cytology
→ Normally, it is similar to the serum amylase ▪ Cytology samples can be stored up to 12 hours under
→ Increase of >3 times seen in acute pancreatitis or refrigeration
pancreatic pseudocyst
Chemical → If malignancy, fungal, or mycobacterial infection is suspected,
→ Other causes of high amylase levels
Examination maximum amount of fluid should be submitted to maximize yield
▪ Gastroduodenal perforation
▪ Acute mesenteric vein thrombosis Normal Synovial Fluid
▪ Intestinal necrosis Table 12. Normal synovial fluid content
● Glucose
→ Has little value ● Straw-colored
Gross
→ In uncomplicated ascites, it is usually similar to ● Clear
Appearance
serum levels ● Moderately viscous
PH 156 CSF, Transudates, Exudates, and Other Fluids 3 of 6
Protein ● 1–3 g/dL (~1/3 plasma level) ● Always performed for synovial fluid because of high sensitivity,
Glucose ● 70-110 mg/dL (similar to plasma level) especially for non-gonococcal joint infections
Uric acid ● 2-8 mg/dL (similar to plasma level) ● Ziehl-Nielsen (ZN) stain has low sensitivity for acid fast bacilli in
Hyaluronate ● 0.3-0.4 g/dL synovial fluid
Cellular ● 0-150 cells/mm3 ● Synovial biopsy is recommended for suspected tuberculous
content ● Includes WBCs, occasional RBCs. and some arthritis
synovial lining cells ● Fungal and mycobacterial cultures are performed only in clinically
suspicious cases
A. RECOMMENDED TESTS ● There is a lot of overlap between various joint disease groups.
Table 13. Recommended tests for synovial fluid. Except for specific result of gram stain, culture, and crystal, other
Routine Tests Additional Tests findings need to be interpreted in context with clinical picture
● Gross examination ● Fungal and acid-fast stains Table 14. Synovial fluid findings as per disease category
→ For color and clarity ● Lactate levels Group I
Findings Normal Group II Group III Group IV
● Cell count ● Lipid levels Non-
Inflammatory Infectious Hemorrhagic
inflammatory
→ Total and differential count ● Serum synovial fluid
● Bacterial culture and gram stain glucose differential Red brown
Yellow
● Chemical examination Clear to Yellow Yellow or
Appearance cloudy
→ For glucose and protein levels straw color transparent purulent xanthochro
turbid
● Crystal examination mic
WBC Count 1-150 < 3,000 3,000 - 50,000 - 50 - 10,000
B. INTERPRETATION 75,000 200,000
Gross Appearance Neutrophil <25% <30% >50% >90% <50%
● Colorless to pale yellow %
→ Normal synovial fluid Presence of Absent Absent Absent Present Present
RBC
● Straw to yellow color
Synovial 0-10 0-10 0-40 20-100 0-20
→ Non-inflammatory and inflammatory conditions
plasma
● Yellow, brown, or greenish color
glucose
→ Septic or infective arthritis difference
● Reddish color (mg/dL)
→ Traumatic tap, traumatic effusion (hemarthrosis), or malignancy
III. CEREBROSPINAL FLUID
Clarity
● Clear/Transparent ● Liquid that surrounds the brain and spinal cord
→ Normal synovial fluid ● Functions as a buoyant cushion for the brain
● Turbid/Cloudy → Denser brain floats in the less dense liquid, allowing movement
→ Inflammatory, infective, or hemorrhagic conditions within the skull
● Chylous fluid appears milky after centrifugation → Acts as a shock absorber for the brain and the spinal cord
▪ With a blow to the head, the initial shock is transferred to the
Viscosity (due to hyaluronate)
entire brain, instead of inflicting damage to one area.
● String test is done to evaluate the level of synovial fluid viscosity ● Maintains constant gross chemical matrix for the CNS
→ After removing the needle or cap from the syringe, synovial fluid ● Transport function
is expressed into a test tube one drop at a time → Involved in the distribution of hypophyseal hormones within the
→ Normal synovial fluid forms “string” ~5 cm long before breaking brain and the clearance of hormones from the brain to the blood
▪ Fluid may cling to the side of the test tube rather than running
down to the bottom Normal CSF
→ Poor viscosity in fluid forms shorter strings Table 15. Reference ranges for normal CSF.
▪ Seen in inflammatory conditions Gross Opening Specific
Glucose Total protein
Biochemical Tests appearance pressure gravity
● Glucose (Synovial fluid glucose-serum glucose level difference) Clear and 50-175
1.006-1.009 40-80 mg/dL 15-45 mg/dL
→ Normal: < 10 mg/dL colorless mm H2O
→ Septic arthritis: 20-60 mg/dL difference ● Leukocytes
● Protein → 0-5 per μL in adults and children
→ Normal: 1/38 g/dL → Up to 30 per μL in newborns
→ Increased levels in inflammatory disorders ● Differential counts
● Lactate dehydrogenase (LDH) → 60-80% lymphocytes
→ Elevated in rheumatoid arthritis, infectious arthritis, and gout → Up to 30% monocytes and macrophages
● Lactate ▪ Somewhat higher in neonates
→ Up to 10x increase is associated to septic arthritis → 2% or less other cells
Cell Count Table 16. Reference ranges for normal CSF (continuation).
● Total cell count Syphilis
→ Upper limit for total WBC: 150-200 cells/μL Gram stain Culture RBC Count
serology
● Normal differential count No RBC unless
→ 20% neutrophils Negative Sterile Negative needle passes through blood
▪ Differential with 75% neutrophils is seen in inflammatory vessels en route to CSF
rheumatoid arthritis and gout
→ 15% lymphocytes A. SAMPLE COLLECTION, STORAGE, AND TRANSPORTATION
▪ Differential with increased lymphocytes is seen in early ● CSF examination is done for the diagnosis of CNS abnormalities
rheumatoid arthritis, chronic infections, and collagen disorders ● Samples are obtained by lumbar, cisternal, or lateral cervical
→ 65% monocytes and macrophages puncture or ventricular cannulas or shunts
→ Typically, 3-4 tubes are drawn
Crystal Examination
▪ Tube 1 – Biochemistry
● Synovial fluid is evaluated under polarized light to recognize the
− Should never be used for microbiology due to contamination
presence of crystals and distinguish the types of crystals present
with skin bacteria
→ Gout: Needle-like monosodium urate crystals
▪ Tube 2 – Microbiology
→ Pseudogout: Calcium pyrophosphate crystals
▪ Tube 3 – Cell Counts
Gram Stain and Culture − Used for maximum tests in the case of a traumatic tap
▪ Tube 4 – Cytology
PH 156 CSF, Transudates, Exudates, and Other Fluids 4 of 6
→ Recommendation: 12 mL of CSF partitions into 3-4 sterile tubes Figure 4. Gross examination of CSF for clots. (Left) Webbed fibrin clot in
▪ CSF should not be allowed to sediment before partitioning TB. (Right) Traumatic fibrin clot. Retrieved from LabsforLifeProject (2018).
Sample Stability Bleeding
● CSF should be analyzed immediately (<1 hour after collection) ● In grossly bloody CSF, it is possible to distinguish if it is due to
● Stability of the CSF sample varies depending on the procedures subarachnoid hemorrhage or traumatic tap
→ Hematologic Analysis
▪ Performed within 1 hour of aspiration
▪ RBCs and WBCs have limited stability in the fluid because
CSF is hypotonic, and cells can rapidly lyse
▪ Timing is critical for WBCs
− Number and type of cells present are clinically important in
o Diagnosing cases of meningitis
o Detecting CNS leukemic involvement
▪ Samples should be maintained at room temp prior to testing
→ Cultures
Figure 5. Gross examination of CSF for bleeding. (Left) Due to
▪ Refrigeration is not recommended
subarachnoid hemorrhage. (Right) Due to traumatic tap.
− Some organisms (e.g., Haemophilus influenzae and Retrieved from LabsforLifeProject (2018).
Neisseria meningitidis) may not survive
● Storage: 3-4 mL at 4ºC C. CELL COUNT
→ General investigations Equipment Required
→ Investigation of bacteria and fungi ● Neubauer chamber
→ Antibody testing ● Microscopic slides
→ Polymerase chain reaction (PCR) ● Leishman’s stain
→ Antigen detection ● Centrifuge
● Large volumes (10-15 mL) are necessary for certain pathogens
(e.g., Mycobacterium tuberculosis, suspected fungi or parasites) Total Count
● Procedure:
B. GROSS EXAMINATION → Mix the specimen thoroughly by gentle inversion, at least 10x
Color → Using a pipette, transfer the undiluted fluid to the hemocytometer
counting chamber
▪ Fill both sides of the counting chamber using proper technique
▪ If a diluent is required, isotonic saline may be used since it
preserves both WBCs and RBCs
− Dilution 1:1 is usually adequate to acquire a cell count
− If the counts are extremely high, dilution with Turk’s fluid
may be done
→ Allow the cells to settle
→ Focus under low power (10x) and adjust condenser and
Figure 3. Gross examination of CSF for color. [L] Bloody sample. diaphragm for maximum visualization
[R] Yellow color. Retrieved from LabsforLifeProject (2018). → Switch to high power (40x) and adjust as necessary
● Hold the sample against a white paper and compare it to a tube of → For an undiluted sample, all 9 squares are counted
distilled water ▪ The necessity to dilute the sample and the number of squares
● If it has any color at all, it is abnormal counted depends on the cellularity of the specimen
→ Reddish or bloody: Presence of blood due to pathology or ▪ Adjustments in the procedure should be made accordingly
trauma during the procedure ▪ Both WBCs and RBCs should be counted; however, these are
→ Yellow: Xanthochromia due to previous hemorrhage or hemolysis counted separately
→ Average the results from both sides of the chamber
Clarity
● To check if the RBCs are crenated or not,
● Clear: Normal CSF → Crenated: Subarachnoid hemorrhage
● Turbidity: Increase in the number of cells → Normal: Traumatic tap
● Possible to distinguish between neutrophils and lymphocytes
and determine the percentage of each type
● Calculation:
𝑁 × 𝐷𝑖𝑙𝑢𝑡𝑖𝑜𝑛 𝑁 × 1 × 10
𝐶𝑒𝑙𝑙𝑠/μ𝐿 = 𝐷𝑒𝑝𝑡ℎ 𝑓𝑎𝑐𝑡𝑜𝑟 × 𝐴𝑟𝑒𝑎 𝑐𝑜𝑢𝑛𝑡𝑒𝑑
= 9
Where:
▪ N: number of cells
▪ Dilution: 1
▪ Depth faction: 1/10
▪ Area counted: 9
Figure 4. Gross examination of CSF for turbidity. Differential WBC Count
Retrieved from LabsforLifeProject (2018).
● Procedure:
Coagulation → Spin the sample at 1500 rpm for 1 minute
● Fibrin clots can be found if the protein content is very high → Discard the supernatant
● Clots can also possible under a traumatic tap condition → Resuspend the elements in the available fluid
→ Make a smear from the sediment
→ Add any Romanowsky stain (e.g., Leishman’s stain)
→ Allow to stand for 1 minute
→ Dilute with buffer of pH 6.8
→ Allow to stand for 3 minutes
→ When dry, view the slide under microscope and do the differential
count of WBCs
● Quality assurance mechanism of interobserver variance (i.e.,
testing by at least 2 different people and analyzing report) is done on
a periodic basis
PH 156 CSF, Transudates, Exudates, and Other Fluids 5 of 6
Interferences → Normal CSF Glucose: 40-80 mg/dL
● Improper mixing before charging → Note: Units are in mg/dL than g/dL as it is in serum protein
● Improper centrifugation determination
● Air bubbles III. REFERENCES
● Sitting time beyond 20 minutes, leading to the disintegration of cells ● LabsforLifeProject (2018). Fluid Examination Specific [YouTube
● Stain debris Video].
D. BIOCHEMISTRY ● LabsforLifeProject (2018). Cerebrospinal Fluid Examination (CSF)
[YouTube Video].
CSF Protein and Glucose ● Turgeon, M.L. (2016). Linné & Ringsrud’s Clinical Laboratory
● Measured in the same way as done in serum samples Science. Elsevier Mosby.
● Look for special instructions provided by manufacturer regarding ● Bishop, M.L., Fody, E.P., & Schoeff, L.E. (2010). Clinical Chemistry
programming or calibrators Techniques, Principles, Correlations. Wolters Kluwer Lippincott
● Interpretation: Williams & Wilkins.
→ Normal CSF Protein: 14-45 mg/dL
▪ Derived from the plasma
PH 156 CSF, Transudates, Exudates, and Other Fluids 6 of 6
You might also like
- Stuxnet and Its Hidden Lessons On The Ethics of CyberweaponsDocument9 pagesStuxnet and Its Hidden Lessons On The Ethics of CyberweaponsprofcameloNo ratings yet
- Aubf Lec - Serous FluidDocument12 pagesAubf Lec - Serous FluidColene MoresNo ratings yet
- B.F Lecture 8 Serous F.analysisDocument23 pagesB.F Lecture 8 Serous F.analysisSalah AbassNo ratings yet
- 2023.LabDx - Trans05.Serous Effusion & Synovial FluidDocument4 pages2023.LabDx - Trans05.Serous Effusion & Synovial FluidstellaNo ratings yet
- Serous FluidDocument1 pageSerous FluidJl OiraNo ratings yet
- AUBF Serous FluidDocument7 pagesAUBF Serous FluidRichelyn Grace B. VenusNo ratings yet
- 5766 Serous FluidsDocument21 pages5766 Serous FluidsAdeniyi AkisekuNo ratings yet
- Pa Tho Physiology of Cavitary EffusionDocument11 pagesPa Tho Physiology of Cavitary EffusionybaeumliNo ratings yet
- Sysmex Educational Enhancement and Development SEED Body FluidsDocument6 pagesSysmex Educational Enhancement and Development SEED Body FluidsbalkisNo ratings yet
- Unit 3 - Transudates and Exudates IIIDocument17 pagesUnit 3 - Transudates and Exudates IIIRubina KhatunNo ratings yet
- SerousDocument8 pagesSerouspekibelssNo ratings yet
- Nursing Foundation 2 Module 6Document6 pagesNursing Foundation 2 Module 6johnbryanmalonesNo ratings yet
- Clase 8 - Examen de Efusiones Torácicas y Abdominales: MVZ Renato Zúñiga FDocument69 pagesClase 8 - Examen de Efusiones Torácicas y Abdominales: MVZ Renato Zúñiga FLisette Velásquez AnticonaNo ratings yet
- Pmls 2 Prelim To FinalsDocument25 pagesPmls 2 Prelim To FinalsisyandanNo ratings yet
- Clinical Microscopy:: Case Study AnalysisDocument12 pagesClinical Microscopy:: Case Study Analysischocoholic potchiNo ratings yet
- Hematology PreliminariesDocument7 pagesHematology PreliminariesRomie SolacitoNo ratings yet
- Cytology of Body FluidDocument28 pagesCytology of Body FluidMalliga SundareshanNo ratings yet
- Serous Fluid Powerpoint HandoutDocument3 pagesSerous Fluid Powerpoint HandoutAnonymous ceYk4p4No ratings yet
- SEROUS-FLUID NotesDocument5 pagesSEROUS-FLUID NotesSpongebob SquarepantsNo ratings yet
- LESSON 8 Special Collection and Point-Of-Care TestingDocument2 pagesLESSON 8 Special Collection and Point-Of-Care TestingAlthea EspirituNo ratings yet
- AUBF Lec M Microscopic Examination of Urine Sediment Part 1Document11 pagesAUBF Lec M Microscopic Examination of Urine Sediment Part 1Haniah DsNo ratings yet
- Fluid and Electrolyte ReplacementDocument60 pagesFluid and Electrolyte ReplacementAlex WagnerNo ratings yet
- Lesson 10Document6 pagesLesson 10GelaaaNo ratings yet
- MLS305 Hema Lab PrelimsDocument11 pagesMLS305 Hema Lab PrelimsEvanka BaguistanNo ratings yet
- Serous Fluid Hand OutDocument3 pagesSerous Fluid Hand OutAhmed AboamerNo ratings yet
- 7 - Fluid Balance - AntinDocument55 pages7 - Fluid Balance - AntinHelen PratiwiNo ratings yet
- Aubf Lec Week 15Document7 pagesAubf Lec Week 15Joanne RemolloNo ratings yet
- Specimen ConsiderationsDocument17 pagesSpecimen ConsiderationsRace MendezNo ratings yet
- Serous Fluid: Presented By: Pauline BautistaDocument13 pagesSerous Fluid: Presented By: Pauline BautistaPauline BautistaNo ratings yet
- Blood Physiology LectureDocument174 pagesBlood Physiology Lectureemmanuelakinola2006No ratings yet
- Body FluidsDocument24 pagesBody FluidsMohamed MidoNo ratings yet
- PMLS 2 Unit 8Document4 pagesPMLS 2 Unit 8Elyon Jirehel AlvarezNo ratings yet
- Sampling: Assistant Instructor. Jinan Hameed Source By:-Practical Clinical BiochemistryDocument24 pagesSampling: Assistant Instructor. Jinan Hameed Source By:-Practical Clinical BiochemistryaddwrNo ratings yet
- Serous Fluid: FormationDocument4 pagesSerous Fluid: FormationemmanuelNo ratings yet
- Exudative Pleural Effusion: Approach To Management: Medicine UpdateDocument10 pagesExudative Pleural Effusion: Approach To Management: Medicine UpdateMukti MuliantoNo ratings yet
- Intravenous Fluids PDFDocument10 pagesIntravenous Fluids PDFGReadRNo ratings yet
- Review of Laboratory and Diagnostic TestsDocument25 pagesReview of Laboratory and Diagnostic TestsCrystal CireraNo ratings yet
- Body Fluids Analysis LectureDocument17 pagesBody Fluids Analysis LectureAsd Asd100% (1)
- Blood TransfusionDocument4 pagesBlood TransfusionYalc LapidNo ratings yet
- Maternal 2 - Blood TransfusionDocument5 pagesMaternal 2 - Blood TransfusionJuliana Anne RamosNo ratings yet
- Specimen Collection HandoutDocument7 pagesSpecimen Collection HandoutCelne CentinoNo ratings yet
- Body Fluids Tsilioni SlidesDocument31 pagesBody Fluids Tsilioni SlidesShaira Jane AlcantaraNo ratings yet
- Fluids and Electrolytes Study GuideDocument13 pagesFluids and Electrolytes Study GuideElizabeth McKeeNo ratings yet
- CC2 Laboratory (Finals)Document118 pagesCC2 Laboratory (Finals)Faith Ann CortezNo ratings yet
- Peritoneal Fluid Analysis: Basic InformationDocument1 pagePeritoneal Fluid Analysis: Basic InformationNoviano Benny RepiNo ratings yet
- EffusionsDocument26 pagesEffusionsfomishisilasNo ratings yet
- Unit Iv Body Fluid AnalysisDocument8 pagesUnit Iv Body Fluid AnalysispriyagerardNo ratings yet
- Glomerulonephritis and The Acute Nephritic Syndrome: Chapter ObjectivesDocument10 pagesGlomerulonephritis and The Acute Nephritic Syndrome: Chapter ObjectivesMiguel AngelNo ratings yet
- Serous Physiology Pleural FluidDocument3 pagesSerous Physiology Pleural FluidGhina Ü MaderaNo ratings yet
- Lesson On Analysis and Body FluidsDocument24 pagesLesson On Analysis and Body FluidsJustin Lawrence VillasNo ratings yet
- Terms/ Choices/questions Given by Other Students With The Same RecallDocument27 pagesTerms/ Choices/questions Given by Other Students With The Same RecallchippaiqweqweNo ratings yet
- Laboratory: Reference: Labtest PDFDocument6 pagesLaboratory: Reference: Labtest PDFChris Denver BancaleNo ratings yet
- Aubf Lab CSFDocument6 pagesAubf Lab CSFAndrei Tumarong AngoluanNo ratings yet
- Seri 1Document30 pagesSeri 1Taufik RamadhanNo ratings yet
- I.V. Fluid Therapy IDocument4 pagesI.V. Fluid Therapy IPrabath ChinthakaNo ratings yet
- Specimen Considerations CCDocument21 pagesSpecimen Considerations CCZeian Jacob BaylaNo ratings yet
- Online Practice Tests, Live Classes, Tutoring, Study Guides Q&A, Premium Content and MoreDocument25 pagesOnline Practice Tests, Live Classes, Tutoring, Study Guides Q&A, Premium Content and MoreabctutorNo ratings yet
- Online Practice Tests, Live Classes, Tutoring, Study Guides Q&A, Premium Content and MoreDocument25 pagesOnline Practice Tests, Live Classes, Tutoring, Study Guides Q&A, Premium Content and MoreYoAmoNYCNo ratings yet
- Online Practice Tests, Live Classes, Tutoring, Study Guides Q&A, Premium Content and MoreDocument25 pagesOnline Practice Tests, Live Classes, Tutoring, Study Guides Q&A, Premium Content and MoreJSlinkNYNo ratings yet
- Metabolic Disorders and Critically Ill Patients: From Pathophysiology to TreatmentFrom EverandMetabolic Disorders and Critically Ill Patients: From Pathophysiology to TreatmentCarole IchaiNo ratings yet
- JILG Students Learn by Serving Others.: Benton High School JILG ReportDocument4 pagesJILG Students Learn by Serving Others.: Benton High School JILG ReportjilgincNo ratings yet
- Action ResearchDocument6 pagesAction Researchbenita valdezNo ratings yet
- Sfdunj Jkon PH 1F 3DM Mep 000014Document1 pageSfdunj Jkon PH 1F 3DM Mep 000014Syauqy AlfarakaniNo ratings yet
- Immuno DiffusionDocument3 pagesImmuno DiffusionSai SridharNo ratings yet
- CPESC Scope of PracticeDocument3 pagesCPESC Scope of Practicealphapinnacle techNo ratings yet
- DichotomousKeyNYFish PDFDocument13 pagesDichotomousKeyNYFish PDFNermine AbedNo ratings yet
- Verb Pattern in EnglishDocument4 pagesVerb Pattern in EnglishValentina Yanella Caudullo SeoaneNo ratings yet
- Variables, Validity & ReliabilityDocument42 pagesVariables, Validity & ReliabilityNsem Rao100% (1)
- Lamellar TearingDocument6 pagesLamellar TearingAndreaNo ratings yet
- 25 Secrets of Mona Lisa RevealedDocument12 pages25 Secrets of Mona Lisa Revealeddeebee80No ratings yet
- Measuring Strain in RocksDocument2 pagesMeasuring Strain in Rocksdarebusi1No ratings yet
- Modeling & Simulation of Spherical Robot Configuration Using Solidworks & MatlabDocument3 pagesModeling & Simulation of Spherical Robot Configuration Using Solidworks & Matlabkarthi0% (1)
- IB Chemistry - SL Topic 7 Questions 1Document19 pagesIB Chemistry - SL Topic 7 Questions 1vaxor16689No ratings yet
- Laporan Kasus (Stroke NHS)Document4 pagesLaporan Kasus (Stroke NHS)keluargacendanaNo ratings yet
- Aegis - Designer and AnalyzerDocument26 pagesAegis - Designer and Analyzeropenid_S1hHcZODNo ratings yet
- Sensitive PracticeDocument122 pagesSensitive PracticeFederica FarfallaNo ratings yet
- Ethics in Accounting A Decision Making Approach 1St Edition Klein Solutions Manual Full Chapter PDFDocument40 pagesEthics in Accounting A Decision Making Approach 1St Edition Klein Solutions Manual Full Chapter PDFLisaMartinykfz100% (9)
- Model QuestionsDocument27 pagesModel Questionskalyan555No ratings yet
- User's Guide: NAS SeriesDocument290 pagesUser's Guide: NAS SeriesJULIO CESAR BERNAL CASASNo ratings yet
- Species Concepts PDFDocument5 pagesSpecies Concepts PDFMayhaaaNo ratings yet
- CCNA1 Mod 6Document28 pagesCCNA1 Mod 6KlokanNo ratings yet
- (1142) Grade XI Admissions 2016-17Document7 pages(1142) Grade XI Admissions 2016-17Naveen ShankarNo ratings yet
- Analytical ExpositionDocument9 pagesAnalytical Expositionkeira raishaNo ratings yet
- Feasibility Study Project Proposal RequirementsDocument2 pagesFeasibility Study Project Proposal RequirementsErick NgosiaNo ratings yet
- Nakshtra Swami and BhramanDocument12 pagesNakshtra Swami and Bhramansagar_m26100% (1)
- TDS - Masterseal 420 HBDocument2 pagesTDS - Masterseal 420 HBVenkata RaoNo ratings yet
- Aspirations of Peace and Nonviolence-Chandan-Sukumar-SenguptaDocument7 pagesAspirations of Peace and Nonviolence-Chandan-Sukumar-SenguptaSENGUPTA CHANDANNo ratings yet
- PhilosophyDocument4 pagesPhilosophyJudalineNo ratings yet