Professional Documents
Culture Documents
Clinical Parasitology-Module 9
Clinical Parasitology-Module 9
Uploaded by
Geresh MagsinoCopyright:
Available Formats
You might also like
- Soap Notes AsthmaDocument6 pagesSoap Notes AsthmaCHRISTINE KARENDINo ratings yet
- OSTEORADIONECROSISDocument38 pagesOSTEORADIONECROSISAbel AbrahamNo ratings yet
- Parasitology Lec 3.01b Blood and Tissue NematodesDocument15 pagesParasitology Lec 3.01b Blood and Tissue NematodesEnaWahahaNo ratings yet
- Lesson 2 Extraintestinal NematodesDocument5 pagesLesson 2 Extraintestinal NematodesCDNo ratings yet
- Wuchereria Bancrofti, Brugia Malayi, Brugia TimoriDocument3 pagesWuchereria Bancrofti, Brugia Malayi, Brugia TimoriJurel GaoatNo ratings yet
- Sheath: Structure of LarvaDocument4 pagesSheath: Structure of Larvaken mendozaNo ratings yet
- Clinical Parasitology-Module 11Document14 pagesClinical Parasitology-Module 11Geresh MagsinoNo ratings yet
- Clinical Parasitology-Module 8Document15 pagesClinical Parasitology-Module 8Geresh MagsinoNo ratings yet
- Blood and Tissue NematodesDocument37 pagesBlood and Tissue NematodesjelenaNo ratings yet
- Filarial Nematodes: Wuchereria BancroftiDocument8 pagesFilarial Nematodes: Wuchereria BancroftiMegumi TadokoroNo ratings yet
- Reviewer For para (Blood and Tissue Nematode)Document4 pagesReviewer For para (Blood and Tissue Nematode)K DNo ratings yet
- 3 - Loa Loa and Onchocerca VolvolusDocument29 pages3 - Loa Loa and Onchocerca VolvolusayaamrsharfNo ratings yet
- Filariae: Wuchereria BancroftiDocument8 pagesFilariae: Wuchereria BancroftiRaiset HermanNo ratings yet
- Midterm ParasitologyDocument18 pagesMidterm ParasitologyAngelic AngelesNo ratings yet
- FilariasisDocument11 pagesFilariasiskartiz008No ratings yet
- Blood Tissue NematodesDocument27 pagesBlood Tissue NematodesAfif Mamen100% (1)
- FilariaDocument85 pagesFilariaRajkishor YadavNo ratings yet
- Clinical Parasitology-Module 3Document12 pagesClinical Parasitology-Module 3Geresh MagsinoNo ratings yet
- Filariasis: Short As 4 Weeks or As Long As 8-16 Months Other Resources 6 Months and As Late As 12 Months After InfectionDocument12 pagesFilariasis: Short As 4 Weeks or As Long As 8-16 Months Other Resources 6 Months and As Late As 12 Months After Infectionchristian quiaoitNo ratings yet
- Merge AbDocument17 pagesMerge AbEricsson CarabbacanNo ratings yet
- Man Bahadur Rana BPH, Acas, NepalDocument34 pagesMan Bahadur Rana BPH, Acas, NepalDipankar NathNo ratings yet
- Filariasis: Short As 4 Weeks or As Long As 8-16 Months Other Resources 6 Months and As Late As 12 Months After InfectionDocument3 pagesFilariasis: Short As 4 Weeks or As Long As 8-16 Months Other Resources 6 Months and As Late As 12 Months After InfectionkyawNo ratings yet
- Arthropods As Vectors of Diseases: Dr. Jennifer O. Pichay AlvaradoDocument4 pagesArthropods As Vectors of Diseases: Dr. Jennifer O. Pichay AlvaradoMon Kristopher F. CastilloNo ratings yet
- Medical Parasitology A Self Instructional Text PDFDriveDocument60 pagesMedical Parasitology A Self Instructional Text PDFDriveDenise Sta. AnaNo ratings yet
- Merged PDF 2021 11 16T12 - 01 - 01Document15 pagesMerged PDF 2021 11 16T12 - 01 - 01Ericsson CarabbacanNo ratings yet
- PARA NematodesDocument23 pagesPARA Nematodes12 Newton - Cayetano, Arafe Nicole A.No ratings yet
- 4.3. Blood and Tissue NematodesDocument89 pages4.3. Blood and Tissue NematodesRediat GossayeNo ratings yet
- Microbiology 19 PDFDocument6 pagesMicrobiology 19 PDFLyka Villagracia AsiloNo ratings yet
- Loa Loa AyaDocument15 pagesLoa Loa AyaayaamrsharfNo ratings yet
- Filarial NematodeDocument18 pagesFilarial NematodeHawre NajmaddinNo ratings yet
- Helemnth ReportDocument15 pagesHelemnth ReportHawre NajmaddinNo ratings yet
- Parasitology Day 9 FilariaeDocument4 pagesParasitology Day 9 Filariaeniczdelosreyes8No ratings yet
- Lesson 5 - PlasmodiumDocument9 pagesLesson 5 - PlasmodiumAnya IgnacioNo ratings yet
- Wu C Here Ria Bancroft IDocument3 pagesWu C Here Ria Bancroft IMariamNo ratings yet
- Filariasis JC - DR Shefali GuptaDocument74 pagesFilariasis JC - DR Shefali GuptaShefali GNo ratings yet
- Filariasis 2015Document56 pagesFilariasis 2015ChandraNo ratings yet
- ROUNDWORMDocument8 pagesROUNDWORMSEAH KAI YEE MoeNo ratings yet
- Mycology TransDocument11 pagesMycology TransKita kitaNo ratings yet
- Lesson 5 Plasmodium SPPDocument8 pagesLesson 5 Plasmodium SPPAnya IgnacioNo ratings yet
- ANCYLOSTOMA DUODENALE Old World HookwormDocument2 pagesANCYLOSTOMA DUODENALE Old World HookwormScarlet AdolfoNo ratings yet
- Vectors PSM ParksDocument36 pagesVectors PSM ParksAshish RajputNo ratings yet
- Additional Notes Only Please Refer To Your Module Definition of TermsDocument4 pagesAdditional Notes Only Please Refer To Your Module Definition of TermsAndrea KamilleNo ratings yet
- Share Modul 1.2.21Document25 pagesShare Modul 1.2.21MECNESIA Tutor 2No ratings yet
- Lecture 7 Nematodes Part 2 New 2023Document19 pagesLecture 7 Nematodes Part 2 New 2023ayaessam392002No ratings yet
- 2.1 MalariaDocument10 pages2.1 MalariaNeil Gabriel EncinaNo ratings yet
- FilariaDocument16 pagesFilariaJessa MayNo ratings yet
- BN Filarial WormDocument137 pagesBN Filarial WormCherenet TomaNo ratings yet
- DNA VIRUSES-handout PDFDocument11 pagesDNA VIRUSES-handout PDFROTHESSA MARY CARINGALNo ratings yet
- Lesson 8 - Nematodes IDocument7 pagesLesson 8 - Nematodes IAnya IgnacioNo ratings yet
- Lymphatic Filariasis ClassDocument68 pagesLymphatic Filariasis ClassthehexhealthNo ratings yet
- Filariasis: Tropmed Block Faculty Medicine USU 2016Document26 pagesFilariasis: Tropmed Block Faculty Medicine USU 2016Tiurma SibaraniNo ratings yet
- Tissue NematodesDocument27 pagesTissue Nematodesbpt2100% (1)
- Parasites and Parasitism (Parasitology)Document3 pagesParasites and Parasitism (Parasitology)Joraine Nichole Roquero VillajuanNo ratings yet
- 7 BIO3243 ElephantiasisDocument11 pages7 BIO3243 ElephantiasisNGOGA NISINGIZWE NESTORNo ratings yet
- Module 9 - Nematodes Part 3Document50 pagesModule 9 - Nematodes Part 3Arnold GarcinesNo ratings yet
- 7 Module 6 Nematodes Part 2Document100 pages7 Module 6 Nematodes Part 2Luke Jovanni TAOCNo ratings yet
- Revision: Types of Life Cycle in Trematoda and CestodaDocument54 pagesRevision: Types of Life Cycle in Trematoda and CestodaMicroscopeGeekNo ratings yet
- Filaria - A Comprehensive StudyDocument63 pagesFilaria - A Comprehensive StudyDayledaniel SorvetoNo ratings yet
- Parasitic Causes of HaematologyDocument65 pagesParasitic Causes of HaematologySolomonNo ratings yet
- 017 Wuchereria BrugiaDocument21 pages017 Wuchereria BrugiaAyop KhNo ratings yet
- Man Bahadur Rana BPH, Acas, NepalDocument34 pagesMan Bahadur Rana BPH, Acas, NepalDipankar NathNo ratings yet
- 5 PyatakDocument21 pages5 PyatakJust HelpingNo ratings yet
- Syllabus Master Tung PDFDocument25 pagesSyllabus Master Tung PDFkamran ahmad100% (1)
- Escala Del Dolor PPPDocument16 pagesEscala Del Dolor PPPMariana SuarezNo ratings yet
- Paediatrics Solved OspeDocument24 pagesPaediatrics Solved OspeSalim KhaleelNo ratings yet
- Chapter 19 AddictionDocument5 pagesChapter 19 AddictionTrixie Myr AndoyNo ratings yet
- Pretend Play Printables I'm A Zoo Keeper - 123 Homeschool 4 MeDocument22 pagesPretend Play Printables I'm A Zoo Keeper - 123 Homeschool 4 Mekantor perencanaan2022No ratings yet
- Pi Is 0828282 X 19315508Document16 pagesPi Is 0828282 X 19315508Mitch TobinNo ratings yet
- A Group Case Study 2nd Sem 1Document46 pagesA Group Case Study 2nd Sem 1Shermaigne Ananayo BuyaNo ratings yet
- Somatoform DisorderDocument30 pagesSomatoform DisorderRujuta BaramateNo ratings yet
- اسئلة طفيليات MCQ مهمة جدا PDFDocument15 pagesاسئلة طفيليات MCQ مهمة جدا PDFفواطم صائب عباس فاضلNo ratings yet
- Mamba Inservice Ic504901aaDocument19 pagesMamba Inservice Ic504901aamayra osorioNo ratings yet
- NP40126 SaeDocument9 pagesNP40126 SaeMohd AljawfiNo ratings yet
- Nur 102Document3 pagesNur 102Fretchel Grace Silverado MesaNo ratings yet
- ADHD in Women Checklist - UpdatedDocument4 pagesADHD in Women Checklist - UpdatedMohamed Gamal HassanNo ratings yet
- ImmunityDocument19 pagesImmunityKailash Nagar100% (1)
- Antibiotic Stewardship in OrthopedicsDocument17 pagesAntibiotic Stewardship in Orthopedicsjomari dvNo ratings yet
- Maam Jean OR SCHED 10112022Document2 pagesMaam Jean OR SCHED 10112022Jean Camille Lazo MendozaNo ratings yet
- ECG Quiz Review and Practice Strip AnswersDocument7 pagesECG Quiz Review and Practice Strip AnswersAANo ratings yet
- Breast Tumours: Introductory NotesDocument8 pagesBreast Tumours: Introductory Notesdiego fernando lobo moncadaNo ratings yet
- RN Targeted Medical Surgical Immune Online Practice 2019Document6 pagesRN Targeted Medical Surgical Immune Online Practice 2019Adriana RemedioNo ratings yet
- Colorectal Cancer Genetic SyndromesDocument1 pageColorectal Cancer Genetic SyndromesRyan GosserNo ratings yet
- 3 - Gastrointestinal Dis - 2020 - Hunter S Tropical Medicine and Emerging InfectDocument11 pages3 - Gastrointestinal Dis - 2020 - Hunter S Tropical Medicine and Emerging InfectThaiz P.SNo ratings yet
- Seizures in Critical Care. A Guide To Diagnosis AnDocument1 pageSeizures in Critical Care. A Guide To Diagnosis AnRENAULTNo ratings yet
- POLYHYDRAMNIOSDocument2 pagesPOLYHYDRAMNIOSyxly imperialNo ratings yet
- Module 9 - Nematodes Part 2Document78 pagesModule 9 - Nematodes Part 2Arnold GarcinesNo ratings yet
- TranslateDocument8 pagesTranslateberliananastasya pNo ratings yet
- Psychiatry: Psychology-Psychiatric Evaluation - 1 (Medical Transcription Sample Report)Document7 pagesPsychiatry: Psychology-Psychiatric Evaluation - 1 (Medical Transcription Sample Report)Nguyên VũNo ratings yet
- Major Depressive Disorder and Difference Between Genders: Dzevad Sabic, Adela Sabic, Amila Bacic-BecirovicDocument4 pagesMajor Depressive Disorder and Difference Between Genders: Dzevad Sabic, Adela Sabic, Amila Bacic-BecirovicDzevad SabicNo ratings yet
Clinical Parasitology-Module 9
Clinical Parasitology-Module 9
Uploaded by
Geresh MagsinoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Clinical Parasitology-Module 9
Clinical Parasitology-Module 9
Uploaded by
Geresh MagsinoCopyright:
Available Formats
Compiled by: EFREN II C.
DEOCADES, RMT
Module
9
Module
9
MTPC 124
CLINICAL
PARASITOLOGY
EFREN II C. DEOCADES, RMT
JMJ Marists Brothers
Notre Dame of Marbel University
NOTRE DAME OF MARBEL UNIVERSITY
College of Arts and Sciences Medical Technology Department
MEDICAL TECHNOLOGY DEPARTMENT
Compiled by: EFREN II C. DEOCADES, RMT
MODULE IX:
The filariae AND MISCELLANEOUS NEMATODES
`
Learning Outcomes
At the end of the session, the students must be able to:
1. thoroughly explain the pathogenesis, epidemiology, prevention and control, treatment,
and diagnosis of clinically-relevant filariae and other miscellaneous nematodes;
2. exemplify mastery of the concept through passing the online assessment.
Introduction
In this module, we will discuss the remaining blood and tissue nematodes. Filarial worms will
be discussed first followed by other nematodes that are of high clinical relevance. These groups of
parasites are important because they can cause debilitating diseases to humans, causing
immobility and unproductiveness especially the group of filariae. The filariae are also characterized
with the presence of biological vectors that are necessary for the development and transmission
of the parasites.
Activity/ Application
The students will be tasked to watch documentaries regarding Nematode cases.
NOTRE DAME OF MARBEL UNIVERSITY
Medical Technology Department
Compiled by: EFREN II C. DEOCADES, RMT
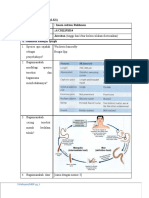
Requires arthropod vector
The Filariae − mosquito, midge, or fly
− Infective larvae injected into humans during
feeding
Filarial Species − Larvae migrate to appropriate tissues and
1. Wuchereria bancrofti – Bancroft’s filaria complete development in adults (process
2. Brugia malayi – Malayan filaria may take up to a year).
3. Loa loa – Eyeworm (African)
− Fertilized adult female worms lay live larvae
4. Onchocerca volvulus – Blinding filaria
(microfilariae).
5. Mansonella ozzardi – New World filaria
− Microfilariae take up residence in blood or
6. Mansonella perstans – Perstans filaria
dermis.
KEY DEFINITIONS − Vector ingests microfilariae during blood
meal.
Filaria (pl. filariae) − Larval development in vector – cycle repeats.
− A group of nematodes (roundworms) in which the
adult worms live in tissue or the lymphatic system LABORATORY DIAGNOSIS
1. Specimen collection time important due to
Elephantiasis parasite periodicity
2. Types of periodicity:
− Enlargement of skin and subcutaneous tissue
1. Nocturnal – occurs at night
2. Diurnal – occurs during the day
Microfilaria (pl. microfilariae)
3. Subperiodic – timing of occurrences not
− The larval stage of the filariae
clear-cut
Periodicity
− The phenomenon whereby parasites present in 1. Wuchereria bancrofti
the bloodstream during a specific time period − Aka Bancroft’s Filarial Worm
− Most prevalent
Sheath − The most common in the Philippines
− Delicate, transparent covering found on select − causes bancroftian filariasis and elephantiasis
microfilariae
Two Forms:
GENERAL CHARACTERISTICS 1. Nocturnal Periodic Form
Adults − found in the peripheral blood during the night
− Creamy white; threadlike appearance between 10 p.m. and 4 a.m.
− Males often half the size of females
2. Second Form
Microfilariae − found only in the Pacific Islands and is
− Slender, vary and overlap in size present in the blood at all times, but more
− Key distinguishing features frequently during the day in the afternoon
1. Distribution of nuclei within tip of tail hours.
2. Presence or absence of sheath
TRE DAME OF MARBEL UNIVERSITY
Medical Technology Department
NOTRE DAME OF MARBEL UNIVERSITY
Medical Technology Department
Compiled by: EFREN II C. DEOCADES, RMT
− ADLA (acute dermatolymphangioadenitis): the
most common acute manifestation of LF, defined
as localized pain, lymphadenitis and/or
lymphangitis and/or cellulitis and local warmth,
with or without systemic manifestations of fever,
nausea, and vomiting.
− Lymphedema most often occurs in the lower
extremities.
− Elephantiasis of lower extremities (especially
the legs)
− Genitals and breasts may also be involved
− Hydrocele: fluid-filled sac within the scrotum, may
occur when adult worms block the retroperitoneal
or subdiaphragmatic lymphatic vessels
Life Cycle Notes − Chyluria: a result of lymphatic rupture and fluid
− Vector: Mosquito (Culex fatigans, Anopheles, or entering the urine
Aedes spp.) − Tropical Pulmonary Eosinophilia (TPE):
− Humans are the definitive host and the elevated serum immunoglobulin E (IgE) level,
reservoir for W. bancrofti. weight loss, low-grade fever, cough and wheezing
− Adult worms reside in lymphatics. at night, and lymphadenopathy; occult filariasis
− Microfilariae live in the blood and lymphatics. − On the death of the adult worm, calcification or
formation of abscesses may occur
Epidemiology − Endosymbiont:
− Subtropical and tropical areas Wolbachia spp.: increases the risk of chronic
− Mosquito breeding occurs in contaminated water infection; obligate intracellular organism; bacterial
in these areas. antigens enhance the host inflammatory
− Indigenous inhabitants are at greater risk of response, leading to increased scarring and
contracting parasite than non-indigenous damage within the host lymphatic system
individuals living in these areas.
Right Leg Elephantiasis
Right Leg Elephantiasis
and Hydrocele
Clinical Symptoms
A. Asymptomatic
− adults who as children were likely exposed
become infected but experience no
symptoms
− Microfilariae and eosinophilia usually
recovered in blood samples
− Physical exam reveals enlarged lymph
nodes, particularly in inguinal region/groin
area
− Typically self-limiting
B. Symptomatic bancroftian filariasis
• General symptoms: Fever, chills,
eosinophilia
• Additional possible symptoms
TRE DAME OF MARBEL UNIVERSITY
Medical Technology Department
NOTRE DAME OF MARBEL UNIVERSITY
Medical Technology Department
Compiled by: EFREN II C. DEOCADES, RMT
Laboratory Diagnosis
Method of choice: fresh Giemsa-stained blood, fluid,
or tissue smear
Other techniques:
1. Filter heparinized blood using nucleopore filter;
examine filter contents
2. Knott technique
3. Serologic tests and PCR have been developed.
Patient symptoms and history often serve as primary
means of diagnosis in endemic areas.
Treatment
1. Diethylcarbamazine (DEC)- choice
2. Ivermectin (Stromectol)
3. Surgical removal Life Cycle Notes
4. Unna’s paste boots
− Vectors: Aedes, Anopheles, or Mansonia species
5. Elastic bandages
of mosquitoes
6. Simple elevation
− Anopheles mosquito can also transmit W.
bancrofti, which may result in a coinfection with
Prevention and Control
both filariae.
1. Use of personal protection when entering known
endemic areas − Adult worms reside in lymphatics.
2. Destroying mosquito breeding grounds − Microfilariae live in the blood and lymphatics.
3. Insecticides
4. Educating inhabitants of endemic areas Epidemiology
5. Mosquito netting/insect repellants − Found in numerous locations around the world
including:
1. Philippines
2. Brugia malayi 2. Sri Lanka
− Aka Malayan Filarial Worm 3. Vietnam
− B. timori is limited to the two islands of Timor, an 4. Specific regions of Japan, China
island of Indonesia − Felines and monkeys at risk for contracting
parasite even though humans are considered to
Two Forms: be the primary definitive host
1. The Nocturnal Form
− is the most common and is located near Clinical Symptoms
areas of coastal rice fields − Often asymptomatic
2. The Nonperiodic Form − Fevers may take months to years to develop after
− associated with infections in areas near initial infection.
swampy forests. − Other symptoms include:
1. Granulomatous lesions
2. Chills
3. Lymphadenopathy
4. Lymphangitis
5. Elephantiasis of legs
TRE DAME OF MARBEL UNIVERSITY
Medical Technology Department
NOTRE DAME OF MARBEL UNIVERSITY
Medical Technology Department
Compiled by: EFREN II C. DEOCADES, RMT
6. Elephantiasis of genitals less common Life Cycle Notes
7. Clinical disease progresses faster after − Vector: Chrysops fly
infection with B. malayi than with W. bancrofti − Adults live and multiply throughout the
8. Microfilariae may appear in the blood in as subcutaneous tissues.
little as 3 to 4 months − Microfiliariae appear in the blood years after
initial infection.
Laboratory Diagnosis − can persist in the human host for up to 17 years
− Method of choice: Fresh Giemsa-stained blood
smear Epidemiology
− Periodicity: typically nocturnal; Subperiodic − Africa – especially in rainforest belt
organisms are possible. − Infection rates estimated at over 70% in areas of
− Knott technique and serologic methods have known vector population existence
been developed and are available.
Clinical Symptoms
Treatment A. Loiasis
− Diethylcarbamazine (DEC) 1. Pruritus or itchiness and localized pain at bite
− Anti-inflammatory drugs may be necessary due site
to inflammatory reactions that may occur after 2. Adult worms may be noticeable when seen
treatment. migrating under the conjunctiva of the eye or
crossing under the skin of the bridge of the
Prevention and Control nose
− Use of personal protection when entering known 3. Calabar swellings
endemic areas
− Destroying mosquito breeding grounds
− Insecticides
− Educating inhabitants of endemic areas
− Mosquito netting
− Insect repellants
3. Loa loa
− Aka Eye worm
− Causes Calabar Swelling, Fugitive Swelling Laboratory Diagnosis
− Method of choice: Fresh Giemsa-stained blood
smear
− Knott technique
− Periodicity: diurnal {between 10:15 a.m. and
2:15 p.m.}
− Presence of eosinophilia and Calabar or transient
subcutaneous swellings aids in diagnosis
− Serologic testing is available
− Adult worm extraction {such as from the eye}
TRE DAME OF MARBEL UNIVERSITY
Medical Technology Department
NOTRE DAME OF MARBEL UNIVERSITY
Medical Technology Department
Compiled by: EFREN II C. DEOCADES, RMT
− Resulting microfilariae migrate throughout
infected nodules, subcutaneous tissues, skin, and
into the eye; rarely seen in peripheral blood.
Epidemiology
− Equatorial Africa and Central America:
1. Includes East Africa, Mexico, Brazil, and
others
− Vector breeds in running water, particularly along
streams and rivers.
Worm Removal from the Eye of an Infected Person
− There are known animal reservoir hosts.
Treatment
Clinical Symptoms
− Surgical removal of adult worms
− Onchocerciasis: river blindness
− Diethylcarbamazine (DEC)
1. Usually results in chronic, non-fatal condition
2. Localized symptoms caused by infected
Prevention and Control
nodule development
− Personal protection
3. Secondary bacterial infections due to
− Destroying vector breeding grounds scratching
− The prophylactic use of DEC 4. Eye involvement may lead to blindness
4. Onchocerca volvulus Laboratory Diagnosis
− Aka Blinding Worm, Convoluted Filaria − Multiple Giemsa-stained slides of tissue biopsies
− Causes River Blindness known as skin snips
1. To obtain uncontaminated sample (with other
microfilariae), skin snips are collected with as
little blood as possible.
− Adults may be seen during opthalmic exam.
− Serologic and PCR methods are available.
Treatment
− Ivermectin for treatment of microfilariae
− No known effective medication that treats both
microfilariae and adults without some toxic effects
or complications
− Long-term treatment may be necessary because
of long life span of adult worms
− Surgical removal of adult worms
Prevention and Control
Life Cycle Notes − Personal protection
− Vector: Black fly genus Simulium − Controlling vector breeding grounds and areas
− Adults encapsulate in subcutaneous fibrous where adults reside with insecticides
tumors and mate.
TRE DAME OF MARBEL UNIVERSITY
Medical Technology Department
NOTRE DAME OF MARBEL UNIVERSITY
Medical Technology Department
Compiled by: EFREN II C. DEOCADES, RMT
5. Mansonella ozzardi 2. Diethylcarbamazine (DEC) is treatment of choice.
Prevention and Control
1. Controlling vector populations
2. Because of small size of vectors, nets and
screening equipment ineffective prevention and
control measures
6. Mansonella perstans
Life Cycle Notes
− Vector: Culicoides sucking midge or Simulium
black fly
− Microfilariae found in blood and capillaries and
intravascular spaces of the skin.
− Emerging adults may reside in body cavities,
visceral fat, and mesenteries, but this is still
undocumented.
Epidemiology Laboratory Diagnosis
− Found exclusively in the Western Hemisphere − Blood
1. North, Central, and South America − Periodicity: non-periodic
2. West Indies and Caribbean
Life Cycle Notes
Clinical Symptoms − Vector: Culcoides sucking midge
A. Asymptomatic − Eye involvement common
B. Symptomatic − Humans primary definitive hosts
1. Urticaria − Incubation period once inside host – unknown
2. Lymphadenitis
3. Skin itching Epidemiology
4. Arthralgias − Africa, Caribbean Islands (select areas)
5. Eosinophilia − Panama
6. Adult worms cause minimal damage to − Northern South America
areas they inhabit − Primates thought to be reservoir hosts
Laboratory Diagnosis Clinical Symptoms
− Giemsa-stained peripheral blood smears − Infections with single worm are common and
− Periodicity: non-periodic cause little if any damage to affected tissue;
symptoms are minimal as well.
Treatment − Asymptomatic
1. Asymptomatic cases are usually not treated.
TRE DAME OF MARBEL UNIVERSITY
Medical Technology Department
NOTRE DAME OF MARBEL UNIVERSITY
Medical Technology Department
Compiled by: EFREN II C. DEOCADES, RMT
− Symptomatic Life Cycle Notes
1. Minor allergic reactions Natural Hosts/Definitive Host: Rats
2. Moderate eosinophilia Intermediate Hosts:
− Other symptoms Mollusks- Snail
1. Calabar swellings Pila luzonica- Kuhol
2. Headache Brotia asperata- Suso
3. Edema MOT: Ingestion of IH
4. Lymphatic discomfort Migrate to the brain and spinal cord causing
5. Evidence suggests a connection to joint and Eosinophilic Meningoencephalitis
bone pain and liver enlargement and pain
Characteristics
Treatment Female Worm: Barber’s Pole Appearance (whitish
− Asymptomatic infections usually not treated uterus, red digestive tract)
− Diethylcarbamazine (DEC), may involve multiple
treatments Female Worm of
− Alternative medication – mebendazole Barber’s Pole Parastrongylus
cantonensis
Prevention and Control
− Vector population control measures
− Personal protection from insect bites
Miscellaneous Nematodes
1. Parastrongylus cantonensis
− previously known as Angiostrongylus sp.,
− Aka Rat Lung Worm
− Causes: Cerebral Angiostrongyliasis
− Parastrongylus costaricensis: Abdominal
Angiostrongyliasis 2. Dirofilaria immitis
− Common Name: Dog Heart Worm
− Very common filarial parasite of dogs
− Clinical manifestations are characterized by
solitary, peripheral nodules in the lung (coin
lesions) or as subcutaneous nodule
TRE DAME OF MARBEL UNIVERSITY
Medical Technology Department
NOTRE DAME OF MARBEL UNIVERSITY
Medical Technology Department
Compiled by: EFREN II C. DEOCADES, RMT
3. Anisakis
− Common Name: Herring’s Worm
− Causes: Herring’s Disease
− Common in Japan
Definitive Host: Whales/ Dolphins
1st IH: Copepods
2nd IH: Smaller Fishes
3rd IH: Larger Fishes (Salmon)
MOT: ingestion of raw fish infected with larvae
Pathology: Abdominal Pain and Granuloma around
Migrating Larvae in Intestinal Wall
4. Toxocara spp.
A. Toxocara canis
− Visceral Larva Migrans
− intestinal ascarid of dogs
B. Toxocara cati
− Ocular Larva Migrans
− intestinal ascarid of cats
References
Belizario Jr., V. Y., & de Leon, W. U. (Eds.). (2015). Medical Parasitology in the
Philippines (3rd ed.). University of the Philippines Press.
Tille, P. M. (2017). Bailey and Scott’s diagnostic microbiology (14th ed.). Elsevier Inc.
Zeibig, E. A. (2013). Clinical Parasitology: A Practical Approach (2nd ed.). Saunders Elsevier.
Assessment
An online, 50-item quiz will be given and will be accessed using the Learning
Management System.
TRE DAME OF MARBEL UNIVERSITY
Medical Technology Department
NOTRE DAME OF MARBEL UNIVERSITY
Medical Technology Department
You might also like
- Soap Notes AsthmaDocument6 pagesSoap Notes AsthmaCHRISTINE KARENDINo ratings yet
- OSTEORADIONECROSISDocument38 pagesOSTEORADIONECROSISAbel AbrahamNo ratings yet
- Parasitology Lec 3.01b Blood and Tissue NematodesDocument15 pagesParasitology Lec 3.01b Blood and Tissue NematodesEnaWahahaNo ratings yet
- Lesson 2 Extraintestinal NematodesDocument5 pagesLesson 2 Extraintestinal NematodesCDNo ratings yet
- Wuchereria Bancrofti, Brugia Malayi, Brugia TimoriDocument3 pagesWuchereria Bancrofti, Brugia Malayi, Brugia TimoriJurel GaoatNo ratings yet
- Sheath: Structure of LarvaDocument4 pagesSheath: Structure of Larvaken mendozaNo ratings yet
- Clinical Parasitology-Module 11Document14 pagesClinical Parasitology-Module 11Geresh MagsinoNo ratings yet
- Clinical Parasitology-Module 8Document15 pagesClinical Parasitology-Module 8Geresh MagsinoNo ratings yet
- Blood and Tissue NematodesDocument37 pagesBlood and Tissue NematodesjelenaNo ratings yet
- Filarial Nematodes: Wuchereria BancroftiDocument8 pagesFilarial Nematodes: Wuchereria BancroftiMegumi TadokoroNo ratings yet
- Reviewer For para (Blood and Tissue Nematode)Document4 pagesReviewer For para (Blood and Tissue Nematode)K DNo ratings yet
- 3 - Loa Loa and Onchocerca VolvolusDocument29 pages3 - Loa Loa and Onchocerca VolvolusayaamrsharfNo ratings yet
- Filariae: Wuchereria BancroftiDocument8 pagesFilariae: Wuchereria BancroftiRaiset HermanNo ratings yet
- Midterm ParasitologyDocument18 pagesMidterm ParasitologyAngelic AngelesNo ratings yet
- FilariasisDocument11 pagesFilariasiskartiz008No ratings yet
- Blood Tissue NematodesDocument27 pagesBlood Tissue NematodesAfif Mamen100% (1)
- FilariaDocument85 pagesFilariaRajkishor YadavNo ratings yet
- Clinical Parasitology-Module 3Document12 pagesClinical Parasitology-Module 3Geresh MagsinoNo ratings yet
- Filariasis: Short As 4 Weeks or As Long As 8-16 Months Other Resources 6 Months and As Late As 12 Months After InfectionDocument12 pagesFilariasis: Short As 4 Weeks or As Long As 8-16 Months Other Resources 6 Months and As Late As 12 Months After Infectionchristian quiaoitNo ratings yet
- Merge AbDocument17 pagesMerge AbEricsson CarabbacanNo ratings yet
- Man Bahadur Rana BPH, Acas, NepalDocument34 pagesMan Bahadur Rana BPH, Acas, NepalDipankar NathNo ratings yet
- Filariasis: Short As 4 Weeks or As Long As 8-16 Months Other Resources 6 Months and As Late As 12 Months After InfectionDocument3 pagesFilariasis: Short As 4 Weeks or As Long As 8-16 Months Other Resources 6 Months and As Late As 12 Months After InfectionkyawNo ratings yet
- Arthropods As Vectors of Diseases: Dr. Jennifer O. Pichay AlvaradoDocument4 pagesArthropods As Vectors of Diseases: Dr. Jennifer O. Pichay AlvaradoMon Kristopher F. CastilloNo ratings yet
- Medical Parasitology A Self Instructional Text PDFDriveDocument60 pagesMedical Parasitology A Self Instructional Text PDFDriveDenise Sta. AnaNo ratings yet
- Merged PDF 2021 11 16T12 - 01 - 01Document15 pagesMerged PDF 2021 11 16T12 - 01 - 01Ericsson CarabbacanNo ratings yet
- PARA NematodesDocument23 pagesPARA Nematodes12 Newton - Cayetano, Arafe Nicole A.No ratings yet
- 4.3. Blood and Tissue NematodesDocument89 pages4.3. Blood and Tissue NematodesRediat GossayeNo ratings yet
- Microbiology 19 PDFDocument6 pagesMicrobiology 19 PDFLyka Villagracia AsiloNo ratings yet
- Loa Loa AyaDocument15 pagesLoa Loa AyaayaamrsharfNo ratings yet
- Filarial NematodeDocument18 pagesFilarial NematodeHawre NajmaddinNo ratings yet
- Helemnth ReportDocument15 pagesHelemnth ReportHawre NajmaddinNo ratings yet
- Parasitology Day 9 FilariaeDocument4 pagesParasitology Day 9 Filariaeniczdelosreyes8No ratings yet
- Lesson 5 - PlasmodiumDocument9 pagesLesson 5 - PlasmodiumAnya IgnacioNo ratings yet
- Wu C Here Ria Bancroft IDocument3 pagesWu C Here Ria Bancroft IMariamNo ratings yet
- Filariasis JC - DR Shefali GuptaDocument74 pagesFilariasis JC - DR Shefali GuptaShefali GNo ratings yet
- Filariasis 2015Document56 pagesFilariasis 2015ChandraNo ratings yet
- ROUNDWORMDocument8 pagesROUNDWORMSEAH KAI YEE MoeNo ratings yet
- Mycology TransDocument11 pagesMycology TransKita kitaNo ratings yet
- Lesson 5 Plasmodium SPPDocument8 pagesLesson 5 Plasmodium SPPAnya IgnacioNo ratings yet
- ANCYLOSTOMA DUODENALE Old World HookwormDocument2 pagesANCYLOSTOMA DUODENALE Old World HookwormScarlet AdolfoNo ratings yet
- Vectors PSM ParksDocument36 pagesVectors PSM ParksAshish RajputNo ratings yet
- Additional Notes Only Please Refer To Your Module Definition of TermsDocument4 pagesAdditional Notes Only Please Refer To Your Module Definition of TermsAndrea KamilleNo ratings yet
- Share Modul 1.2.21Document25 pagesShare Modul 1.2.21MECNESIA Tutor 2No ratings yet
- Lecture 7 Nematodes Part 2 New 2023Document19 pagesLecture 7 Nematodes Part 2 New 2023ayaessam392002No ratings yet
- 2.1 MalariaDocument10 pages2.1 MalariaNeil Gabriel EncinaNo ratings yet
- FilariaDocument16 pagesFilariaJessa MayNo ratings yet
- BN Filarial WormDocument137 pagesBN Filarial WormCherenet TomaNo ratings yet
- DNA VIRUSES-handout PDFDocument11 pagesDNA VIRUSES-handout PDFROTHESSA MARY CARINGALNo ratings yet
- Lesson 8 - Nematodes IDocument7 pagesLesson 8 - Nematodes IAnya IgnacioNo ratings yet
- Lymphatic Filariasis ClassDocument68 pagesLymphatic Filariasis ClassthehexhealthNo ratings yet
- Filariasis: Tropmed Block Faculty Medicine USU 2016Document26 pagesFilariasis: Tropmed Block Faculty Medicine USU 2016Tiurma SibaraniNo ratings yet
- Tissue NematodesDocument27 pagesTissue Nematodesbpt2100% (1)
- Parasites and Parasitism (Parasitology)Document3 pagesParasites and Parasitism (Parasitology)Joraine Nichole Roquero VillajuanNo ratings yet
- 7 BIO3243 ElephantiasisDocument11 pages7 BIO3243 ElephantiasisNGOGA NISINGIZWE NESTORNo ratings yet
- Module 9 - Nematodes Part 3Document50 pagesModule 9 - Nematodes Part 3Arnold GarcinesNo ratings yet
- 7 Module 6 Nematodes Part 2Document100 pages7 Module 6 Nematodes Part 2Luke Jovanni TAOCNo ratings yet
- Revision: Types of Life Cycle in Trematoda and CestodaDocument54 pagesRevision: Types of Life Cycle in Trematoda and CestodaMicroscopeGeekNo ratings yet
- Filaria - A Comprehensive StudyDocument63 pagesFilaria - A Comprehensive StudyDayledaniel SorvetoNo ratings yet
- Parasitic Causes of HaematologyDocument65 pagesParasitic Causes of HaematologySolomonNo ratings yet
- 017 Wuchereria BrugiaDocument21 pages017 Wuchereria BrugiaAyop KhNo ratings yet
- Man Bahadur Rana BPH, Acas, NepalDocument34 pagesMan Bahadur Rana BPH, Acas, NepalDipankar NathNo ratings yet
- 5 PyatakDocument21 pages5 PyatakJust HelpingNo ratings yet
- Syllabus Master Tung PDFDocument25 pagesSyllabus Master Tung PDFkamran ahmad100% (1)
- Escala Del Dolor PPPDocument16 pagesEscala Del Dolor PPPMariana SuarezNo ratings yet
- Paediatrics Solved OspeDocument24 pagesPaediatrics Solved OspeSalim KhaleelNo ratings yet
- Chapter 19 AddictionDocument5 pagesChapter 19 AddictionTrixie Myr AndoyNo ratings yet
- Pretend Play Printables I'm A Zoo Keeper - 123 Homeschool 4 MeDocument22 pagesPretend Play Printables I'm A Zoo Keeper - 123 Homeschool 4 Mekantor perencanaan2022No ratings yet
- Pi Is 0828282 X 19315508Document16 pagesPi Is 0828282 X 19315508Mitch TobinNo ratings yet
- A Group Case Study 2nd Sem 1Document46 pagesA Group Case Study 2nd Sem 1Shermaigne Ananayo BuyaNo ratings yet
- Somatoform DisorderDocument30 pagesSomatoform DisorderRujuta BaramateNo ratings yet
- اسئلة طفيليات MCQ مهمة جدا PDFDocument15 pagesاسئلة طفيليات MCQ مهمة جدا PDFفواطم صائب عباس فاضلNo ratings yet
- Mamba Inservice Ic504901aaDocument19 pagesMamba Inservice Ic504901aamayra osorioNo ratings yet
- NP40126 SaeDocument9 pagesNP40126 SaeMohd AljawfiNo ratings yet
- Nur 102Document3 pagesNur 102Fretchel Grace Silverado MesaNo ratings yet
- ADHD in Women Checklist - UpdatedDocument4 pagesADHD in Women Checklist - UpdatedMohamed Gamal HassanNo ratings yet
- ImmunityDocument19 pagesImmunityKailash Nagar100% (1)
- Antibiotic Stewardship in OrthopedicsDocument17 pagesAntibiotic Stewardship in Orthopedicsjomari dvNo ratings yet
- Maam Jean OR SCHED 10112022Document2 pagesMaam Jean OR SCHED 10112022Jean Camille Lazo MendozaNo ratings yet
- ECG Quiz Review and Practice Strip AnswersDocument7 pagesECG Quiz Review and Practice Strip AnswersAANo ratings yet
- Breast Tumours: Introductory NotesDocument8 pagesBreast Tumours: Introductory Notesdiego fernando lobo moncadaNo ratings yet
- RN Targeted Medical Surgical Immune Online Practice 2019Document6 pagesRN Targeted Medical Surgical Immune Online Practice 2019Adriana RemedioNo ratings yet
- Colorectal Cancer Genetic SyndromesDocument1 pageColorectal Cancer Genetic SyndromesRyan GosserNo ratings yet
- 3 - Gastrointestinal Dis - 2020 - Hunter S Tropical Medicine and Emerging InfectDocument11 pages3 - Gastrointestinal Dis - 2020 - Hunter S Tropical Medicine and Emerging InfectThaiz P.SNo ratings yet
- Seizures in Critical Care. A Guide To Diagnosis AnDocument1 pageSeizures in Critical Care. A Guide To Diagnosis AnRENAULTNo ratings yet
- POLYHYDRAMNIOSDocument2 pagesPOLYHYDRAMNIOSyxly imperialNo ratings yet
- Module 9 - Nematodes Part 2Document78 pagesModule 9 - Nematodes Part 2Arnold GarcinesNo ratings yet
- TranslateDocument8 pagesTranslateberliananastasya pNo ratings yet
- Psychiatry: Psychology-Psychiatric Evaluation - 1 (Medical Transcription Sample Report)Document7 pagesPsychiatry: Psychology-Psychiatric Evaluation - 1 (Medical Transcription Sample Report)Nguyên VũNo ratings yet
- Major Depressive Disorder and Difference Between Genders: Dzevad Sabic, Adela Sabic, Amila Bacic-BecirovicDocument4 pagesMajor Depressive Disorder and Difference Between Genders: Dzevad Sabic, Adela Sabic, Amila Bacic-BecirovicDzevad SabicNo ratings yet