Professional Documents
Culture Documents
E Vascular (Blue Keyword Pyq)
E Vascular (Blue Keyword Pyq)
Uploaded by
Irsyad SiddeeqCopyright:
Available Formats
You might also like
- Study Notes Family MedicineDocument49 pagesStudy Notes Family MedicineMedShare85% (27)
- Medicine Cheat SheetsDocument16 pagesMedicine Cheat SheetsRisa Muthmainah100% (1)
- Clinical Medicine Cheat Sheet Ebook PDFDocument18 pagesClinical Medicine Cheat Sheet Ebook PDFMoka100% (1)
- Common Cases in Vascular SurgeryDocument72 pagesCommon Cases in Vascular Surgerynohazz100% (2)
- Cirugía - Gastrointestinal Emergencies Evidence-Based Answers To Key Clinical Questions 2019Document463 pagesCirugía - Gastrointestinal Emergencies Evidence-Based Answers To Key Clinical Questions 2019David ReyesNo ratings yet
- Adhesive CapsulitisDocument7 pagesAdhesive CapsulitisMariane GumbanNo ratings yet
- Seminar PVD Y5B2Document51 pagesSeminar PVD Y5B2Kamilla AbdullahNo ratings yet
- Electrical Wire Burn, For Which Children Must Be Admitted ForDocument7 pagesElectrical Wire Burn, For Which Children Must Be Admitted Forraja020No ratings yet
- Acute Limb Ischemia Vs Critical Limb Ischemia: Clinical PracticeDocument54 pagesAcute Limb Ischemia Vs Critical Limb Ischemia: Clinical PracticeKiara GovenderNo ratings yet
- Cardio I: Shock, CHF, HTN, ACS Cheat Sheet: by ViaDocument3 pagesCardio I: Shock, CHF, HTN, ACS Cheat Sheet: by ViaMariana NannettiNo ratings yet
- Acute Limb Ischaemia (ALI) Refers To The Sudden: Interruption of Arterial Blood SupplyDocument36 pagesAcute Limb Ischaemia (ALI) Refers To The Sudden: Interruption of Arterial Blood SupplyAuliyah SeptianiNo ratings yet
- Cap 12Document27 pagesCap 12Saul RivasNo ratings yet
- Limb Ischemia VascularDocument6 pagesLimb Ischemia Vascularalbadrimohammed1997No ratings yet
- Vasculitis: Disorder Vessels Pathology Presentation Test TX OtherDocument3 pagesVasculitis: Disorder Vessels Pathology Presentation Test TX OthermcwnotesNo ratings yet
- Clinical MedicineDocument18 pagesClinical MedicineRishikesh AsthanaNo ratings yet
- Chapter 36Document3 pagesChapter 36Samantha QuintoNo ratings yet
- Arterial Disease (Critical Limb Ischaemia)Document2 pagesArterial Disease (Critical Limb Ischaemia)dragtoss2No ratings yet
- Medicine Revision - Neurology TableDocument10 pagesMedicine Revision - Neurology TableUnomoshNo ratings yet
- Myocardial Infarction and StrokeDocument13 pagesMyocardial Infarction and StrokeSunghoonOnlyNo ratings yet
- Dr. Dioszeghy Peter MononeuropathiesDocument52 pagesDr. Dioszeghy Peter MononeuropathiesAhmad abu-dayyehNo ratings yet
- Peripheral Vascular DiseaseDocument7 pagesPeripheral Vascular DiseaseRosalinda PerigoNo ratings yet
- Arterial DiseaseDocument57 pagesArterial DiseaseYil MosNo ratings yet
- IV Surgery PDFDocument265 pagesIV Surgery PDFاللهم أصلح أمريNo ratings yet
- Peripheral Arterial DiseaseDocument5 pagesPeripheral Arterial Diseaseampogison08No ratings yet
- Defibrillation Is The Definitive Treatment For The Life-Threatening Cardiac ArrhythmiasDocument4 pagesDefibrillation Is The Definitive Treatment For The Life-Threatening Cardiac ArrhythmiasErika RiceNo ratings yet
- DRUG-STUDY-FORMAT-Binangonan Lakeview 2ndDocument2 pagesDRUG-STUDY-FORMAT-Binangonan Lakeview 2ndDianne UlandayNo ratings yet
- Regional Anaesthesia: Anna WelbournDocument49 pagesRegional Anaesthesia: Anna WelbournAnna Welbourn100% (1)
- RaDocument40 pagesRaMuhammad MakkiNo ratings yet
- Peripheral Arterial Occlusive DiseaseDocument6 pagesPeripheral Arterial Occlusive DiseaseAila HinlogNo ratings yet
- Myasthenia Gravis: MG-epidemiologyDocument3 pagesMyasthenia Gravis: MG-epidemiologyRemigius RiyanNo ratings yet
- Atherosclerosis Angina Pectoris Myocardial InfarctionDocument2 pagesAtherosclerosis Angina Pectoris Myocardial InfarctionKaren Mae AlcantaraNo ratings yet
- Peripheral Arterial Occlusive DiseaseDocument43 pagesPeripheral Arterial Occlusive DiseaseadystiNo ratings yet
- Vascular Note by Joel ArudchelvamDocument52 pagesVascular Note by Joel ArudchelvamJoel Arudchelvam100% (1)
- Stroke CVDDocument9 pagesStroke CVDangel.senido0198No ratings yet
- IM Part 1Document48 pagesIM Part 1sasghfdgNo ratings yet
- IM Part 1 and 2 CombinedDocument100 pagesIM Part 1 and 2 CombinedsasghfdgNo ratings yet
- 2 Hemiplegia TIAs 452Document30 pages2 Hemiplegia TIAs 452vmj8tyh5dsNo ratings yet
- Acute Limb Ischemia Vs Critical Limb Ischemia: Clinical PracticeDocument51 pagesAcute Limb Ischemia Vs Critical Limb Ischemia: Clinical PracticedrhendyjuniorNo ratings yet
- RheumatologyDocument21 pagesRheumatologyApsaraNo ratings yet
- Simposium Papdi 3-Hari 1-5. Ws 1 - Dr. Lita-Untuk Share-2. Dr. LitaDocument46 pagesSimposium Papdi 3-Hari 1-5. Ws 1 - Dr. Lita-Untuk Share-2. Dr. LitaRangga Alam VaneoNo ratings yet
- Disease/syndrome Inciting Incident Structures Affected PoliomyelitisDocument12 pagesDisease/syndrome Inciting Incident Structures Affected PoliomyelitismrhemmatNo ratings yet
- Room #106 DSDocument2 pagesRoom #106 DSALYSSA GAILE ESPIRITUNo ratings yet
- Seminar-Quadripplegia, Paraplegia, MNDDocument107 pagesSeminar-Quadripplegia, Paraplegia, MNDSalsabila Al-BasheerNo ratings yet
- ShitDocument15 pagesShitEden Marie FranciscoNo ratings yet
- Medurg MidtermDocument4 pagesMedurg Midtermmark OrpillaNo ratings yet
- Sports MedicineDocument32 pagesSports Medicinersimranjit100% (1)
- 2 Cardio Lecture PDFDocument9 pages2 Cardio Lecture PDFNadia AbdurasidNo ratings yet
- FIX Leg UlcerDocument59 pagesFIX Leg UlcerDekka Andra100% (2)
- Cardio My Opa Thies ChartDocument2 pagesCardio My Opa Thies ChartSolomon Seth SallforsNo ratings yet
- Nesiritide2Document2 pagesNesiritide2Christine Pialan SalimbagatNo ratings yet
- Q1.Flaccid Paresis: Diagnostical VariantsDocument47 pagesQ1.Flaccid Paresis: Diagnostical VariantsNelson OduorNo ratings yet
- Proximal Femur Fractures: Sulita Turaganiwai s130364Document26 pagesProximal Femur Fractures: Sulita Turaganiwai s130364Wālē NandNo ratings yet
- Rheuma (Gout, CPD, Rheumatoid Arthritis, Osteoarthritis)Document2 pagesRheuma (Gout, CPD, Rheumatoid Arthritis, Osteoarthritis)Jezreel Yanah De LeonNo ratings yet
- Med Surg BundleDocument82 pagesMed Surg BundleThe Treasure ChestNo ratings yet
- Chronic Limb Ischemia: Prof. Dr. A.B.Singh UnitDocument59 pagesChronic Limb Ischemia: Prof. Dr. A.B.Singh UnitDr. Saad SiddiquiNo ratings yet
- Chapter 41 - Tingling and NumbnessDocument7 pagesChapter 41 - Tingling and NumbnessJonalyn MejellanoNo ratings yet
- Modern Anaesthesia:: A Concise Guide to the Study and Practice of Anaesthesia.From EverandModern Anaesthesia:: A Concise Guide to the Study and Practice of Anaesthesia.No ratings yet
- Article in Press: Age-Related Hair Changes in Men: Mechanisms and Management of Alopecia and GrayingDocument5 pagesArticle in Press: Age-Related Hair Changes in Men: Mechanisms and Management of Alopecia and Grayingpasid harlisaNo ratings yet
- The Aftereffects of Dynamic Exercise On Ambulatory Blood PressureDocument7 pagesThe Aftereffects of Dynamic Exercise On Ambulatory Blood PressureTAINAH DE PAULANo ratings yet
- MWS 130S, MWS 140S MWS 330B, MWS 330S, MWS 340B, MWS 430S: Welcome To The Family. Let's Get StartedDocument56 pagesMWS 130S, MWS 140S MWS 330B, MWS 330S, MWS 340B, MWS 430S: Welcome To The Family. Let's Get StartedMirjana PrekovicNo ratings yet
- Vitamina DDocument57 pagesVitamina DGabriel HerreraNo ratings yet
- PAMA NursingCaseStudy Revised PDFDocument77 pagesPAMA NursingCaseStudy Revised PDFJeofy PamaNo ratings yet
- Yds Kamp Gã N 1 Yds Eyds Kelime Sorularä 18 02 2022Document5 pagesYds Kamp Gã N 1 Yds Eyds Kelime Sorularä 18 02 2022Alihan GökNo ratings yet
- Nepal Health Professional Council: Syllabus For Professional Licensing Examination of Grade A-Diagnostic Health LabDocument10 pagesNepal Health Professional Council: Syllabus For Professional Licensing Examination of Grade A-Diagnostic Health LabBhageshwar ChaudharyNo ratings yet
- Eye & EarDocument27 pagesEye & EarZamzam IsmailNo ratings yet
- Adesola Tolulope Akanmu Final ProjectDocument104 pagesAdesola Tolulope Akanmu Final Projectajuguisrael6No ratings yet
- Eight Principles For Patient-Centred and Family-Centred Care For Newborns in The Neonatal Intensive Care UnitDocument5 pagesEight Principles For Patient-Centred and Family-Centred Care For Newborns in The Neonatal Intensive Care UnitPaola RoigNo ratings yet
- MiorelDocument1 pageMiorelApostolos T.No ratings yet
- 13 Vassileva Pediatric DRLDocument57 pages13 Vassileva Pediatric DRLLavinia BaracNo ratings yet
- Blood Vessel Detection From Retinal Fundas ImagesDocument10 pagesBlood Vessel Detection From Retinal Fundas ImagesNaoufal NaoufalNo ratings yet
- Electroencephalography (EEG) in The Diagnosis of Seizures and Epilepsy - UpToDate PDFDocument37 pagesElectroencephalography (EEG) in The Diagnosis of Seizures and Epilepsy - UpToDate PDFRobert MîndreanuNo ratings yet
- Nursingcrib Com NURSING CARE PLAN Hepatitis A PDFDocument2 pagesNursingcrib Com NURSING CARE PLAN Hepatitis A PDFswapnilazarusNo ratings yet
- Imaging For Neuro-Ophthalmic and Orbital Disease - A ReviewDocument24 pagesImaging For Neuro-Ophthalmic and Orbital Disease - A ReviewMashhoor AlfayezNo ratings yet
- Theories of Ageing: DR Prema BalusamyDocument19 pagesTheories of Ageing: DR Prema Balusamyprema balusamyNo ratings yet
- Free Download Jim Hanvey Detective Octavus Roy Cohen Full Chapter PDFDocument51 pagesFree Download Jim Hanvey Detective Octavus Roy Cohen Full Chapter PDFbarbara.johnson937100% (20)
- PathologyDocument32 pagesPathologyShashanka PoudelNo ratings yet
- Vitamin B6 Deficiency: Brown MJ, Ameer MA, Beier KDocument9 pagesVitamin B6 Deficiency: Brown MJ, Ameer MA, Beier Knadin nNo ratings yet
- Ilovepdf MergedDocument503 pagesIlovepdf MergedRitika NigamNo ratings yet
- Oxygen Therapy Powerpoint - Jan 2016 Student ViewDocument47 pagesOxygen Therapy Powerpoint - Jan 2016 Student ViewMark Anthony AlcantaraNo ratings yet
- ACL Injury: DR Keith HoltDocument14 pagesACL Injury: DR Keith HoltAnum TahirNo ratings yet
- Myofunctional Orthodontics and Myofunctional TherapyDocument1 pageMyofunctional Orthodontics and Myofunctional TherapysirahNo ratings yet
- Waht-Nur-065 V7Document25 pagesWaht-Nur-065 V7Else FashiosNo ratings yet
- Nursing Documentation - Frameworks and Barriers PDFDocument10 pagesNursing Documentation - Frameworks and Barriers PDFDany Marin RNo ratings yet
- Parent Ver SCH 0 6yrsDocument2 pagesParent Ver SCH 0 6yrsSrinivasamurthy KamarthiNo ratings yet
- Aditya Birla Sun Life Insurance Life Shield PlanDocument12 pagesAditya Birla Sun Life Insurance Life Shield PlanRitesh AgrawalNo ratings yet
- Table of Content: Risk AssesmentDocument25 pagesTable of Content: Risk AssesmentvijayNo ratings yet
E Vascular (Blue Keyword Pyq)
E Vascular (Blue Keyword Pyq)
Uploaded by
Irsyad SiddeeqOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
E Vascular (Blue Keyword Pyq)
E Vascular (Blue Keyword Pyq)
Uploaded by
Irsyad SiddeeqCopyright:
Available Formats
Vascular – Vascular – Vascular MOZZAR
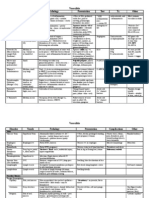
NO LIST OF DIAGNOSIS PATHO/RISK FACTORS/ CAUSES CLINICAL PRESENTATION/ COMPLICATIONS INVESTIGATION MANAGEMENT
1 Lower Extremities ‐ Systemic atherosclerotic process with Intermittent claudication – reproducible muscles Classification: Fontaine’s Classification Mx for asymptomatic pt
Arterial Disease subintimal lipid and fibrous material discomfort, induced by exercise, relieved with rest (Europe) or Rutherford Classification (USA) Best medical therapy – smoking cessation, healthy diet,
(LEAD) accumulation diffuse stenosis of CLTI – rest pain, need opioid analgesia, >2 weeks, exercise, lipid control, HTN control, DM control, single anti‐
peripheral arteries diminished blood gangrene/ ulcers over toes or feet, ABPI ≤0.5 Ankle‐brachial pressure index (>0.9 normal, platelet therapy
supply 0.5‐0.9 occluded, <0.5 critical ischemia rest Mx for symptomatic (claudication) pt
‐ Risk factors; existing dz (DM, CAD, stroke, Ischemic rest pain – severe pain in distal lower limb, pain) Supervised exercise training
TIA), non‐modifiable (age, gender, FHx), at rest, at night, wakes pt from sleep, aggravated by Arterial Duplex ultrasound – 1st line imaging for Lifelong anti‐platelet drugs – Aspirin 100mg or clopidogrel
modifiable (smoking, HTN, lifting limb, relieved by dependency, often requires PAD 75mg
hyperlipidaemia, DM, obesity) opioids ‐ Normal; triphasic Pharmacological agents to decrease walking impairment –
‐ Abnormal; biphasic and Cilostazol, naftidrofuryl
Ischemic ulcers – often painful, on tips of toes, bunion monophasic waves Revascularization therapy
area, over metatarsal heads, lateral malleolus, deep, Basic lab Ix, transcutaneous oxygen pressure Mx of chronic limb ischemia
dry, punctate (TcPO2), CT angiogram with iodinated contrast, Endovascular – lower limb angiography, angioplasty KIV
MR angiogram with contrast stenting
Stenosis of lower aorta & common iliac – buttock Open surgical intervention with bypass grafting
claudication, impotence Angiogram with digital subtraction – GOLD Endarterectomy – for severe stenosis of common femoral and
Stenosis of external iliac – thigh claudication STANDARD for evaluating arterial tree prior to profunda femoris arteries
Stenosis of superficial femoral – calf claudication revascularization Mx of gangrenous limb
Infection and pain control
Prompt revascularization
Amputation (dead, damaged, dangerous, damn nuisance)
2 Buerger’s disease ‐ Aka thromboangiitis obliterans Foot, leg, arm, or hand claudication Angiography of all 4 limbs – segmental Smoking cessation
‐ Progressive non‐atherosclerotic Progress to calf claudication, eventually ischemic rest occlusions, “skip” lesions, extensive
segmental inflammatory disease pain, ulceration on toes, feet, or fingers collateralization “cock‐screw collaterals”
3 Acute limb ischemia ‐ Sudden decrease in limb perfusion that Classic 6 P’s; Pain, paraesthesia, pain, pallor, Biochemical; FBC, RP, GXM, Trop I Early anticoagulation – IV heparin bolus 3000‐5000 units (70
threatens viability of limb perishingly cold, paralysis, pulselessness units/kg), follow with IV heparin infusion at 1000 units/hr (10‐
‐ Present within 2/52 of acute event Imaging; Duplex ultrasound, CXR/ECG, CT 15 units/kg/hr), ideal PTT is 2‐2.5 times normal
‐ Risk factors; Arterial embolism, Acute Pain – acute, start off in distal part, progresses angiogram Measure to improve existing perfusion – keep foot dependent,
thrombosis, Arterial trauma, Dissecting proximally avoid pressure to heel, O2 supply, correct hypotension
aortic aneurysm Paraesthesia – progression; light touch vibration Surgical emergency requiring active intervention – Emergency
‐ Rutherford Criteria for ALI; Stage I (limb proprioception – deep pain pressure sense thrombectomy/ embolectomy
viable), Stage II (limb threatened), Stage III Paralysis – poor prognostic sign. (Initial; heavy limb), KIV fasciotomy to prevent compartment syndrome
(non‐viable) (late irreversible ischaemia; muscle turgidity)
[Cx; reperfusion injury, rhabdomyolysis,
compartment syndrome]
4 Carotid disease ‐ Symptomatic carotid stenosis – stenosis in Asymptomatic; carotid bruit Best medical therapy – BP <140/90, statin Tx, stop smoking,
internal carotid artery leading to Symptomatic; carotid territory – hemi‐motor/ hemi‐ stop alcohol, exercise, diet modification, reduce weight, anti‐
symptoms of amaurosis fugax, TIA, sensory signs, monocular blindness (amaurosis platelet Tx
ipsilateral ischemic stroke fugax), higher cortical dysfunction (ie dysphagia, Carotid endarterectomy – mostly if pt symptomatic
visuospatial neglect)
5 Subclavian Steal ‐ Arteriosclerotic stenotic plaque at origin More commonly occurs on left arm Bypass graft from common carotid to subclavian artery distal
syndrome of subclavian Claudication of arm to stenosis
Posterior neurologic signs eg hearing loss, tinnitus,
blurred vision, dizziness, vertigo, loss of muscle
coordination, or ataxia, fainting
6 Aortic dissection ‐ Abnormal blood flow through focal defect Anterior chest pain or pain – sudden onset, tearing Biochemical – FBC, RP, Trop I, coagulation Main aim; reduces left ventricular pressure while maintaining
in intima into medial later. Blood return to sensation, mimicking MI profile, GXM, ABG/ lactate adequate distal organ perfusion
true lumen of artery distally or ruptures Abdominal pain – possible mesenteric ischemic Imaging; Stanford A (surgical emergency) – primary open surgical repair
externally Syncope – cerebrovascular involved ‐ ECG – ST, T wave changes (repair ascending aorta ± aortic valve replacement)
‐ Risk factors; advanced age, HTN, smoking, Upper extremity Sx (pain, weakness, paraesthesia) – ‐ CXR – widened mediastinum, Stanford B (medical emergency) – IV labetalol to control HR
male, structural abnormalities of aortic subclavian A involved pleural effusion, abnormal aortic and produce vasodilation. Require surgery if got Cx
wall, collagen vascular condition Lower extremity Sx – iliac/ femoral A involved contour
‐ CT aortogram – GOLD STANDARD
Vascular – Vascular – Vascular MOZZAR
(Marfan’s syndrome, Ehler‐Danlos Cx – bleeding, cardiac arrhythmias, neurological ‐ 2D echo
syndrome), pregnancy dysfunction, acute renal impairment, multi‐organ
‐ Stanford Classification; Stanford A (involve failure
ascending aorta), Stanford B (not involve
ascending aorta)
‐ DeBakey classification
7 Abdominal aortic ‐ Aortic diameter >50% larger (normal Asymptomatic – found incidentally, pulsatile/ Diagnostic imaging Asymptomatic AAA
aneurysm ~2cm) expansile abdominal mass, or on imaging Ultrasound abdomen – assess size and position No role for surgical repair, ‘best care’ favours surveillance
‐ Most AAA develop below renal arteries Classical presentation – hypotension, intense CT aortogram/ MR aortogram Medical Mx; smoking cessation, optimize BP, statins to reduce
(infra‐renal artery) abdominal pain radiating to back, pulsatile abdominal Portable CXR to look for dissection/ aneurysmal growth rates
‐ Risk factors; Modifiable (smoking, HTN), mass mediastinal widening Surgical option; Open AAA repair or Endovascular aneurysm
non‐modifiable (male, FHx, connective Local compression – radicular symptoms in thigh and repair
tissue disorder, advanced age, COPD, groin (nerve root compression), GI, urinary Pre‐operative Ix
hyperhomocysteinemia obstruction FBC, RP, PT/PTT, GXM, ECG Symptomatic AAA
Rupture into IVC – audible abdominal bruit, venous Echocardiogram/ Pulmonary function test Indications; any size painful or tender, any size that is causing
HTN (swollen cyanotic legs, lower GI bleed, distal embolization
hematuria) Option; open surgery or endovascular approach
Distal embolization – intraluminal thrombus
emboli ALI or mottling of lower trunk and Ruptured AAA
extremity Can rupture anterior into peritoneal cavity or posterolaterally
into retroperitoneal space
PE; visible pulsation on abdomen, pulsation and mass Option; open surgery or endovascular approach
in epigastric region felt on deep palpation, mass is Acute Mx; stabilize pt, fluid resuscitation, urgent CT
expansile (fingers pushed upwards and outwards) angiogram, NBM GI decompression with NG tube, open repair,
IV broad spectrum antibiotic, analgesia
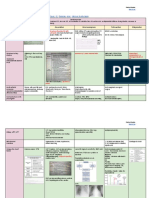
8 Chronic Venous ‐ Venous HTN results from obstruction to Venous dilatation – telangiectasias, reticular veins, Venous duplex ultrasound – evidence of Venous compression therapy using elastic stockings/ wraps
Insufficiency (CVI) venous flow (tumour compression, varicosities, corona phlebectatica venous reflux, ultrasound features of DVT Laser therapy – endovenous thermal ablation
pregnancy, DVT), dysfunction of venous Oedema – pitting: Hallmark of CVI MR venogram Meds‐ antibiotics
valves (varicose veins), or failure of Skin changes – hyperpigmentation, phlegmasia alba Lab studies; CBC, thrombophilia panel, Surgical treatment – ligation, ambulatory phlebectomy, vein
“venous pump” (dependent on adequate dolens, phlegmasia cerulea dolens, atrophie blanche, microbiology bypass, vein valvuloplasty
contraction. Stroke, muscular weakness venous stasis eczema, lipodermatosclerosis, cellulitis Non‐surgical treatment – sclerotherapy (chemical ablation)
can cause failure) Venous ulcer formation – typically over medial
‐ CEAP classification; Clinical, Etiologic, malleolus, shallow, flat ulcer, sloping edges, base may Weight Mx, leg elevation, exercise, avoid wearing tight
Anatomic, Pathophysiologic be sloughy or granulating, usually quite moist‐looking clothing, avoid long standing and sitting
Leg fullness, aching discomfort, heaviness, nocturnal
leg cramps, bursting upon standing
9 Varicose vein ‐ Dilated tortuous subcutaneous vein that it Asymptomatic Venous duplex ultrasound Conservative
≥3mm in diameter measured in upright Symptomatic – non‐specific pain, tingling, aching, Indications; recurrent varicose veins, history of Lifestyle changes – decrease time spent standing, weight loss
position burning, muscle cramps, swelling, sensation of superficial thrombophlebitis or DVT Graduated compression stockings
‐ Risk factors; age, occupation, weight, throbbing or heaviness, itching skin, restless leg, leg Medications eg Daflon
posture (crossing legs all time), increased tiredness, worsen with heat, worsen throughout
abdominal pressure (constipation, chronic course of day, relieved by resting or elevating legs or Surgical
cough), pelvic tumour compressing deep wearing elastic stockings Indications; Cx present, Sx (pain, bleeding, thrombophlebitis,
veins, FHx discomfort), cosmesis
Cx; thrombophlebitis, bleeding, hyperpigmentation, Options; endovenous laser/ radio‐frequency ablation of
eczema, ulceration saphenous vein, US‐guided injection foam sclerotherapy
10 Venous ulcers ‐ Cause; by any cause of CVI Exclude infection and other Cx; blood test, Non‐surgical; 4‐layer compression bandage, analgesia,
inflammatory markers, wound swab for gram antibiotics, avoid trauma, rest and elevate leg, compression
stain and culture, X‐ray stockings should be fitted once healed and continued for life
Venous duplex ultrasound Surgical ± endovenous ablation
ABPI
Biopsy venous ulcer if cannot exclude
malignant transformation
Vascular – Vascular – Vascular MOZZAR
11 Deep venous ‐ Formation of a blood clot in the deep veins Unilateral leg pain and swelling DVT Wells’ Score should be calculated: Direct oral anticoagulants* (DOACs) as first line
thrombosis of a limb, most commonly affecting those Other symptoms include low‐grade pyrexia, pitting ‐ Score less than or equal to 1 – DVT is clinically Anticoagulation treatment should be continued for 3 months
of the legs or pelvis oedema, tenderness, or prominent superficial veins unlikely, requires a further D‐dimer test to in those with a provoked DVT, however in those with a
Importantly, 65% of DVTs are asymptomatic exclude proximal DVT and a persistent risk factor or high risk of DVT
‐ Score greater than 1 – DVT is clinically likely recurrence may require lifelong anticoagulation
and a DVT diagnosis should be confirmed via
either a ultrasound scan (more common) or a Mechanical Thromboprophylaxis; Antiembolic stockings (AES),
contrast venography (rarely used) Intermittent pneumatic compression (IPC, more commonly
used in theatre)
Pharmacological Thromboprophylaxis; Low molecular weight
heparin (LMWH), unless poor renal function (eGFR<30) then
consider unfractionated heparin (UFH)
12 Pulmonary ‐ Risk factor; recent surgery, thrombophilia, Dyspnoea, chest pain, palpitation, syncope D‐dimer – if negative, excludes pulmonary Haemodynamic unstable Supportive Tx (O2, fluid challenge,
embolism leg fracture, prolonged bed rest/ reduced Preceding leg pain, cough, haemoptysis, fever, embolism vasopressor adrenaline). Immediate bedside echo. Confirm Dx
mobility, malignancy, pregnancy/ syncope FBC, U&E, Baseline clotting via CTPA. Anticoagulation – IV UFH
postpartum Cyanosis, tachypnoea, tachycardia, raised JVP, pleural ABG Definitive Tx – reperfusion Tx systemic thrombolysis IV rtPA
rub, pleural effusion, hypotension CXR – dilated pulmonary artery, linear Haemodynamic stable
atelectasis, pleural effusion, reduced vascular Confirm via CTPA (high risk), serum D‐dimer
Cx; pulmonary infarction, pleural effusion, right‐sided markings, wedge‐shaped infarct Anticoagulation – SC LMWH
heart failure, peripheral oedema, massive PE can CTPA – test of choice for high risk pt Long term Anticoagulation warfarin/DOAC min for 3months
cause lethal Cx like cardiac arrest, circulatory collapse ECG – tachycardia, RBBB, S1Q3T3
and cardiogenic shock
You might also like
- Study Notes Family MedicineDocument49 pagesStudy Notes Family MedicineMedShare85% (27)
- Medicine Cheat SheetsDocument16 pagesMedicine Cheat SheetsRisa Muthmainah100% (1)
- Clinical Medicine Cheat Sheet Ebook PDFDocument18 pagesClinical Medicine Cheat Sheet Ebook PDFMoka100% (1)
- Common Cases in Vascular SurgeryDocument72 pagesCommon Cases in Vascular Surgerynohazz100% (2)
- Cirugía - Gastrointestinal Emergencies Evidence-Based Answers To Key Clinical Questions 2019Document463 pagesCirugía - Gastrointestinal Emergencies Evidence-Based Answers To Key Clinical Questions 2019David ReyesNo ratings yet
- Adhesive CapsulitisDocument7 pagesAdhesive CapsulitisMariane GumbanNo ratings yet
- Seminar PVD Y5B2Document51 pagesSeminar PVD Y5B2Kamilla AbdullahNo ratings yet
- Electrical Wire Burn, For Which Children Must Be Admitted ForDocument7 pagesElectrical Wire Burn, For Which Children Must Be Admitted Forraja020No ratings yet
- Acute Limb Ischemia Vs Critical Limb Ischemia: Clinical PracticeDocument54 pagesAcute Limb Ischemia Vs Critical Limb Ischemia: Clinical PracticeKiara GovenderNo ratings yet
- Cardio I: Shock, CHF, HTN, ACS Cheat Sheet: by ViaDocument3 pagesCardio I: Shock, CHF, HTN, ACS Cheat Sheet: by ViaMariana NannettiNo ratings yet
- Acute Limb Ischaemia (ALI) Refers To The Sudden: Interruption of Arterial Blood SupplyDocument36 pagesAcute Limb Ischaemia (ALI) Refers To The Sudden: Interruption of Arterial Blood SupplyAuliyah SeptianiNo ratings yet
- Cap 12Document27 pagesCap 12Saul RivasNo ratings yet
- Limb Ischemia VascularDocument6 pagesLimb Ischemia Vascularalbadrimohammed1997No ratings yet
- Vasculitis: Disorder Vessels Pathology Presentation Test TX OtherDocument3 pagesVasculitis: Disorder Vessels Pathology Presentation Test TX OthermcwnotesNo ratings yet
- Clinical MedicineDocument18 pagesClinical MedicineRishikesh AsthanaNo ratings yet
- Chapter 36Document3 pagesChapter 36Samantha QuintoNo ratings yet
- Arterial Disease (Critical Limb Ischaemia)Document2 pagesArterial Disease (Critical Limb Ischaemia)dragtoss2No ratings yet
- Medicine Revision - Neurology TableDocument10 pagesMedicine Revision - Neurology TableUnomoshNo ratings yet
- Myocardial Infarction and StrokeDocument13 pagesMyocardial Infarction and StrokeSunghoonOnlyNo ratings yet
- Dr. Dioszeghy Peter MononeuropathiesDocument52 pagesDr. Dioszeghy Peter MononeuropathiesAhmad abu-dayyehNo ratings yet
- Peripheral Vascular DiseaseDocument7 pagesPeripheral Vascular DiseaseRosalinda PerigoNo ratings yet
- Arterial DiseaseDocument57 pagesArterial DiseaseYil MosNo ratings yet
- IV Surgery PDFDocument265 pagesIV Surgery PDFاللهم أصلح أمريNo ratings yet
- Peripheral Arterial DiseaseDocument5 pagesPeripheral Arterial Diseaseampogison08No ratings yet
- Defibrillation Is The Definitive Treatment For The Life-Threatening Cardiac ArrhythmiasDocument4 pagesDefibrillation Is The Definitive Treatment For The Life-Threatening Cardiac ArrhythmiasErika RiceNo ratings yet
- DRUG-STUDY-FORMAT-Binangonan Lakeview 2ndDocument2 pagesDRUG-STUDY-FORMAT-Binangonan Lakeview 2ndDianne UlandayNo ratings yet
- Regional Anaesthesia: Anna WelbournDocument49 pagesRegional Anaesthesia: Anna WelbournAnna Welbourn100% (1)
- RaDocument40 pagesRaMuhammad MakkiNo ratings yet
- Peripheral Arterial Occlusive DiseaseDocument6 pagesPeripheral Arterial Occlusive DiseaseAila HinlogNo ratings yet
- Myasthenia Gravis: MG-epidemiologyDocument3 pagesMyasthenia Gravis: MG-epidemiologyRemigius RiyanNo ratings yet
- Atherosclerosis Angina Pectoris Myocardial InfarctionDocument2 pagesAtherosclerosis Angina Pectoris Myocardial InfarctionKaren Mae AlcantaraNo ratings yet
- Peripheral Arterial Occlusive DiseaseDocument43 pagesPeripheral Arterial Occlusive DiseaseadystiNo ratings yet
- Vascular Note by Joel ArudchelvamDocument52 pagesVascular Note by Joel ArudchelvamJoel Arudchelvam100% (1)
- Stroke CVDDocument9 pagesStroke CVDangel.senido0198No ratings yet
- IM Part 1Document48 pagesIM Part 1sasghfdgNo ratings yet
- IM Part 1 and 2 CombinedDocument100 pagesIM Part 1 and 2 CombinedsasghfdgNo ratings yet
- 2 Hemiplegia TIAs 452Document30 pages2 Hemiplegia TIAs 452vmj8tyh5dsNo ratings yet
- Acute Limb Ischemia Vs Critical Limb Ischemia: Clinical PracticeDocument51 pagesAcute Limb Ischemia Vs Critical Limb Ischemia: Clinical PracticedrhendyjuniorNo ratings yet
- RheumatologyDocument21 pagesRheumatologyApsaraNo ratings yet
- Simposium Papdi 3-Hari 1-5. Ws 1 - Dr. Lita-Untuk Share-2. Dr. LitaDocument46 pagesSimposium Papdi 3-Hari 1-5. Ws 1 - Dr. Lita-Untuk Share-2. Dr. LitaRangga Alam VaneoNo ratings yet
- Disease/syndrome Inciting Incident Structures Affected PoliomyelitisDocument12 pagesDisease/syndrome Inciting Incident Structures Affected PoliomyelitismrhemmatNo ratings yet
- Room #106 DSDocument2 pagesRoom #106 DSALYSSA GAILE ESPIRITUNo ratings yet
- Seminar-Quadripplegia, Paraplegia, MNDDocument107 pagesSeminar-Quadripplegia, Paraplegia, MNDSalsabila Al-BasheerNo ratings yet
- ShitDocument15 pagesShitEden Marie FranciscoNo ratings yet
- Medurg MidtermDocument4 pagesMedurg Midtermmark OrpillaNo ratings yet
- Sports MedicineDocument32 pagesSports Medicinersimranjit100% (1)
- 2 Cardio Lecture PDFDocument9 pages2 Cardio Lecture PDFNadia AbdurasidNo ratings yet
- FIX Leg UlcerDocument59 pagesFIX Leg UlcerDekka Andra100% (2)
- Cardio My Opa Thies ChartDocument2 pagesCardio My Opa Thies ChartSolomon Seth SallforsNo ratings yet
- Nesiritide2Document2 pagesNesiritide2Christine Pialan SalimbagatNo ratings yet
- Q1.Flaccid Paresis: Diagnostical VariantsDocument47 pagesQ1.Flaccid Paresis: Diagnostical VariantsNelson OduorNo ratings yet
- Proximal Femur Fractures: Sulita Turaganiwai s130364Document26 pagesProximal Femur Fractures: Sulita Turaganiwai s130364Wālē NandNo ratings yet
- Rheuma (Gout, CPD, Rheumatoid Arthritis, Osteoarthritis)Document2 pagesRheuma (Gout, CPD, Rheumatoid Arthritis, Osteoarthritis)Jezreel Yanah De LeonNo ratings yet
- Med Surg BundleDocument82 pagesMed Surg BundleThe Treasure ChestNo ratings yet
- Chronic Limb Ischemia: Prof. Dr. A.B.Singh UnitDocument59 pagesChronic Limb Ischemia: Prof. Dr. A.B.Singh UnitDr. Saad SiddiquiNo ratings yet
- Chapter 41 - Tingling and NumbnessDocument7 pagesChapter 41 - Tingling and NumbnessJonalyn MejellanoNo ratings yet
- Modern Anaesthesia:: A Concise Guide to the Study and Practice of Anaesthesia.From EverandModern Anaesthesia:: A Concise Guide to the Study and Practice of Anaesthesia.No ratings yet
- Article in Press: Age-Related Hair Changes in Men: Mechanisms and Management of Alopecia and GrayingDocument5 pagesArticle in Press: Age-Related Hair Changes in Men: Mechanisms and Management of Alopecia and Grayingpasid harlisaNo ratings yet
- The Aftereffects of Dynamic Exercise On Ambulatory Blood PressureDocument7 pagesThe Aftereffects of Dynamic Exercise On Ambulatory Blood PressureTAINAH DE PAULANo ratings yet
- MWS 130S, MWS 140S MWS 330B, MWS 330S, MWS 340B, MWS 430S: Welcome To The Family. Let's Get StartedDocument56 pagesMWS 130S, MWS 140S MWS 330B, MWS 330S, MWS 340B, MWS 430S: Welcome To The Family. Let's Get StartedMirjana PrekovicNo ratings yet
- Vitamina DDocument57 pagesVitamina DGabriel HerreraNo ratings yet
- PAMA NursingCaseStudy Revised PDFDocument77 pagesPAMA NursingCaseStudy Revised PDFJeofy PamaNo ratings yet
- Yds Kamp Gã N 1 Yds Eyds Kelime Sorularä 18 02 2022Document5 pagesYds Kamp Gã N 1 Yds Eyds Kelime Sorularä 18 02 2022Alihan GökNo ratings yet
- Nepal Health Professional Council: Syllabus For Professional Licensing Examination of Grade A-Diagnostic Health LabDocument10 pagesNepal Health Professional Council: Syllabus For Professional Licensing Examination of Grade A-Diagnostic Health LabBhageshwar ChaudharyNo ratings yet
- Eye & EarDocument27 pagesEye & EarZamzam IsmailNo ratings yet
- Adesola Tolulope Akanmu Final ProjectDocument104 pagesAdesola Tolulope Akanmu Final Projectajuguisrael6No ratings yet
- Eight Principles For Patient-Centred and Family-Centred Care For Newborns in The Neonatal Intensive Care UnitDocument5 pagesEight Principles For Patient-Centred and Family-Centred Care For Newborns in The Neonatal Intensive Care UnitPaola RoigNo ratings yet
- MiorelDocument1 pageMiorelApostolos T.No ratings yet
- 13 Vassileva Pediatric DRLDocument57 pages13 Vassileva Pediatric DRLLavinia BaracNo ratings yet
- Blood Vessel Detection From Retinal Fundas ImagesDocument10 pagesBlood Vessel Detection From Retinal Fundas ImagesNaoufal NaoufalNo ratings yet
- Electroencephalography (EEG) in The Diagnosis of Seizures and Epilepsy - UpToDate PDFDocument37 pagesElectroencephalography (EEG) in The Diagnosis of Seizures and Epilepsy - UpToDate PDFRobert MîndreanuNo ratings yet
- Nursingcrib Com NURSING CARE PLAN Hepatitis A PDFDocument2 pagesNursingcrib Com NURSING CARE PLAN Hepatitis A PDFswapnilazarusNo ratings yet
- Imaging For Neuro-Ophthalmic and Orbital Disease - A ReviewDocument24 pagesImaging For Neuro-Ophthalmic and Orbital Disease - A ReviewMashhoor AlfayezNo ratings yet
- Theories of Ageing: DR Prema BalusamyDocument19 pagesTheories of Ageing: DR Prema Balusamyprema balusamyNo ratings yet
- Free Download Jim Hanvey Detective Octavus Roy Cohen Full Chapter PDFDocument51 pagesFree Download Jim Hanvey Detective Octavus Roy Cohen Full Chapter PDFbarbara.johnson937100% (20)
- PathologyDocument32 pagesPathologyShashanka PoudelNo ratings yet
- Vitamin B6 Deficiency: Brown MJ, Ameer MA, Beier KDocument9 pagesVitamin B6 Deficiency: Brown MJ, Ameer MA, Beier Knadin nNo ratings yet
- Ilovepdf MergedDocument503 pagesIlovepdf MergedRitika NigamNo ratings yet
- Oxygen Therapy Powerpoint - Jan 2016 Student ViewDocument47 pagesOxygen Therapy Powerpoint - Jan 2016 Student ViewMark Anthony AlcantaraNo ratings yet
- ACL Injury: DR Keith HoltDocument14 pagesACL Injury: DR Keith HoltAnum TahirNo ratings yet
- Myofunctional Orthodontics and Myofunctional TherapyDocument1 pageMyofunctional Orthodontics and Myofunctional TherapysirahNo ratings yet
- Waht-Nur-065 V7Document25 pagesWaht-Nur-065 V7Else FashiosNo ratings yet
- Nursing Documentation - Frameworks and Barriers PDFDocument10 pagesNursing Documentation - Frameworks and Barriers PDFDany Marin RNo ratings yet
- Parent Ver SCH 0 6yrsDocument2 pagesParent Ver SCH 0 6yrsSrinivasamurthy KamarthiNo ratings yet
- Aditya Birla Sun Life Insurance Life Shield PlanDocument12 pagesAditya Birla Sun Life Insurance Life Shield PlanRitesh AgrawalNo ratings yet
- Table of Content: Risk AssesmentDocument25 pagesTable of Content: Risk AssesmentvijayNo ratings yet