Professional Documents
Culture Documents
Hiperbilirrubinemia Directa
Hiperbilirrubinemia Directa
Uploaded by
Ronal Cadillo MedinaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hiperbilirrubinemia Directa
Hiperbilirrubinemia Directa
Uploaded by
Ronal Cadillo MedinaCopyright:
Available Formats
Article
gastroenterology
Conjugated Hyperbilirubinemia:
Screening and Treatment in Older Infants and Children
Rula Harb, MD,* Daniel W. Thomas, MD
Objectives
After completing this article, readers should be able to:
Author Disclosure Drs Harb and Thomas did not disclose any nancial relationships relevant to this article.
1. Describe the metabolism of bilirubin. 2. Evaluate a child of any age who has conjugated hyperbilirubinemia. 3. Recognize the signs and symptoms of Wilson disease.
Introduction
Jaundice refers to yellow discoloration of the skin, sclera, mucous membranes, and body uids. It is a common problem that can be the presenting sign for many disorders. The challenge for the physician is to identify patients who need additional evaluation. The differential diagnosis for jaundice is age-specic; this review addresses the causative conditions in infants beyond the newborn period, older children, and adolescents. Jaundice is caused by elevated serum bilirubin concentrations. It is apparent in infants when the serum bilirubin value is greater than 4 to 5 mg/dL (68.4 to 85.5 mcmol/L) and in older children at values greater than 2 to 3 mg/dL (34.2 to 51.3 mmol/L). Serum total bilirubin is measured in the laboratory as the sum of two components: unconjugated (indirect) and conjugated (direct) fractions. The terms direct and conjugated hyperbilirubinemia often are used interchangeably. However, this usage is not always accurate because direct bilirubin may include both the conjugated fraction and bilirubin bound to albumin (delta bilirubin). Delta bilirubin is formed by covalent bonding between conjugated bilirubin in the serum and albumin; it is metabolized with albumin and has a similar half-life of 21 days. The presence of delta bilirubin often prolongs direct hyperbilirubinemia while results of the other liver tests are normalizing. Many hospitals continue to measure direct bilirubin by a method that includes both direct and delta bilirubin. Clinicians should consider asking for a breakdown of the direct bilirubin fraction if the jaundice is prolonged or presenting atypically. Conjugated hyperbilirubinemia is dened as a conjugated bilirubin concentration greater than 2 mg/dL (34.2 mmol/L) or more than 20% of total bilirubin. It is the biochemical marker of cholestasis used most commonly and dened as perturbation of bile ow. Although jaundice is seen commonly in newborns who have physiologic jaundice, breastfeeding and breast milk jaundice, red blood cell defects, and hemolysis, these are conditions of unconjugated (indirect) hyperbilirubinemia. Causes of unconjugated hyperbilirubinemia in the older infant/child are not reviewed in this article. Conjugated hyperbilirubinemia is less common, affecting approximately 1 in 2,500 infants. This condition is never normal at any age, and distinguishing cholestasis from noncholestatic causes of jaundice is crucial. Prolonged hyperbilirubinemia of greater than 2 to 3 weeks duration requires additional investigation.
Bilirubin Metabolism
The liver has many functions, many of which depend on its ability to secrete bile. Bile secretion is the method by which the liver excretes toxins, modulates cholesterol metabolism, and aids in the intestinal digestion and absorption of lipids and fat-soluble vitamins. Bile is composed of water, bile acids (cholic and chenodeoxycholic acids), phospholipids, cholesterol, bile pigment (bilirubin), electrolytes, xenobiotics, and metabolized drugs. Impairment of bile ow or secretion by the liver results in backup
*Childrens Hospital of Los Angeles, Los Angeles, Calif. Editorial Board. Pediatrics in Review Vol.28 No.3 March 2007 83
gastroenterology
conjugated hyperbilirubinemia
come signicant in cases of bowel obstruction, where relatively more bilirubin is deconjugated and absorbed, thereby increasing serum bilirubin concentrations and worsening jaundice.
Jaundice in the Infant
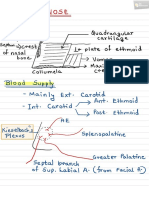
Prolonged jaundice in the infant (lasting beyond 2 to 3 weeks after birth) is abnormal and requires additional investigation. It is paramount to fractionate the bilirubin in infants who have abnormal or Figure 1. Bilirubin production in the reticuloendothelial system. RBC red blood cell prolonged jaundice to identify those who have conjugated hyperof its constituents within the liver canaliculi and hepabilirubinemia and recognize the disorders that may be tocytes, ultimately creating cholestatic damage to the amenable to early medical intervention (eg, galacliver. tosemia, urinary tract infection) or surgery (eg, biliary Bilirubin is the product of heme breakdown in the atresia, choledochal cyst). In addition, early diagnosis reticuloendothelial cells of the spleen and liver (Fig. 1). facilitates the institution of necessary nutritional and The end product of this metabolic pathway is watermedical support to promote optimal growth and develinsoluble unconjugated bilirubin, which is bound to opment. albumin in the circulation. Unconjugated bilirubin is The causes of cholestatic jaundice in the infant vary taken up and metabolized in the liver to conjugated and can be divided into two primary categories: obstrucbilirubin (Fig. 2). Conjugated bilirubin is secreted into tive and hepatocellular. A detailed classication is listed the biliary system by a specic transporter. Defects in in Table 1. The four most common causes of persistent bilirubin conjugation cause unconjugated hyperbilirucholestatic jaundice in infants are discussed. binemia (Gilbert syndrome and Crigler-Najjar syndromes I and II). Hepatocellular disease can cause a Extrahepatic Biliary Atresia (EHBA) mixed unconjugated and conjugated hyperbilirubinemia EHBA is the most common and serious cause of produe to both impaired bilirubin conjugation and canaliclonged cholestatic jaundice in infants. It results from a ular excretion. Defects in conjugated bilirubin excretion progressive and destructive inammatory process that cause isolated conjugated hyperbilirubinemia without affects both the extra- and intrahepatic biliary tree. The cholestasis (Rotor and Dubin-Johnson syndromes). cause of EHBA has not been identied clearly. Two Other mutations in membrane transporters of other orclinical forms have been dened: an embryonic/fetal ganic anions, such as bile acids, are linked with several form, which constitutes 20% of cases, and a perinatal/ diseases, including cystic brosis, adrenoleukodystrophy, acquired type, which comprises the remaining 80% of and the familial intrahepatic cholestasis syndromes. cases. (1) The embryonic type has an earlier onset, has no Once bile is excreted from the liver, it is stored in the jaundice-free interval, and is associated with other nongallbladder until a meal activates duodenal cholecystokihepatic anomalies or syndromic features, such as isolated nin release and expulsion of gallbladder contents into the cardiovascular and gastrointestinal anomalies (intestinal intestine. Conjugated bilirubin cannot be reabsorbed by malrotation, preduodenal portal vein, abdominal situs intestinal epithelial cells and is degraded by intestinal inversus) and splenic anomalies (polysplenia, asplenia). ora into stercobilin and urobilinogen, which are exThe acquired type is not associated with other congenital creted into stool. A small portion of conjugated bilirubin anomalies, usually occurs in an otherwise healthy term is deconjugated by intestinal beta-glucuronidase. The infant, and has a jaundice-free interval followed by the unconjugated bilirubin can be reabsorbed into the circudevelopment of jaundice in the rst few postnatal weeks. lation and returned to the liver, which is known as Both forms share the cardinal features of cholestatic enterohepatic bilirubin circulation. The amount of bilijaundice, hepatomegaly, and acholic stools. rubin reabsorbed normally is very small, but it can beEHBA was universally fatal before the Kasai hepato84 Pediatrics in Review Vol.28 No.3 March 2007
gastroenterology
conjugated hyperbilirubinemia
Figure 2. Bilirubin conjugation. Movement of bilirubin (B) from the circulation into the hepatocyte occurs at the hepatocyte basolateral membrane with the help of a membrane carrier protein. Binding of B to glutathione-S-transferase (GST) facilitates movement into the rough endoplasmic reticulum (RER), where conjugation with glucuronic acid (GA) is enabled by bilirubin ceridine diphosphate glucuronosyl transferase 1A1 (UGT1A1). The conjugated bilirubin is excreted into bile at the hepatocyte canalicular membrane through a process mediated by the membrane-bound transporter cMOAT (canalicular multispecic organic anion transporter). Alb albumin, cytosol the uid within a cell that contains the cells oranelles, B-GA conjugated bilirubin (mono- and di-glucuronides). Adapted from Gourley GR. Bilirubin metabolism. In: Walker WA, Goulet OJ, Kleinman RE, et al, eds. Pediatric Gastrointestinal Disease: Pathophysiology, Diagnosis, Management. 4th ed. Hamilton, Ontario, Canada: BC Decker, Inc; 2004:1344 1362.
rence has decreased as specic disorders that cause a similar clinical and histologic picture have been identied (eg, alpha-1-antitrypsin deciency, defective bile acid synthesis and transport). The diagnosis is made in infants who have prolonged cholestatic jaundice and typical biopsy ndings of disrupted hepatic architecture, multinucleated giant hepatocytes, focal hepatocyte necrosis, expansion of portal triads with inammatory inltrate, and extramedullary hematopoiesis in addition to the absence of another disorder. Electron microscopy often is useful in diagnosis. The prognosis of idiopathic hepatitis is variable and depends on whether a metabolic or infectious cause ultimately is diagnosed. Jaundice usually resolves by 3 to 4 months of age; persistence of jaundice beyond this age warrants additional evaluation.
Alagille Syndrome (AGS)
portoenterostomy was introduced by Dr Morio Kasai in 1959. This procedure establishes bile ow in up to 80% of patients if performed prior to 60 days after birth. The success rate decreases as the infants age increases, with bile ow established in up to 45% of infants 60 to 90 days of age and 10% of infants 90 to 120 days of age. (1) These results underscore the importance of diagnosing this condition early. Approximately one third of patients require liver transplant in the rst postnatal year, one third require it in their teens, and one third live with some liver function after the Kasai procedure into adulthood. (1) It is estimated that approximately 50% of patients who have good results from the initial Kasai surgery still become transplant candidates later in life.
Idiopathic Neonatal Hepatitis
Idiopathic neonatal hepatitis, also known as giant cell hepatitis, used to be considered the most common cause of neonatal cholestasis. However, its relative occur-
AGS also is known as syndromic bile duct paucity or arteriohepatic dysplasia. It is an autosomally dominant inherited with low penetrance disorder of bile duct paucity that occurs in conjunction with syndromic extrahepatic ndings. The defect in AGS is a mutation of the Jagged 1 (JAG1) gene, which is mapped to chromosome 20p12 and encodes a ligand for the Notch signaling pathway, which is important in cell fate determination. The diagnosis can be made in the patient who has a marked reduction of intrahepatic bile ducts on liver biopsy in association with other cardiac, ocular, skeletal, and facial abnormalities. The bile duct paucity may not be apparent in early infancy. AGS usually presents in the rst 3 postnatal months and must be distinguished from biliary atresia and other causes of nonsyndromic paucity. It may be diagnosed in older children who have persistent cholestatic jaundice and in adults after diagnosis in a related child. In the original series described by Alagille in 1975, (2) 15 of 30 patients who had cholestatic jaundice and hepatic ductular hypoplasia with intact extrahepatic bile
Pediatrics in Review Vol.28 No.3 March 2007 85
gastroenterology
conjugated hyperbilirubinemia
Differential Diagnosis of Cholestatic Jaundice in the Infant
Table 1.
Obstructive
Extrahepatic biliary atresia Choledochal cyst Spontaneous perforation of the bile duct Inspissated bile Mass: stone, tumor
Hepatocellular
Idiopathic neonatal hepatitis Disorders of the intrahepatic bile ducts Alagille syndrome (arteriohepatic dysplasia/syndromic paucity of the intrahepatic bile ducts) Nonsyndromic paucity of the intrahepatic bile ducts Congenital hepatic brosis with bile duct cysts (Caroli disease) Metabolic disorders Disorders of amino acid metabolism Tyrosinemia Disorders of lipid metabolism Gaucher disease Niemann-Pick disease Cholesterol ester storage disease (Wolman syndrome) Disorders of carbohydrate metabolism Galactosemia Hereditary fructose intolerance Glycogen storage disease Disorders of bile acid metabolism and transport excretion Zellweger syndrome and other disorders of peroxisomal metabolism Disorders of bilirubin transport (do not cause cholestatic liver injury) Dubin-Johnson syndrome Rotor syndrome Mitochondrial disorders Alpha-1-antitrypsin deciency Cystic brosis Neonatal iron storage disease Endocrine disorders Hypothyroidism Hypopituitarism and septo-optic dysplasia Infectious Sepsis (urinary tract infection, endotoxemia, enterocolitis) TORCH infections (toxoplasmosis, cytomegalovirus, herpesvirus, rubella, syphilis) Hepatitis B, non-typeable hepatitis Human immunodeciency virus Drugs and Toxins Total parenteral nutrition Medications Fetal alcohol syndrome Other Vascular anomalies Budd-Chiari syndrome Hepatoendothelioma/hemangioma Cardiac insufciency and hypoperfusion Chromosomal abnormalities Trisomy 21 Trisomy 18
ducts had other common features. These included a characteristic facies (prominent forehead, deep-set eyes with mild hypertelorism, straight nose, and small, pointed chin), a systolic murmur caused by peripheral pulmonic stenosis, vertebral arch defects, growth retardation, mild-to-moderate mental retardation, and hypogonadism in boys. Emerick and associates (3) studied 92 patients who had AGS and found cholestasis in 96%, bile duct paucity in 85%, cardiac murmur in 97%, vertebral anomalies in 51%, characteristic facies in 96%, eye ndings (posterior embryotoxon) in 78%, and renal anomalies in 40%. Minor features included growth retardation (87%), mental retardation (2%), developmental delay (16%), and pancreatic insufciency (41%). Alagille and colleagues (4) have recommended that the diagnosis be made by conrming the existence of cholestasis and two of the other four abnormalities. Factors that contribute signicantly to mortality in AGS include cardiac disease (other cardiac defects besides peripheral pulmonic stenosis such as tetralogy of Fallot), intracranial hemorrhage, and progressive liver disease.
Alpha-1-Antitrypsin Deciency
Alpha-1-antitrypsin is a member of the serine protease inhibitor family (the serpins) that protects the connective tissue from degradation by inhibition of neutrophil elastase, cathepsin G, and proteinase 3. Although lung disease associated with alpha-1-antitrypsin deciency is attributed to markedly reduced concentrations, liver disease results from retention of the abnormally folded protein in the endoplasmic reticulum (ER) of the hepatocyte (the site of synthesis of most alpha-
86 Pediatrics in Review Vol.28 No.3 March 2007
gastroenterology
conjugated hyperbilirubinemia
1-antitrypsin). Alpha-1-antitrypsin is a polymorphic protein that has allelic variants dened by isoelectric focusing of the plasma and classied according to the protease inhibitor (Pi) phenotype. Structural variants that have normal plasma concentrations or functional activity are known as PiM alpha-1-antitrypsin. Variants in which alpha-1-antitrypsin is not detected are known as null allelic variants and when inherited with another null variant, are associated with early development of emphysema but no liver disease. Variants that have reduced alpha-1-antitrypsin activity include the PiZ and PiS. The PiZ homozygote is the condition associated most commonly with liver and lung disease. Alpha-1-antitrypsin deciency is the most common genetic cause of acute and chronic liver disease in chil-
Alpha-1- antitrypsinofdeciency ischronic the most common genetic cause acute and
liver disease in children.
dren and the most common genetically caused disorder necessitating liver transplantation in children. Presentation of liver disease in ZZ homozygotes is variable. In a review of 44 patients, Volpert and colleagues (5) reported that the age of diagnosis of alpha-1-antitrypsin deciency-associated liver disease was younger than 1 month in 10 patients, 1 month to 1 year in 21 patients, and older than 1 year in 13 patients. One of every 10 patients has prolonged jaundice in infancy, and 1 of 100 develops cirrhosis and requires transplantation. (6) Other clinical presentations include neonatal hepatitis syndrome, mild elevation of transaminase values in the toddler, portal hypertension and cirrhosis in the child or adolescent, chronic hepatitis in the adult, and hepatocellular carcinoma in the adult. Diagnosis is made by demonstrating an abnormal Pi phenotype (PiZZ) and periodic acid-Schiff-positive, diastase-resistant globules in the ER of hepatocytes.
Conjugated hyperbilirubinemia results from obstructive or hepatocellular causes. Biliary stones and sludge can obstruct the common bile duct and cause subsequent jaundice. Other causes of obstructive jaundice in this age group include parasitic infestations (ascaris, liver ukes), primary sclerosing cholangitis, choledochal cyst, and tumors. Hepatocellular causes of conjugated hyperbilirubinemia, such as viral or medication-related hepatitis, can result in jaundice. Clinically apparent liver disease from chronic hepatitis B infection has decreased markedly due to the effective implementation of the vaccine for this disorder. Signs of active hepatitis C usually occur in adults and are not discussed in detail in this article. Wilson disease and autoimmune hepatitis are relatively uncommon causes of hyperbilirubinemia but are two important entities for the pediatrician to recognize early because treatment that may prevent progression is available. Other hepatocellular disorders are detailed in Table 2.
Wilson Disease
Wilson disease is an autosomal recessive disorder of copper homeostasis. The affected gene is on chromosome 13 and encodes a highly conserved copper-transporting P-type adenosine triphosphatase (ATP7b) that excretes copper into bile. Copper is an essential trace element that participates in cellular respiration, iron oxidation, pigment formation, and antioxidant defense. It is absorbed from copper-rich foods from the stomach and duodenum, bound to ceruloplasmin in the circulation, and excreted by the liver into bile. The prevalence of Wilson disease is 1 in 30,000 and is equal among all ethnic groups. The condition presents in most patients as either hepatic or central nervous system involvement. Liver disease occurs at an average age of 10 to 13 years in 45% of patients and rarely is seen before 3 years of age. Some 35% of patients present with neurologic signs (tremor, rigidity, dysarthria) a decade older than patients who have hepatic involvement; 10% present with psychiatric disturbances (depression, new-onset school problems, impulsive behavior); and 10% present with other manifestations, including hemolytic anemia, Fanconi syndrome (glycosuria, aminoaciduria), and cardiomyopathy. Thus, patients who have Wilson disease can have a mixed conjugated and unconjugated hyperbilirubinemia, depending on which disease manifestations are present.
Pediatrics in Review Vol.28 No.3 March 2007 87
Jaundice in the Older Child/Adolescent
New-onset cholestatic jaundice in the older child and adolescent always requires additional investigation. It is essential to fractionate the bilirubin to differentiate cholestatic jaundice from unconjugated hyperbilirubinemia due to hemolysis or defective bilirubin conjugation, as occurs in Gilbert syndrome.
gastroenterology
conjugated hyperbilirubinemia
Table 2.
Differential Diagnosis of Cholestatic Jaundice in the Older Child and Adolescent
Choledochal cyst Mass: stone, tumor, parasite
Obstructive
Hepatocellular
Autoimmune Autoimmune hepatitis Primary sclerosing cholangitis Primary biliary cirrhosis Disorders of the intrahepatic bile ducts Alagille syndrome (arteriohepatic dysplasia/ syndromic paucity of the intrahepatic bile ducts) Nonsyndromic paucity of the intrahepatic bile ducts Congenital hepatic brosis/Caroli disease Metabolic disorders Wilson Disease Disorders of bilirubin transport Dubin-Johnson syndrome Rotor syndrome Mitochondrial disorders Alpha-1-antitrypsin deciency Cystic brosis Hemochromatosis Endocrine disorders Hypothyroidism Infectious Sepsis (endotoxemia, enterocolitis) Hepatitis A, B, C, E, non-typeable hepatitis Human immunodeciency virus Drugs and toxins Total parenteral nutrition Medications Other Vascular anomalies Budd-Chiari syndrome Hemangioma Cardiac insufciency and hypoperfusion Chromosomal abnormalities Trisomy 21
basal ganglia and include parkinsonian symptoms. KF rings often are present in patients who have neurologic symptoms, but may be absent in patients who have liver disease. Wilson disease is diagnosed in the patient who has signs and symptoms consistent with the disease in addition to laboratory ndings of impaired hepatic copper metabolism. The serum ceruloplasmin concentration is decreased because copper is not conjugated to the apoceruloplasmin synthesized by the hepatocyte. The unconjugated apoceruloplasmin is degraded rapidly. Measurement of urinary copper in a 24-hour collection is increased. A liver biopsy quantitating hepatic copper content is a helpful diagnostic tool, and a liver that has normal copper content excludes the diagnosis. A slitlamp examination can be performed to evaluate for KF rings. Denitive genetic testing is now available for Wilson disease. Therapy is geared toward attaining and maintaining normal copper homeostasis. Oral D-penicillamine and trientine are copper chelators. Zinc acetate prevents the absorption of copper from the gastrointestinal tract. Patients are counseled to avoid copper-rich foods such as shellsh, legumes, nuts, chocolate, and liver. Liver transplantation is the treatment of choice for selected patients who have either advanced liver disease or fulminant liver failure.
Autoimmune Hepatitis (AIH)
AIH is an inammatory hepatitis characterized by the development of pathologic autoantibodies to normal host proteins and a dense mononuclear inltrate in the portal tracts in the absence of another cause. AIH can be subdivided into two general categories classied by the type of autoantibodies produced: anti-nuclear antibody/ anti-smooth muscle antibody (ANA/SMA) AIH, and anti-liver kidney microsomal antibody 1 (LKM1) AIH. In a study of 52 patients who had AIH, investigators found that the median age at presentation of ANA/SMA AIH was 10.5 years and that for LKM1 AIH was 7.4 years. (7) Some 75% of patients were female. Three patterns of presentation were noted: 1) Acute hepatitis was the pattern in most patients having both types, with nausea, vomiting, anorexia, fatigue, and abdominal pain, followed by jaundice, dark urine, and pale stools. Duration of illness varied from 2 weeks to 2 months in this group. 2) Another group (30%) had the insidious onset of disease of longer duration (6 mo to 2 yr), with relapsing jaundice, progressive fatigue, headache, anorexia, and weight loss.
Hepatic involvement ranges from asymptomatic transaminitis to acute liver failure with jaundice, cirrhosis, hepatic necrosis, and encephalopathy. Liver biopsy can show nonspecic ndings of steatosis and glycogen deposition. Micronodular cirrhosis and piecemeal necrosis also can be seen. Kaiser-Fleischer (KF) rings, representing copper deposition in Descemets membrane, are visible on a slitlamp examination of the eye. Neurologic symptoms are attributed to copper deposition in the
88 Pediatrics in Review Vol.28 No.3 March 2007
gastroenterology
conjugated hyperbilirubinemia
3) A small percent of patients, who had no prior history of jaundice, had complications of portal hypertension. AIH is suspected on the basis of clinical characteristics and demonstration of the autoantibodies, as well as an elevated immunoglobulin G value. Denitive diagnosis is made on liver biopsy, where the typical histologic picture is a dense mononuclear inltrate invading the hepatic parenchyma (periportal hepatitis), with periportal necrosis. In most cases, the disease responds well to immunosuppressive therapy. Urgent liver transplantation is indicated if the patient presents in acute fulminant hepatic failure.
biliary atresia, choledochal cyst, or gallstone disease. Additionally, the birth and perinatal histories, past medical and surgical histories, family history (including consanguinity), medication and dietary histories, social activity and school performance histories, and travel history should be sought.
Physical Examination
The clinician should note if the patient is well- or illappearing as well as irritable or drowsy. Both signs may indicate encephalopathy, infection, or metabolic derangement. Microcephaly in the infant may indicate congenital infection. Recognition of dysmorphism is valuable. Eyes should be examined for posterior embryotoxon or KF rings. The systolic murmur of peripheral pulmonic stenosis, usually heard in the back as well as the front, suggests AGS. Hepatomegaly typically is present, but a small liver may indicate cirrhosis and end-stage liver disease. Splenomegaly, ascites, and prominent vasculature such as caput medusa suggest portal hypertension and chronic liver disease. An infants diaper should be examined for pale stools and dark urine. Neurologic evaluation should be undertaken for ataxia and asterixis.
Evaluation of the Jaundiced Patient
Although jaundice is relatively common in the rst 2 weeks after birth and is observed frequently in newborns, jaundice in the older infant and child always is abnormal and requires more investigation. Additional evaluation of children who have conjugated hyperbiliru-
The keyjaundice is fractionation of when laboratory test to obtain evaluating the
bilirubin.
binemia and chronic liver disease should involve looking for the complications of cholestasis, such as coagulopathy, fat malabsorption, ascites, and encephalopathy, to initiate appropriate therapy. Finally, a child who has conjugated hyperbilirubinemia or evidence of chronic liver disease should be referred to a pediatric gastroenterologist.
Laboratory Tests
The key laboratory test to obtain when evaluating jaundice is fractionation of the bilirubin. Indirect or unconjugated hyperbilirubinemia usually indicates excessive red blood cell destruction at any age. Direct or conjugated hyperbilirubinemia indicates a hepatobiliary disorder. Hepatic transaminase concentrations are elevated in the presence of hepatocellular injury. The alkaline phosphatase and gamma glutamyl transferase values often are increased with obstructive conditions. Liver function, including prothrombin time, albumin, and cholesterol, should be measured. The remainder of the evaluation should be tailored to the specic patient. Hemolytic anemia can be seen in patients who have Wilson disease. Thyroid function tests can be obtained if hypothyroidism is suspected. Other age-specic tests may be considered, including TORCH (toxoplasmosis, rubella, cytomegalovirus, herpes simplex) titers, blood and urine cultures, alpha-1-antitrypsin Pi phenotype, iron prole, chloride sweat test, urine-reducing substances (galactosemia), and a metabolic screen in young infants. Testing for Wilson disease (ceruloplasmin) or for AIH is appropriate in older children.
Pediatrics in Review Vol.28 No.3 March 2007 89
History
The age of the patient and history of presentation give important clues to the cause of the jaundice. Some conditions of infantile cholestasis and conjugated hyperbilirubinemia present early in life, such as biliary atresia, AGS, and inherited metabolic disorders. Others often manifest beyond infancy, such as AIH and Wilson disease. Diseases such as cystic brosis and alpha-1antitrypsin deciency can present as either neonatal cholestasis or later in life as chronic liver disease. Signs such as poor feeding, irritability, and vomiting may be associated with a metabolic condition, such as galactosemia, or suggest encephalopathy. The presence of acholic stools suggests an obstructive process such as
gastroenterology
conjugated hyperbilirubinemia
Imaging
Real-time ultrasonography is an important diagnostic tool in the evaluation of the jaundiced patient. The absence of a gallbladder on a fasting examination in an infant is suggestive but not diagnostic of biliary atresia. Ultrasonography may demonstrate gallstones, choledochal cyst, or ascites. A Doppler ultrasonographic study of the portal circulation may identify portal hypertension or portal vein thrombosis. Hepatobiliary scintigraphy with technetium-labeled iminodiacetic acid analogs may help differentiate obstructive jaundice from nonobstructive causes. In the case of obstructive jaundice, the hepatic uptake of tracer is normal, but there is no intestinal excretion. In cases of severe hepatocellular disease, uptake into the liver is delayed, but tracer eventually is excreted into the intestine. Premedication with phenobarbital for 3 to 5 days prior to the study enhances biliary excretion and imaging of the isotope.
min concentrations with supplementation. Management of the complications of chronic liver disease and portal hypertension in conjunction with a pediatric gastroenterologist is essential. All children, particularly those who have chronic liver disease, should be immunized, including both hepatitis A and B, using the guidelines of the American Academy of Pediatrics. It is appropriate to refer any child who evidences acute, severe liver disease or a chronic liver condition to a pediatric transplant center for evaluation.
References
1. Balistreri WF, Grand R, Hoofhagle JH, et al. Biliary atresia:
current concepts and research directions. Hepatology. 1996;23: 16821692 2. Alagille D, Odievre M, Gautier M, et al. Hepatic ductular ` hypoplasia associated with characteristic facies, vertebral malformations, retarded physical growth, mental and sexual development, and cardiac murmur. J Pediatr. 1975;86:6371 3. Emerick KM, Rand EB, Goldmuntz E, et al. Features of Alagille syndrome in 92 patients: frequency and relation to prognosis. Hepatology. 1999;29:822 829 4. Alagille D, Estrada A, Hadchouel M, et al. Syndromic paucity of interlobular bile ducts (Alagille syndrome or arteriohepatic dysplasia): review of 80 cases. J Pediatr. 1987;110:195200 5. Volpert D, Molleston JP, Perlmutter DH. Alpha-1-antitrypsin deciency-associated liver disease progresses slowly in some children. J Pediatr Gastroenterol Nutr. 2000;31:258 263 6. Carrell RW, Lomas DA. Alpha1-antitrypsin deciency: a model for conformational diseases. N Engl J Med. 2002;346:4553 7. Mieli-Vergani G, Vergani D. Immunological liver diseases in children. Semin Liver Dis. 1998;18:271279
Liver Biopsy
Ultimately, many patients require a liver biopsy for denitive and reliable diagnosis. The liver biopsy can be performed percutaneously, with or without ultrasonographic guidance, or surgically. In addition to evaluation by an experienced pathologist for specic histologic features, liver tissue can be used to quantify iron and copper content and for electron microscopy to detect certain metabolic conditions.
Management of Jaundice
Treatment is directed at the specic underlying disorder, although persistent cholestasis generally can cause retention of bile acids, bilirubin, and cholesterol; decreased excretion of bile acids into the intestine with resulting fat malabsorption; and hepatocellular damage that eventually causes portal hypertension and end-stage liver disease. Some general principles apply to the management of these consequences independent of the specic cause. These principles include optimizing nutrition by employing the use of medium-chain triglyceride-containing formula or supplements and monitoring fat-soluble vita-
Suggested Reading
Gitlin JD. Wilson disease. Gastroenterology. 2003;125:1868 1877 McLin VA, Balistreri WF. Approach to neonatal cholestasis. In: Walker WA, Goulet OJ, Kleinman RE, et al, eds. Pediatric Gastrointestinal Disease: Pathophysiology, Diagnosis, Management. 4th ed. Hamilton, Ontario, Canada: BC Decker Inc; 2004:1079 1091 Moyer V, Freese DK, Whitington PF, et al. Guideline for the evaluation of cholestatic jaundice in infants: recommendations of the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. J Pediatr Gastroenterol Nutr. 2004; 39:115128
90 Pediatrics in Review Vol.28 No.3 March 2007
gastroenterology
conjugated hyperbilirubinemia
PIR Quiz
Quiz also available online at www.pedsinreview.org. 1. Conjugated hyperbilirubinemia is: A. B. C. D. E. A marker of accelerated hemoglobin breakdown. A normal nding in otherwise healthy adolescents. Always linked with cholestasis. Less common than unconjugated hyperbilirubinemia. Synonymous with direct hyperbilirubinemia.
2. A 4-week-old breastfeeding boy is jaundiced and has a total bilirubin concentration of 13 mg/dL (222.3 mmol/L). The laboratory test that maximizes diagnostic efciency is: A. B. C. D. E. A complete blood count. A reticulocyte count. Bilirubin fractionation. Gamma glutamyl transferase. Hepatic transaminase.
3. A 4-week-old breastfeeding boy has become increasingly jaundiced. The pregnancy was unremarkable. Delivery was at term, and the infant was appropriate for gestational age. The jaundice was not noted in the hospital. Findings on the physical examination, other than jaundice, are unremarkable. Today, the total bilirubin concentration is 13 mg/dL (222.3 mmol/L), with a direct fraction of 6 mg/dL (102.6 mmol/L). Of the following, the condition that is most likely ruled out by these ndings is: A. B. C. D. E. Alagille syndrome. Alpha-1-antitrypsin deciency. Extrahepatic biliary atresia. Neonatal hepatitis. Physiologic jaundice.
4. A previously healthy 15-year-old girl develops jaundice and fatigue. She does not complain of colicky abdominal pain associated with meals. She has had no known exposure to hepatotoxins. Aside from jaundice and appearing mildly ill, ndings on her physical examination are unremarkable. Initial laboratory evaluation reveals a bilirubin concentration of 11 mg/dL (188.1 mmol/L) with a direct fraction of 4 mg/dL (68.4 mmol/L), and elevated hepatic transaminases, but no evidence of Epstein-Barr or hepatitis A, B, or C virus. As suspected from the history, ultrasonography reveals a normal gallbladder and biliary tree. Serum ceruloplasmin and autoantibody results are inconclusive. Pi typing reveals PiMM, and the patient proceeds to liver biopsy. Copper content of the sample is normal. Of the following, the patient is most likely to have: A. B. C. D. E. Alpha-1-antitrypsin deciency. Autoimmune hepatitis. Choledochal cyst. Gilbert syndrome. Wilson disease.
5. Wilson disease is diagnosed denitively through: A. B. C. D. E. Genetic testing. Liver biopsy. Serum ceruloplasmin concentrations. Slitlamp examination. Urinary copper excretion.
Pediatrics in Review Vol.28 No.3 March 2007 91
You might also like
- GMC Official PLAB 1 Question SampleDocument8 pagesGMC Official PLAB 1 Question Samplemuntaser100% (1)
- Conjugated Hyperbilirubinemia:: Screening and Treatment in Older Infants and ChildrenDocument11 pagesConjugated Hyperbilirubinemia:: Screening and Treatment in Older Infants and ChildrendjebrutNo ratings yet
- Peadiatrics Assignment - Mr. KangwaDocument11 pagesPeadiatrics Assignment - Mr. KangwaTahpehs PhiriNo ratings yet
- Jaundice - StatPearls - NCBI BookshelfDocument11 pagesJaundice - StatPearls - NCBI BookshelfCONSTANTIUS AUGUSTONo ratings yet
- JAUNDICE pptm-1Document29 pagesJAUNDICE pptm-1jismi vallachiraNo ratings yet
- Causes: Neonatal Jaundice or Neonatal Hyperbilirubinemia, or Neonatal Icterus (From The GreekDocument7 pagesCauses: Neonatal Jaundice or Neonatal Hyperbilirubinemia, or Neonatal Icterus (From The GreekIzzah100% (1)
- Pediatrics in Review33 (7) 291Document14 pagesPediatrics in Review33 (7) 291Barbara Helen Stanley100% (1)
- Assessment of Jaundice in The Hospitalized Patient PDFDocument16 pagesAssessment of Jaundice in The Hospitalized Patient PDFlaura canoNo ratings yet
- Consequences of Hyperbilirubinemia:: Kernicterus Is The Major Consequence of Neonatal Hyperbilirubinemia. Although It IsDocument3 pagesConsequences of Hyperbilirubinemia:: Kernicterus Is The Major Consequence of Neonatal Hyperbilirubinemia. Although It IsAradhanaRamchandaniNo ratings yet
- Neonatal JaundiceDocument12 pagesNeonatal JaundiceAlya Afifa100% (1)
- HyperbilirubinemiaDocument48 pagesHyperbilirubinemiaEdrik Luke Pialago100% (2)
- 8 BilirubinDocument25 pages8 BilirubinTagreed DerarNo ratings yet
- Neonatal JaundiceDocument12 pagesNeonatal JaundiceGiska T PutriNo ratings yet
- Neonatal JaundiceDocument77 pagesNeonatal Jaundiceodhiambovictor2424No ratings yet
- Neonatal CholestasisDocument13 pagesNeonatal Cholestasisgts999No ratings yet
- Clase 3 HepatogramaDocument9 pagesClase 3 HepatogramajuanpbagurNo ratings yet
- Difference Between Physiologic Jaundice and Pathologic JaundiceDocument2 pagesDifference Between Physiologic Jaundice and Pathologic JaundiceNurulAqilahZulkifli100% (4)
- Liver Function Test (TSB)Document25 pagesLiver Function Test (TSB)shafyd ramdanNo ratings yet
- Ictericia Diagnostico Ravindran2020Document7 pagesIctericia Diagnostico Ravindran2020Francisco CarpioNo ratings yet
- LP Anak HiperbilirubinDocument33 pagesLP Anak HiperbilirubinputudewiNo ratings yet
- Dissertation ON A Clinical Study On Obstructive JaundiceDocument66 pagesDissertation ON A Clinical Study On Obstructive JaundicePravat SatpathyNo ratings yet
- Core Concepts Bilirrubin MetabolismDocument9 pagesCore Concepts Bilirrubin MetabolismAngelina ChunNo ratings yet
- Jaundice EnglishDocument5 pagesJaundice EnglishArinaManaSikanaNo ratings yet
- Jaundice: Know AsDocument21 pagesJaundice: Know Asnitesh kotianNo ratings yet
- PPPPDocument6 pagesPPPPChristy Ada IjeomaNo ratings yet
- Pathogenesis and Etiology of Unconjugated Hyperbilirubinemia in The NewbornDocument45 pagesPathogenesis and Etiology of Unconjugated Hyperbilirubinemia in The NewbornJaner BanosNo ratings yet
- Neonatal Jaundice (Hyperbilirubinemia)Document20 pagesNeonatal Jaundice (Hyperbilirubinemia)fatimaabuhamda6No ratings yet
- 33 34 IV 12 Atresia BiliarisDocument13 pages33 34 IV 12 Atresia BiliarisTasia AmeliaNo ratings yet
- J Mpsur 2017 09 012Document7 pagesJ Mpsur 2017 09 012riffarsyad100% (1)
- 1 Core Concepts Bilirubin MetabolismDocument9 pages1 Core Concepts Bilirubin Metabolismlink0105No ratings yet
- Neonatal JaundiceDocument4 pagesNeonatal JaundiceChristian Eduard de DiosNo ratings yet
- Clinical Significance of Bilirubin in Liver Function TestsDocument24 pagesClinical Significance of Bilirubin in Liver Function TestsAbdulsalam JumaiNo ratings yet
- Uvod:: Total BilirubinDocument5 pagesUvod:: Total BilirubingrgicosNo ratings yet
- Physiological JaundiceDocument23 pagesPhysiological JaundiceNoor Shahirah AyubNo ratings yet
- Metabolisme Bilirubin Blok 11 2016Document22 pagesMetabolisme Bilirubin Blok 11 2016Astri Hardianti RahimNo ratings yet
- Jaundice: in Older Children and AdolescentsDocument10 pagesJaundice: in Older Children and AdolescentshectorNo ratings yet
- Bac GroundDocument6 pagesBac GroundRitu Ayu PutriNo ratings yet
- Jaundice in The Adult PatientDocument6 pagesJaundice in The Adult Patientrbatjun576No ratings yet
- Liver FunctionDocument30 pagesLiver FunctionAra ShirikaNo ratings yet
- Jaundice: in Older Children and AdolescentsDocument10 pagesJaundice: in Older Children and AdolescentsjoslinmtggmailcomNo ratings yet
- Neonatal JaundiceDocument48 pagesNeonatal JaundiceRemy MartinsNo ratings yet
- 2 Jaundice in The NBDocument33 pages2 Jaundice in The NBCheru DugaseNo ratings yet
- JaundiceDocument4 pagesJaundiceAbo Omar Ahmed100% (1)
- Liver PathologyDocument35 pagesLiver Pathologynhgwdwffp2No ratings yet
- Disease JaundiceDocument19 pagesDisease JaundiceMeena KoushalNo ratings yet
- BIOCHEM Jaundice FinalDocument54 pagesBIOCHEM Jaundice FinalJohnRobynDiezNo ratings yet
- Case StudiesDocument28 pagesCase StudiespeanantNo ratings yet
- Crs Hiperbilirubinemia EricDocument30 pagesCrs Hiperbilirubinemia Ericerix firmando100% (1)
- Neonatal JaundiceDocument24 pagesNeonatal JaundiceChetan SekhriNo ratings yet
- Approach To Neonatal JaundiceDocument36 pagesApproach To Neonatal JaundiceDrMubashir ShaikhNo ratings yet
- Refer atDocument28 pagesRefer atAngga NuralamNo ratings yet
- Neonatal Jaundice CmeDocument39 pagesNeonatal Jaundice CmeGideon K. Mutai100% (1)
- NEONATAL - JAUNDICE - Al SabbahDocument61 pagesNEONATAL - JAUNDICE - Al SabbahGidu SaidNo ratings yet
- IctericiaDocument19 pagesIctericiadavid pinedaNo ratings yet
- Core Concepts:: Bilirubin MetabolismDocument9 pagesCore Concepts:: Bilirubin MetabolismManasye AlanNo ratings yet
- Neonatal JaundiceDocument30 pagesNeonatal JaundiceAnonymous Y3fqBduNo ratings yet
- UNIT HyperbilirubinemiaDocument17 pagesUNIT Hyperbilirubinemiaurmila dewanNo ratings yet
- Neonatal Hyperbilirubinemia and JaundiceDocument8 pagesNeonatal Hyperbilirubinemia and JaundiceAndreea GeorgianaNo ratings yet
- Neonatal HyperbilirubinemiaDocument36 pagesNeonatal HyperbilirubinemiamahmmoudeltaweelNo ratings yet
- Chapter 4. JaundiceDocument29 pagesChapter 4. JaundiceShravan SharmaNo ratings yet
- Von Gierke Disease, (Glycogen Storage Disorder I) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandVon Gierke Disease, (Glycogen Storage Disorder I) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- The Acute Hemoabdomen: Topic OverviewDocument23 pagesThe Acute Hemoabdomen: Topic OverviewWeiwei CierraNo ratings yet
- Austin Journal of Tropical Medicine & HygieneDocument5 pagesAustin Journal of Tropical Medicine & HygieneAustin Publishing GroupNo ratings yet
- Cutaneous Metastases in Breast CancerDocument4 pagesCutaneous Metastases in Breast CancerLorelie AsisNo ratings yet
- Nose PDFDocument6 pagesNose PDFNiranjanPandeyNo ratings yet
- Thyroid CancerDocument34 pagesThyroid CancerSahirNo ratings yet
- Individualized Neoantigen-Specific ImmunotherapyDocument16 pagesIndividualized Neoantigen-Specific ImmunotherapyEhed AymazNo ratings yet
- Test: Total Hemoglobin (HGB or HB)Document38 pagesTest: Total Hemoglobin (HGB or HB)Angiela JaurigueNo ratings yet
- Rectal ExaminationDocument21 pagesRectal ExaminationAlexandra HornariuNo ratings yet
- Clinical Research CoordinatorDocument1 pageClinical Research Coordinatorapi-77731042No ratings yet
- Standar Singkatan RSCMDocument54 pagesStandar Singkatan RSCMyannastiNo ratings yet
- Nutrition and Weight ManagementDocument185 pagesNutrition and Weight ManagementKritika Taya100% (1)
- Schramm A., Gellrich N-C., Schmelzeisen R.-Navigational Surgery of The Facial Skeleton (2007)Document172 pagesSchramm A., Gellrich N-C., Schmelzeisen R.-Navigational Surgery of The Facial Skeleton (2007)Remus ChirciuNo ratings yet
- Cementum - A Dynamic Structure UdayDocument85 pagesCementum - A Dynamic Structure UdayVishali Rayapudi100% (1)
- Jurnal r5Document8 pagesJurnal r5Rezkina Azizah PutriNo ratings yet
- Baraclude™ (Entecavir) Baraclude™ (Entecavir) Tablets Baraclude™ (Entecavir) Oral SolutionDocument25 pagesBaraclude™ (Entecavir) Baraclude™ (Entecavir) Tablets Baraclude™ (Entecavir) Oral SolutiondrchughNo ratings yet
- 1 s2.0 S2405896315008587 Main PDFDocument6 pages1 s2.0 S2405896315008587 Main PDFGagandeep Singh KukrejaNo ratings yet
- Chronic Kidney Disease 2012Document455 pagesChronic Kidney Disease 2012Ðr SalmaNo ratings yet
- AMLS Mobile Reference GuideDocument6 pagesAMLS Mobile Reference GuideLim Jun Bin100% (1)
- Material Safety Data Sheet Msds HalotronDocument6 pagesMaterial Safety Data Sheet Msds HalotronHasnin ArifianiNo ratings yet
- Medical Nutrition Therapy For Cancer PreventionDocument5 pagesMedical Nutrition Therapy For Cancer PreventionotaNo ratings yet
- Prinsip Poct Dan Faktor Yang Mempengaruhi Hasil Poct FinalDocument33 pagesPrinsip Poct Dan Faktor Yang Mempengaruhi Hasil Poct Finalahmad syaifulNo ratings yet
- DaleBredesen Final AlzheimersDocument42 pagesDaleBredesen Final AlzheimersJohn William Sugden100% (5)
- KDJVol33No4 KeralaDentalJournal 2Document62 pagesKDJVol33No4 KeralaDentalJournal 2Loly SinagaNo ratings yet
- MS CA and EN Ans KeyDocument15 pagesMS CA and EN Ans KeyAydh Dim-Mac RsclNo ratings yet
- Investigations in Rheumatology: What's New?Document10 pagesInvestigations in Rheumatology: What's New?i can always make u smile :DNo ratings yet
- Template Continued On Page 2: Indication: References: NCCN Supportive CareDocument2 pagesTemplate Continued On Page 2: Indication: References: NCCN Supportive CareJaneNo ratings yet
- Etoposide Package Insert PDFDocument2 pagesEtoposide Package Insert PDFAndreaNo ratings yet
- Oite 2006Document823 pagesOite 2006dastroh100% (1)
- CAFL DatabaseDocument178 pagesCAFL Databasetonym35100% (1)