Professional Documents
Culture Documents
Rcsann 2018 0087
Rcsann 2018 0087
Uploaded by
andre krysaCopyright:
Available Formats
You might also like
- Radix Entomolaris - MansiDocument49 pagesRadix Entomolaris - MansiPawan Yadav Pachwania100% (2)
- Retrosigmoid Approach To Vestibular SchwannomasDocument5 pagesRetrosigmoid Approach To Vestibular SchwannomaskuntawiajiNo ratings yet
- 05Document2 pages05Ahsan JamilNo ratings yet
- Kjellberg 1971Document6 pagesKjellberg 1971Samantha AdrianneNo ratings yet
- Pseudoaneurisma Traumatico de La Arteria BraquialDocument8 pagesPseudoaneurisma Traumatico de La Arteria Braquialalfredo ferregut sanchezNo ratings yet
- Jdapm 22 61Document5 pagesJdapm 22 61andre krysaNo ratings yet
- PolitraumaDocument9 pagesPolitraumaemo230485No ratings yet
- CraniectomyDocument6 pagesCraniectomyale saenzNo ratings yet
- The Management of Intracranial AbscessesDocument3 pagesThe Management of Intracranial AbscessesDio AlexanderNo ratings yet
- TonsillectomyDocument5 pagesTonsillectomyThomasMáximoMancinelliRinaldoNo ratings yet
- All Previous Essay SurgeryDocument170 pagesAll Previous Essay Surgeryalsfyabdullah2021No ratings yet
- Johs Trigger DigitsDocument12 pagesJohs Trigger DigitsDanielz FranceNo ratings yet
- Sem5 - Spinal Cord CompressionDocument11 pagesSem5 - Spinal Cord CompressionOlga Manco GuzmánNo ratings yet
- Thoracic Outlet SyndromeDocument37 pagesThoracic Outlet SyndromeChaman Lal KarotiaNo ratings yet
- J Neurosurg Pediatr Article p701Document4 pagesJ Neurosurg Pediatr Article p701mirmasottNo ratings yet
- Regional Anesthesia and Eye SurgeryDocument7 pagesRegional Anesthesia and Eye SurgeryharumNo ratings yet
- Craniotomy: Jump To Navigation Jump To SearchDocument6 pagesCraniotomy: Jump To Navigation Jump To SearchsakuraleeshaoranNo ratings yet
- Ghan em 2005Document5 pagesGhan em 2005asfwegereNo ratings yet
- Anaesthesia For NeurosurgeryDocument4 pagesAnaesthesia For NeurosurgeryjcaegNo ratings yet
- Cervical Epidural For Total Thyroidectomy in A Patient With Large Thyroid Nodule With Retrosternal Extension With Superior Vena Caval Compression SyndromeDocument2 pagesCervical Epidural For Total Thyroidectomy in A Patient With Large Thyroid Nodule With Retrosternal Extension With Superior Vena Caval Compression SyndromeInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- J2011.Decompressive Craniectomy Technical NoteDocument6 pagesJ2011.Decompressive Craniectomy Technical NoteKysy CodonNo ratings yet
- 267 English 1Document8 pages267 English 1Abante_gammaNo ratings yet
- Revchilanestv49n01 17-1Document5 pagesRevchilanestv49n01 17-1claudia YamunaquéNo ratings yet
- Transient Gerstmann-SyndromeDocument3 pagesTransient Gerstmann-Syndromemuhammad fahrizaNo ratings yet
- Oamjms 9c 146Document5 pagesOamjms 9c 146Seno adipNo ratings yet
- Median Sternotomy ProcedureDocument5 pagesMedian Sternotomy ProcedureNelly NehNo ratings yet
- The Minipterional Craniotomy For Anterior.5Document8 pagesThe Minipterional Craniotomy For Anterior.5J Alan SantosNo ratings yet
- Lateral Epicondylitis: Instructional Review: Shoulder and ElbowDocument7 pagesLateral Epicondylitis: Instructional Review: Shoulder and ElbowzoreNo ratings yet
- (10920684 - Neurosurgical Focus) Surgical Management of Trigeminal Schwannomas - Defining The Role For Endoscopic Endonasal ApproachesDocument9 pages(10920684 - Neurosurgical Focus) Surgical Management of Trigeminal Schwannomas - Defining The Role For Endoscopic Endonasal ApproachesasiyazaidiaNo ratings yet
- Anaesthesia For Trauma PatientsDocument5 pagesAnaesthesia For Trauma Patientscahya candraNo ratings yet
- Cobb - Endoscopic Carpal Tunnel ReleaseDocument8 pagesCobb - Endoscopic Carpal Tunnel ReleaseJohnny WangNo ratings yet
- Prasad 2009Document4 pagesPrasad 2009Alexandru FleșchiuNo ratings yet
- Tuberculosis of SpineDocument11 pagesTuberculosis of SpineSepti RahadianNo ratings yet
- Stomach, Ened, Endino, Rib, Crushed, Hiatus, Life,: 5) - Symptoms Symptoms PermanentDocument4 pagesStomach, Ened, Endino, Rib, Crushed, Hiatus, Life,: 5) - Symptoms Symptoms PermanentayuNo ratings yet
- All Previous Essay Surgery 2Document162 pagesAll Previous Essay Surgery 2DR/ AL-saifiNo ratings yet
- CranioplastyDocument9 pagesCranioplastyPamela MierNo ratings yet
- Hydrocephalus and Trigeminal Neuralgia: Exploring The Association and Management OptionsDocument5 pagesHydrocephalus and Trigeminal Neuralgia: Exploring The Association and Management Optionsakhmad ridhaniNo ratings yet
- Anaesthesia For Chronic Spinal Cord LesionsDocument4 pagesAnaesthesia For Chronic Spinal Cord Lesionsqzh987No ratings yet
- (Journal of Neurosurgery) Neuroendoscopic Approach To Intraventricular LesionsDocument10 pages(Journal of Neurosurgery) Neuroendoscopic Approach To Intraventricular LesionsAniaNo ratings yet
- Left Ventricular Volume Reduction: HistoryDocument6 pagesLeft Ventricular Volume Reduction: HistoryPeter Paul PascualNo ratings yet
- Rothon-Microsurgical Anatomy of The White Matter Tracts.16Document20 pagesRothon-Microsurgical Anatomy of The White Matter Tracts.16J. Mario Vasquez MorenoNo ratings yet
- Correction of The Soft Tissue Pollybeak Using Triamcinolone InjectionDocument5 pagesCorrection of The Soft Tissue Pollybeak Using Triamcinolone Injectionmiglena-filipova-5062No ratings yet
- Transsphenoidal Hypophysectomy:: Postsurgical CT FindingsDocument6 pagesTranssphenoidal Hypophysectomy:: Postsurgical CT FindingsnurNo ratings yet
- Anesthetic Management of A Patient of Valvular Heart Disease Posted For Inguinal Hernioplasty A Case ReportDocument3 pagesAnesthetic Management of A Patient of Valvular Heart Disease Posted For Inguinal Hernioplasty A Case ReportInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Katsarma 2011Document2 pagesKatsarma 2011usmandumassarNo ratings yet
- Oncologic Emergencies: 1. Structural-Obstructive Oncologic Emergencies 1.1. Superior Vena Cava SyndromeDocument5 pagesOncologic Emergencies: 1. Structural-Obstructive Oncologic Emergencies 1.1. Superior Vena Cava SyndromeFreddy PanjaitanNo ratings yet
- Mar 2008Document9 pagesMar 2008debyanditaNo ratings yet
- Treating Thoracic Injuries: CE Article 1Document12 pagesTreating Thoracic Injuries: CE Article 1HendroNo ratings yet
- Articulo AnaDocument5 pagesArticulo AnaPaulina Marquez RojasNo ratings yet
- Anaesthetic Challenges and Management of Myelomeningocele RepairDocument6 pagesAnaesthetic Challenges and Management of Myelomeningocele RepairprastiaNo ratings yet
- Bainton 1990Document2 pagesBainton 1990KaranPadhaNo ratings yet
- BCR 2015 213039 2Document4 pagesBCR 2015 213039 2meirisaafifahNo ratings yet
- TMJ 2Document7 pagesTMJ 2Parvathy R NairNo ratings yet
- Acute Iatrogenic Complications After Mitral Valve RepairDocument7 pagesAcute Iatrogenic Complications After Mitral Valve Repairricardo villaNo ratings yet
- Aneurysmal Subarachnoid HemorrhageDocument17 pagesAneurysmal Subarachnoid Hemorrhageaperfectcircle7978No ratings yet
- Anesthesia Regional y Sindrome Compartamental Nov 21Document5 pagesAnesthesia Regional y Sindrome Compartamental Nov 21ema moralesNo ratings yet
- Brain TumorDocument1 pageBrain TumorChase XerolfNo ratings yet
- Penetrating Neck Trauma - CameronDocument4 pagesPenetrating Neck Trauma - CameronVerónica VidalNo ratings yet
- 0-306-48407-2 - 35 - 2023-02-23T214346.871Document13 pages0-306-48407-2 - 35 - 2023-02-23T214346.871drsubramanianNo ratings yet
- Dislocation of the Temporomandibular Joint: A Guide to Diagnosis and ManagementFrom EverandDislocation of the Temporomandibular Joint: A Guide to Diagnosis and ManagementNigel Shaun MatthewsNo ratings yet
- Kiani 2016Document4 pagesKiani 2016andre krysaNo ratings yet
- Barnard 1990Document2 pagesBarnard 1990andre krysaNo ratings yet
- Alveolar Distraction: Elçin Esenlik,, Evellyn M. Demitchell-RodriguezDocument11 pagesAlveolar Distraction: Elçin Esenlik,, Evellyn M. Demitchell-Rodriguezandre krysaNo ratings yet
- J-1 SWT Orientation Documents - Updated 8-2022Document22 pagesJ-1 SWT Orientation Documents - Updated 8-2022andre krysaNo ratings yet
- Health Insurance Marketplace Notice - Rev 2020Document3 pagesHealth Insurance Marketplace Notice - Rev 2020andre krysaNo ratings yet
- Brain Tumor and Clinical FindingsDocument21 pagesBrain Tumor and Clinical FindingsAlbert Ciam100% (1)
- Weekly Epi Update 79Document19 pagesWeekly Epi Update 79Lee Ji EunNo ratings yet
- Cirrhosis SummaryDocument20 pagesCirrhosis SummaryMike GNo ratings yet
- Neutrophil Maturity in CancerDocument11 pagesNeutrophil Maturity in Cancerxwxdazhong407No ratings yet
- PDF 1 PerceptionDocument70 pagesPDF 1 Perceptionsushma shresthaNo ratings yet
- Pathology Lec 1Document16 pagesPathology Lec 1hamadNo ratings yet
- INOTROPESDocument28 pagesINOTROPESsinghal297% (30)
- Thesis Synopsis For Drug De-Addiction CentreDocument5 pagesThesis Synopsis For Drug De-Addiction CentreNikhil Saxena50% (4)
- Angioedema and It's Homoeopathic TherapeuticsDocument9 pagesAngioedema and It's Homoeopathic TherapeuticsSandip VaghelaNo ratings yet
- Alcohol-Related Psychosis Clinical PresentationDocument5 pagesAlcohol-Related Psychosis Clinical PresentationRavi KumarNo ratings yet
- Hernia FTDDocument71 pagesHernia FTDEmmanuel Papa AcquahNo ratings yet
- Name of Drug Mechanism of Action Indications Side Effects Nursing ConsiderationsDocument9 pagesName of Drug Mechanism of Action Indications Side Effects Nursing ConsiderationsJaysellePuguonTabije100% (1)
- Intensified Pulse Polio ImmunisationDocument30 pagesIntensified Pulse Polio ImmunisationAdrishyaNo ratings yet
- AoweifnDocument2 pagesAoweifnMichael C. PhamNo ratings yet
- Test Bank For Medical Terminology A Living Language 7th Edition Bonnie Fremgen, Suzanne FruchtDocument49 pagesTest Bank For Medical Terminology A Living Language 7th Edition Bonnie Fremgen, Suzanne Fruchteducationaldocument012No ratings yet
- Therapeutic Drug IndexDocument32 pagesTherapeutic Drug Indexibano626No ratings yet
- SalmonellaDocument9 pagesSalmonellaAlyssa Jane MagkalasNo ratings yet
- Mobile PTH Testing: Tosoh SolutionsDocument2 pagesMobile PTH Testing: Tosoh SolutionsAhmed LarbiNo ratings yet
- YU 2007 GSL STRUCTURES ComprehensiveDocument50 pagesYU 2007 GSL STRUCTURES ComprehensiveRamona Neka TamoNo ratings yet
- Laboratory Investigation ReportDocument1 pageLaboratory Investigation ReportMd blackNo ratings yet
- Textbook Clinical Neurology Lange Roger P Simon Ebook All Chapter PDFDocument53 pagesTextbook Clinical Neurology Lange Roger P Simon Ebook All Chapter PDFdaniel.miller496100% (18)
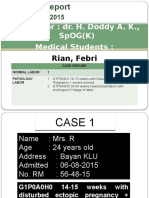
- Supervisor: Dr. H. Doddy A. K., Spog (K) Medical Students:: Rian, FebriDocument12 pagesSupervisor: Dr. H. Doddy A. K., Spog (K) Medical Students:: Rian, FebriRian Segal HidajatNo ratings yet
- RUBRIC Endotracheal SuctioningDocument4 pagesRUBRIC Endotracheal Suctioning11- Nolasco, Mary Rose F.No ratings yet
- Laporan DK1 P4Document57 pagesLaporan DK1 P4Afifah Marwah Al-QadrieNo ratings yet
- 4 Core Steps of EincDocument52 pages4 Core Steps of Eincjamaica cabriga100% (1)
- Treatment PDADocument8 pagesTreatment PDAijaldo ajahNo ratings yet
- Human Health and DiseasesDocument4 pagesHuman Health and DiseasesRoshan KarthikeyanNo ratings yet
- Metabolism (Ncm-216)Document10 pagesMetabolism (Ncm-216)Sofronio OmboyNo ratings yet
- Abnormal Weight Gain in Infant As The Risk of Stunting in Later LifeDocument35 pagesAbnormal Weight Gain in Infant As The Risk of Stunting in Later LifeWint ArdhayaniNo ratings yet
Rcsann 2018 0087
Rcsann 2018 0087
Uploaded by
andre krysaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Rcsann 2018 0087
Rcsann 2018 0087
Uploaded by
andre krysaCopyright:
Available Formats
ONLINE CASE REPORT
Ann R Coll Surg Engl 2018; 100: e174–e175
doi 10.1308/rcsann.2018.0087
Management of a temporomandibular joint
synovial cyst in a case complicated by severe
trigeminocardiac reflex
S El-Habbash, P Padaki, S Bayoumi, P Ross
North Manchester General Hospital, Pennine Acute Hospitals NHS Trust, Manchester, UK
ABSTRACT
The trigeminocardiac reflex is a rare occurrence in patients undergoing maxillofacial surgery, with a reported incidence of 1–2%.
Clinical signs and symptoms include bradycardia, nausea, with further stimulation potentially leading to cardiac dysrhythmias,
ectopic beats, atrioventricular blocks and asystole. Most maxillofacial procedures, including temporomandibular joint procedures,
are considered low risk. We report the first case of a tender temporomandibular joint synovial cyst whose management was compli-
cated by severe trigeminocardiac reflex resulting in asystole. We suggest that in such cases communication between surgeons and
the anaesthesia team is of paramount importance and informing the anaesthetist intraoperatively prior to the manipulation of the
capsule or temporomandibular joint meniscus is recommended in the prevention or successful treatment of this condition.
KEYWORDS
TMJ – Synovial cyst – Trigeminocardiac reflex – Temporomandibular joint
Accepted 18 March 2018
CORRESPONDENCE TO
Salwa El-Habbash, E: salwa89@gmail.com
Introduction consultant colleague who undertook temporomandibular
joint surgeries and a decision was taken to monitor the cyst.
Trigeminocardiac reflex was first described as the oculocar-
This was complicated, however, by significant pain and a
diac reflex in 1908 and was attributed to pressure-induced
new onset of recurrent locking of the temporomandibular
cardiac reflex that caused cardiac depression through the
joint. As a result of this, the patient underwent eminectomy,
stimulation of the vagal nerve. Today it is described as a sud-
with the aim of creating space for the meniscus and the cyst,
den decrease in heart rate of more than 20% of the baseline
and to facilitate free movement of the meniscus. This did not
values, dysrhythmias or sinoatrial arrest.1 We present a case
result in alleviation of the symptoms and so high condylec-
of a tender cyst in the temporomandibular joint, whose treat-
tomy was planned following further discussion at the head
ment was complicated by severe trigeminocardiac reflex,
and neck multidisciplinary team meeting. High condylec-
and its subsequent management.
tomy was the next best option, as meniscectomy including
removal of synovial cyst was not deemed possible owing to
Case history the aforementioned complication at initial surgery.
A 56-year-old woman with no significant medical history The patient was pre-emptively administered 200 micro-
presented with a tender bony lump on the left zygomatic grams glycopyrrolate intravenously at the time of meniscal
arch. Magnetic resonance imaging revealed a 1-cm ganglion manipulation and since this did not result in bradycardia,
cyst related to the left temporomandibular joint (Figs 1 and meniscectomy and cyst excision were carried out with inter-
2). On examination, the lump appeared to be fixed, increas- positional abdominal fat graft insertion and high condylec-
ing in size and painful. A plan was devised for open explora- tomy was abandoned, as this was a more aggressive
tion of the left temporomandibular joint with cyst excision. treatment option with attendant risks such as a discrepancy
Attempted cyst excision under general anaesthesia resulted in the occlusion. The patient had a significant reduction in
in asystole on manipulation of the cyst. The heart rate imme- pain following surgery and no longer experienced locking of
diately returned to normal with release of the tissue and the temporomandibular joint.
administration of 300 micrograms of atropine intravenously.
The procedure was aborted and incisional biopsy, which had Discussion
already been taken, showed it to be a simple synovial cyst.
Management options were discussed at the head and Trigeminocardiac reflex is a rare occurrence in patients
neck multidisciplinary team meeting, together with a undergoing maxillofacial surgery, with a reported incidence
e174 Ann R Coll Surg Engl 2018; 100: e174–e175
EL-HABBASH PADAKI BAYOUMI ROSS MANAGEMENT OF A TEMPOROMANDIBULAR JOINT SYNOVIAL CYST
IN A CASE COMPLICATED BY SEVERE TRIGEMINOCARDIAC REFLEX
of 1–2%.2 The trigeminocardiac reflex is activated when
sensory branches of the trigeminal nerve are mechanically
stimulated by pressure, stretching, or movement.3 This sets
off an arc in which vagal stimulation leads to a cardiac
depressor response.3 Most cases are associated with a 10–
50% reduction in heart rate, which returns to normal upon
cessation of the stimulus.1 Clinical signs and symptoms
include bradycardia, nausea, faintness with further stimula-
tion potentially leading to cardiac dysrhythmias, ectopic
beats, atrioventricular blocks and asystole.4
Predisposing risk factors include cardiac disease, hypo-
xaemia, hypercapnia, as well as children.2 Lubbers et al.
have suggested a surgical stratification of risk factors
wherein most maxillofacial procedures, including temporo-
mandibular joint procedures, are considered low risk.2
Following recognition of the onset of reflex bradycardia,
avoidance of predisposing factors, halting the surgical stim-
ulus, intravenous administration of atropine or glycopyrro-
late and anaesthesia of the afferent nerves are the suggested
treatment options.1,4 In our case, all of the above were done,
with the exception of anaesthesia of the afferent nerve,
which was not necessary as the asystole resolved with the
other measures. We suggest communication between sur-
Figure 1 Magnetic resonance image: coronal view geons and the anaesthesia team is of paramount importance
and informing the anaesthetist intraoperatively prior to the
manipulation of the capsule or temporomandibular joint
meniscus is recommended in the prevention or successful
treatment of this condition. With temporomandibular joint
surgery being considered a low-risk surgery for the develop-
ment of trigeminocardiac reflex, and with an incidence as
low as 1–2%, it can be argued that routine administration of
pre-emptive anticholinergic drugs may not be advisable and
hence was not undertaken in our case at the initial surgery.
References
1. Bohluli B, Ashtiani AK, Khayampoor A, Sadr-Eshkevari P. Trigeminocardiac
reflex. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009; 108: 184–188.
2. Lübbers HD, Zweifel D, Gratz KW, Kruse A. Classification of potential risk
factors for trigeminocardiac reflex in craniomaxillofacial surgery. J Oral
Maxillofac Surg 2010; 68: 1,317–1,321.
3. Dillon M, Power A, Mannion C. Trigeminocardiac reflex. Br J Oral Maxillofac
Surg 2017; 55: 445–446.
4. Scott Roberts R, Best JA, Sharpio RD. Trigeminocardiac reflex during
temperomandibular joint arthroscopy: report of a case. J Oral Maxillofac Surg
1999; 57: 854–856.
Figure 2 Magnetic resonance image: axial view
Ann R Coll Surg Engl 2018; 100: e174–e175 e175
You might also like
- Radix Entomolaris - MansiDocument49 pagesRadix Entomolaris - MansiPawan Yadav Pachwania100% (2)
- Retrosigmoid Approach To Vestibular SchwannomasDocument5 pagesRetrosigmoid Approach To Vestibular SchwannomaskuntawiajiNo ratings yet
- 05Document2 pages05Ahsan JamilNo ratings yet
- Kjellberg 1971Document6 pagesKjellberg 1971Samantha AdrianneNo ratings yet
- Pseudoaneurisma Traumatico de La Arteria BraquialDocument8 pagesPseudoaneurisma Traumatico de La Arteria Braquialalfredo ferregut sanchezNo ratings yet
- Jdapm 22 61Document5 pagesJdapm 22 61andre krysaNo ratings yet
- PolitraumaDocument9 pagesPolitraumaemo230485No ratings yet
- CraniectomyDocument6 pagesCraniectomyale saenzNo ratings yet
- The Management of Intracranial AbscessesDocument3 pagesThe Management of Intracranial AbscessesDio AlexanderNo ratings yet
- TonsillectomyDocument5 pagesTonsillectomyThomasMáximoMancinelliRinaldoNo ratings yet
- All Previous Essay SurgeryDocument170 pagesAll Previous Essay Surgeryalsfyabdullah2021No ratings yet
- Johs Trigger DigitsDocument12 pagesJohs Trigger DigitsDanielz FranceNo ratings yet
- Sem5 - Spinal Cord CompressionDocument11 pagesSem5 - Spinal Cord CompressionOlga Manco GuzmánNo ratings yet
- Thoracic Outlet SyndromeDocument37 pagesThoracic Outlet SyndromeChaman Lal KarotiaNo ratings yet
- J Neurosurg Pediatr Article p701Document4 pagesJ Neurosurg Pediatr Article p701mirmasottNo ratings yet
- Regional Anesthesia and Eye SurgeryDocument7 pagesRegional Anesthesia and Eye SurgeryharumNo ratings yet
- Craniotomy: Jump To Navigation Jump To SearchDocument6 pagesCraniotomy: Jump To Navigation Jump To SearchsakuraleeshaoranNo ratings yet
- Ghan em 2005Document5 pagesGhan em 2005asfwegereNo ratings yet
- Anaesthesia For NeurosurgeryDocument4 pagesAnaesthesia For NeurosurgeryjcaegNo ratings yet
- Cervical Epidural For Total Thyroidectomy in A Patient With Large Thyroid Nodule With Retrosternal Extension With Superior Vena Caval Compression SyndromeDocument2 pagesCervical Epidural For Total Thyroidectomy in A Patient With Large Thyroid Nodule With Retrosternal Extension With Superior Vena Caval Compression SyndromeInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- J2011.Decompressive Craniectomy Technical NoteDocument6 pagesJ2011.Decompressive Craniectomy Technical NoteKysy CodonNo ratings yet
- 267 English 1Document8 pages267 English 1Abante_gammaNo ratings yet
- Revchilanestv49n01 17-1Document5 pagesRevchilanestv49n01 17-1claudia YamunaquéNo ratings yet
- Transient Gerstmann-SyndromeDocument3 pagesTransient Gerstmann-Syndromemuhammad fahrizaNo ratings yet
- Oamjms 9c 146Document5 pagesOamjms 9c 146Seno adipNo ratings yet
- Median Sternotomy ProcedureDocument5 pagesMedian Sternotomy ProcedureNelly NehNo ratings yet
- The Minipterional Craniotomy For Anterior.5Document8 pagesThe Minipterional Craniotomy For Anterior.5J Alan SantosNo ratings yet
- Lateral Epicondylitis: Instructional Review: Shoulder and ElbowDocument7 pagesLateral Epicondylitis: Instructional Review: Shoulder and ElbowzoreNo ratings yet
- (10920684 - Neurosurgical Focus) Surgical Management of Trigeminal Schwannomas - Defining The Role For Endoscopic Endonasal ApproachesDocument9 pages(10920684 - Neurosurgical Focus) Surgical Management of Trigeminal Schwannomas - Defining The Role For Endoscopic Endonasal ApproachesasiyazaidiaNo ratings yet
- Anaesthesia For Trauma PatientsDocument5 pagesAnaesthesia For Trauma Patientscahya candraNo ratings yet
- Cobb - Endoscopic Carpal Tunnel ReleaseDocument8 pagesCobb - Endoscopic Carpal Tunnel ReleaseJohnny WangNo ratings yet
- Prasad 2009Document4 pagesPrasad 2009Alexandru FleșchiuNo ratings yet
- Tuberculosis of SpineDocument11 pagesTuberculosis of SpineSepti RahadianNo ratings yet
- Stomach, Ened, Endino, Rib, Crushed, Hiatus, Life,: 5) - Symptoms Symptoms PermanentDocument4 pagesStomach, Ened, Endino, Rib, Crushed, Hiatus, Life,: 5) - Symptoms Symptoms PermanentayuNo ratings yet
- All Previous Essay Surgery 2Document162 pagesAll Previous Essay Surgery 2DR/ AL-saifiNo ratings yet
- CranioplastyDocument9 pagesCranioplastyPamela MierNo ratings yet
- Hydrocephalus and Trigeminal Neuralgia: Exploring The Association and Management OptionsDocument5 pagesHydrocephalus and Trigeminal Neuralgia: Exploring The Association and Management Optionsakhmad ridhaniNo ratings yet
- Anaesthesia For Chronic Spinal Cord LesionsDocument4 pagesAnaesthesia For Chronic Spinal Cord Lesionsqzh987No ratings yet
- (Journal of Neurosurgery) Neuroendoscopic Approach To Intraventricular LesionsDocument10 pages(Journal of Neurosurgery) Neuroendoscopic Approach To Intraventricular LesionsAniaNo ratings yet
- Left Ventricular Volume Reduction: HistoryDocument6 pagesLeft Ventricular Volume Reduction: HistoryPeter Paul PascualNo ratings yet
- Rothon-Microsurgical Anatomy of The White Matter Tracts.16Document20 pagesRothon-Microsurgical Anatomy of The White Matter Tracts.16J. Mario Vasquez MorenoNo ratings yet
- Correction of The Soft Tissue Pollybeak Using Triamcinolone InjectionDocument5 pagesCorrection of The Soft Tissue Pollybeak Using Triamcinolone Injectionmiglena-filipova-5062No ratings yet
- Transsphenoidal Hypophysectomy:: Postsurgical CT FindingsDocument6 pagesTranssphenoidal Hypophysectomy:: Postsurgical CT FindingsnurNo ratings yet
- Anesthetic Management of A Patient of Valvular Heart Disease Posted For Inguinal Hernioplasty A Case ReportDocument3 pagesAnesthetic Management of A Patient of Valvular Heart Disease Posted For Inguinal Hernioplasty A Case ReportInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Katsarma 2011Document2 pagesKatsarma 2011usmandumassarNo ratings yet
- Oncologic Emergencies: 1. Structural-Obstructive Oncologic Emergencies 1.1. Superior Vena Cava SyndromeDocument5 pagesOncologic Emergencies: 1. Structural-Obstructive Oncologic Emergencies 1.1. Superior Vena Cava SyndromeFreddy PanjaitanNo ratings yet
- Mar 2008Document9 pagesMar 2008debyanditaNo ratings yet
- Treating Thoracic Injuries: CE Article 1Document12 pagesTreating Thoracic Injuries: CE Article 1HendroNo ratings yet
- Articulo AnaDocument5 pagesArticulo AnaPaulina Marquez RojasNo ratings yet
- Anaesthetic Challenges and Management of Myelomeningocele RepairDocument6 pagesAnaesthetic Challenges and Management of Myelomeningocele RepairprastiaNo ratings yet
- Bainton 1990Document2 pagesBainton 1990KaranPadhaNo ratings yet
- BCR 2015 213039 2Document4 pagesBCR 2015 213039 2meirisaafifahNo ratings yet
- TMJ 2Document7 pagesTMJ 2Parvathy R NairNo ratings yet
- Acute Iatrogenic Complications After Mitral Valve RepairDocument7 pagesAcute Iatrogenic Complications After Mitral Valve Repairricardo villaNo ratings yet
- Aneurysmal Subarachnoid HemorrhageDocument17 pagesAneurysmal Subarachnoid Hemorrhageaperfectcircle7978No ratings yet
- Anesthesia Regional y Sindrome Compartamental Nov 21Document5 pagesAnesthesia Regional y Sindrome Compartamental Nov 21ema moralesNo ratings yet
- Brain TumorDocument1 pageBrain TumorChase XerolfNo ratings yet
- Penetrating Neck Trauma - CameronDocument4 pagesPenetrating Neck Trauma - CameronVerónica VidalNo ratings yet
- 0-306-48407-2 - 35 - 2023-02-23T214346.871Document13 pages0-306-48407-2 - 35 - 2023-02-23T214346.871drsubramanianNo ratings yet
- Dislocation of the Temporomandibular Joint: A Guide to Diagnosis and ManagementFrom EverandDislocation of the Temporomandibular Joint: A Guide to Diagnosis and ManagementNigel Shaun MatthewsNo ratings yet
- Kiani 2016Document4 pagesKiani 2016andre krysaNo ratings yet
- Barnard 1990Document2 pagesBarnard 1990andre krysaNo ratings yet
- Alveolar Distraction: Elçin Esenlik,, Evellyn M. Demitchell-RodriguezDocument11 pagesAlveolar Distraction: Elçin Esenlik,, Evellyn M. Demitchell-Rodriguezandre krysaNo ratings yet
- J-1 SWT Orientation Documents - Updated 8-2022Document22 pagesJ-1 SWT Orientation Documents - Updated 8-2022andre krysaNo ratings yet
- Health Insurance Marketplace Notice - Rev 2020Document3 pagesHealth Insurance Marketplace Notice - Rev 2020andre krysaNo ratings yet
- Brain Tumor and Clinical FindingsDocument21 pagesBrain Tumor and Clinical FindingsAlbert Ciam100% (1)
- Weekly Epi Update 79Document19 pagesWeekly Epi Update 79Lee Ji EunNo ratings yet
- Cirrhosis SummaryDocument20 pagesCirrhosis SummaryMike GNo ratings yet
- Neutrophil Maturity in CancerDocument11 pagesNeutrophil Maturity in Cancerxwxdazhong407No ratings yet
- PDF 1 PerceptionDocument70 pagesPDF 1 Perceptionsushma shresthaNo ratings yet
- Pathology Lec 1Document16 pagesPathology Lec 1hamadNo ratings yet
- INOTROPESDocument28 pagesINOTROPESsinghal297% (30)
- Thesis Synopsis For Drug De-Addiction CentreDocument5 pagesThesis Synopsis For Drug De-Addiction CentreNikhil Saxena50% (4)
- Angioedema and It's Homoeopathic TherapeuticsDocument9 pagesAngioedema and It's Homoeopathic TherapeuticsSandip VaghelaNo ratings yet
- Alcohol-Related Psychosis Clinical PresentationDocument5 pagesAlcohol-Related Psychosis Clinical PresentationRavi KumarNo ratings yet
- Hernia FTDDocument71 pagesHernia FTDEmmanuel Papa AcquahNo ratings yet
- Name of Drug Mechanism of Action Indications Side Effects Nursing ConsiderationsDocument9 pagesName of Drug Mechanism of Action Indications Side Effects Nursing ConsiderationsJaysellePuguonTabije100% (1)
- Intensified Pulse Polio ImmunisationDocument30 pagesIntensified Pulse Polio ImmunisationAdrishyaNo ratings yet
- AoweifnDocument2 pagesAoweifnMichael C. PhamNo ratings yet
- Test Bank For Medical Terminology A Living Language 7th Edition Bonnie Fremgen, Suzanne FruchtDocument49 pagesTest Bank For Medical Terminology A Living Language 7th Edition Bonnie Fremgen, Suzanne Fruchteducationaldocument012No ratings yet
- Therapeutic Drug IndexDocument32 pagesTherapeutic Drug Indexibano626No ratings yet
- SalmonellaDocument9 pagesSalmonellaAlyssa Jane MagkalasNo ratings yet
- Mobile PTH Testing: Tosoh SolutionsDocument2 pagesMobile PTH Testing: Tosoh SolutionsAhmed LarbiNo ratings yet
- YU 2007 GSL STRUCTURES ComprehensiveDocument50 pagesYU 2007 GSL STRUCTURES ComprehensiveRamona Neka TamoNo ratings yet
- Laboratory Investigation ReportDocument1 pageLaboratory Investigation ReportMd blackNo ratings yet
- Textbook Clinical Neurology Lange Roger P Simon Ebook All Chapter PDFDocument53 pagesTextbook Clinical Neurology Lange Roger P Simon Ebook All Chapter PDFdaniel.miller496100% (18)
- Supervisor: Dr. H. Doddy A. K., Spog (K) Medical Students:: Rian, FebriDocument12 pagesSupervisor: Dr. H. Doddy A. K., Spog (K) Medical Students:: Rian, FebriRian Segal HidajatNo ratings yet
- RUBRIC Endotracheal SuctioningDocument4 pagesRUBRIC Endotracheal Suctioning11- Nolasco, Mary Rose F.No ratings yet
- Laporan DK1 P4Document57 pagesLaporan DK1 P4Afifah Marwah Al-QadrieNo ratings yet
- 4 Core Steps of EincDocument52 pages4 Core Steps of Eincjamaica cabriga100% (1)
- Treatment PDADocument8 pagesTreatment PDAijaldo ajahNo ratings yet
- Human Health and DiseasesDocument4 pagesHuman Health and DiseasesRoshan KarthikeyanNo ratings yet
- Metabolism (Ncm-216)Document10 pagesMetabolism (Ncm-216)Sofronio OmboyNo ratings yet
- Abnormal Weight Gain in Infant As The Risk of Stunting in Later LifeDocument35 pagesAbnormal Weight Gain in Infant As The Risk of Stunting in Later LifeWint ArdhayaniNo ratings yet