Professional Documents
Culture Documents
Emergency and Disaster Nursing
Emergency and Disaster Nursing
Uploaded by
Rachell PobleteOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Emergency and Disaster Nursing
Emergency and Disaster Nursing
Uploaded by
Rachell PobleteCopyright:
Available Formats
EMERGENCY AND DISASTER NURSING
DEFINITION OF TERMS BURNS
→ EMERGENCY – serious, unexpected, and often → Priority is fluid losses d/t fluid shifting from burns
dangerous situation requiring immediate action → Fluid shifting → cellular injury → albumin loss →
→ DISASTER – sudden event, such as accident or natural decreased oncotic pressure → prevent pulling of water
catastrophe, that causes great damage or loss of life from the interstitial to intravascular space → stasis of
○ E.g., earthquakes, typhoon water in the interstitial space (third spacing) → edema,
○ E.g., manmade terrorism, war ascites, fluid at pericardium
Who is your priority patient? • Fluid shifting happens from intravascular/blood
a. Patient with hantavirus syndrome- respiratory disorder r/t vessel (functional) to interstitial/third space (non-
ingestion/inhalation of rodent body fluids (common in floods, functional)
urine of rats)
→ If no scenario, fluid is priority
b. Patient with takutsubi disorder- cardiomyopathy
c. Patient with alice in wonderland syndrome- visual disorder
(small things look bigger, c/c)
d. Patient with Zollinger ellison syndrome- increases GIT
functioning that leads to possibility of ulcers
DEGREE DEPTH LAYER PAIN EDEMA CHARACTERISTICS
Superficial/
No Red, blanching - not
superficial partial
FIRST Epidermis Yes (X) third space → included in parkland
(X) fluid losses formula
E.g., sunburn
Red, blisters, weeping,
Deep partial/ partial
mottled (nagkukulubot)
thickness
Yes → Blisters and weeping
SECOND Dermis Yes third spacing → are d/t third spacing
E.g., scald burn
fluid losses → edema
(talsik ng mainit na
→ Included in parkland
mantika)
formula
No
Red, mottled, yellow
d/t very deep
Epidermis, dermis, (subcutaneous), brown
burn (burned Yes
subcutaneous/ (muscle), white (bone),
THIRD Full thickness burns nerves, third spacing →
hypodermis, black charred, leathery-
destroyed fluid losses
muscles, bones Included in parkland
nerve
formula
endings)
PARKLAND FOR (4) MULA Adult
→ Total ml of fluid to be replaced in the first 24 hours → Head and neck: 9
• 50% first 8 hours = 5000ml • Anterior: 4.5
• 50% in the last 16 hours = 5000ml • Posterior: 4.5
• Example total ml in the first 24 hours = 10,000ml → Trunk: 36
→ TBSA (total body surface area) x body weight in kg x • Anterior Trunk: 18
4ml (constant) o Chest: 9
→ Example: Adult 28% TBSA burn, weighs 100lbs. What o Abdomen: 9
is the total ml in the last 16 hours? • Posterior Trunk: 18
• 100lbs/2.2 = 45.5 kg → Arm: 9
• 28 x 45.5 x 4ml = 5096ml (first 24 hours) • Anterior: 4.5
• 5096/2 = 2548 ml (last 16 hours) • Posterior: 4.5 or
• Volume is greater in the first 8 hours d/t risk for fluid • Upper arm: 4.5
collapse • Forearm: 4.5
→ Leg: 18
RULE OF NINES • Anterior: 9
→ In palmar method, the palm of the patient is used. This • Posterior: 9
is not accurate → Perineum: 1
→ Example: Adult 200lbs with first degree burns at
anterior chest and posterior right leg. Deep partial
burns at arms and left anterior leg. What is the ml in the
first 24 hours?
• Body weight 200 lbs = 90.9 kgs
• TBSA = 9 x 2 (18) + 9 = 27% TBSA
• 90.9 kg x 27% TBSA x 4 mL = 9817.2 ml for first
24 hours
• 9817 ml / 2 = 4908.6/4909 ml in the first 8 hours
→ Example: Adult 72 kg with full thickness burns at
anterior trunk (18%) and perineum (1%), deep partial
burns at anterior right leg (9%) and posterior left leg PHASES OF BURN INJURY
(9%). What is the ml in the first 8 hours? First Phase: Emergent Phase/Shock/Resuscitative
• BW 72 kgs → 24-48 hours
• TBSA = 18 + 18 + 1 = 37% TBSA → Problem: fluid deficit
• 72 kgs x 37 x 4 ml = 10,656 mL in the first 24 hours → Priority: fluid resuscitation/replacement
• 10,656 ml/2 = 5328 mL in the first 8 hours • Best fluid: PLR
→ Example: Adult 150lbs suffered burns, third degree at • Situational: Airway is Priority when,
right anterior arm (4.5%), left arm (9%). First degree at o (+) inhalation injury (facial burns, singed facial
right leg. Second degree at anterior head (4.5%). What hair, soot, bronchospasm - AEB wheezes/
is the ml in the last 16 hours? stridor/DOB)
• BW 150 lbs = 68.2 kgs → Priority assessment: vital signs
• TBSA = 4.5 + 9 + 4.5 = 18% TBSA → Priority laboratory value: HCT
• 68.2 kgs x 18 x 4 ml = 4910.4 ml for the first 24 → Symptoms:
hours • ↓BP- compensatory mechanism (↑RR, ↑HR)
• 4910.4/2 = 2455.2 for the last 16 hours • ↓Urine output- compensatory mechanism to
conserve fluid
Infant • ↑hematocrit- concentrated blood d/t dehydration
→ Head: 18 • Hyperkalemia and hyponatremia - presence of
• Anterior: 9 cellular injury → shifting of electrolytes
• Posterior: 9 o Normal: potassium in, sodium out (PISO)
→ Trunk: 36 → Management (in the EMERGENT PHASE):
• Anterior Trunk: 18 • Priority is fluid; if (+) inhalation injury- airway
o Chest: 9 o It is vital to replace fluids immediately
o Abdomen: 9 • WOF: severe pain- administer
• Posterior Trunk: 18 morphine/fentanyl/demerol (opioids)
→ Arm: 9 o Do not put toothpaste on burns as it may cause
• Anterior: 4.5 further irritation
• Posterior: 4.5 or o First aid management:
• Upper arm: 4.5 ▪ Running water
• Forearm: 4.5 ▪ Wash with soap and water to prevent
→ Leg: 14 tetanus
• Anterior: 7 ▪ Moist to dry, apply antibiotic ointment
• Posterior: 7 • WOF: curling's ulcer- stress ulcer r/t burn (↑HCl) →
→ Perineum: not counted administer antacids, PPIs (-zoles), H2 blockers (-
→ Example: The patient suffers superficial burns on the dine)
chest, posterior left leg, and anterior right thigh; deep
partial burns on the whole head (18%), posterior trunk Second Phase: Acute Phase/Diuretic
(18%), right and left forearm (4.5% + 4.5%); and full → Post 48 hours-5 days
thickness burns of the abdomen (9%), and anterior left → Risk for infection
leg (7%). How much is the TBSA of the patient that → Symptoms:
would be included in the parkland formula? = 61% • ↑BP, ↑RR, ↑HR d/t vascular resistance
TBSA o Blood vessels are forced d/t accumulation of
• TBSA = 18 + 18 + 4.5 + 4.5 + 9 + 7 = 61% TBSA fluids (expected)
→ Example: 12 lbs sustained full thickness burns at right • ↑Urine output- fluids are replaced already
leg (14%), abdomen (9%) and perineum (X). Superficial o Best determinant for effectiveness of the fluid
burns at the head and neck. Partial thickness at arms therapy
(18%) and posterior trunk (18%). What is the mL in the • Hypokalemia and hyponatremia
first 8 hours? o Diluted sodium d/t abundance of fluids
• BW 12lbs = 5.5 kgs • ↓Hematocrit- overhydrated → diluted blood
• TBSA = 14 + 9 + 18 + 18 = 59% TBSA (expected)
• 5.5 kgs x 59 TBSA x 4mL = 1,298mL in the first 24 → Management:
hours • Priority is to prevent infection
• 1,298 ml/2 = 649 mL in the first 8 hours o Teach the patient to do handwashing
→ Example: 4kgs with second degree burn at the anterior o Use PPEs
trunk (18%) and left leg (14%). Third degree burns at o Place the patient in a private positive pressure
the right arm (9%) and posterior left arm (4.5%), head room
and neck are also affected (18%). What is the mL in the o Assist in wound/scab/eschar debridement
first 24 hours? (sterile) to promote wound healing, promote
• BW = 4kgs absorption of antibiotic ointment that doesn't
• TBSA = 18 + 14 + 9 + 4.5 + 18 = 63.5% pass the eschar
• 4 kgs x 63.5% TBSA x 4 mL = 1,016 mL in the first ▪ Silver nitrate (sulfadiazine)- faster healing
24 hours ▪ Mafenide acetate - new drug (more
expensive) - passes the eschar, offers
lesser pain
❖ AE: hemolytic anemia
➢ To prevent AE, apply drug thinly-
1/16 - 1/18 inch
o Situational: (+) Circumferential burn → Simple Triage
↑pressure → compartment syndrome (pallor, → Easy to perform because patient status is considered
pain, paresthesia, paralysis, pulselessness, → START- Simple Triage And Rapid treatment
poikilothermia- from hot to cold) • 3 main groups:
▪ Compartment syndrome is d/t o Respiration - airway and breathing problems
compression of the muscles → ↓blood flow o Perfusion - circulation: blood or fluid losses
→ necrosis → amputation o Mental status- disability, psychological
▪ Management: fasciotomy disorders (LOC)
Prioritization Rules
→ Adult
• If age is not given
• Prioritization: ABCD
o Bronchospasm before bleeding
• For cardiac arrest: CompressionAB
• Unexpected > expected symptoms
• Systemic > localized
o Acute before chronic
→ Pedia: danger signs (CUVA)
• Convulsions
• Unable to feed
• Vomits everything
• Abnormally sleepy
→ Geria- confusion
Third Phase: Recovery Phase • Safety issue
→ >5days • Sign of infection
→ Focus: rehabilitation • Bleeding
→ Symptoms: all stable including lab values • Dehydration
→ Goal: Promote/restore optimal function • Cerebral hypoxia
• Scars - body image disturbance - refer to plastic → Psychiatric disorders (physiological > psychological)
surgery • E.g., Anorexia nervosa- meal planning > coping
• Contractures - prevention: functional position → Pedia (most vulnerable) > geria > adult
(extend/flex)
Priority
A. MI with severe substernal crushing chest pain -
PRIORITY
B. Myasthenia Gravis with Ptosis - not life threatening
A. Multiple Myeloma with bone pain and lesions - expected
(ABC disability)
B. Internal radiation with weakness and pallor - expected
• Skin Graft to promote wound healing C. Chemotherapy patient with mild fever - unexpected =
o Ensure blood perfusion neutropenic fever (priority: risk for infection)
o Avoid dislodgement D. Testicular cancer with groin pain and enlargement -
o Place the patient on the unaffected site expected
o Bed cradle with blanket
A. Angina pectoris patient with stabbing pain after
nitroglycerin administration - unexpected
B. Patient for angiography who is anxious about the surgery
- expected
C. Cardiac tamponade with hypotension and heart murmurs
- expected
D. Abdominal Aortic Aneurysm (AAA) with mild leg pain
and pulsating abdominal mass - expected; leg pain
indicates rupture
Types of Skin Graft
A. Patient with conjunctivitis with redness and crusting on
→ Autograft- from self
the eyes- expected
→ Isograft/Synergistic- from twin
B. Patient with rocky mountain spotted fever with rashes
→ Homograft/Allograft- from another human and fever- expected
→ Heterograft/Xenograft - from animals (fish skin) C. Patient with HIV with decreased WBC levels and raise
• Porcine- pig skin purplish lesion - unexpected (Kaposi Sarcoma - patient
o Contraindicated to Muslims progressed to AIDS)
• Bovine- cow skin D. Patient with meningitis with arching of the back and
nuchal rigidity - expected
TRIAGE
A. Patient third trimester with BP of 159/95 with mild pre-
→ to sort of classify patients according to priority
eclampsia - expected; >160 = eclampsia
→ Most important ethical principle is justice (fairness, B. Patient post shoulder dystocia delivery with grade 2
equity- based on the need) episiotomy - expected
C. Patient with ectopic pregnancy with unilateral
• Unequal pupils > fracture
abdominal pain and shoulder pain - shoulder pain → External – pre-hospital, unstructured, limited resources,
indicates rupture → sepsis focus is first aid, priority is high survival over low survival
D. Patient first trimester pregnancy who is unsure of the • Cardiac arrest < chest pain
current status - expected • Unequal pupils < open fracture
• Chest pain (needs care) > fracture
A. 2-year-old with DOB and severe pneumonia -
• Red > yellow > green > black (low survival)
unexpected
→ Reverse triage - DISASTER, massive, military scenario.
B. 5-year-old with asthma and wheezing - airway problem
C. 15-year-old adolescent drunk with stab wound on the
Obsolete resources. Priority is most stable
chest - breathing and bleeding problem • War, terrorisms, earthquake
D. 2-year-old with food poisoning who vomits • Priority is green > yellow > red > black
everything - dehydration, danger signs are priority in • Principle of utilitarianism: greatest good for the
pediatric clients greatest number
E. 1 year old post head trauma who is difficult to awaken -
Sample Question
LOC (neuro); expected
Building collapse - external (high survival- red)
1. Cardiac arrest - black
Advanced Triage 2. Chest pain - red
→ Patient status and resources are considered 3. Leg fracture - yellow
4. Sprain - green
• War - reverse (4; same situation)
Types of Advanced Triage
• ward - internal (1; same situation)
→ Internal – hospital, structured (+) resources, focus is
• 20 patients rushed to the emergency department -
definitive care, priority is sickest > well
shift to external (2; same situation)
• Cardiac arrest > chest pain
Cases/patient Time 3 tier External Examples
UNRESPONSIVE WITH UNSTABLE VS
→ Cardiac arrest
→ Cervical SCI - phrenic nerve which is
Life threatening
responsible for the control of respiration
ABCD, low Immediate Emergent Black
(diaphragm)
survival
• Neck brace is important
→ Fixed/ unequal pupils
→ Blood/fluid loss >60%
UNRESPONSIVE WITH STABLE VS
→ Chest pain
→ Chest injuries
→ Blood/fluid loss 40-60%
LT condition, high → SCI below the cervical
15-30 min Emergent Red
survival → Cerebral embolism- Stroke
→ Cardiac embolism -possible angina/MI
→ Pulmonary embolism- rashes/petechiae at the
chest
→ Flat bone fracture as it can lead to bleeding
Non-LT, but → Stable head/eye/ear/ abdominal injuries
treatment needed <2 hours Urgent Yellow → Blood/fluid loss <40%
ASAP → Fractures
AMBULATORY
Non-LT, treatment Non-urgent/TIA → Sprain
<24 hours Green
non-ASAP - May go home → Strain
→ Minor cuts or bruises
GOALS OF EMERGENCY CARE •
Activate the plan! - Incidence Command System
→ Prevent injury- Mitigation/Preparedness phase (The plan is activated when there is an increase of
→ Preserve life- Response admissions)
→ Promote recovery- Recovery phase • Priority: Physio over Psycho, TRIAGE!
4. Recovery - post disaster
DISASTER PHASES MANAGEMENT • Promote rehabilitation
1. Mitigation - before disaster • Priority: Physio over Psycho
• Lessen the damages and loss of life • After physio is stabilized, psych first aid
• Focused on architectural adjustments (e.g., o Diffusion- done in the first 36 hours, informal
earthquake proof buildings), urban planning, psychological help (all have the capacity to be
information dissemination therapeutic)
2. Preparedness - before disaster o Debriefing- done after 36 hours, formal help
• Create a plan to determine roles, leaders, (done by professionals)
intercommunication ▪ Prevent PTSD, suicide, depression
• Training and drills - most expensive phase
3. Response - intra disaster
PRINCIPLES OF EMERGENCY CARE •Chin lift- (-) cervical injury; best way to open airway;
→ Assess applied if there is no situation
• Patient status and environment for SAFETY (The • Tubes
patient and nurse should be safe!) o Oropharyngeal/mouth guard - contraindication
→ Ask for help first (team approach); outside - activate if with (+) gag, vomiting, aspiration risk, (+)
EMS (emergency medical services) or ERS (emergency facial trauma
response services) ▪ Inserted upward → downward
• Ask for resources ▪ Downward can cause injury to the hard
• It is safer if there are more resources palate
→ Intervene ▪ (+) facial trauma- can aggravate injury
• Based on assessment o Nasopharyngeal - contraindicated (+) CSF
• Stabilize the patient leakage
→ Do no harm - non-malfeasance ▪ Sign of basilar/skull fracture
→ Advanced - longer tubes, direct to the lungs; done by
TYPES OF SURVEY AND ASSESSMENT MD
→ Primary Survey: Rapid • Laryngeal tube - if not available proceed to ET
• Goal: Establish the priority problem (to determine • Endotracheal tube
the priority intervention) • Tracheostomy - last resort because it is most
• Disadvantage – incomplete invasive
o Initial assessment, unstable client (lesser time
to assess) EMERGENCY MANAGEMENT - BLS
• After primary survey → primary intervention (to
stabilize the patient) Respiratory Arrest (-RR, +PR, UNRESPONSIVE)- rescue
• Airway, Breathing, Circulation, Disability breathing
(neurologic) → Bag valve mask (ambu bag) ideally
• IF CARDIAC ARREST: CompressionAB
• Primary check is LOC
o Responses (AVPU- alert verbal pain
unresponsive)
• (-) BVM: one way valve or face shield is ideal
o GCS takes time to obtain
• Demographics
o Name
o Mouth to mouth is not recommended
o Contact person
o Religion- to know contraindications (e.g., → Adult and advanced airway
Jehovah’s witness) • E.g., advanced airway: with tracheostomy, 5 years
• Pulse checking: old- 10 rescue breaths
o Adult/Child - carotid • Frequency: 10/min, 1 breath/6sec (too much may
o Infant - Brachial compress the heart)
• RR check - rise and fall of the chest → Children - 12/min, 1 breath/5sec
• Skin check for perfusion • If vomiting is present, stop → left side lying →
o Pallor suction
o Cyanosis • Vomiting could lead to aspiration
o Jaundice
→ Secondary Survey: complete and thorough Cardiac Arrest (-PR, -RR, UNRESPONSIVE) - SARAP
• Disadvantage – takes time → Survey scene/responder
• Done after stabilization → Announce/introduce self
• Assess Cephalocaudal- head to toe → Response
• Baseline VS, GCS → Activate ERS
• History of complaint → Pulse and respiration check- within 10 seconds to
• Diagnostics and laboratory prevent delay in CPR
→ CPR- push hard and fast
EMERGENCY MANAGEMENT - AIRWAY • INTERVENE: compress q 2min
→ Airway management- basic/advanced • RATE: 120 max (100-120/min)
→ Basic - easy to perform, done by RN, BLS, jaw thrust, • QUALITY: push hard and fast
chin lift • ADULT: 30 compressions: 2 breathing
• Jaw thrust- (+) cervical injury to maintain the neck o 2-man pedia rescue - 15:2
at neutral position; hit by a vehicle • LANDMARK: lower half of sternum
o Lock elbows in place
o Allow chest recoil FIRST AID MANAGEMENT: MARINE STINGS
• HAND POSITION: → Consequence: Severe inflammation
o Adult (>9yo): 2 hands → Signs and Symptoms:
o Child (1-8yo): 1 hand • Itching
o Infant: 2 fingers (index & middle or both • Redness
thumbs) • Swelling
• DEPTH: • Redness
o Adult: 2-2.4 inches • Warm sensation
o Child: max 2 inches → Management:
o Infant: max 1.5 inches 1. Flush with saline water
• Stop CPR if: 2. Apply acetic acid (vinegar)
• Defibrillation: pulseless, vtach, vfib 3. Warm compress
• Exhausted
• ERS arrival FIRST AID MANAGEMENT: SNAKE BITES
• Physician declared death of px → Consequence: Blood clots, respiratory depression
• Px is revived/Return of Spontaneous Circulation → Venomous Snake:
(ROSC) • Triangular head
o (+) HR • Pit nostril for heat senses
o No RR, stop CPR → rescue breathing • Stir/vertical eyes
• With fangs
FIRST AID MANAGEMENT: HEMORRHAGE
→ TYPES:
• Arterial – bright red, spurting
o Oxygenated blood, ↑pressure
• Venous – dark red, oozing (↓pressure)
→ Management:
→ Management:
• Do not suck the site
1. Wear gloves to protect self from infections
• Do not cut
2. Apply pressure (tourniquet is allowed for severe
bleeding) • No warm or cold compress
3. Elevate the site to promote venous return o Cold compress will restrict blood flow
4. PNSS for BT o Warm compress → vasodilation → rapid blood
▪ Universal donor: O- flow → rapid spread of toxin
• Allow constrictive bands
FIRST AID MANAGEMENT: ANIMAL BITES - Dogs, Cats, • Proper management: Priority is safety
Bats 1. Lower the site
→ Consequence: Rabies, Tetanus 2. Immobilize to prevent flow of toxin
• Rabies - dangerous: neck 3. Clean the wound
4. Anti-venom ASAP (SE: arthralgia)
• Tetanus came from soil
→ Signs and Symptoms:
FIRST AID MANAGEMENT: POISONING
• Bite marks
→ Consequence: depends on the poison
• Swelling
• Common: Toddler - they explore via mouth
• Redness
→ Prevention:
→ Management: Anti Rabies/Anti Tetanus
• Avoid storage of poison at food containers
• GOAL: To slower down the movement of the
• Lock poison at cabinet out of children’s reach
tetany
→ Management: If (+) poisoning
1. Lower site
2. Immobilize • Do not stimulate vomiting- avoid emetics (syrup of
3. Cold compress ipecac) d/t risk of aspiration
4. Klean the wound • Position the client left side lying to prevent gastric
emptying (prevent absorption in the intestines)
FIRST AID MANAGEMENT: BEE STINGS • Assess type of poison and amount - call poison
→ Consequence: center
• Allergic - antihistamine • Activated charcoal - 1-2g/kg every 4-8 hours/ burnt
• Anaphylactic - epinephrine > bronchodilator > bread
steroids • Gastric lavage - within 4 hours
→ Signs and Symptoms: • Chelation therapy - blood cleansing (via binding
• Swelling agent - succimer/chemet); if the poison reached
the blood already
• Redness
• Itchy Skin
COMMON ANTIDOTES
→ Management:
→ Anticholinergics SNS - cholinergics PSNS
• PRIORITY: Remove stinger, scrape with card
→ Acetaminophen - N acetylcysteine
1. Lower site
→ Benzodiazepine - flumazenil
2. Immobilize
3. Cold compress → Beta blockers - glucagon
4. Klean the wound (first thing to do) → Calcium channel blockers - glucagon
→ Digoxin - digibind/digifab
→ Heparin - protamine sulfate
→ Iron - defuroxime
→ Magnesium sulfate - calcium gluconate
→ Nitrate - methylene blue
→ Opioid - naloxone
→ Thrombolytics - aminocaproic acid
→ Warfarin - vitamin K, green leafy vegetables
You might also like
- Bengkalis Muria - Jurnal Khusus - Hanifah Hilyah SyahDocument9 pagesBengkalis Muria - Jurnal Khusus - Hanifah Hilyah Syahreza hariansyahNo ratings yet
- Energy Audit of KCC Traction Substation, VijaywadaDocument2 pagesEnergy Audit of KCC Traction Substation, Vijaywadathailamuthu100% (1)
- Emergency and Disaster NursingDocument7 pagesEmergency and Disaster NursingencarguezpaolochelNo ratings yet
- UntitledDocument4 pagesUntitledHannah AmerolNo ratings yet
- Vascular NotesDocument5 pagesVascular NotesAstha Tusharbhai PatelNo ratings yet
- BURNSDocument14 pagesBURNSRIAH BILLANESNo ratings yet
- Gram Negative Bacilli - RespiratoryDocument4 pagesGram Negative Bacilli - RespiratoryrefuapalackyNo ratings yet
- Madrid Surg Notes IntDocument5 pagesMadrid Surg Notes IntdoctorcreepticNo ratings yet
- DV 1Document32 pagesDV 1Mujahidin ArismanNo ratings yet
- Anestesi (Farmakologi)Document15 pagesAnestesi (Farmakologi)Nurul AzizahNo ratings yet
- Burn Depth Characteristics: 1800 ALFREDDocument1 pageBurn Depth Characteristics: 1800 ALFREDNadhila A ByantNo ratings yet
- PA HyperthyroidismDocument7 pagesPA HyperthyroidismEben Alameda-PalapuzNo ratings yet
- Estimated Time of Death:: Cooling of The BodyDocument2 pagesEstimated Time of Death:: Cooling of The BodynoramalinaabdmanafNo ratings yet
- The Immortal SealDocument2 pagesThe Immortal Sealelderfc.librasNo ratings yet
- Kompre Mei 2022 BG RoyDocument74 pagesKompre Mei 2022 BG RoyputriaulianifNo ratings yet
- Pharmacology Exam 2Document3 pagesPharmacology Exam 2Joelle DwekNo ratings yet
- Pressure InjuriesDocument1 pagePressure InjuriesPaola OrtizNo ratings yet
- Inflammatory Diseases of The Skin: M. Angelica Selim, M.D. Dermatopathology Unit Pathology DepartmentDocument53 pagesInflammatory Diseases of The Skin: M. Angelica Selim, M.D. Dermatopathology Unit Pathology DepartmentIsaac MaderoNo ratings yet
- Inflammatory Diseases of The Skin: M. Angelica Selim, M.D. Dermatopathology Unit Pathology DepartmentDocument53 pagesInflammatory Diseases of The Skin: M. Angelica Selim, M.D. Dermatopathology Unit Pathology DepartmentDr Jyotiprakash ChoudhuryNo ratings yet
- The Change The World Board Game: Grammar ReviewDocument2 pagesThe Change The World Board Game: Grammar Reviewlees10088No ratings yet
- Anatomy 2Document1 pageAnatomy 2Casey Rae YanoNo ratings yet
- Bimbingan 7Document4 pagesBimbingan 7sean 102018039No ratings yet
- Bedah 2 Dr. UswaDocument36 pagesBedah 2 Dr. UswaSiq Febri SmnjtkNo ratings yet
- Ent Chanting by DR - ParasDocument34 pagesEnt Chanting by DR - ParasSaravanan DevarajNo ratings yet
- Me 1Document39 pagesMe 1Mansi BansalNo ratings yet
- Name: - LRNDocument2 pagesName: - LRNjrose fay amatNo ratings yet
- 1990s MB - SpreadDocument3 pages1990s MB - SpreadBruno SouzaNo ratings yet
- (DRM) 1.06A Papulosquamous Diseases (Dra. Paliza and Dra. Ismael)Document7 pages(DRM) 1.06A Papulosquamous Diseases (Dra. Paliza and Dra. Ismael)Jolaine ValloNo ratings yet
- OrtopedieDocument40 pagesOrtopedieNaomi CurcanuNo ratings yet
- PlatyhelminthesDocument7 pagesPlatyhelminthesAbhijeet AdhikaryNo ratings yet
- Resumen de Fonetica-Primer CuatrimestreDocument18 pagesResumen de Fonetica-Primer CuatrimestreGonzalo MenaNo ratings yet
- ArthropodsDocument2 pagesArthropodsJulia IshakNo ratings yet
- Kukel WerdDocument3 pagesKukel WerdRicky YurdanaNo ratings yet
- Integumentary SystemDocument7 pagesIntegumentary SystemJOANNA MARIE INVENTORNo ratings yet
- Most Important Questions: Digestion & Absorption Breathing & Exchange of GasesDocument112 pagesMost Important Questions: Digestion & Absorption Breathing & Exchange of GasesRana RikNo ratings yet
- Most Important Questions: Digestion & Absorption Breathing & Exchange of GasesDocument112 pagesMost Important Questions: Digestion & Absorption Breathing & Exchange of GasesRana RikNo ratings yet
- Ent Quick RecapDocument33 pagesEnt Quick Recapshanurajput0No ratings yet
- Integumentary System Reviewer PDF Skin Nail (Anatomy) 2Document1 pageIntegumentary System Reviewer PDF Skin Nail (Anatomy) 2Shiem TrabocNo ratings yet
- CP SynapsesDocument7 pagesCP Synapsespotro patoNo ratings yet
- Dermatology ConditionsDocument8 pagesDermatology ConditionsmeilunlyNo ratings yet
- Flat Raised/ Depressed Raised DepressedDocument6 pagesFlat Raised/ Depressed Raised DepressedMaida PootNo ratings yet
- All Hormones & Disorders - One ShotDocument62 pagesAll Hormones & Disorders - One Shotsalmasaleha806No ratings yet
- Poster (Healable)Document1 pagePoster (Healable)ppnidpk rsumNo ratings yet
- A Wound With Coagulative Necrosis Is Called Burn. A Burn Is A Wound in Which There Is Coagulative Necrosis of The TissueDocument17 pagesA Wound With Coagulative Necrosis Is Called Burn. A Burn Is A Wound in Which There Is Coagulative Necrosis of The Tissuewww nambisons comNo ratings yet
- PikaduraDocument4 pagesPikaduraVictor EduardoNo ratings yet
- Autonomic Nervous System 05 Class Notes MBBS Prof 2nd YearDocument27 pagesAutonomic Nervous System 05 Class Notes MBBS Prof 2nd YeardevNo ratings yet
- Gyne Notes Infections 01Document2 pagesGyne Notes Infections 01kirsten evidenteNo ratings yet
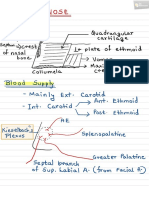
- Nose PDFDocument6 pagesNose PDFNiranjanPandeyNo ratings yet
- EarthwormDocument24 pagesEarthworm10306anshkumarNo ratings yet
- Solutions To Thomas' Calculus Early Transcendentals (9780134439020), Pg. 1031, Ex. 22 Homework Help and Answers SladerDocument1 pageSolutions To Thomas' Calculus Early Transcendentals (9780134439020), Pg. 1031, Ex. 22 Homework Help and Answers SladerNutthanon HwungsawartNo ratings yet
- Ion ChannelsDocument8 pagesIon Channelspotro patoNo ratings yet
- 7 Oragn SystemsDocument11 pages7 Oragn SystemsTobit Andre CaballoNo ratings yet
- Derma 21 Dermatoses From Physical Factors NutritionDocument5 pagesDerma 21 Dermatoses From Physical Factors NutritionKrisha BalorioNo ratings yet
- 2400 Zone v1.2 SinglesDocument4 pages2400 Zone v1.2 SinglesshimmyNo ratings yet
- Pediatric Nursing: Immediate Care For Newborn (OLD)Document8 pagesPediatric Nursing: Immediate Care For Newborn (OLD)KristaRicaAbayabayNo ratings yet
- MIX Reviewer 2022Document54 pagesMIX Reviewer 2022shaikha.amariNo ratings yet
- ANAPHY - Midterms ReviewerDocument15 pagesANAPHY - Midterms ReviewerTiffany WongNo ratings yet
- Health AssessmentDocument48 pagesHealth AssessmentVorgy Bench SantiagoNo ratings yet
- Part I Travel Documents Issued by Third Countries and Territorial Entities en 0Document124 pagesPart I Travel Documents Issued by Third Countries and Territorial Entities en 0drlazyboyNo ratings yet
- FrogDocument65 pagesFrognarayan sahNo ratings yet
- Reasoning and Logic - Lesson 2Document10 pagesReasoning and Logic - Lesson 2Nehal GaurNo ratings yet
- Bohren Et Al Lancet MH Series 4 2023Document12 pagesBohren Et Al Lancet MH Series 4 2023Thierry UhawenimanaNo ratings yet
- Vistamore SDN BHD Project Quality Plan Section 1Document8 pagesVistamore SDN BHD Project Quality Plan Section 1Wan Mohamad Noor Hj IsmailNo ratings yet
- Sheet 6 Electronics - AnswerDocument10 pagesSheet 6 Electronics - AnswerOla SamirNo ratings yet
- Therapeutic Approaches: Indian School MuscatDocument10 pagesTherapeutic Approaches: Indian School MuscatNidhee SharmaNo ratings yet
- Finance AssignmentDocument7 pagesFinance AssignmentMeshack MateNo ratings yet
- Committee Opinion No 664 Refusal of Medically.45Document8 pagesCommittee Opinion No 664 Refusal of Medically.45w yNo ratings yet
- Factors That Affect Time Management of Humanities and Social Sciences Grade 11 Senior High School StudentsDocument8 pagesFactors That Affect Time Management of Humanities and Social Sciences Grade 11 Senior High School StudentsCamile IgnacioNo ratings yet
- Cuaderno de Actividades: Programa Nacional de InglésDocument5 pagesCuaderno de Actividades: Programa Nacional de InglésIselina RNo ratings yet
- Red Bull Copy Paste NetDocument6 pagesRed Bull Copy Paste NetNives AmbrožičNo ratings yet
- Adsorption of Acetic Acid On Charcoal SurfaceDocument3 pagesAdsorption of Acetic Acid On Charcoal SurfaceFrankyFan90% (10)
- 5 Structural Geology March 2019Document117 pages5 Structural Geology March 2019thamirad100% (2)
- Total Brochure UK LoRes 0609 PDFDocument32 pagesTotal Brochure UK LoRes 0609 PDFMohammed RayanNo ratings yet
- PG Medical Admitted Candidates Combined Rank WiseDocument8 pagesPG Medical Admitted Candidates Combined Rank WiseNimesh SommanekNo ratings yet
- Comparative Study of Different Waste Biomass For Energy ApplicationDocument6 pagesComparative Study of Different Waste Biomass For Energy Applicationvitor_alberto_7No ratings yet
- I Am DepressedDocument8 pagesI Am DepressedwisgeorgekwokNo ratings yet
- Electrodes For Titration PDFDocument2 pagesElectrodes For Titration PDFjhuampeNo ratings yet
- Braintech Engineers PVT LTDDocument8 pagesBraintech Engineers PVT LTDMANVENDRA SINGHNo ratings yet
- CLC 18-10Nb: A NB Stabilized 18Cr-10Ni Austenitic Stainless Steel (347 Grade)Document4 pagesCLC 18-10Nb: A NB Stabilized 18Cr-10Ni Austenitic Stainless Steel (347 Grade)PeterWayNo ratings yet
- January: Date Company NameDocument20 pagesJanuary: Date Company NameMatthewNo ratings yet
- N-Channel Enhancement Mode MOSFET: Product SummaryDocument5 pagesN-Channel Enhancement Mode MOSFET: Product Summaryserrano.flia.coNo ratings yet
- Universiti Teknologi Mara Final Examination: Confidential AS/MAR2012/PHY310Document9 pagesUniversiti Teknologi Mara Final Examination: Confidential AS/MAR2012/PHY310luminousspaceNo ratings yet
- Course Syllabus in SuccessionDocument16 pagesCourse Syllabus in SuccessionCharina BalunsoNo ratings yet
- Embragues para Motores EstacionariosDocument12 pagesEmbragues para Motores EstacionariosJiyaYsqn100% (1)
- West Nile Virus Associated With Equid Encephalitis in Brazil, 2018Document10 pagesWest Nile Virus Associated With Equid Encephalitis in Brazil, 2018Monica Shinneider de SousaNo ratings yet
- Project Fianace 1Document46 pagesProject Fianace 17karswapnilNo ratings yet
- SAMAP 15 ProceedingsDocument84 pagesSAMAP 15 ProceedingsOm Parkash SharmaNo ratings yet
- Income Tax NotesDocument18 pagesIncome Tax NotesVikash kumarNo ratings yet
- Motives IDocument10 pagesMotives Imerin sunilNo ratings yet