Professional Documents
Culture Documents
Eent Midterms
Eent Midterms
Uploaded by
David Dwane Art SilorioCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Eent Midterms
Eent Midterms
Uploaded by
David Dwane Art SilorioCopyright:
Available Formats
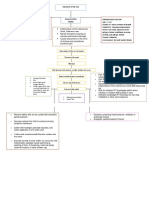
NCM116j - EENT Midterms
Based on the discussion by Ms. Elsie P. Miguel, RN MN
LENS
Module 1 Anatomy of the Eyes - Sits directly behind the pupil
- This is a clear layer that focuses the light the
pupil takes in
- Held in place by the ciliary muscles, which
allow the lens to change shape depending on
the amount of light that hits it so it can be
properly focused
CILIARY BODY AND MUSCLE
- The ciliary body is a part of the eye that
includes the ciliary muscle, which controls
the shape of the lens, and the ciliary
epithelium, which produces the aqueous
humor
SCLERA
- The ciliary body is a ring-shaped tissue that
- Commonly referred to as the “whites” of the
holds and controls the movement of the eye
eye
lens, and thus, it helps to control the shape of
- A smooth, white layer on the outside, but the
the lens
inside is brown and contains grooves that
help the tendons of the eye attach properly
CONJUNCTIVA
- Provides structure and safety for the inner
- These are layers of mucus which help keep
workings of the eye, but is also flexible so that
the outside of the eye moist
the eye can move to seek out objects as
- If the eye dries out it can become itchy and
necessary
painful
- It can also become more susceptible to
IRIS
damage or infection
- The area of the eye that contains the pigment
which gives the eye its color
- If the conjunctiva glands become infected the
- This area surrounds the pupil and uses the
patient will develop “pink eye”
dilator pupillae muscles to widen or close the
pupil
RETINA
- Allows the eye to take in more or less light
- The light focused by the lens will be
depending on how bright it is around you
transmitted onto the retina
- If it is too bright, the iris will shrink the pupil
- This is made of rods and cones arranged in
so that they eye can focus more effectively
layers, which will transmit light into chemicals
and electrical pulses
CORNEA
- The retina is located in the back of the eye,
- The outer covering of the eye
and is connected to the optic nerves that will
- This dome-shaped layer protects your eye
transmit the images the eye sees to the brain
from elements that could cause damage to
so they can be interpreted
the inner parts of the eye
- There are several layers of the cornea,
OPTIC NERVE
creating a tough layer that provides
- The optic nerve is located in the back of the
additional protection
eye
- These layers regenerate very quickly, helping
- The optic nerves relay messages from your
the eye to eliminate damage more easily
eyes to your brain to create visual images
- The cornea also allows the eye to properly
focus on light more effectively
MACULA
- Those who are having trouble focusing their
- The macula is located near the center of the
eyes properly can have their corneas
retina; its function is to process harp, clear,
surgically reshaped to eliminate this problem
straight-ahead vision
PUPIL
VITREOUS BODY
- Appears as black dot in the middle of the eye
- The vitreous humor is the gel located in the
- This black area is actually a hole that takes in
back of the eye which helps it hold its shape
light so the eye can focus on the objects in
front of it
Compiled by Rikko Angelo Alganion
NCM116j - EENT Midterms
Based on the discussion by Ms. Elsie P. Miguel, RN MN
- This gel takes in nutrients from the ciliary REFRACTIVE MEDIA
body, aqueous humor and the retinal vessels ● CORNEA- is the transparent layer that forms
so the eye can remain healthy the external coat of the anterior portion of
- When debris finds its way into the vitreous the eye
humor, it causes the eye to perceive “floaters,” ● AQUEOUS HUMOR - watery fluid filling the
or spots that move across the vision area that eye’s anterior chamber that serves as
cannot be attributed to objects in the refracting medium and maintains hydrostatic
environment intraocular pressure (IOP)
● LENS - biconvex crystalline body located
behind the pupil that changes shape for
Module 2 Eyes accommodation
● VITREOUS HUMOR - jelly-like substance
IMPORTANT FUNCTION filling the posterior cavity behind the lens,
Vision depends on a complex coordination of ocular maintaining the shape of the eye
structures that mediate passage of light rays reflected
from an external object to PHYSICAL EXAMINATION
the retina and transmit INSPECTION
visual images to the brain - Eye: symmetry, color, pupil size
for interpretation. - PERRLA (Pupils are equal, round and reactive
-PROVIDE A PATHWAY to light and accommodation)
FOR VISUAL STIMULI - Lacrimal apparatus: nontender
- Visual acuity: 20/20 OU (both eyes),
Consists of layers/coats: - No diplopia
➢ Outer, protective layer - Conjunctiva clear; sclera white
➢ Middle, vascular layer - EOMI: extraocular movements intact
➢ Inner, neural layer - Retinal vessels normal; no hemorrhages, spots
➢ Refractive media or patches
PALPATION
OUTER (Protective Layer) - Check eyelids for nodules
● SCLERA - white, opaque, fibrous connective - Palpate the eye by gently pushing into the
tissue orbit without discomfort
● CORNEA – anterior continuation of the sclera, OCULAR HISTORY
which is transparent and avascular - Elicit a description of the present illness and
chief complaint.
MIDDLE (Vascular Layer) - Explore the client’s health history for risk
● CHOROID – is a thin, pigmented membrane factors.
containing blood vessels that supply eye ● What does the patient perceive to be the
tissues problem?
● CILIARY BODY – anterior continuation of the ● Is visual acuity diminished?
choroid containing muscles that change the ● Does the patient experience blurred, double,
shape of the lens to focus vision or distorted vision?
● IRIS- is the central extension of the ciliary ● Is there pain? Is it sharp or dull? Is it worse
when blinking?
● Are both eyes affected?
● Is there a history of discharge? If so, inquire
about color, consistency and odor.
● Describe the onset of the problem. Is it
worsening?
INNER (Neural Layer)
● RETINA – contains layers of nerve cells,
including rods and cones, that translate light
waves into neural impulses for transmission to
the brain.
Compiled by Rikko Angelo Alganion
NCM116j - EENT Midterms
Based on the discussion by Ms. Elsie P. Miguel, RN MN
Plates are bound together in a booklet. Each
DIAGNOSTIC TESTS plate of the booklet are dots of primary colors
VISUAL ACUITY that are integrated into a background of
Snellen Chart secondary colors. The dots are arranged in
- Cover one eye simple patterns
- Client identify - Diminished color vision - unable to identify
the letters (at hidden shapes
any line) - Central vision conditions - difficulty
- Repeat for the identifying colors
second eye
- Record visual TONOMETRY
acuity Measures IOP to screen
designated by for and manage
that line glaucoma. The device
used for measuring IOP
VISUAL is an accurately
ACUITY calibrated applanation
Tested for tonometer, which
both (14 measures the pressure
inches away) needed to flatten the cornea.
distance and - Topical anesthesia is given prior test, since
(20 feet the probe touches the highly sensitive cornea
away) vision, - AVOID squeezing the eyelids, holding their
and is breath, or performing
performed - Valsalva - may increase IOP
on each eye
SLIT-LAMP
separately with a standard EXAMINATION
Snellen chart for distance and Binocular microscope
a Rosenbaum pocket screener mounted on a table,
for near vision. enables the user to
examine the eye with
Tumbling “E”, “illiterate E”, magnification of 10 to
number or picture chart is used 40 times the real
if the person is illiterate or image. It can be broad
unable to read the English to a narrow beam of light for different parts of the
alphabet eye.
EXAMPLE DOCUMENTATION OPHTHALMOSCOPY
A patient reads all five letters from the 20/20 line on Provides a magnified view
the Snellen Chart with the right eye (OD) and three of of the retina and optic
the five letters on the 20/30 line with the left eye nerve with the use of a
(OS); the visual acuity is documented as OD 20/20 light.
and OS 20/30 - Exam of optic disc
or posterior of
If the patient cannot see the big “E” at the top of the eyeball.
chart, the examiner should determine if the patient
can count fingers. CF/3 ft
DIAGNOSTIC EVALUATION
COLOR VISION TESTING EXTERNAL EYE EXAMINATION
(Ishihara Polychromatic Symmetry and placement of eyelids, pupils and
Plates) muscles. CNs III, IV and VI - control movement and
- Can be used to pupil size.
establish whether
a person’s color ECTROPION - Outwardly turned lower lid
vision is within ESOTROPIA - Eye turns inward
normal range. EXOTROPIA - Eye turns outward
Compiled by Rikko Angelo Alganion
NCM116j - EENT Midterms
Based on the discussion by Ms. Elsie P. Miguel, RN MN
PTOSIS - Drooping eye BALANCE- essential for maintaining body movement,
EXOPHTHALMOS - Protruding eyeballs and retracted position and coordination.
eyelids
ECTROPION
It is a condition in
which your eyelid
turns outward. This
leaves the inner
eyelid surface
exposed and prone
to irritation. Ectropion is more common in older
adults, and it generally affects only the lower eyelid.
ENTROPION
A condition where the
eyelid folds inwards.
This results in the skin
and eyelashes rubbing
the eyeball causing
irritation and
discomfort.
Eye drop Administration
STRUCTURES OF THE EAR
- Instill 1 or 2 drops in
The ear is divided into three parts:
the middle of the
- External
lower conjunctival
- Middle
sac
- Internal Ear
- Do not allow tip of
applicator to come
EXTERNAL EAR
in contact with the
The external ear is composed of the following
eye
structures:
- Do not drop directly on the cornea
1. Auricle or pinna
- Close eyes gently
2. External auditory canal (ear canal)
AURICLE
Module 3 Structures of the Ear Composed of cartilage, (except for the fat and
subcutaneous tissue in the earlobe), collects sound
waves and directs vibrations into the external
auditory canal.
EXTERNAL AUDITORY CANAL
Approx. 2-3cm long, ends at the tympanic membrane
skin of the canal contains hair, sebaceous glands and
ceruminous glands, which secrete a brown, wax like
substance called cerumen
MIDDLE EAR
1. Tympanic Membrane
2. Ossicles
IMPORTANT FUNCTION TYMPANIC MEMBRANE
Delicate-sensory organ with the dual function of EARDRUM, pearly gray and translucent, has three
hearing and balance. layers of tissue - outer layer, middle layer and inner
HEARING- essential for normal development and layer.
maintenance of speech, and ability to communicate - Pars tensa – 80% composed of all three layers
with others. - Pars flaccida- 20% lacks middle layer
Compiled by Rikko Angelo Alganion
NCM116j - EENT Midterms
Based on the discussion by Ms. Elsie P. Miguel, RN MN
- Inspect for size, symmetry, and angle of
OSSICLES attachment to the head.
Contains the three smallest bones - malleus, incus - N: no pain noted during manipulation of the
and stapes, assisting in the transmission of sound. auricle, otherwise presence of acute external
Footplate of the stapes transmits sound to the inner otitis is suspected
ear.
1. Ossicles (Malleus, Incus, Stapes) WHISPER TEST
Mechanically transmitting sound was the tympanic - Cover the untested ear with the palm of the
membrane through the oval window to the inner ear. hand → examiner whispers softly from a
distance of 1-2 feet from the unoccluded ear
2. Windows and out of patient’s sight
The middle ear contains 2 windows who reflect their - N: patient can correctly repeat what was
shape. whispered
- Round window – is an opening in the inner
ear from which the sound vibrations exit.
- Oval window – is an opening in the inner ear
into which sound vibrations
3. Eustachian tube (Auditory tube)
Provides air passage from the naso to the middle ear.
During yawning, sneezing and swallowing, the
palatine muscle opens the tube to equalize pressure
on both tympanic membrane.
TEST FOR AUDITORY ACUITY TEST
4. Mastoid
1. Rinne – compares air conduction to bone
These are air-filled spaces that aid the middle ear in a
conduction to help differentiate conductive
changes in pressure.
from sensorineural hearing loss
2. Weber – to assess conduction of sound
INNER EAR
through bones
It is housed deep within thetemporal bone. Organs
for hearing (cochlea), balance (semicircular canal),
RINNE TEST
nerve cranial VII (facial nerve) and VIII
Tuning Fork Test
(vestibulocochlear nerve)
- Distinguish between conductive and
sensorineural hearing loss
Cochlea and semicircular canals are housed in the
- Activated tuning fork: mastoid bone and in
bony labyrinth → surrounds the membranous
front of the ear
labyrinth, bathed in a fluid called perilymph.
- Examiner shifts the stem of a vibrating tuning
fork between two positions: 2 inches from the
• Bony labyrinth
opening of the ear canal (AC) and against the
• 3 Semicircular canals: organ of balance
mastoid bone (BC)
• Cochlea: organ of Corti, receptor for hearing
- As the position changes, the patient is asked
to indicate which tone is louder or when the
DIAGNOSTIC TESTS
tone is no longer audible.
OCULAR HISTORY
- Elicit a description of the present illness and
chief complaint.
- Explore the client’s health history for risk
factors.
- Ear Pain(Otalgia)
- Hearing Loss
- Vertigo
- Tinnitus (ringing in the ears)
- Ear drainage (Otorhea)
- Infection N: air-conducted sound is louder than the
bone-conducted sound.
ASSESSMENT
INSPECTION WEBER TEST
- Inspect for deformities, lesions and discharge - Useful for detecting unilateral hearing loss
Compiled by Rikko Angelo Alganion
NCM116j - EENT Midterms
Based on the discussion by Ms. Elsie P. Miguel, RN MN
- Uses bone conduction to test lateralization DIAGNOSTIC EVALUATION
of sound AUDIOMETRY
- Grasp it firmly by its stem and tapping it on - Single most important diagnostic instrument
the examiner’s knee or hand, then place on - PURE-TONE - sound stimulus consists of a
the patient’s head or forehead pure or musical tone
- N: hears the sound equally in both ears, or - SPEECH AUDIOMTERY - spoken word is used
describes the sound as centered in the middle to determine ability to hear
of the head.
FREQUENCY - refers to the number of sound
waves emanating from a source per second, or
Hertz
PITCH - describes frequency (tone with 100Hz is
low pitch, 10,000Hz is high pitch)
INTENSITY - measures loudness in decibel (dB)
AUDIOMETRY
- Screening test for hearing loss and diagnostic
test to determine degree and type of hearing
loss.
CONDUCTIVE HEARING LOSS - hears the sound
better in the affected ear
SENSORINUERAL HEARING LOSS- hears the
sound in the better-hearing ear
COMPARISON OF WEBER AND RINNE TESTS CALORIE TEST STIMULATION
- Done by an ear irrigation of cold or warm
Hearing Status Weber Rinne
water
Normal Sound is heard Air conduction - Pre and Post Procedure - Obeserve for
Hearing in both ears is audible nystagmus, nausea and vomiting
longer than
bone
conduction in
both ears
Conductive Sound is heard Sound is best
Hearing loss best in affected heard as long
ear (hearing or longer in
loss) affected ear
OTOSCOPY
(hearing loss)
- Examination of external ear and tympanic
Sensorineural Sound is heard Air conduction membrane with the use of otoscope
Hearing loss best in normal is audible
hearing ear longer than
bone
conduction in
affected ear
Compiled by Rikko Angelo Alganion
NCM116j - EENT Midterms
Based on the discussion by Ms. Elsie P. Miguel, RN MN
EAR IRRIGATION
- Common solutions:
1. Waram tap water or NSS
2. Glycerin and water, hydrogen peroxide
- The microphone on the outside of the hearing
aid picks up sound from the air as it enters
the ear and converts sound waves into digital
signals
- The amplifier strengthens the digital signals
- The speaker converts the digital signals into
vibrations that then pass through the inner
ear to the brain
- A tiny battery powers the hearing aid
- A microchip - a miniature computer that
helps us tune and personalize your hearing
aid to your individual needs
- Visually inspect external ear with otoscope
- Temp: near body temp (37 C)
- To soften cerumen, add mineral oil drops or
hydrogen peroxide
- Position patient on the side with the affected
ear uppermost
- Rubber bulb syringe or water pressure device
- Adult: pull up;
- Child: pull down
- Direct water flow toward the top of ear
- STOP: if nausea, vomiting, dizziness
HEARING AIDS
- Keep dry; do not wet while bathing or
swimming
- Avoid: hair spray, cosmetics, oils around ear
- Keep extra batteries on hand
- Turn off the hearing aid when not in use.
- Avoid exposing to extremes temp
- Clean ear mold part with mild soap and water;
do not get it excessively wet
- Clean cerumen (middle part)
Compiled by Rikko Angelo Alganion
You might also like
- 1 - Principles of Hearing Aid AudiologyDocument350 pages1 - Principles of Hearing Aid AudiologyCarlos GoodwinNo ratings yet
- Ent MCQ A PFD PDFDocument61 pagesEnt MCQ A PFD PDFKay Bristol0% (1)
- Opto Reviewe2Document8 pagesOpto Reviewe2isseylimboNo ratings yet
- Eye AnatomyDocument4 pagesEye AnatomyILAH REANNIE ENRIQUEZNo ratings yet
- 5 Assessment and Diagnostic Procedures For Visual and Eye DisordersDocument5 pages5 Assessment and Diagnostic Procedures For Visual and Eye DisordersNica EnriquezNo ratings yet
- ATENGCO - Activity11 The Sense OrgansDocument8 pagesATENGCO - Activity11 The Sense OrgansJoann Mae PudaderaNo ratings yet
- 5 - The Visual System and Mechanisms of PerceptionDocument13 pages5 - The Visual System and Mechanisms of PerceptionElmer SalazarNo ratings yet
- Special Senses 1Document14 pagesSpecial Senses 1Juan Miguel TevesNo ratings yet
- 5 Special SensesDocument8 pages5 Special SensesEdel GapasinNo ratings yet
- Human Eye and The Colourful WorldDocument12 pagesHuman Eye and The Colourful WorldSuchita JhaNo ratings yet
- Our Sense of Sight and LightDocument6 pagesOur Sense of Sight and LightnorafaizalNo ratings yet
- Chapter 1 f3Document113 pagesChapter 1 f3FAthiyah Abdul RahimNo ratings yet
- Specific Objectives Notes Practical: Section ADocument14 pagesSpecific Objectives Notes Practical: Section AaWDwaDNo ratings yet
- NeuroSensory - Eye Part 2Document38 pagesNeuroSensory - Eye Part 2Zed P. EstalillaNo ratings yet
- External Eye: Internal EyeDocument2 pagesExternal Eye: Internal EyeJustin John NavarroNo ratings yet
- C1 F3 BiodiversityDocument112 pagesC1 F3 BiodiversityNurul Shafiah Mustafa KamalNo ratings yet
- The Human EyeDocument9 pagesThe Human Eyegiana 4e100% (1)
- Reviewer G10 Todamax - 1Document11 pagesReviewer G10 Todamax - 1Aiza Casinillo CabatinganNo ratings yet
- The Eye Is Made Up of THREE LayersDocument2 pagesThe Eye Is Made Up of THREE LayersMarissa AsimNo ratings yet
- Week 15Document2 pagesWeek 15Paul SahagunNo ratings yet
- 2.07 Tutorial Week 3Document4 pages2.07 Tutorial Week 3GraciaNo ratings yet
- Structure of The EyeDocument2 pagesStructure of The EyeminaNo ratings yet
- Special SensesDocument5 pagesSpecial SensesKathrene Angel GumilaoNo ratings yet
- Biology - Structure of EyeDocument3 pagesBiology - Structure of EyeLeung BibiNo ratings yet
- Special Senses NotesDocument3 pagesSpecial Senses NotesChelsa LeyritanaNo ratings yet
- Special SensesDocument29 pagesSpecial Sensesmawel100% (2)
- Ha Eyes and Ears 1Document7 pagesHa Eyes and Ears 1SICAT, Keeshan KeithNo ratings yet
- EENTDocument21 pagesEENTMary Beth AbelidoNo ratings yet
- A. Eye Balls D. Lacrimal Glands: 1. External Structures of The EyeDocument7 pagesA. Eye Balls D. Lacrimal Glands: 1. External Structures of The EyebeayapNo ratings yet
- Looking After Our EyesDocument24 pagesLooking After Our EyesWutt Yee Moe MyintNo ratings yet
- The Main Parts of The Eye and Their FunctionDocument5 pagesThe Main Parts of The Eye and Their FunctionJoshuaNo ratings yet
- Week 15Document2 pagesWeek 15Diana MontaosNo ratings yet
- Ch-11-Human Eye and The Colouful World 285-307 Physics Sem-1Document22 pagesCh-11-Human Eye and The Colouful World 285-307 Physics Sem-1MAYUR DESAI II BeingMD in PHYSICS IINo ratings yet
- Eye and Ear - 2019Document3 pagesEye and Ear - 2019Mr. RWord100% (1)
- Eyes Health AssessmenttDocument34 pagesEyes Health AssessmenttMhiaBuenafeNo ratings yet
- Procedure Materials: Cornea Optic Nerve Scler ADocument4 pagesProcedure Materials: Cornea Optic Nerve Scler AJohn FisherNo ratings yet
- Perceptual DisturbancesDocument7 pagesPerceptual DisturbancesVin SageNo ratings yet
- EENT Review ManualDocument19 pagesEENT Review ManualJohn Darvin TanNo ratings yet
- Eye LabDocument2 pagesEye LabElizabeth AlvarezNo ratings yet
- Grade 11 Biology The EyeDocument5 pagesGrade 11 Biology The EyeDexter TorringtonNo ratings yet
- 13.2 Sense Organ - EyeDocument28 pages13.2 Sense Organ - EyeMuhammad Amin SuhaimiNo ratings yet
- Biology Eye NotesDocument12 pagesBiology Eye NotesBalakrishnan MarappanNo ratings yet
- 3.2 Sense OrganDocument8 pages3.2 Sense OrganMod HollNo ratings yet
- Eye Optics and AccommodationDocument14 pagesEye Optics and AccommodationJúnior AlvesNo ratings yet
- Science ReviewerDocument10 pagesScience ReviewerAngeli FernandezNo ratings yet
- Structure and FunctionDocument15 pagesStructure and FunctionGOODWIN GALVANNo ratings yet
- Brightness - Amplitude of Wave High Wave-Brighter, Low Have - DullDocument3 pagesBrightness - Amplitude of Wave High Wave-Brighter, Low Have - Dullpreetirajput2412No ratings yet
- Iris Muscle - (Most Anterior Extension: EyeballDocument8 pagesIris Muscle - (Most Anterior Extension: EyeballBianx Flores DosdosNo ratings yet
- Waves Aranoco Ppt-Anatomy of The EyeDocument40 pagesWaves Aranoco Ppt-Anatomy of The EyeARNOLD ARANOCONo ratings yet
- Major 1 Difficulty in SeeingDocument2 pagesMajor 1 Difficulty in SeeingChristine Mae CalfoforoNo ratings yet
- b30 m1 l05 AssignmentDocument3 pagesb30 m1 l05 AssignmentYusuf GuledNo ratings yet
- Eent + OrthoDocument87 pagesEent + OrthoKaris HemmingsNo ratings yet
- RBA Eye Grade 4 6 10x1Document12 pagesRBA Eye Grade 4 6 10x1Felixdino09No ratings yet
- Anatomy and Physiology of The EyeDocument18 pagesAnatomy and Physiology of The EyeMargaretha AdhiningrumNo ratings yet
- Eye and Ear 2.1 Human EyeDocument12 pagesEye and Ear 2.1 Human Eyechakshana kannangaraNo ratings yet
- The-EyeDocument26 pagesThe-EyeBaciu Florina GabrielaNo ratings yet
- Lesson 2 The Structure and Functions of The EyeDocument12 pagesLesson 2 The Structure and Functions of The EyeNguyễn Gia LộcNo ratings yet
- Human Eye Sec4 BioDocument10 pagesHuman Eye Sec4 BioFrancine TheophilaNo ratings yet
- Chapter 4 - Perception and SensationDocument6 pagesChapter 4 - Perception and Sensationecaber.a12343991No ratings yet
- Finals - Eyes and EarsDocument4 pagesFinals - Eyes and EarsCrisanta Grace OpondaNo ratings yet
- Low Vision: Assessment and Educational Needs: A Guide to Teachers and ParentsFrom EverandLow Vision: Assessment and Educational Needs: A Guide to Teachers and ParentsNo ratings yet
- A Simple Guide to the Eye and Its Disorders, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to the Eye and Its Disorders, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Untitled DocumentDocument7 pagesUntitled DocumentDavid Dwane Art SilorioNo ratings yet
- Form D Chess MenDocument2 pagesForm D Chess MenDavid Dwane Art SilorioNo ratings yet
- Tally FinalDocument3 pagesTally FinalDavid Dwane Art SilorioNo ratings yet
- SAssignment 1.3Document1 pageSAssignment 1.3David Dwane Art SilorioNo ratings yet
- Rosario Week13Document2 pagesRosario Week13David Dwane Art SilorioNo ratings yet
- Learning FeedbackDocument1 pageLearning FeedbackDavid Dwane Art SilorioNo ratings yet
- Cellular Aberration Lecture 1Document93 pagesCellular Aberration Lecture 1David Dwane Art SilorioNo ratings yet
- Assignment IV.4Document2 pagesAssignment IV.4David Dwane Art SilorioNo ratings yet
- Notes Health Care Delivery SystemDocument6 pagesNotes Health Care Delivery SystemDavid Dwane Art SilorioNo ratings yet
- Notes Primary Health Care ApproachDocument5 pagesNotes Primary Health Care ApproachDavid Dwane Art SilorioNo ratings yet
- PATHFIT Attendance and Grade SheetDocument2 pagesPATHFIT Attendance and Grade SheetDavid Dwane Art SilorioNo ratings yet
- Course Insight Summary Sheet#2Document2 pagesCourse Insight Summary Sheet#2David Dwane Art SilorioNo ratings yet
- Learning Contract PHIHUM CDocument2 pagesLearning Contract PHIHUM CDavid Dwane Art SilorioNo ratings yet
- LP#2 Intoduction To PhilosophyDocument3 pagesLP#2 Intoduction To PhilosophyDavid Dwane Art SilorioNo ratings yet
- Module 1 DELIV SDLDocument8 pagesModule 1 DELIV SDLDavid Dwane Art SilorioNo ratings yet
- Csom 090615124432 Phpapp01Document36 pagesCsom 090615124432 Phpapp01Ibrahim QuadriNo ratings yet
- TympanometerDocument12 pagesTympanometerAli ImranNo ratings yet
- Anatomi TelingaDocument15 pagesAnatomi Telingaerika indrajayaNo ratings yet
- 2012 ICD 9 CM Diagnosis CodesDocument41 pages2012 ICD 9 CM Diagnosis CodesRs Era MedikaNo ratings yet
- Nervous System - Summary NotesDocument9 pagesNervous System - Summary NotesHarshNo ratings yet
- Disorders of The EarDocument8 pagesDisorders of The EarVinz Khyl G. CastillonNo ratings yet
- Sensory Organs: Medical Surgical NursingDocument17 pagesSensory Organs: Medical Surgical NursingHoney PrasadNo ratings yet
- Ear Nose and Throat QuizDocument6 pagesEar Nose and Throat QuizParsaant SinghNo ratings yet
- 15.the Anatomy of The Ear 2017 NewDocument109 pages15.the Anatomy of The Ear 2017 NewMuhammed100% (1)
- ENT - Diseases of The External Ear, Middle Ear and MastoidDocument7 pagesENT - Diseases of The External Ear, Middle Ear and MastoidChristian LantanoNo ratings yet
- EAR MCQs Points Rida NaqviDocument6 pagesEAR MCQs Points Rida NaqviÅli Raza ChaudaryNo ratings yet
- 1-5 Hear N SightDocument19 pages1-5 Hear N SightNor ShuhadaNo ratings yet
- Tympanoplasty Indications, Types, ProcedureDocument55 pagesTympanoplasty Indications, Types, ProcedurePrasanna DattaNo ratings yet
- Perforated EardrumDocument5 pagesPerforated EardrumElvinNo ratings yet
- CH 15Document8 pagesCH 15naguguNo ratings yet
- Pedia Prof - OamilDocument147 pagesPedia Prof - OamilOne Click Online ShopNo ratings yet
- 100 Items QuestionsDocument22 pages100 Items Questionsdianneako100% (1)
- Unit 5. Interaction and HealthDocument11 pagesUnit 5. Interaction and Healthtamarita90No ratings yet
- Ears Lecture GuideDocument56 pagesEars Lecture GuidemajNo ratings yet
- 2018 Autumn Me 5241 Engineering Acoustics Course NotesDocument171 pages2018 Autumn Me 5241 Engineering Acoustics Course NotesAkinyemiNo ratings yet
- DissertationDocument109 pagesDissertationSayan BanerjeeNo ratings yet
- Ossicles: The Malleus, The Incus, and The StapesDocument6 pagesOssicles: The Malleus, The Incus, and The StapesLili M.No ratings yet
- Gambar Membran TimpaniDocument6 pagesGambar Membran TimpaniMilya SariNo ratings yet
- 중이염 Otitis MediaDocument213 pages중이염 Otitis MediaChangho LeeNo ratings yet
- Temporal Bone AnatomyDocument27 pagesTemporal Bone AnatomyWesam Al-TawilNo ratings yet
- 1ear AnatomyDocument33 pages1ear AnatomyMarijaNo ratings yet
- Chapter-12 SoundDocument27 pagesChapter-12 SoundDevansh GuptaNo ratings yet
- The EarDocument13 pagesThe EarOjambo FlaviaNo ratings yet