Professional Documents
Culture Documents
Schafer 1998 Renal Water and Ion Transport Systems
Schafer 1998 Renal Water and Ion Transport Systems
Uploaded by
André e Ana Paula CostaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Schafer 1998 Renal Water and Ion Transport Systems
Schafer 1998 Renal Water and Ion Transport Systems
Uploaded by
André e Ana Paula CostaCopyright:
Available Formats
A P S R E F R E S H E R C O U R S E R E P O R T
RENAL WATER AND ION TRANSPORT SYSTEMS
James A. Schafer
Departments of Physiology and Biophysics, Nephrology Training and Research Center,
University of Alabama at Birmingham, Birmingham, Alabama 35294
he teaching of renal physiology is an ever-evolving and fascinating opportunity to
T learn as well as to teach. Regardless of the particular format of our teaching, a
constantly waxing tide of detailed information forces us to be selective. We
cannot teach it all. In my own lectures and discussions of renal ion and water transport
systems, I try to 1) avoid complex and detailed areas that are not essential to a basic
understanding of renal function, 2) highlight the commonalities of transport processes
among segments, 3) relate the details of transporters to clinical conditions that are
especially interesting, 4) make connections between physiological details and clinical
therapy, and 5) stress quantitative problems. Although generally simple, the quantitative
understanding is essential to appreciate the role of the kidney in homeostasis and
derangements thereof. When I review what I have taught, I try to integrate multiple basic
mechanisms in individual segments to produce a picture of ‘‘whole kidney’’ function.
AM. J. PHYSIOL. 275 (ADV. PHYSIOL. EDUC. 20): S119–S131, 1998.
Key words: isosmotic volume reabsorption; glucose reabsorption; aquaporins; renal
diseases; diuretics; homeostasis; steady state; creatinine balance
The teaching of renal physiology is an ever-evolving This presentation deals with some of the challenges
and fascinating opportunity to learn as well as to involved in approaching these ideals when teaching
teach. Whatever the format in which we teach this about renal water and ion transport systems in the
subject, be it traditional lectures, problem-based learn- multiple nephron segments. Here, I summarize my
ing, or some combination, an ever-growing body of own methods of dealing with the more complex
information forces us to select those details that are topics, including those that are better taught only
most relevant for the medical student and put them in superficially. I also present some of my favorite
useful and interesting contexts. This focus on the examples that relate discrete renal transporter defects
medical student is also valid for our PhD graduate
to interesting diseases and the therapeutic interven-
students. There is simply too much information for us
tions for those diseases. It is also my firm belief that
to expect them to learn the whole body of informa-
most of the key concepts in renal physiology depend
tion about each organ system, as might have been
possible 20 or 30 years ago. On the other hand, our on a good quantitative understanding of the processes
graduate students still need the breadth of a general involved, and for that reason, I also spend some
physiology course to fulfill their roles as both scien- verbiage developing my own approach to improving
tists and teachers. Hopefully, the future physiologist the students’ quantitative understanding. Finally, I
will have this breadth of knowledge that will facilitate provide some examples of basic overviews that inte-
the integration of molecular and genetic information grate the detail of epithelial transport mechanisms
with physiological and pathophysiological processes; into a picture of the ‘‘whole kidney’’ effects of
i.e., to be the link from molecule to clinic. changes in the operation of those transporters.
1043 - 4046 / 98 – $5.00 – COPYRIGHT r 1998 THE AMERICAN PHYSIOLOGICAL SOCIETY
VOLUME 20 : NUMBER 1 – ADVANCES IN PHYSIOLOGY EDUCATION – DECEMBER 1998
S119
Downloaded from journals.physiology.org/journal/advances (187.106.035.231) on February 19, 2024.
A P S R E F R E S H E R C O U R S E R E P O R T
WHY TEACH NEPHRON FUNCTION?
Many of our nephrology and pathology colleagues
might disagree with the detail with which we present
the transepithelial transport processes involved in the
function of the nephron. After all, they might argue,
the most important and common renal diseases are
not disorders of tubular transport. Glomerular immu-
nopathology, specifically glomerulonephritis, is by far
the most prevalent cause of chronic and end-stage
renal disease. It might seem, therefore, that we should
concentrate our teaching on glomerular function and
immunology to the exclusion of renal transport pro-
cesses. The counterpoint to this argument is that an
understanding of how the kidney maintains salt and
water balance through regulation of its multiple trans-
port processes is essential for understanding fluid and
electrolyte disorders and for the rational choice of
therapy for those disorders. Fluid and electrolyte
disorders are much more common than glomerular
disease, and most physicians deal with these disorders
daily. As just one of many examples, the most com-
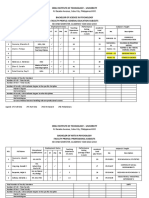
mon fluid and electrolyte disorder in the hospital FIG. 1.
setting is hyponatremia, and 50% of hyponatremic Isosmotic volume reabsorption in proximal tubule.
Distribution of osmotically driven water flow between
patients die. Also, the concepts learned in understand-
transcellular and paracellular pathways (junctional
ing renal epithelial transport processes are closely complexes and lateral intercellular spaces) remains
related to similar processes occurring in many other controversial. This issue may be addressed experimen-
systems, for example, intestinal absorption and secre- tally in the near future because of development of a
tion, and electrolyte balance in the respiratory system mouse strain with a knockout of aquaporin-1 (AQP1;
Ref. 14).
and in the brain.
outlined in Fig. 1. The important points to stress are as
AVOID EXPLAINING COMPLEX CONCEPTS
follows (18). 1) Water movement across the epithe-
WHEN THEY ARE NOT ESSENTIAL
lium and all regions of the nephron occurs in response
In addressing the more complex topics in renal salt to an osmotic gradient, whether that gradient is
and water transport, the lecturer has to make the localized to a small region such as the intracellular
decision of whether a full discussion is warranted. All spaces or between two compartments such as the
of the topics that we teach involve details and com- tubular lumen and the interstitial fluid. 2) The essen-
plexities that could require hours of self-study for the tial ingredient for (nearly) isosmotic volume absorp-
student to begin to appreciate. A primary job of the tion is the extremely high osmotic water permeability
teacher is to decide whether a full discussion of the of the proximal tubule. Because of this high water
topic is worth the time that it would take from more permeability, only a very small osmolality difference,
important, more clinically applicable, subjects. An one that was not easily measured in early studies, is
example dear to my own heart is the process by which needed to drive the observed rates of volume reabsorp-
fluid is reabsorbed isosmotically from the proximal tion. 3) The active transport of solutes makes the
tubule. Despite the large volume of information on lumen slightly dilute and the interstitial fluid slightly
this subject that my colleagues and I, and many others, hypertonic. 4) The actively reabsorbed solutes such as
have laboriously gathered (2, 4, 18, 28), I feel that the glucose, amino acids, and bicarbonate have higher
student can appreciate the essence of isosmotic vol- reflection coefficients than NaCl; thus the preferential
ume absorption according to the simple principles reabsorption of these solutes results in the develop-
VOLUME 20 : NUMBER 1 – ADVANCES IN PHYSIOLOGY EDUCATION – DECEMBER 1998
S120
Downloaded from journals.physiology.org/journal/advances (187.106.035.231) on February 19, 2024.
A P S R E F R E S H E R C O U R S E R E P O R T
ment of a larger ‘‘effective’’ osmolality difference across the medullary interstitium, where it contributes to the
the epithelium. Students should already be familiar medullary hypertonicity and enhances water reabsorp-
with the concept of a reflection coefficient, but even if tion from the descending limb of the loop of Henle.
they are not, they should be able to intuitively grasp These points encompass the essential ingredients of
the fact that solutes of lower permeability (and thus the countercurrent multiplication system, and using
higher reflection coefficient) will make a greater these points, the teacher can examine mechanisms by
contribution to the true osmolality of interstitium com- which the medullary osmolality gradient can be dis-
pared with the fluid remaining in the tubule lumen, turbed. One can discuss, for example, the effects of
which becomes increasingly composed of NaCl, which changes in medullary blood flow, saline loading, loop
replaces the preferentially reabsorbed solutes. diuretics, low-protein diets, and water diuresis on the
medullary concentration gradient.
Another area that I find too demanding in time for the
student to understand in detail is the mechanism of SIMPLIFY THE DETAILS OF EPITHELIAL
countercurrent multiplication, especially passive coun- TRANSPORT AND HIGHLIGHT THE
tercurrent multiplication in the inner medulla. Cer- COMMONALITIES AMONG SEGMENTS
tainly, the postulation and experimental verification One of the most important characteristics of the
of the countercurrent multiplication system was one nephron is its ability to dissociate salt and water
of the most intellectually gratifying achievements of transport in various segments. Some nephron seg-
renal physiology research. For that reason, I believe ments, including the thin and thick ascending limbs of
many of us have given it undue emphasis in our the loop of Henle and the collecting duct in the
practical teaching. If the students want to know these absence of vasopressin (AVP), are very water imperme-
details, I refer them to an appropriate text. However, able. In these water-impermeable segments, solute
at least in the lecture setting, I stress the essential reabsorption results in dilution of the tubular fluid. In
ingredients for the development of medullary hyperto- contrast, most cell membranes, including those of the
nicity and the clinically important events that would proximal tubule and thin descending limb of the loop
interfere with the urinary concentrating and diluting of Henle, are very water permeable under all circum-
ability. Obviously, the crucial element is active NaCl stances. This high water permeability is a conse-
reabsorption by the thick ascending limb of the loop quence of the presence of a water channel that has
of Henle via the Na1-K1-2Cl cotransporter (BSC1). The come to be referred to as aquaporin-1 (AQP1). I find
students can well appreciate that this active solute the students interested to know that this water chan-
reabsorption, which occurs in a segment that is water nel is found in many cells, including red blood cells,
impermeable, should concentrate the medullary inter- and that it contributes to the very high water perme-
stitium. They can also readily appreciate that the ability of the proximal tubule and the descending limb
countercurrent arrangement and low blood flow rate of the loop of Henle, where it is present in both
through the vasa recta curtail the ‘‘washout’’ of the luminal and basolateral membranes (Fig. 2).
hypertonicity that would occur in most other tissues.
The second component is the addition of urea to the Perhaps even more interesting in terms of water
tubular fluid in the thin limbs of the loop of Henle, permeability is the collecting duct. The luminal mem-
which increases the amount of urea that is delivered brane of the principal cells in this segment can be
to the thick ascending limb of the loop of Henle. Urea regulated from nearly water impermeable, in the
is then trapped in the tubular lumen, because all absence of AVP, to quite water permeable in the
nephron segments from the thick ascending limb presence of the hormone. The intrinsically low water
through the outer medullary collecting duct are imper- permeability of these cells is increased by the inser-
meable to urea. However, because of the presence of tion of another aquaporin (AQP2; see Fig. 2) into the
a urea transporter (UT1) in the most distal portion of luminal membrane. AQP2 is stored in vesicles in the
the inner medullary collecting duct, urea can diffuse cytoplasm of the principal cells of the collecting duct
passively across this epithelium. When the urine urea and the connecting tubule arcades. Basolateral mem-
concentration is very high, as in antidiuresis, urea branes of the principal cells, which remain water
diffuses from the inner medullary collecting duct to permeable even in the absence of AVP, contain yet
VOLUME 20 : NUMBER 1 – ADVANCES IN PHYSIOLOGY EDUCATION – DECEMBER 1998
S121
Downloaded from journals.physiology.org/journal/advances (187.106.035.231) on February 19, 2024.
A P S R E F R E S H E R C O U R S E R E P O R T
FIG. 2. FIG. 3.
Characteristics of primary aquaporin water channels All nephron segments have common transport proper-
found in kidney. CHIP28 and WCH-CD are alternate ties: a single layer of cells connected by junctional
names that were previously used for AQP1 and AQP2, complexes near their luminal aspects, basolateral Na1-
respectively. AVP, vasopressin; DLH, descending limb K1-ATPase, and passive Na1 entry across the luminal
of the loop of Henle; IMCD, inner medullary collecting entry that may be dissipative or coupled to active
duct; DI, diabetes insipidus. Right arrow indicates antiport or cotransport of other solutes (S). It is
production. See text for fuller explanations. primarily the details of the luminal entry process that
differ among nephron segments.
two other aquaporins: AQP3 and AQP4. At this point,
it is instructive to point out that mutations in human intracellular voltage. However, most epithelia, includ-
AQP2 that result in nephrogenic diabetes insipidus ing all the nephron segments, are unique because this
have been identified and that there may be as yet transporter is localized only to the basolateral mem-
unidentified abnormalities in AQP3 or AQP4 that brane. 3) In all nephron segments, the Na1-K1-ATPase
could also interfere with the ability to concentrate the develops an Na1 electrochemical potential gradient
urine. (For references to aquaporins, see Refs. 1, 7, 12, across the opposite membrane, i.e., the luminal mem-
14, and 23.) brane; thus there is a driving force for the passive
entry of Na1 from the lumen into the epithelial cell.
In discussing the details of transport processes, it is This entry may occur through an electrogenic Na1
also useful to generalize about transepithelial trans- channel, such as the amiloride-sensitive Na1 channel
port before dealing with the details of individual in the collecting duct, in which case the potential
systems. For example, when I introduce transport in energy embodied in the Na1 electrochemical poten-
the proximal tubule, as shown in Fig. 3, I first point tial gradient is dissipated. However, if the movement
out the aspects that are common to all regions of the of Na1 is coupled to the movement of another solute,
nephron. 1) The epithelium is a single cell layer, and for example, by an antiporter, such as the Na1/H1
cells are joined by junctional complexes near their exchanger (NHE3) in the proximal tubule, or by a
apical border. This topology provides two pathways cotransporter, such as the Na1-glucose symporter,
by which solutes can traverse the epithelium, either then the energy available in the Na1 electrochemical
through the cell or through the paracellular pathway, potential gradient can be used to perform useful
i.e., the junctional complexes and lateral intercellular work. That useful work is the active transport of the
spaces. 2) All epithelial cells in the nephron have the coupled solutes against their own electrochemical
Na1-K1-ATPase that is common to virtually every cell potential gradients. It should be emphasized to the
in the body. This Na1-K1-ATPase is responsible for student that this general plan for the transport of Na1
maintaining a low intracellular Na1 concentration and holds true throughout the nephron. That is, the Na1
for developing the ion gradients that lead to a negative electrochemical potential gradient is maintained by
VOLUME 20 : NUMBER 1 – ADVANCES IN PHYSIOLOGY EDUCATION – DECEMBER 1998
S122
Downloaded from journals.physiology.org/journal/advances (187.106.035.231) on February 19, 2024.
A P S R E F R E S H E R C O U R S E R E P O R T
the basolateral Na1-K1-ATPase, and this potential
energy gradient provides the driving force for passive
entry of Na1 into the cell across the luminal mem-
brane either alone or in combination with secondary
active transport of other solutes. It is only the details
of the transporters, usually those on the luminal
membrane, that vary from one nephron segment to
another. I try constantly to refer back to this overall
scheme to avoid the students becoming belabored by
the details of specific transporters in each nephron
segment.
RELATE TRANSPORTER DETAILS
TO CLINICAL CONDITIONS THAT
ARE ESPECIALLY INTERESTING
In my experience, medical students are more willing
to address the details of an epithelial transport process
that are associated with clinically relevant defects. FIG. 4.
Graduate students are now acutely aware of the direct Secondary active transport of glucose by Na1-glucose
associations between gene mutations and functional cotransporters SGLT1 and SGLT2. Although these 2
transporters are quite similar, and both are expressed
defects and are also receptive to these practical
in proximal tubule, subtle differences in molecular
applications of basic science. Thus, whenever pos- details of their operation explain profound pheno-
sible, I try to relate the details of the operation of a typic differences produced by loss-of-function muta-
membrane transporter to a particular clinical situa- tions. G, glucose; Tm , maximum renal reabsorption
tion. A perfect example is a comparison of the two rate, or transport maximum.
Na1-glucose cotransporters that are found in the
kidney: SGLT1 and SGLT2 (Fig. 4). (The number glucose-galactose malabsorption syndrome that is char-
associated with the acronyms of these two transport- acterized by severe diarrhea and dehydration, but it
ers presents the order in which they were cloned and has little effect on the renal reabsorption of glucose.
sequenced. This can be somewhat confusing, because There are multiple mutant forms of SGLT2 in the
the SGLT1 protein cotransports two Na1 in associa- human population that are associated with different
tion with one glucose, whereas the SGLT2 has a 1:1 forms of familial renal glucosuria. However, this
stoichiometry.) In the kidney, SGLT2 is the primary condition is relatively benign, and its effects are
transporter and is found in the proximal convoluted restricted to the kidney because SGLT2 is not found in
tubule, whereas the SGLT1 cotransporter is found in the intestine. This example provides students with an
the proximal straight tubule. Because of the higher excellent example of how relatively small differences
stoichiometry of SGLT1, the transporter can develop a in quite similar transporters can lead to quite different
concentration gradient (lumen to cell) of up to disease phenotypes (for details, see Refs. 9, 10, 15,
1:10,000, whereas SGLT2 develops only a 1:100 gradi- and 29).
ent. Thus it appears that SGLT2 serves to reabsorb the
bulk of the glucose filtered in the kidney, whereas Another condition that integrates genetics, molecular
SGLT1 is able to reabsorb the last bit of sugar against a biology, physiology, and disease in a most elegant
high transepithelial concentration gradient (3, 19, 22). collage is Liddle’s syndrome. Liddle’s syndrome is a
rare autosomal dominant disease that was first de-
Where is the clinical interest here? The answer is that scribed by Grant Liddle et al. (13) in 1963. It is
genetic defects occur in both transporters in humans characterized by severe hypertension, often leading to
that result in completely different phenotypes as stroke even at a young age. It is also frequently
illustrated in Fig. 4. A single base pair mutation in associated with hypokalemia and metabolic alkalosis.
SGLT1, which causes a loss of function, produces the Thus, in most aspects, Liddle’s syndrome looks very
VOLUME 20 : NUMBER 1 – ADVANCES IN PHYSIOLOGY EDUCATION – DECEMBER 1998
S123
Downloaded from journals.physiology.org/journal/advances (187.106.035.231) on February 19, 2024.
A P S R E F R E S H E R C O U R S E R E P O R T
similar to primary aldosteronism, i.e., the overproduc- which resides in Southern Alabama, is relatively exten-
tion of aldosterone by an adrenal carcinoma or diffuse sive, and immortalized lymphocytes obtained from
renal hyperplasia. However, as determined by bioas- family members were used for DNA analysis. It was
says, which at the time of Liddle’s report were found that Liddle’s syndrome was associated with a
available in his laboratory and a few others, it was mutation in the b-ENaC sequence that resulted in an
determined that plasma renin and aldosterone levels early truncation in the COOH-terminal region (20).
were both immeasurable, and the condition was not This truncation results in an overactive Na1 channel
ameliorated by the aldosterone receptor antagonist that is not regulated normally and can explain the
spironolactone. Liddle and his co-workers could find excessive Na1 reabsorption seen in Liddle’s patients.
no hormonal explanation for the abnormality, and, on Since these original findings, several similar kindreds
the basis of the physiological information of that time, have been identified with other mutations in the
they correctly concluded in 1963 that the defect COOH-terminal regions of the b- and g-subunits (24).
probably represented an unregulated absorption of It is also interesting that the congenital form of
Na1 by the distal nephron. Their suggested treatment, pseudohypoaldosteronism is associated with a muta-
which is the administration of triamterene or amilo- tion in the internal region of the a-ENaC subunit that
ride in combination with a low-Na1 diet, remains the results in a loss-of-function mutation rather than the
treatment of choice. As shown in Fig. 5, since 1963, gain-of-function observed in Liddle’s syndrome (6).
we have learned that the target of amiloride and
triamterene action is the electrogenic Na1 channel Students are fascinated with this kind of information
found in the luminal membrane of the principal cell of because it so beautifully transfers information from
the collecting duct. This channel, referred to as the the basic physiology of the kidney, which allowed
epithelial Na1 channel (ENaC), consists of three sub- Grant Liddle to interpret the syndrome he observed,
units labeled a, b, and g, which were originally cloned to the final resolution of the clinical problem by the
and sequenced by Cecilia Canessa in Bernard Rossier’s application of molecular biology and physiology. This
laboratory just four years ago (5). Once the genetic example can be used to demonstrate the reasons for
sequence for these channel subunits was known and the other manifestations of the Liddle’s syndrome. As
their position on human chromosomes ascertained, it shown in Fig. 5, if the Na1 channel is unregulated and
was possible to examine whether there was a muta- ‘‘wide open,’’ the high Na1 conductance of the
tion associated with one of the subunits that results in luminal membrane would depolarize it, just as the
Liddle’s syndrome. Fortunately, the Liddle’s kindred, activation of Na1 channels in nerve or muscle mem-
brane results in depolarization of those cells. The
result of this depolarization is a more favorable K1
electrochemical potential gradient that drives the
passive movement of K1 out of the principal cells into
the lumen, thus enhancing K1 excretion and leading
to the hypokalemia that is observed in at least some of
the patients. The associated alkalosis may also be a
result of an increased lumen-negative voltage that
favors H1 secretion.
It is also important to point out that these syndromes
illustrate the importance of Na1 balance in maintain-
ing normal blood pressure and volumes of body fluid
compartments. About 25,000 meq of Na1 are filtered
per day by the glomeruli in two adult human kidneys,
FIG. 5. but less than 2,000 meq/day are reabsorbed in the
Transport processes in principal cell of collecting
duct. A lumen-negative voltage of 230 mV (compared
distal tubule and collecting duct, with the vast major-
with interstitium) is taken as an average, but it can ity being reabsorbed in the proximal tubule and the
vary with relative luminal Na1 and K1 conductances. ascending limb of the loop of Henle. Aldosterone
VOLUME 20 : NUMBER 1 – ADVANCES IN PHYSIOLOGY EDUCATION – DECEMBER 1998
S124
Downloaded from journals.physiology.org/journal/advances (187.106.035.231) on February 19, 2024.
A P S R E F R E S H E R C O U R S E R E P O R T
regulates the reabsorption of ,500 meq of the 2,000 have reasonable affinity for both the mineralocorticoid
meq reabsorbed by the distal tubule and collecting and glucocorticoid (type I and type II) receptors in
duct. Thus, in the total absence of aldosterone, only aldosterone responsive tissues. However, because of
,500 meq/day are excreted, and at very high aldoste- the presence of an enzyme, 11b-hydroxysteroid dehy-
rone levels, Na1 excretion can be reduced nearly to drogenase (11b-OH HSD), cortisol is degraded to the
zero. The important point to stress is that aldosterone inactive cortisone. This allows aldosterone, which is
is operating on only a very small fraction of the filtered usually present in much lower concentration in the
Na1 load, but this regulation of Na1 excretion in the plasma than glucocorticoids, to react with mineralocor-
range of 0–1% of the filtered load is extremely critical. ticoid and, to some extent, glucocorticoid receptors
The retention of only 150 meq of Na1 (with accompa- in aldosterone target tissues such as the principal cell
nying monovalent anions) requires the retention of 1 of the cortical collecting duct. The 11b-HSD can be
liter of water to make it isotonic. Given the fine nature inhibited by certain compounds and drugs such as
of this regulation, it is remarkable that disturbances, glycyrrhetinic acid (in licorice) and gossypol, which
such as those produced by defects in ENaC, can lead leads to a syndrome that is very similar to Liddle’s
to either salt wasting in the case of the a-subunit syndrome or apparent hyperaldosteronism (11, 25,
mutation or Na1 retention with severe hypertension 26). The syndrome is also caused by mutations in the
in the case of the b- and g-subunit mutations. human 11b-HSD gene (16, 27).
There are additional excellent examples of transporter Bartter’s syndrome (Fig. 6) illustrates the importance
or enzyme mutations that have interesting clinical of specific transporters in the thick ascending limb of
correlations, some of which are described in Fig. 6. In the loop of Henle that result in the development of a
the case of apparent mineralocorticoid excess, the lumen-positive voltage and thus favor Ca21 reabsorp-
underlying facts are that glucocorticoids such as cortisol tion. Mutations in BSC1 as well as mutations in the
luminal K1 channel (ROMK) or in the basolateral Cl2
channel have been linked to Bartter’s syndrome. All
these defects lead to decreased salt reabsorption in
the thick ascending limb of the loop of Henle, and
thus to a concentrating defect with increased Na1
delivery to the collecting duct. The latter leads to salt
wasting with an elevation of renin and aldosterone
concentrations. Na1 reabsorption by the collecting
duct is increased by the aldosterone. In addition, the
increased Na1 delivery as well as the aldosterone
produce inappropriate levels of K1 and H1 secretion,
leading to hypokalemia and metabolic alkalosis. These
effects are accompanied by a relative failure to absorb
Ca21 and hypercalciuria. Gitelman’s syndrome is a
similar condition with all of the characteristics of
Bartter’s syndrome but with hypo- rather than hyper-
calciuria and hypomagnesemia. This syndrome results
from a loss-of-function mutation in the thiazide-
sensitive NaCl cotransporter (TSC1), which is found
in the distal convoluted tubule. By examining abnor-
FIG. 6. malities in transporters or enzymes associated with
Associations between defects at molecular level and syndromes such as these, the teacher can provide
pathophysiology of disease states they produce. superb examples of the importance of physiological
11b-OH HSD, 11b hydroxysteroid dehydrogenase;
ENaC, epithelial Na1 channel; ROMK, inwardly rectify-
detail in the context of clinical understanding (for
ing K1 channel found in luminal membrane of thick references to Bartter’s and Gitelman’s syndromes, see
ascending limb of loop of Henle. Ref. 8, 17, and 21).
VOLUME 20 : NUMBER 1 – ADVANCES IN PHYSIOLOGY EDUCATION – DECEMBER 1998
S125
Downloaded from journals.physiology.org/journal/advances (187.106.035.231) on February 19, 2024.
A P S R E F R E S H E R C O U R S E R E P O R T
FIG. 7.
Unique transporters and enzymes are targets for diuretic therapy. In proximal tubule,
acetazolamide inhibits carbonic anyhdrase, decreasing HCO2 3 and Na
1 reabsorption;
mannitol acts as an osmotic diuretic. In thick ascending limb, furosemide and bumetanide
inhibit Na1-K1-2Cl cotransporter (BSC1) by competition for Cl2 receptor. Cl2 receptor is
also the target for inhibitory effect of thiazide diuretics on NaCl cotransporter (TSC1) in
distal convoluted tubule. In principal cells of collecting duct, amiloride and triamterene
block Na1 channel (ENaC).
RELATING PHYSIOLOGICAL DETAILS In the distal convoluted tubule, the thiazide diuretics
TO THERAPY interfere with the chloride recognition site on TSC1.
Thus the diuretic inhibits NaCl reabsorption in the
As shown in Fig. 7, the mechanisms of action of drugs
distal convoluted tubule and increases its delivery to
such as diuretics can also be used to illustrate physi-
the collecting duct with the same consequences on
ological processes. The action of acetazolamide (Dia-
K1 secretion. However, because the thiazides act only
mox) can be used to illustrate the mechanism of
in the cortex, where the distal convoluted tubule is
bicarbonate reabsorption in the proximal tubule. The
located, they interfere primarily with the ability of the
diuretic and natriuretic effects of a failure to reabsorb
kidney to dilute the urine. In contrast, furosemide, by
bicarbonate can also be related to the similar effects of
inhibiting NaCl reabsorption in the medulla, interferes
mannitol operating as an osmotic diuretic. It is also
with both the concentrating and diluting abilities of
known that furosemide and similar drugs such as
the kidney. I have already discussed the fourth panel
bumetanide interfere with the chloride recognition
in Fig. 7, which is the action of amiloride and
site on BSC1, which results in inhibition of Na1 and
triamterene to block the Na1 channel in the principal
Ca21 reabsorption by the thick ascending limb of the
cell of the collecting duct.
loop of Henle, leading to natriuresis and diuresis.
Again, the teacher should stress the effects on in-
QUANTITATIVE PROBLEMS ARE ESSENTIAL
creased salt and water delivery to the distal nephron in
promoting K1 secretion, resulting in hypokalemia as Despite the fact that our students generally have a
well as hypercalciuria. good background in the physical sciences, they are
VOLUME 20 : NUMBER 1 – ADVANCES IN PHYSIOLOGY EDUCATION – DECEMBER 1998
S126
Downloaded from journals.physiology.org/journal/advances (187.106.035.231) on February 19, 2024.
A P S R E F R E S H E R C O U R S E R E P O R T
often slow to transfer basic concepts from the physi- maintained constant by the AVP feedback system, and
cal sciences to biology. For example, students fre- as a consequence, plasma Na1 concentration is also
quently confuse the concentration of a solute with the normally kept quite constant. If the plasma Na1
amount of the solute in a fluid compartment. Students concentration is constant, one can then immediately
should be led to recognize that a concentration is see that ECF volume is proportional to the total body
defined by an amount of the solute in a given volume. Na1 and is not reflected by the plasma Na1 concentra-
Similarly, they need to grasp the concept that mass tion. In other words, if PNa . constant, then ECF
flow, which is the amount of material flowing per unit volume is proportional to the amount of Na1 in the
of time at some point along the nephron (for example, body by rearrangement of the equation
the rate of filtration or excretion, or the rate of Na1
flow at the end of the proximal tubule), is equal to the total body amount of Na1
PNa < < constant
product of the concentration and the flow rate, shown ECF volume
with the use of some sample units as
thus
Mass flow (mmol / min) 5 concentration (mmol/l)
3 flow (l/min) ECF volume ~ total body amount of Na1
In summary, changes in plasma osmolality are usually
Students lacking this understanding often do not
indicative of problems in water balance, whereas
appreciate why, in mannitol diuresis, more Na1 is
changes in ECF volume are related to body Na1
excreted (a natriuresis) despite the fact that the Na1
balance.
concentration of the tubular fluid in the late proximal
tubule is less than that in the plasma and thus less than
Another difficult quantitative concept is that of a
normal. As simple as the concept may seem, the
‘‘steady state.’’ Students can intuitively appreciate
teacher must be sure that the students appreciate that
homeostasis in terms of the maintenance of a constant
the mass flow of Na1 at this point in the nephron is volume and composition of body fluid compartments,
greater because of the highly increased flow rate which can be attributed to the fact that daily intake
despite the lower Na1 concentration. and production of substances are matched by an
equivalent daily output of those substances. This
Similarly, the determinants of concentration need to matching of output to input and production is a steady
be appreciated by the student to understand why the state, and when that steady state is poised with ideal
plasma Na1 concentration is not an indicator of (i.e., normal) body fluid volumes and composition, the
extracellular fluid (ECF) volume. Because Na1 and its condition is referred to as homeostasis. Whenever
associated anions make up most of the osmolality of there are disturbances of body solute, water, or
the plasma, the plasma Na1 concentration is a good acid-base balance, a new steady state is generally
indicator of the plasma osmolality, which can be achieved fairly quickly, but that steady state repre-
approximated as sents a nonideal steady state, one not equivalent to
homeostasis. I have found it very useful to present
Posm < 2 ? PNa these concepts to the student in terms of a very
important clinical parameter that is used to assess the
or yet more exactly as progress of renal disease—the plasma creatinine con-
centration or creatinine clearance.
Pglucose BUN
Posm < 2 ? PNa 1 1
18 2.4 As shown in Fig. 8, for a steady state of creatinine to
exist in the body, the rate of creatinine excretion must
where Posm, PNa, and Pglucose are, respectively, the be equal to the rate of creatinine production by
plasma osmolality, Na1 (in mmol/l), and glucose (in metabolism. This rate of production is ,1.8 g for a
mg/dl) concentrations, and BUN is the blood urea typical (70–80 kg) adult human on a Western diet.
nitrogen (in mg/dl). Plasma osmolality is normally Neglecting the small amount of secretion, we can
VOLUME 20 : NUMBER 1 – ADVANCES IN PHYSIOLOGY EDUCATION – DECEMBER 1998
S127
Downloaded from journals.physiology.org/journal/advances (187.106.035.231) on February 19, 2024.
A P S R E F R E S H E R C O U R S E R E P O R T
The question that I challenge the students with is,
‘‘How quickly is such a new steady state achieved?’’ I
choose the hypothetical example of removing one
kidney and assuming no compensation by the other
kidney and no other complications. Most students can
quickly determine that the patient will come back into
balance when the plasma creatinine concentration
has doubled so that at one-half the GFR and double the
plasma creatinine concentration, the excretion rate is
FIG. 8. equal to the normal production rate. How long would
Steady-state balance of creatinine in the body persists it take to attain this new steady state after removal of
even in patients with chronic renal failure, but only the one kidney? A rigorous solution of this problem
because the plasma creatinine concentration (PCr) requires compartmental analysis with the solution of a
rises to make excretion equal production. This ex-
ample assumes a daily creatinine production of 1.8
differential equation, the result of which is shown by
g/day, which is typical for a 70- to 80-kg adult. GFR, the plot in Fig. 9. However, I would never attempt to
glomerular filtration rate. explain it to any student (other than an engineer) in
approximate that the creatinine excretion rate is equal
to the creatinine filtration rate, which, in turn, is equal
to the product of the glomerular filtration rate (GFR)
and the plasma creatinine concentration. This rate of
filtration must be equal to the rate of excretion or the
rate of production of ,1.8 grams/day. Thus the
plasma creatinine concentration is inversely propor-
tional to the GFR as shown by the last equation in Fig.
8. We are all familiar with the graphical form of the
last equation in Fig. 8, which shows an asymptotically
increasing plasma creatinine concentration with pro-
gressive reductions in GFR.
This analysis certainly helps the student to understand
why the plasma creatinine concentration is a fairly
good indicator of the glomerular filtration rate, pro-
vided there are no large fluctuations in diet or meta-
bolic rate. However, I find that most students still have
a preconception that, in chronic renal failure, plasma
creatinine concentration and BUN are elevated be-
cause the kidney is excreting lesser amounts of these
by-products of metabolism than are being produced.
This assumption seems to be intuitively connected
with the idea of kidney failure. However, the student FIG. 9.
needs to appreciate that a patient with chronic renal Time required for reestablishment of creatinine steady-
failure is actually in creatinine balance, i.e., a steady state balance if GFR were to be instantaneously re-
duced from 180 to 90 l/day at time 0. The solution of
state with respect to creatinine, but only when the
the compartmental model (see Quantitative problems
plasma creatinine concentration has increased so that are essential) assumes a daily creatinine production
the rate of creatinine filtration is equal to the rate of rate of 1.8 g/day, and that creatinine is uniformly
production. distributed in a total body water volume of 40 liters.
VOLUME 20 : NUMBER 1 – ADVANCES IN PHYSIOLOGY EDUCATION – DECEMBER 1998
S128
Downloaded from journals.physiology.org/journal/advances (187.106.035.231) on February 19, 2024.
A P S R E F R E S H E R C O U R S E R E P O R T
FIG. 10.
Effect of furosemide on salt and water balance and urinary concentrating ability. An
example of integrating detailed mechanistic information from all segments of the
nephron into an understanding of ‘‘whole kidney function’’ in an important clinical
problem, i.e., why do ‘‘loop diuretics’’ tend to cause hypokalemia, divalent cation loss,
and diminished urine concentrating ability? DCT, distal convoluted tubule; CCD, cortical
collecting duct.
this way. Instead, I attempt to get the student to REVIEW: PUTTING MULTIPLE BASIC
appreciate the ‘‘ball park’’ rate at which the plasma MECHANISMS INTO AN INTEGRATED PICTURE
creatinine concentration would change based on the OF ‘‘WHOLE KIDNEY’’ FUNCTION
total body content of creatinine and the rate of its
When I review salt and water transport systems in the
production. As outlined at the bottom of Fig. 9, if one
assumes that creatinine is distributed at a concentra- kidney, I try to provide the student with examples that
tion of ,1 mg/dl uniformly throughout the total body integrate multiple mechanisms of nephron function
water volume of ,40 liters, then the total body and the daily balance of solutes and water by the body.
content of creatinine would be ,400 mg. If the daily One such example is the effect of the diuretic furose-
rate of creatinine production is 1,800 mg/day, the mide, as shown in Fig. 10. Of course, the primary
student can then readily appreciate that it will prob- action of furosemide as denoted by step 1 in Fig. 10 is
ably take less than one day for the patient to come into inhibition of BSC1, which results in decreased reab-
a new steady state of creatinine balance, even with sorption of NaCl, K1, and divalent cations and also
this very abrupt decrease in GFR. The important point results in a decrease in the medullary hypertonicity.
to be made here is that until end-stage renal disease is Second, the reduction in medullary hypertonicity
reached, the individual with chronic renal failure is decreases osmotic reabsorption of water from the
really in a steady state with regard to the balance of descending limb of the loop of Henle. Third, this
water and solutes by the kidney. However, this steady decrease in water extraction and salt reabsorption in
state can be achieved only with nonideal or nonhomeo- the loop of Henle results in increased water and salt
static fluid volumes and solute concentrations. Again, delivery to the distal convoluted tubule and collecting
I find these quantitative details to be of the utmost duct. The presence of an increased Na1 concentration
importance for the student to appreciate what is really enhances the driving force for Na1 reabsorption via
meant by salt (or solute) and water balance. the amiloride-sensitive Na1 channel in the principal
VOLUME 20 : NUMBER 1 – ADVANCES IN PHYSIOLOGY EDUCATION – DECEMBER 1998
S129
Downloaded from journals.physiology.org/journal/advances (187.106.035.231) on February 19, 2024.
A P S R E F R E S H E R C O U R S E R E P O R T
cells of the collecting duct and also depolarizes the 4. Barfuss, D. W., and J. A. Schafer. Rate of formation and
luminal membrane so that there is an increase driving composition of absorbate from proximal nephron segments.
Am. J. Physiol. 247 (Renal Fluid Electrolyte Physiol. 16):
force for K1 secretion. The overall result, shown as F117–F129, 1984.
step 5 of Fig. 10, is an increased excretion of NaCl, 5. Canessa, C. M., L. Shild, G. Buell, B. Thorens, I. Gautschi,
water, K1, and divalent cations, and the urine osmolal- J.-D. Horisberger, and B. C. Rossier. Amiloride-sensitive
ity approaches isotonicity. The loss of salt and water in epithelial Na1 channel is made of three homologous subunits.
turn serves as a stimulus to renin production, leading Nature 367: 463–467, 1994.
6. Chang, S. S., S. Grunder, A. Hanukoglu, A. Rosler, P. M.
to increased aldosterone secretion by the adrenal
Mathew, I. Hanukoglu, L. Schild, Y. Lu, R. A. Shimkets, C.
glands, which in turn, enhances step 4, i.e., increased Nelson-Williams, B. C. Rossier, and R. P. Lifton. Mutations
reabsorption of Na1 and secretion of K1 in the in subunits of the epithelial sodium channel cause salt wasting
principal cells of the collecting duct. Obviously, with hyperkalaemic acidosis, pseudohypoaldosteronism type 1.
exactly the same sequence of events would occur if Nat. Genet. 12: 248–253, 1996.
7. Chou, C. L., T. Ma, B. Yang, M. A. Knepper, and A. S.
there were a loss-of-function mutation in BSC1, as
Verkman. Fourfold reduction of water permeability in inner
occurs in Bartter’s syndrome (see above). One can medullary collecting duct of aquaporin-4 knockout mice. Am. J.
also discuss the changes in reabsorption of Ca21 and Physiol. 274 (Cell Physiol. 43): C549–C554, 1998.
Mg21 and how the balance of these divalent cations is 8. Hebert, S. C., and S. C. Gullans. Editorial comment on ‘‘The
affected. Using schema such as these, the teacher can molecular basis of inherited alkalosis: Bartter’s and Gitelman’s
review and reinforce many of the important details of syndrome.’’ Am. J. Physiol. 271 (Renal Fluid Electrolyte
Physiol. 40): F957–F959, 1996.
the transport processes involved in salt and water 9. Hediger, M. A., M. J. Coady, T. S. Ikeda, and E. M. Wright.
reabsorption, while at the same time integrating those Expression cloning and cDNA sequencing of the Na1/glucose
processes to develop a comprehensive picture of co-transporter. Nature 330: 379–381, 1987.
‘‘whole kidney’’ physiology and pathophysiology. 10. Hediger, M. A., and D. B. Rhoads. Molecular physiology of
sodium-glucose cotransporters. Physiol. Rev. 74: 993–1026,
I acknowledge my own teachers, particularly Drs. Horace Daven- 1994.
port, John Jacquez, Richard Malvin, and Arthur Vander at the 11. Kamel, K. S., M. L. Halperin, M. D. Faber, S. P. Steigerwalt,
University of Michigan, and Dr. Thomas Andreoli, who was my C. Heilig, and R. G. Narins. Disorders of potassium balance.
postdoctoral mentor. All of these individuals held the teaching art in In: The Kidney (5th ed.), edited by B. M. Brenner. Philadelphia,
high esteem and were recognized by students for the excellence of PA: Saunders, 1996, p. 999–1037.
their teaching. My first-hand exposure to such masters of the art 12. Knepper, M. A. Molecular physiology of urinary concentrating
were essential to my own development. What examples! I am also mechanism: regulation of aquaporin water channels by vasopres-
grateful for the patience of my students, past and present, and for sin. Am. J. Physiol. 272 (Renal Physiol. 41): F3–F12, 1997.
the questions they constantly ask that made me reevaluate what and 13. Liddle, G. W., T. Bledsoe, and W. S. Coppage. A familial renal
how I am teaching. I very much appreciate the helpful comments disorder simulating primary aldosteronism but with negligible
on the manuscript by Dr. Teresa Wilborn and Ryan Morris. aldosterone secretion. Trans. Am. Assoc. Physicians. 76: 199–
213, 1963.
Research support for some of the studies mentioned from this lab 14. Ma, T., B. Yang, A. Gillespie, E. J. Carlson, C. J. Epstein,
came from National Institute of Diabetes and Digestive and Kidney and A. S. Verkman. Severely impaired concentrating ability in
Diseases Grants DK-25519 and DK-45768. transgenic mice lacking aquaporin-1 water channels (Abstract).
Address for reprint requests: J. A. Schafer, Dept. of Physiology and FASEB J. 12: A331, 1998.
Biophysics, 958 MCLM Bldg., 1918 Univ. Blvd., Birmingham, AL 15. Martı́n, M. G., E. Turk, M. P. Lostao, C. Kerner, and E. M.
35294-0005. Wright. Defects in Na1 glucose cotransporter (SGLT1) traffick-
ing and function cause glucose-galactose malabsorption. Nat.
References Genet. 12: 216–220, 1996.
16. Mune, T., F. M. Rogerson, H. Nikkilä, A. K. Agarwal, and
1. Agre, P., G. M. Preston, B. L. Smith, J. S. Jung, S. Raina, C. P. C. White. Human hypertension caused by mutations in the
Moon, W. B. Guggino, and S. Nielsen. Aquaporin CHIP: the kidney isozyme of 11b-hydroxysteroid dehydrogenase. Nat.
archetypal molecular water channel. Am. J. Physiol. 265 (Renal Genet. 10: 394–399, 1995.
Fluid Electrolyte Physiol. 34): F463–F476, 1993. 17. Pollak, M. R., V. B. Delaney, R. M. Graham, and S. C.
2. Andreoli, T. E., and J. A. Schafer. External solution driving Hebert. Gitelman’s Syndrome (Bartter’s variant) maps to the
forces for isotonic fluid absorption in proximal tubules. Federa- thiazide-sensitive cotransporter gene locus on chromosome
tion Proc. 38: 154–160, 1979. 16q13 in a large kindred. J. Am. Soc. Nephrol. 7: 2244–2248,
3. Barfuss, D. W., and J. A. Schafer. Differences in active and 1996.
passive glucose transport along the proximal nephron. Am. J. 18. Schafer, J. A. Transepithelial osmolality differences, hydraulic
Physiol. 241 (Renal Fluid Electrolyte Physiol. 10): F322–F332, conductivities, and volume absorption in the proximal tubule.
1981. Annu. Rev. Physiol. 52: 709–726, 1990.
VOLUME 20 : NUMBER 1 – ADVANCES IN PHYSIOLOGY EDUCATION – DECEMBER 1998
S130
Downloaded from journals.physiology.org/journal/advances (187.106.035.231) on February 19, 2024.
A P S R E F R E S H E R C O U R S E R E P O R T
19. Schafer, J. A., and J. C. Williams, Jr. Transport of metabolic 24. Warnock, D. G. Liddle syndrome: an autosomal dominant form
substrates by the proximal nephron. Annu. Rev. Physiol. 47: of human hypertension. Kidney Int. 53: 18–24, 1998.
103–125, 1985. 25. Whorwood, C. B., J. I. Mason, M. L. Ricketts, A. J. Howie,
20. Shimkets, R. A., D. G. Warnock, C. M. Bositis, C. Nelson- and P. M. Stewart. Detection of human 11b-hydroxysteroid
Williams, J. H. Hansson, M. Schambelan, J. Gill, Jr., S. dehydrogenase isoforms using reverse-transcriptase-polymer-
Ulick, R. V. Milora, J. W. Findling, C. M. Canessa, B. C. ase chain reaction and localization of the type 2 isoform to renal
Rossier, and R. P. Lifton. Liddle’s syndrome: heritable human collecting ducts. Mol. Cell. Endocrinol. 110: R7–R12, 1995.
hypertension caused by mutations in the beta subunit of the 26. Whorwood, C. B., M. C. Sheppard, and P. M. Steward.
epithelial sodium channel. Cell 79: 407–414, 1994. Licorice inhibits 11b-hydroxysteroid dehydrogenase ribo-
21. Simon, D. B., and R. P. Lifton. The molecular basis of nucleic acid level and potentiates glucocorticoid action. Endo-
inherited hypokalemic alkalosis: Bartter’s and Gitelman’s syn- crinology 132: 2287–2296, 1993.
dromes. Am. J. Physiol. 271 (Renal Fluid Electrolyte Physiol. 27. Whorwood, C. B., and P. M. Stewart. Human hypertension
40): F961–F966, 1996. caused by mutations in the 11b-hydroxysteroid dehydrogenase
22. Turner, R. J., and A. Moran. Heterogeneity of sodium- gene: a molecular analysis of apparent mineralocorticoid ex-
dependent D-glucose transport sites along the proximal tubule: cess. J. Hypertens. Suppl. 14: S19–S24, 1996.
evidence from vesicle studies. Am. J. Physiol. 242 (Renal Fluid 28. Williams, J. C., Jr., and J. A. Schafer. Cortical interstitium as a
Electrolyte Physiol. 11): F406–F414, 1982. site for solute polarization during tubular absorption. Am. J.
23. Verkman, A. S., A. N. Van Hoek, T. H. Ma, A. Frigeri, W. R. Physiol. 254 (Renal Fluid Electrolyte Physiol. 23): F813–F823,
Skach, A. Mitra, B. K. Tamarappoo, and J. Farinas. Water 1988.
transport across mammalian cell membranes. Am. J. Physiol. 29. Wright, E. M. The intestinal Na1/glucose cotransporter. Annu.
270 (Cell Physiol. 39): C12–C30, 1996. Rev. Physiol. 55: 575–589, 1993.
VOLUME 20 : NUMBER 1 – ADVANCES IN PHYSIOLOGY EDUCATION – DECEMBER 1998
S131
Downloaded from journals.physiology.org/journal/advances (187.106.035.231) on February 19, 2024.
You might also like
- Essentials of Anatomy and Physiology 1st Edition Saladin Solutions Manual Full Chapter PDFDocument26 pagesEssentials of Anatomy and Physiology 1st Edition Saladin Solutions Manual Full Chapter PDFarianytebh100% (18)
- PHYS170 SyllabusDocument9 pagesPHYS170 SyllabusjshensonNo ratings yet
- Cultural Diversity and NursingDocument21 pagesCultural Diversity and Nursingfatha83% (6)
- New Ways of Thinking About (And Teaching About) Intestinal Epithelial FunctionDocument10 pagesNew Ways of Thinking About (And Teaching About) Intestinal Epithelial FunctionSinisa RisticNo ratings yet
- A2 Biology Syllabus 9700: Unit 2: Regulation and ControlDocument18 pagesA2 Biology Syllabus 9700: Unit 2: Regulation and ControladuhaikNo ratings yet
- The Kidneys Matter: Johannes Loffing Francois Verrey Carsten A. WagnerDocument3 pagesThe Kidneys Matter: Johannes Loffing Francois Verrey Carsten A. WagnerRania T. SabriNo ratings yet
- Rajiv Gandhi College of Nursing: Sub: Child Health NursingDocument14 pagesRajiv Gandhi College of Nursing: Sub: Child Health NursingS G100% (1)
- Congenital Hydronephrosis Disease or ConditionDocument8 pagesCongenital Hydronephrosis Disease or ConditionIrfan Syauqi AriantoNo ratings yet
- Renal SyllabusDocument16 pagesRenal SyllabusorangenarwhalNo ratings yet
- Homeostasis, The Milieu Intérieur, and The Wisdom of The Nephron 2014 PDFDocument10 pagesHomeostasis, The Milieu Intérieur, and The Wisdom of The Nephron 2014 PDFMg GfNo ratings yet
- Renal Circadian Biorhythms in Lifelong LUTSDocument9 pagesRenal Circadian Biorhythms in Lifelong LUTSMDrakeNo ratings yet
- Clin Physio Funct Imaging - 2013 - Munkholm - Mucociliary Clearance Pathophysiological AspectsDocument7 pagesClin Physio Funct Imaging - 2013 - Munkholm - Mucociliary Clearance Pathophysiological AspectsIkon ikonicNo ratings yet
- Intra Renal Cori CycleDocument21 pagesIntra Renal Cori Cyclesuman palNo ratings yet
- Defecation NcbiDocument19 pagesDefecation NcbimuthiaNo ratings yet
- TFG Paula AceytunoDocument37 pagesTFG Paula AceytunoMaria SilvaNo ratings yet
- Moore LG. 2001. Human Genetic Adaptation To High AltitudeDocument23 pagesMoore LG. 2001. Human Genetic Adaptation To High AltitudeFlor TurcoNo ratings yet
- FLUID, ELECTROLYTE, AND ACID-BASE PHYSIOLOGY - A PROBLEM-BASED APPROACH (4E) (2010) (UnitedVRG) PDFDocument614 pagesFLUID, ELECTROLYTE, AND ACID-BASE PHYSIOLOGY - A PROBLEM-BASED APPROACH (4E) (2010) (UnitedVRG) PDFCristinaLucan100% (2)
- preprints202312.2003.v1Document18 pagespreprints202312.2003.v1Valery Principe MoraNo ratings yet
- (Systems of The Body) Morton, Dion G. - Smith, Margaret E - The Digestive System - Systems of The Body Series (2014, Elsevier Health Sciences UK)Document226 pages(Systems of The Body) Morton, Dion G. - Smith, Margaret E - The Digestive System - Systems of The Body Series (2014, Elsevier Health Sciences UK)lucianandreibedruleaNo ratings yet
- The Surgical Management of Necrotizing Enterocolitis - July 2018Document4 pagesThe Surgical Management of Necrotizing Enterocolitis - July 2018Hengky TanNo ratings yet
- Essentials of Anatomy and Physiology 1st Edition Saladin Solutions ManualDocument5 pagesEssentials of Anatomy and Physiology 1st Edition Saladin Solutions Manualdaineil2td100% (33)
- Pulmonary Surfactant Pathophysiology - Current Models and Open QuestionsDocument11 pagesPulmonary Surfactant Pathophysiology - Current Models and Open QuestionsGabriel Eduardo Castro RiosNo ratings yet
- BIOMEDE 331 - The Belmont LabDocument13 pagesBIOMEDE 331 - The Belmont LabjimNo ratings yet
- 2013 Basic Concepts of Fluid and Electrolyte TherapyDocument137 pages2013 Basic Concepts of Fluid and Electrolyte Therapytd5xb7w4dpNo ratings yet
- (B) Mechanisms of Peptide and Protein Absorption: Hugh N. NellansDocument26 pages(B) Mechanisms of Peptide and Protein Absorption: Hugh N. Nellansuetian111No ratings yet
- Pediatrics in Review 1989 DeWitt 6 12Document10 pagesPediatrics in Review 1989 DeWitt 6 12DewinsNo ratings yet
- Hypertonic Stress in The Kidney: A Necessary Evil: Min Seong Kwon, Sun Woo Lim and H. Moo KwonDocument7 pagesHypertonic Stress in The Kidney: A Necessary Evil: Min Seong Kwon, Sun Woo Lim and H. Moo Kwoncrina1980No ratings yet
- Edwards MurrayreviewDocument4 pagesEdwards MurrayreviewIkha ArsyadNo ratings yet
- Regulation of Renal HemodynamicsDocument15 pagesRegulation of Renal HemodynamicsallerasicNo ratings yet
- Diving Physiology of Marine Mammals and Seabirds, by Paul PonganisDocument3 pagesDiving Physiology of Marine Mammals and Seabirds, by Paul PonganisMissPleyadesNo ratings yet
- Moxham Et Al-2015-Clinical AnatomyDocument11 pagesMoxham Et Al-2015-Clinical AnatomyJohnNo ratings yet
- Diare Non InflamasiDocument4 pagesDiare Non InflamasiSiti MunawwarahNo ratings yet
- Hillaireau H and Couvreur P Nanocarriers Entry inDocument25 pagesHillaireau H and Couvreur P Nanocarriers Entry inrizkymuzakkiNo ratings yet
- Nutritional Support in The Perioperative Period: 4 Fluid Balance and Metabolism in SurgeryDocument29 pagesNutritional Support in The Perioperative Period: 4 Fluid Balance and Metabolism in SurgeryFreddy Negron HuamaniNo ratings yet
- Judul ReferatDocument13 pagesJudul ReferatsyongebobNo ratings yet
- First Year MBBSDocument25 pagesFirst Year MBBSTofik MohammedNo ratings yet
- Osmo LarityDocument17 pagesOsmo LarityTubocurareNo ratings yet
- Biomechanics of The Thorax - ResearchDocument11 pagesBiomechanics of The Thorax - ResearchheriNo ratings yet
- Full Essentials of Anatomy and Physiology 1St Edition Saladin Solutions Manual Online PDF All ChapterDocument28 pagesFull Essentials of Anatomy and Physiology 1St Edition Saladin Solutions Manual Online PDF All Chapterleoneeke-ade-munde957100% (5)
- Teaching & Learning Contract For Yearly Scheme of Work For Form Five Biology 2014Document13 pagesTeaching & Learning Contract For Yearly Scheme of Work For Form Five Biology 2014halimi_foaedNo ratings yet
- Silverthorne 2018-Learning by Osmosis An Approach To Teaching Osmolarity and TonicityDocument10 pagesSilverthorne 2018-Learning by Osmosis An Approach To Teaching Osmolarity and TonicityIlham NugrohoNo ratings yet
- Wang 14te408 Fieldlesson2Document8 pagesWang 14te408 Fieldlesson2api-251571132No ratings yet
- Perspectives: Coexistence of Passive and Carrier-Mediated Processes in Drug TransportDocument18 pagesPerspectives: Coexistence of Passive and Carrier-Mediated Processes in Drug TransportzaynmalikNo ratings yet
- Update On Foregut Molecular Embryology and Role of Regenerative Medicine TherapiesDocument9 pagesUpdate On Foregut Molecular Embryology and Role of Regenerative Medicine TherapiesmikeNo ratings yet
- BiomekanikDocument474 pagesBiomekanikRicaariani MyGeisha SmashblastNo ratings yet
- Instant Download PDF Essentials of Anatomy and Physiology 1st Edition Saladin Solutions Manual Full ChapterDocument28 pagesInstant Download PDF Essentials of Anatomy and Physiology 1st Edition Saladin Solutions Manual Full Chapteralvimxhexhi100% (9)
- Full download Essentials of Anatomy and Physiology 1st Edition Saladin Solutions Manual all chapter 2024 pdfDocument28 pagesFull download Essentials of Anatomy and Physiology 1st Edition Saladin Solutions Manual all chapter 2024 pdfmukatimoorut100% (9)
- Cerebellar Ataxia: Pathophysiology and RehabilitationDocument24 pagesCerebellar Ataxia: Pathophysiology and RehabilitationNistara Singh ChawlaNo ratings yet
- ANPH-M1-CU2. The Cell & Cellular Metabolism and Reproduction (Mitosis and Meiosis)Document26 pagesANPH-M1-CU2. The Cell & Cellular Metabolism and Reproduction (Mitosis and Meiosis)ajdNo ratings yet
- Pathology of the Bile Duct 2017Document215 pagesPathology of the Bile Duct 2017KaruminaNo ratings yet
- Seminars in Cell & Developmental BiologyDocument10 pagesSeminars in Cell & Developmental BiologyagathapradanaNo ratings yet
- Pathology of The Bile Duct 2017 - Yasuni Nakanuma PDFDocument215 pagesPathology of The Bile Duct 2017 - Yasuni Nakanuma PDFHîrjoabă IoanNo ratings yet
- Pathophysiologic, Translational and Clinical Aspects of Postoperative Ileus - A ReviewDocument15 pagesPathophysiologic, Translational and Clinical Aspects of Postoperative Ileus - A ReviewRebecca BlackburnNo ratings yet
- Infectious Diarrhea: Cellular and Molecular MechanismsDocument18 pagesInfectious Diarrhea: Cellular and Molecular Mechanismsmedicalfuture2uNo ratings yet
- Session 1 Intro To Physiology - Cell PhysiologyDocument13 pagesSession 1 Intro To Physiology - Cell Physiologyyuto.daan.swuNo ratings yet
- PhysiomeDocument4 pagesPhysiomesuman palNo ratings yet
- RPT Biology Form 5Document18 pagesRPT Biology Form 5Mohamad Khairie Rano IbrahimNo ratings yet
- Frontiers in Respiratory Physiology - Grand ChallengeDocument2 pagesFrontiers in Respiratory Physiology - Grand ChallengeAlfi OktafaniNo ratings yet
- Proyecto DialisisDocument6 pagesProyecto DialisisVh TR100% (1)
- Basic Concepts of Fluid and Electrolyte TherapyDocument136 pagesBasic Concepts of Fluid and Electrolyte Therapymuhammad ajiNo ratings yet
- Interpretation of Urodynamic Studies: A Case Study-Based GuideFrom EverandInterpretation of Urodynamic Studies: A Case Study-Based GuideNo ratings yet
- Performance Task No. 2-Arc, Chord and Central AnglesDocument2 pagesPerformance Task No. 2-Arc, Chord and Central AnglesJell De Veas TorregozaNo ratings yet
- Hull Millwork. Newsletter 2003-10 BWDocument3 pagesHull Millwork. Newsletter 2003-10 BWJohn Evans0% (1)
- Primary Health CareDocument30 pagesPrimary Health CareHydra Olivar - PantilganNo ratings yet
- Semidetailed Lesson Plan Boyle's Law JhsDocument3 pagesSemidetailed Lesson Plan Boyle's Law JhsTeacher Derick DaetNo ratings yet
- Seven Qualities of A Good LeaderDocument1 pageSeven Qualities of A Good LeaderToronto_ScorpionsNo ratings yet
- Itinerary of TravelDocument4 pagesItinerary of TravelChelle ChelleNo ratings yet
- 7.1 HashCalcDocument5 pages7.1 HashCalcBolajiKoyiNo ratings yet
- Biological Psychology - ppt12Document15 pagesBiological Psychology - ppt12avirgNo ratings yet
- Reflective Journal - 9Document3 pagesReflective Journal - 9Katriel Ziv LasNo ratings yet
- GEP1 - A089 - Orientation 10-2022Document32 pagesGEP1 - A089 - Orientation 10-2022Bang LeNo ratings yet
- Summary of Testing Phases PDFDocument9 pagesSummary of Testing Phases PDFTamil SelviNo ratings yet
- The Fight Over The Rizal LawDocument2 pagesThe Fight Over The Rizal LawDarwin FlamencoNo ratings yet
- Literature Review On HR Policies and Its ImplementationDocument5 pagesLiterature Review On HR Policies and Its ImplementationbctfnerifNo ratings yet
- BS PscyhDocument3 pagesBS Pscyhmarl labitadNo ratings yet
- Rhyme TimeDocument14 pagesRhyme TimeDabhi AnilNo ratings yet
- Midterm Film Review PaperDocument3 pagesMidterm Film Review PaperEnes KaraibrahimogluNo ratings yet
- IBTL Final CompressedDocument104 pagesIBTL Final CompressedSheila B. ParadoNo ratings yet
- IB Math AI HL Practice Exam - Voronoi DiagramsDocument1 pageIB Math AI HL Practice Exam - Voronoi DiagramsMardhiyah Mardis100% (1)
- Md. Atiqur Rahman PDFDocument1 pageMd. Atiqur Rahman PDFatikur atikNo ratings yet
- UtiDocument2 pagesUtiBasant karn50% (2)
- AI EvaluationDocument24 pagesAI Evaluationashmita11No ratings yet
- Teach Your Parents KenKenDocument4 pagesTeach Your Parents KenKenJames ConnollyNo ratings yet
- Susan Wallace Hypno Woman Run by A Woman 2013Document16 pagesSusan Wallace Hypno Woman Run by A Woman 2013Bob Cook100% (1)
- Online Meeting Literacy Reflection RubricDocument2 pagesOnline Meeting Literacy Reflection RubricMia mooreNo ratings yet
- ACADEMIC TASK #3 - Reflection Paper On ECEDucationDocument3 pagesACADEMIC TASK #3 - Reflection Paper On ECEDucationGne Rose GañoNo ratings yet
- Lesson Plan - Educ27Document6 pagesLesson Plan - Educ27Alain Delon Lim SerinoNo ratings yet
- NSTP Chapter 3Document32 pagesNSTP Chapter 3Grecel Joy BaloteNo ratings yet
- Unit 1 General Test: Name - Julian Camilo Perez MendezDocument12 pagesUnit 1 General Test: Name - Julian Camilo Perez MendezCarlos Daniel Mendez BonillaNo ratings yet
- MDmetrix Names Caradigm Co-Founder and COO Warren Ratliff As Chief Executive OfficerDocument3 pagesMDmetrix Names Caradigm Co-Founder and COO Warren Ratliff As Chief Executive OfficerPR.comNo ratings yet