Professional Documents
Culture Documents
TVP-2020-1112 Managing Feline Urethral Obstruction
TVP-2020-1112 Managing Feline Urethral Obstruction
Uploaded by
Lucas Dos Santos MacedoCopyright:
Available Formats
You might also like
- Ehrlichiosisand Anaplasmosis:: An UpdateDocument42 pagesEhrlichiosisand Anaplasmosis:: An UpdateMargarita CCNo ratings yet
- Canine Aural HematomaDocument6 pagesCanine Aural Hematomakenikenranisa100% (1)
- Fim Item ScoringDocument10 pagesFim Item Scoringhaythamalshikh0120% (1)
- Paraphimosis in The DogDocument4 pagesParaphimosis in The DogErick GarciaNo ratings yet
- Lymphoid Leukemia in DogsDocument15 pagesLymphoid Leukemia in Dogstaner_soysurenNo ratings yet
- How To Anaesthetize A GiraffeDocument4 pagesHow To Anaesthetize A Giraffeltrathie3087100% (2)
- Canine InsulinomaDocument5 pagesCanine Insulinomasoff4ikaNo ratings yet
- Mucocele 2Document13 pagesMucocele 2FEY YENG SOFIA FUNG GUADALUPENo ratings yet
- AHS Canine Guidelines 11 13 20Document37 pagesAHS Canine Guidelines 11 13 20Ana Clara Pessôa100% (1)
- FELINE-Clinical Forms of Acquired Myasthenia Gravis in CatsDocument7 pagesFELINE-Clinical Forms of Acquired Myasthenia Gravis in Catstaner_soysurenNo ratings yet
- Materia Medica PuraDocument224 pagesMateria Medica PuraMorgan CabreraNo ratings yet
- Enf Discal Intervertebral (II)Document16 pagesEnf Discal Intervertebral (II)pedro jaraNo ratings yet
- CANINE-Pathophysiology of Organ Failure in Severe Acute Pancreatitis in DogsDocument10 pagesCANINE-Pathophysiology of Organ Failure in Severe Acute Pancreatitis in Dogstaner_soysurenNo ratings yet
- Diagnosis of Pancreatitis in Dogs and Cats: ReviewDocument14 pagesDiagnosis of Pancreatitis in Dogs and Cats: ReviewMiruna ChiriacNo ratings yet
- general systemic states د.عزيزةDocument75 pagesgeneral systemic states د.عزيزةAhmed Hamdy NaDa100% (2)
- Fever of Unknown OriginDocument4 pagesFever of Unknown OriginPatricia PopNo ratings yet
- Immunotherapy With Banerji ProtocolDocument43 pagesImmunotherapy With Banerji ProtocolSur E JahanNo ratings yet
- Feline Vocalization - Excessive: Why Is My Cat Persistently Crying?Document4 pagesFeline Vocalization - Excessive: Why Is My Cat Persistently Crying?Brook Farm Veterinary CenterNo ratings yet
- Veterinary Focus 27.1Document52 pagesVeterinary Focus 27.1Νίκος ΚριτσοταλάκηςNo ratings yet
- Monografi AtropinDocument48 pagesMonografi AtropinWahyu AgustinaNo ratings yet
- Siamese CatDocument5 pagesSiamese CatDummy1 AccountNo ratings yet
- TX TableDocument1 pageTX TableLaureece Salm ApduhanNo ratings yet
- Top 5 Leukogram PatternsDocument3 pagesTop 5 Leukogram PatternsSandraHermosilloNo ratings yet
- Atlas of Gastrointestinal Endoscopy in Dogs and CatsDocument8 pagesAtlas of Gastrointestinal Endoscopy in Dogs and CatsDama Ayu RaniNo ratings yet
- L19 - Pelvic Pain & EndometriosisDocument8 pagesL19 - Pelvic Pain & EndometriosisBrandonRyanF.MosidinNo ratings yet
- Howto Companion April2008Document3 pagesHowto Companion April2008lybrakissNo ratings yet
- Acute Pain in CatsDocument10 pagesAcute Pain in CatsLINDA BELMONTNo ratings yet
- FELINE-Peritoneopericardial Diaphramatic Hernia in CatsDocument13 pagesFELINE-Peritoneopericardial Diaphramatic Hernia in Catstaner_soysuren100% (1)
- FelineCalicivirus FactSheet PDFDocument5 pagesFelineCalicivirus FactSheet PDFJuniClaudia13No ratings yet
- Brown C (2013) Patient Care Report For Feline Patient With Urethral ObstructionDocument5 pagesBrown C (2013) Patient Care Report For Feline Patient With Urethral ObstructionRob PNo ratings yet
- Anestesia EquinosDocument26 pagesAnestesia EquinosKiimBerly RcNo ratings yet
- Suspensory Ligament Rupture Tech During Small Animal OH PDFDocument8 pagesSuspensory Ligament Rupture Tech During Small Animal OH PDFRiesky NudialestariNo ratings yet
- AnaplasmosisDocument1 pageAnaplasmosisDumapis RichardNo ratings yet
- PDF Small Animal Medical Differential Diagnosis A Book of Lists Mark S Thompson Ebook Full ChapterDocument53 pagesPDF Small Animal Medical Differential Diagnosis A Book of Lists Mark S Thompson Ebook Full Chapterelaine.dawson903100% (1)
- In Practice Blood Transfusion in Dogs and Cats1Document7 pagesIn Practice Blood Transfusion in Dogs and Cats1何元No ratings yet
- Therapeutic Diet What We Need To ConsiderDocument4 pagesTherapeutic Diet What We Need To Consideranarosli251No ratings yet
- Sni 3950-2014Document88 pagesSni 3950-2014Dya Yda'sNo ratings yet
- 4 Diabetes MellitusDocument26 pages4 Diabetes MellitusnomiskemalNo ratings yet
- ABC of Emergency Vet Triage 1691081646Document15 pagesABC of Emergency Vet Triage 1691081646Alina TeodorescuNo ratings yet
- CANINE-PAthogenesis of Acute Canine Gastric Dilatation-Volvulus SyndromDocument7 pagesCANINE-PAthogenesis of Acute Canine Gastric Dilatation-Volvulus Syndromtaner_soysurenNo ratings yet
- Biomedical Therapy: Journal ofDocument16 pagesBiomedical Therapy: Journal ofantoniojgteixeira100% (1)
- Medicine and SurgeryDocument26 pagesMedicine and SurgerySophia Mitz Aya-ayNo ratings yet
- Veterinary Hospital AbstractDocument1 pageVeterinary Hospital AbstractMichelleNo ratings yet
- A Aha Diabetes GuidelinesDocument10 pagesA Aha Diabetes GuidelinesOvidiu PinteaNo ratings yet
- 01 Redalyc Martinez RizoDocument14 pages01 Redalyc Martinez RizoStefanie Valeria Espinoza TorrakaNo ratings yet
- Wound Care Management For The Equine PractitionerDocument212 pagesWound Care Management For The Equine PractitionerLucia ZamoloNo ratings yet
- Canine Atopic DermatitisDocument16 pagesCanine Atopic Dermatitisserbanbogdans536667% (3)
- Canine Mast Cell TumorsDocument5 pagesCanine Mast Cell TumorsCarol LeslieNo ratings yet
- Colic in HorsesDocument2 pagesColic in HorsesRamos SHNo ratings yet
- Rumen MotilityDocument32 pagesRumen MotilityAbhay Singh100% (1)
- Urinary Catheter Placement For Feline ObstructionDocument6 pagesUrinary Catheter Placement For Feline ObstructionWilliam ChandlerNo ratings yet
- FELINE - Chronic Bacterial Skin Infections in CatsDocument9 pagesFELINE - Chronic Bacterial Skin Infections in Catstaner_soysurenNo ratings yet
- Clinical Canine and Feline Reproduction: Evidence-Based AnswersFrom EverandClinical Canine and Feline Reproduction: Evidence-Based AnswersNo ratings yet
- Cephalosporins in Veterinary MedicineDocument23 pagesCephalosporins in Veterinary MedicineSunil100% (3)
- CANINE-Mechanism of Thrombocytopenia in Dogs With CancerDocument11 pagesCANINE-Mechanism of Thrombocytopenia in Dogs With Cancertaner_soysuren100% (1)
- Feline Acute Kidney Injury. 2. Approach To Diagnosis, Treatment and PrognosisDocument9 pagesFeline Acute Kidney Injury. 2. Approach To Diagnosis, Treatment and PrognosisMartín QuirogaNo ratings yet
- Review and Update of Benign PRDocument6 pagesReview and Update of Benign PRAgung KaryawinaraNo ratings yet
- The Laboratory Diagnosis of Feline Kidney DiseaseDocument7 pagesThe Laboratory Diagnosis of Feline Kidney DiseaseCabinet VeterinarNo ratings yet
- Diagnosis and Management of Acute Pancreatitis andDocument11 pagesDiagnosis and Management of Acute Pancreatitis andMarcelitaTaliaDuwiriNo ratings yet
- 2011 - AASLD - Management of Acute Liver FailureDocument22 pages2011 - AASLD - Management of Acute Liver FailuremohamedelsayedelmenyawyNo ratings yet
- Piis0085253815527324 PDFDocument5 pagesPiis0085253815527324 PDFdodong skyroseNo ratings yet
- CATHETERIZATIONDocument3 pagesCATHETERIZATIONrnrmmanphdNo ratings yet
- Bladder Irrigation Toolkit PDFDocument9 pagesBladder Irrigation Toolkit PDFJanuardi IndraNo ratings yet
- Implementing An Evidence-Based Practice Protocol For Prevention of Catheterized Associated Urinary Tract Infections in A Progressive Care UnitDocument9 pagesImplementing An Evidence-Based Practice Protocol For Prevention of Catheterized Associated Urinary Tract Infections in A Progressive Care UnitLina Mahayaty SembiringNo ratings yet
- Surgical Instrumentation: Iii. Grasping and HoldingDocument37 pagesSurgical Instrumentation: Iii. Grasping and Holdingkaren carpioNo ratings yet
- Abdellah's TheoryDocument6 pagesAbdellah's TheoryBaldeep GrewalNo ratings yet
- Clinical Guidelines (Nursing) - Indwelling Urinary Catheter - Insertion and Ongoing CareDocument8 pagesClinical Guidelines (Nursing) - Indwelling Urinary Catheter - Insertion and Ongoing CareLeeNo ratings yet
- Fundamentals Mt2 NovDocument16 pagesFundamentals Mt2 NovRika MaeNo ratings yet
- Urinary Incontinence ModuleDocument103 pagesUrinary Incontinence Modulesny007No ratings yet
- Infection Control Assessment ToolDocument30 pagesInfection Control Assessment ToolPMNo ratings yet
- DME Fee Schedule WCB PDFDocument34 pagesDME Fee Schedule WCB PDFMarina BroniNo ratings yet
- Urinary Catheter in A HorseDocument6 pagesUrinary Catheter in A Horsemouxritsa_83No ratings yet
- Nursing and Surgical Tender Items List 2021-22Document20 pagesNursing and Surgical Tender Items List 2021-22Muhammad Aqeel IrshadNo ratings yet
- Urine Incontinence Care: Urine Catheters Urine Bags AccessoriesDocument24 pagesUrine Incontinence Care: Urine Catheters Urine Bags AccessoriesMerveNo ratings yet
- Urinary Catheterization For PediatricsDocument6 pagesUrinary Catheterization For PediatricsMichael Montinola100% (1)
- PrelimDocument6 pagesPrelimCutypieCyrlah BarrientosNo ratings yet
- Previous Board Exam Questions No RatioDocument56 pagesPrevious Board Exam Questions No RatioNovemia Rose TisonNo ratings yet
- Article Bladder RetrainingDocument9 pagesArticle Bladder RetrainingRaenette DavidNo ratings yet
- Diagnostic Imaging of Lower Urinary Tract DiseaseDocument25 pagesDiagnostic Imaging of Lower Urinary Tract DiseaseSoyKlicheRodriguezNo ratings yet
- Urethral Trauma - Injuries Poisoning - MSD Manual Professional EditionDocument2 pagesUrethral Trauma - Injuries Poisoning - MSD Manual Professional EditionNaufal NaswanNo ratings yet
- Model Answer of Formative Written OSCADocument6 pagesModel Answer of Formative Written OSCAAhmed SamahaNo ratings yet
- Thomas M Hooton, MD Kalpana Gupta, MD, MPH Stephen B Calderwood, MD Allyson Bloom, MDDocument14 pagesThomas M Hooton, MD Kalpana Gupta, MD, MPH Stephen B Calderwood, MD Allyson Bloom, MDMusicBestLiveNo ratings yet
- Groupd Ebp PresentationDocument38 pagesGroupd Ebp Presentationapi-384226081No ratings yet
- Surgical InstrumentsDocument28 pagesSurgical InstrumentsNama Best100% (1)
- Voto Angela ResumeDocument1 pageVoto Angela Resumeapi-272451466No ratings yet
- ch116 Part2Document102 pagesch116 Part2p'eng matchima h.No ratings yet
- Perineal Care FinalDocument9 pagesPerineal Care Finalp4sion100% (2)
- Educational Module For Nursing Assistants in Long-Term Care Facilities: Urinary Tract Infections and Asymptomatic BacteriuriaDocument35 pagesEducational Module For Nursing Assistants in Long-Term Care Facilities: Urinary Tract Infections and Asymptomatic BacteriuriaPH Ph GnsoNo ratings yet
- Exam Key ms3Document33 pagesExam Key ms3joanneNo ratings yet
- Catheterization and EnemaDocument49 pagesCatheterization and EnemakhaimahalenylenNo ratings yet
TVP-2020-1112 Managing Feline Urethral Obstruction
TVP-2020-1112 Managing Feline Urethral Obstruction
Uploaded by
Lucas Dos Santos MacedoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
TVP-2020-1112 Managing Feline Urethral Obstruction
TVP-2020-1112 Managing Feline Urethral Obstruction
Uploaded by
Lucas Dos Santos MacedoCopyright:
Available Formats
MANAGEMENT STRATEGIES PEER REVIEWED
MASTERS OF DISGUISE
Diagnosis of feline urethral
obstruction is straightforward,
but the difficulty lies in
recognition of the problem at
home, as cats are masters of
hiding illness.
MANAGEMENT STRATEGIES
Managing Feline
Urethral Obstruction
Kelly St. Denis, MSc, DVM, DABVP (Feline Practice)
Charing Cross Cat Clinic, Brantford, Ont.
Feline urethral obstruction (UO) is a common an uncommon cause of FLUTD. Predisposing factors
presenting emergency in veterinary medicine. Prognosis for feline UO are listed in BOX 1.1,3
for survival with proper, timely treatment is 90% to
95%, and recurrence rates are estimated to be 15% to Cats are masters at hiding illness. As a result, the early
40%.1 UO is secondary to feline lower urinary tract signs of UO may go unnoticed and the problem may
disease (FLUTD), a clinical entity with a variety of not be recognized until hours or days after it begins.
etiologies. Feline idiopathic cystitis (FIC) accounts for Clinical signs of UO include periuria, pollakiuria,
53% of FLUTD cases, followed by urolithiasis (29%) stranguria, dysuria, and oliguria. Microscopic or
and urethral plugs (18%).2 Urethral plugs may consist macroscopic hematuria may be noted. As UO advances,
of crystals (e.g., magnesium phosphate, calcium clinical signs include vomiting, lethargy, and collapse.
oxalate), cellular matter, mucus/mucoid matter, or The hallmark clinical sign of UO is a painful, firm, full
other accumulations. Urinary tract infection (UTI) is to overdistended urinary bladder with little to no urine
passing from the urethra. Clinical parameters may
include normo- to hyperthermia and bradycardia or
tachycardia with or without arrhythmias.
BOX 1 Factors Predisposing to
Feline Urethral Obstruction
DIAGNOSTIC TESTING
Krishantha Madumal/shutterstock.com
SEX: Male or neutered male
Diagnostic testing in UO patients is critical to
AGE: 2 to 4 years
identifying complications. TABLE 1 lists diagnostic tests
BODY SIZE: Obesity, higher body condition
for UO patients in order of priority. Urgent tests
score
include blood gas and serum electrolyte measurements
BREED: Higher in non-pedigree cats; no
breed predisposition and electrocardiography (ECG). Results of these tests
LIFESTYLE: Indoor, multicat household
allow targeted stabilization of possible life-threatening
OTHER: Inter-cat issues; decreased water
metabolic and electrolyte disturbances. Radiographic
intake imaging to detect the presence of obstructing
urethroliths guides the approach to urinary catheter
placement and bladder decompression (FIGURE 1).
78 NOVEMBER/DECEMBER 2020 todaysveterinarypractice.com
PEER REVIEWED MANAGEMENT STRATEGIES
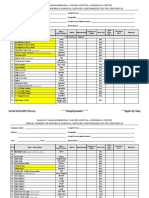
TABLE 1 Priority of Diagnostic Tests in Patients With Urinary Obstruction
PRIORITY TEST IDENTIFY AND TREAT
Blood gases
Urgent Metabolic acidosis (common in urinary obstruction patients)
Serum electrolytes Na+, Cl-, HCO -
Urgent Serum electrolytes K+, iCa++ Hyperkalemia, hypocalcemia
Urgent Electrocardiography Cardiac arrhythmias pertaining to electrolyte disturbances
Uroliths, obstructing urethroliths; nephroliths and ureteroliths may
High priority Radiography
also be seen
Blood urea nitrogen, creatinine,
Priority Acute kidney injury secondary to obstruction
symmetric dimethylarginine
Important Urinalysis ± urine culture Crystalluria, pyuria, bacteriuria
Important Complete blood count Anemia, leukocytosis, neutrophilia
Important Clinical chemistry Concurrent disease
Important Ultrasonography (if available) Urinary tract changes
Determining the renal status of the patient is a priority, immediate and ongoing priority. The PLATTER
as severe kidney injury may affect prognosis and client algorithm can guide the use of analgesic care (BOX 2).4
decisions. Other diagnostic tests provide valuable Validated pain scales such as the Glasgow Composite
information for ongoing patient care but are not Measure Pain Scale–Feline (aprvt.com) and the Feline
critical to early stabilization. Grimace Scale (felinegrimacescale.com) minimize
subjectivity and provide consistency in evaluation.
PATIENT STABILIZATION A multimodal approach to analgesia is essential, using
The approach to stabilization varies with each case. The analgesics from several drug classes. Analgesic options
establishment of a tailored list of priorities is essential, are presented in TABLE 2. Nonsteroidal anti-
with the goal being to achieve all in a timely fashion. inflammatory drugs (NSAIDs) should be used with
caution. Use in patients that are dehydrated, have
confirmed kidney disease, or have unknown kidney
Analgesia function should be avoided until the patient is
A necessity for UO patients, analgesia is often neglected rehydrated and/or resolution of azotemia is confirmed.
in the rush to treat the obstruction and related While NSAIDs may not show a direct benefit in
complications. Provision of analgesia should be an preventing recurrence of UO in FIC patients,5,6 they
BOX 2 PLATTER Algorithm for the
Continuum of Analgesia
PLan: Perform a patient-specific pain
assessment and formulate a treatment
plan.
Anticipate: While existing needs are
treated, identify future needs and
administer preventive analgesia.
TreaT: Provide appropriate treatment
commensurate with the type, severity,
and duration of expected or existing pain.
Evaluate: Evaluate the patient’s response
to analgesics using a validated pain
FIGURE 1. Radiographic imaging facilitates the scoring tool.
identification of obstructing urethroliths. A 12-year-old Return: As the patient’s needs change,
spayed, domestic longhaired cat presented with a history of formulate a new plan.
stranguria and dysuria that had progressed to oliguria. An
obstructing urethrolith can be seen (arrow).
todaysveterinarypractice.com NOVEMBER/DECEMBER 2020 79
MANAGEMENT STRATEGIES PEER REVIEWED
should be considered as a beneficial component of potassium, and, as most UO cats have metabolic
multimodal analgesia. acidosis, their alkalinizing effect can be beneficial in
restoring pH in the first 12 hours of fluid therapy.1,8,9
In contrast, 0.9% NaCl is acidifying and may
Fluid Therapy compromise attempts to restore acid-base balance.8
The goals of fluid therapy for UO patients include
support of intravascular volume, dilution of serum POD with urine production in excess of 2 mL/kg/h
potassium, and correction of metabolic derangements. occurs within 4 to 6 hours after relief of obstruction in
Patients presented with cardiovascular collapse should as many as 46% to 74% of patients.10,11 It is a result of
receive shock doses of crystalloid solutions (50 to the accumulation of osmotically active substances in
55 mL/kg IV)7 in bolus fractions to restore vascular the blood. Pressure necrosis, medullary washout, and
volume.1 The first bolus of 25% of the calculated shock antidiuretic hormone resistance may also contribute to
dose should be administered over 15 to 20 minutes, POD. Monitoring of fluid input/output and changes in
followed by reassessment of the patient’s perfusion body weight assists in early identification of POD.
parameters. Additional boluses of fluids can be Fluid therapy is tailored to ongoing fluid losses. Since
administered in 25% increments. If the patient is not POD can lead to kaliuresis, monitoring of serum
responding after 50% of the calculated shock dose has potassium is recommended, and potassium should be
been administered, colloids may be required.7 supplemented if required.
Once intravascular fluid volume is stabilized, fluid rates
should be based on replacement of interstitial Hyperkalemia Management
dehydration amounts plus maintenance fluid at 2 to 3 Hyperkalemia is a potentially life-threatening
mL/kg/h.1 Anecdotally, higher rates of 10 to 20 mL/kg complication of UO. It may be evident early in patient
may be chosen in an effort to “flush out” the urinary assessment, based on the presence of arrhythmias,
tract and reduce hyperkalemia and/or in anticipation of bradycardia, or tachycardia.
postobstructive diuresis (POD).8,9
ECG patterns alter with worsening hyperkalemia. With
Balanced electrolyte solutions such as lactated Ringer’s mild potassium elevations (5.5 to 6.5 mEq/L), classic
solution and Plasma-Lyte (Baxter, baxter.com) contain early changes include tall T waves with a prolonged
low levels of potassium (4 to 5 mEq/L) and are safe for QRS complex. Mild elevations in potassium usually
use in hyperkalemic UO patients.7,8 They do not resolve in response to dilutional fluid therapy (10 to
negatively affect the rate of normalization of serum 20 mL/kg/h).1
TABLE 2 Analgesic Drugs for Consideration in the Treatment and Management of
Pain Secondary to Urethral Obstruction
DRUG CLASS DOSE DISADVANTAGES AND SIDE EFFECTS
0.01–0.03 mg/kg transmucosal, IM,
Buprenorphine
Opioid IV q4–12h Dysphoria, unusual behaviors, mydriasis,
Buprenorphine, Partial µ agonist hyperthermia
80–120 µg/kg SC q72h
sustained release
Opioid K
Butorphanol agonist/µ 0.2–0.4 mg/kg IV, IM, SC q1–4h Limited analgesia
antagonist
Opioid
5–10 µg/kg IV, IM, SC q1–3h Respiratory depression, bradycardia, urinary
Fentanyl µ agonist/K
CRI 2–5 µg/kg/hr IV retention, hyperthermia
agonist
Gabapentin Calcium channel 5–15 mg/kg PO q12h
Transient ataxia, transient sedation
Pregabalin modulator 1–2 mg/kg PO q12h
0.1 mg/kg PO day 1, then Vomiting (rare)
Meloxicam
COX-2–selective 0.05 mg/kg q24h Limit use in patients with kidney disease,
NSAID 1 mg/kg PO q24h for a total of unknown kidney function, and/or
Robenacoxib dehydration
3 doses
CRI=constant-rate infusion
80 NOVEMBER/DECEMBER 2020 todaysveterinarypractice.com
PEER REVIEWED MANAGEMENT STRATEGIES
Moderate hyperkalemia of 6 to 8 mmol/L requires where decompressive cystocentesis was used, the risk of
immediate fluid therapy and treatment. Regular insulin bladder tear or rupture and/or clinically significant
administered at 0.1 to 0.25 IU/kg IV will drive an abdominal effusion was determined to be low.13,14
intracellular shift of potassium within 1 hour.12 To
reduce the risk of hypoglycemia, 10% to 20% dextrose Relief of the UO and placement of a urinary catheter
should be given as a bolus of 0.5 g/kg. Intravenous should not be attempted without heavy sedation or full
fluids can be supplemented with 1% to 2% dextrose to general anesthesia.1 Use of a coccygeal epidural can
maintain blood glucose levels.12 reduce sedative and anesthetic requirements and
improve comfort levels during the recovery phase.15
Serum potassium elevations in excess of 8 mmol/L are
severe and require additional treatment to protect
cardiac function. Calcium gluconate is administered Catheter Choice
slowly at 50 to 100 mg/kg IV, with continuous ECG Urinary catheters are available in a variety of materials,
monitoring. Calcium gluconate has a myocardial sizes, and configurations (TABLE 3). For initial
protective effect for 20 to 30 minutes.12 unblocking, more rigid catheters such as olive tip
catheters or polypropylene catheters are often selected,
although the rigidity of these catheters may increase the
Hypocalcemia Management risk of urethral trauma. As rigid catheters are not ideal
Hypocalcemia may occur as a complication of UO as indwelling catheters, placement of a second, softer
related to reduced renal clearance of phosphorus.12 catheter is necessary after unblocking, which increases
Decreases in ionized calcium to below 1.6 mEq/L can the risk of urethral trauma and irritation. Catheters
lead to impaired cardiac electrical and mechanical made of polytetrafluoroethylene and polyurethane are
function. Intravenous calcium gluconate may be more rigid at room temperatures and soften at body
indicated as described above. temperature. They are ideal for both unblocking and
placement as an indwelling catheter.
BLADDER DECOMPRESSION In cats with a UO, urinary catheter sizes should be no
AND RELIEF OF UO larger than 3.5 to 5 Fr. Smaller urethral catheters
Once the patient has been stabilized, bladder (3.5 Fr) may be associated with decreased risk of
decompression and relief of the urinary obstruction are recurrent obstruction 24 hours after catheter removal.16
necessary. Decompressive cystocentesis is a valid Indwelling urinary catheters are generally left in place
approach to relieve bladder pressure and associated pain for 1 to 3 days, although no conclusive data exist to
in the initial phases of treatment and has been evaluated specify duration.1 Factors to consider include patient
as a safe alternative treatment for UO when finances do stability, resolution of biochemical abnormalities,
not permit urinary catheterization.13 In cases of UO POD, and gross and microscopic character of urine.
TABLE 3 Urinary Catheter Selection for Relief of Urethral Obstruction
CATHETER PROS CONS
Stainless steel olive tip Most rigid, with variable-size olive-shaped tip Higher risk of urethral trauma
for relief of obstruction Not designed for indwelling use
Polypropylene Most rigid, relieves obstruction Higher risk of urethral trauma
(tomcat) Open-ended and side-hole options More reactive/irritating than polyvinyl
Not recommended for indwelling use
Polyvinyl Softer for indwelling Side holes not ideal for relief of
(red rubber) obstruction
Polytetrafluoroethylene Firmer at room temperature for unblocking, Higher cost
(“slippery Sam”) softens at body temperature for indwelling
Less reactive than polypropylene and polyvinyl
Polyurethane Firmer at room temperature for unblocking, Higher cost
(tomcat small urinary catheter) softens at body temperature for indwelling
Less reactive than polypropylene and polyvinyl
Product may include flushing stylet
todaysveterinarypractice.com NOVEMBER/DECEMBER 2020 81
MANAGEMENT STRATEGIES PEER REVIEWED
Collection System urethral smooth muscle relaxation, has a rapid onset of
A closed collection system facilitates monitoring of action, and is the antispasmodic of choice. Potential
catheter patency, measurement of urine output, and side effects include hypotension, lethargy, ptyalism,
early identification of POD. It may reduce urine soiling diarrhea, anorexia, and malodorous stool.19
and scalding. Anecdotally, clinicians may prefer open Phenoxybenzamine is a less effective alpha-1 adrenergic
systems based on concerns about the comfort level of antagonist sometimes used for UO. It requires up to a
the patient and obstruction of urine flow with a closed week to take effect.1 Acepromazine may be used to
system. Closed urinary catheter systems are reduce proximal urethral pressures, acting also as a
recommended as the standard of care.17 sedative; however, the risks of hypotension are
significantly higher than with prazosin or
phenoxybenzamine.
Complications
UTI is uncommon in UO patients.18 The use of an Given the limited effect of antispasmodics on the feline
indwelling urinary catheter presents a low risk for urethra, their need as a treatment for UO has been
acquired UTI.18 Empiric use of antibiotics is not called into question. Controlled studies have failed to
warranted at the time of presentation or during demonstrate a benefit of their use.1 Although a 2013
treatment.17 Urine culture after 24 hours of study failed to find a difference in the incidence of
catheterization or at the time of catheter removal has recurrent UO and severity of lower urinary tract signs
been recommended.1,18 However, in the absence of among cats receiving prazosin and those receiving
clinical signs associated with cystitis, the identification placebo,19 larger studies are still needed.
of pyuria in urine sediment or bacteriuria by urine
culture does not necessarily warrant treatment.17
Antianxiety Medications
Detrusor atony can occur as a result of bladder During the postobstruction recovery phase and
overstretch during a prolonged, untreated UO. Recovery following discharge, antianxiety medications may be
of normal detrusor function is promoted by keeping indicated. Patients diagnosed with FIC sometimes
the bladder small during the days after relief of the benefit from short- or long-term use of antianxiety
obstruction. Indwelling urinary catheters or manual medications such as alprazolam or amitriptyline. The
bladder expression may suffice. Parasympathomimetic use of these medications should not replace appropriate
drugs such as bethanechol increase smooth muscle dietary and/or environmental modifications.
contractility and may further support detrusor recovery.12
Side effects of bethanechol include vomiting and
diarrhea; this drug should not be used in patients with Nutritional Therapy
active UO or high risk of recurrent UO. Urinary prescription diets play a role in the
management of UO secondary to urolithiasis. Some of
these diets promote elimination of crystalluria,
POSTOBSTRUCTION dissolution of struvite uroliths, and/or the prevention
SUPPORTIVE CARE of subsequent urolith formation. At least one of these
diets has also been shown to reduce recurrence of
Analgesia several clinical signs associated with FIC.20
Multimodal analgesia (TABLE 2) should be continued
based on patient reassessment (BOX 2) in the clinic and
after discharge of the patient from the hospital. Surgical Intervention
In the case of life-threatening urolith UO, surgical
removal of the uroliths may be indicated. However, if
Muscle Relaxant/ patients can be safely unobstructed and stabilized,
Antispasmodic Medications dietary dissolution of existing sterile struvite stones is a
The feline urethra is composed of smooth muscle along less invasive and less costly treatment option.21,22
the proximal quarter to third of its length and skeletal Urolith size should be reassessed 2 weeks after diet
muscle distally. Only proximal portions of the feline initiation to determine if dietary dissolution is possible.
urethra are responsive to smooth muscle relaxants. A 50% or greater reduction in the stone size indicates
Prazosin (alpha-1 adrenergic antagonist) can cause likely success for dietary dissolution.22
82 NOVEMBER/DECEMBER 2020 todaysveterinarypractice.com
PEER REVIEWED MANAGEMENT STRATEGIES
11. Fröhlich L, Hartmann K, Sautter-Louis C, Dorsch R. Postobstructive
Environmental Management diuresis in cats with naturally occurring lower urinary tract obstruction:
incidence, severity and association with laboratory parameters on
Meeting the environmental needs of cats and providing admission. J Feline Med Surg 2016;18(1):809-817.
the appropriate number and distribution of resources is 12. Little S. The Cat: Clinical Medicine and Management. St. Louis, MO:
key to reducing anxiety and often appropriate in the Elsevier Saunders; 2011.
13. Cooper ES, Owens TJ, Chew DJ, Buffington CAT. A protocol for
treatment of FLUTD.23,24 The American Association of managing urethral obstruction in male cats without urethral
Feline Practitioners/International Society of Feline catheterization. JAVMA 2010;237(11):1261-1266.
Medicine guidelines on environmental needs in cats23 14. Gerken KK, Cooper ES, Butler AL, Chew DJ. Association of abdominal
effusion with a single decompressive cystocentesis prior to
and guidelines to diagnosing and resolving house- catheterization in male cats with urethral obstruction. J Vet Emerg Crit
soiling behavior in cats24 are excellent resources for Care 2020;30(1):11-17.
15. O’Hearn AK, Wright BD. Coccygeal epidural with local anesthetic
advising clients. In cases of FIC, multimodal for catheterization and pain management in the treatment of feline
environmental modification has been demonstrated to urethral obstruction. J Vet Emerg Crit Care 2011;21(1):50-52.
reduce lower urinary tract signs and signs of anxiety in 16. Hetrick PF, Davidow EB. Initial treatment factors associated with feline
urethral obstruction recurrence rate: 192 cases (2004-2010). JAVMA
potentially reducing the risk of FIC-related UO.25 2013;243(4):512-519.
17. Weese JS, Blondeau J, Boothe D, et al. International Society for
Companion Animal Infectious Diseases (ISCAID) guidelines for the
diagnosis and management of bacterial urinary tract infections in dogs
CONCLUSION and cats. Vet J 2019;247:8-25.
Feline UO is a common emergency. Diagnosis of UO 18. Cooper ES, Lasley E, Daniels JB, Chew DJ. Incidence of bacteriuria
at presentation and resulting from urinary catheterization in feline
in cats is straightforward, but the difficulty lies in urethral obstruction. J Vet Emerg Crit Care 2019;29(5):472-477.
recognition of the problem at home. Client education 19. Reineke EL, Thomas EK, Syring RS, et al. The effect of prazosin
on outcome in feline urethral obstruction. J Vet Emerg Crit Care
is key to prevention as well as prompt treatment. 2017;27(4):387-396.
Diagnostic testing facilitates identification of 20. Kruger JM, Lulich JP, MacLeay J. Comparison of foods with differing
nutritional profiles for long-term management of acute nonobstructive
complicating metabolic and electrolyte disturbances, idiopathic cystitis in cats. JAVMA 2015;247(5):508-517.
and treatment is aimed at providing analgesia and 21. Lulich JP, Kruger JM, Macleay JM, et al. Efficacy of two commercially
stabilization of the patient prior to attempts at UO available, low-magnesium, urine-acidifying dry foods for the
dissolution of struvite uroliths in cats. JAVMA 2013;243(8):1147-1153.
relief. Lifelong care in the form of diet and
22. Lulich JP, Berent AC, Adams LG, et al. ACVIM small animal consensus
environmental modification is likely necessary. recommendations on the treatment and prevention of uroliths in dogs
and cats. J Vet Intern Med 2016;30(5):1564-1574.
23. Ellis SLH, Rodan I, Carney HC, et al. AAFP and ISFM feline
environmental needs guidelines. J Feline Med Surg 2013;15(3):219-230.
References 24. Carney HC, Sadek TP, Curtis TM, et al. AAFP and ISFM guidelines for
diagnosing and solving house-soiling behavior in cats. J Feline Med
1. Cooper ES. Controversies in the management of feline urethral
Surg 2014;16(7):579-598.
obstruction. J Vet Emerg Crit Care 2015;25(1):130-137.
25. Buffington CAT, Westropp JL, Chew DJ, Bolus RR. Clinical evaluation
2. Gerber B, Eichenberger S, Reusch CE. Guarded long-term prognosis in
of multimodal environmental modification (MEMO) in the management
male cats with urethral obstruction. J Feline Med Surg
of cats with idiopathic cystitis. J Feline Med Surg 2006;8(4):261-268.
2008;10(1):16-23.
3. Jukes A, Lui M, Morton JM, et al. Associations between increased body
condition score, bodyweight, age and breed with urethral obstruction
in male castrated cats. Vet J 2019;244:7-12.
4. Epstein ME, Rodan I, Griffenhagen G, et al. 2015 AAHA/AAFP pain
management guidelines for dogs and cats. J Feline Med Surg
2015;17(3):251-272.
Kelly St. Denis
5. Dorsch R, Zellner F, Schulz B, et al. Evaluation of meloxicam for the
treatment of obstructive feline idiopathic cystitis. J Feline Med Surg Dr. St. Denis is a practicing feline medicine specialist,
2016;18(11):925-933. board certified with the American Board of Veterinary
6. Nivy R, Segev G, Rimer D, et al. A prospective randomized study of Practitioners in the specialty of feline practice. In her
efficacy of 2 treatment protocols in preventing recurrence of clinical early career she trained in molecular biology and
signs in 51 male cats with obstructive idiopathic cystitis. J Vet Intern immunology, working in the field of cancer research. In
Med 2019;33(5):2117-2123.
1999 she graduated from the Ontario Veterinary College,
7. Davis H, Jensen T, Johnson A, et al. 2013 AAHA/AAFP fluid therapy going on to own and operate the Charing Cross Cat
guidelines for dogs and cats. JAAHA 2013;49(3):149-159.
Clinic from 2007 to 2020. Dr. St. Denis is the 2020-
8. Drobatz KJ, Cole SG. The influence of crystalloid type on acid–base
2021 president for the American Association of Feline
and electrolyte status of cats with urethral obstruction. J Vet Emerg
Crit Care 2008;18(4):355-361. Practitioners and an active volunteer in the organization,
9. Cunha MG, Freitas GC, Carregaro AB, et al. Renal and cardiorespiratory
participating in many committees and task forces. Dr.
effects of treatment with lactated Ringer’s solution or physiologic St. Denis is a consultant on the Veterinary Information
saline (0.9% NaCl) solution in cats with experimentally induced Network in feline internal medicine.
urethral obstruction. Am J Vet Res 2010;71(7):840-846.
10. Francis BJ, Wells RJ, Rao S, Hackett TB. Retrospective study to
characterize post-obstructive diuresis in cats with urethral obstruction.
J Feline Med Surg 2010;12(8):606-608.
todaysveterinarypractice.com NOVEMBER/DECEMBER 2020 83
You might also like
- Ehrlichiosisand Anaplasmosis:: An UpdateDocument42 pagesEhrlichiosisand Anaplasmosis:: An UpdateMargarita CCNo ratings yet
- Canine Aural HematomaDocument6 pagesCanine Aural Hematomakenikenranisa100% (1)
- Fim Item ScoringDocument10 pagesFim Item Scoringhaythamalshikh0120% (1)
- Paraphimosis in The DogDocument4 pagesParaphimosis in The DogErick GarciaNo ratings yet
- Lymphoid Leukemia in DogsDocument15 pagesLymphoid Leukemia in Dogstaner_soysurenNo ratings yet
- How To Anaesthetize A GiraffeDocument4 pagesHow To Anaesthetize A Giraffeltrathie3087100% (2)
- Canine InsulinomaDocument5 pagesCanine Insulinomasoff4ikaNo ratings yet
- Mucocele 2Document13 pagesMucocele 2FEY YENG SOFIA FUNG GUADALUPENo ratings yet
- AHS Canine Guidelines 11 13 20Document37 pagesAHS Canine Guidelines 11 13 20Ana Clara Pessôa100% (1)
- FELINE-Clinical Forms of Acquired Myasthenia Gravis in CatsDocument7 pagesFELINE-Clinical Forms of Acquired Myasthenia Gravis in Catstaner_soysurenNo ratings yet
- Materia Medica PuraDocument224 pagesMateria Medica PuraMorgan CabreraNo ratings yet
- Enf Discal Intervertebral (II)Document16 pagesEnf Discal Intervertebral (II)pedro jaraNo ratings yet
- CANINE-Pathophysiology of Organ Failure in Severe Acute Pancreatitis in DogsDocument10 pagesCANINE-Pathophysiology of Organ Failure in Severe Acute Pancreatitis in Dogstaner_soysurenNo ratings yet
- Diagnosis of Pancreatitis in Dogs and Cats: ReviewDocument14 pagesDiagnosis of Pancreatitis in Dogs and Cats: ReviewMiruna ChiriacNo ratings yet
- general systemic states د.عزيزةDocument75 pagesgeneral systemic states د.عزيزةAhmed Hamdy NaDa100% (2)
- Fever of Unknown OriginDocument4 pagesFever of Unknown OriginPatricia PopNo ratings yet
- Immunotherapy With Banerji ProtocolDocument43 pagesImmunotherapy With Banerji ProtocolSur E JahanNo ratings yet
- Feline Vocalization - Excessive: Why Is My Cat Persistently Crying?Document4 pagesFeline Vocalization - Excessive: Why Is My Cat Persistently Crying?Brook Farm Veterinary CenterNo ratings yet
- Veterinary Focus 27.1Document52 pagesVeterinary Focus 27.1Νίκος ΚριτσοταλάκηςNo ratings yet
- Monografi AtropinDocument48 pagesMonografi AtropinWahyu AgustinaNo ratings yet
- Siamese CatDocument5 pagesSiamese CatDummy1 AccountNo ratings yet
- TX TableDocument1 pageTX TableLaureece Salm ApduhanNo ratings yet
- Top 5 Leukogram PatternsDocument3 pagesTop 5 Leukogram PatternsSandraHermosilloNo ratings yet
- Atlas of Gastrointestinal Endoscopy in Dogs and CatsDocument8 pagesAtlas of Gastrointestinal Endoscopy in Dogs and CatsDama Ayu RaniNo ratings yet
- L19 - Pelvic Pain & EndometriosisDocument8 pagesL19 - Pelvic Pain & EndometriosisBrandonRyanF.MosidinNo ratings yet
- Howto Companion April2008Document3 pagesHowto Companion April2008lybrakissNo ratings yet
- Acute Pain in CatsDocument10 pagesAcute Pain in CatsLINDA BELMONTNo ratings yet
- FELINE-Peritoneopericardial Diaphramatic Hernia in CatsDocument13 pagesFELINE-Peritoneopericardial Diaphramatic Hernia in Catstaner_soysuren100% (1)
- FelineCalicivirus FactSheet PDFDocument5 pagesFelineCalicivirus FactSheet PDFJuniClaudia13No ratings yet
- Brown C (2013) Patient Care Report For Feline Patient With Urethral ObstructionDocument5 pagesBrown C (2013) Patient Care Report For Feline Patient With Urethral ObstructionRob PNo ratings yet
- Anestesia EquinosDocument26 pagesAnestesia EquinosKiimBerly RcNo ratings yet
- Suspensory Ligament Rupture Tech During Small Animal OH PDFDocument8 pagesSuspensory Ligament Rupture Tech During Small Animal OH PDFRiesky NudialestariNo ratings yet
- AnaplasmosisDocument1 pageAnaplasmosisDumapis RichardNo ratings yet
- PDF Small Animal Medical Differential Diagnosis A Book of Lists Mark S Thompson Ebook Full ChapterDocument53 pagesPDF Small Animal Medical Differential Diagnosis A Book of Lists Mark S Thompson Ebook Full Chapterelaine.dawson903100% (1)
- In Practice Blood Transfusion in Dogs and Cats1Document7 pagesIn Practice Blood Transfusion in Dogs and Cats1何元No ratings yet
- Therapeutic Diet What We Need To ConsiderDocument4 pagesTherapeutic Diet What We Need To Consideranarosli251No ratings yet
- Sni 3950-2014Document88 pagesSni 3950-2014Dya Yda'sNo ratings yet
- 4 Diabetes MellitusDocument26 pages4 Diabetes MellitusnomiskemalNo ratings yet
- ABC of Emergency Vet Triage 1691081646Document15 pagesABC of Emergency Vet Triage 1691081646Alina TeodorescuNo ratings yet
- CANINE-PAthogenesis of Acute Canine Gastric Dilatation-Volvulus SyndromDocument7 pagesCANINE-PAthogenesis of Acute Canine Gastric Dilatation-Volvulus Syndromtaner_soysurenNo ratings yet
- Biomedical Therapy: Journal ofDocument16 pagesBiomedical Therapy: Journal ofantoniojgteixeira100% (1)
- Medicine and SurgeryDocument26 pagesMedicine and SurgerySophia Mitz Aya-ayNo ratings yet
- Veterinary Hospital AbstractDocument1 pageVeterinary Hospital AbstractMichelleNo ratings yet
- A Aha Diabetes GuidelinesDocument10 pagesA Aha Diabetes GuidelinesOvidiu PinteaNo ratings yet
- 01 Redalyc Martinez RizoDocument14 pages01 Redalyc Martinez RizoStefanie Valeria Espinoza TorrakaNo ratings yet
- Wound Care Management For The Equine PractitionerDocument212 pagesWound Care Management For The Equine PractitionerLucia ZamoloNo ratings yet
- Canine Atopic DermatitisDocument16 pagesCanine Atopic Dermatitisserbanbogdans536667% (3)
- Canine Mast Cell TumorsDocument5 pagesCanine Mast Cell TumorsCarol LeslieNo ratings yet
- Colic in HorsesDocument2 pagesColic in HorsesRamos SHNo ratings yet
- Rumen MotilityDocument32 pagesRumen MotilityAbhay Singh100% (1)
- Urinary Catheter Placement For Feline ObstructionDocument6 pagesUrinary Catheter Placement For Feline ObstructionWilliam ChandlerNo ratings yet
- FELINE - Chronic Bacterial Skin Infections in CatsDocument9 pagesFELINE - Chronic Bacterial Skin Infections in Catstaner_soysurenNo ratings yet
- Clinical Canine and Feline Reproduction: Evidence-Based AnswersFrom EverandClinical Canine and Feline Reproduction: Evidence-Based AnswersNo ratings yet
- Cephalosporins in Veterinary MedicineDocument23 pagesCephalosporins in Veterinary MedicineSunil100% (3)
- CANINE-Mechanism of Thrombocytopenia in Dogs With CancerDocument11 pagesCANINE-Mechanism of Thrombocytopenia in Dogs With Cancertaner_soysuren100% (1)
- Feline Acute Kidney Injury. 2. Approach To Diagnosis, Treatment and PrognosisDocument9 pagesFeline Acute Kidney Injury. 2. Approach To Diagnosis, Treatment and PrognosisMartín QuirogaNo ratings yet
- Review and Update of Benign PRDocument6 pagesReview and Update of Benign PRAgung KaryawinaraNo ratings yet
- The Laboratory Diagnosis of Feline Kidney DiseaseDocument7 pagesThe Laboratory Diagnosis of Feline Kidney DiseaseCabinet VeterinarNo ratings yet
- Diagnosis and Management of Acute Pancreatitis andDocument11 pagesDiagnosis and Management of Acute Pancreatitis andMarcelitaTaliaDuwiriNo ratings yet
- 2011 - AASLD - Management of Acute Liver FailureDocument22 pages2011 - AASLD - Management of Acute Liver FailuremohamedelsayedelmenyawyNo ratings yet
- Piis0085253815527324 PDFDocument5 pagesPiis0085253815527324 PDFdodong skyroseNo ratings yet
- CATHETERIZATIONDocument3 pagesCATHETERIZATIONrnrmmanphdNo ratings yet
- Bladder Irrigation Toolkit PDFDocument9 pagesBladder Irrigation Toolkit PDFJanuardi IndraNo ratings yet
- Implementing An Evidence-Based Practice Protocol For Prevention of Catheterized Associated Urinary Tract Infections in A Progressive Care UnitDocument9 pagesImplementing An Evidence-Based Practice Protocol For Prevention of Catheterized Associated Urinary Tract Infections in A Progressive Care UnitLina Mahayaty SembiringNo ratings yet
- Surgical Instrumentation: Iii. Grasping and HoldingDocument37 pagesSurgical Instrumentation: Iii. Grasping and Holdingkaren carpioNo ratings yet
- Abdellah's TheoryDocument6 pagesAbdellah's TheoryBaldeep GrewalNo ratings yet
- Clinical Guidelines (Nursing) - Indwelling Urinary Catheter - Insertion and Ongoing CareDocument8 pagesClinical Guidelines (Nursing) - Indwelling Urinary Catheter - Insertion and Ongoing CareLeeNo ratings yet
- Fundamentals Mt2 NovDocument16 pagesFundamentals Mt2 NovRika MaeNo ratings yet
- Urinary Incontinence ModuleDocument103 pagesUrinary Incontinence Modulesny007No ratings yet
- Infection Control Assessment ToolDocument30 pagesInfection Control Assessment ToolPMNo ratings yet
- DME Fee Schedule WCB PDFDocument34 pagesDME Fee Schedule WCB PDFMarina BroniNo ratings yet
- Urinary Catheter in A HorseDocument6 pagesUrinary Catheter in A Horsemouxritsa_83No ratings yet
- Nursing and Surgical Tender Items List 2021-22Document20 pagesNursing and Surgical Tender Items List 2021-22Muhammad Aqeel IrshadNo ratings yet
- Urine Incontinence Care: Urine Catheters Urine Bags AccessoriesDocument24 pagesUrine Incontinence Care: Urine Catheters Urine Bags AccessoriesMerveNo ratings yet
- Urinary Catheterization For PediatricsDocument6 pagesUrinary Catheterization For PediatricsMichael Montinola100% (1)
- PrelimDocument6 pagesPrelimCutypieCyrlah BarrientosNo ratings yet
- Previous Board Exam Questions No RatioDocument56 pagesPrevious Board Exam Questions No RatioNovemia Rose TisonNo ratings yet
- Article Bladder RetrainingDocument9 pagesArticle Bladder RetrainingRaenette DavidNo ratings yet
- Diagnostic Imaging of Lower Urinary Tract DiseaseDocument25 pagesDiagnostic Imaging of Lower Urinary Tract DiseaseSoyKlicheRodriguezNo ratings yet
- Urethral Trauma - Injuries Poisoning - MSD Manual Professional EditionDocument2 pagesUrethral Trauma - Injuries Poisoning - MSD Manual Professional EditionNaufal NaswanNo ratings yet
- Model Answer of Formative Written OSCADocument6 pagesModel Answer of Formative Written OSCAAhmed SamahaNo ratings yet
- Thomas M Hooton, MD Kalpana Gupta, MD, MPH Stephen B Calderwood, MD Allyson Bloom, MDDocument14 pagesThomas M Hooton, MD Kalpana Gupta, MD, MPH Stephen B Calderwood, MD Allyson Bloom, MDMusicBestLiveNo ratings yet
- Groupd Ebp PresentationDocument38 pagesGroupd Ebp Presentationapi-384226081No ratings yet
- Surgical InstrumentsDocument28 pagesSurgical InstrumentsNama Best100% (1)
- Voto Angela ResumeDocument1 pageVoto Angela Resumeapi-272451466No ratings yet
- ch116 Part2Document102 pagesch116 Part2p'eng matchima h.No ratings yet
- Perineal Care FinalDocument9 pagesPerineal Care Finalp4sion100% (2)
- Educational Module For Nursing Assistants in Long-Term Care Facilities: Urinary Tract Infections and Asymptomatic BacteriuriaDocument35 pagesEducational Module For Nursing Assistants in Long-Term Care Facilities: Urinary Tract Infections and Asymptomatic BacteriuriaPH Ph GnsoNo ratings yet
- Exam Key ms3Document33 pagesExam Key ms3joanneNo ratings yet
- Catheterization and EnemaDocument49 pagesCatheterization and EnemakhaimahalenylenNo ratings yet