Professional Documents
Culture Documents
Renal Function
Renal Function
Uploaded by
Janely EstreraCopyright:
Available Formats
You might also like
- Urinary System Lecture NotesDocument8 pagesUrinary System Lecture NotesBettina ColobongNo ratings yet
- Urinary Renal SystemDocument24 pagesUrinary Renal Systemremotigue.brettelNo ratings yet
- Renal DisordersDocument14 pagesRenal DisordersPrince Rener Velasco Pera100% (1)
- Unit - Ii Human Anatomy and PhysiologyDocument15 pagesUnit - Ii Human Anatomy and PhysiologyRK YeleswarapuNo ratings yet
- Final Exam Review - Bio 172Document21 pagesFinal Exam Review - Bio 172Erin McElhaney QuirkNo ratings yet
- Anph111 Reviewer (Urinary & Endocrine)Document7 pagesAnph111 Reviewer (Urinary & Endocrine)Maria Clarisse ReyesNo ratings yet
- Chapter 18 Anaphy TransesDocument5 pagesChapter 18 Anaphy TransesHoly HaeinNo ratings yet
- PP24 Functioning of The KidneyDocument79 pagesPP24 Functioning of The Kidneyangie432meNo ratings yet
- الجهاز البولىDocument6 pagesالجهاز البولىNajwa AbdualgaderNo ratings yet
- Selected Lecture Notes Chapter 25: The Urinary System: I. Kidney Functions and AnatomyDocument12 pagesSelected Lecture Notes Chapter 25: The Urinary System: I. Kidney Functions and AnatomyMarilia BonorinoNo ratings yet
- Activity 4 Human Body CareDocument9 pagesActivity 4 Human Body CareAzael GómezNo ratings yet
- The Urinary SystemDocument18 pagesThe Urinary Systemabdulrehmanfaisal54No ratings yet
- The Urinary and Reproductive System (J.R) - Policarpio MAT Gen. Sci.Document60 pagesThe Urinary and Reproductive System (J.R) - Policarpio MAT Gen. Sci.john ronald PolicarpioNo ratings yet
- Anatomy and Physiology of The KidneysDocument21 pagesAnatomy and Physiology of The Kidneysccbrown750% (2)
- Kidney Function - ExcretionDocument15 pagesKidney Function - Excretionznayune82No ratings yet
- Renal SystemDocument29 pagesRenal Systemjsreyes.402No ratings yet
- Urinary System 1. List The Functions of The KidneysDocument6 pagesUrinary System 1. List The Functions of The KidneysheerNo ratings yet
- Ch20 Answer Key 12edition CorrectedDocument11 pagesCh20 Answer Key 12edition CorrectedTeuku Muhammad LizarNo ratings yet
- Urinary Tract ReciewDocument5 pagesUrinary Tract ReciewRobert LotzerNo ratings yet
- Medsurg LeDocument179 pagesMedsurg Leremotigue.brettelNo ratings yet
- MIRADOR, Kiana AnaphyAct16Document4 pagesMIRADOR, Kiana AnaphyAct16Kiana MiradorNo ratings yet
- Urinary Elimination: (Midterm)Document14 pagesUrinary Elimination: (Midterm)Mina RacadioNo ratings yet
- Excretory SystemDocument2 pagesExcretory SystemDearly Niña OsinsaoNo ratings yet
- CHAPTER 18 ANAPHY TransesDocument5 pagesCHAPTER 18 ANAPHY TransesHoly HaeinNo ratings yet
- The Kidney Excretion and OsmoregulationDocument12 pagesThe Kidney Excretion and OsmoregulationLashaunte Hodge HobsonNo ratings yet
- PDF Document 2Document14 pagesPDF Document 2Vari MafiaNo ratings yet
- Lec 18Document4 pagesLec 18Lyanna Louise SantosNo ratings yet
- Life Processes - Excretion - Humans & Plants - OriginalDocument36 pagesLife Processes - Excretion - Humans & Plants - Originalnouraft.07No ratings yet
- Renal SystemDocument17 pagesRenal SystemLess CastilloNo ratings yet
- 5 19 Excretory System PDFDocument12 pages5 19 Excretory System PDFHNo ratings yet
- Chapter 6Document3 pagesChapter 6John ErickNo ratings yet
- Excretory Products and Their EliminationDocument9 pagesExcretory Products and Their EliminationBiju MylachalNo ratings yet
- Chapter 9 Excretory System PDFDocument17 pagesChapter 9 Excretory System PDFErica Ann Ical100% (1)
- Assessment of Patients With Renal Disorders Management of Urinary Tract DisordersDocument16 pagesAssessment of Patients With Renal Disorders Management of Urinary Tract DisordersJhosita Flora LarocoNo ratings yet
- Human Physiology Ii: School of BiochemistryDocument15 pagesHuman Physiology Ii: School of Biochemistrykeerthana t reddyNo ratings yet
- Excretion in Humans VIII NOTESDocument6 pagesExcretion in Humans VIII NOTESfulhambrighton0No ratings yet
- Urinary SystemDocument77 pagesUrinary SystemJushelle Anne Tigoy PilareNo ratings yet
- Excretory Products and Their EliminationDocument13 pagesExcretory Products and Their Eliminationaravind kishanNo ratings yet
- 3 - Excretion NotesDocument33 pages3 - Excretion NotesJenny YoonNo ratings yet
- QuestionsDocument4 pagesQuestionsA GoswamiNo ratings yet
- Wella S, VIRINA Bsn-I: Review Question Urinary SystemDocument4 pagesWella S, VIRINA Bsn-I: Review Question Urinary SystemEllee HadesNo ratings yet
- Urinary SystemDocument28 pagesUrinary Systemgabanule brandonNo ratings yet
- Understanding Medical Surgical Nursing - 0849-0849Document1 pageUnderstanding Medical Surgical Nursing - 0849-0849Anas TasyaNo ratings yet
- Hafeezullah: Subject:Anatomy Topic: Anatomy of Excretory System Roll No: 15 Semester: 1 RepeaterDocument10 pagesHafeezullah: Subject:Anatomy Topic: Anatomy of Excretory System Roll No: 15 Semester: 1 RepeaterMuhammad ShahzaibNo ratings yet
- XQ WFHKLJW WWHAfu 0 DGWFDocument10 pagesXQ WFHKLJW WWHAfu 0 DGWFGiridharan & Balaji RNNo ratings yet
- KidneyDocument8 pagesKidneyRaj JadhavNo ratings yet
- Urinary SystemDocument9 pagesUrinary SystemMa Ellen LumauagNo ratings yet
- Introduction and Assessment of The Renal - Urological SystemDocument182 pagesIntroduction and Assessment of The Renal - Urological SystemValerie Suge-Michieka100% (1)
- Lecture Slides - Urinary SystemDocument41 pagesLecture Slides - Urinary SystemReneilwe MoshidiNo ratings yet
- Excretion: Excretory Organ Excretory ProductDocument3 pagesExcretion: Excretory Organ Excretory ProductKekeletsoNo ratings yet
- Chapter 19 Points To RememberDocument5 pagesChapter 19 Points To RememberSaksham YadavNo ratings yet
- Important Points of Excretory SystemDocument3 pagesImportant Points of Excretory SystemDhruv Nair IX ANo ratings yet
- Chapter 25 - Urinary System - Class OutlineDocument22 pagesChapter 25 - Urinary System - Class Outlinestupidisg00gleofcourseNo ratings yet
- Urinary RenalDocument44 pagesUrinary RenalgorekaNo ratings yet
- B2U3 Excretorysystem Notes 06Document5 pagesB2U3 Excretorysystem Notes 06Kudakwashe ChikazheNo ratings yet
- Genitourinary SystemDocument30 pagesGenitourinary SystemKarenNo ratings yet
- (BIO) Chapter 9 - Excretion in HumansDocument14 pages(BIO) Chapter 9 - Excretion in Humansanya desilvaNo ratings yet
- 11 Biology Chapter 20.Document4 pages11 Biology Chapter 20.jackieaj093No ratings yet
- Kidney Diseases, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandKidney Diseases, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- What Are The Advantages and Disadvantages of A Water Level ContrDocument8 pagesWhat Are The Advantages and Disadvantages of A Water Level ContrGod's willNo ratings yet
- Medical Terminolgy Trans 1 115 SlidesDocument14 pagesMedical Terminolgy Trans 1 115 SlidesSophia Nicole LibaoNo ratings yet
- Valves Quality Control PlanDocument1 pageValves Quality Control Planjok1974No ratings yet
- Narasimham Committee: By: Pranav Dagar 2019PBA9202 MBAC401Document12 pagesNarasimham Committee: By: Pranav Dagar 2019PBA9202 MBAC401Diksha VashishthNo ratings yet
- Massage Therapy PDFDocument1 pageMassage Therapy PDFVirgilio BernardinoNo ratings yet
- Taenia SagitaDocument3 pagesTaenia SagitaNur LiyanaNo ratings yet
- CHRA 1st Reprint 2018 PDFDocument149 pagesCHRA 1st Reprint 2018 PDFMohd Jamalil Azam MustafaNo ratings yet
- Full Download Ebook Ebook PDF Nutrition Science and Applications 4th Edition by Lori A Smolin PDFDocument42 pagesFull Download Ebook Ebook PDF Nutrition Science and Applications 4th Edition by Lori A Smolin PDFbessie.skubis114100% (42)
- Bhopal Gas Tragedy Causes, Effects and Aftermath - GeeksforGeeksDocument1 pageBhopal Gas Tragedy Causes, Effects and Aftermath - GeeksforGeeksmxdczc5yxzNo ratings yet
- Ilovepdf Merged PDFDocument8 pagesIlovepdf Merged PDFHeta PanchalNo ratings yet
- Report Beauty and Wellness Market in IndiaDocument35 pagesReport Beauty and Wellness Market in IndiaRenu R NairNo ratings yet
- NC State PDFDocument27 pagesNC State PDFquantum16No ratings yet
- Australian/New Zealand StandardDocument9 pagesAustralian/New Zealand StandardhanryNo ratings yet
- Dintzis ExerciseDocument5 pagesDintzis ExerciserichschurNo ratings yet
- The Inconvenient Truth About Cancer and Mobile PhonesDocument2 pagesThe Inconvenient Truth About Cancer and Mobile PhonesVictoria caroline Mendes de jesusNo ratings yet
- 046: Unsafe Acts vs. Unsafe Conditions: Background Discussion Leader Duties For This SessionDocument2 pages046: Unsafe Acts vs. Unsafe Conditions: Background Discussion Leader Duties For This SessionVarahi VigneshNo ratings yet
- Dcode EFC-Healthcare Snapshot (February 2021) - 1Document7 pagesDcode EFC-Healthcare Snapshot (February 2021) - 1hussienNo ratings yet
- WWW - Irctc.co - in Eticketing Printticket - JSF PNR 41298787 PDFDocument1 pageWWW - Irctc.co - in Eticketing Printticket - JSF PNR 41298787 PDFManav GaneshNo ratings yet
- Acid Value and Amine Value of Fatty Quaternary Ammonium ChloridesDocument3 pagesAcid Value and Amine Value of Fatty Quaternary Ammonium ChloridesShaker Qaidi100% (1)
- Serie-6-Ttv Brochure enDocument16 pagesSerie-6-Ttv Brochure envaneaNo ratings yet
- Present Tense Exercise 18Document1 pagePresent Tense Exercise 18Adrijan AlispahićNo ratings yet
- NEK606 JScableDocument40 pagesNEK606 JScablenc_eanNo ratings yet
- Drug and Alcohol Testing in The WorkplaceDocument16 pagesDrug and Alcohol Testing in The WorkplaceYasmin KayeNo ratings yet
- Saudi Arabian Standard SASO IEC 60601-2-57/2012Document35 pagesSaudi Arabian Standard SASO IEC 60601-2-57/2012Gigi EssegiNo ratings yet
- WOC HepatitisDocument1 pageWOC Hepatitisdestri wulandariNo ratings yet
- RTN 320 V100 Quick Installation Guide 02Document37 pagesRTN 320 V100 Quick Installation Guide 02Juan Pablo CharrisNo ratings yet
- Baylon RatioDocument4 pagesBaylon RatioJaessa Feliciano100% (1)
- Plasterers Stilts Fact Sheet 3955 PDFDocument4 pagesPlasterers Stilts Fact Sheet 3955 PDFneyemhey2348513No ratings yet
- LEBV4830 04 MartinDocument380 pagesLEBV4830 04 MartinjibvNo ratings yet
- Geothermal Energy: The Power of Heat Right Under Your FeetDocument70 pagesGeothermal Energy: The Power of Heat Right Under Your FeetSarthak DixitNo ratings yet
Renal Function
Renal Function
Uploaded by
Janely EstreraOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Renal Function
Renal Function
Uploaded by
Janely EstreraCopyright:
Available Formats
GENITO-URINARY SYSTEM and then enter the proximal convoluted
tubule (PCT).
ANATOMY AND PHYSIOLOGY E. TUBULES
A. KIDNEY ANATOMY a. The tubules include the PCT, the loop of
1. Each person has two kidneys, which are Henle, and the distal convoluted tubule
located behind the peritoneum; they are (DCT).
attached at the level of the last thoracic b. The PCT receives filtrate from the
and first three lumbar vertebrae, on the glomerular capsule and reabsorbs water
right and left sides. and electrolytes through active and
2. The kidneys are enclosed in the renal passive transport.
capsule. c. The descending loop of Henle passively
3. The renal cortex is the outer layer of the reabsorbs water from the filtrate.
renal capsule, which contains blood- d. The ascending loop of Henle passively
filtering mechanisms (glomeruli). reabsorbs sodium and chloride from the
4. The renal medulla is the inner region, filtrate and helps maintain osmolality.
which contains the renal pyramids and e. The DCT actively and passively
renal tubules. removes sodium and water.
5. Together, the renal cortex, pyramids, f. The filtered fluid is converted to urine in
and medulla constitute the the tubules; then the urine moves to the
parenchyma. pelvis of the kidney.
g. The urine flows from the pelvis of the
B. NEPHRONS kidneys through the ureters and empties
a. Located within the parenchyma into the bladder.
b. Composed of glomerulus and
tubules FUNCTIONS OF KIDNEYS
c. Selectively secretes and 1. Maintain acid–base balance
reabsorbs ions and filtrates, 2. Excrete end products of body
including fluid, wastes, metabolism
electrolytes, acids, and bases 3. Control fluid and electrolyte balance
4. Excrete bacterial toxins, water-soluble
The nephrons are the functional units of medications, and medication
the kidney. metabolites
5. Secrete renin to regulate the blood
C. GLOMERULUS pressure (BP) and erythropoietin to
a. Each nephron contains tufts of stimulate the bone marrow to produce
capillaries, which filter large plasma red blood cells
proteins and blood cells. 6. Synthesize vitamin D for calcium
b. Blood flows into the glomerular absorption and regulation of the
capillaries from the afferent arteriole and parathyroid hormones
flows out of the glomerular capillaries
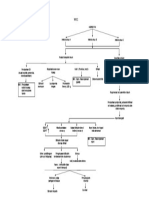
into the efferent arteriole. Urine Formation
D. BOWMAN’S CAPSULE Blood
1. Thin double-walled capsule that ↓
surrounds the glomerulus Renal Artery
a. Fluid and particles from the blood such ↓
as electrolytes, glucose, amino acids, Small Arteries called Arterioles
and metabolic waste (glomerular filtrate) ↓
are filtered through the glomerular Nephrons (functional unit of kidney)
membrane into a fluid-filled space in ↓
Bowman’s capsule (Bowman’s space) Bowman’s capsule
↓
Afferent Arteriole 2. Urinary urgency and frequency
↓ 3. Nocturia
Glomerulus 4. Inability to start (hesitancy) or continue a
↓ urinary stream
Efferent arteriole 5. Feelings of incomplete bladder emptying
↓ ↓ 6. Post-void dribbling from overflow
Filtered Blood Glomerular Filtrate incontinence (later sign)
↓ ↓ 7. Urinary retention and bladder distention
Renal Veins PCT 8. Hematuria
↓ ↓ 9. Urinary stasis and UTIs
Back to the Body Loop of Henle 10. Dysuria and bladder pain
↓
DCT Interventions
↓ Encourage fluid intake of up to 2000 to
Collecting Duct 3000 mL/day unless contraindicated.
↓ Prepare for urinary catheterization to
(Urine) Waste Products drain the bladder and prevent distention.
↓ Avoid administering medications that
Ureters cause urinary retention, such as
↓ anticholinergics, antihistamines,
Bladder decongestants, and antidepressants.
Administer medications as prescribed to
Tubular absorption and secretion shrink the prostate gland and improve
PCT urine flow.
absorbs H2O, Na, Glucose, Amino Acid, Administer medications as prescribed to
Urea back to blood relax prostatic smooth muscle and
Secretes wastes, drugs, improve urine flow.
Instruct the client to decrease intake of
RAS caffeine and artificial sweeteners and
Descending LOH – Absorbs water limit spicy or acidic foods.
Ascending LOH – Absorbs Sodium Instruct the client to follow a timed
DCT – Secretes K, H voiding schedule.
Collecting Duct – reabsorbs H2O Prepare the client for surgery or invasive
procedures as prescribed (see Chapter
45, Figs. 45.6)
BENIGN PROSTATIC HYPERTROPHY
(HYPERPLASIA)
Benign prostatic hypertrophy (benign BLADDER CANCER
prostatic hyperplasia; BPH) is a slow Bladder cancer is a papillomatous growth in
enlargement of the prostate gland, with the bladder urothelium that undergoes
hypertrophy and hyperplasia of normal malignant changes and that may infiltrate
tissue. the bladder wall.
Enlargement compresses the urethra,
resulting in partial or complete Predisposing factors
obstruction. 1. Cigarette smoking
Usually occurs in those older than 50 2. Exposure to industrial chemicals, and
years exposure to radiation
SIGNS AND SYMPTOMS Common sites of metastasis
1. Diminished size and force of urinary 2. Liver
stream (early sign of BPH)
3. Bones ● Targeted Therapy: Medications targeting
4. Lung specific molecules involved in cancer
growth.
As the tumor progresses, it can extend into MEDICATIONS:
the rectum, vagina, other pelvic soft tissues, ● Chemotherapy Drugs:
and retroperitoneal structures. ● Cisplatin, Gemcitabine, Methotrexate:
Commonly used in bladder cancer
ASSESSMENT
treatment.
1. Gross or microscopic, painless
● Immunotherapy:
hematuria (most common sign)
● Bacillus Calmette-Guérin (BCG): Intravesical
2. Frequency, urgency, dysuria
3. Clot-induced obstruction immunotherapy to stimulate an immune
4. Bladder wash specimens and biopsy response against cancer cells.
confirm diagnosis. ● Pembrolizumab, Atezolizumab: Checkpoint
inhibitors targeting the immune system.
DIAGNOSIS: NURSING INTERVENTIONS:
● Cystoscopy: A procedure to examine the ● Preoperative and Postoperative Care:
inside of the bladder using a thin tube ○ Education: Provide information on
with a camera. procedures, potential complications,
● Biopsy: Removal of a small tissue and postoperative care.
sample for laboratory examination. ○ Psychosocial Support: Address
● Imaging Studies: concerns, fears, and emotional well-
○ CT Scan: To assess the extent being.
of the cancer and identify ● Symptom Management:
potential spread. ○ Pain Control: Administer pain
○ MRI: Magnetic resonance medications as prescribed.
imaging may provide detailed ○ Fatigue Management: Encourage
images of the bladder. rest and provide support for fatigue.
○ Urine Cytology: Examination of ● Side Effect Management:
urine for cancer cells. ○ Nausea and Vomiting: Administer
○ Intravenous Pyelogram (IVP): antiemetic medications as needed.
An X-ray of the urinary tract ○ Monitoring for Complications: Watch
after injection of a contrast dye. for potential side effects of
TREATMENTS: treatments and report promptly.
● Surgery: ● Cystectomy Care:
○ Transurethral Resection of ○ Stoma Care: For patients with an
Bladder Tumor (TURBT): ostomy after cystectomy.
Removal of small tumors ■ Wound Care: Monitor and
through the urethra. care for incisions or surgical
● Partial or Radical Cystectomy: Partial or wounds.
complete removal of the bladder. ● Psychosocial Support:
● Chemotherapy: Systemic or intravesical ■ Counseling: Provide
(directly into the bladder) administration emotional support and
of drugs to kill cancer cells. resources for coping.
● Immunotherapy: Stimulating the immune ■ Communication:
system to target and destroy cancer Maintain open
cells. communication with the
● Radiation Therapy: Using high-energy patient and family.
rays to target and kill cancer cells.
10. Pulmonary Edema
11. Anorexia
12. Cardiovascular Problems
CHRONIC KIDNEY DISEASE (CKD)
CKD is a slow, progressive, irreversible loss ASSESSMENT
in kidney function, with a GFR less than or 1. Assess body systems for the
equal to 60 mL per minute for 3 months or manifestations of CKD
longer. 2. Assess psychological changes, which
It occurs in stages (with loss of 75% of could include emotional lability,
functioning nephrons, the client becomes withdrawal, depression, anxiety, denial,
symptomatic) and eventually results in dependence–independence conflict,
uremia or end-stage kidney disease (with changes in body image, and suicidal
loss of 90% to 95% of functioning behavior.
nephrons).
Hypervolemia can occur because of the DIAGNOSIS:
kidneys’ inability to excrete sodium and ● Blood Tests:
water; hypovolemia can occur because of ○ Creatinine and Blood Urea
the kidneys’ inability to conserve sodium Nitrogen (BUN): Elevated levels
and water. indicate impaired kidney
CKD affects all major body systems and function.
may require dialysis or kidney ○ Glomerular Filtration Rate
transplantation to maintain life. (GFR): A measure of kidney
function.
○ Electrolyte Levels: Assessing
imbalances such as high
potassium.
○ Urinalysis: Examination of urine
for abnormalities.
● Imaging Studies:
○ Ultrasound: To visualize the
kidneys and identify structural
PRIMARY CAUSES
abnormalities.
11. May follow AKI
○ CT Scan or MRI: Detailed
12. Diabetes mellitus and other metabolic
disorders imaging for assessing kidney
13. Hypertension structure.
14. Chronic urinary obstruction ○ Kidney Biopsy: In some cases,
15. Recurrent infections a sample of kidney tissue is
16. Renal artery occlusion taken for examination.
17. Autoimmune disorders
NURSING INTERVENTIONS
SIGNS AND SYMPTOMS 1. Monitor vital signs, especially for signs
1. Proteinuria of hypertension, tachycardia, tachypnea,
2. Polyuria, nocturia (Early Signs) and an irregular heart rate.
3. Oliguria, Anuria (Late Signs) 3. Monitor urine and intake and output
4. Diluted, straw colored urine hourly and urine color and
5. Hematuria characteristics and check laboratory
6. Anemia results.
7. Muscle Weakness and Cramps 4. Monitor daily weight (same scale, same
8. Poor skin turgor clothes, same time of day), noting that
9. Pruritus
an increase of 0.5 to 1 lb/day (0.25 to ○ Age: The risk increases with
0.5 kg/day) indicates fluid retention. age, and it is more common in
5. Monitor for altered level of people over 40.
consciousness caused by uremia ○ Gender: Men are more likely
6. Monitor the lungs for fine crackles, than women to develop kidney
wheezes, and rhonchi, and monitor for cancer.
edema, which can indicate uid ○ Obesity: Overweight individuals
overload.
have an increased risk.
7. Administer the prescribed diet, which is
○ High Blood Pressure:
usually a low- to moderate-protein (to
Hypertension is a risk factor for
decrease the workload on the kidneys)
and high-carbohydrate diet; ill clients kidney cancer.
may require nutritional support with ○ Genetic Factors: Hereditary
supplements, enteral feedings, or conditions, such as von Hippel-
parenteral nutrition. Lindau (VHL) disease.
8. Restrict potassium and sodium intake as ○ Family History: A family history
prescribed based on the electrolyte of kidney cancer may increase
level. the risk.
9. Administer medications as prescribed; ○ Occupational Exposure: Certain
be alert to the mechanism for workplace exposures to
metabolism and excretion of all chemicals like asbestos or
prescribed medications. cadmium.
10. Be alert to nephrotoxic medications,
which may be prescribed. ASSESSMENT
11. Be alert to the PHCP’s adjustment of
Dull flank pain
medication dosages for kidney injury.
Palpable renal mass
12. Prepare the client for dialysis if
Painless gross hematuria
prescribed; continuous renal
replacement therapy may be used in Weight Loss
AKI to treat fluid volume overload or Hematuria
rapidly developing azotemia and
metabolic acidosis. DIAGNOSIS:
● Blood Tests:
○ Creatinine and Blood Urea
KIDNEY TUMORS Nitrogen (BUN): Elevated levels
Kidney tumors may be benign or indicate impaired kidney
malignant, bilateral or unilateral. function.
Common sites of metastasis of ○ Glomerular Filtration Rate
malignant tumors include bone, lungs, (GFR): A measure of kidney
liver, spleen, and the other kidney. function.
The exact cause of renal carcinoma is ○ Electrolyte Levels: Assessing
unknown. imbalances such as high
potassium.
CAUSES:
○ Urinalysis: Examination of urine
● The specific causes of kidney cancer
for abnormalities.
are not always clear, but several risk
● Imaging Studies:
factors are associated with its
○ Ultrasound: To visualize the
development:
kidneys and identify structural
○ Smoking: Smokers have a
abnormalities.
higher risk of kidney cancer.
○ CT Scan or MRI: Detailed g. Maintain the client in a semi-Fowler’s
imaging for assessing kidney position.
structure. h. If a nephrostomy tube is in place, do not
● Kidney Biopsy: In some cases, a irrigate (unless specifically prescribed)
sample of kidney tissue is taken for or manipulate the tube.
examination.
MEDICATIONS: KIDNEY STONES / NEPHROLITIASIS
Calculi are stones that can form
● Tyrosine Kinase Inhibitors (TKIs):
anywhere in the urinary tract; however,
○ Sunitinib (Sutent)
the most frequent site is the kidneys.
○ Pazopanib (Votrient)
Problems resulting from calculi are
○ Cabozantinib (Cabometyx) severe intermittent pain, obstruction,
● mTOR Inhibitors: tissue trauma, secondary hemorrhage,
○ Everolimus (Afinitor) and infection.
○ Temsirolimus (Torisel) The stone can be located through
● Checkpoint Inhibitors: radiography of the kidneys, ureters, and
○ Nivolumab (Opdivo) bladder; IV pyelography; computed
○ Ipilimumab (Yervoy) tomography (CT) scanning; and renal
○ Pembrolizumab (Keytruda ultrasonography.
A stone analysis is done after passage
RADICAL NEPHRECTOMY to determine the type of stone and assist
a. Surgical removal of the entire kidney, in determining treatment.
adjacent adrenal gland, and renal artery Urolithiasis refers to the formation of
and vein urinary calculi; these form in the ureters.
b. Radiation therapy and possibly Nephrolithiasis refers to the formation
chemotherapy may follow radical of kidney calculi; these form in the renal
nephrectomy. parenchyma.
c. Before surgery, radiation may be used When a calculus occludes the ureter
to embolize (occlude) the arteries and blocks the flow of urine, the ureter
supplying the kidney to reduce bleeding dilates, producing hydro-ureter (see Fig.
during nephrectomy. 55.5).
If the obstruction is not removed, urinary
Postoperative interventions stasis results in infection, impairment of
a. Monitor vital signs for signs of bleeding renal function on the side of the
(hypotension and tachycardia). blockage, hydronephrosis (see Fig.
b. Monitor for abdominal distention, 55.5), and irreversible kidney damage.
decreases in urinary output, and
alterations in level of consciousness as Causes
signs of bleeding; check the bed linens 1. Family history of stone formation
under the client for bleeding. 2. Diet high in calcium, vitamin D, protein,
c. Monitor for signs of adrenal oxalate, purines, or alkali
insufficiency, which include a large 3. Obstruction and urinary stasis
urinary output followed by hypotension 4. Dehydration
and subsequent oliguria. 5. Use of diuretics, which can cause
d. Administer fluids and packed red blood volume depletion
cells intravenously as prescribed. 6. UTIs and prolonged urinary
e. Monitor intake and output and daily catheterization
weight. 7. Immobilization
f. Monitor for a urinary output of 30 to 50 8. Hypercalcemia and hyperparathyroidism
mL/hr to ensure adequate renal function. 9. Elevated uric acid level, such as in gout
facilitate the passage of the stone and
SIGNS AND SYMPTOMS prevent infection; monitor for
1. Renal colic, which originates in the obstruction.
lumbar region and radiates around the 6. Administer fluids intravenously as
side and down to the testicles in men prescribed if unable to take fluids orally
and to the bladder in women or in adequate amounts to increase the
2. Ureteral colic, which radiates toward the flow of urine and facilitate passage of
genitalia and thighs the stone.
3. Sharp, severe pain of sudden onset 7. Provide warm baths and heat to the
4. Dull, aching pain in the kidney flank area (massage therapy should be
5. Nausea and vomiting, pallor, and avoided).
diaphoresis during acute pain 8. Administer analgesics at regularly
6. Urinary frequency, with alternating scheduled intervals as prescribed to
retention relieve pain.
7. Signs of a UTI 9. Assess the client’s response to pain
8. Low-grade fever medication.
9. High numbers of red blood cells, WBCs, 10. Assist the client in performing relaxation
and bacteria noted in the urinalysis techniques to assist in relieving pain.
report 11. Encourage client ambulation, if stable, to
10. Gross hematuria promote the passage of the stone.
12. Turn and reposition the immobilized
DIAGNOSIS: client to promote passage of the stone.
● Blood Tests: 13. Instruct the client in the diet restrictions
○ Creatinine and Blood Urea specific to the stone composition if
Nitrogen (BUN): Elevated levels prescribed (Box 55.13).
indicate impaired kidney 14. Prepare the client for surgical
function. procedures if prescribed.
○ Glomerular Filtration Rate
SURGICAL MANAGEMENT
(GFR): A measure of kidney
1. Cystoscopy
function.
2. Extracorporeal Shock Wave
○ Electrolyte Levels: Assessing
Lithotripsy (ESWL)
imbalances such as high a. noninvasive mechanical
potassium. procedure for breaking up
○ Urinalysis: Examination of urine stones located in the kidney or
for abnormalities. upper ureter so that they can
● Imaging Studies: pass spontaneously or be
○ Ultrasound: To visualize the removed by other methods
kidneys and identify structural b. A stent may be placed to
abnormalities. facilitate passing stone
CT Scan or MRI: Detailed imaging for assessing fragments.
kidney structure c. Fluoroscopy is used to visualize
the stone, and ultrasonic waves
Interventions are delivered to the area of the
1. Monitor vital signs, especially stone to disintegrate it.
temperature, for signs of infection. d. The stones are passed in the
2. Monitor intake and output. urine within a few days.
3. Assess for fever, chills, and infection. e. The client is taught to watch for
4. Monitor for nausea, vomiting, and signs of urinary obstruction,
diarrhea. bleeding, or hematoma
5. Encourage fluid intake up to 3000 formation.
mL/day, unless contraindicated, to
f. Instruct the client to increase b. Prolonged prerenal ischemia
fluid intake to flush out the stone c. Intrarenal infection or obstruction
fragments. d. Nephrotoxicity (Box 55.3)
3. Percutaneous lithotripsy 3. Post-renal: Between the kidney and urethral
a. An invasive procedure in which meatus, such as:
a guide is inserted under a. Bladder neck obstruction
fluoroscopy near the area of the b. Bladder cancer
stone; an ultrasonic wave is c. Renal calculi
aimed at the stone to break it d. Post-renal infection
into fragments.
b. Percutaneous lithotripsy may be Phases of AKI
performed via cystoscopy or Onset: Begins with precipitating event
nephroscopy (a small flank
incision is needed for Oliguric phase
nephroscopy). o For some clients, oliguria does not
4. Partial or total nephrectomy occur and the urine output is normal;
a. Performed for extensive kidney otherwise, the duration of oliguria is
damage, renal infection, severe 8 to 15 days; the longer the
obstruction from stones or duration, the less chance of
tumors, and prevention of stone recovery.
recurrence o Sudden decrease in urine output;
urine output is less than 400
mL/day.
ACUTE KIDNEY INJURY (AKI) o Signs of excess fluid volume:
Renal Failure Hypertension, edema, pleural and
pericardial effusions, dysrhythmias,
Rapid loss of kidney function from renal cell heart failure, and pulmonary edema
damage. o Signs of uremia: Anorexia, nausea,
Occurs abruptly and can be reversible vomiting, and pruritus
AKI leads to cell hypoperfusion, cell death, o Signs of metabolic acidosis:
and decompensation of renal function. Kussmaul’s respirations
The prognosis depends on the cause and o Signs of neurological changes:
the condition of the client.
Tingling of extremities, drowsiness
Near-normal or normal kidney function may
progressing to disorientation, and
resume gradually.
then coma
o Signs of pericarditis: Friction rub,
Causes
chest pain with inspiration, and low-
1. Pre-renal: Outside the kidney; caused by
grade fever
intravascular volume depletion such as with:
Diuretic phase
a. Blood loss associated with trauma
o Urine output rises slowly, followed
or surgery
by diuresis (4 to 5 L/day).
b. Dehydration
o Excessive urine output indicates that
c. Decreased cardiac output (as with
cardiogenic shock) damaged nephrons are recovering
d. Decreased peripheral vascular their ability to excrete wastes.
resistance o Dehydration, hypovolemia,
e. hypotension, and tachycardia can
f. Decreased renovascular blood flow occur.
g. Pre-renal infection or obstruction o Level of consciousness improves.
2. Intra-renal: Within the parenchyma of the Recovery phase (convalescent)
kidney
a. Tubular necrosis
o Recovery is a slow process; Weigh Daily
complete recovery may take 1 to 2 High CHO
years. Low CHON, Na, K
o Urine volume returns to normal.
o Memory improves. PHARMACOLOGIC
o Strength increases. Kayaxelate
o The older adult is less likely than a o For hyperkalemia
younger adult to regain full kidney Diuretics
function. o For hypernatremia
AKI Laboratory Findings Nursing Diagnosis
1. Onset 1. Activity Intolerance
2. Oliguric Phase 2. Excess/Deficient fluid volume
Elevated blood urea nitrogen
(BUN) and serum creatinine
levels
Decreased urine specific gravity
(prerenal causes) or normal
(intrarenal causes) DIALYSIS
Decreased glomerular filtration Anticoagulant is used
rate (GFR) and creatinine o Prepare antidote
clearance No BP taking on affected arm or arm
Hyperkalemia with fistula
Normal or decreased serum Auscultate bruit sound
sodium level Palpate thrill
Hypervolemia PERITONEAL DIALYSIS
Hypocalcemia Infuse
Hyperphosphatemia Dwell
Outflow
3. Diuretic Phase Warm dialysate before use
Gradual decline in BUN and First few bottles of drainage has normal
serum creatinine levels, but still pink-tinged
elevated Cloudy Dialysate
Continued low creatinine o Infection
clearance with improving GFR o Report to doctor
Hypokalemia If drainage stops
Hyponatremia o Turn patient to side
Hypovolemia
4. Recovery Phase (Convalescent) Nursing Interventions
Increased GFR 1. Monitor vital signs, especially for signs
Stabilization or continual decline of hypertension, tachycardia, tachypnea,
in BUN and serum creatinine and an irregular heart rate.
levels toward normal 2. Monitor urine and intake and output
Complete recovery (may take 1 hourly and urine color and
to 2 years) characteristics and check laboratory
results.
MANAGEMENT 3. Monitor daily weight (same scale, same
Regular Insulin administration clothes, same time of day), noting that
Dialysis an increase of 0.5 to 1 lb/day (0.25 to
Water and Sodium Restriction 0.5 kg/day) indicates fluid retention.
4. Monitor for altered level of Causes
consciousness caused by uremia 1. Allergens or irritants, such as soaps,
5. Monitor the lungs for fine crackles, sprays, bubble bath, perfumed sanitary
wheezes, and rhonchi, and monitor for napkins
edema, which can indicate fluid 2. Bladder distention
overload. 3. Calculus
6. Administer the prescribed diet, which is 4. Hormonal changes, influencing
usually a low- to moderate-protein (to alterations in vaginal flora
decrease the workload on the kidneys) 5. Indwelling urinary catheters
and high-carbohydrate diet; ill clients 6. Invasive urinary tract procedures
may require nutritional support with 7. Loss of bactericidal properties of
supplements, enteral feedings, or prostatic secretions
parenteral nutrition. 8. Microorganisms
7. Restrict potassium and sodium intake as 9. Poor-fitting vaginal diaphragms
prescribed based on the electrolyte 10. Sexual intercourse
level. 11. Synthetic underwear and pantyhose
8. Administer medications as prescribed; 12. Urinary stasis
be alert to the mechanism for 13. Wet bathing suits
metabolism and excretion of all
prescribed medications.
9. Be alert to nephrotoxic medications,
which may be prescribed. Assessment
10. Be alert to the PHCP’s adjustment of 1. Frequency and urgency
medication dosages for kidney injury. 2. Burning on urination
11. Prepare the client for dialysis if 3. Voiding in small amounts
prescribed; continuous renal 4. Incomplete emptying of the bladder
replacement therapy may be used in AKI 5. Lower abdominal discomfort or back
to treat fluid volume overload or rapidly discomfort, bladder spasms
developing azotemia and metabolic 6. Cloudy, dark, foul-smelling urine
acidosis. 7. Hematuria
8. Malaise, chills, fever
9. WBC count greater than 11,000 mm3
ACUTE CYSTITIS (URINARY TRACT (11.0 × 109/L) on urinalysis
INFECTION)
Cystitis (urinary tract infection [UTI]) is an Interventions
inflammation of the bladder from an 1. Before administering prescribed
infection, obstruction of the urethra, or other antibiotics, obtain a urine specimen for
irritants culture and sensitivity, if prescribed, to
The most common causative organisms are identify bacterial growth.
Escherichia coli and Enterobacter, 2. Encourage the client to increase fluids
Pseudomonas, and Serratia species. up to 3000 mL/day, especially if the
Cystitis is more common in women, because client is taking a sulfonamide;
women have a shorter urethra than men and sulfonamides can form crystals in
the urethra in the woman is located close to concentrated urine.
the rectum. 3. Administer prescribed medications,
Sexually active and pregnant women are which may include analgesics,
most vulnerable to cystitis. antiseptics, antispasmodics, antibiotics,
Acute cystitis should not be confused with and antimicrobials.
interstitial cystitis which is a chronic 4. Maintain an acid urine pH (5.5); instruct
condition of the bladder associated with pain the client about foods to consume to
and pressure of the bladder. maintain acidic urine.
5. Provide heat to the abdomen or sitz
baths for complaints of discomfort.
6. Note that if the client is prescribed an
aminoglycoside, sulfonamide, or
nitrofurantoin, the actions of these
medications are decreased by acidic
urine.
7. Use sterile technique when inserting a
urinary catheter.
8. Provide meticulous perineal care for the
client with an indwelling catheter.
9. Discourage caffeine products such as
coffee, tea, and cola.
10. Client education
a. Avoid alcohol.
b. Take medications as prescribed.
c. Take antibiotics on schedule
and complete the entire course
of medications as prescribed,
which may be 10 to 14 days.
d. Repeat the urine culture
following treatment.
e. Prevent recurrence of cystitis
You might also like
- Urinary System Lecture NotesDocument8 pagesUrinary System Lecture NotesBettina ColobongNo ratings yet
- Urinary Renal SystemDocument24 pagesUrinary Renal Systemremotigue.brettelNo ratings yet
- Renal DisordersDocument14 pagesRenal DisordersPrince Rener Velasco Pera100% (1)
- Unit - Ii Human Anatomy and PhysiologyDocument15 pagesUnit - Ii Human Anatomy and PhysiologyRK YeleswarapuNo ratings yet
- Final Exam Review - Bio 172Document21 pagesFinal Exam Review - Bio 172Erin McElhaney QuirkNo ratings yet
- Anph111 Reviewer (Urinary & Endocrine)Document7 pagesAnph111 Reviewer (Urinary & Endocrine)Maria Clarisse ReyesNo ratings yet
- Chapter 18 Anaphy TransesDocument5 pagesChapter 18 Anaphy TransesHoly HaeinNo ratings yet
- PP24 Functioning of The KidneyDocument79 pagesPP24 Functioning of The Kidneyangie432meNo ratings yet
- الجهاز البولىDocument6 pagesالجهاز البولىNajwa AbdualgaderNo ratings yet
- Selected Lecture Notes Chapter 25: The Urinary System: I. Kidney Functions and AnatomyDocument12 pagesSelected Lecture Notes Chapter 25: The Urinary System: I. Kidney Functions and AnatomyMarilia BonorinoNo ratings yet
- Activity 4 Human Body CareDocument9 pagesActivity 4 Human Body CareAzael GómezNo ratings yet
- The Urinary SystemDocument18 pagesThe Urinary Systemabdulrehmanfaisal54No ratings yet
- The Urinary and Reproductive System (J.R) - Policarpio MAT Gen. Sci.Document60 pagesThe Urinary and Reproductive System (J.R) - Policarpio MAT Gen. Sci.john ronald PolicarpioNo ratings yet
- Anatomy and Physiology of The KidneysDocument21 pagesAnatomy and Physiology of The Kidneysccbrown750% (2)
- Kidney Function - ExcretionDocument15 pagesKidney Function - Excretionznayune82No ratings yet
- Renal SystemDocument29 pagesRenal Systemjsreyes.402No ratings yet
- Urinary System 1. List The Functions of The KidneysDocument6 pagesUrinary System 1. List The Functions of The KidneysheerNo ratings yet
- Ch20 Answer Key 12edition CorrectedDocument11 pagesCh20 Answer Key 12edition CorrectedTeuku Muhammad LizarNo ratings yet
- Urinary Tract ReciewDocument5 pagesUrinary Tract ReciewRobert LotzerNo ratings yet
- Medsurg LeDocument179 pagesMedsurg Leremotigue.brettelNo ratings yet
- MIRADOR, Kiana AnaphyAct16Document4 pagesMIRADOR, Kiana AnaphyAct16Kiana MiradorNo ratings yet
- Urinary Elimination: (Midterm)Document14 pagesUrinary Elimination: (Midterm)Mina RacadioNo ratings yet
- Excretory SystemDocument2 pagesExcretory SystemDearly Niña OsinsaoNo ratings yet
- CHAPTER 18 ANAPHY TransesDocument5 pagesCHAPTER 18 ANAPHY TransesHoly HaeinNo ratings yet
- The Kidney Excretion and OsmoregulationDocument12 pagesThe Kidney Excretion and OsmoregulationLashaunte Hodge HobsonNo ratings yet
- PDF Document 2Document14 pagesPDF Document 2Vari MafiaNo ratings yet
- Lec 18Document4 pagesLec 18Lyanna Louise SantosNo ratings yet
- Life Processes - Excretion - Humans & Plants - OriginalDocument36 pagesLife Processes - Excretion - Humans & Plants - Originalnouraft.07No ratings yet
- Renal SystemDocument17 pagesRenal SystemLess CastilloNo ratings yet
- 5 19 Excretory System PDFDocument12 pages5 19 Excretory System PDFHNo ratings yet
- Chapter 6Document3 pagesChapter 6John ErickNo ratings yet
- Excretory Products and Their EliminationDocument9 pagesExcretory Products and Their EliminationBiju MylachalNo ratings yet
- Chapter 9 Excretory System PDFDocument17 pagesChapter 9 Excretory System PDFErica Ann Ical100% (1)
- Assessment of Patients With Renal Disorders Management of Urinary Tract DisordersDocument16 pagesAssessment of Patients With Renal Disorders Management of Urinary Tract DisordersJhosita Flora LarocoNo ratings yet
- Human Physiology Ii: School of BiochemistryDocument15 pagesHuman Physiology Ii: School of Biochemistrykeerthana t reddyNo ratings yet
- Excretion in Humans VIII NOTESDocument6 pagesExcretion in Humans VIII NOTESfulhambrighton0No ratings yet
- Urinary SystemDocument77 pagesUrinary SystemJushelle Anne Tigoy PilareNo ratings yet
- Excretory Products and Their EliminationDocument13 pagesExcretory Products and Their Eliminationaravind kishanNo ratings yet
- 3 - Excretion NotesDocument33 pages3 - Excretion NotesJenny YoonNo ratings yet
- QuestionsDocument4 pagesQuestionsA GoswamiNo ratings yet
- Wella S, VIRINA Bsn-I: Review Question Urinary SystemDocument4 pagesWella S, VIRINA Bsn-I: Review Question Urinary SystemEllee HadesNo ratings yet
- Urinary SystemDocument28 pagesUrinary Systemgabanule brandonNo ratings yet
- Understanding Medical Surgical Nursing - 0849-0849Document1 pageUnderstanding Medical Surgical Nursing - 0849-0849Anas TasyaNo ratings yet
- Hafeezullah: Subject:Anatomy Topic: Anatomy of Excretory System Roll No: 15 Semester: 1 RepeaterDocument10 pagesHafeezullah: Subject:Anatomy Topic: Anatomy of Excretory System Roll No: 15 Semester: 1 RepeaterMuhammad ShahzaibNo ratings yet
- XQ WFHKLJW WWHAfu 0 DGWFDocument10 pagesXQ WFHKLJW WWHAfu 0 DGWFGiridharan & Balaji RNNo ratings yet
- KidneyDocument8 pagesKidneyRaj JadhavNo ratings yet
- Urinary SystemDocument9 pagesUrinary SystemMa Ellen LumauagNo ratings yet
- Introduction and Assessment of The Renal - Urological SystemDocument182 pagesIntroduction and Assessment of The Renal - Urological SystemValerie Suge-Michieka100% (1)
- Lecture Slides - Urinary SystemDocument41 pagesLecture Slides - Urinary SystemReneilwe MoshidiNo ratings yet
- Excretion: Excretory Organ Excretory ProductDocument3 pagesExcretion: Excretory Organ Excretory ProductKekeletsoNo ratings yet
- Chapter 19 Points To RememberDocument5 pagesChapter 19 Points To RememberSaksham YadavNo ratings yet
- Important Points of Excretory SystemDocument3 pagesImportant Points of Excretory SystemDhruv Nair IX ANo ratings yet
- Chapter 25 - Urinary System - Class OutlineDocument22 pagesChapter 25 - Urinary System - Class Outlinestupidisg00gleofcourseNo ratings yet
- Urinary RenalDocument44 pagesUrinary RenalgorekaNo ratings yet
- B2U3 Excretorysystem Notes 06Document5 pagesB2U3 Excretorysystem Notes 06Kudakwashe ChikazheNo ratings yet
- Genitourinary SystemDocument30 pagesGenitourinary SystemKarenNo ratings yet
- (BIO) Chapter 9 - Excretion in HumansDocument14 pages(BIO) Chapter 9 - Excretion in Humansanya desilvaNo ratings yet
- 11 Biology Chapter 20.Document4 pages11 Biology Chapter 20.jackieaj093No ratings yet
- Kidney Diseases, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandKidney Diseases, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- What Are The Advantages and Disadvantages of A Water Level ContrDocument8 pagesWhat Are The Advantages and Disadvantages of A Water Level ContrGod's willNo ratings yet
- Medical Terminolgy Trans 1 115 SlidesDocument14 pagesMedical Terminolgy Trans 1 115 SlidesSophia Nicole LibaoNo ratings yet
- Valves Quality Control PlanDocument1 pageValves Quality Control Planjok1974No ratings yet
- Narasimham Committee: By: Pranav Dagar 2019PBA9202 MBAC401Document12 pagesNarasimham Committee: By: Pranav Dagar 2019PBA9202 MBAC401Diksha VashishthNo ratings yet
- Massage Therapy PDFDocument1 pageMassage Therapy PDFVirgilio BernardinoNo ratings yet
- Taenia SagitaDocument3 pagesTaenia SagitaNur LiyanaNo ratings yet
- CHRA 1st Reprint 2018 PDFDocument149 pagesCHRA 1st Reprint 2018 PDFMohd Jamalil Azam MustafaNo ratings yet
- Full Download Ebook Ebook PDF Nutrition Science and Applications 4th Edition by Lori A Smolin PDFDocument42 pagesFull Download Ebook Ebook PDF Nutrition Science and Applications 4th Edition by Lori A Smolin PDFbessie.skubis114100% (42)
- Bhopal Gas Tragedy Causes, Effects and Aftermath - GeeksforGeeksDocument1 pageBhopal Gas Tragedy Causes, Effects and Aftermath - GeeksforGeeksmxdczc5yxzNo ratings yet
- Ilovepdf Merged PDFDocument8 pagesIlovepdf Merged PDFHeta PanchalNo ratings yet
- Report Beauty and Wellness Market in IndiaDocument35 pagesReport Beauty and Wellness Market in IndiaRenu R NairNo ratings yet
- NC State PDFDocument27 pagesNC State PDFquantum16No ratings yet
- Australian/New Zealand StandardDocument9 pagesAustralian/New Zealand StandardhanryNo ratings yet
- Dintzis ExerciseDocument5 pagesDintzis ExerciserichschurNo ratings yet
- The Inconvenient Truth About Cancer and Mobile PhonesDocument2 pagesThe Inconvenient Truth About Cancer and Mobile PhonesVictoria caroline Mendes de jesusNo ratings yet
- 046: Unsafe Acts vs. Unsafe Conditions: Background Discussion Leader Duties For This SessionDocument2 pages046: Unsafe Acts vs. Unsafe Conditions: Background Discussion Leader Duties For This SessionVarahi VigneshNo ratings yet
- Dcode EFC-Healthcare Snapshot (February 2021) - 1Document7 pagesDcode EFC-Healthcare Snapshot (February 2021) - 1hussienNo ratings yet
- WWW - Irctc.co - in Eticketing Printticket - JSF PNR 41298787 PDFDocument1 pageWWW - Irctc.co - in Eticketing Printticket - JSF PNR 41298787 PDFManav GaneshNo ratings yet
- Acid Value and Amine Value of Fatty Quaternary Ammonium ChloridesDocument3 pagesAcid Value and Amine Value of Fatty Quaternary Ammonium ChloridesShaker Qaidi100% (1)
- Serie-6-Ttv Brochure enDocument16 pagesSerie-6-Ttv Brochure envaneaNo ratings yet
- Present Tense Exercise 18Document1 pagePresent Tense Exercise 18Adrijan AlispahićNo ratings yet
- NEK606 JScableDocument40 pagesNEK606 JScablenc_eanNo ratings yet
- Drug and Alcohol Testing in The WorkplaceDocument16 pagesDrug and Alcohol Testing in The WorkplaceYasmin KayeNo ratings yet
- Saudi Arabian Standard SASO IEC 60601-2-57/2012Document35 pagesSaudi Arabian Standard SASO IEC 60601-2-57/2012Gigi EssegiNo ratings yet
- WOC HepatitisDocument1 pageWOC Hepatitisdestri wulandariNo ratings yet
- RTN 320 V100 Quick Installation Guide 02Document37 pagesRTN 320 V100 Quick Installation Guide 02Juan Pablo CharrisNo ratings yet
- Baylon RatioDocument4 pagesBaylon RatioJaessa Feliciano100% (1)
- Plasterers Stilts Fact Sheet 3955 PDFDocument4 pagesPlasterers Stilts Fact Sheet 3955 PDFneyemhey2348513No ratings yet
- LEBV4830 04 MartinDocument380 pagesLEBV4830 04 MartinjibvNo ratings yet
- Geothermal Energy: The Power of Heat Right Under Your FeetDocument70 pagesGeothermal Energy: The Power of Heat Right Under Your FeetSarthak DixitNo ratings yet