Professional Documents
Culture Documents
Levi Pathobiology 2002
Levi Pathobiology 2002
Uploaded by
rifkyfauzan725Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Levi Pathobiology 2002
Levi Pathobiology 2002
Uploaded by
rifkyfauzan725Copyright:
Available Formats
Review
Received: February 19, 2002
Pathobiology 2002–03;70:55–68
Accepted: July 29, 2002
DOI: 10.1159/000067305
Peyer’s Patches: Organized Lymphoid
Structures for the Induction of Mucosal
Immune Responses in the Intestine
L.H.C. Makala N. Suzuki H. Nagasawa
National Research Center for Protozoan Diseases, Obihiro University of Agriculture and Veterinary Medicine,
Hokkaido, Japan
Key Words Background
Distribution W Structure W Ontogeny W Immune response W
IgA Joseph Hans Conrad Peyer, a Swiss anatomist and
physician (1653–1712) in 1677 provided the first accurate
description of the discrete lymphoid aggregates in the
Abstract intestinal wall, which have come to bear his name [1, 2].
Peyer’s patches (PP) comprise transmucosal clusters of In the mid-19th century, Brucke provided illustrations of
lymphoid follicles overlaid with a specialized lympho- the microscopic appearance of Peyer’s patches (PP) in
epithelium and consequently play a central role in the dogs and cats, also noting that the tissues were organized
induction of mucosal immune responses in the gut. into discrete follicles, surrounded by connective tissue [3].
Despite considerable achievements in the last 3 decades, Three decades later, Fleming established that PP were
in our understanding of how PP are involved in the localized sites of intense lymphocyte division and consid-
induction of immune responses, much remains to be ered the reactive centres in lymph nodes and PP follicles
learned about these major organized lymphoid organs. to be similar [4]. Thus began the convention, which most
The history and current status of PP termed ‘the major immunologists still follow to date that the specialized sites
inductive site of immune responses’ is reviewed. The of lymphocyte division in lymph nodes, spleens and PP
present understanding of PP biology and function, taking follicles were germinal centres. Later, Carlens [5] made
into account their preferential and unique retention of the important observation that PP of cows, sheep, pigs
immune competent cells at specific sites, is discussed. and horses developed at specific regions of the gut during
Copyright © 2002 S. Karger AG, Basel fetal life and that after birth they had distinctive develop-
mental patterns. These structures have also been termed
intestinal tonsils or aggregated follicles [reviewed in 2, 6–
8]. Early research concentrated on describing the anatom-
ical distribution of PP along the intestine and their histol-
ogy. The expansion of cellular immunology in the late
1960’s and the definition of the role of T and B lympho-
© 2002 S. Karger AG, Basel H. Nagasawa, MD
ABC 1015–2008/02/0702–0055$18.50/0 National Research Center for Protozoan Diseases
Fax + 41 61 306 12 34 Obihiro University of Agriculture and Veterinary Medicine
E-Mail karger@karger.ch Accessible online at: Inada-Cho, Obihiro, Hokkaido 080-8555 (Japan)
www.karger.com www.karger.com/pat Tel. +81 155 49 5644, Fax +81 155 49 5643, E-Mail nrcpmi@obihiro.ac.jp
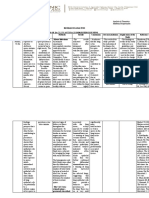
Table 1. Names, dates, scientific findings and theories that emerge in the history of the development of Peyer’s patches
Authors Dates Scientic finding/theory Reference
Peyer 1677 PP are mucus-secreting lymphoid aggregates 1
Brucke 1851 PP are discrete lymphoid follicles connected to lymphatics and surrounded 3
by connective tissues
Fleming 1885 PP are localised sites of lymphocyte division and found to have similarities 4
with germinal centres
Carlens 1928 jejunal (discrete) PP and ileal (continuous) PP have distinct developmental 5
patterns
Cooper and Lawton 1973 PP are sites of antigen handling and induction of IgA mucosal immune 11, 13
Craig and Cebra 1971 responses and other immune responses
Griebel and Hein 1996 PP are a site for the systemic B cell pool and generation of the primary 6–8, 24, 25
Neutra et al. 2001 immunoglobulin repertoire and PP lymphocytes also play a key role in 56, 57
Kraehenbuhl and Neutra 2000 induction of lympho-epithelium and M cells
Reynolds 1985
Reynolds et al. 1985
Kerneis et al. 1997, 2000
Data obtained from paper referenced in the text [6].
cytes gave great impetus to studies on the function of lym- can be removed easily. From experiments with bursec-
phoid tissues in mammals that may be secondary organs tomized chickens it was shown that the bursa has a major
from which progenitors involved in the regulation of role in antibody production [9]. Experiments in which
immune responses may be derived. It is also important to chickens were either bursectomized or thymectomized
mention that, beyond the original structural and morpho- suggested that the cells concerned in humoral antibody
logical studies conducted 20–25 years ago, very little work responses and cell-mediated immune responses were de-
has been carried out on the structure and morphology of rived from the bursa of Fabricus (B cells) and thymus (T
PP in mammals in the last decade. It is generally accepted cells) respectively [10]. It has been suggested that lym-
that PP are important structures in the gut wall for the phoid follicles in the gut of mammals may serve a similar
initiation of immune reactions. However, major species function as the bursa in birds [reviewed in 11]. In pig,
differences have often been ignored and recent progress in sheep and cattle, the ileal PP (IPP) probably still serves
understanding the regulation of M cell development and this function. However, some studies indicate that in
antigen uptake is often not included in textbooks of most mammals, cell from a number of organs are able to
immunology. Therefore, the need for a review on the differentiate into antibody producing cells [12]. Previous
structure and function of PP cannot be overemphasized. and recent studies have demonstrated that PP are a source
Most of the recent work on PP has been biased towards of precursor cells for IgA production [13–16]. The names,
the role of Peyer’s patch B cells as a source of IgA precur- dates and scientific findings and theories that emerge in
sor cells and the role of Peyer’s patch T cells as regulating the history of the development of PP are summarized in
cells involved in the control of immunoglobulin isotype, table 1.
both of which will be discussed in a later section of this
review.
Extensive studies have been carried out on the bursa of Distribution and Structure of the
Fabricus in birds which is similar in some respects to PP. Peyer’s Patches
The bursa is a hollow plicated sac, which contains a large
number of lymphoid follicles. It is connected to the cloaca PP comprise transmucosal clusters of lymphoid folli-
by a narrow canal, the bursal duct. The bursa is the major cles in the small intestine, which appear ellipsoidal when
follicular lymphoid tissue in the intestine of birds and it viewed from the serosal surface of the small intestine. In
56 Pathobiology 2002–03;70:55–68 Makala/Suzuki/Nagasawa
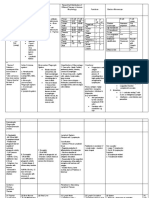
Table 2. Distribution and development of
Peyer’s patches in the different species Species Number of Peyer’s patches Development Reference
that have been studied ileum jejunum
Guinea pig 18–23 postnatal 80, 90
Rat 15–22 postnatal 2, 63, 79, 94
Rabbit sacculus rotundus 2–10 postnatal 13, 21, 27, 29, 98, 99
Human several 150–250 prenatal 22
Horses several 240–320 prenatal 5
Cattle single 25–45 prenatal 5, 17, 27
Sheep single 25–40 prenatal 5, 26, 61
Mice 5–14 postnatal 26, 28, 61, 89
Pig single 11–33 prenatal 18–20, 23, 30, 60, 111
Dog single 25–30 prenatal 78
Chicken (birds) bursa of Fabricius 2–4 postnatal 9–11
Data were obtained from papers referenced in the text (note – the PP equivalent in birds is
the bursa of Fabricius).
Table 3. Compartments,
sub-compartments and the main cell Compartments Sub-compartments Main cell types
types in a typical Peyer’s patch lymphoid non-lymphoid
Follicle1 corona T & B cells
medulla small T and B cells follicular dendritic
cortex lymphoblasts cells, macrophages
Inter-follicular area1–3 – T lymphocytes interdigitating
dendritic cells (IDC),
macrophages
Dome1, 2 – plasma cells macrophages
B cells IDC
T cells monocytes
Lympho-epithelium1 – T and B cells M cells, enterocytes
plasma cells
Data were obtained from papers referenced in the text [20, 54].
IDC = Interdigitating dendritic cells.
1 Fibroblastic reticulum cells usually are found present in all the above compartments.
2 Reticular and collagen fibers are abundant in the dome and inter-follicular areas.
3 High endothelial venules are located in the inter-follicular areas.
rats, PP are usually 3–4 mm long [2] but in larger animals, of PP [17, 23–25]. In these species a large continuous PP
for example cattle, PP may extend up to 4 m along the extends along the terminal segment of the intestine. In
intestine [17]. PP numbers vary between species [18–20] sheep this patch extends for 2–3 m and involutes at about
and they are located along the anti-mesenteric margin of 1 year of age [26] and in cattle it extends for up to 4 m
the intestine [17]. In rabbits 5–9 PP are normally present along the terminal ileum. The inter-host species compari-
[21], whereas in man there may be as many as 100–300 son of the distribution and development of PP in which
[22]. Studies in humans [22], sheep, horses [5] and cattle PP have been studied are shown in table 2. From the spe-
[17] have shown that the ileum has the greatest density of cies studied in sufficient detail (table 3), it is possible to
PP. In pigs, sheep and cattle there are two separate types define two broad groups with distinct anatomical and
Peyer’s Patches: Organized Lymphoid Pathobiology 2002–03;70:55–68 57
Structures
Fig. 1. A simplified diagrammatic represen-
tation of the transverse section of a typical
Peyer’s patch, showing compartments. (Data
were obtained from papers referenced in the
text [20].)
developmental patterns in terms of the amount of PP tis- DPP, approximately 25–35 in number, are comparatively
sue found in different segments of the small intestine. The small, are distributed along the jejunum and proximal
first group (I) includes ruminants, pigs, dogs, horses and ileum and are persistent throughout life.
humans [6]. In these, PP are unequally distributed along Detailed histological studies of PP have been carried
the small intestine, with more occurring in the ileum than out in mice [28], rats [2], rabbits [29], cattle [27] and
in the jejunum. Moreover, in these species, the IPP occurs sheep [26]. In pig, work has been carried out on the mor-
as a single continuous aggregation of lymphoid follicles, phology, numbers and sizes of PP [19, 20, 30]. A trans-
commencing at or near the ileo-cecal junction and extend- verse section of a typical PP and its cell types are shown
ing cranially for a variable distance. In group II species, diagrammatically in figure 1, as illustrated in our pre-
namely rabbits, rodents and chickens (birds), the distribu- vious work [20]. The follicles of PP are usually pear
tion of PP occurs at more or less random intervals along shaped. The region between the follicle and the lympho-
the ileum and jejunum [2, 27]. While the development of epithelium is called the dome. The lymphoid cells in the
PP in group-I species is prenatal, the development of dome are mainly T cells, plasma cells, interdigitating den-
group II species is postnatal. Some group II species, dritic cells and tangible body macrophages as demon-
namely the rabbit and the birds have a specialized gut- strated in previous and recent studies [19, 27, 28, 31–33].
associated lymphoid tissue in other regions of the intes- In rabbits, rats and mice the majority of epithelial cells
tine, i.e., the sacculus rotundus and an exaggerated appen- overlying the dome and the follicles have a microvillus
dix in rabbits, and the bursa of Fabricius in chicken. Work brush border, but 20–30% have microfolds at the luminal
has shown that in species with a large terminal ileum PP, surface and have been called microfold or M cells [12].
the function of this structure is probably quite different The lympho-epithelium or follicle-associated epithelium
from that of discrete PP (DPP) [26]. The involvement of of PP in rats, mice and rabbits [34–36] contain B and T
the ileal PP in B cell differentiation has been reported. lymphocytes than villous epithelium. Moreover, a few
This may likely be its function. In sheep the jejunal or plasma cells have been reported to occur in the rat M cell
58 Pathobiology 2002–03;70:55–68 Makala/Suzuki/Nagasawa
Fig. 2. Photomicrographs of indirect immu-
noperoxidase stained sections of pig discrete
Peyer’s patches at 35 days of age (!150)
showing leukocytes expressing: A CD2
(MSA4); B CD3 (FY-1HZ); C SwC3
(742215); D MHC class II – SLA-DR
(MSA3). SwC3 (742215) is a monocyte/gran-
ulocyte marker sometimes known as the my-
eloid marker. Cluster of differentiation (CD)
or swine workshop cluster number (SwC3)
designating specificity of the antigens used.
The clone numbers are shown in brackets as
sanctioned by the Veterinary Immunology
Committee of the International Union of
Immunological Scientists. LE = Lympho-
epithelium; DO = dome; FO = follicle; IFA =
inter-follicular area.
pockets [37]. Although M cells have been studied for more viewed in 38]. The ultra-structure and several immuno
than 20 years, clear-cut definitions for the identification and lectin histochemical properties of M cells vary ac-
of M cells independent of species and location do not cording to species and locations along the intestine [38].
exist. In order to study M cells on a light microscopic lev- Lectins detecting fucose or N-acetyl-galactosamine selec-
el, several groups established histochemical markers that tively labelled M cells in rabbit cecal patches [39, 40] and
detect cytoplasmic or membrane-bound molecules spe- in BALB/c mice lectins of Ulex europaeus (UEA-1) and
cific for M cells. Current markers include enzymatic Lotus tetragonolobus (LTA) [41, 42]. However, it is still
activities, unidentified proteins that are bound by mono- unclear whether the detection of M cells by lectins can be
clonal antibodies, cytoskeletal perculiarities, and certain generalized or restricted to certain species and sites of
terminal saccharides of glycoproteins and glycolipids [re- GALT. In other studies, Gebert et al. [40] showed that
Peyer’s Patches: Organized Lymphoid Pathobiology 2002–03;70:55–68 59
Structures
vimentin, an intermediate filament protein, is expressed The dome of the PP extends through a channel in the
in rabbit M cells in addition to cytokeratin [43], especially muscularis mucosa and expands in the submucosa to
cytokeratin peptides 18 and 19. In the mouse, M cells form the bodies of follicles. Pollard and Sharon [58]
express MHC class II antigens and IL-1 as is the case with described this region in mouse as a germinal zone and
other epithelial cells and they have been shown to play an there are similarities with the germinal centres found in
important role in transporting luminal antigens into PP the lymph nodes and spleens. In the mouse, the medullary
[reviewed in 7, 8, 44–47]. Bockman and Cooper [48] zone of the PP follicles contain small lymphocytes (B and
showed that colloidal carbon and ferritin in the lumen of T cells), lymphoblasts, follicular dendritic cells and mac-
the intestine were taken up by epithelial cells associated rophages [28]. Macrophages are presumed to be the cells
with PP of the mouse. The epithelial cells associated with responsible for the uptake of carbon in mice chronically
the adjacent villi did not take up any of this material. In fed carbon in their drinking water [59]. In mice and rab-
some circumstances villous epithelial cells have been bits the medullary zone of PP is surrounded serosally and
found to take up material from the lumen of the intestine laterally by a cortical zone containing small lymphocytes,
[49], but it seems this activity is small by comparison to blast cells and many mitotic cells indicating that this is the
the epithelial cells overlying the follicles of the PP. In region where cell proliferation is occurring [27]. The
experiments involving the morphometric analysis of lyso- medulla of the follicle is separated from the dome region
somes in M cells, Owen et al. [50] established that the by a dense cuff of small lymphocytes called the corona
small volume fraction of dense bodies (lysosomes) in M [27, 31].
cells provides an explanation for transport of luminal The body of the follicle in the submucosa is sur-
material across the epithelium by M cells without lyso- rounded by a connective tissue-sheath and the region
somal degradation. Both soluble molecules, for example, between the follicles is referred to as the interfollicular
horseradish peroxidase [51] and viable micro-organisms, area (IFA). In the rabbit appendix [27, 31] and in some PP
for example Salmonella typhimurium [52], have been in calves [27], adjacent follicles are separated by only a
shown to be taken up by M cells after entering PP in mice. narrow connective tissue space, which contains blood and
These observations are consistent with the hypothesis that lymph vessels. However, the follicles of most PP are sepa-
M cells provide controlled transport of undegraded-lumi- rated from each other by a densely packed region of lym-
nal particles and macromolecules into lymphoid follicles phoid cells, which extends from the muscularis mucosa to
for immunologic surveillance and initiation of appro- the submucosa. This region contains mainly macrophages
priate immune responses [7, 8, 53–55]. Kerneis et al. [56] and interdigitating cells, small lymphocytes and blast cells
assessed the ability of PP lymphocytes to convert entero- [27, 28]. Small numbers of plasma cells [28], macrophages
cytes into M cells. In a series of experiments the authors [28, 29] and mitotic cells [31] have also been found in this
were able to show that when lymphocytes freshly isolated region. B and T cells leave PP out of the mucosa via effer-
from PP were injected into the duodenal mucosa of recip- ent lymphatics and into the blood circulation. Thereafter,
ient mice at sites lacking organized lymphoid tissues, PP- these cells enter the cysterna chyli, returning the cells to
like structures had developed. In a more recent study, the venous circulation via the thoracic duct re-entering
Kerneis et al. [57] showed that PP lymphocytes co-cul- the intestine via high endothelial venules in the IFA. The
tured with Caco-2 cells trigger the phenotypic conversion compartments, sub-compartments and the main cell
of enterocytes into M cells that express morphological and types in a typical PP are summarized in table 3.
functional M cell properties [reviewed in 57]. Given this
stimulating and provocative data on the induction of M
cells by lymphoid cells, it should now be possible to iden- Ontogeny of Peyer’s Patches
tify signals produced by lymphocytes responsible for M
cell function, to help characterize the mechanisms me- Follicles have been identified by mid gestation in the
diating cytoskeletal re-organization and transcytosis as intestine of pigs [60] and sheep [26, 61]. However, they do
well as analyse the cellular machinery mediating micro- not appear until around the time of birth in mice [62], rats
organism translocation through M cells, thus facilitating [2, 62] and rabbits [27]. Recent data using knockout mice
the design of oral vaccines and efficient mucosal drug has shown that formation of PP requires complex interac-
delivery systems. These observations support the hypoth- tions between the gut epithelium, the mesenchyme, and
esis that PP lymphocytes play a key role in the induction bone-marrow-derived hematopoietic progenitors and this
of lymphoid follicle associated epithelium and M cells. has provided insight into the molecular nature of the sig-
60 Pathobiology 2002–03;70:55–68 Makala/Suzuki/Nagasawa
nals that mediate PP ontogeny [64, 65]. In a series of genic stimulation could bring about differentiation in
experiments, the authors have shown that PP are first vis- these species. The development of PP has been studied
ible at approximately 15.5 weeks gestation after which after birth in germ free environment mice [58], rats [79]
there is a rapid spurt in the development and maturation and guinea pigs [80]. Each of these studies showed that if
of lymphoid follicles so that at any given point of time animals are kept in a germ free environment, PP remain
new foci of PP development are continuously formed at a small and do not differentiate, but in a conventional envi-
rapid rate. Brandtzaeg [66] and Brandtzaeg et al. [67] ronment, PP take a normal appearance [81]. In gnotobiot-
summarized mechanisms for induction of specific local ic pigs, Pabst et al. [18], and in large white landrace pigs,
immunity, with emphasis on the molecular events that Makala et al. [20] established that age and microbial con-
determine the distribution of primed lymphoid cells to tent of the gut both influence the size of the PP, but their
provide adaptive mucosal surface defence in humans. In a numbers and position remain constant.
series of studies in humans, they concluded that adaptive The relationship between the development of PP and
immune protection of mucuous membranes is provided response to antigen can, in some aspects, be deduced from
mainly by secretory IgA (sIgA) antibodies [67–71]. Partly studies of the appendix tissue, which has certain structur-
because human IgA lacks ordinary complement activat- al similarities to PP. The effect of antigen on the develop-
ing properties, immune exclusion performed by sIgA anti- ment of PP and the appendix has also been studied by
bodies in principally a noninflammatory protective mech- isolating intestinal lymphoid follicles from the intestinal
anism [69]. This first line of defence is accomplished contents. Stramignoni et al. [82] ligated the appendix half
through an ingenious cooperation between the mucosal B way along its length in rabbits 4 h after birth. In these ani-
cell system and the epithelial glycoprotein called secretory mals the intestinal contents had no access to the distal half
component (SC). This is quantitatively the most impor- of the appendix whereas they could enter the proximal
tant receptor of the immune system because it is responsi- half. During the first week the development of PP was
ble for external transport of locally produced polymeric normal in the isolated segment and the follicles grew to a
IgA (pIgA). Polymeric IgA has been shown to bind to the moderate size. During the second week the follicles in the
J-chain in the region of contact between 7S monomers of normal segment of the appendix became very large and
sIgA [72–74] and mediates the transcytosis of IgA to the differentiated into cortex and medulla. In the isolated seg-
luminal surface of the epithelium [75–77]. The B cells ment the follicles grew slowly and failed to show this dif-
responsible for the local pIgA production are initially ferentiation. It could be suggested from this work that the
stimulated in lympho-epithelial structures, particularly development of the lymphoid follicles depends on stimu-
the PP in the distal small intestine, from which they lation by bacterial antigen [20, 58] in conjunction with
migrate as memory cells to exocrine tissues all over the normal intestinal microflora [20, 83]. However, it is
body. doubtful whether such a general conclusion can be ex-
Studies in pigs have shown that at birth PP are visible tended to all species, especially those in which PP have
to the naked eye and histologically they are composed of been reported to mature before birth.
mononuclear cells [19, 20, 60]. In both mice and rabbits
the follicles are small at the end of gestation but after birth
they increase rapidly in size and differentiate into distinct Induction of Immune Responses by
zones [60]. The rapid postnatal development of the folli- Peyer’s Patches
cles in these species suggest that this may be in response to
luminal antigens [20]. Despite the proximity of the gut- Evidence exists that mucosal PP are the primary site of
associated lymphoid tissues (GALT) to antigens in the antigen handling [15, 16, 19, 20, 84–88]. Certainly the cell
intestinal lumen, the evidence that the development of types, which have become associated with the induction
these tissues is influenced by antigenic stimulation is of immune responses can be recognised in PP [20, 33] (fig-
uncertain and conflicting [11]. The proximity of PP lym- ure 2). B cells have been demonstrated in PP of mice [89],
phoid follicles to the highly antigenic contents of the intes- guinea pigs [90] and rabbits [91]. T cells have been dem-
tine has led to the suggestion that the high rate of prolifer- onstrated in PP of mice [92], although Perey and Gutt-
ation in these areas may be due to antigenic stimulation. man [93] have shown that cells derived from PP do not
It is still uncertain what effect, if any, antigen has on PP. have the same capacity for mediating a graft-versus-host
Follicular differentiation of PP has been reported to response as T cells obtained from the other lymphoid tis-
occur in utero in dogs [78]. It is likely therefore, that anti- sues. T cells have also been identified in PP of guinea pigs
Peyer’s Patches: Organized Lymphoid Pathobiology 2002–03;70:55–68 61
Structures
[90], in rats [94] and rabbits [95]. The fact that specific PP of mice were unable to respond to antigen because the
lymphocyte subsets and APC are essential for various T cells and B cells of the patch were denied access to mac-
immune reactions and have to lie in close vicinity cannot rophages or dendritic cells.
be over-emphasized. Therefore it is important to know However, more recent reports indicate that cells within
the subset composition of lymphocytes in PP dome epi- the PP can take up and present antigens to local T cells or
thelium. Here, per 100 Ìm of epithelium, 3.6 lympho- transport them to other sites for subsequent processing
cytes were seen in specific pathogen free mice and 11.3 and/or presentation. The capability of the intestinal cells
lymphocytes in conventional mice [96] indicating the to take up and transport antigens is supported by the find-
stimulating effect of microbial antigens. In adult rats, two ing that veiled cells migrating from rat and mouse intes-
times more lymphocytes were found in the epithelium of tine are capable of transporting bacterial antigens in rat/
the domes than that of the villi [34]. In humans, an even mouse infected with Salmonella typhimurium [100]. Kel-
higher difference was demonstrated, but with a greater sall and Strober [101, 102] have demonstrated the pres-
inter-individual variation, e.g., a median of 3.0 lympho- ence of two populations of PP dendritic cells in mouse,
cytes (range 2.1–5.3) per unit area of the dome epithelium one of which forms a dense layer just beneath the dome
in contrast to 1.2 (range 1.0–1.6) for the villus epithelium epithelium and another phenotypically distinct popula-
[37]. In rats, the lymphoid cells associated with M cells tion in the IFA. In this study PP dendritic cells were
were distributed as follows: 15 B 3% small lymphocytes, shown to be capable of inducing proliferation in T cells in
24 B 3% medium lymphocytes, 16 B 4% immunoblasts, vivo and vitro, suggesting that the DC population in the
and 5 B 1% plasma cells [34, 38]. The ratio of helper to T PP are uniquely positioned for the processing of antigens
cytotoxic lymphocytes is 0.6:10 in the villus, but 4:10 in and that PP dendritic cells are effective at processing and
the dome epithelium, which indicates a much higher fre- presenting antigens to naı̈ve T cells. It is likely then, that
quency of T helper cells in the dome epithelium [37]. In a the induction of intestinal immune responses can take
more recent report by the same group, nearly three quar- place in PP. It is now generally accepted that cells from
ters of all T cells in the dome epithelium were found to be PP, when stimulated by antigens, do not mature into anti-
T helper cells (CD4+, range 40–90%) [54]. In similar stud- body forming cells until they migrate to other regions of
ies, Andersen et al. [97] systematically characterized pig the body.
IPP follicular lymphocytes and showed that about 90% B
cells were positive for surface immunoglobulin G (sIgM+)
and expressed an immature phenotype characterized by Migration of Cells to Peyer’s Patches
the expression of a myeloid marker sWC3 (74-22-15) and
two molecules recognized by IPP B cell specific mono- In experiments with parabiotic chick embryos in which
clonal antibodies (F4/4, F12/35). In a series of experi- a chromosome marker was used to identify cells of one of
ments the authors concluded that pig IPP were equivalent the pair have shown that cells in the embryonic bursa of
to sheep IPP. Fabricius are migratory cells derived from the circulation
Contradictory evidence for the existence of antigen- [103]. Although conclusive evidence has not been ob-
presenting cells (APC) in PP was provided by early work. tained it seems likely that cells in the developing intestinal
In the PP of rabbits all the cells needed for the induction follicles of mammals are also cells, which migrate to these
of immune responses are present [29]. Henry et al. [98] tissues from the blood.
showed that cell cultures prepared from rabbit PP pro- The generation of IgA responses involves the migra-
duced plaque-forming cells in vitro when mixed with tion of B and T cells from PP out of the mucosa and into
sheep erythrocytes. The same study showed a lack of the blood circulation, re-entering the intestine via high
response to this antigen in vivo, perhaps an indication of endothelial venules in IFA and residing finally in the la-
the compartmentalization of the various cell types essen- mina propria (LP) as fully differentiated cells [13, 104]. In
tial in the induction of an immune response in PP. In con- a recent study, Bowman et al. [105] showed that thymus
trast to these results, Kagnoff and Campbell [99] showed expressed chemokine (TECK), CCL25 is a potent and
that suspensions of cells from mouse PP did not give rise selective chemo-attractant for IgA antibody secreting
to specific antibody-forming cells when mixed with heter- cells, efficiently recruiting IgA producing cells from
ologous red blood cells. When peritoneal macrophages spleen, PP and MLN which may help target IgA produc-
were added to the cell suspension, antibody-forming cells ing cells to the gut wall, thus helping to define and segre-
appeared. Kagnoff and Campbell [99] suggested that the gate the intestinal immune response. Extra-vascular re-
62 Pathobiology 2002–03;70:55–68 Makala/Suzuki/Nagasawa
cruitment of immune and inflammatory cells is controlled cluded from these results that the lightly labelled cells
by dynamically regulated complementary adhesion mole- were derived from the thymus. These results suggest that
cules and chemokines expressed on the surface of circulat- the IFA is a T cell area.
ing leucocytes and on the endothelium of venules. Such The structural architecture of the patch was further
molecules regulate the trafficking (recirculation) of naı̈ve defined by studies analysing migration of injected cells to
lymphocytes through organized lymphoid tissue and par- different patch tissues, for example the IFA was clearly
ticularly the homing of primed B and T cells to immuno- defined as a T-dependent area [27, 117]. It has been
logical effector sites, such as the mucosae, as well as the shown in the mouse that labelled thymocytes migrate to
extravasation of different leucocytes in inflammation the T-dependent IFA of PP [117–120]. A similar distribu-
[106, 107]. Experimental data has shown that certain lym- tion of thymus-derived cells was observed when calf thy-
phoid adhesion molecules are more strongly expressed by mus cells were labelled in vivo by injecting 3H-thymidine
unprimed (naı̈ve) than primed (memory) lymphocytes. It directly into the thymus [27]. Experiments in mice [89]
is well documented that the adhesion molecule (MAD- and rabbits [121] have shown that most cells in the IFA of
CAM-1) is shared between PP and the LP and also shows PP have thymic antigens on their surface. Calkins et al.
considerable expression on HEV in the mesenteric lymph [95] used cells from the IFA of the rabbit appendix and
nodes [108]. The molecular mechanisms directing the showed that many of the cells responded to the T cell
integrated dissemination of immune cells from the gut mitogen, PHA, while few were sIg+, again supporting the
associated lymphoid tissues to exocrine sites beyond the view that the IFA is a T cell compartment. There is cell
gut are poorly defined, although they form the functional traffic within the IFA [reviewed in 89]. Lymphocytes are
basis for several desired oral vaccines [109]. In sheep and thought to migrate from the blood into the tissues of the
cattle the pathway taken by migratory lymphocytes has IFA via post capillary venules [122]. The importance of
been well described [reviewed in 110]. However, McFar- the thymus in the development of the IFA has also been
lin and Binns [111] established that the pig has a unique shown in observations made on lambs thymectomized in
structure of MLN, which enables PP derived lymphocytes utero [123]. The IFA in these animals were small and acel-
in afferent lymph to enter the blood circulation within the lular, correlating with lower rate of migration of cells into
MLN. In all other species examined, the migrating cells the area, because after thymectomy the recirculating pool
leave the MLN in efferent lymph and enter the cysterna contains fewer lymphocytes [124].
chyli, returning the cells to the venous circulation via the With regard to patch follicle, Parrot and Ferguson
thoracic duct. [117] studied the migratory properties of bone marrow
Gowan and Knight [112] first showed that small lym- derived cells obtained from the spleen of mice which had
phocytes obtained from the thoracic duct lymph of rats been thymectomized, lethally irradiated and transfused
and infused intravenously accumulated in PP. This obser- with cells obtained from the bone marrow. On re-injec-
vation has since been extended to show that the migration tion the labelled cells were shown to localise in the medul-
of thoracic duct lymphocytes occurs selectively to differ- la of the follicles of the PP. Bone marrow-derived cells
ent regions of the PP [113]. Thus, blast cells obtained obtained from the thoracic duct lymph of rats, localize in
from the thoracic duct lymph of rats localised in the LP of a similar way following their injection intravenously
villi between follicles of the patch and occasionally in the [116], as none marrow-derived cells in the rabbit do [125].
IFA of PP. They never accumulate in the lymphoid folli- However, in the rabbit these cells accumulated in the cor-
cles [114]. Similar data were obtained in rabbit by Perey ona of the follicles in the appendix [125]. Calkins et al.
and Milne [115]. Howard et al. [116] made similar obser- [95] teased cells from the corona and the dome region of
vations in the rat. They showed that lightly labelled cells the follicles of the rabbit appendix and showed that they
accumulated in a band around the medulla, especially were IgA+ and IgM+. Studies have shown that the medul-
towards the mucosa in the region equivalent to the dome lary zone of PP follicles contain small lymphocytes, blast
and corona in rabbits. In addition, cells from the thoracic cells and plasma cells [28] suggesting that the follicle con-
duct lymph of rats, which had been thymectomized, tains both B and T cells.
lethally irradiated and reconstituted with bone marrow Little is known about the movement of cells between
had similar migratory properties to those of the lightly the different regions of the follicle. During development,
labelled cells in the thoracic duct lymph of normal rats. the dome region expands to form the follicle [2] and
Few heavily labelled cells were located in IFA of PP when experiments on regeneration of the rabbit appendix after
injected cells were from thymectomized rats. They con- X-irradiation have also been interpreted to indicate that
Peyer’s Patches: Organized Lymphoid Pathobiology 2002–03;70:55–68 63
Structures
cells migrate from the dome to the follicle [126]. From did not develop normal oral tolerance to protein antigens.
observations on the structure of the rabbit PP and appen- However, in a recent study, Yamamoto and colleagues
dix follicle, Waksman et al. [27] have suggested that cells [135] showed that PP are not a strict requirement for
entering the follicle from the dome are induced to prolif- induction of mucosal IgA antibody responses in the gas-
erate once they arrive there. trointestinal tract, suggesting an alternative mucosal im-
mune system. By immunohistochemistry, the authors
showed that PP-null mice possessed significant numbers
Peyer’s Patches as a Source of IgA Precursor of IgA+ plasma cells in the LP and that oral immunization
Cells of the PP null mice with OVA plus cholera toxin as a
mucosal adjuvant resulted in antigen specific mucosal IgA
In a previous section, evidence has been presented and serum IgG antibody responses.
which shows that IgA plasma cells in the intestine origi-
nate from IgA blast cells present in lymph draining from
the intestine. There is evidence to suggest that many of Role of Peyer’s Patch Cells in Immunoglobulin
these cells are produced in PP [127, 128]. It is generally Isotype Regulation
accepted that, after antigenic stimulation in the PP, IgA+
lymphoblasts (B220+IgA+) migrate through the lymph There is still a controversy regarding the role of antigen
and blood circulation, and eventually home to the LP of in initiating these events [136]. However, as IgA plasma
the intestine. Craig and Cebra [91] transferred cells ob- cells are much reduced in the gut of germ free animals
tained from different lymphoid organs into allogeneic [137], it seems likely that intestinal antigens are necessary
rabbits, which had been lethally irradiated. The cells of to induce precursor cells in PP to differentiate into IgA
donor origin had an allotypic marker (B4) on the light plasma cells. Schaffner et al. [138, 139] have suggested
chain of the sIg, which could be detected by immunofluo- that in birds the bursa of Fabricius may be the major site
rescence techniques. These experiments showed that cells where contact occurs between lymphoid cells and the anti-
obtained from the popliteal lymph nodes mostly gave rise gens in the lumen of the intestine. As cells migrate from
to IgG specific plasma cells in the spleen, but cells from the bursa at an early stage of differentiation this would
PP repopulated the LP of the intestine with IgA plasma account for the observation that cells in the bursa produce
cells. This observation has since been confirmed in exper- little detectable antibody [138, 139]. Evidence presented
iments in which rabbits were given autologous PP cells in previous sections suggests that the same situation may
intravenously [129]. Cells obtained from rabbit PP have hold true for PP. The main difference between the bursa
also been shown to migrate to the mucosa of the respirato- and PP seems to be that while the bursa is the source of B
ry tract and differentiate into IgA plasma cells. The respi- cells, which develop into plasma cells specific for each
ratory tract contains lymphoid follicles, termed BALT class of Ig [reviewed in 138, 139], the cells from PP are
with many similar characteristics to PP [130, 131]. Rud- precursors predominantly of the IgA-specific plasma cells
zik et al. [129] have shown that cells from these areas also [91, 104].
have the ability to repopulate the LP of the gut and respi- The role of T cells in immunoglobulin isotype regula-
ratory tract when injected intravenously. The migration tion is still unclear. Since the time it was recognised that T
of cells from the organised lymphoid tissue of one muco- cells play a role in B cell isotype differentiation [140, 141],
sal surface to other mucosal surfaces in the body may be identification of the site of T cell action within the B cell
an important mechanism for disseminating immune re- differentiation pathway has been the goal of research in
sponsiveness or nonresponsiveness (tolerance) and forms many laboratories. Kawanishi et al. [142] established that
the basis for the common mucosal immune system [86, T cell clones derived from PP, but not from spleen func-
130–134]. Tolerance represents the most common and tion as class specific switch cells, which induce B cell dif-
important response of the host to environmental antigens, ferentiation to sIgA+ B cells. Evidence that T cells regulate
including food and comensal bacterial components, for isotype differentiation at the level of naı̈ve murine B cells
the maintenance of an appropriate immunological ho- comes from several sources. Kawanishi et al. [143, 144]
meostasis. In order to examine whether PP could play an demonstrated that sIgM+sIgA – B cells could be induced to
important role for the maintenance of oral tolerance, Fuji- switch sIgA+ B cells in the presence of T cell clones
hashi and co-workers [15, 16] found that PP-null mice derived from GALT. These sIgA+ B cells could then be
retained their capability to produce sIgA antibodies but induced to secrete IgA in the presence of additional exoge-
64 Pathobiology 2002–03;70:55–68 Makala/Suzuki/Nagasawa
nous lymphokine [142]. Isakson et al. [145] showed that uncommitted sIgM+sIgG – B cells as well as IgA, thus
murine sIgM+sIgG – B cells could be induced to secrete bringing about both switch and expansion of sIgA+ B cells.
IgG1 rather than IgG3 when stimulated by LPS in the In the IgE system. Ishizaka [153] and Nutman et al. [154]
presence of the T cell derived factor IL-4 [146]. In the detected T cell factors with Ig-binding properties that
human, Mayer et al. [147] demonstrated that sIgM+sIgG – selectively enhanced the differentiation of sIgE+ B cells.
B cells could be induced to differentiate into IgG and IgA Recently, Gardby and Lycke et al. [155] in a series of ex
secreting B cells in the presence of T cells derived from a vivo experiments revealed that CD19-deficient mice ex-
patient with Sezary syndrome. In a recent study, Fagaras- hibited poor responsiveness to oral immunization despite
an et al. [127, 128] showed that culturing LP and PP IgM+ evidence of unaltered total IgA level, germinal centres and
B cells together with stromal cells enhances preferential IgA-isotype switching in PP, thus providing compelling
switching and differentiation of B cells to IgA+ plasma evidence for the differential regulation of serum and
cells, suggesting that IgA+ cells in the gut are generated in mucosal IgA immunity. Taken together, the evidence
situ from B220+IgM+ lymphocytes. These reports suggest from all the cited data suggests that T cells can act on B
that switch and expansion of isotype-committed B cells cells to cause both switch of uncommitted B cells as well
are regulated by separate T cell populations. as differential expansion of isotype-committed B cells and
There is compelling evidence that T cells act during that the PP provides a structural environment which per-
isotype differentiation by preferentially expanding a pre- mits the productive interactions between T cell subsets
committed B cell pool. Kiyono et al. [148, 149] and Mayer and sIg+ B cells to take place.
et al. [150, 151] found that murine antigen-specific T cell
clones derive from PP specifically expanded sIgA+ B cells
but not sIgA – B cells via an IgA-binding factor. Benson Acknowledgements
and Strobber [152] addressed the question of T cell regu-
We are indebted to the Japanese Society for the Promotion of
lation of B cell isotype differentiation by using a non-neo-
Science (JSPS) for financial support. The first author is supported by
plastic human tissue source. T cell clones were generated a research fellowship from JSPS for young scientists. This work was
from lymphoid follicles in normal appendiceal tissue. It also supported by grants from the Ministry of Education, Science,
was established that individual T cell clones could act on Sports and Culture.
References
1 Peyer JC (1677): Exercitatio ant. De glandulis 9 Glick B, Chang TW, Jaap RG: The bursa of 15 Fujihashi K, Dohi T, Rennert PD, Yamamoto
intestinarum earumque usu et affectionibus. Fabricius and antibody production. Poultry Sci M, Koga T, Kiyono H, McGhee JR: Peyer’s
Schaffausen; in Garrison FH (ed): An Introduc- 1956;35:224–229. patches are required for oral tolerance to pro-
tion to the History of Medicine, ed 4. Philadel- 10 Warner NL, Szenberg A, Burnet AJ: The im- teins. Proc Natl Acad Sci USA 2001;98:3310–
phia, Saunders, 1929, p 264. munological role different lymphoid organs in 3315.
2 Hummel KP: The structure and development the chicken. I. Dissociation of immunological 16 Fujihashi K, Kato H, van Ginkel FW, Koga T,
of the lymphatic tissues in the intestine of the responsiveness. Aust J Exp Med 1962;40:373– Boyaka PN, Jackson RJ, Kato R, Hagiwara Y,
albino rat. Am J Anat 1965;57:351–364. 378. Etani Y, Goma I, Fujihashi K, Kiyono H,
3 Brucke E: Denkschr. Kaiserl. Acad. Wissen., 11 Cooper MD, Lawton AR: The mammalian McGhee JR: A revisit of mucosal IgA immuni-
Math-Naturw. Classe 1851;2:21–26. bursa equivalent: Does lymphoid differentia- ty and oral tolerance. Acta Odontol Scand
4 Flemming W: Arch Mikr Anat 1885;24:50–51. tion along cell lines begin in the gut-associated 2001;59:301–308.
5 Carlens O: Studien über Lymphatische Gewe- lymphoepithelial tissues (GALT) of mammals? 17 Doughri AB, Altera KP, Kainer RA: Some
be des Darms. Z Anat Entwicklungsgesch 1928; Contemp Topics Immunobiol 1973;1:49–56. developmental aspects of the bovine fetal gut.
86:393–394. 12 Owen JJ, Wright DE, Habu S, Raff MC, Coo- Zentralbl Vet Med A 1972;19:417–427.
6 Griebel PJ, Hein WR: Expanding the role of per MD: Studies on the generation of B lym- 18 Pabst R, Geist M, Rothkotter HJ, Fritz FJ:
Peyer’s patches in B-cell ontogeny. Immunol phocytes in fetal liver and bone marrow. J Postnatal development and lymphocyte pro-
Today 1996;17:30–39. Immunol 1977;118:2067–2072. duction of jejunal and ileal Peyer’s patches in
7 Neutra MR, Mantis NJ, Kraehenbuhl JP: Col- 13 Craig SW, Cebra JJ: Peyer’s patches: An en- normal and gnotobiotic pigs. Immunology
laboration of epithelial cells with organized riched source of precursors for IgA-producing 1988;64:539–544.
mucosal lymphoid tissues. Nat Immunol 2001; immunocytes in the rabbit. J Exp Med 1971; 19 Makala LHC: Isolation and characterization of
2:1004–1009. 134:188–200. pig Peyer’s patch dendritic cells; PhD thesis,
8 Kraehenbuhl JP, Neutra MR: Epithelial M 14 Silvey KJ, Hutchings AB, Vajdy M, Petzke Bristol, 1996.
cells: Differentiation and function. Annu Rev MM, Neutra MR: Role of immunoglobulin A
Cell Dev Biol 2000;16:301–332. in protection against reovirus entry into mu-
rine Peyer’s patches. J Virol 2001;75:10870–
10879.
Peyer’s Patches: Organized Lymphoid Pathobiology 2002–03;70:55–68 65
Structures
20 Makala LHC, Kamada T, Nishikawa Y, Naga- 36 Ermak TH, Steger HJ, Pappo J: Phenotypically 51 Owen RL: Sequential uptake of horseradish
sawa H, Igarashi I, Fujisaki K, Suzuki N, Mi- distinct subpopulations of T cells in domes and peroxidase by lymphoid follicle epithelium of
kami T, Haverson K, Bailey M, Stokes CR, M-cell pockets of rabbit gut-associated lym- Peyer’s patches in the normal unobstructed
Bland PW: Ontogeny of pig discrete Peyer’s phoid tissues. Immunology 1990;71:530–537. mouse intestine: An ultrastructural study. Gas-
patches: Distribution and morphometric anal- 37 Bjerke K, Brandtzaeg P, Fausa O: T cell distri- troenterology 1977;72:440–451.
ysis. Pathobiology 2000;68:275–282. bution is different in follicle-associated epithe- 52 Jones BD, Ghori N, Falkow S: Salmonella
21 Perey DY, Cooper MD, Good RA: The mam- lium of human Peyer’s patches and villous epi- typhimurium initiates murine infection by pen-
malian homologue of the avian bursa of Fabri- thelium. Clin Exp Immunol 1988;74:270–275. etrating and destroying the specialized epithe-
cius. I. Neonatal extirpation of Peyer’s patch- 38 Gebert A, Rothkotter HJ, Pabst R: M cells in lial M cells of the Peyer’s patches. J Exp Med
type lymphoepithelial tissues in rabbits: Meth- Peyer’s patches of the intestine. Int Rev Cytol 1994;180:15–23.
ods and inhibition of development of humoral 1996;167:91–159. 53 Owen RL, Pierce NF, Apple RT, Cray WC Jr:
immunity. Surgery 1968;64:614–621. 39 Gebert A, Hach G: Differential binding of lec- M cell transport of Vibrio cholerae from the
22 Cornes JS: Peyer’s patches in the human gut. tins to M cells and enterocytes in the rabbit intestinal lumen into Peyer’s patches: A mecha-
Proc R Soc Med 1965;58:716–730. cecum. Gastroenterology 1993;105:1350– nism for antigen sampling and for microbial
23 Binns RM, Licence ST: Patterns of migration 1361. transepithelial migration. J Infect Dis
of labeled blood lymphocyte subpopulations: 40 Gebert A, Hach G, Bartels H: Co-localization 1986b;153:1108–1118.
Evidence for two types of Peyer’s patches in the of vimentin and cytokeratins in M-cells of rab- 54 Farstad IN, Halstensen TS, Fausa O, Brandt-
young pigs. Adv Exp Med Biol 1985;186:661– bit gut-associated lymphoid tissue (GALT). zaeg P: Heterogeneity of M-cell-associated B
668. Cell Tissue Res 1992;269:331–340. and T cells in human Peyer’s patches. Immu-
24 Reynolds JD: Evidence of differences between 41 Gebhard A, Gebert A: Brush cells of the mouse nology 1994;83:457–464.
Peyer’s patches and germinal centres. Adv Exp intestine possess a specialized glycocalyx as 55 Yamanaka T, Straumfors A, Morton H, Fausa
Med Biol 1985;186:111–118. revealed by quantitative lectin histochemistry: O, Brandtzaeg P, Farstad I: M cell pockets of
25 Reynolds JD, Pabst R, Bordman G: Evidence Further evidence for a sensory function. J His- human Peyer’s patches are specialized exten-
for the existence of two distinct types of Peyer’s tochem Cytochem 1999;47:799–808. sions of germinal centers. Eur J Immunol 2001;
patches in sheep. Adv Exp Med Biol 1985;186: 42 Clark MA, Jepson MA, Simmons NL, Booth 31:107–117.
101–109. TA, Hirst BH: Differential expression of lectin- 56 Kerneis S, Bogdanova A, Kraehenbuhl JP,
26 Reynolds JD: The development and physiology binding sites defines mouse intestinal M-cells. J Pringault E: Conversion by Peyer’s patch lym-
of the gut associated lymphoid systems in Histochem Cytochem 1993;41:1679–1687. phocytes of human enterocytes into M cells
lambs; PhD thesis, John Curtis School of Medi- 43 Gebert A, Rothkotter HJ, Pabst R: Cytokeratin that transport bacteria. Science 1997;277:949–
cal Research, Australian National University, 18 is an M-cell marker in porcine Peyer’s 952.
Canberra, 1976. patches. Cell Tissue Res 1994;276:213–221. 57 Kerneis S, Caliot E, Stubbe H, Bogdanova A,
27 Sobhon P: The light and electron microscopic 44 Owen RL, Nemanic P: Antigen processing Kraehenbuhl J, Pringault E: Molecular studies
studies of Peyer’s patches in non-germ free structures of the mammalian intestinal tract: of the intestinal mucosal barrier physiopatho-
adult mice. J Morphol 1971;135:457–481. An SEM study of lymphoepithelial organs; in logy using cocultures of epithelial and immune
28 Faulk WP, McCormic JN, Goodman JR, Yof- Scanning Electron Microscopy. AMFO Hare, cells: A technical update. Microbes Infect 2000;
frey JM, Fudenberg HH: Peyer’s patches: Mor- SEM, 1978, vol II. 2:1119–1124.
phologic studies. Cell Immunol 1971;1:500– 45 Nagura H, Ohtani H, Masuda T, Kimura M, 58 Pollard M, Sharon N: Responses of the Peyer’s
520. Nakamura S: HLA-DR expression on M cells patches in germ free mice to antigenic stimula-
29 Waksman BH, Ozer H, Blythman HE: Appen- overlying Peyer’s patches is a common feature tion. Infect Immun 1970;2:96–106.
dix and gamma M antibody formation. VI. The of human small intestine. Acta Pathol Jpn 59 Joel DD, Laissue JA, LeFevre ME: Distribu-
functional anatomy of the rabbit appendix. Lab 1991;41:818–823. tion and fate of ingested carbon particles in
Invest 1973;28:614–626. 46 Allan CH, Mendrick DL, Trier JS: Rat intesti- mice. J Reticuloendothel Soc 1978;24:477–
30 Pabst R: The anatomical basis for the immune nal M cells contain acidic endosomal-lysosom- 487.
function of the gut. Anat Embryol 1987;176: al compartments and express class II major his- 60 Chapman HA, Johnson JS, Cooper MD: On-
135–144. tocompatibility complex determinants. Gas- togeny of Peyer’s patches and immunoglobu-
31 Ponomarova TV: Lymphoid apparatus of rab- troenterology 1993;104:698–708. lin-containing cells in pigs. J Immunol 1974;
bit intestine under normal conditions and after 47 Onori P, Franchitto A, Sferra R, Vetuschi A, 112:555–563.
artificial sensitization. Ark Anat Gistol Em- Gaudio E: Peyer’s patches epithelium in the 61 Cole GJ, Morris B: The lymphoid apparatus of
briol 1963;48:55–63. rat: A morphological, immunohistochemical, the sheep: Its growth, development and signifi-
32 Makala LHC, Haverson K, Stokes CR, Bailey and morphometrical study. Dig Dis Sci 2001; cance in immunologic reactions. Adv Vet Sci
M, Bland PW: Isolation and characterization of 46:1095–1104. Comp Med 1973;17:225–263.
pig Peyer’s patch dendritic cells. Vet Immunol 48 Bockman DE, Cooper MD: Pinocytosis by epi- 62 Ferguson A, Parrott DM: The effect of antigen
Immunopathol 1998;61:67–81. thelium associated with lymphoid follicles in deprivation on thymus-dependent and thymus-
33 Makala LH, Kamada T, Nagasawa H, Igarashi the bursa of Fabricius, appendix, and Peyer’s independent lymphocytes in the small intestine
I, Fujisaki K, Suzuki N, Mikami T, Haverson patches: An electron microscopic study. Am J of the mouse. Clin Exp Immunol 1972;12:477–
K, Bailey M, Stokes CR, Bland PW: Ontogeny Anat 1973;136:455–477. 488.
of pig discrete Peyer’s patches: Expression of 49 Walker WA, Isselbacher KJ: Uptake and trans- 63 Sminia T, Janse EM, Plesch BEC: Ontogeny of
surface antigens. J Vet Med Sci 2001;63:625– port of macromolecules by the intestine. Possi- Peyer’s patches of the rat. Anat Rec 1983;207:
636. ble role in clinical disorders. Gastroenterology 309–316.
34 Jarry A, Robaszkiewicz M, Brousse N, Potet F: 1974;67:531–550. 64 Finke D, Kraehenbuhl JP: Formation of
Immune cells associated with M cells in the fol- 50 Owen RL, Apple RT, Bhalla DK: Morphomet- Peyer’s patches. Curr Opin Genet Dev 2001;
licle-associated epithelium of Peyer’s patches ric and cytochemical analysis of lysosomes in 11:561–567.
in the rat: An electron- and immuno-electron- rat Peyer’s patch follicle epithelium. Their re- 65 Bhide SA, Wadekar KV, Koushik SA: Peyer’s
microscopic study. Cell Tissue Res 1989;255: duction in volume fraction and acid phospha- patches are precocious to the appendix in hu-
293–298. tase content in M cells compared to adjacent man development. Dev Immunol 2001;8:159–
35 Ermak TH, Owen RL: Differential distribution enterocytes. Anat Rec 1986;216:521–527. 166.
of lymphocytes and accessory cells in mouse 66 Brandtzaeg P: The human intestinal immune
Peyer’s patches. Anat Rec 1986;215:144–152. system: Basic cellular and humoral mechanisms.
Baillières Clin Rheumatol 1996;10:1–24.
66 Pathobiology 2002–03;70:55–68 Makala/Suzuki/Nagasawa
67 Brandtzaeg P, Farstad IN, Haraldsen G, Jahn- 85 Owen RL, Allen CL, Stevens DP: Phagocytosis 99 Kagnoff MF, Campbell S: Functional charac-
sen FL: Cellular and molecular mechanisms for of Giardia muris by macrophages in Peyer’s teristics of Peyer’s patch lymphoid cells. I.
induction of mucosal immunity. Dev Biol patch epithelium in mice. Infect Immun 1981; Induction of humoral antibody and cell-me-
Stand 1998;92:93–108. 33:591–601. diated allograft reactions. J Exp Med 1974;
68 Brandtzaeg P, Baekkevold ES, Morton HC: 86 Tsuji NM, Mizumachi K, Kurisaki J: Interleu- 139:398–406.
From B to A the mucosal way. Nat Immunol kin-10-secreting Peyer’s patch cells are respon- 100 Mayrhofer G, Holt PG, Papadimitriou JM:
2001;2:1093–1104. sible for active suppression in low-dose oral tol- Functional characteristics of the veiled cells
69 Brandtzaeg P, Bjerke K, Kett K, Kvale D, Rog- erance. Immunology 2001;103:458–464. in afferent lymph from the rat intestine. Im-
num TO, Scott H, Sollid LM, Valnes K: Pro- 87 MacDonald TT, Monteleone G: IL-12 and Th1 munology 1986;58:379–387.
duction and secretion of immunoglobulins in immune responses in human Peyer’s patches. 101 Kelsall BL, Strober W: The role of dendritic
the gastrointestinal tract. Ann Allergy 1987;59: Trends Immunol 2001;22:244–247. cells in antigen processing in the Peyer’s
21–39. 88 Maeda Y, Noda S, Tanaka K, Sawamura S, patch. Ann NY Acad Sci 1996;778:47–54.
70 Brandtzaeg P: Molecular and cellular aspects of Aiba Y, Ishikawa H, Hasegawa H, Kawabe N, 102 Kelsall BL, Strober W: Distinct populations
the secretory immunoglobulin system. APMIS Miyasaka M, Koga Y: The failure of oral toler- of dendritic cells are present in the subepithe-
1995;103:1–19. ance induction is functionally coupled to the lial dome and T cell regions of the murine
71 Brandtzaeg P, Bjerke K: Human Peyer’s absence of T cells in Peyer’s patches under Peyer’s patch. J Exp Med 1996;183:237–247.
patches: Lympho-epithelial relationships and germfree conditions. Immunobiology 2001; 103 Moore MA, Owen JJ: Experimental studies
characteristics of immunoglobulin-producing 204:442–457. on the development of the bursa of Fabricius.
cells. Immunol Invest 1989;18:29–45. 89 Weissman IL: Development and distribution Dev Biol 1966;14:40–51.
72 Brandtzaeg P: Two types of IgA immunocytes of immunoglobulin-bearing cells in mice. 104 Husband AJ, Kramer DR, Bao S, Sutherland
in man. Nat New Biol 1973;243:142–153. Transplant Rev 1975;24:159–176. RM, Beagley KW: Regulation of mucosal IgA
73 Brandtzaeg P: Presence of J chain in human 90 Levin DM, Rosenstreich DL, Reynolds HY: responses in vivo: Cytokines and adjuvants.
immunocytes containing various immunoglob- Immunologic responses in the gastrointestinal Vet Immunol Immunopathol 1996;54:179–
ulin classes. Nature 1974;252:418–420. tract of the guinea pig. I. Characterization of 186.
74 Brandtzaeg P: Mucosal and glandular distribu- Peyer’s patch cells. J Immunol 1973;111:980– 105 Bowman EP, Kuklin NA, Youngman KR, La-
tions of immunoglobulin components: Differ- 983. zarus NH, Kunkel EJ, Pan J, Greenberg HB,
ential localization of free and bound SC in 91 Craig SW, Cebra JJ: Rabbit Peyer’s patches, Butcher EC: The intestinal chemokine thy-
secretory epithelial cells. J Immunol 1974;112: appendix and popliteal lymph node B lympho- mus-expressed chemokine (CCL25) attracts
1553–1559. cytes: A comparative analysis of their mem- IgA antibody-secreting cells. J Exp Med 2002;
75 Brandtzaeg P, Krajci P, Lamm ME, Kaetzel brane immunoglobulin components and plas- 195:269–275.
CS: Epithelial and hepatobiliary transport of ma cell precursor potential. J Immunol 1975; 106 Springer TA: Traffic signals for lymphocyte
polymeric immunoglobulins; in Ogra PL, Mes- 114:492–502. recirculation and leukocyte emigration: the
tecky L, Lamm ME, Strober W, McGhee JR, 92 Friedberg SH, Weissman IL: Lymphoid tissue multistep paradigm. Cell 1994;76:301–314.
Bienenstock J (eds): Handbook of Mucosal Im- architecture. II. Ontogeny of peripheral T and 107 Butcher EC, Picker LJ: Lymphocyte homing
munology. Orlando, Academic Press, 1994, B cells in mice: Evidence against Peyer’s and homeostasis. Science 1996;272:60–66.
pp 113–126. patches as the site of generation of B cells. J 108 Briskin MJ, McEvoy LM, Butcher EC: MAd-
76 Brandtzaeg P, Prydz H: Direct evidence for an Immunol 1974;113:1477–1492. CAM-1 has homology to immunoglobulin
integrated function of J chain and secretory 93 Perey DY, Guttmann RD: Peyer’s patch cells. and mucin-like adhesion receptors and to
component in epithelial transport of immuno- Absence of graft-versus-host reactivity in mice IgA1. Nature 1993;363:461–464.
globulins. Nature 1984;311:71–73. and rats. Lab Invest 1972;27:427–433. 109 Mestecky J, Abraham R, Ogra PL: Common
77 Brandtzaeg P: Role of J chain and secretory 94 Levin DM, Rosenstreich DL, Wahl SM, Rey- mucosal immune system and strategies for
component in receptor-mediated glandular and nolds HY: Peyer’s patch lymphocytes: Demon- the development of vaccines effctive at muco-
hepatic transport of immunoglobulins in man. stration of the integrity of afferent and efferent sal surfaces; in Ogra PL, Mestecky J, Lamm
Scand J Immunol 1985;22:111–146. T-cell functions in the guinea pig and rat. J ME, Strober W, McGhee JR, Bienenstock J
78 Bryant BJ, Shifrine M: Histogenesis of lymph- Immunol 1974;113:1935–1941. (eds): Handbook of Mucosal Immunology.
nodes during development of the dog. J Reticu- 95 Calkins CE, Ozer H, Waksman BH: B cells in Orlando, Academic Press, 1994, pp 357–372.
loendothel Soc 1972;12:96–107. the appendix and other lymphoid organs of the 110 Morris B, Courtice FC: Cells and immuno-
79 Thorbecke GJ: Some histological and function- rabbit: Stimulation of DNA synthesis by anti- globulins in lymph. Lymphology 1977;10:62–
al aspects of lymphoid tissue in germ free ani- immunoglobulin. Cell Immunol 1975;18:187– 70.
mals. I. Morphological studies. Ann NY Acad 198. 111 McFarlin DE, Binns RM: Lymph node func-
Sci 1959;78:237–241. 96 Rell KW, Lamprecht J, Sicinski P, Bem W, tion and lymphocyte circulation in the pig.
80 Krumml J, Ludvick J, Trebichevsky I, Mandel Rowinski J: Frequency of occurrence and dis- Adv Exp Med Biol 1973;29:87–93.
L, Korvac F: Morphology of germfree piglets. tribution of the intra-epithelial lymphoid cells 112 Gowan JL, Knight EJ: The route of recircula-
Folio Microbiol Praha 1969;24:441–444. in the follicle-associated epithelium in pheno- tion in the rat. Proc R Soc 1964;159:257–
81 Pollard M: Immunologic activation of Peyer’s typically normal and athymic nude mice. J 259.
patches in germ-free mice. Fed Proc 1970;29: Anat 1987;152:121–131. 113 Hall JG, Smith ME: Homing of lymph-borne
811–816. 97 Andersen JK, Takamatsu H, Oura CA, Brookes immunoblasts to the gut. Nature 1970;226:
82 Stramignoni A, Mollo F, Rua S, Palestro G: SM, Pullen L, Parkhouse RE: Systematic char- 262–263.
Development of the lymphoid tissue in the rab- acterization of porcine ileal Peyer’s patch. I. 114 Hall JG, Parry DM, Smith ME: The distribu-
bit appendix isolated from the intestinal tract. J Apoptosis-sensitive immature B cells are the tion and differentiation of lymph-borne im-
Pathol 1969;99:265–269. predominant cell type. Immunology 1999;98: munoblasts after intravenous injection into
83 Perey DY, Good RA: Experimental arrest and 612–621. syngeneic recipients. Cell Tissue Kinet 1972;
induction of lymphoid development in intesti- 98 Henry C, Faulk WP, Kuhn L, Yoffey JM, 5:269–281.
nal lymphoepithelial tissues of rabbits. Lab In- Fudenberg HH: Peyer’s patches: Immunologic 115 Perey DY, Milne RW: Rabbit gut-associated
vest 1968;18:15–26. studies. J Exp Med 1970;131:1200–1210. lymphoid tissue: Major pathway for thoracic
84 Bienenstock J, Befus AD: Mucosal immunolo- duct lymphocyte circulation. Lab Invest
gy. Immunology 1980;41:249–270. 1975;33:678–686.
Peyer’s Patches: Organized Lymphoid Pathobiology 2002–03;70:55–68 67
Structures
116 Howard JC, Hunt SV, Gowans JL: Identifica- 130 Bienenstock J, Johnston N, Perey DY: Bron- 144 Kawanishi H, Saltzman L, Strober W: Mech-
tion of marrow-derived and thymus-derived chial lymphoid tissue. I. Morphologic charac- anisms regulating IgA class-specific immuno-
small lymphocytes in the lymphoid tissue and teristics. Lab Invest 1973;28:686–692. globulin production in murine gut-associated
thoracic duct lymph of normal rats. J Exp 131 Bienenstock J, Johnston N, Perey DY: Bron- lymphoid tissues. II. Terminal differentiation
Med 1972;135:200–219. chial lymphoid tissue. II. Functional charac- of postswitch sIgA-bearing Peyer’s patch B
117 Parrot DMV, Fergusson A: Migration of lym- teristics. Lab Invest 1973;28:693–698. cells. J Exp Med 1983;158:649–669.
phocytes within the mouse small intestine. 132 Challacombe SJ, Tomasi TB: Systemic toler- 145 Isakson PC, Pure E, Vitetta ES, Krammer
Immunology 1974;26:571–576. ance and secretory immunity after oral im- PH: T cell-derived B cell differentiation fac-
118 Joel DD, Hess MW, Cottier H: Magnitude munization. J Exp Med 1980;152:1459– tor(s). Effect on the isotype switch of murine
and pattern of thymic lymphocyte migration 1472. B cells. J Exp Med 1982;155:734–748.
in neonatal mice. J Exp Med 1972;135:907– 133 Mowat AM: The role of the gut-associated 146 Vitetta ES, Ohara J, Myers CD, Layton JE,
923. lymphoid tissues in food allergy. Proc 4th Int Krammer PH, Paul WE: Serological, bio-
119 Chanana AD, Joel DD, Schaedeli J, Hess Symp Clinical Nutrition, 1993, p 1. chemical, and functional identity of B cell-
MW, Cottier H: Thymus cell migration: 134 Mowat AM: Oral tolerance and regulation of stimulatory factor 1 and B cell differentiation
3HTdR-labeled and theta-positive cells in pe- immunity to dietary antigens; in Ogra PL, factor for IgG1. J Exp Med 1985;162:1726–
ripheral lymphoid tissues of newborn mice. Mestecky JM, Lamm ME, Strobber W, 1731.
Adv Exp Med Biol 1973;29:79–85. McGhee JR, Bienenstock J (eds): A Hand- 147 Mayer L, Posnett DN, Kunkel HG: Human
120 Chanana AD, Schaedeli J, Hess MW, Cottier book of Mucosal Immunology. San Diego, malignant T cells capable of inducing an im-
H: Predominance of theta-positive lympho- Academic Press, 1994, p 185. munoglobulin class switch. J Exp Med 1985;
cytes in gut-associated and peripheral lym- 135 Yamamoto M, Rennert P, McGhee JR, 161:134–144.
phoid tissues of newborn mice. J Immunol Kweon MN, Yamamoto S, Dohi T, Otake S, 148 Kiyono H, Cooper MD, Kearney JF, Mostell-
1973;110:283–285. Bluethmann H, Fujihashi K, Kiyono H: Al- er LM, Michalek SM, Koopman WJ, McGhee
121 Fujiwara S, Armstrong RM, Cinader B: Thy- ternate mucosal immune system: Organized JR: Isotype specificity of helper T cell clones.
mus dependent area detected by immunoflu- Peyer’s patches are not required for IgA re- Peyer’s patch Th cells preferentially collabo-
orescence I. Development of T-area in young sponses in the gastrointestinal tract. J Immu- rate with mature IgA B cells for IgA re-
rabbits. Jpn J Exp Med 1974;44:359–363. nol 2000;164:5184–5191. sponses. J Exp Med 1984;159:798–811.
122 Schoefl GI: The migration of lymphocytes 136 Jones PP, Craig SW, Cebra JJ, Herzenberg 149 Kiyono H, Mosteller-Barnum LM, Pitts AM,
across the vascular endothelium in lymphoid LA: Restriction of gene expression in B lym- Williamson SI, Michalek SM, McGhee JR:
tissue: A reexamination. J Exp Med 1972; phocytes and their progeny. II. Commitment Isotype-specific immunoregulation: IgA-
136:568–588. to immunoglobulin heavy chain isotype. J binding factors produced by Fc alpha recep-
123 Cole GJ, Morris B: The growth and develop- Exp Med 1974;140:452–469. tor-positive T cell hybridomas regulate IgA
ment of lambs thymectomized in utero. Aust 137 Crabbe PA, Bazin H, Eyssen H, Heremans responses. J Exp Med 1985;161:731–747.
J Exp Med Sci 1971;49:33–53. JF: The normal microbial flora as a major 150 Mayer L, Fu SM, Kunkel HG: Human T cell
124 Pearson LD, Simpson-Morgan MW, Morris stimulus for proliferation of plasma cells syn- hybridomas secreting factors for IgA-specific
B: Lymphopoiesis and lymphocyte recircula- thesizing IgA in the gut: The germ-free intesti- help, polyclonal B cell activation, and B cell
tion in the sheep fetus. J Exp Med 1976;143: nal tract. Int Arch Allergy Appl Immunol proliferation. J Exp Med 1982;156:1860–
167–186. 1968;34:362–375. 1865.
125 Durkin HG, Caporale L, Thorbecke GJ: Mi- 138 Schaffner T, Hess MW, Cottier H: A rapprais- 151 Mayer L, Fu SM, Kunkel HG: Regulation of
gratory patterns of B lymphocytes. I. Fate of al of bursal functions. Ser Haematol 1974;7: B cell activation and differentiation with fac-
cells from central and peripheral lymphoid 568–592. tors generated by human T cell hybridomas.
organs in the rabbit and its selective altera- 139 Schaffner T, Mueller J, Hess MW, Cottier H, Immunol Rev 1984;78:119–135.
tion by anti-immunoglobulin. Cell Immunol Sordat B, Ropke C: The bursa of Fabricius: A 152 Benson EB, Strober W: Regulation of IgA
1975;16:285–300. central organ providing for contact between secretion by T cell clones derived from the
126 Blythman HE, Waksman BH: Effect of irra- the lymphoid system and intestinal content. human gastrointestinal tract. J Immunol
diation and appendicostomy on appendix Cell Immunol 1974;13:304–312. 1988;140:1874–1882.
structure and responses of appendix cells to 140 Elson CO, Heck JA, Strober W: T-cell regula- 153 Ishizaka K: Isotope-specific T cell factors for
mitogens. J Immunol 1973;111:171–182. tion of murine IgA synthesis. J Exp Med the IgE response. Crit Rev Immunol 1985;5:
127 Fagarasan S, Kinoshita K, Muramatsu M, 1979;149:632–643. 229–262.
Ikuta K, Honjo T: In situ class switching and 141 Mongini PK, Stein KE, Paul WE: T cell regu- 154 Nutman TB, Volkman DJ, Hussain R, Fauci
differentiation to IgA-producing cells in the lation of IgG subclass antibody production in AS, Ottesen EA: Filarial parasite-specific T
gut lamina propria. Nature 2001;413:639– response to T-independent antigens. J Exp cell lines: Induction of IgE synthesis. J Immu-
643. Med 1981;153:1–12. nol 1985;134:1178–1184.
128 Fagarasan S, Shinkura R, Kamata T, Nogaki 142 Kawanishi H, Saltzman LE, Strober W: Char- 155 Gardby E, Lycke NY: CD19-deficient mice
F, Ikuta K, Honjo T: Mechanism of B1 cell acteristics and regulatory function of murine exhibit poor responsiveness to oral immuni-
differentiation and migration in GALT. Curr con A-induced, cloned T cells obtained from zation despite evidence of unaltered total IgA
Top Microbiol Immunol 2000;252:221–229. Peyer’s patches and spleen: Mechanisms reg- levels, germinal centers and IgA-isotype
129 Rudzik R, Clancey RL, Perey DY, Day RP, ulating isotype-specific immunoglobulin pro- switching in Peyer’s patches. Eur J Immunol
Bienenstock J: Repopulation with IgA-con- duction by Peyer’s patch B cells. J Immunol 2000;30:1861–1871.
taining cells of bronchial and intestinal lami- 1982;129:475–483.
na propria after transfer of homologous 143 Kawanishi H, Saltzman LE, Strober W:
Peyer’s patch and bronchial lymphocytes. J Mechanisms regulating IgA class-specific im-
Immunol 1975;114:1599–1604. munoglobulin production in murine gut-asso-
ciated lymphoid tissues. I. T cells derived
from Peyer’s patches that switch sIgM B cells
to sIgA B cells in vitro. J Exp Med 1983;157:
433–450.
68 Pathobiology 2002–03;70:55–68 Makala/Suzuki/Nagasawa
You might also like
- Beating Cancer With Nutrition - Optimal Nutrition Can Improve The Outcome in Medically-Treated Cancer Patients (PDFDrive)Document556 pagesBeating Cancer With Nutrition - Optimal Nutrition Can Improve The Outcome in Medically-Treated Cancer Patients (PDFDrive)Muhammad Mawardi Abdullah100% (13)
- Dodson 1973Document1 pageDodson 1973CoNo ratings yet
- Hox10 and Hox11 Genes Are Required To Globally Pattern The Mammalian SkeletonDocument6 pagesHox10 and Hox11 Genes Are Required To Globally Pattern The Mammalian SkeletongomaNo ratings yet
- Comparing Two Intestinal Porcine Epithelial Cell Lines (Ipecs) : Morphological Differentiation, Function and MetabolismDocument20 pagesComparing Two Intestinal Porcine Epithelial Cell Lines (Ipecs) : Morphological Differentiation, Function and MetabolismCristina BulgaruNo ratings yet
- 2011 BFnature09655 MOESM201 ESMDocument11 pages2011 BFnature09655 MOESM201 ESMliqinggreenNo ratings yet
- The Wonderful Story of Monoclonal Antibodies: Marie C BénéDocument7 pagesThe Wonderful Story of Monoclonal Antibodies: Marie C BénéNurkhalis BintangNo ratings yet
- 2003 Cce Citoesqueleto e CalcioDocument3 pages2003 Cce Citoesqueleto e CalcioCaio LeônidasNo ratings yet
- Histomorphology of The Pancreas in MynaDocument6 pagesHistomorphology of The Pancreas in MynaIndian Journal of Veterinary and Animal Sciences RNo ratings yet
- TMP 6 DAEDocument16 pagesTMP 6 DAEFrontiersNo ratings yet
- Ni Hms 585691Document20 pagesNi Hms 585691Anonymous 1EQutBNo ratings yet
- Brain, Behavior, and ImmunityDocument9 pagesBrain, Behavior, and ImmunityHelio RochaNo ratings yet
- Fimmu 11 00587Document12 pagesFimmu 11 00587ThormmmNo ratings yet
- Animal Models 1Document4 pagesAnimal Models 1Sanem CimenNo ratings yet
- Journal of Pediatric Surgery: Justin P. Wagner, Veronica F. Sullins, James C.Y. DunnDocument6 pagesJournal of Pediatric Surgery: Justin P. Wagner, Veronica F. Sullins, James C.Y. DunnNiningFirganMr-GenNo ratings yet
- Document 1 FDR SeDocument5 pagesDocument 1 FDR SeMaria Angelika BughaoNo ratings yet
- ChickenPeyersPatchesJI1980 PDFDocument9 pagesChickenPeyersPatchesJI1980 PDFDulce AmorNo ratings yet
- Sikasunge Et Al. 2009Document9 pagesSikasunge Et Al. 2009Luz Cielo Manrique CordovaNo ratings yet
- Acido Urico y La Respuesta InmuneDocument2 pagesAcido Urico y La Respuesta InmuneShagrath1989No ratings yet
- 1 s2.0 S1074552112004206 Main PDFDocument9 pages1 s2.0 S1074552112004206 Main PDFmanel ladjNo ratings yet
- Bowmaker 1998Document7 pagesBowmaker 1998marialopezmartinez424No ratings yet
- Nitric Oxide and Beta GlucansDocument11 pagesNitric Oxide and Beta GlucansKaren Claire HorcaNo ratings yet
- Group 6-3ebio: Assoc Prof. Loida R. Medina, PHD, RMT, RmicroDocument4 pagesGroup 6-3ebio: Assoc Prof. Loida R. Medina, PHD, RMT, RmicroAnne Olfato ParojinogNo ratings yet
- Cell Biology in Agriculture and Food SciencesDocument8 pagesCell Biology in Agriculture and Food SciencesLloyd MalictayNo ratings yet
- Octopus GenomeDocument18 pagesOctopus GenomeProsenjit PalNo ratings yet
- Plenary (Tue, 6 Sept 2016) : Problem 3-Gastrointestinal SystemDocument114 pagesPlenary (Tue, 6 Sept 2016) : Problem 3-Gastrointestinal SystemShitta InayahNo ratings yet
- Discussion.: All ProteinDocument7 pagesDiscussion.: All ProteinQadiir AlamNo ratings yet
- Z (H) VI Biotech 4Document69 pagesZ (H) VI Biotech 4Ladla ArainNo ratings yet
- 1 s2.0 S0012160614000475 MainDocument22 pages1 s2.0 S0012160614000475 MainSebastian HernandezNo ratings yet
- Joa 228 487Document8 pagesJoa 228 487rosangelaNo ratings yet
- Immunology of Fish: John E CushingDocument36 pagesImmunology of Fish: John E CushingDidier VelandiaNo ratings yet
- @content12562626 PDFDocument8 pages@content12562626 PDFDulce AmorNo ratings yet
- Stazione Zoologica Anton Dohrn - NapoliDocument17 pagesStazione Zoologica Anton Dohrn - NapoliAndersinclair AndersinclairNo ratings yet
- Primo Vascular System A Unique Biological System SDocument10 pagesPrimo Vascular System A Unique Biological System SMaria SaragocaNo ratings yet
- The Immunology of The Vermiform Appendix: A Review of The LiteratureDocument9 pagesThe Immunology of The Vermiform Appendix: A Review of The LiteratureHafiz OdinNo ratings yet
- Phox2b y Sueño Derivado de Astrocito PDFDocument27 pagesPhox2b y Sueño Derivado de Astrocito PDFLEISLY TATIANA OVIEDO GOMEZNo ratings yet
- TMP 1 EE0Document12 pagesTMP 1 EE0FrontiersNo ratings yet
- Archaea Cloaked in Mystery CurbioDocument5 pagesArchaea Cloaked in Mystery CurbiokiritinoNo ratings yet
- Invertebrate Cartilages, Notochordal Cartilage and Cartilage OriginsDocument16 pagesInvertebrate Cartilages, Notochordal Cartilage and Cartilage OriginsShu Shujaat LinNo ratings yet
- #AW - Cooper, 2003Document13 pages#AW - Cooper, 2003Andi WirdaniNo ratings yet
- Enteric Nervous SystemDocument12 pagesEnteric Nervous SystemedgarNo ratings yet
- Cfos, Jun y ExploracionDocument12 pagesCfos, Jun y ExploracionLuisa Fernanda Acevedo ReyesNo ratings yet
- Smith y Harper 2013 Causes of The Cambrian ExplosionDocument3 pagesSmith y Harper 2013 Causes of The Cambrian ExplosionlieselherverNo ratings yet
- Profound Gene Expression Changes in The Epithelial Monolayer of Active Ulcerative Colitis and Crohn's DiseaseDocument23 pagesProfound Gene Expression Changes in The Epithelial Monolayer of Active Ulcerative Colitis and Crohn's DiseaseYaumil ChoiriNo ratings yet
- Daftar PustakaDocument2 pagesDaftar PustakaRosintchi MirsalNo ratings yet
- Lund 2006Document17 pagesLund 2006marialuizacdasilvaNo ratings yet
- Microanatomical Studies of The Trachea in PigeonDocument5 pagesMicroanatomical Studies of The Trachea in PigeonIndian Journal of Veterinary and Animal Sciences RNo ratings yet
- Isolation of Streptococcus Pneumoniae Biofilm Mutants and Their Characterization During Nasopharyngeal ColonizationDocument13 pagesIsolation of Streptococcus Pneumoniae Biofilm Mutants and Their Characterization During Nasopharyngeal ColonizationRin ChanNo ratings yet
- Cell Culture HandbookDocument30 pagesCell Culture HandbookRamasamy VelmuruganNo ratings yet
- 3769 FullDocument12 pages3769 FullAgnes GintingNo ratings yet
- On The Colorimetry of Neuropeptide Y Hypothalamus and Ligamentous Parts in Male and Female Deer Immunohistochemical Analysis Report May 2021Document16 pagesOn The Colorimetry of Neuropeptide Y Hypothalamus and Ligamentous Parts in Male and Female Deer Immunohistochemical Analysis Report May 2021Athenaeum Scientific PublishersNo ratings yet
- The Evolution and Genomic Basis of Beetle Diversity: SignificanceDocument9 pagesThe Evolution and Genomic Basis of Beetle Diversity: SignificanceDANIELA MALAGÓN MONTAÑONo ratings yet
- Inflammation, Wound Healing, and Tissue Role of Substance P Neuropeptide inDocument11 pagesInflammation, Wound Healing, and Tissue Role of Substance P Neuropeptide insririniaNo ratings yet
- Molecular Regulation of Pancreatic Beta-Cell Mass DevelopmentDocument14 pagesMolecular Regulation of Pancreatic Beta-Cell Mass DevelopmentAndrei MitescuNo ratings yet
- Alveolar RegenerationDocument12 pagesAlveolar RegenerationWidia MeliawatiNo ratings yet
- tmp7FB6 TMPDocument11 pagestmp7FB6 TMPFrontiersNo ratings yet
- Untangling The Early Diversification of Eukaryotes: A Phylogenomic Study of The Evolutionary Origins of Centrohelida, Haptophyta and CryptistaDocument10 pagesUntangling The Early Diversification of Eukaryotes: A Phylogenomic Study of The Evolutionary Origins of Centrohelida, Haptophyta and CryptistaCarmen CaballeroNo ratings yet
- Des Car GableDocument10 pagesDes Car GableDago CastilloNo ratings yet
- Developmento of Vestibular SystemDocument11 pagesDevelopmento of Vestibular Systempaula.rhytmosNo ratings yet
- Iji2013 151028Document8 pagesIji2013 151028Kershaun MathewNo ratings yet
- Model Organisms in Spinal Cord RegenerationFrom EverandModel Organisms in Spinal Cord RegenerationCatherina G. BeckerNo ratings yet
- Ucu Iii Post Test July 4 2023 RatioDocument74 pagesUcu Iii Post Test July 4 2023 RatioVince C. MatamisNo ratings yet
- Colloidal Gold and Silver - The Use of Colloidal Gold - Then and NowDocument11 pagesColloidal Gold and Silver - The Use of Colloidal Gold - Then and NowDevon NarokNo ratings yet
- Immunopatho MCQ 2Document21 pagesImmunopatho MCQ 2Ebenizer DestaNo ratings yet
- Super Immunity by Joel Fuhrman, M.D.Document31 pagesSuper Immunity by Joel Fuhrman, M.D.HarperOne (an imprint of HarperCollins)85% (20)
- Lesson Plan - First Line of DefenseDocument3 pagesLesson Plan - First Line of Defenseapi-515540804No ratings yet
- Anti Phospholipid Inova OrgentecDocument16 pagesAnti Phospholipid Inova OrgentecMohamed AliNo ratings yet
- MDTruth - PathDocument433 pagesMDTruth - Pathabdul88fNo ratings yet
- Truth in AdvertisingDocument3 pagesTruth in AdvertisingClyde TanNo ratings yet
- Who Has The Flu Pre Lab InformationDocument18 pagesWho Has The Flu Pre Lab InformationAnvitha EllankiNo ratings yet
- The Ultimate Simple Protocol For Cancer Stage IV ProtocolDocument7 pagesThe Ultimate Simple Protocol For Cancer Stage IV ProtocolpgmessageNo ratings yet
- Introduction To ImmunologyDocument14 pagesIntroduction To Immunologykaiyeol exoNo ratings yet
- Final Micro ModuleDocument231 pagesFinal Micro ModuleSamuel SisayNo ratings yet
- Hilton Et Al, 1997 (Ab To BSA) PDFDocument10 pagesHilton Et Al, 1997 (Ab To BSA) PDFFarkhanda SadafNo ratings yet
- T O /O C: HE KRA Kraa OmplexDocument56 pagesT O /O C: HE KRA Kraa OmplexJames100% (1)
- Leishmaniasis in Humans (GP 14)Document30 pagesLeishmaniasis in Humans (GP 14)طارق عكاشةNo ratings yet
- 7 Natural Remedies For Epstein Barr VirusDocument40 pages7 Natural Remedies For Epstein Barr VirusDraganescu Violeta33% (3)
- Budwig Guide 2021.01Document37 pagesBudwig Guide 2021.01tem o0pNo ratings yet
- Q&A: What Are Pathogens, and What Have They Done To and For Us?Document6 pagesQ&A: What Are Pathogens, and What Have They Done To and For Us?yusuf mathiinul hakimNo ratings yet
- Disorders of White Blood Cells and Lymphoid TissuesDocument30 pagesDisorders of White Blood Cells and Lymphoid Tissuesammar amerNo ratings yet
- General Conference HlabuDocument88 pagesGeneral Conference HlabuKTP College Veng Aizawl86% (35)
- PG - ZOOLOGY-New CBCS Syllabus-NBU-2022-23Document35 pagesPG - ZOOLOGY-New CBCS Syllabus-NBU-2022-23Subhrangshu Ray Sarkar IX B 34No ratings yet
- The Town Where No One DiesDocument15 pagesThe Town Where No One DiesCbeClearNo ratings yet
- Applied ImmunologyDocument12 pagesApplied ImmunologyJia Ling100% (1)
- Ontogeny and Phylogeny of Immune SystemDocument3 pagesOntogeny and Phylogeny of Immune SystemPM Basiloy - AloNo ratings yet
- Lymphatic System SummaryDocument2 pagesLymphatic System SummaryLizbeth Quinn BatangosoNo ratings yet
- mRNA VaccinesDocument27 pagesmRNA VaccinesBOMMIDI JAHNAVI (RA2132001010057)100% (1)
- 2021 How I Treat Adult T-Cell Leukemia-LymphomaDocument12 pages2021 How I Treat Adult T-Cell Leukemia-Lymphomamateusmalacarne96No ratings yet
- 8 InfectiousDocument113 pages8 InfectiousLeng IlyNo ratings yet
- Capillarys ImmunotypingDocument62 pagesCapillarys ImmunotypingAbdel Razzak Mikati100% (1)