Professional Documents
Culture Documents
Holmes 2002
Holmes 2002
Uploaded by
Rolando Miranda PeñaCopyright:
Available Formats
You might also like
- Risk Assessment - Aluminium WorksDocument4 pagesRisk Assessment - Aluminium Worksburak0% (1)
- Activity Hazard AnalysisDocument7 pagesActivity Hazard AnalysisAnthony MacatangayNo ratings yet
- A Comparison of Obstetric Maneuvers For The Acute Management of Shoulder DystociaDocument7 pagesA Comparison of Obstetric Maneuvers For The Acute Management of Shoulder DystociaNellyn Angela HalimNo ratings yet
- Jurnal Diagnostik ADocument8 pagesJurnal Diagnostik AImtina AhdaNo ratings yet
- Out 21Document5 pagesOut 21Noven MezaNo ratings yet
- Prediction of Adverse Cardiac Outcomes in High-Risk Mexican Patients With Chest Pain in The Emergency DepartmentDocument6 pagesPrediction of Adverse Cardiac Outcomes in High-Risk Mexican Patients With Chest Pain in The Emergency Departmentluis sanchezNo ratings yet
- Lally2013 PDFDocument8 pagesLally2013 PDFFebry NurkamilaNo ratings yet
- Achondroplasia Natural History Study (CLARITY)Document7 pagesAchondroplasia Natural History Study (CLARITY)jakelinelagoadvNo ratings yet
- Ferro 2008Document8 pagesFerro 2008Carlos RiquelmeNo ratings yet
- C2 U5 Williams Et Al Critical Care Clinics 2013Document32 pagesC2 U5 Williams Et Al Critical Care Clinics 2013Diego CrucesNo ratings yet
- J Jpedsurg 2008 06 024Document1 pageJ Jpedsurg 2008 06 024afsdsaadsNo ratings yet
- Anesthesia-Pediatric Perioperative Cardiac Arrest Poca RegistryDocument7 pagesAnesthesia-Pediatric Perioperative Cardiac Arrest Poca Registryjcarl_20063003No ratings yet
- Radiol 221926Document9 pagesRadiol 221926Sakkuru Yeyen LiviaNo ratings yet
- Thursday, October 10, 2013 4:10 - 5:10 Concurrent Session: TraumaDocument2 pagesThursday, October 10, 2013 4:10 - 5:10 Concurrent Session: TraumaPeko PekoNo ratings yet
- 1756 0500 6 477 PDFDocument6 pages1756 0500 6 477 PDFanon_118437533No ratings yet
- 1092 0684 Article Pe11Document8 pages1092 0684 Article Pe11Abhilash VemulaNo ratings yet
- Asensio, JA, (2020) - Tratamiento Quirúrgico de Las Lesiones de La Arteria Braquial y Predictores de Resultado.Document12 pagesAsensio, JA, (2020) - Tratamiento Quirúrgico de Las Lesiones de La Arteria Braquial y Predictores de Resultado.Edgar Geovanny Cardenas FigueroaNo ratings yet
- HydrocephalusDocument8 pagesHydrocephaluscaliptra36No ratings yet
- Accuracy of Trauma Ultrasound in Major Pelvic InjuryDocument5 pagesAccuracy of Trauma Ultrasound in Major Pelvic InjuryEvelyn GrandaNo ratings yet
- Ucm 439476Document1 pageUcm 439476Fadel BilondatuNo ratings yet
- Flaherty 2016Document6 pagesFlaherty 2016Diornald MogiNo ratings yet
- Fried Frailty Pred Surg Outcomes AmCSurg 10Document8 pagesFried Frailty Pred Surg Outcomes AmCSurg 10edos838No ratings yet
- HSDC CBC 2015Document5 pagesHSDC CBC 2015Bob sponjaNo ratings yet
- Cost and Outcomes of Assessing Patients With Chest Pain in An Australian Emergency DepartmentDocument7 pagesCost and Outcomes of Assessing Patients With Chest Pain in An Australian Emergency DepartmentPeter ThaiNo ratings yet
- Clinical Findings and Diagnostic Value of Post-Traumatic Thoracic Radiographs in Dogs and Cats With Blunt TraumaDocument10 pagesClinical Findings and Diagnostic Value of Post-Traumatic Thoracic Radiographs in Dogs and Cats With Blunt TraumaAna CicadaNo ratings yet
- WTACritical Decisions Management of Rib FracturesDocument4 pagesWTACritical Decisions Management of Rib FracturesToàn NguyễnNo ratings yet
- Long-Term Outcomes After Surgical Treatment of Pediatric Neurogenic Thoracic Outlet SyndromeDocument11 pagesLong-Term Outcomes After Surgical Treatment of Pediatric Neurogenic Thoracic Outlet Syndromewalter fire 0057No ratings yet
- 564 Full PDFDocument7 pages564 Full PDFMi MihaelaNo ratings yet
- NEXUS Chest Validation of A Decision Instrument For Selective Chest Imaging in Blunt TraumaDocument7 pagesNEXUS Chest Validation of A Decision Instrument For Selective Chest Imaging in Blunt TraumaAnastasia EkaNo ratings yet
- Marshall1991 The Outcome of Severe Closed Head InjuryDocument9 pagesMarshall1991 The Outcome of Severe Closed Head InjuryJulieta PereyraNo ratings yet
- Bossi - Echocardiogric EvaluationDocument8 pagesBossi - Echocardiogric EvaluationSzendeNo ratings yet
- Berg 2012Document7 pagesBerg 2012Mario Espinosa GamezNo ratings yet
- Use of The Skeletal Survey in The Evaluation of Child MaltreatmentDocument3 pagesUse of The Skeletal Survey in The Evaluation of Child MaltreatmentAprilia DhammashintaNo ratings yet
- Chest Trauma in Athletic Medicine - Article.Document7 pagesChest Trauma in Athletic Medicine - Article.salmankhan09215No ratings yet
- Elkhunovich2016 The Utility of Cranial Ultrasound For Detection of IntracranialDocument6 pagesElkhunovich2016 The Utility of Cranial Ultrasound For Detection of IntracranialModou NianeNo ratings yet
- Cervical Spine Clearance 2009Document7 pagesCervical Spine Clearance 2009Abdulelah Al.luhaybiNo ratings yet
- ANGHELESCU Et Al Clinical and Diagnostic Imaging Findings Predict Anesthetic Complications in Children With Malignant MMDocument9 pagesANGHELESCU Et Al Clinical and Diagnostic Imaging Findings Predict Anesthetic Complications in Children With Malignant MMJill SweetNo ratings yet
- Clearing The Cervical Spine of Adult Victims of TraumaDocument7 pagesClearing The Cervical Spine of Adult Victims of TraumaVince AzevoucheNo ratings yet
- Femur Fractures Should Not Be Considered Distracting Injuries For CervicalDocument6 pagesFemur Fractures Should Not Be Considered Distracting Injuries For CervicalnellyNo ratings yet
- Evaluation of Chest Pain in Primary Care Patients-AAFPDocument3 pagesEvaluation of Chest Pain in Primary Care Patients-AAFPnouval_iqbalNo ratings yet
- Complications Predicting Perioperative Mortality in Patients Undergoing Elective Craniotomy A Population Based StudyDocument11 pagesComplications Predicting Perioperative Mortality in Patients Undergoing Elective Craniotomy A Population Based Study49hr84j7spNo ratings yet
- Cervical Angiograms in Cervical Spine Trauma Patients 5 Years After The Data: Has Practice Changed?Document4 pagesCervical Angiograms in Cervical Spine Trauma Patients 5 Years After The Data: Has Practice Changed?edi_wsNo ratings yet
- Research: CATCH: A Clinical Decision Rule For The Use of Computed Tomography in Children With Minor Head InjuryDocument8 pagesResearch: CATCH: A Clinical Decision Rule For The Use of Computed Tomography in Children With Minor Head InjuryCarlos Martin Yafac RiscoNo ratings yet
- NASCETDocument9 pagesNASCETektosNo ratings yet
- Conference Paper: Rapid Physical Assessment of The Injured ChildDocument4 pagesConference Paper: Rapid Physical Assessment of The Injured ChildMaiush JbNo ratings yet
- (10920684 - Neurosurgical Focus) Predictors of Outcome of Subdural Empyema in ChildrenDocument6 pages(10920684 - Neurosurgical Focus) Predictors of Outcome of Subdural Empyema in ChildrenFatima RamirezNo ratings yet
- Trauma Medular - Cervical Trauma ColumnaDocument28 pagesTrauma Medular - Cervical Trauma ColumnayustinjulianavNo ratings yet
- Ajr 09 2544Document7 pagesAjr 09 2544Elly LutfiasariNo ratings yet
- Nejmoa 2026141Document14 pagesNejmoa 2026141Matheus FelipeNo ratings yet
- Timing of Cranioplasty After Decompressive Craniectomy ForDocument5 pagesTiming of Cranioplasty After Decompressive Craniectomy ForjoerizalNo ratings yet
- Nestelberger Et Al 2019 Predicting Major Adverse Events in Patients With Acute Myocardial InfarctionDocument13 pagesNestelberger Et Al 2019 Predicting Major Adverse Events in Patients With Acute Myocardial InfarctionNJEBARIKANUYE EugèneNo ratings yet
- Ultrasonido Doppler Temprano AMSDocument7 pagesUltrasonido Doppler Temprano AMSKaren Marbelly OrozcoNo ratings yet
- 1 s2.0 S0735109720344223 MainDocument12 pages1 s2.0 S0735109720344223 MainRizky AisNo ratings yet
- The Impact of Obesity On Severely Injured Children and AdolescentsDocument4 pagesThe Impact of Obesity On Severely Injured Children and AdolescentsUswatun HasanahNo ratings yet
- Early Predictors of Mortality in HemodynamicallyDocument7 pagesEarly Predictors of Mortality in HemodynamicallytesfahuntekletilahunNo ratings yet
- Emergency Medical Services Intervals and Survival in Trauma: Assessment of The "Golden Hour" in A North American Prospective CohortDocument16 pagesEmergency Medical Services Intervals and Survival in Trauma: Assessment of The "Golden Hour" in A North American Prospective CohortrutnomleniNo ratings yet
- World Neurosurg 2021 Apr 2 Camino-Willhuber GDocument6 pagesWorld Neurosurg 2021 Apr 2 Camino-Willhuber GFernando SousaNo ratings yet
- Abdominal Ultrasound Is An Unreliable Modality For The Detection of Hemoperitoneum in Patients With Pelvic FractureDocument6 pagesAbdominal Ultrasound Is An Unreliable Modality For The Detection of Hemoperitoneum in Patients With Pelvic FractureEvelyn GrandaNo ratings yet
- 2003-Academic Emergency MedicineDocument154 pages2003-Academic Emergency MedicinealiceNo ratings yet
- Proceedings of The 2014 Spring Meeting of The Society of British 2014Document40 pagesProceedings of The 2014 Spring Meeting of The Society of British 2014rabiatul adawiyahNo ratings yet
- Posterior Fossa Epidural Hematomas in CHDocument5 pagesPosterior Fossa Epidural Hematomas in CHmirmasottNo ratings yet
- Office Based Anesthesia Complications: Prevention, Recognition and ManagementFrom EverandOffice Based Anesthesia Complications: Prevention, Recognition and ManagementGary F. BoulouxNo ratings yet
- First Aid in Electric ShockDocument2 pagesFirst Aid in Electric ShockLevin ChespedinNo ratings yet
- SOPs Handling First AidDocument2 pagesSOPs Handling First AidsridharNo ratings yet
- CPM Question Bank With SolutionDocument78 pagesCPM Question Bank With SolutionDevansh RaiNo ratings yet
- Learner Guide SITXWHS005 - Participate in Safe Work PracticesDocument32 pagesLearner Guide SITXWHS005 - Participate in Safe Work PracticessalazarayieNo ratings yet
- Hazard Identification and ControlDocument93 pagesHazard Identification and ControlMarwa MohammadNo ratings yet
- Grafik Kecelakaan 2016 PDFDocument2 pagesGrafik Kecelakaan 2016 PDFragilNo ratings yet
- Analyzing Construction Site Accidents in KuwaitDocument28 pagesAnalyzing Construction Site Accidents in Kuwaitzeyad alsaroriNo ratings yet
- Online National Electronic Injury Surveillance System (ONEISS) FactsheetDocument14 pagesOnline National Electronic Injury Surveillance System (ONEISS) FactsheetOliVerNo ratings yet
- HSE Presentation On Supervisors Training HseprofDocument31 pagesHSE Presentation On Supervisors Training HseprofGavin VassellNo ratings yet
- Pubmed InjuryORkn SetDocument392 pagesPubmed InjuryORkn SetLucas de BritoNo ratings yet
- Daftar PustakaDocument2 pagesDaftar PustakaNurul Safiah SuhaimiNo ratings yet
- Occupational Accidents and InjuryDocument43 pagesOccupational Accidents and InjuryAnam FatimaNo ratings yet
- Knee ExercisesDocument4 pagesKnee ExercisesRaj PhysioNo ratings yet
- HIRA - Fixed Scaffold and Wall BreakingDocument6 pagesHIRA - Fixed Scaffold and Wall BreakingSujan Augustin100% (2)
- Proper TypingDocument19 pagesProper Typingmary glorNo ratings yet
- Awareness of Injury Prevention 1Document11 pagesAwareness of Injury Prevention 1Avegaile PaduaNo ratings yet
- Trauma Alert Criteria Brevard County Fire Rescue Trauma Alert Criteria Brevard County Fire RescueDocument3 pagesTrauma Alert Criteria Brevard County Fire Rescue Trauma Alert Criteria Brevard County Fire Rescueshaun shepherdNo ratings yet
- Toolbox Talks: Hand Tool SafetyDocument1 pageToolbox Talks: Hand Tool Safetyserdar yücelNo ratings yet
- Effects of Nordic Hamstring Exercise On Hamstring InjuriesDocument10 pagesEffects of Nordic Hamstring Exercise On Hamstring InjuriesArathyNo ratings yet
- HSE Report-Plastering-439Document5 pagesHSE Report-Plastering-439jameelNo ratings yet
- JSA Additional Lamp Paiton 3Document10 pagesJSA Additional Lamp Paiton 3MarhendraNo ratings yet
- 2008 07 What Is Process SafetyDocument1 page2008 07 What Is Process SafetyYuda HerdiantoNo ratings yet
- Nervous System Head InjuryDocument11 pagesNervous System Head InjurydimlyNo ratings yet
- Final Thesis (Dr. Neeraj)Document79 pagesFinal Thesis (Dr. Neeraj)Prosenjit BhowalNo ratings yet
- Sports Medical History FormDocument2 pagesSports Medical History Formgilikarn9960No ratings yet
- 3 - Unsafe Unhealthy Acts ConditionsDocument18 pages3 - Unsafe Unhealthy Acts ConditionsAchilles SantiagoNo ratings yet
- HIRADC - 001 - Survey WorkDocument3 pagesHIRADC - 001 - Survey WorkZhafri SyazwiNo ratings yet
- Montrell Jolly Probable CauseDocument3 pagesMontrell Jolly Probable CauseLeigh EganNo ratings yet
Holmes 2002
Holmes 2002
Uploaded by
Rolando Miranda PeñaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Holmes 2002
Holmes 2002
Uploaded by
Rolando Miranda PeñaCopyright:
Available Formats
PEDIATRICS/ORIGINAL CONTRIBUTION
A Clinical Decision Rule for Identifying
Children With Thoracic Injuries After Blunt
Torso Trauma
From the Division of Emergency James F. Holmes, MD* See related article, p. 500, and editorial, p. 537.
Medicine, Department of Internal Peter E. Sokolove, MD*
Medicine,* the Department of William E. Brant, MD‡
Radiology,‡ and the Department of Study objective: We sought to determine the prevalence of
Nathan Kuppermann, MD, MPH*§
Pediatrics,§ University of California– thoracic injuries in children sustaining blunt torso trauma and
Davis School of Medicine,
Sacramento, CA. to develop a clinical prediction rule to identify children with
these injuries.
Author contributions are provided
at the end of this article. Methods: We prospectively enrolled pediatric patients (<16
Received for publication June 6, 2001. years) who presented to the emergency department of a Level I
Revision received December 28, 2001.
Accepted for publication
trauma center with blunt torso trauma and underwent chest
January 10, 2002. radiography. Clinical findings were recorded in a standardized
Presented at the Society for Academic fashion by the ED faculty physician. Thoracic injuries included
Emergency Medicine annual meeting, the following: pulmonary contusion, hemothorax, pneumotho-
Atlanta, GA, May 2001.
rax, pneumomediastinum, tracheal-bronchial disruption, aortic
Address for reprints: James F. injury, hemopericardium, pneumopericardium, cardiac contu-
Holmes, MD, University of California–
Davis Medical Center, Division of sion, rib fracture, sternal fracture, or any injury to the diaphragm.
Emergency Medicine, 2315 Stockton Multiple logistic regression and recursive partitioning analyses
Boulevard, PSSB 2100, Sacramento,
CA 95817-2282; 916-734-1539,
were performed to generate a clinical prediction rule for identi-
fax 916-734-7950; E-mail fying children with these injuries.
jfholmes@ucdavis.edu.
Results: Nine hundred eighty-six patients with a mean age of
Copyright © 2002 by the American
College of Emergency Physicians.
8.3±4.8 years were enrolled. Eighty (8.1%; 95% confidence
interval [CI] 6.5% to 10.0%) patients sustained thoracic injuries.
0196-0644/2002/$35.00 + 0
47/1/122901 Multiple logistic regression and recursive partitioning analyses
doi:10.1067/mem.2002.122901 identified the following predictors of thoracic injuries: low sys-
tolic blood pressure (14% with injury versus 2% without injury;
adjusted odds ratio [OR] 4.6), elevated age-adjusted respiratory
rate (51% versus 16%; adjusted OR 2.9), abnormal results on
examination of the thorax (68% versus 36%; adjusted OR 3.6),
abnormal chest auscultation findings (14% versus 1%; adjusted
OR 8.6), femur fracture (13% versus 5%; adjusted OR 2.2), and
a Glasgow Coma Scale (GCS) score of less than 15 (61% versus
26%; adjusted OR 3.3). Seventy-eight (98%; 95% CI 91% to
100%) of the 80 patients with thoracic injuries had at least 1 of
these predictive factors. Three hundred thirty-six (37%) children
had none of these predictive factors, including 2 (0.6%; 95% CI
4 9 2 ANNALS OF EMERGENCY MEDICINE 39:5 MAY 2002
CLINICAL DECISION RULE FOR PEDIATRIC TRAUMA
Holmes et al
0.1% to 2.1%) with thoracic injuries. These 2 injuries, however, trauma; blunt traumatic event with extremity paralysis;
did not require any intervention. multiple bone fractures; a CRAMS score (measuring circu-
lation, respiration, abdomen, motor responses, and
Conclusion: Predictors of thoracic injury in children sustaining speech) of 8 or less3; a physical examination suggestive of
blunt torso trauma include low systolic blood pressure, elevated torso injury after blunt trauma; or a Pediatric Trauma
respiratory rate, abnormal results on thoracic examination, Score of 8 or less after blunt trauma. Patients not under-
abnormal chest auscultation findings, femur fracture, and a GCS going chest radiography in the ED or transferred to our
score of less than 15. These predictors can be used to create a facility after initial evaluation at an outside ED were
sensible clinical decision rule for the identification of children excluded.
with thoracic injuries. Patients underwent a complete physical examination
by the faculty emergency physician. Vital signs and physi-
[Holmes JF, Sokolove PE, Brant WE, Kuppermann N. A clinical cal examination findings were documented on a struc-
decision rule for identifying children with thoracic injuries after tured data collection sheet after physical examination.
blunt torso trauma. Ann Emerg Med. May 2002;39:492-499.] Data sheets were completed as soon as possible after the
physical examination and before chest radiography results
INTRODUCTION were known in the majority of cases. Low systolic blood
pressure was defined by the following age-adjusted cutoff
Thoracic injuries account for 14% of pediatric trauma- points for the initial ED systolic blood pressure: age 0 to 1
related deaths and are second only to head injuries as a month, systolic blood pressure of less than 70 mm Hg; 1
cause of death in pediatric patients experiencing blunt month to 5 years, systolic blood pressure of less than 80
trauma.1 After physical examination, chest radiography mm Hg; and 5 to 15 years, systolic blood pressure of less
is the initial diagnostic test for the identification of tho- than 90 mm Hg.4 Initial respiratory rates were considered
racic injuries.2 Chest radiographs, however, may not be elevated if they were more than 2 SDs above the age-
necessary for all pediatric patients with blunt trauma. adjusted mean on the basis of a previously defined scale.5
Although chest radiography is noninvasive and rela- The results of the thoracic examination were consid-
tively inexpensive, it becomes costly if universally applied ered abnormal if erythema, abrasions, contusions, lacera-
to patients at low risk for thoracic injuries. In addition, tions, crepitus, or tenderness were identified on the ante-
chest radiography exposes the patient to radiation and rior or posterior thorax. Findings on auscultation of the
requires either transportation of the patient to the radio- chest were considered abnormal if breath sounds were
graphic suite or a radiology technician to be present at the decreased or absent or if crackles or rhonchi were present.
patient’s bedside. Identification of predictors of thoracic The patients’ abdominal examination results were con-
injury, therefore, may provide clinicians with useful in- sidered to be abnormal if tenderness to palpation was
formation to enhance clinical and cost efficiency. present. The patients’ levels of consciousness were mea-
The objectives of this study were to determine the sured with the GCS for children at least 2 years old and
prevalence of thoracic injuries in a population of pedi- with the pediatric GCS for children younger than 2 years.6
atric patients presenting to the emergency department Patients with a GCS score of less than 15 were considered
after blunt torso trauma and to create a clinical decision to have a decreased level of consciousness.
rule to identify children with these injuries. Thoracic injury was considered present if the patient
had an identified injury to a structure within the thorax,
M AT E R I A L S A N D M E T H O D S including pulmonary contusion, hemothorax, pneumo-
thorax, pneumomediastinum, tracheal-bronchial disrup-
The study was conducted at a Level I trauma center be- tion, aortic injury, hemopericardium, pneumoperi-
tween April 1996 and September 1998. We prospectively cardium, cardiac contusion, radiographically identified
enrolled pediatric patients younger than 16 years old sus- rib fracture, sternal fracture, or any injury to the dia-
taining blunt trauma if they had any of the following and phragm. Isolated rib fractures were categorized as tho-
underwent chest radiography during ED evaluation: blunt racic injuries because of the greater morbidity and mor-
torso trauma from a significant mechanism of injury tality associated with rib fractures in children compared
(motor vehicle crash, automobile versus pedestrian, falls with in adults and because of the greater impact forces
of >10 feet); decreased level of consciousness (Glasgow required to fracture the less calcified ribs of children.7
Coma Scale [GCS] <15) in association with blunt torso Injuries were considered present if identified on any of
MAY 2002 39:5 ANNALS OF EMERGENCY MEDICINE 4 9 3
CLINICAL DECISION RULE FOR PEDIATRIC TRAUMA
Holmes et al
the following: plain chest radiography, abdominal or internally by using 10-fold cross-validation. Recursive
chest computed tomography (CT), bronchoscopy, tho- partitioning may be preferable to multiple logistic regres-
rascopy, tube thoracostomy, thoracotomy, laparotomy, sion when the objective is to develop a decision rule with
angiography, ECG, or echocardiography. All diagnostic the highest sensitivity.9
studies beyond chest radiography were obtained at the We considered the same 7 variables for entry into a
discretion of the treating physicians. Faculty radiologists multivariate logistic regression analysis, and variables
interpreted all radiographic studies. demonstrating a significant association (P<.05) with tho-
Patients were admitted to the hospital at the discretion racic injury were considered independent predictors of
of the faculty emergency physicians in conjunction with chest injury. To validate the logistic regression model, we
the trauma surgery team. All admitted patients were fol- performed 2 separate bootstrap resampling procedures
lowed through their hospital courses for identification of with 1,000 iterations each. Bootstrap resampling ran-
thoracic injuries and therapy for those injuries. Patients domly selects patients from the original database with
were considered to require specific therapy for a thoracic replacement to create new databases of the same size as
injury if they underwent tube thoracostomy, thoracotomy, the original database. These new databases are subse-
therapeutic bronchoscopy, or endotracheal intubation. quently used to test the model attributes.10-12 This proce-
Patients discharged to home after ED evaluations were dure generates conservative estimates of confidence
contacted by telephone 1 week after discharge to deter- intervals (CIs) and assesses the stability of the model. We
mine clinical status. Patients without symptoms of tho- obtained 95% bias-corrected CIs of the investigated vari-
racic injury at the telephone follow-up were considered ables in the bootstrap analysis. We then repeated the mul-
not to have a thoracic injury. On completion of the study, tivariate analysis on 1,000 bootstrap databases to identify
we reviewed the trauma registry and continuing quality- the percentage of iterations in which each predictive vari-
improvement records of the participating institution to able was identified as an independent predictor (P<.05)
determine whether any enrolled patients discharged from of thoracic injury. We considered the selection of a vari-
the ED or inpatient ward without the diagnosis of thoracic able to be validated if it was selected as significant in
injury were later given a diagnosis of such injuries. greater than 50% of the bootstrap iterations.11
Continuous data were reported as the mean±1 SD. We calculated the sensitivity, specificity, positive pre-
Variables hypothesized a priori to be associated with chest dictive value, negative predictive value, and positive and
injury were entered into both multiple logistic regression negative likelihood ratios for those variables considered
and binary recursive partitioning analyses. These variables important in both of these models. We then calculated the
included the following: low systolic blood pressure, elevated risks of injury in the presence of any of the risk factors
respiratory rate, abnormal thoracic examination results, versus the absence of all the risk factors.
abnormal thoracic auscultation findings, abdominal tender- Sample size was based on the requirement of 10 out-
ness, femur fracture, and a GCS score of less than 15. comes of interest (thoracic injury) per predictor variable
We performed binary recursive partitioning in addi- analyzed in a logistic regression analysis.13,14 Data analy-
tion to multiple logistic regression to develop a model sis was performed with STATA 6.0 for Windows (STATA
that maximized sensitivity for identifying children with Corporation, College Station, TX) statistical software.
thoracic injuries, while also maximizing specificity. We Answer Tree statistical software (version 2.0, SPSS Inc.,
planned to use those variables identified in either the Chicago, IL) was used to conduct the recursive partition-
recursive partitioning or logistic regression analyses for ing. The study was approved by the Human Subjects
inclusion in the decision rule. Research Committee at our institution.
Binary recursive partitioning refers to an analytic tech-
nique by which patients are divided into subpopulations R E S U LT S
(nodes) on the basis of risk profiles for the outcome of
interest.8 Each subpopulation is subsequently subdivided A total of 986 patients were enrolled during a 28-month
to minimize misclassification of patients. The process is period. The mean age of the population was 8.3±4.8
continued until either a subpopulation is homogeneous years, and the median PediatricTrauma Score was 10
with regard to the outcome variable or too small to be sub- (interquartile range 9 to 11). Mechanisms of injury
divided further. The results of a recursive partitioning included motor vehicle crash in 348 (35%), automobile
analysis are typically displayed in a tree-like format that is versus pedestrian in 244 (27%), fall in 160 (16%), auto-
easy for the clinician to follow. The analysis was validated mobile versus bicycle in 87 (9%), bicycle fall in 53 (5%),
4 9 4 ANNALS OF EMERGENCY MEDICINE 39:5 MAY 2002
CLINICAL DECISION RULE FOR PEDIATRIC TRAUMA
Holmes et al
crush injuries in 36 (4%), assault in 28 (3%), child abuse on further studies (CT, angiography, or echocardiography).
in 14 (1%), and other in 16 (1%). These 30 patients were ultimately given a diagnosis of the
Eighty (8.1%; 95% CI 6.5% to 10.0%) patients were following injuries: pneumothorax (n=11), hemothorax
determined to have thoracic injuries. The mean age of (n=3), pulmonary contusion (n=20), rib fracture (n=9),
these 80 patients was 8.9±5.2 years, and the median cardiac contusion (n=1), pericardial effusion (n=1), and
Pediatric Trauma Score was 8 (interquartile range 5 to sternal fracture (n=1).
10). Fifty-four (68%) patients with thoracic injuries had Five hundred sixty-one (57%) patients had imaging
abnormalities on their thoracic examinations, including studies in addition to chest radiography. Five hundred
the following: erythema (n=1), abrasions (n=41), contu- fifty-five (56%) patients underwent abdominal CT, of
sions (n=9), lacerations (n=1), crepitus (n=8), and ten- whom 56 (10%) demonstrated thoracic injuries. Eight
derness (n=24). Patients with thoracic injuries and a GCS patients underwent chest CT scanning, of whom 3 (38%)
score of 15 were more likely to have thoracic tenderness had thoracic injuries. Eleven patients underwent angiog-
(18/31 [58%; 95% CI 39% to 75%]) than those patients raphy of the thoracic aorta, and 2 (18%) had thoracic aor-
with thoracic injuries and a GCS score of 13 or 14 (2/12 tic injuries.
[17%; 95% CI 2% to 48%]; odds ratio [OR] 6.9; 95% CI Fifty (63%; 95% CI 51% to 73%) of 80 patients with
1.3 to 37). Eleven patients with chest injuries had low chest injuries underwent specific therapies. Twenty-six
systolic blood pressures. (33%; 95% CI 22% to 44%) patients underwent tube tho-
Six hundred twenty-one (63%) patients were admitted racostomy. Three (4%; 95% CI 1% to 11%) patients
to the hospital. Telephone follow-up was obtained for underwent thoracotomy. Thirty-eight (45%; 95% CI 34%
329 (90%) of the 365 patients discharged to home, and all to 57%) patients underwent endotracheal intubation.
were asymptomatic at the time of follow-up. There were Seven (9%; 95% CI 4% to 17%) patients underwent bron-
no apparent cases of missed thoracic injuries among choscopy.
patients in this study on review of the trauma registry and Results of the multiple logistic regression analysis are
continuing quality improvement records. shown in Table 2. Independent predictors of thoracic
The frequencies of specific thoracic injuries identified injury included low systolic blood pressure, elevated res-
are listed in Table 1. Thirty-eight (48%) patients had mul- piratory rate, abnormal thoracic examination results,
tiple thoracic injuries. Fifty (63%; 95% CI 51% to 73%) of abnormal chest auscultation findings, and a GCS score of
the 80 patients with thoracic injuries had an injury visual- less than 15. Femur fracture showed a trend toward statis-
ized on initial ED chest radiography. The remaining thirty tical significance. The area under the model receiver
(37%) patients had their thoracic injuries identified only operating characteristic curve was 0.82. The model
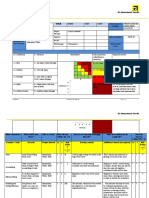
Table 1.
Frequency of thoracic injuries in the study population. Table 2.
Results of multiple logistic regression.
Frequency Among Frequency
Patients With Among Total Frequency With
Thoracic Injuries Population (n=986), Which Variable
Type of Injury No. (n=80), % (95% CI) % (95% CI) Bias: Was Identified
Adjusted Corrected P as an Independent
Pulmonary contusion 57 71 (60–81) 5.8 (4.4–7.4) Variable OR 95% CI* Value Predictor,* %
Rib fracture 28 35 (25–46) 2.8 (1.9–4.1)
Isolated rib fracture 9 11 (5–20) 0.9 (0.4–1.7) Hypotension 4.6 1.0–13.8 .003 78
Pneumothorax 20 25 (16–36) 2.0 (1.2–3.1) GCS score <15 3.3 1.9–5.6 <.001 99
Hemothorax 9 11 (5–20) 0.9 (0.4–1.7) Abnormal thoracic 3.6 2.1–6.4 <.001 100
Hemopneumothorax 5 6 (2–14) 0.5 (0.2–1.2) examination results
Pneumomediastinum* 6 8 (3–16) 0.6 (0.2–1.3) Abnormal chest 8.6 1.9–31.3 <.001 91
Cardiac 5 6 (2–14) 0.5 (0.2–1.3) auscultation findings
Aortic 2 3 (0–9) 0.2 (0.0–0.7) Elevated respiratory rate 2.9 1.5–5.1 <.001 94
Diaphragmatic injury 1 1 (0–7) 0.1 (0.0–0.6) Femur fracture 2.2 0.9–5.1 .08 39
Sternal fracture 1 1 (0–7) 0.1 (0.0–0.6) Abdominal tenderness 1.1 0.6–1.9 .76 7
*Includes 2 patients with tracheal lacerations. *
In bootstrap validation, as described in the “Materials and Methods” section.
MAY 2002 39:5 ANNALS OF EMERGENCY MEDICINE 4 9 5
CLINICAL DECISION RULE FOR PEDIATRIC TRAUMA
Holmes et al
demonstrated satisfactory goodness-of-fit, as measured abnormal thoracic examination, an abnormal chest aus-
with the Hosmer-Lemeshow test (P=.70). The bootstrap cultation finding, femur fracture, or a GCS score of <15)
analysis identified all 5 variables as independent predic- was present in 650 (66%; 95% CI 63% to 69%) patients
tors of thoracic injury in more than 50% of the 1,000 undergoing chest radiography. Included in this group
bootstrap iterations (Table 2). were 78 (sensitivity 98%; 95% CI 91% to 100%) of the 80
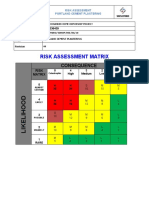
The results of the recursive partitioning analysis are patients with thoracic injuries. Three hundred thirty-six
demonstrated in the Figure. In the resulting tree, the most (34%) patients had none of these predictive factors dur-
important variable, chest auscultation, is the top node of ing the ED evaluation, including 2 (0.6%; 95% CI 0.1% to
the decision tree. As the tree branches, the risk of thoracic 2.1%) patients with thoracic injuries. These 2 patients are
injury can be estimated for particular combinations of described in Table 4.
variables. This multivariate analysis identified the same 5 One of the 2 injured patients without any of the high-
predictor variables as the multiple logistic regression risk predictors experienced shortness of breath during
analysis but added femur fracture as an important vari- ED observation but after initial evaluation. This patient
able in the model. had both a pulmonary contusion and a pneumothorax
The sensitivity, specificity, positive and negative pre- identified on abdominal CT scan, but only the pulmonary
dictive values, and positive and negative likelihood ratios contusion was visualized on ED chest radiography. The
for each of the high-risk variables identified in either child was observed in the hospital for 3 days but without
analysis are presented in Table 3. At least 1 of the predic- specific therapy for these injuries. The second patient had
tors of thoracic injury identified in either analysis (low a pulmonary contusion visualized only on abdominal CT
systolic blood pressure, an elevated respiratory rate, an scan. This patient was observed in the hospital for 1 day
Figure.
Results of the recursive No injury 906 (92%)
partitioning analysis. Thoracic injury 80 (8%)
Each box represents the Abnormal
Yes No
number of patients with auscultation
and without thoracic
No injury 9 (45%) No injury 897 (93%)
injury given the particular Thoracic injury 11 (55%) Thoracic injury 69 (7%)
combination of variables.
Yes Low systolic No
blood pressure
No injury 12 (55%) No injury 885 (94%)
Thoracic injury 10 (45%) Thoracic injury 59 (6%)
Yes Tachypnea No
No injury 135 (84%) No injury 750 (96%)
Thoracic injury 26 (16%) Thoracic injury 33 (4%)
Yes GCS score <15 No
No injury 173 (91%) No injury 577 (97%)
Thoracic injury 17 (9%) Thoracic injury 16 (3%)
Yes Abnormal thoracic No
examination results
No injury 218 (94%) No injury 359 (99%)
Thoracic injury 13 (6%) Thoracic injury 3 (1%)
Yes Femure No
fracture
No injury 25 (96%) No injury 334 (99%)
Thoracic injury 1 (4%) Thoracic injury 2 (0.6%)
4 9 6 ANNALS OF EMERGENCY MEDICINE 39:5 MAY 2002
CLINICAL DECISION RULE FOR PEDIATRIC TRAUMA
Holmes et al
and was discharged home without further incident or patient population. Rib fractures are considered to occur
therapy. less frequently in children than in adults yet are associ-
ated with other significant injuries in the pediatric popu-
DISCUSSION lation.7 Similar to previous studies, aortic injuries,
diaphragmatic injuries, and sternal fractures were rare in
In this series of pediatric patients with blunt trauma evalu- this population,1,15,19 and no patient enrolled in the
ated in the ED, 8% of those undergoing chest radiography study had a bronchial injury identified.
had thoracic injuries. Clinical findings associated with Abnormal chest auscultation findings had the highest
thoracic injuries included low systolic blood pressure, ele- predictive value for thoracic injury, with a positive likeli-
vated respiratory rate, abnormal results on thoracic exam- hood ratio indicating a large effect on posttest likelihood
ination, abnormal chest auscultation findings, femur frac- of disease. In our study, 35% of patients with pneumotho-
ture, and a GCS score of less than 15. Twelve percent of races and 18% of patients with pulmonary contusions
patients with any one of these factors had thoracic injury had abnormal findings on auscultation of the chest. One
versus 0.6% of patients without any of these risk factors. prior study demonstrated that 46% of children with pul-
Pulmonary contusion was the most prevalent thoracic monary contusions have abnormal findings on chest aus-
injury identified in this population, which is similar to cultation.20
what has been seen in prior studies.1,15-18 After pul- Tachypnea was present in more than half of the patients
monary contusion, pneumothoraces and rib fractures with thoracic injuries when age-adjusted standards were
were the most prevalent injuries in our study population. applied. One prior study reported that more than 90% of
Rib fractures, however, were identified in only 3% of the children with pulmonary contusions have respiratory
Table 3.
Accuracy of clinical findings for predicting chest injury.
Sensitivity, % Specificity, % PPV, % NPV, %
Clinical Findings (95% CI) (95% CI) (95% CI) (95% CI) LR (+) LR (–)
Abnormal chest auscultation findings 14 (7–23) 99 (98–100) 55 (32–77) 93 (91–94) 14.0 0.9
Low systolic blood pressure 14 (7–23) 98 (97–99) 44 (24–65) 93 (91–94) 7.0 0.9
GCS score <15 61 (50–72) 74 (71–77) 17 (13–22) 96 (94–97) 2.3 0.5
Abnormal thoracic examination results 68 (56–78) 64 (60–67) 14 (11–18) 96 (94–97) 1.9 0.5
Elevated respiratory rate 51 (40–63) 84 (81–86) 22 (16–29) 95 (93–97) 3.2 0.6
Femur fracture 13 (6–22) 95 (93–96) 18 (9–30) 92 (91–94) 2.6 0.9
Any of the high-risk criteria* 98 (91–100) 37 (34–40) 12 (10–15) 99 (98–100) 1.6 0.05
PPV, Positive predictive value; NPV, negative predictive value; LR, likelihood ratio.
*
Includes any 1 of the 6 listed variables.
Table 4.
Findings in the 2 patients with thoracic injuries but without any of the high-risk criteria.*
Age, y Injury Method of Diagnosis Additional Clinical Findings Additional Injuries Therapy†
5 Pulmonary contusion and pneumothorax Chest radiograph, abdominal CT scan Developed shortness of Liver laceration Observation
breath in the ED
12 Pulmonary contusion Abdominal CT scan Microscopic hematuria None Observation
*
High-risk criteria included any 1 of the following: low systolic blood pressure, elevated respiratory rate, abnormal thoracic examination results, abnormal chest auscultation findings, femur fracture,
or GCS score of <15.
†
Therapy indicates treatment for the thoracic injury.
MAY 2002 39:5 ANNALS OF EMERGENCY MEDICINE 4 9 7
CLINICAL DECISION RULE FOR PEDIATRIC TRAUMA
Holmes et al
rates of greater than 20 breaths/min, and 46% have respi- have had chest radiography obtained. Thus, only one
ratory rates of greater than 30 breaths/min, although this patient with thoracic injury would have potentially been
study did not adjust respiratory rates for age.20 Because missed. This patient’s injury (pulmonary contusion) was
normal respiratory rates in children vary by age, the not visualized on ED chest radiography and did not re-
assessment and analysis of the respiratory rate should be quire therapy.
age adjusted. Only one prior study has attempted to define indica-
Abnormalities of the thoracic examination had the tions for chest radiography in pediatric patients sustain-
highest sensitivity for identifying thoracic injuries. These ing blunt trauma.23 That study found closed-head injury
abnormalities were present in more than two thirds of and out-of-hospital intubation to be the only predictors
patients with thoracic injuries. Some believe that thoracic of abnormalities on chest radiography.23 The authors rec-
injuries may occur in children without tenderness on ommended obtaining chest radiographs in pediatric
examination of the thorax.2 It is hypothesized that, be- patients who have undergone closed-head injury requir-
cause children’s ribs are more pliable, they may not ing intubation, have undergone smoke inhalation, or
demonstrate external evidence of injury, despite the have sustained blunt thoracic or abdominal trauma.23
application of significant force. Our study also demon- The conclusions of the study, however, may have been
strates that alert children may frequently have thoracic limited by its small size and retrospective data collection.
injuries, despite an apparent lack of chest-wall tenderness. There are several limitations to this study that are wor-
Of the 6 high-risk criteria, a decreased level of con- thy of comment. Although chest radiographs were ob-
sciousness had the second highest sensitivity but the low- tained on all patients, this imaging modality is not per-
est specificity. It is not surprising that patients with a fectly sensitive for identification of all patients with
mechanism of injury resulting in a traumatic brain injury thoracic injuries. Thirty percent to 40% of thoracic injuries
frequently also have experienced sufficient force to the among children are not identified on the initial ED chest
torso to put them at risk for injury to the chest. In addi- radiograph.24-27 Pulmonary contusions, rib fractures,
tion, both children and adults with decreased levels of and pneumothoraces are the most frequent chest injuries
consciousness often have unreliable physical examina- not identified by means of plain radiography.11,24-27 In
tions.2,21,22 In the current study, patients with thoracic our study, many patients did not have further evaluation
injuries and a GCS score of 13 or 14 were significantly less beyond chest radiography, and thus some chest injuries
likely to have thoracic tenderness than injured patients may have gone undetected. Patients discharged from the
with a GCS score of 15. ED, however, had telephone follow-up. Therefore, if
Low systolic blood pressure was also independently injuries were missed, they were likely to be minor. In
associated with thoracic injury and had a positive likeli- addition, only patients undergoing chest radiography
hood ratio indicative of a test with a moderate-to-large were included in this study. It is also possible that some
effect on posttest probability of disease. Hypotension in patients presenting during the study period who did not
the pediatric trauma patient, however, is an infrequent undergo chest radiography had thoracic injuries that
occurrence because children are generally able to main- were never identified. Because these injuries would be
tain normal blood pressures despite significant blood anticipated to be minor and clinically silent, the necessity
loss.2 Hemothoraces, pneumothoraces, and cardiac and of identifying these additional patients is unclear.
aortic injuries are thoracic injures that may cause hypo- We did not assess the presence of hypoxia (and abnor-
tension. A chest radiograph is therefore imperative in the mal pulse oximetry) as a predictor of thoracic injury. Most
hypotensive pediatric trauma patient to rapidly identify children sustaining blunt trauma receive supplemental
such injuries. oxygen during their out-of-hospital evaluation and trans-
Femur fracture was an important predictor in the re- portation. This affects the presence and detection of
cursive partitioning analysis and approached significance hypoxia once evaluated in the ED. Most would agree,
in the logistic regression analysis. The presence of a femur however, that patients who manifest hypoxia should have
fracture implies significant blunt force and causes sub- a chest radiograph obtained.
stantial pain, which might distract the patient from not- The study was conducted at a Level I trauma center,
ing chest pain or tenderness. and many patients had high-force mechanisms of injury.
Two patients with thoracic injuries were not identified Therefore, the results may not be generalizable to all ED
by these criteria; however, 1 patient developed shortness settings. Physicians were requested to complete the data
of breath during ED observation and would therefore sheets as soon as possible after the physical examination
4 9 8 ANNALS OF EMERGENCY MEDICINE 39:5 MAY 2002
CLINICAL DECISION RULE FOR PEDIATRIC TRAUMA
Holmes et al
and before chest radiography. Because of ethical consider- 5. Illif A, Lee VA. Pulse rate, respiratory rate, and body temperature of children between two
months and eighteen years of age. Child Dev. 1952;23:237-245.
ations, however, the treating physicians were likely aware
6. Reilly PL, Simpson DA, Sprod R, et al. Assessing the conscious level in infants and young
of the initial chest radiograph results in a small number of children: a paediatric version of the Glasgow Coma Scale. Childs Nerv Syst. 1988;4:30-33.
patients. These patients who underwent bedside radiog- 7. Garcia VF, Gotschall CS, Eichelberger MR, et al. Rib fractures in children: a marker of
raphy were likely the most severely injured and would severe trauma. J Trauma. 1990;30:695-700.
likely need chest radiography regardless of the physical 8. Brieman L, Friedman JH, Olshen RA, et al. Classification and Regression Trees. Washington,
examination findings. In addition, because of the con- DC: Champan & Hall; 1994.
straints of faculty availability, interrater reliability was not 9. Stiell IG, Wells GA. Methodologic standards for the development of clinical decision rules
in emergency medicine. Ann Emerg Med. 1999;33:437-447.
assessed for physical findings. Finally, although the vari-
10. Altman DG, Andersen PK. Bootstrap investigation of the stability of a cox regression model.
ables identified in these analyses were validated inter- Stat Med. 1989;8:771-783.
nally, external validation is necessary to further assess the 11. Chen CH, George SL. The bootstrap and identification of prognostic factors via Cox’s pro-
generalizability of our findings before specific recom- portional hazards regression model. Stat Med. 1985;4:39-46.
mendations can be made. 12. Efron B, Tibshirani R. Statistical data analysis in the computer age. Science. 1991;253:390-
395.
This study provides information useful to the clinician
13. Harrell FE, Lee KL, Mark DB. Multivariate prognostic models: issues in developing models, eval-
evaluating pediatric patients with blunt trauma. The pre-
uating assumptions and adequacy, and measuring and reducing errors. Stat Med. 1996;15:361-387.
dictive variables identified in this study are clinically
14. Concato J, Feinstein AR, Holford TR. The risk of determining risk with multivariate models.
intuitive and easy to recall. Although these criteria should Ann Intern Med. 1993;118:201-210.
not replace clinical judgment, the identification of these 15. Nakayama DK, Ramenofsky ML, Rowe MI. Chest injuries in childhood. Ann Surg. 1989;210:770-
factors should assist the clinician in managing pediatric 775.
patients who have sustained blunt thoracic trauma. 16. Allen MS, Cox CS. Pulmonary contusion in children: diagnosis and management. South
Med J. 1998;91:1099-1106.
Patients without any of these findings are at very low risk
17. Roux P, Fisher RM. Chest injuries in children: an analysis of 100 cases of blunt chest trauma
for having clinically important thoracic injuries, and from motor vehicle accidents. J Pediatr Surg. 1992;27:551-555.
chest radiography is unlikely to be useful. 18. Smyth BT. Chest trauma in children. J Pediatr Surg. 1979;14:41-47.
In summary, predictors of thoracic injury in pediatric 19. Reilly JP, Brandt ML, Mattox KL, et al. Thoracic trauma in children. J Trauma. 1993;34:329-
patients with blunt trauma include low systolic blood 331.
pressure, elevated respiratory rate, abnormal thoracic 20. Bonadio WA, Hellmich T. Post-traumatic pulmonary contusion in children. Ann Emerg Med.
examination results, abnormal chest auscultation find- 1989;18:1050-1052.
ings, femur fracture, and a GCS score of less than 15. 21. Beaver BL, Colombani PM, Fal A, et al. The efficacy of computed tomography in evaluating
abdominal injuries in children with major head trauma. J Pediatr Surg. 1987;22:1117-1122.
These predictors can be used to derive a sensible and sen-
22. Hoffman JR, Mower WR, Wolfson AB, et al. Validity of a set of clinical criteria to rule out
sitive clinical decision rule. Children with any of these injury to the cervical spine in patients with blunt trauma. N Engl J Med. 2000;343:94-99.
predictors should undergo chest radiography. Children 23. Parish RA, Watson M, Rivara FP. Why obtain arterial blood gases, chest x-rays, and clotting
without any of these predictors have a very low likelihood studies in injured children? Experience in a regional trauma center. Pediatr Emerg Care.
of thoracic injury. 1986;2:218-221.
24. Karaaslan T, Meuli R, Androux R, et al. Traumatic chest lesions in patients with severe
Author contributions: JFH conceived the study. JFH, PES, and NK designed the study. JFH, head trauma: a comparative study with computed tomography and conventional chest
WEB, PES, and NK participated in data collection. WEB participated in radiographic inter- roentgenograms. J Trauma. 1995;39:1081-1086.
pretation. JFH and NK participated in data analysis. JFH and NK participated in manuscript 25. Sivit CJ, Taylor GA, Eichelberger MR. Visceral injury in battered children: a changing per-
preparation and all authors in manuscript revision. All authors take responsibility for the spective. Radiology. 1994;173:559-561.
paper as a whole. 26. McClellan BA, Ali J, Towers MJ, et al. Role of the trauma-room chest x-ray film in assess-
ing the patient with severe blunt traumatic injury. Can J Surg. 1996;39:36-41.
We thank Nicole Glaser, MD, for her critical review and helpful comments on this article. 27. Manson D, Babyn PS, Palder S, et al. CT of blunt chest trauma in children. Pediatr Radiol.
1993;23:1-5.
REFERENCES
1. Cooper A, Barlow B, DiScala C, et al. Mortality and truncal injury: the pediatric perspective.
J Pediatr Surg. 1994;29:33-38.
2. American College of Surgeons. Advanced Trauma Life Support of the American College of
Surgeons: Advanced Trauma Life Support for Doctors. 6th ed. Chicago, IL: American College of
Surgeons; 1997.
3. Gormican SP. CRAMS scale: field triage of trauma victims. Ann Emerg Med. 1982;11:132-135.
4. Task Force on Blood Pressure Control in Children. Report of the Second Task Force on Blood
Pressure Control in Children-1987: National Heart, Lung, and Blood Institute, Bethesda, Maryland.
Pediatrics. 1987;79:1-25.
MAY 2002 39:5 ANNALS OF EMERGENCY MEDICINE 4 9 9
You might also like
- Risk Assessment - Aluminium WorksDocument4 pagesRisk Assessment - Aluminium Worksburak0% (1)
- Activity Hazard AnalysisDocument7 pagesActivity Hazard AnalysisAnthony MacatangayNo ratings yet
- A Comparison of Obstetric Maneuvers For The Acute Management of Shoulder DystociaDocument7 pagesA Comparison of Obstetric Maneuvers For The Acute Management of Shoulder DystociaNellyn Angela HalimNo ratings yet
- Jurnal Diagnostik ADocument8 pagesJurnal Diagnostik AImtina AhdaNo ratings yet
- Out 21Document5 pagesOut 21Noven MezaNo ratings yet
- Prediction of Adverse Cardiac Outcomes in High-Risk Mexican Patients With Chest Pain in The Emergency DepartmentDocument6 pagesPrediction of Adverse Cardiac Outcomes in High-Risk Mexican Patients With Chest Pain in The Emergency Departmentluis sanchezNo ratings yet
- Lally2013 PDFDocument8 pagesLally2013 PDFFebry NurkamilaNo ratings yet
- Achondroplasia Natural History Study (CLARITY)Document7 pagesAchondroplasia Natural History Study (CLARITY)jakelinelagoadvNo ratings yet
- Ferro 2008Document8 pagesFerro 2008Carlos RiquelmeNo ratings yet
- C2 U5 Williams Et Al Critical Care Clinics 2013Document32 pagesC2 U5 Williams Et Al Critical Care Clinics 2013Diego CrucesNo ratings yet
- J Jpedsurg 2008 06 024Document1 pageJ Jpedsurg 2008 06 024afsdsaadsNo ratings yet
- Anesthesia-Pediatric Perioperative Cardiac Arrest Poca RegistryDocument7 pagesAnesthesia-Pediatric Perioperative Cardiac Arrest Poca Registryjcarl_20063003No ratings yet
- Radiol 221926Document9 pagesRadiol 221926Sakkuru Yeyen LiviaNo ratings yet
- Thursday, October 10, 2013 4:10 - 5:10 Concurrent Session: TraumaDocument2 pagesThursday, October 10, 2013 4:10 - 5:10 Concurrent Session: TraumaPeko PekoNo ratings yet
- 1756 0500 6 477 PDFDocument6 pages1756 0500 6 477 PDFanon_118437533No ratings yet
- 1092 0684 Article Pe11Document8 pages1092 0684 Article Pe11Abhilash VemulaNo ratings yet
- Asensio, JA, (2020) - Tratamiento Quirúrgico de Las Lesiones de La Arteria Braquial y Predictores de Resultado.Document12 pagesAsensio, JA, (2020) - Tratamiento Quirúrgico de Las Lesiones de La Arteria Braquial y Predictores de Resultado.Edgar Geovanny Cardenas FigueroaNo ratings yet
- HydrocephalusDocument8 pagesHydrocephaluscaliptra36No ratings yet
- Accuracy of Trauma Ultrasound in Major Pelvic InjuryDocument5 pagesAccuracy of Trauma Ultrasound in Major Pelvic InjuryEvelyn GrandaNo ratings yet
- Ucm 439476Document1 pageUcm 439476Fadel BilondatuNo ratings yet
- Flaherty 2016Document6 pagesFlaherty 2016Diornald MogiNo ratings yet
- Fried Frailty Pred Surg Outcomes AmCSurg 10Document8 pagesFried Frailty Pred Surg Outcomes AmCSurg 10edos838No ratings yet
- HSDC CBC 2015Document5 pagesHSDC CBC 2015Bob sponjaNo ratings yet
- Cost and Outcomes of Assessing Patients With Chest Pain in An Australian Emergency DepartmentDocument7 pagesCost and Outcomes of Assessing Patients With Chest Pain in An Australian Emergency DepartmentPeter ThaiNo ratings yet
- Clinical Findings and Diagnostic Value of Post-Traumatic Thoracic Radiographs in Dogs and Cats With Blunt TraumaDocument10 pagesClinical Findings and Diagnostic Value of Post-Traumatic Thoracic Radiographs in Dogs and Cats With Blunt TraumaAna CicadaNo ratings yet
- WTACritical Decisions Management of Rib FracturesDocument4 pagesWTACritical Decisions Management of Rib FracturesToàn NguyễnNo ratings yet
- Long-Term Outcomes After Surgical Treatment of Pediatric Neurogenic Thoracic Outlet SyndromeDocument11 pagesLong-Term Outcomes After Surgical Treatment of Pediatric Neurogenic Thoracic Outlet Syndromewalter fire 0057No ratings yet
- 564 Full PDFDocument7 pages564 Full PDFMi MihaelaNo ratings yet
- NEXUS Chest Validation of A Decision Instrument For Selective Chest Imaging in Blunt TraumaDocument7 pagesNEXUS Chest Validation of A Decision Instrument For Selective Chest Imaging in Blunt TraumaAnastasia EkaNo ratings yet
- Marshall1991 The Outcome of Severe Closed Head InjuryDocument9 pagesMarshall1991 The Outcome of Severe Closed Head InjuryJulieta PereyraNo ratings yet
- Bossi - Echocardiogric EvaluationDocument8 pagesBossi - Echocardiogric EvaluationSzendeNo ratings yet
- Berg 2012Document7 pagesBerg 2012Mario Espinosa GamezNo ratings yet
- Use of The Skeletal Survey in The Evaluation of Child MaltreatmentDocument3 pagesUse of The Skeletal Survey in The Evaluation of Child MaltreatmentAprilia DhammashintaNo ratings yet
- Chest Trauma in Athletic Medicine - Article.Document7 pagesChest Trauma in Athletic Medicine - Article.salmankhan09215No ratings yet
- Elkhunovich2016 The Utility of Cranial Ultrasound For Detection of IntracranialDocument6 pagesElkhunovich2016 The Utility of Cranial Ultrasound For Detection of IntracranialModou NianeNo ratings yet
- Cervical Spine Clearance 2009Document7 pagesCervical Spine Clearance 2009Abdulelah Al.luhaybiNo ratings yet
- ANGHELESCU Et Al Clinical and Diagnostic Imaging Findings Predict Anesthetic Complications in Children With Malignant MMDocument9 pagesANGHELESCU Et Al Clinical and Diagnostic Imaging Findings Predict Anesthetic Complications in Children With Malignant MMJill SweetNo ratings yet
- Clearing The Cervical Spine of Adult Victims of TraumaDocument7 pagesClearing The Cervical Spine of Adult Victims of TraumaVince AzevoucheNo ratings yet
- Femur Fractures Should Not Be Considered Distracting Injuries For CervicalDocument6 pagesFemur Fractures Should Not Be Considered Distracting Injuries For CervicalnellyNo ratings yet
- Evaluation of Chest Pain in Primary Care Patients-AAFPDocument3 pagesEvaluation of Chest Pain in Primary Care Patients-AAFPnouval_iqbalNo ratings yet
- Complications Predicting Perioperative Mortality in Patients Undergoing Elective Craniotomy A Population Based StudyDocument11 pagesComplications Predicting Perioperative Mortality in Patients Undergoing Elective Craniotomy A Population Based Study49hr84j7spNo ratings yet
- Cervical Angiograms in Cervical Spine Trauma Patients 5 Years After The Data: Has Practice Changed?Document4 pagesCervical Angiograms in Cervical Spine Trauma Patients 5 Years After The Data: Has Practice Changed?edi_wsNo ratings yet
- Research: CATCH: A Clinical Decision Rule For The Use of Computed Tomography in Children With Minor Head InjuryDocument8 pagesResearch: CATCH: A Clinical Decision Rule For The Use of Computed Tomography in Children With Minor Head InjuryCarlos Martin Yafac RiscoNo ratings yet
- NASCETDocument9 pagesNASCETektosNo ratings yet
- Conference Paper: Rapid Physical Assessment of The Injured ChildDocument4 pagesConference Paper: Rapid Physical Assessment of The Injured ChildMaiush JbNo ratings yet
- (10920684 - Neurosurgical Focus) Predictors of Outcome of Subdural Empyema in ChildrenDocument6 pages(10920684 - Neurosurgical Focus) Predictors of Outcome of Subdural Empyema in ChildrenFatima RamirezNo ratings yet
- Trauma Medular - Cervical Trauma ColumnaDocument28 pagesTrauma Medular - Cervical Trauma ColumnayustinjulianavNo ratings yet
- Ajr 09 2544Document7 pagesAjr 09 2544Elly LutfiasariNo ratings yet
- Nejmoa 2026141Document14 pagesNejmoa 2026141Matheus FelipeNo ratings yet
- Timing of Cranioplasty After Decompressive Craniectomy ForDocument5 pagesTiming of Cranioplasty After Decompressive Craniectomy ForjoerizalNo ratings yet
- Nestelberger Et Al 2019 Predicting Major Adverse Events in Patients With Acute Myocardial InfarctionDocument13 pagesNestelberger Et Al 2019 Predicting Major Adverse Events in Patients With Acute Myocardial InfarctionNJEBARIKANUYE EugèneNo ratings yet
- Ultrasonido Doppler Temprano AMSDocument7 pagesUltrasonido Doppler Temprano AMSKaren Marbelly OrozcoNo ratings yet
- 1 s2.0 S0735109720344223 MainDocument12 pages1 s2.0 S0735109720344223 MainRizky AisNo ratings yet
- The Impact of Obesity On Severely Injured Children and AdolescentsDocument4 pagesThe Impact of Obesity On Severely Injured Children and AdolescentsUswatun HasanahNo ratings yet
- Early Predictors of Mortality in HemodynamicallyDocument7 pagesEarly Predictors of Mortality in HemodynamicallytesfahuntekletilahunNo ratings yet
- Emergency Medical Services Intervals and Survival in Trauma: Assessment of The "Golden Hour" in A North American Prospective CohortDocument16 pagesEmergency Medical Services Intervals and Survival in Trauma: Assessment of The "Golden Hour" in A North American Prospective CohortrutnomleniNo ratings yet
- World Neurosurg 2021 Apr 2 Camino-Willhuber GDocument6 pagesWorld Neurosurg 2021 Apr 2 Camino-Willhuber GFernando SousaNo ratings yet
- Abdominal Ultrasound Is An Unreliable Modality For The Detection of Hemoperitoneum in Patients With Pelvic FractureDocument6 pagesAbdominal Ultrasound Is An Unreliable Modality For The Detection of Hemoperitoneum in Patients With Pelvic FractureEvelyn GrandaNo ratings yet
- 2003-Academic Emergency MedicineDocument154 pages2003-Academic Emergency MedicinealiceNo ratings yet
- Proceedings of The 2014 Spring Meeting of The Society of British 2014Document40 pagesProceedings of The 2014 Spring Meeting of The Society of British 2014rabiatul adawiyahNo ratings yet
- Posterior Fossa Epidural Hematomas in CHDocument5 pagesPosterior Fossa Epidural Hematomas in CHmirmasottNo ratings yet
- Office Based Anesthesia Complications: Prevention, Recognition and ManagementFrom EverandOffice Based Anesthesia Complications: Prevention, Recognition and ManagementGary F. BoulouxNo ratings yet
- First Aid in Electric ShockDocument2 pagesFirst Aid in Electric ShockLevin ChespedinNo ratings yet
- SOPs Handling First AidDocument2 pagesSOPs Handling First AidsridharNo ratings yet
- CPM Question Bank With SolutionDocument78 pagesCPM Question Bank With SolutionDevansh RaiNo ratings yet
- Learner Guide SITXWHS005 - Participate in Safe Work PracticesDocument32 pagesLearner Guide SITXWHS005 - Participate in Safe Work PracticessalazarayieNo ratings yet
- Hazard Identification and ControlDocument93 pagesHazard Identification and ControlMarwa MohammadNo ratings yet
- Grafik Kecelakaan 2016 PDFDocument2 pagesGrafik Kecelakaan 2016 PDFragilNo ratings yet
- Analyzing Construction Site Accidents in KuwaitDocument28 pagesAnalyzing Construction Site Accidents in Kuwaitzeyad alsaroriNo ratings yet
- Online National Electronic Injury Surveillance System (ONEISS) FactsheetDocument14 pagesOnline National Electronic Injury Surveillance System (ONEISS) FactsheetOliVerNo ratings yet
- HSE Presentation On Supervisors Training HseprofDocument31 pagesHSE Presentation On Supervisors Training HseprofGavin VassellNo ratings yet
- Pubmed InjuryORkn SetDocument392 pagesPubmed InjuryORkn SetLucas de BritoNo ratings yet
- Daftar PustakaDocument2 pagesDaftar PustakaNurul Safiah SuhaimiNo ratings yet
- Occupational Accidents and InjuryDocument43 pagesOccupational Accidents and InjuryAnam FatimaNo ratings yet
- Knee ExercisesDocument4 pagesKnee ExercisesRaj PhysioNo ratings yet
- HIRA - Fixed Scaffold and Wall BreakingDocument6 pagesHIRA - Fixed Scaffold and Wall BreakingSujan Augustin100% (2)
- Proper TypingDocument19 pagesProper Typingmary glorNo ratings yet
- Awareness of Injury Prevention 1Document11 pagesAwareness of Injury Prevention 1Avegaile PaduaNo ratings yet
- Trauma Alert Criteria Brevard County Fire Rescue Trauma Alert Criteria Brevard County Fire RescueDocument3 pagesTrauma Alert Criteria Brevard County Fire Rescue Trauma Alert Criteria Brevard County Fire Rescueshaun shepherdNo ratings yet
- Toolbox Talks: Hand Tool SafetyDocument1 pageToolbox Talks: Hand Tool Safetyserdar yücelNo ratings yet
- Effects of Nordic Hamstring Exercise On Hamstring InjuriesDocument10 pagesEffects of Nordic Hamstring Exercise On Hamstring InjuriesArathyNo ratings yet
- HSE Report-Plastering-439Document5 pagesHSE Report-Plastering-439jameelNo ratings yet
- JSA Additional Lamp Paiton 3Document10 pagesJSA Additional Lamp Paiton 3MarhendraNo ratings yet
- 2008 07 What Is Process SafetyDocument1 page2008 07 What Is Process SafetyYuda HerdiantoNo ratings yet
- Nervous System Head InjuryDocument11 pagesNervous System Head InjurydimlyNo ratings yet
- Final Thesis (Dr. Neeraj)Document79 pagesFinal Thesis (Dr. Neeraj)Prosenjit BhowalNo ratings yet
- Sports Medical History FormDocument2 pagesSports Medical History Formgilikarn9960No ratings yet
- 3 - Unsafe Unhealthy Acts ConditionsDocument18 pages3 - Unsafe Unhealthy Acts ConditionsAchilles SantiagoNo ratings yet
- HIRADC - 001 - Survey WorkDocument3 pagesHIRADC - 001 - Survey WorkZhafri SyazwiNo ratings yet
- Montrell Jolly Probable CauseDocument3 pagesMontrell Jolly Probable CauseLeigh EganNo ratings yet