Professional Documents
Culture Documents
Concept Map Templatef21
Concept Map Templatef21
Uploaded by
api-741272284Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Concept Map Templatef21
Concept Map Templatef21
Uploaded by
api-741272284Copyright:
Available Formats
1
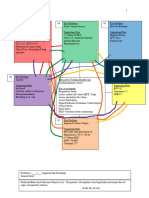
Step 2. Support problems with clinical patient data, including abnormal physical
assessment findings, treatments, medications, and IV’s, abnormal diagnostic and lab Data don’t
tests, medical history, emotional state and pain. Also, identify key assessments that are know where
related to the reason for health care (chief medical diagnosis/surgical procedure) and put to put in
boxes:
these in the central box. If you do not know what box to put data in, then put it off to the
side of the map.
#1 Key Problem/ND #2 Key Problems/ND #3 Key Problem/ND
Impaired gas exchange Risk for decreased tissue Deficient Fluid Volume
SOB perfusion hypotension
4L NC Fluid loss from surgery Recent fluid loss
CAD Hx of CAD, DM2 from Open Heart
DM 2 Hypotension 2L of NS
Diminished lung sounds Arterial line 500ml of Albumin
Pressors pressors
2.5L of fluids bolused
# Key Problem/ND:
#4 Key Problem/ND
Risk for blood clots
Pneumatic
Reason For Needing Health Care Compression device
in use
NSTEMI + CABG x 3 “Blood Thinners,”
like Plavix and
Aspirin
Patient immobile for
long stretch of time
Post-Op patient
# Key Problem/ND #6 Key Problem/ND #5 Key Problem/ND
Risk for Infection Risk for bleeding
Open Heart Surgery “Blood Thinners”
Prophylactic antibiotics CABG x 3
Indwelling Catheter 4 Chest tubes
Incisions on legs for
veins
Step 3: Draw lines between related problems. Number boxes as you prioritize problems.
P. Schuster, Concept Mapping: A Critical Thinking Approach, Davis, 2002.
2
LASTLY- label the problem with a nursing diagnosis.
Step 4: Identification of goals, outcomes and interventions.
Step 5: Evaluation of Outcomes
Problem # 1: Impaired Gas Exchange
General Goal: Patient’s 02 Sat will remain above 90%
Predicted Behavioral Outcome Objective (s): The patient will not feel SOB or show any signs of respiratory
distress.
on the day of care.
Nursing Interventions Patient Responses
1. 4L of 02 on NC 1. Pt SAT remained above 90%
2. Continuous O2 monitoring 2. Pt showed good oxygenation.
3. High fowlers positioning 3. Patient’s breathing improved.
4. Swallow test post extubation 4. Airway protected.
5. Patient taught how to cough. 5. Pt able to remove secretions.
6. ABG 6. PaO2 125.4 at 15:10
7. 7.
8. 8.
Evaluation of outcome objectives: Patient’s breathing was symmetrical and unlabored with a normal RR.
Outcome Met
Problem # 2: Risk for decreased tissue perfusion
General Goal: MAP > 65 and Capillary refill < 3 seconds
Predicted Behavioral Outcome Objective (s): The patient will respond and tolerate interventions well
on the day of care.
Nursing Interventions Patient Responses
1. Give bolus as needed 1. Patients’ blood pressure went up.
2. Titrate Vasopressin drip 2. MAP remained > 65
3. Blood thinners provided 3. No S&S of blood clots
4. Catheter and chest tubes 4. Able to accurately I&O’s
5. Monitor cap refill 5. < 3 sec in all extremities
6. Administer Tamsulosin 6. Helped afterload on the Heart
7. 7.
8. 8.
Evaluation of outcome objectives: Capillary refill remained less than three seconds, BP stabilized along with
MAP (which was greater than 65). Able to start weaning patient off vasopressin. Outcome Met
Problem #3: Deficient fluid volume r/t intra operative procedure
General Goal: Patient’s blood pressure will stabilize SBP >90
P. Schuster, Concept Mapping: A Critical Thinking Approach, Davis, 2002.
3
Predicted Behavioral Outcome Objective (s): The patient will remain calm and cooperative
on the day of care.
Nursing Interventions Patient Responses
9. 2.5L worth of fluids bolused 9. Patients BP went up.
10. Taught to brace when coughing. 10. Minimized BP drops
11. 25g of Albumin 11. Help keep fluid in right place
12. Vasopressin 0.04u/min 12. Helped stabilize BP
13. Monitor chest tubes 13. No excessive blood loss
14. Administer Tamsulosin 14. Helped afterload on heart
15. 15.
16. 16.
Evaluation of outcome objectives: Patients blood pressure rose above 110 SBP and we were able to titrate off
Vasopressin. No excessive blood loss through chest tubes. Outcome Met.
Problem # 4: Risk for blood clots
General Goal: No S&S of blood clots
Predicted Behavioral Outcome Objective (s): The patient will be calm and cooperative
on the day of care.
Nursing Interventions Patient Responses
1. Pneumatic compression device 1. No S&S of blood clot in right leg
2. Administer 75mg Clopidogrel 2.No Adverse reactions
3. Education on incentive spirometer 3. Patient was cooperative
4. Administer baby Aspirin 4. No adverse reactions
5. Check pulses in lower extremities 5. Pedal Pulse +1 BL
6. ACE wrap on left leg 6. Compressed to help blood flow
7. 7.
8. 8.
Evaluation of outcome objectives: Patient showed no signs or symptoms of a thrombus. Outcome Met.
Step 3: Draw lines between related problems. Number boxes as you prioritize problems.
LASTLY- label the problem with a nursing diagnosis.
Step 4: Identification of goals, outcomes and interventions.
Step 5: Evaluation of Outcomes
Problem # 5: Risk for Bleeding
General Goal: No excessive Blood loss
P. Schuster, Concept Mapping: A Critical Thinking Approach, Davis, 2002.
4
Predicted Behavioral Outcome Objective (s): The patient will remain calm and cooperative
on the day of care.
Nursing Interventions Patient Responses
17. Monitor for S&S of bleeding. 17. No S&S of abnormal bleeding
18. Check dressings. 18. Dressings Dry and Intact
19. Monitor chest tubes 19. No excessive blood loss
20. Educate patient on safety 20. Unable to educate pt d/t sedatives
21. Patient restrained for safety 21. Pt didn’t fight the restraints
22. Monitor BP and HR 22. HR stable (60-100), low BP
23. 23.
24. 24.
Evaluation of outcome objectives: Patient had a normal amount of drainage from the chest tubes. No signs of
bleeding anywhere else. Outcome Met
Problem # 6: Risk for infection
General Goal: No S&S of infection.
Predicted Behavioral Outcome Objective (s): The patient will remain calm and cooperative
on the day of care.
Nursing Interventions Patient Responses
1. Interval temperature checks 1. Highest temp 99.9
2. check drainage on chest tubes. 2. No abnormal appearance
3. Check temperature around sites 3. Consistent with body temperature
4. Administer prophylactic Antibiotics 4. No Adverse side effects.
5. Check incision sites 5. Unable to assess.
6. Monitor Labs 6. Last WBC 7.5
7. 7.
8. 8.
Evaluation of outcome objectives: Some surgical sites we were UTA, no abnormal drainage or wounds on
what we could see. Outcome partially met.
P. Schuster, Concept Mapping: A Critical Thinking Approach, Davis, 2002.
You might also like
- Oculofacial Plastic and Reconstructive SurgeryDocument562 pagesOculofacial Plastic and Reconstructive SurgeryGimena Dapena100% (5)
- Nursing Care Plan For HypertensionDocument5 pagesNursing Care Plan For Hypertensionmariejo89% (84)
- Grand Osce ReviewerDocument16 pagesGrand Osce ReviewerBA Ong100% (1)
- Nursing Care Plan and Drug Study: University of Cebu - Banilad Campus Banilad, Cebu City College of NursingDocument16 pagesNursing Care Plan and Drug Study: University of Cebu - Banilad Campus Banilad, Cebu City College of NursingVinz OñoNo ratings yet
- CC Concept MapDocument11 pagesCC Concept Mapapi-546355187No ratings yet
- Clinical Replacement Student Packet-3Document12 pagesClinical Replacement Student Packet-3ida100% (1)
- Nursing Care Plan For HypertensionDocument5 pagesNursing Care Plan For HypertensionJessy MalloNo ratings yet
- Chapter 032Document22 pagesChapter 032dtheart2821100% (1)
- Sheila Dalton Case Study-1Document4 pagesSheila Dalton Case Study-1tommy0% (7)
- Nursing Care Plan - Post-OpDocument2 pagesNursing Care Plan - Post-OpKismet Summons88% (8)
- Concept Map Critical CareDocument5 pagesConcept Map Critical Careapi-546401036No ratings yet
- Ashley Wolanzyk Concept MapDocument5 pagesAshley Wolanzyk Concept Mapapi-455796674No ratings yet
- Assessment and Concept Map Care Plan For Critical Care PatientDocument11 pagesAssessment and Concept Map Care Plan For Critical Care Patientapi-546697029No ratings yet
- Concept Map FinalDocument5 pagesConcept Map Finalapi-545001894No ratings yet
- Brooke Baker Concept Map 4840 Complex Care: P. Schuster, Concept Mapping: A Critical Thinking Approach, Davis, 2002Document10 pagesBrooke Baker Concept Map 4840 Complex Care: P. Schuster, Concept Mapping: A Critical Thinking Approach, Davis, 2002api-546799391No ratings yet
- Clinical Judgment Plan of Care Long FormDocument12 pagesClinical Judgment Plan of Care Long Formapi-699835864No ratings yet
- Assessment and Concept Map Care Plan For Critical Care PatientDocument8 pagesAssessment and Concept Map Care Plan For Critical Care Patientapi-593853954No ratings yet
- Critical Care Concept Map Template Final 2Document6 pagesCritical Care Concept Map Template Final 2api-740444719No ratings yet
- Concept Map Part LLDocument5 pagesConcept Map Part LLapi-663568963No ratings yet
- Risk NCP Decreased Cardiac OutputDocument2 pagesRisk NCP Decreased Cardiac OutputMICHELLE FACTONo ratings yet
- Concept MapDocument5 pagesConcept Mapapi-546509005No ratings yet
- Heath Day 4 Care Plan 3Document12 pagesHeath Day 4 Care Plan 3api-639508852No ratings yet
- CHF Cardiomegaly Volume OverloadDocument1 pageCHF Cardiomegaly Volume Overloadnursing concept mapsNo ratings yet
- NCP FormatDocument4 pagesNCP FormatCoreen Kaye TanNo ratings yet
- BradycardiaDocument8 pagesBradycardialetonierNo ratings yet
- Jerash University Faculty of Nursing Critical Care Nursing Practicum Case StudyDocument9 pagesJerash University Faculty of Nursing Critical Care Nursing Practicum Case StudytasneemNo ratings yet
- Complex Care Clinical Concept Map Sara Ciletti Youngstown State UniversityDocument9 pagesComplex Care Clinical Concept Map Sara Ciletti Youngstown State Universityapi-590353096No ratings yet
- Concept Map Final Copy1Document7 pagesConcept Map Final Copy1api-608271845No ratings yet
- Concept Map Critical CareDocument6 pagesConcept Map Critical Careapi-498759347No ratings yet
- Prioritization Delegation and Assignment 3Rd Edition Lacharity Solutions Manual Full Chapter PDFDocument25 pagesPrioritization Delegation and Assignment 3Rd Edition Lacharity Solutions Manual Full Chapter PDFEarlCollinsmapcs100% (11)
- Concept Map Format For CLADocument41 pagesConcept Map Format For CLAAdellaine Lois GreyNo ratings yet
- Clinical Evaluation ReportDocument14 pagesClinical Evaluation ReportGavrila VeronicaNo ratings yet
- Concept Map CompletedDocument5 pagesConcept Map Completedapi-730811728No ratings yet
- Concept Map CCDocument4 pagesConcept Map CCapi-738778945No ratings yet
- (Download PDF) Prioritization Delegation and Assignment 3rd Edition LaCharity Solutions Manual Full ChapterDocument27 pages(Download PDF) Prioritization Delegation and Assignment 3rd Edition LaCharity Solutions Manual Full Chapterroychepachii100% (5)
- 4832 Concept MapDocument9 pages4832 Concept Mapapi-663135887No ratings yet
- Episode 163 Acute Heart Failure Part 1Document8 pagesEpisode 163 Acute Heart Failure Part 1Dk YadavNo ratings yet
- Heart Failure (Congestive Heart Failure) FINALDocument6 pagesHeart Failure (Congestive Heart Failure) FINALKristian Karl Bautista Kiw-isNo ratings yet
- Concept Map Part LLDocument5 pagesConcept Map Part LLapi-662892413No ratings yet
- Concept Map Critical CareDocument6 pagesConcept Map Critical Careapi-508559825No ratings yet
- Jose Martinez Care PlanDocument7 pagesJose Martinez Care PlanJulia BrownNo ratings yet
- 2022 Care PlanDocument8 pages2022 Care Planapi-601587526No ratings yet
- ArrestDocument9 pagesArrestBimaIndraNo ratings yet
- Rizki Yani Askep GadarDocument8 pagesRizki Yani Askep Gadarashfiana wirdhiaNo ratings yet
- Shock and Inotropes With DR Sumesh AroraDocument54 pagesShock and Inotropes With DR Sumesh AroraAhmed AhmedNo ratings yet
- Concept Map PedsDocument6 pagesConcept Map Pedsapi-498759347No ratings yet
- Nursing Care Plan For HypertensionDocument3 pagesNursing Care Plan For HypertensionFranco Razon100% (2)
- Concept Map Template - Andreanna TocickiDocument5 pagesConcept Map Template - Andreanna Tocickiapi-741174198No ratings yet
- Concept Map f21 FinishedDocument5 pagesConcept Map f21 Finishedapi-601070065No ratings yet
- Pre-Operative Assessment Study Guide REVISED: 2018: Created By: Edited By: Dr. Chris Young June 2018Document30 pagesPre-Operative Assessment Study Guide REVISED: 2018: Created By: Edited By: Dr. Chris Young June 2018Navdeep RandhawaNo ratings yet
- CC Concept MapDocument6 pagesCC Concept Mapapi-741058487No ratings yet
- Med-Surg - Cardiovascular Review Questions Flashcards - QuizletDocument26 pagesMed-Surg - Cardiovascular Review Questions Flashcards - QuizletBenjamin EspinosaNo ratings yet
- PGDT Protocol Summary ReferenceDocument32 pagesPGDT Protocol Summary Referenceghg sddNo ratings yet
- Hurst - Content Review - Cardio (Edit)Document8 pagesHurst - Content Review - Cardio (Edit)Elaine NorbergNo ratings yet
- Heart of the Field "Refresher & Nha Certification Quick Notes"From EverandHeart of the Field "Refresher & Nha Certification Quick Notes"No ratings yet
- Respiratory Therapy: 66 Test Questions Student Respiratory Therapists Get Wrong Every Time: (Volume 2 of 2): Now You Don't Have Too!: Respiratory Therapy Board Exam Preparation, #2From EverandRespiratory Therapy: 66 Test Questions Student Respiratory Therapists Get Wrong Every Time: (Volume 2 of 2): Now You Don't Have Too!: Respiratory Therapy Board Exam Preparation, #2No ratings yet
- Labs & Imaging for Primary Eye Care: Optometry In Full ScopeFrom EverandLabs & Imaging for Primary Eye Care: Optometry In Full ScopeNo ratings yet
- Respiratory Therapy: 66 Test Questions Student Respiratory Therapists Get Wrong Every Time: (Volume 1 of 2): Now You Don't Have Too!: Respiratory Therapy Board Exam Preparation, #1From EverandRespiratory Therapy: 66 Test Questions Student Respiratory Therapists Get Wrong Every Time: (Volume 1 of 2): Now You Don't Have Too!: Respiratory Therapy Board Exam Preparation, #1No ratings yet
- Intubating the Critically Ill Patient: A Step-by-Step Guide for Success in the ED and ICUFrom EverandIntubating the Critically Ill Patient: A Step-by-Step Guide for Success in the ED and ICURachel GarvinNo ratings yet
- Nursing Mnemonics: The Ultimate Tips and Notes For NursesFrom EverandNursing Mnemonics: The Ultimate Tips and Notes For NursesRating: 5 out of 5 stars5/5 (1)
- English Project - Boomer YearsDocument14 pagesEnglish Project - Boomer YearsGushyNo ratings yet
- Mental Illness Rehabilition Center and HospitalDocument12 pagesMental Illness Rehabilition Center and HospitalJaspergroup 15100% (1)
- Hudak DevelopmentofanUpperExtremityOutcomeMeasure-DASHDocument10 pagesHudak DevelopmentofanUpperExtremityOutcomeMeasure-DASHRossana CustodioNo ratings yet
- Synovial Sarcoma in Head and Neck: A Case ReportDocument3 pagesSynovial Sarcoma in Head and Neck: A Case ReportFabian Camelo OtorrinoNo ratings yet
- Critical Care, 136-145.: Daftar PustakaDocument4 pagesCritical Care, 136-145.: Daftar PustakaFirwanNo ratings yet
- CT Scan Request 2nd PageDocument1 pageCT Scan Request 2nd PageAina HaravataNo ratings yet
- Quality of Vision (Essential Optics)Document142 pagesQuality of Vision (Essential Optics)SmaraNo ratings yet
- Functional Outcome Analysis of Tibia Fracture Managed by Tens Nailing in Paediatric Age GroupDocument15 pagesFunctional Outcome Analysis of Tibia Fracture Managed by Tens Nailing in Paediatric Age GroupSenthil RajaNo ratings yet
- Uterine Prolapsed: By. Pn. MurtiningsihDocument18 pagesUterine Prolapsed: By. Pn. MurtiningsihraiNo ratings yet
- Sample PRC Form: Minor CasesDocument1 pageSample PRC Form: Minor Casespertru08No ratings yet
- 6 Cutaneous Amalgam Tattoo in A Dental ProfessionalDocument2 pages6 Cutaneous Amalgam Tattoo in A Dental ProfessionalleilyanisariNo ratings yet
- Passy-Muir Valves, Accessories, & Connections GuideDocument2 pagesPassy-Muir Valves, Accessories, & Connections GuideCristian AcostaNo ratings yet
- Perminant Exam (١)Document170 pagesPerminant Exam (١)Larina MohammedNo ratings yet
- SBNS Neurological UnitsDocument8 pagesSBNS Neurological UnitsparapooNo ratings yet
- PERIOPERATIVE NURSING CARE - MacatangayDocument2 pagesPERIOPERATIVE NURSING CARE - MacatangayGaea AngelaNo ratings yet
- Lip SupportDocument9 pagesLip SupportFrancisco Antonio Vargas GuevaraNo ratings yet
- Aidaa IcuDocument9 pagesAidaa IcuebmkrNo ratings yet
- Prostho Short NotesDocument84 pagesProstho Short Notessamiksha100% (1)
- SPINE Supplement April 2017 PDFDocument33 pagesSPINE Supplement April 2017 PDFGuna KalanjiyamNo ratings yet
- Fractional CO2Document4 pagesFractional CO2Rahul Pillai100% (1)
- Rehabilitation Versus Surgical Reconstruction For Non-Acute Anterior Cruciate Ligament InjuryDocument11 pagesRehabilitation Versus Surgical Reconstruction For Non-Acute Anterior Cruciate Ligament InjuryJesusNavarrete97No ratings yet
- Advanced Arthroscopy of The Temporomandibular JointDocument23 pagesAdvanced Arthroscopy of The Temporomandibular JointRaphaela TravassosNo ratings yet
- Bontilao V.Gerona GR No. 176675 September 15, 2010 FactsDocument2 pagesBontilao V.Gerona GR No. 176675 September 15, 2010 Factserxha ladoNo ratings yet
- Consumer Protection Act in HealthcareDocument23 pagesConsumer Protection Act in HealthcarePradeeba ChinnaduraiNo ratings yet
- Comparison of Different Kinesio Taping Techniques Following Third Molar SurgeryDocument10 pagesComparison of Different Kinesio Taping Techniques Following Third Molar SurgerygreynerNo ratings yet
- Pyloric Stenosis: CLASS:-B.Sc. Nursing 3 YearDocument38 pagesPyloric Stenosis: CLASS:-B.Sc. Nursing 3 Yearshikha100% (2)
- Perception and Awareness of Oral and Maxillofacial Surgery Speciality Among Medical Postgraduate TraineesDocument5 pagesPerception and Awareness of Oral and Maxillofacial Surgery Speciality Among Medical Postgraduate TraineesAmadea EmanuelaNo ratings yet
- Appendicitis: Prof E. C. Ohanaka Consultant SurgeonDocument17 pagesAppendicitis: Prof E. C. Ohanaka Consultant SurgeonTaylorNo ratings yet