Professional Documents
Culture Documents
Surgical Removal of Moles
Surgical Removal of Moles
Uploaded by
kahkashanahmed065Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Surgical Removal of Moles
Surgical Removal of Moles
Uploaded by
kahkashanahmed065Copyright:
Available Formats
www.cosmoderma.
org
CosmoDerma
Focus
Surgical removal of moles
Rashi Pangti1, Somesh Gupta1
Department of Dermatology and Venereology, All India Institute of Medical Sciences, New Delhi, India.
1
Melanocytic nevi are the common benign proliferation of melanocytes. These can be congenital
or acquired. Acquired melanocytic nevi, also known as moles, appear from childhood to usually
midlife, are present in all races, and are more in number in the white population.
Moles can be classified based on the depth at which the melanocytic nevus cells or
*Corresponding author: nevomelanocytes are present. Single nevus cells in the basal layer with nests of nevus cells
Dr. Somesh Gupta, are present in the tips of rete ridges or between them, in the case of junctional nevus. In
Professor, Department of addition to the junctional component, compound nevus has nevomelanocytes in the dermis,
Dermatology and Venereology, arranged as nests, cords, or single units. Intradermal nevus has only the dermal component
All India Institute of Medical of the compound nevus. As melanocytes move from the epidermis to the dermis, they
Sciences, New Delhi, India. gradually lose their ability to produce pigment. Junctional nevus presents as a flat, pigmented
someshgupta@hotmail.com brown macule while a compound nevus is a slightly raised, brown papule with the color of
the brown ranging from light to dark according to the individual’s skin color. Intradermal
Received : 06 July 2021 nevi present as skin-colored, dome-shaped papule or nodule with hair projecting from the
Accepted : 07 July 2021 surface at times.[1]
Published : 19 July 2021
The diagnosis of moles is usually made on clinical morphology. In instances, when doubt arises
regarding the diagnosis, dermoscopy, and reflectance confocal microscopy are of added value
DOI
10.25259/CSDM_32_2021 in the diagnosis as they are non-invasive modalities. However, histopathology remains the gold
standard for confirmation. All excised specimens should be sent for histopathology as a rule of
Quick Response Code: thumb.
These moles, in common layman language, referred to as beauty spots or marks; however, when
large or located on cosmetically sensitive sites, such as on nose, may cause cosmetic concern to
patients.
Some other skin lesions sometimes may mimic melanocytic nevi. These include dysplastic nevi,
pigmented basal cell carcinoma, seborrheic keratosis, and melanoma. In this review, we shall
focus on the surgical removal of moles by various surgical methods, the reason of which is mostly
cosmetic in nature or at times repeated trauma to them. Thus, its removal comes with the given
proposition of cosmetic excellence.
SHAVE EXCISION
It is commonly used for the removal of small junctional or compound nevi. The steps of shave
excision are as follows.
is is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others
to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
©2021 Published by Scientific Scholar on behalf of Cosmo Derma
Cosmoderma 2021 • 1(27) | 1
Pangti and Gupta: Removal of moles
After the cleaning and draping of the mole to be removed, significant advantage is that a completely excised lesion can
first, the skin around the mole is stretched between the be sent for histopathology. If suspicion of any dysplasia, an
forefinger and the middle finger in a direction perpendicular incision with full depth of the dermis and 2 mm margins is
to the relaxed skin tension lines (RSTLs). Infiltrative local desirable.[7]
anesthesia is given into and around the lesion. This gives a In a trial comparing the sutured elliptical excision with
slight elevation to the lesion, which facilitates the procedure shave excision of intradermal moles, it was seen that the
of shave excision. Now, a surgical blade numbered 11 or 15 average scar size at 6 months after shave excision was much
attached to the Bard-Parker scalpel number 3, held parallel lesser than after elliptical excision (P < 0.05). However,
to the surface of the skin, in a horizontal motion is swept 28.6% of patients who had undergone shave excision had
across through the part of the mole projecting above the recurrence vis-à-vis none of the patients in the elliptical
surrounding skin surface.[2] Instead of a surgical blade, excision group. The patient satisfaction score, as well as the
an ordinary razor blade broke in half after sterilization evaluation score by the physician, was comparable in both
can also be used.[3] Homeostasis is achieved by pressure or groups.[8]
electrocautery.
The advantages of this procedure are that it is a simple
procedure with minimal skill required, quick to perform,
does not require suturing, and healing is faster. The
disadvantages are that its use is limited to smaller, elevated
moles, high chances of recurrence as the removal by
this method is superficial and the inadequate sample for
histopathology as the sample obtained is only of the upper
layers of skin. a
In a study of moles treated with shave excision and
electrocautery for homeostasis, at the end of 6–8 months,
46% of head-and-neck nevi had no visible scar and the
remainder had a cosmetically acceptable scar. Regrowth of
hair was seen in 24% of hairy nevi.[4] Recurrence was reported
by Ferrandiz et al. in 19.6% of total 204 cases at 3 months
after shave excision.[5] Lee et al. looked at the effectiveness b
of secondary intention after shave excision of benign tumors Figure 1: (a) A compound melanocytic nevus just above the upper
on lid margins and found it to be safe and effective. Through lip, at baseline. (b) Good results at 6 months after serial excision
healing by secondary intention, a decrease of around 50% is (two sessions of surgical excision and closure).
seen in the size of the defect.[6]
COLD KNIFE EXCISION AND CLOSURE
This method of surgical removal can also be used for all types
of moles.
The RSTLs are noted and an elliptical incision is given with
longitudinal axis along the RSTLs. A single bold incision
with precision is given using the surgical blade number 15 a
mounted on a Bard-Parker handle.[2] The excised part is cut
using scissors ensuring to include a depth till deep dermis to
reduce the chances of recurrences. Adequate undermining is
done; if the excision was done over a bony area or over areas
where the skin is stretched, more undermining is required
so that there is no tension between the sutured margins.
The open ends are sutured in two layers using buried
b
subcutaneous sutures and simple interrupted skin sutures
[Figures 1-3]. Figure 2: (a) A congenital melanocytic nevus at a cosmetically
important site (the tip of the nose), at baseline. (b) Three months
In the hands of an experienced dermatosurgeon, cold knife after serial excision (two sessions of surgical excision and closure)
excision brings the best esthetic results. Furthermore, a has resulted in a cosmetically acceptable scar.
Cosmoderma 2021 • 1(27) | 2
Pangti and Gupta: Removal of moles
a b c
Figure 3: (a) A compound melanocytic nevus on the chin, at baseline. (b) Two months after undergoing first surgical excision of a part of
melanocytic nevus. (c) Right after the second session of surgical excision of the rest of the melanocytic nevus (serial excision).
SERIAL EXCISION dermal part which is removed but the surrounding tapering
part of the nevus (junctional component) is left behind.[11]
For bigger moles, serial excision at conveniently spaced-out
time intervals is the best approach. This brings about reducing To evade the “dog ears” formation after suturing punch
the size of the mole at each procedure while not compromising excisions, Gupta et al. proposed the defect after punch
on the esthetics as every time the incision includes the scarred excision to be filled with a punch graft taken from the
tissue or the suture line from the previous procedure(s). posterior auricular area of the patient. The authors reported
Serial excision is a kind of tissue expansion. Once we excise a superior results with this method.[12]
small area, the tissue is expanded because of its elasticity. This
allows us to carry out the second procedure with much ease RADIOFREQUENCY (RF) EXCISION
and close without tension [Figures 1-3].[9] Another advantage
This method of surgical removal can be used for all types
is serial excision of the mole reduces the loss of normal tissue.
of moles. The initial steps of preparation of the part and
We can, also, remove a round lesion by serially excising it
infiltrative anesthesia are the same as for shave excision. For
without “dog ear” formation. To avoid “dog ear” formation,
smaller and flat moles, surface RF ablation can be done in
the ratio of length and breadth of the incision is kept as 3:1.
which the tip of the RF probe (monopolar in cutting mode) is
touched on the surface of the mole. The power setting of RF
PUNCH EXCISION AND CLOSURE, AND is kept at a lower value to minimize the collateral heating and
PUNCH EXCISION AND PUNCH GRAFTING charring of skin.[13] Subsequently, surface RF ablation can be
Punch excision is ideal for small moles, usually <5 mm done till the dermis.
in diameter. A biopsy punch is chosen according to the For elevated and/or bigger moles, an elliptical incision is
diameter of the mole. made around the whole mole, perpendicular to the RSTLs,
After putting the punch around the mole, the punch is held using the flat RF monopolar probe in cutting mode. The
vertically and rotated gradually in a clockwise direction mole is removed using scissors and undermining is done to
while traction is given in a direction perpendicular to ensure tension-free apposition of the two ends. The defect
the long axis of the RSTLs. The excised part is held with is then closed in two layers, using absorbable sutures for the
forceps and the base cut with scissors. An interrupted inner layer and non-absorbable sutures for closing the skin.
suture or two is put in place using non-absorbable suture Alternatively, the mole removed using an RF probe from
material.[2] Alternatively, the wound can be allowed to heal its base and the wound is allowed to heal with secondary
with secondary intention. intention. The sample can still be sent for histopathology.
The pros of using this method are that it is quick and easy The upside to this procedure is the easy homeostasis using
to perform, not requiring much technique. The cons are the RF probe with the swift switch to the coagulation mode
residual nevus and that closing a round defect after punch in the RF machine. The downside is that cosmetic results may
excision can cause “dog ears” formation. not be great with RF due to the transfer of energy to also the
surrounding area.[13]
Residual nevi were found in 24.9% of reexcision which were
initially shave or punch excised in a study by Cohen et al. LASERS
These residual nevi were more often seen after punch excisions
than with shave excisions.[10] In cases of compound nevi, there Both ablative- and pigment-specific lasers or their
is usually a tapering junctional component with the central combination can be used for removal of acquired
dermal component. Punch excisions take care of the central melanocytic nevi. Er: YAG and CO2 (ablative) lasers have
Cosmoderma 2021 • 1(27) | 3
Pangti and Gupta: Removal of moles
been used with good efficacy in treating moles. Short- Dermatology. 9th ed. Oxford, UK: John Wiley and Sons, Ltd.;
pulsed Er: YAG laser has shown promising results in flat 2016. p. 132.18-21.
and slightly raised moles.[10,13,14] Among pigment-specific 2. Bhide D. Simple dermatosurgical procedures: Biopsy, curettage
lasers, studies using Q-switched alexandrite (755 nm), and chemical cautery. In: Venkataram M, editor. Textbook of
Cutaneous and Aesthetic Surgery. 2nd ed. New Delhi, India:
ruby (694 nm), and Nd: YAG (1064 nm) lasers have
Jaypee Brothers Medical Publishers; 2017. p. 269-73.
shown good results.[11,15,16] Multiple sessions are required,
3. Levy SB. The razor blade in dermatologic practice. Cutis
moles do not get removed completely, and recurrences 1976;17:402.
after treatment are commonly seen. Flat junctional moles 4. Hudson-Peacock MJ, Bishop J, Lawrence CM. Shave excision of
show better response than elevated compound nevi as the benign papular naevocytic naevi. Br J Plast Surg 1995;48:318-22.
junctional part gets removed completely with lasers but the 5. Ferrandiz L, Moreno-Ramirez D, Camacho FM. Shave excision
intradermal part either gets partially treated or recurs. The of common acquired melanocytic nevi: Cosmetic outcome,
disadvantage is that the tissue sample is not available for recurrences, and complications. Dermatol Surg 2005;31:1112-5.
histological confirmation. 6. Lee JM, Lee H, Lee TE, Park M, Baek S. Second intention
healing after shave excision of benign tumors on the lid
margin. Ann Dermatol 2011;23:463-7.
CONCLUSION 7. Tursen U, Kaya TI, Ikizoglu G. Round excision of small,
There is a dearth of scientific literature on the treatment benign, papular and dome-shaped melanocytic nevi on the
face. Int J Dermatol 2004;43:844-6.
options for moles and their comparison as to which treatment
8. Soares AS, Manzoni AP, de Souza CD, Weber MB, Watanabe T,
modality is better than the other. Moles can be easily removed
Camini L. Comparative analysis between sutured elliptical excision
by any of the aforementioned methods. However, it comes and shaving of intradermal melanocytic nevi: A randomized
with a caveat of recurrence after their removal. The choice clinical trial. Surg Cosmetic Dermatol 2016;8:316-20.
of the method of removal of moles is at the discretion of the 9. Arneja JS, Gosain AK. Giant congenital melanocytic nevi of
clinician in terms of availability of the set-up for a particular the trunk and an algorithm for treatment. J Craniofac Surg
option, the skill required for the method, the size, shape, and 2005;16:886-93.
location of the mole, suspicion of malignancy, as well as on 10. Cohen LM, Hodge SJ, Owen LG, Callen JP. Atypical melanocytic
informed choice of the patient. nevi: Clinical and histopathologic predictors of residual tumor
at reexcision. J Am Acad Dermatol 1992;27:701-6.
In case of slightest doubt regarding the diagnosis, it is of 11. Sardana K, Chakravarty P, Goel K. Optimal management
paramount importance that we send the excised part for of common acquired melanocytic nevi (moles): Current
histopathology as moles can resemble few pre-malignant and perspectives. Clin Cosmet Investig Dermatol 2014;7:89-103.
malignant lesions. 12. Gupta S, Handa S, Kumar B, Rai R. Surgical pearl: Punch
excision and grafting for removal of mole. J Am Acad Dermatol
Declaration of patient consent 1999;41:635-7.
13. Pangti R, Dixit A, Gupta S. Bipolar forceps of a high-power
The authors certify that they have obtained all appropriate electrosurgical unit for precise removal of small benign skin
patient consent. lesions. J Am Acad Dermatol 2020;82:e155-6.
14. Baba M, Bal N. Efficacy and safety of the short-pulse erbium:
YAG laser in the treatment of acquired melanocytic nevi.
Financial support and sponsorship
Dermatol Surg 2006;32:256-60.
Nil. 15. Westerhof W, Gamei M. Treatment of acquired junctional
melanocytic naevi by Q-switched and normal mode ruby laser.
Br J Dermatol 2003;148:80-5.
Conflicts of interest
16. Duke D, Byers HR, Sober AJ, Anderson RR, Grevelink JM.
There are no conflicts of interest. Treatment of benign and atypical nevi with the normal-mode
ruby laser and the Q-switched ruby laser: Clinical improvement
but failure to completely eliminate nevomelanocytes. Arch
REFERENCES Dermatol 1999;135:290-6.
1. Stefanaki I, Antoniou C, Stratigos A. Benign melanocytic
proliferations and melanocytic naevi. In: Griffiths CE, Barker J, How to cite this article: Pangti R, Gupta S. Surgical removal of moles.
CosmoDerma 2021;1:27.
Bleiker T, Chalmers R, Creamer D, editors. Rook’s Textbook of
Cosmoderma 2021 • 1(27) | 4
You might also like
- Utilizing Free Skin Grafts in The Repair of Surgical Wounds: Madalene C. Y. HengDocument11 pagesUtilizing Free Skin Grafts in The Repair of Surgical Wounds: Madalene C. Y. HengDefri ChanNo ratings yet
- Acne Scars: Subcision: Methods and TechniquesDocument3 pagesAcne Scars: Subcision: Methods and TechniquesLuiz Henrique CararetoNo ratings yet
- AnnMaxillofacSurg62204-7504388 020504Document6 pagesAnnMaxillofacSurg62204-7504388 020504mascoNo ratings yet
- Removal of Salivary Gland Mucocele Using 980Nm Diode Laser: Case ReportDocument3 pagesRemoval of Salivary Gland Mucocele Using 980Nm Diode Laser: Case Reportmaya morenoNo ratings yet
- Multiple Adjacent Gingival Recessions: Which Technique To Use, Tunnel or Flap?Document8 pagesMultiple Adjacent Gingival Recessions: Which Technique To Use, Tunnel or Flap?oliverglezNo ratings yet
- 2014 Article 1741Document4 pages2014 Article 1741anton suponoNo ratings yet
- Original Article: Farideh Nejat, Nima Baradaran, Mostafa El KhashabDocument4 pagesOriginal Article: Farideh Nejat, Nima Baradaran, Mostafa El KhashabGuz CaemmNo ratings yet
- Subcision 40 PatientsDocument8 pagesSubcision 40 Patientsxj112358No ratings yet
- Modified Rhomboid Flap For Facial ReconstructionDocument3 pagesModified Rhomboid Flap For Facial ReconstructionahujasurajNo ratings yet
- Reconstrucción Defectos Nasales PDFDocument18 pagesReconstrucción Defectos Nasales PDFSara OmNo ratings yet
- Gox 5 E1230Document6 pagesGox 5 E1230Brînduşa CiobanuNo ratings yet
- Biopsy Techniques Diagnosis of Melanoma: Neil A. Swanson, MD, Ken K. Lee, MD, Annalisa Gorman, MD, Han N. Lee, MDDocument4 pagesBiopsy Techniques Diagnosis of Melanoma: Neil A. Swanson, MD, Ken K. Lee, MD, Annalisa Gorman, MD, Han N. Lee, MDdaniel satyoNo ratings yet
- Basal Cell Carcinoma: General FeaturesDocument5 pagesBasal Cell Carcinoma: General FeaturesSel ViaNo ratings yet
- AnnMaxillofacSurg 2020 10 1 182 286169Document5 pagesAnnMaxillofacSurg 2020 10 1 182 286169pratiksha malhotraNo ratings yet
- Reconstruction After Skin Cancer Removal: More Than Just "Filling A Hole"Document2 pagesReconstruction After Skin Cancer Removal: More Than Just "Filling A Hole"irsalinahusnaNo ratings yet
- Carbuncle Excision TechniqueDocument3 pagesCarbuncle Excision TechniquetseeckunNo ratings yet
- Aesth Plast Surg - 2019 - 43 - 652-657Document6 pagesAesth Plast Surg - 2019 - 43 - 652-657HemerobibliotecaHospitalNo ratings yet
- Comparing Cannula Based Subcision With The Common Needle Method: A Clinical TrialDocument7 pagesComparing Cannula Based Subcision With The Common Needle Method: A Clinical Trial郭先薈No ratings yet
- Lembi CutaneiDocument6 pagesLembi CutaneiGianfranco MuntoniNo ratings yet
- Subcision de CicatrizDocument2 pagesSubcision de CicatrizGaviota75No ratings yet
- Basis of Dimple CreationDocument6 pagesBasis of Dimple Creationkusuma rNo ratings yet
- Simple Technique For Facial DimpleDocument4 pagesSimple Technique For Facial DimpleAdi WijayantoNo ratings yet
- Closure of Defects of The Malar Region: Mehmet Mutaf, MD, Ertan Gu Nal, MD, and Metin Temel, MDDocument4 pagesClosure of Defects of The Malar Region: Mehmet Mutaf, MD, Ertan Gu Nal, MD, and Metin Temel, MDgokhanNo ratings yet
- Surgical Eye ProceduresDocument4 pagesSurgical Eye ProceduresLeonela SánchezNo ratings yet
- 5phase II Periodontal TherapyDocument54 pages5phase II Periodontal TherapyKaraz StudiosNo ratings yet
- Art:10.1007/s00266 013 0134 0Document10 pagesArt:10.1007/s00266 013 0134 0FabianaNisanNo ratings yet
- Review Article: Skin GraftDocument6 pagesReview Article: Skin Graftfitri dwi astutiNo ratings yet
- Procedimientos Vulva PDFDocument14 pagesProcedimientos Vulva PDFTheodoraAlinaNo ratings yet
- Surgical Technique For Optimal OutcomesDocument11 pagesSurgical Technique For Optimal OutcomesAndrei EncisoNo ratings yet
- Tilleman 2004Document7 pagesTilleman 2004이호원No ratings yet
- Complications of Strabismus Surgery: DellenDocument14 pagesComplications of Strabismus Surgery: DellenDeny Rahmat PamungkasNo ratings yet
- Fascia Suspension Lift A Facelift Technique Without Skin Excision andDocument10 pagesFascia Suspension Lift A Facelift Technique Without Skin Excision and7rayosomonishangoNo ratings yet
- In Vivo Intraoral Reflectance Confocal Microscopy of An Amalgam TattooDocument4 pagesIn Vivo Intraoral Reflectance Confocal Microscopy of An Amalgam TattooEndah AzNo ratings yet
- Wire Subcision For Complete Release of Depressions, Subdermal Attachments, and ScarsDocument8 pagesWire Subcision For Complete Release of Depressions, Subdermal Attachments, and ScarsLuciano AbbaNo ratings yet
- Anatomy of The Skin and The Pathogenesis of Nonmelanoma Skin CancerDocument4 pagesAnatomy of The Skin and The Pathogenesis of Nonmelanoma Skin CancerariskaNo ratings yet
- Research Microneedling in DermatologyDocument10 pagesResearch Microneedling in DermatologyErik BrooksNo ratings yet
- Incision and DrainageDocument35 pagesIncision and DrainageVilma Delos Reyes100% (1)
- Plastic Surgery: Pablo L. Padilla, Kimberly H. Khoo, Trung Ho, Eric L. Cole, Ramón Zapata Sirvent, Linda G. PhillipsDocument29 pagesPlastic Surgery: Pablo L. Padilla, Kimberly H. Khoo, Trung Ho, Eric L. Cole, Ramón Zapata Sirvent, Linda G. Phillipssportillag1No ratings yet
- Vulvar ProceduresDocument14 pagesVulvar Proceduresjft842No ratings yet
- Bille Et Al 2019Document5 pagesBille Et Al 2019Walid SasiNo ratings yet
- Crawley 2015Document6 pagesCrawley 2015Eduardo HernándezNo ratings yet
- Jurnal Scar RevisionDocument8 pagesJurnal Scar Revisionnurul rezki fitrianiazisNo ratings yet
- Two Advancement Flaps For Eyelid Margin Reconstruction of Small and Medium Defects and A Novel Design To Reduce Ocular InjuryDocument13 pagesTwo Advancement Flaps For Eyelid Margin Reconstruction of Small and Medium Defects and A Novel Design To Reduce Ocular InjuryhilderhNo ratings yet
- Short Scar Rhytidectomy Tech 2014 Atlas of The Oral and Maxillofacial SurgerDocument16 pagesShort Scar Rhytidectomy Tech 2014 Atlas of The Oral and Maxillofacial Surgerlaljadeff12No ratings yet
- Efficacy of Microneedling With 70% Glycolic Acid PeelDocument6 pagesEfficacy of Microneedling With 70% Glycolic Acid PeelHanna NabilaNo ratings yet
- Djohan2010bening&malignan TumorDocument13 pagesDjohan2010bening&malignan Tumorkiki0% (1)
- A Safe Nonsurgical Rhinoplasty ProcedureDocument5 pagesA Safe Nonsurgical Rhinoplasty ProcedureKerlida SantosNo ratings yet
- Jkms 29 751 PDFDocument7 pagesJkms 29 751 PDFalexander nezwyNo ratings yet
- Rugas de Acordeon 2012Document10 pagesRugas de Acordeon 2012Dr. Frederico NevesNo ratings yet
- Artificial Neural Network For Skincancer DetectionDocument7 pagesArtificial Neural Network For Skincancer DetectionInternational Journal of Application or Innovation in Engineering & ManagementNo ratings yet
- Descemet Membrane Detachment During Cataract Surgery: Etiology and ManagementDocument7 pagesDescemet Membrane Detachment During Cataract Surgery: Etiology and Managementjorge vegaNo ratings yet
- Mingival Curettage PDFDocument52 pagesMingival Curettage PDFheycoolalexNo ratings yet
- Capítulo 10 SerdevDocument19 pagesCapítulo 10 SerdevErik BrooksNo ratings yet
- Oralmucocele AcasereportDocument5 pagesOralmucocele AcasereportxxxNo ratings yet
- 64 - Skin TumorsDocument20 pages64 - Skin TumorsAlexa GabrielaNo ratings yet
- Sadick 2018Document13 pagesSadick 2018IrsalinaHusnaAzwirNo ratings yet
- Unique Clinical Aspects of Nasal ScarringDocument10 pagesUnique Clinical Aspects of Nasal ScarringKerlida SantosNo ratings yet
- DM2022 8705436Document6 pagesDM2022 8705436MufassiraturrahmahNo ratings yet
- Oculoplastic Surgery: A Practical Guide to Common DisordersFrom EverandOculoplastic Surgery: A Practical Guide to Common DisordersEssam A. El ToukhyNo ratings yet
- Sandeep Kodali ppk-2Document6 pagesSandeep Kodali ppk-2kahkashanahmed065No ratings yet
- DownloadDocument9 pagesDownloadkahkashanahmed065No ratings yet
- DIR Summer 2023 BF Atypical FibroxanthomaDocument2 pagesDIR Summer 2023 BF Atypical Fibroxanthomakahkashanahmed065No ratings yet
- Facial Anatomy and The Application of Fillers andDocument12 pagesFacial Anatomy and The Application of Fillers andkahkashanahmed065No ratings yet
- AAD BF Chemotherapy Specific Cutaneous ReactionsDocument3 pagesAAD BF Chemotherapy Specific Cutaneous Reactionskahkashanahmed065No ratings yet
- Quiz Review Exam ETASDocument183 pagesQuiz Review Exam ETASkahkashanahmed065No ratings yet
- AAD BF Head and Neck Lesions InfantDocument2 pagesAAD BF Head and Neck Lesions Infantkahkashanahmed065No ratings yet
- AAD BF Non TB Cutaneous Mycobact InfectionsDocument3 pagesAAD BF Non TB Cutaneous Mycobact Infectionskahkashanahmed065No ratings yet
- AAD BF Paisley Tie DiagnosisDocument2 pagesAAD BF Paisley Tie Diagnosiskahkashanahmed065No ratings yet
- DIR Fall 2023 BF Ticks ONLINEDocument3 pagesDIR Fall 2023 BF Ticks ONLINEkahkashanahmed065No ratings yet
- AAD BF Retinoid Biology 2Document2 pagesAAD BF Retinoid Biology 2kahkashanahmed065No ratings yet
- Female Androgenetic Alopecia A Risk Factor For.4Document6 pagesFemale Androgenetic Alopecia A Risk Factor For.4kahkashanahmed065No ratings yet
- RoutledgesManualofEtiquette 10001646Document264 pagesRoutledgesManualofEtiquette 10001646kahkashanahmed065No ratings yet
- AAD BF Bones Eyes NailsDocument5 pagesAAD BF Bones Eyes Nailskahkashanahmed065No ratings yet
- AAD BF Herbal Supplements in DermatologyDocument2 pagesAAD BF Herbal Supplements in Dermatologykahkashanahmed065No ratings yet
- AAD BF Cutaneous Mycobact Infections PDFDocument3 pagesAAD BF Cutaneous Mycobact Infections PDFkahkashanahmed065No ratings yet
- AAD BF Cutaneous Manifestations of HIV InfectionsDocument2 pagesAAD BF Cutaneous Manifestations of HIV Infectionskahkashanahmed065No ratings yet
- Etas 2022-1Document1,135 pagesEtas 2022-1kahkashanahmed065No ratings yet
- AAD BF HistiocytosisDocument2 pagesAAD BF Histiocytosiskahkashanahmed065No ratings yet
- Public Gdcmassbookdig Standardbookofet00ster Standardbookofet00sterDocument264 pagesPublic Gdcmassbookdig Standardbookofet00ster Standardbookofet00sterkahkashanahmed065No ratings yet
- IJD - Volume 1 - Issue 2 - Pages 22-23Document2 pagesIJD - Volume 1 - Issue 2 - Pages 22-23kahkashanahmed065No ratings yet
- Genetic Disorders of PigmentationDocument58 pagesGenetic Disorders of Pigmentationkahkashanahmed065No ratings yet
- NarmadhadeviDocument127 pagesNarmadhadevikahkashanahmed065No ratings yet
- Telltale Signs of Skin Trespassers - Clues To Superficial MycosisDocument5 pagesTelltale Signs of Skin Trespassers - Clues To Superficial Mycosiskahkashanahmed065No ratings yet
- 5CC 2020 Virtual Conference Program PDFDocument29 pages5CC 2020 Virtual Conference Program PDFhuyenthanh1807No ratings yet
- MO DermatologyDocument2 pagesMO DermatologyMohamed AbbasNo ratings yet
- 10 1016@j Det 2018 05 008Document8 pages10 1016@j Det 2018 05 008Renata GoulartNo ratings yet
- Basics of Skin Lesions EntranceDocument22 pagesBasics of Skin Lesions EntranceMohammed AsifNo ratings yet
- 382 EHS Hospitals ListDocument39 pages382 EHS Hospitals ListRams RamsNo ratings yet
- 29 TB TTHL Danh Muc Sach Ngoai Van Tham KhaoDocument134 pages29 TB TTHL Danh Muc Sach Ngoai Van Tham Khaojames18b5No ratings yet
- Scott Hannah cr1Document2 pagesScott Hannah cr1api-568558610No ratings yet
- Synopsis RguhsDocument6 pagesSynopsis RguhsahmedNo ratings yet
- Camouflage Therapy: Victoria L. RaynerDocument4 pagesCamouflage Therapy: Victoria L. RaynerTushar SoniNo ratings yet
- J Deutsche Derma Gesell - 2014Document6 pagesJ Deutsche Derma Gesell - 2014silviaNo ratings yet
- Neonatal Skin Disorders and The Emergency Medicine Physician PDFDocument10 pagesNeonatal Skin Disorders and The Emergency Medicine Physician PDFsamerdkhNo ratings yet
- 3 Case Report Geographic Tongue Haritsa BudimanDocument10 pages3 Case Report Geographic Tongue Haritsa Budimanharitsa budimanNo ratings yet
- Daftar Obat Dari BG DeniDocument19 pagesDaftar Obat Dari BG DeniRizki TriwijayaNo ratings yet
- Pityriasis Alba Pityriasis AlbaDocument11 pagesPityriasis Alba Pityriasis AlbaSSGeaNo ratings yet
- Dermatology Revision E6.5 'Document35 pagesDermatology Revision E6.5 'Riya SharmaNo ratings yet
- Classification of LeprosyDocument65 pagesClassification of Leprosycharmaine_olivia_1No ratings yet
- Scabies Home Remedies Treatment and ImagesDocument3 pagesScabies Home Remedies Treatment and ImagesIyan DwiNo ratings yet
- PL NaavenDocument1 pagePL Naavendhesi.ulandhariNo ratings yet
- Traumatic InjuriesDocument45 pagesTraumatic Injuriesibrahim bataNo ratings yet
- Derma ReviewerDocument22 pagesDerma ReviewerAlyssandra LucenoNo ratings yet
- Blushing in Black Skin: F I D Konotey-AhuluDocument2 pagesBlushing in Black Skin: F I D Konotey-AhuluEllaNo ratings yet
- Hailey Hailey DiseaseDocument3 pagesHailey Hailey DiseaseFeby SintiaNo ratings yet
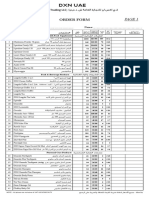
- DXN UaeDocument2 pagesDXN Uaeعبيدة علي (OB)No ratings yet
- 4 StagesDocument2 pages4 StagesCandice Maureen Riconalla-ChanNo ratings yet
- L3 15 Aug 23Document13 pagesL3 15 Aug 23anjis pisanNo ratings yet
- Harvard Referencing: Guide: (Please Note: This Document Was Downloaded From Citethisforme Web Tool, URL )Document13 pagesHarvard Referencing: Guide: (Please Note: This Document Was Downloaded From Citethisforme Web Tool, URL )Benjamin K JaravazaNo ratings yet
- Perioral Dermatitis SlideDocument19 pagesPerioral Dermatitis Slidekacaacdhgjhlk100% (1)
- TINEA CORPORIS InggrisDocument2 pagesTINEA CORPORIS Inggrisal filaNo ratings yet
- Hydrocortisone 0.5% and 1.0% CreamDocument2 pagesHydrocortisone 0.5% and 1.0% CreamHardiyanti banduNo ratings yet
- Bullous DiseasesDocument19 pagesBullous DiseasesVicky Ilda ViantiniNo ratings yet